Abstract
Background:
Mallet finger is a common injury involving a detachment of the terminal extensor tendon from the distal phalanx. This injury is usually treated with immobilization in a cast or splint. The purpose of this study is to compare outcomes of mallet fingers treated with either a cast (Quickcast) or a traditional thermoplastic custom-fabricated orthosis.
Methods:
Our study was a prospective, assessor-blinded, single-center randomized clinical trial of 58 consecutive patients with the diagnosis of bony or soft tissue mallet finger treated with immobilization. Patients were randomized to either an orfilight thermoplastic custom-fabricated orthosis or a Quickcast orthosis. Patients were evaluated at 3, 6, and 10 weeks for bony and 4, 8, and 12 weeks for soft tissue mallets. Skin complications, pain with orthosis, compliance, need for surgical intervention, and extensor lag were compared between the 2 groups.
Results:
Both bony and soft tissue mallet finger patients experienced significantly less skin complications (33% vs 64%) and pain (11.2 vs 21.6) when using Quickcast versus an orfilight thermoplastic custom-fabricated orthosis. The soft tissue mallet group revealed a greater difference in pain, favoring Quickcast (6.2 vs 22). No significant difference in final extensor droop or need for secondary surgery was found between the 2 groups.
Conclusions:
Quickcast immobilization for the treatment of mallet finger demonstrated fewer skin complications and less pain compared with orfilight custom-fabricated splints.
Keywords: mallet finger, extension splinting, tendinous mallet finger, swan-neck deformity, extensor droop
Introduction
Mallet finger is a common hand injury involving a detachment of the terminal extensor tendon from the distal phalanx. 1 Tendon injuries range from partial to complete. When there is an avulsion fracture of the distal phalanx at the point of tendon attachment, the injury is termed a bony mallet finger, whereas a pure tendon avulsion is termed a soft tissue mallet. 1 The injury is thought to result from eccentric loading, where an external flexion force is applied to an extended distal interphalangeal (DIP) joint, or can occur due to a laceration on the dorsal aspect of the finger.1,2
Management of mallet finger is generally nonsurgical for most closed bony and soft tissue mallet injuries using finger-based orthoses. 3 Surgical intervention is reserved for open and chronic mallet finger cases or for those involving a large avulsion fragment or joint subluxation. Splint treatment has been associated with complications, including skin ulceration, nail deformity, failure of tendon reattachment, and pain.4,5 Splint treatment is also associated with an average residual extensor lag of 7.6°. 6
The best type of orthosis for the treatment of mallet finger remains unclear. 7 The purpose of this study was to compare immobilization efficacy using an orfilight thermoplastic custom-fabricated orthosis (TCFO) versus a Quickcast (QC; Quickcast Preston Medical, Warrenville, Illinois) for nonoperative management of acute soft and bony mallet injuries. We hypothesized that immobilization with QC would result in fewer skin complications, decreased pain, higher patient compliance, and decreased extensor lag compared with an orfilight TCFO.
Materials and Methods
A prospective, assessor-blinded, single-center randomized clinical trial was conducted on patients with the diagnosis of acute bony mallet or soft tissue mallet finger treated with immobilization. Our institution’s ethics committee approved the study prior to initiation. Inclusion criteria included age greater than 18 years, closed injury, date of injury less than 12 weeks prior to initiation of the study, and no other associated injuries of the affected hand. Eligible patients also had intact skin at the first encounter. Exclusion criteria included patients with severe osteoarthritis of the affected finger, mallet thumb, history of prior surgery, a fracture fragment size involving more than one-third of DIP joint articular surface, those unable to read or comprehend written instruction, and those who declined participation in the study. All patients gave informed consent prior to the start of the study.
Patients were randomized to either an orfilight TCFO (Figure 1) or a QC orthosis (Figure 2) made by certified hand therapists at our institution. Of note, QC is composed of fiberglass material that is fabric coated with a polymer that is temperature-sensitive. Quickcast can be placed directly onto skin without padding. Hand therapists received training on how to apply both the orfilight TCFO and QC orthosis prior to the start of the study, and this was standardized. Patients were randomized using a computer randomization program that assigned them to number 0 or 1 for QC versus TCFO, respectively. Patients were grouped for analysis as follows: QC for soft tissue mallets, TCFO for soft tissue mallets, QC for bony mallets, and TCFO for bony mallets.
Figure 1.

The orfilight thermoplastic custom-fabricated orthosis.
Figure 2.

The Quickcast orthotic.
Patients with bony mallet injuries were treated for 6 weeks using full-time immobilization followed by 4 weeks of night-only splinting. The soft tissue mallet group was treated with full-time immobilization for 8 weeks followed by 4 weeks of night-only splinting. The timing of immobilization was established using existing guidelines. 3 Immobilization position was zero degrees or slight hyperextension at the DIP joint for both groups. During full-time immobilization, the TCFO group was directed to wear the splint 24 hours per day, 7 days per week, with the only exception being for skin care, which included washing their hand at their discretion. They were instructed to support their DIP joint in hyperextension when the orthosis was off. The participants documented the frequency of TCFO removal.
Conversely, the QC group, during the full-time wear period, was instructed to wear the cast full-time without exception and to report to free-of-charge weekly visits for cast changes performed by the same therapists. Skin washing of the finger for the QC group was performed during the cast changes. The weekly QC refitting aided in assuring a consistent appropriate tight fit as edema decreased; meanwhile, the TCFO group did not require these extra visits as they were trained on how to keep the splint fitted via velcro strap adjustments.
Patients were followed at 3, 6, and 10 weeks for bony and 4, 8, and 12 weeks for soft tissue mallet injuries. Skin complications, pain, patient compliance, and extensor lag at final follow-up were recorded and compared between the 2 groups. The treating surgeon was blinded to the type of immobilization used during the entire study. On the day of physician follow-up visits, patients would first see the hand therapist who would remove their orthosis prior to seeing the physician. Both the patient and the treating physicians filled evaluation forms at each visit.
Patient evaluation forms included questions on skin appearance, pain, perceived finger position, orthotic care, and wear pattern. Skin appearance used a 3-point Likert scale, with 0 representing intact skin; 1, minor irritation; and 2, significant irritation. For pain, a numerical rating scale ranging from 0 to 100 was used, where 100 represented the worst pain possible and 0 represented no pain. Finger position was rated using a 5-point Likert scale consisting of perfect, minimally bent, bent, very much bent, or unacceptable. Orthotic care was rated using a 5-point Likert scale (no hassle, minimal burden, moderate burden, very difficult, or unacceptable) and encompassed the following criteria: wearing the cast or splint, attending weekly adjustment visits, and ability to keep orthosis clean. A scale was used to describe wear pattern (never took it off, took it off once or twice, occasionally off, or mostly off). Of note, the questionnaire forms were assessed for readability and comprehension by patients prior to the start of the study.
Physician forms included questions on skin appearance, finger posture, and a patient complaint section. Finger posture was measured in degrees using a goniometer and was recorded using the following scale: 0° representing no extension lag and 5°, 10°, 15°, 20°, 25°, 30°, 35°, and >40° representing extension lag or swan-neck deformity at each follow-up visit. Participants were seen and assessed by the same physician at every follow-up. Both groups received instructions to begin night-only immobilization for the last 4 weeks of the study using a prefabricated splint. Final finger posture was assessed after the completion of both continuous immobilization and night splinting for both groups.
Statistical Analysis
The Fisher exact test was used for categorical data, and the Student t test was used for continuous variables. Significance was set at P < .05. An a priori power analysis based on a repeated-measures study comparing factors between groups, predicated on 80% power and α of 0.05, determined that a total of 52 patients were needed, with 13 in each subgroup. Other assumptions were that the group membership contributed 16% of the overall variance, and the correlation between successive measurements for the same patient was 0.5.
Results
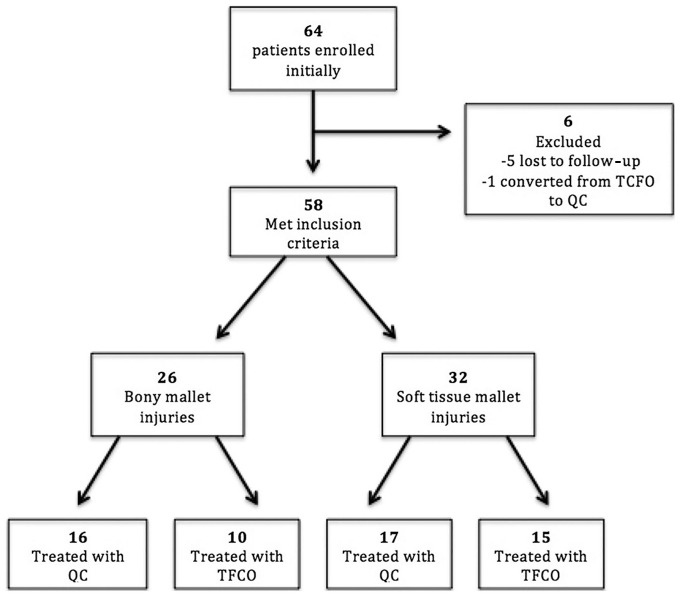
A total of 64 patients were initially enrolled in the study. In this group, 5 patients were lost to follow-up, and 1 patient was converted from orfilight TCFO to QC after the first follow-up due to poor orthotic fit and patient preference (Figure 3). There were 23 women and 35 men with a mean age of 50.1 years (range = 21-74 years).
Figure 3.
Participant inclusion/exclusion flowchart illustrating process of patient selection and final groups.
Note. TCFO = thermoplastic custom-fabricated orthosis; QC = Quickcast.
Patient survey data (Table 1) revealed substantially less skin complications (minor and significant irritation) in patients that were treated with QC compared with TCFO (P = .03), regardless of whether it was a bony (Table 2) or soft tissue (Table 3) mallet injury. The QC group also experienced significantly less pain compared with patients treated with TCFO (P = .02). Furthermore, a subgroup analysis of the soft tissue mallet group resulted in an even greater difference in pain perceived, favoring QC over TCFO (P = .01). There were no significant differences found between the use of QC and TCFO regarding cast/splint care difficulty (P = .29) and wear pattern (P = .23). Moreover, there was no significant difference in final extensor lag between the QC and TCFO groups (P = .20).
Table 1.
Outcomes of QC Versus TCFO.
| QC |
TCFO |
P value | |
|---|---|---|---|
| n = 33 | n = 25 | ||
| Type, No. (%) | .706 | ||
| Bony mallet | 16 (48.5) | 10 (40.0) | |
| Soft mallet | 17 (51.5) | 15 (60.0) | |
| Skin complications, No. (%) | .03 | ||
| Intact | 22 (66.7) | 9 (36.0) | |
| Minor irritation | 11 (33.3) | 16 (64.0) | |
| Significant irritation | 0 (0) | 0 (0) | |
| Pain (mean score) | 11.2 | 21.6 | .02 |
| Splint cast care, No. (%) | .29 | ||
| No hassle | 9 (27.3) | 2 (8.00) | |
| Minimal burden | 20 (60.6) | 21 (84.0) | |
| Moderate burden | 4 (12.1) | 2 (8.00) | |
| Very difficult | 0 (0) | 0 (0) | |
| Unacceptable | 0 (0) | 0 (0) | |
| Wear pattern, No. (%) | .23 | ||
| Never off | 14 (42.4) | 6 (24.0) | |
| Once/twice off | 11 (33.3) | 11 (44.0) | |
| Occasionally off | 7 (21.2) | 7 (28.0) | |
| Mostly off | 1 (3.03) | 1 (4.00) | |
| Final finger posture, No. (%) | .20 | ||
| P | 12 (36.4) | 5 (20.0) | |
| MN | 18 (54.5) | 16 (64.0) | |
| B | 2 (6.06) | 3 (12.0) | |
| VB | 1 (3.03) | 1 (4.00) | |
| U | 0 (0%) | 0 (0) | |
| Physician survey data, No. (%) | |||
| Skin | .43 | ||
| Intact | 30 (90.9) | 21 (84.0) | |
| Minor irritation | 3 (9.09) | 4 (16.0) | |
| Significant irritation | 0 (0) | 0 (0) | |
| Final mean extensor lag, deg | 5.24 | 6.94 | .15 |
| Patient complaint, No. (%) | .24 | ||
| No | 28 (84.8) | 19 (76.0) | |
| Yes | 5 (15.2) | 6 (24.0) | |
Note. QC = Quickcast; TCFO = thermoplastic custom-fabricated orthosis; P = perfect; MN = minimally bent; B = bent; VB = very bent; U = unacceptable.
Table 2.
Outcomes of QC Versus TCFO for Soft Tissue Mallet Injuries.
| QC |
TCFO |
P value | |
|---|---|---|---|
| n = 17 | n = 15 | ||
| Skin complications, No. (%) | .08 | ||
| Intact | 13 (76.5) | 6 (40.0) | |
| Minor irritation | 4 (23.5) | 9 (60.0) | |
| Significant irritation | 0 (0) | 0 (0) | |
| Pain (mean score) | 6.2 | 22 | .01 |
| Splint cast care, No. (%) | .21 | ||
| No hassle | 5 (29.4) | 1 (6.67) | |
| Minimal burden | 11 (64.7) | 13 (86.7) | |
| Moderate burden | 1 (5.88) | 1 (6.67) | |
| Very difficult | 0 (0) | 0 (0) | |
| Unacceptable | 0 (0) | 0 (0) | |
| Wear pattern, No. (%) | .51 | ||
| Never off | 7 (41.2) | 4 (26.7) | |
| Once/twice off | 8 (47.1) | 6 (40.0) | |
| Occasionally off | 1 (5.88) | 4 (26.7) | |
| Mostly off | 1 (5.88) | 1 (6.67) | |
| Final finger posture, No. (%) | .31 | ||
| P | 7 (41.2) | 3 (20.0) | |
| MN | 9 (52.9) | 8 (53.3) | |
| B | 1 (5.88) | 3 (20.0) | |
| VB | 0 (0.00) | 1 (6.67) | |
| U | 0 (0) | 0 (0) | |
| Physician survey data, No. (%) | |||
| Skin | .65 | ||
| Intact | 15 (88.2) | 12 (80.0) | |
| Minor irritation | 2 (11.8) | 3 (20.0) | |
| Final mean extensor lag, deg | 6.06 | 10.31 | .07 |
| Patient complaint, No. (%) | .42 | ||
| No | 14 (82.4) | 10 (66.7) | |
| Yes | 3 (17.6) | 5 (33.3) | |
Note. QC = Quickcast; TCFO = thermoplastic custom-fabricated orthosis; P = perfect; MN = minimally bent; B = bent; VB = very bent; U = unacceptable.
Table 3.
Outcomes of QC Versus TCFO for Bony Mallet Injuries.
| QC |
TCFO |
P value | |
|---|---|---|---|
| n = 16 | n = 10 | ||
| Skin complications, No. (%) | .25 | ||
| Intact | 9 (56.2) | 3 (30.0) | |
| Minor irritation | 7 (43.8) | 7 (70.0) | |
| Significant irritation | 0 (0) | 0 (0) | |
| Pain (mean score) | 16.6 | 21.0 | .46 |
| Splint cast care, No. (%) | .51 | ||
| No hassle | 4 (25.0) | 1 (10.0) | |
| Minimal burden | 9 (56.2) | 8 (80.0) | |
| Moderate burden | 3 (18.8) | 1 (10.0) | |
| Very difficult | 0 (0) | 0 (0) | |
| Unacceptable | 0 (0) | 0 (0) | |
| Wear pattern, No. (%) | .27 | ||
| Never off | 7 (43.8) | 2 (20.0) | |
| Once/twice off | 3 (18.8) | 5 (50.0) | |
| Occasionally off | 6 (37.5) | 3 (30.0) | |
| Mostly off | 0 (0) | 0 (0) | |
| Final finger posture, No. (%) | .87 | ||
| P | 5 (31.2) | 2 (20.0) | |
| MN | 9 (56.2) | 8 (80.0) | |
| B | 1 (6.25) | 0 (0.00) | |
| VB | 1 (6.25) | 0 (0.00) | |
| U | 0 (0) | 0 (0) | |
| Physician survey data, No. (%) | |||
| Skin | .98 | ||
| Intact | 15 (93.8) | 9 (90.0) | |
| Minor irritation | 1 (6.25) | 1 (10.0) | |
| Significant irritation | 0 (0) | 0 (0) | |
| Final mean extensor lag, deg | 4.38 | 5.30 | .49 |
| Patient complaint, No. (%) | .94 | ||
| No | 14 (87.5) | 9 (90.0) | |
| Yes | 2 (12.5) | 1 (10.0) | |
Note. QC = Quickcast; TCFO = thermoplastic custom-fabricated orthosis; P = perfect; MN = minimally bent; B = bent; VB = very bent; U = unacceptable.
The physician survey data demonstrated no significant difference between QC and TCFO regarding skin complications (P = .43), patient complaints (P = .24), or final extensor lag (P = .15) (Table 1).
Discussion
Closed soft tissue and bony mallet finger injuries are common and usually treated nonoperatively with orthosis immobilization of the DIP joint. 7 Quickcast immobilization was associated with less orthotic-related pain and fewer skin complications compared with an orfilight TCFO. Studies have demonstrated that improper application, early removal, or noncompliance with full-time orthosis use can result in a significant extension lag, swan-neck deformity, and DIP joint osteoarthritis.3,8-10 Prefabricated extension splints do not fit every patient equally. Orfilight splints can be thick and bulky, limiting ventilation, comfort, and ease of wear. Quickcast, which is thinner and more porous, may be more comfortable and breathable while still allowing for custom molding.
Our study found significantly fewer patient-rated skin complications in the QC group compared with the orfilight TCFO group. This may be due to QC’s ability to more thoroughly wrap around a finger providing superior compression and thus better edema control. Avoiding substantial edema is important, as excessive edema has demonstrated to be detrimental to wound healing through decrease in blood flow. 9 Similarly, a randomized trial comparing QC and a thermoplastic splint found less edema with QC at the end of the immobilization period and a significant association between amount of edema and final DIP joint extension. 10 Moreover, less edema likely contributed to fewer additional skin complications such as ulceration and irritation, which are more likely to occur if an orthosis fits inappropriately.
Orthosis-related skin complications could lead to decrease in compliance. Poor patient compliance in nonoperative mallet finger treatment has been noted as a main drawback that often leads to poor results. 11 Prefabricated extension orthotics do not fit every patient equally, so having a customizable option is ideal. Although both QC and orfilight TCFO are custom-fit, we believe that the porosity of QC helps decrease moisture that can help decrease the incidence of skin issues, especially maceration. Furthermore, material differences may have played a role in fewer skin complications, favoring QC; however, there are no studies that have made this comparison, so this is an area for future study. Experiencing lower skin complications during immobilization can subsequently improve patient compliance and therefore increase treatment success.
Both the soft tissue and bony mallet groups experienced significantly less pain with QC compared with TCFO use. The ability to obtain a more personalized fit with QC may explain the lower discomfort associated with its wear. In addition, the QC group had a new cast made by a therapist weekly, which provides several opportunities for addressing orthosis fit issues that may not as easily be fixed with thermoplastic orthosis.
It is logical to consider that management and outcomes for soft tissue and bony mallet injuries may differ. However, most studies investigating nonsurgical management of mallet injuries included either 1 or both bony and tendinous injuries combined. Therefore, our randomized controlled trial (RCT) study is unique in that it compares QC with a traditional orthotic that includes a subgroup analysis of bony and soft tissue injuries. This analysis revealed that the soft tissue group showed an even greater difference in perceived pain, favoring QC. Acute bony injuries may lead to more edema and pain compared with tendinous injuries possibly blunting some of the benefits of using QC versus a thermoplastic orthosis. Another possibility is that our study did not have enough power to identify the significant additional difference in pain in the bony mallets, as there were fewer patients in that group compared with the tendinous group.
Both the QC and orfilight TCFO groups showed no statistically significant differences in orthosis ease of use and care. Using wear pattern as a surrogate for compliance, our study did not show significant differences in compliance with TCFO compared with QC immobilization in both the bony and soft tissue mallet groups.
We found greater final extension lags with orfilight TCFO immobilization in both soft tissue and bony mallet injuries. Patients treated with QC had a mean extensor lag of 5.2°, whereas patients treated with TCFO had a mean extensor lag of 6.9°. However, this difference did not reach statistical significance potentially due to a small sample size. Moreover, our subgroup analysis found that the soft tissue QC group ended up with a lower mean extensor lag compared with the TCFO group, which almost reached significance. Furthermore, in all groups, the patients with the greatest final extension lag (>40°) belonged to the soft tissue TCFO group. In an RCT by Tocco and colleagues using QC in a similar setting, a lower mean extensor lag for patients treated with QC patients compared with a thermoplastic splint was found (approximately <5° vs 9°, respectively); this finding also fell short of reaching statistical significance (P = .05). 10 Even though significance was not reached in our study, this suggests that, when using final extensor lag as a surrogate for treatment success, both bony and soft tissue mallet injuries may more successfully be treated using a QC, and this benefit is even more significant when treating the latter group. These findings suggest that experiencing less orthosis-associated pain and skin complications may be significant factors in increasing patient compliance. In this study, patients with final extensor lag of greater than 40° were not fully compliant with orthosis wear and noted pain with orthotic. Additional randomized controlled studies with larger study groups are needed to further expand on these findings.
Our findings expand on the study by Tocco et al, 10 the only other randomized study comparing QC with a thermoplastic splint. This study included a total of 57 cases of acute soft tissue and bony mallet injuries. They looked at DIP joint extensor lag, treatment success, edema, hand function, and complications. Although they found less edema with QC, no statistically significant differences between orthosis type were found. In our study with a larger cohort, soft tissue and bony mallets were separated into subgroups, and we did find statistically significant fewer skin complications and less pain, favoring QC. In addition, we also compared orthotic ease of care and wear pattern and determined no significant differences.
There were some limitations to our study. Although we had one of the largest randomized studies to date comparing mallet immobilization treatments, we still had a relatively small sample. Second, we only included acute mallet injuries; however, there may be little clinical relevance of focusing on the conservative treatment for chronic mallet fingers as they are typically treated surgically. 12 Third, although therapists received training in QC application prior to the study, most therapists likely demonstrated a learning curve while they perfected their casting method. This learning curve could have led to less comfortable QC orthotics early in the study. However, no imbalance of negative QC results in the beginning of our study was found to suggest that therapist experience played a significant role in our results. Equivalent therapist or orthotist training may limit the potential to extrapolate these results elsewhere. Another potential limitation may have been the required weekly therapy visits for casting change for the QC group. Weekly visits can be seen as inconvenient and can potentially negatively affect satisfaction with treatment; however, this was not observed in our study. The opposite may be true; the QC group received more face-to-face interaction, which may have led to better wear patterns due to unintended reinforcement of wear requirements by therapists as they were not to provide additional instructions during those visits. In addition, although the weekly visits for the QC group were free of charge in our study, this may not be a realistic option in other practices. Therefore, studying the associated cost could be an area of further analysis for future larger studies. This study may have also been prone to the Hawthorne effect, which refers to behavioral changes among participants when they know they are being observed. 13 However, this bias likely affected both the QC and the TCFO groups equally as both were followed closely throughout the study, likely leading to an overall higher trial compliance. Finally, this was a single institution study, which may affect generalizability of the results.
Conclusion
Our findings demonstrate that mallet finger immobilization using QC compared with a more traditional orfilight TCFO is associated with fewer skin complications and less orthotic-related pain. Pain and skin complications may have had a more significant impact on compliance than do other factors. Overall, QC immobilization for the treatment of acute soft tissue and bony mallet fingers seems to be more comfortable and is associated with fewer skin complications than a prefabricated orthotic likely due to its lighter fit and less reactivity toward skin, subsequently keeping patients more compliant with its use.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. There were no animal subjects involved in this study.
Statement of Informed Consent: All patients enrolled in the study gave informed consent to participate, and no identifying factors were used.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Priscilla K. Cavanaugh  https://orcid.org/0000-0001-6808-3437
https://orcid.org/0000-0001-6808-3437
Cynthia Watkins  https://orcid.org/0000-0003-1740-4696
https://orcid.org/0000-0003-1740-4696
Christopher Jones  https://orcid.org/0000-0003-1478-489X
https://orcid.org/0000-0003-1478-489X
References
- 1. Baratz ME, Schmidt CC, Hughes TB. Extensor tendon injuries. In: Green DP, Pederson WC, Hotckiss RN, et al., eds. Green’s Operative Hand Surgery. 5th ed. Edinburgh, Scotland: Churchill Livingstone; 2005:187-217. [Google Scholar]
- 2. Yeh PC, Shin SS. Tendon ruptures: mallet, flexor digitorum profundus. Hand Clin. 2012;28:425-430. [DOI] [PubMed] [Google Scholar]
- 3. Smit JM, Beets MR, Zeebregts CJ, et al. Treatment options for mallet finger: a review. Plast Reconstr Surg. 2010;126(5): 1624-1629. [DOI] [PubMed] [Google Scholar]
- 4. Lester B, Jeong GK, Perry D, et al. A simple effective splinting technique for the mallet finger. Am J Orthop. 2000;29:202-206. [PubMed] [Google Scholar]
- 5. Stern PJ, Kastrup JJ. Complications and prognosis of treatment of mallet finger. J Hand Surg Am. 1988;13:329-334. [DOI] [PubMed] [Google Scholar]
- 6. Lin JS, Samora JB. Surgical and nonsurgical management of mallet finger: a systematic review. J Hand Surg Am. 2018;43(2):146-163. [DOI] [PubMed] [Google Scholar]
- 7. Geyman JP, Fink K, Sullivan SD. Conservative versus surgical treatment of mallet finger: a pooled quantitative literature evaluation. J Am Board Fam Pract. 1998;11(5): 382-390. [DOI] [PubMed] [Google Scholar]
- 8. Bachoura A, Ferikes AJ, Lubahn JD. A review of mallet finger and jersey finger injuries in the athlete. Curr Rev Musculoskelet Med. 2017;10:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Villeco JP, Mackin EJ, Hunter JM. Edema: therapist’s management. In: Hunter JM, Mackin EJ, Callahan AD, eds. Rehabilitation of the Hand: Surgery and Therapy. 5th ed. St. Louis, MO: Mosby; 2002:183-193. [Google Scholar]
- 10. Tocco S, Boccolari P, Landi A, et al. Effectiveness of cast immobilization in comparison to the gold-standard self-removal orthotic intervention for closed mallet fingers: a randomized clinical trial. J Hand Ther. 2013;26:191-201. [DOI] [PubMed] [Google Scholar]
- 11. Salazar Botero S, Hidalgo Diaz JJ, Benaïda A, et al. Review of acute traumatic closed mallet finger injuries in adults. Arch Plast Surg. 2016;43(2):134-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Suzuki T, Iwamoto T, Sato K. Surgical treatment for chronic tendon mallet injury. J Hand Surg Am. 2018;43(8):780.e1-780.e5. [DOI] [PubMed] [Google Scholar]
- 13. Chen LF, Vander Weg MW, Hofmann DA, et al. The Hawthorne effect in infection prevention and epidemiology. Infect Control Hosp Epidemiol. 2015;36(12):1444-1450. [DOI] [PubMed] [Google Scholar]