Abstract
Background:
Surgical excision for postaxial polydactyly type B is advocated to avoid long-term complications. Excision with local anesthesia (LA) in infancy represents a safe and effective treatment for this condition, although general anesthesia (GA) is employed by many surgeons. We present a comparison of surgical outcomes, cost, and time between LA and GA to support widespread change in management.
Methods:
A retrospective review of patients under 12 months of age undergoing surgical polydactyly excision by a single surgeon was performed. Anesthesia type, patient demographics, and complications were recorded. Comparisons were made between LA and GA groups on procedure cost, operating time, length of stay (LOS), and time from procedure end to discharge. Stepwise forward regression was used to identify the best model for predicting total costs.
Results:
Ninety-one infants with a mean age of 3 months (±1.9) were examined; 51 (56%) underwent LA alone, 40 (44%) underwent GA. Mean operating time was 11.53 ± 4.36 minutes, with no difference observed between anesthesia groups (P = .39). LA infants had a significantly shorter LOS (2.5 vs 3.5 hours; P < .05), quicker postoperative discharge (32 vs 65 minutes, P < .05), and fewer overall expenses, 2803 vs 6067 U.S. dollars (USD), P < .05. Two minor surgical complications (1 in each group) were reported.
Conclusions:
This study demonstrates significantly decreased cost, LOS, and time to discharge using LA alone for surgical excision of postaxial polydactyly type B. Results suggest the approach is quick, economical, and avoids the risks of GA in early infancy.
Keywords: anesthesia, local, post axial, polydactyly
Introduction
Postaxial or ulnar polydactyly type B consists of a pedunculated rudimentary digit attached to the small finger by soft tissue. 1 It is a common congenital anomaly, with an incidence of approximately 1 in 150 infants of African descent and 1 in 1500 to 3000 Caucasian infants.2-4 Approximately 85% of African American infants with polydactyly have a family history of this condition, which exhibits an autosomal dominant pattern of inheritance and rarely has a syndromic association. 2 In these infants, approximately 70% demonstrate bilateral postaxial polydactyly. 4
Treatment options for postaxial polydactyly type B include observation, ligation with suture, vascular clip ligation, or surgical excision. 5 Suture ligation may be performed in the nursery, home, or physician’s office and consists of tying suture material at the base of the supernumerary digit to occlude blood flow across the skin bridge, resulting in necrosis and subsequent auto-amputation. 6 Unfortunately, complications of suture or clip ligation include gangrene and infection, bleeding, failure of the digit to auto-amputate, painful neuroma formation, and unacceptable residual bumps.2,5,7–10, 11 When suture ligation is used as a treatment technique, the accessory nerves of the extra digit occasionally protrude at the level of the skin to produce a painful neuroma. 12 In a cohort of infants treated with this approach, 40% were found to have a residual tender bump at the site of ligation when examined postoperatively. 2 Painful neuromas, bumps, and other complications may require secondary surgery to correct.
Initial surgical excision using an elliptical incision with high ligation and retraction of the accessory digital nerve has been encouraged to avoid potential complications and improve outcomes.8,11 Simmons recommended that elective excision be performed under general anesthesia (GA) when a child is older than 6 months. 13 Delaying surgery decreases the risks associated with GA in early infancy, such as failure of airway management, cardiac arrest, and death. 14 However, as the neurocognitive impact of GA under age 3 or 4 is still unclear, some suggest delaying elective procedures even later than 6 months. 15 Despite the relative safety of this approach, it still ultimately requires subjecting the child to GA and postpones removal of the extra digits which can be stressful for the family. Excision of postaxial polydactyly type B using local anesthesia (LA) alone has been supported in the literature as a safe and effective treatment with good clinical outcomes. 8 Unfortunately, these small retrospective studies focus primarily on surgical outcomes and do not provide comparisons to GA. Existing research also fails to explore differences in cost among treatment methods.2,7,8,12 Accordingly, we present a comparison between local and GA for excision of postaxial polydactyly type B with respect to surgical outcomes, costs, and operative time to advocate for widespread change in the management of this condition.
Material and Methods
Study Design and Metrics
Study activities were undertaken following approval from our Institutional Review Board. A retrospective chart review of 91 patients under 12 months of age who underwent surgical excision of unilateral or bilateral type B postaxial polydactyly by a single surgeon from January 12, 2015 to January 5, 2018 was performed. Anesthesia type (local or general) and patient demographics (sex, age, race, and laterality) were recorded, as were any surgical or anesthetic complications. Data related to the total cost of each procedure were collected. Distinctions were made between professional charges (costs associated with the surgeon/provider) and hospital charges (costs associated with anesthesia, use of facilities, etc.). Total time spent in the hospital and at various stages of operating room (OR) utilization was also tracked. In addition, a parent satisfaction survey was performed as part of concurrent quality improvement. Our primary aim was to assess whether the incidence of complications differs between the 2 anesthesia groups. Secondarily, we sought to compare the average cost of polydactyly excisions using local or GA to determine if 1 approach offers significant costs savings.
Surgical Protocol
Preoperative management
Once assessed by the surgeon in clinic, polydactyly excision was scheduled according to institutional guidelines for age (see Figure 1). Families elected to have polydactyly surgery performed under either LA or GA following an informed discussion with the surgeon. The same surgical technique was used in both GA and LA patients examined in this study. All procedures were performed in an OR setting, either an ambulatory surgery center or main OR. Minor differences in pre- and postoperative care, dictated by a combination of age and type of anesthesia used, are noted where applicable. All infants undergoing LA were allowed to feed up until the time of surgery. In approximately half (43%) of the LA patients, EMLA™ (lidocaine 2.5% and prilocaine 2.5%) topical anesthesia was applied a minimum of 30 minutes prior to surgery.
Figure 1.
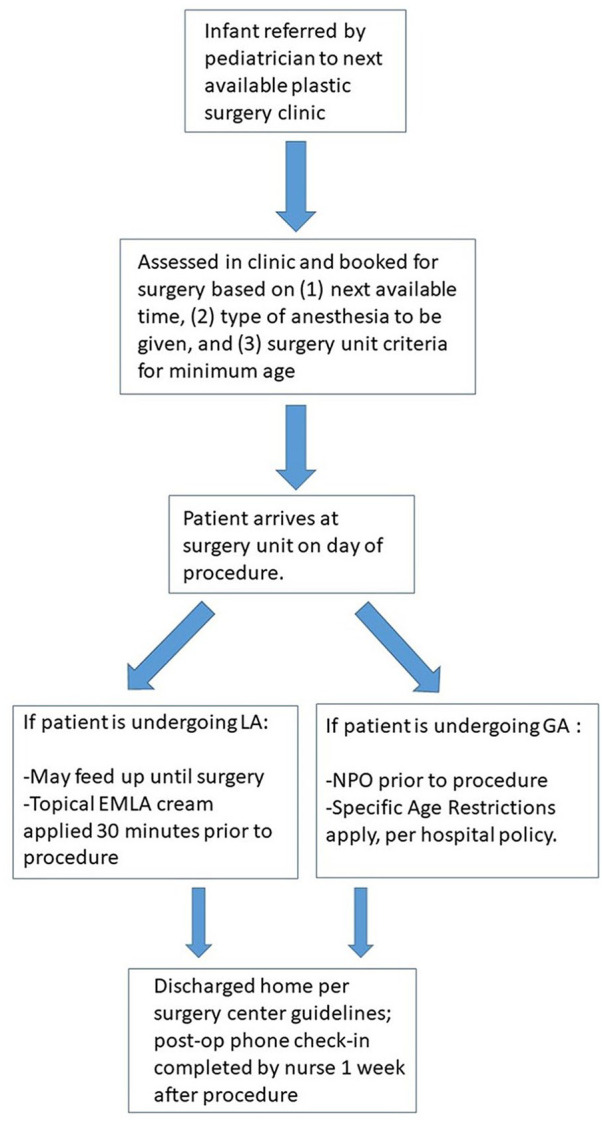
Protocol for management of infant presenting with postaxial polydactyly type B.
Note. LA, local anesthesia; GA, general anesthesia; NPO, nothing by mouth.
Procedure
Infants were taken to the OR, swaddled, and placed in a papoose or securely positioned on the OR table. Sweet-Ease (sucrose 24%) with a pacifier was provided if the infant was fussy. Using sterile technique, 1% lidocaine with epinephrine (1:100 000) was injected at the base of each extra digit and allowed to take effect. Typical injection doses of lidocaine ranged from 0.5 to 2 mL. Sterile prep and drape was then performed. The surgical site was checked for pain prior to making an incision. Under 2.5x loupe magnification, the digits were excised using an elliptical incision at the base with high ligation and retraction of the accessory digital nerve. Cautery on a setting of 10 (coag/pure/fulgurate, Valleylab Force FX™ generator C with Instant Response technology) was used for arterial hemostasis. Skin closure was performed with 5-0 chromic suture, followed by Dermabond glue. No additional dressing was placed.
Postoperative management
Infants were discharged home once surgery center guidelines were met. No postoperative medications were provided, although families were informed they could give the infant Tylenol at home as needed. Instructions for management of the surgical site and contact information were provided to the family prior to discharge. Phone follow-up was performed by a plastic surgery nurse 1 week following the procedure. Between January 1, 2018 and January 1, 2019, a nurse practitioner solicited feedback from families of patients who underwent polydactyly excision under LA as part of the postoperative phone call. Respondents were asked to rank their satisfaction with the procedure on a Likert-type scale ranging from “very unsatisfied” to “very satisfied” and offer overall thoughts on the experience.
Data Analysis
Independent t-tests and Wilcoxon rank sum tests were used to detect differences between the local and GA groups with regard to cost, procedure time, total OR time, and time from procedure end to discharge. Group comparisons on demographic variables were performed using chi square and Fisher’s exact tests. Univariate regression analyses were used to determine the impact of the following independent variables on the total cost of polydactyly excision: age at surgery, gender, surgery location, total time in the OR, length of stay (LOS), and laterality (bilateral vs unilateral excision). Stepwise forward regression was applied to select the independent variables that contributed to the final multivariable model for predicting the total cost of the procedure.
Results
At total of 91 surgical patients were included in the analysis. Forty (44%) underwent GA and 51 (56%) underwent LA. Mean age of the study sample was 3 months (± 1.9) and 55 (60%) were male. Fifty-five (60%) infants were of Black/African American heritage. Of the remaining infants, 15 (16%) were described as multiracial (16%), 11 (12%) were white, 4 (5%) were Hispanic, and 6 (7%) identified as another race. The 4 groups that comprised the minority of patients were collapsed into 1 group of 36 (40%) infants for binary analysis.
Two surgical complications (1 in each anesthesia group) were reported; no complications related to the administration of anesthesia were noted. Table 1 summarizes patient characteristics, outcomes, and independent variables with means ± standard deviation (SD), medians (interquartile range [IQR]), and frequency (%) as appropriate.
Table 1.
Independent Variable Comparisons: General Versus Local Anesthesia.
| Univariate independent variables | General (n = 40) | Local (n = 51) | P-value |
|---|---|---|---|
| Age at surgery (months) | 3.8 (3.1, 5.7) | 2.5 (1.6, 3.12) | <.05 |
| Male | 24 (60%) | 31 (61%) | .94 |
| Laterality (bilateral vs unilateral) | 27 (67%) | 31 (61%) | .51 |
| African American versus other | 22 (55%) | 33 (65%) | .35 |
| Time outcomes | |||
| Total operative, minutes | 11.00 ± 4.04 | 11.94 ± 4.59 | .39 |
| Total time in operating room, minutes | 30 (26, 38) | 23 (20, 28) | <.05 |
| Length of stay, hours. | 3.5 (3, 4.1) | 2.5 (2.2, 2.7) | <.05 |
| Time from procedure end to discharge, minutes | 65 (54, 74) | 32 (25, 41) | <.05 |
| Charge outcomes a | |||
| Hospital charges | 6067 (5948, 7243) | 2803 (2749, 2851) | <.05 |
| Professional charges | 2137 (1644, 2397) | 2268 (1694, 2470) | .19 |
| Total charges (professional + hospital charges) | 8322 (7676, 9627) | 5041 (4415, 5219) | <.05 |
Data represent mean USD (U.S. Dollars).
Significant values (<.05) in bold.
Patients who received GA were significantly older than those who received LA (P < .05). With respect to selected time variables, those in the GA group spent more time in the OR (P < .05), experienced a longer wait between procedure end and discharge (P < .05), and spent more time at the hospital overall (P < .05). Mean operating time between the groups was equivalent. In terms of cost, those who underwent GA had higher hospital charges (P < .05) and total charges than the LA group (P < .05). Professional charges alone were not significantly different between the 2 groups (P = .19).
Univariate significant predictors of total charges included anesthesia type (P < .05), age at surgery (P < .05), laterality (P < .05), total time in the OR (P < .05), and LOS (P < .05) (Table 2).
Table 2.
Univariate Regression Models: Total Charges vs Independent Variables.
| Independent variable | Coeff (SE) a | P-value |
|---|---|---|
| Anesthesia type | 3749.38 (222.81) | <.05 |
| Male | –300.09 (461.39) | .52 |
| African American vs other race | –209.02 (461.95) | .65 |
| Laterality (bilateral vs unilateral) | 1394.76 (446.55) | .05 |
| Total time in OR | 154.97 (16.31) | <.05 |
| Length of stay (hours) | 240.97 (43.36) | <.05 |
Note. SE = standard error; OR = operating room.
Data represent mean USD (U.S. Dollars).
Significant values (<.05) in bold.
Stepwise forward regression revealed that the model containing GA, total time in the OR, and laterality was the best for predicting total charges. One average, total hospital charges increased by 3,063.94 USD when GA was used in placed of LA. For every minute increase in OR time, total charges increased on average by 71.86 USD. Bilateral excision also contributed to higher cost: an average increase of 409.48 USD was observed for procedures involving both hands (Table 3).
Table 3.
Adjusted Regression Model: Total Charges..
| Total charges a | Predictor | Coeff | SE | Lower CL | Upper CL | P-value |
|---|---|---|---|---|---|---|
| Adjusted Model | General anesthesia | 3063.94 | 173.91 | 2718.28 | 3409.59 | <.05 |
| Total time in OR | 71.86 | 9.90 | 52.17 | 91.54 | <.05 | |
| Bilateral excision | 409.48 | 179.09 | 153.53 | 865.44 | <.05 |
Note. SE = standard error; OR = operating room; CL = confidence limits.
Data represent mean USD (U.S. Dollars).
Of 28 families, 17 were successfully contacted for the parent satisfaction survey. All families were satisfied with the procedure with 14 selecting the highest possible satisfaction rating.
Discussion
Treatment goals for postaxial polydactyly type B emphasize the use of safe and effective techniques that produce successful outcomes including complete removal of excess tissue, prevention of neuroma formation, and cosmetically displeasing residual bumps, with minimal complications such as infection, bleeding, and failure of the digit to auto-amputate. 15 While controversy exists in the literature regarding the ideal method for removing these extra digits, surgical excision avoids the common complications encountered with other methods and minimizes the need for secondary surgery.7,8,12,16 However, with respect to surgical excision, concerns have been raised about the safety of subjecting young infants to GA, as well as potentially needless costs associated with this treatment. 17
A number of studies suggest that GA may have long-term negative implications for neurocognitive development when administered in early infancy.15,18,19 Although GA is generally very safe, additional risks in young infants include failure of airway management that may lead to severe complications such as cardiac arrest and death. 14 In order to avoid these risks, elective surgeries such as postaxial polydactyly excision are frequently postponed until at least 6 to 12 months of age. Unfortunately, this approach not only delays excision of the digits, but ultimately still exposes the child to the risks of GA. Patients in our study who underwent LA were able to avoid complications associated with GA and have the procedure completed much earlier.
Our study presents surgical excision of postaxial polydactyly type B with LA alone as a safe and economic alternative to the use of GA. Of 91 infants who underwent polydactyly excision over an 18-month period, only 2 presented with minor complications (superficial infection treated with oral antibiotics). Advocates for the use of GA express concern for sub-optimal outcomes, presumably from decreased ability to control an infant’s motion using LA alone. 16 Our study demonstrates no difference in complications or outcomes between GA and LA groups, and in fact found significantly decreased cost, length of hospital stay, and total OR time with LA alone. Proponents of GA also suggest that parents may experience an emotional toll resulting from their infant’s excision under LA. 6 We address this by performing the procedure in a controlled surgical environment with the parent remaining in the waiting area until the procedure is completed. Furthermore, while the age of our patients was prohibitive to determining patient satisfaction with the procedure, our survey of qualitative surgical outcomes suggests the use of LA was well received by parents. Although the number of families surveyed was limited, all reported they would recommend LA to other families whose children needed to undergo the same procedure. Open-ended feedback revealed parents were pleased with the option of excising their child’s extra digits within the first few months of life and being able to avoid “knocking out” their child with GA. LA requires no sedation and is easily administered in young infants, avoiding the potential neurotoxic effects of GA while providing a complete sensory block for safe and effective removal of extra digits. There is no minimum age for administration, thus polydactyly excision can be performed any time after birth with LA alone. Epinephrine in the local anesthetic provides excellent hemostasis and eliminates the need and discomfort of a tourniquet. EMLA topical anesthetic may be applied prior to injection of LA to decrease the pain of injection. While it is not entirely clear of the EMLA’s effect on pain at the injection site, we currently feel it adds an extra measure of comfort to the procedure and are now consistent in use for all LA procedures. While many infants cry briefly at the time of injection and swaddling, most are calmed with warm blankets and Sweet-Ease. Having the infants feed immediately prior to the procedure also seems to improve comfort with many infants falling asleep during the procedure. The procedure is performed in a controlled surgical OR environment by a surgeon with pediatric hand surgery expertise. A set up with the infant swaddled or in a papoose and an assistant to firmly hold the infant’s hand and digit throughout the procedure ensured no complications secondary to movement of the infant. No complications of LA were noted in the study, and there were no instances that required the procedure be aborted or converted to GA. The main risk of local anesthetic use is toxicity, which can be avoided by injecting no more than 7 mg/kg per dose of lidocaine with epinephrine. 20 As 1 to 2 mL of lidocaine is typically injected for the procedure, the risk of toxicity is extremely low.
Our analysis noted significant differences for total time in the OR and total length of hospital stay for infants undergoing GA. Surgical time to perform the procedure under LA or GA was not significantly different. Increased time in the OR and hospital were predictive of increased hospital charges and, consequently, total charges. Costs associated with room and staff utilization would be expected to increase with time. According to our model, total charges increased by approximately 3063.94 USD when the procedure was performed with GA and approximately 71.86 USD for each additional minute spent in the OR (irrespective of the type of anesthesia used).
Due to variability in factors such as insurance reimbursement rates and differences in individual deductibles at the time of polydactyly excision, the direct impact of these cost reductions for families is difficult to quantify. There is, however, a sub-group of patients for whom the financial savings may translate into tangible community benefits. Approximately 66% of all infants who underwent postaxial polydactyly excision between January 1, 2015 and January 10, 2018 were enrolled in a state Medicaid plan participating in Partners for Kids (PFK), a pediatric accountable care organization (ACO). Providers and institutions participating in this ACO are incentivized to provide optimal care to patients at a lower cost through “upstream” practices that sustain patient health (eg, annual well visits, better stewardship of prescription medication, and care coordination). 21 Under this ACO, the hospital is given a lump sum of money to cover the care of all patients enrolled in eligible Medicaid plans. Money saved by practicing care with a focus on preventative medicine is then reinvested in regional health initiatives.
Limitations of our study include the retrospective nature of data collection, and the decision to only examine procedures performed by a single surgeon at 1 institution. Given the surgical procedure was designed to excise the neuroma with a cosmetically acceptable appearance, we performed phone follow-up with families 1 week after the procedure and asked them to return to clinic only if they had concerns. Our philosophy is to avoid the burden of unnecessary follow-up appointments for families, particularly given that the literature suggests surgical intervention successfully eliminates painful neuromas and incomplete excisions.7,8,16,22 While currently our surgery center is the optimal environment to safely perform these procedures, future directions include the possibility of performing these procedures in the office setting to further decrease the associated burden and costs.
Our study demonstrates significantly decreased cost, length of time in the OR, and overall hospital stay using LA alone for the surgical excision of postaxial polydactyly type B. No differences in surgical outcomes or complications between the 2 groups were found, and the incidence of complications was extremely low overall. Preliminary satisfaction assessments indicate that the use of LA is well received by parents. Results of this study suggest that surgical excision of postaxial polydactyly under LA alone is a safe and economical approach that can avoid the risks of GA in early infancy and should be the standard of care for the treatment of this condition.
Acknowledgments
The authors wish to thank Ann E. Salvator for her assistance with the biostatistics for this project.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent: No patient identifying information is present in the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Kim A. Bjorklund  https://orcid.org/0000-0001-7176-2537
https://orcid.org/0000-0001-7176-2537
References
- 1. Temtany SA, McKusick VA. Polydactyly as an isolated malformation. Birth Def. 1978;14:364-392. [Google Scholar]
- 2. Watson BT, Hennrikus WL. Postaxial type B polydactyly: prevalence and treatment. J Bone Joint Surg Am. 1997;79(1):65-68. [DOI] [PubMed] [Google Scholar]
- 3. Woolf CM, Myrianthopoulos NC. Polydactyly in American negroes and whites. Am J Hum Genet. 1973;25(4):397-404. [PMC free article] [PubMed] [Google Scholar]
- 4. Hiro ME, Gottschalk HP, Light TR. Ulnar polydactyly and ulnar dimelia. In: Laub DR, ed. Congenital Anomalies of the Upper Extremity. Boston, MA: Springer; 2015:261-272. [Google Scholar]
- 5. Abzug JM, Kozin SH. Treatment of postaxial polydactyly type B. J Hand Surg Am. 2013;38(6):1223-1225. [DOI] [PubMed] [Google Scholar]
- 6. Comer GC, Potter M, Ladd AL. Polydactyly of the hand. J Am Acad Orthop Surg. 2018;26(3):75-82. [DOI] [PubMed] [Google Scholar]
- 7. Mullick S, Borschel GH. A selective approach to treatment of ulnar polydactyly: preventing painful neuroma and incomplete excision. Pediatr Dermatol. 2010;27(1):39-42. [DOI] [PubMed] [Google Scholar]
- 8. Katz K, Linder N. Postaxial type B polydactyly treated by excision in the neonatal nursery. J Pediatr Orthop. 2011;31(4):448-449. [DOI] [PubMed] [Google Scholar]
- 9. Frieden IJ, Chang MW, Lee I. Suture ligation of supernumerary digits and “tags”: an outmoded practice. Arch Pediatr Adolesc Med. 1995;149(11):1284. [DOI] [PubMed] [Google Scholar]
- 10. Heras L, Barco J, Cohen A. Unusual complication of ligation of rudimentary ulnar digit. J Hand Surg Br. 1999;24(6):750-751. [DOI] [PubMed] [Google Scholar]
- 11. Rayan GM, Frey B. Ulnar polydactyly. Plast Reconstr Surg. 2001;107(6):1449-1454. [DOI] [PubMed] [Google Scholar]
- 12. Ahmad Z, Park AJ. The milk anesthesia management of neonatal accessory digits: the 6 year Coventry and Warwickshire experience. J Med Soc. 2014;28:149-153. [Google Scholar]
- 13. Simmons BP. Polydactyly. Hand Clin. 1985;1(3):545-565. [PubMed] [Google Scholar]
- 14. Fiadjoe JE, Nishisaki A, Jagannathan N, et al. Airway management complications in children with difficult tracheal intubation from the pediatric difficult intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016;4(1):37-48. [DOI] [PubMed] [Google Scholar]
- 15. Lei S, Ko R, Sun LS. Neurocognitive impact of anesthesia in children. Adv Anesth. 2018;36(1):125-137. [DOI] [PubMed] [Google Scholar]
- 16. Leber GE, Gosain AK. Surgical excision of pedunculated supernumerary digits prevents traumatic amputation neuromas. Pediatr Dermatol. 2003;20(2):108-112. [DOI] [PubMed] [Google Scholar]
- 17. Mills JK, Ezaki M, Oishi SN. Ulnar polydactyly: long-term outcomes and cost-effectiveness of surgical clip application in the newborn. Clin Pediatr (Phila). 2014;53(5):470-473. [DOI] [PubMed] [Google Scholar]
- 18. Ing C, DiMaggio C, Whitehouse A, et al. Long term differences in language and cognitive function after childhood exposure to anesthesia. Pediatrics. 2012;130(3):e476-e485. [DOI] [PubMed] [Google Scholar]
- 19. Wilder RD, Flick RP, Sprung J, et al. Early exposure to anesthesia and learning disabilities in a population based birth cohort. Anesthesiology. 2009;110(4):796-804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Berde JB. Toxicity of local anesthetics in infants and children. J Pediatr. 1993;122(5):S14-S20. [DOI] [PubMed] [Google Scholar]
- 21. Nationwide Children’s Hospital. Partners for kids: pediatric accountable care. https://www.nationwidechildrens.org/impact-quality/partners-for-kids-pediatric-accountable-care. Accessed September 16, 2019.
- 22. Singer G, Thein S, Kraus T, et al. Ulnar polydactyly: an analysis of appearance and postoperative outcome. J Pediatr Surg. 2014;49(3):474-476. doi: 10.1016/j.jpedsurg.2013.06.029. [DOI] [PubMed] [Google Scholar]


