Abstract
Purpose of review
People living with HIV (PLWH) are commonly co-infected with Mycobacterium tuberculosis, particularly in high-transmission resource-limited regions. Despite expanded access to antiretroviral therapy and tuberculosis (TB) treatment, TB remains the leading cause of death among PLWH. This review discusses recent advances in the management of TB in PLWH and examines emerging therapeutic approaches to improve outcomes of HIV-associated TB.
Recent findings
Three recent key developments have transformed the management of HIV-associated TB. First, the scaling-up of rapid point-of-care urine-based tests for screening and diagnosis of TB in HIV-infected patients has facilitated early case detection and treatment. Second, increasing the availability of potent new and repurposed drugs to treat drug-resistant TB has generated optimism about the treatment and outcome of multidrug-resistant and extensively drug-resistant TB. Third, expanded access to the integrase inhibitor dolutegravir to treat HIV in resource-limited regions has simplified the management of TB/HIV co-infected patients and minimised serious adverse events.
Summary
While it is unequivocal that substantial progress has been made in early detection and treatment of HIV-associated TB, significant therapeutic challenges persist. To optimise the management and outcomes of TB in HIV, therapeutic approaches that target the pathogen as well as enhance the host response should be explored.
Keywords: Tuberculosis, HIV, New, Therapeutic approaches, Treatment outcomes
Introduction
Tuberculosis (TB) and human immunodeficiency virus (HIV) co-infection is the most devastating infectious disease combination across the globe. Mycobacterium tuberculosis (Mtb) and HIV have a synergistic relationship within the host, potentiating each other (1). TB increases HIV replication and accelerates HIV-disease(2). Whereas, HIV impairs Mtb-specific immune response, and promotes the progression and clinical severity of TB(2–4). As a result, of the 10 million people who developed active TB disease globally in 2019, 8.2% (820,000) were PLWH. During the same period, 1.2 million HIV-negative patients (13%) and 208,000 PLWH (25%) died of TB(5). The highest burden of the syndemic is in Africa, where more than 75% of HIV-associated TB occurs(6). Southern Africa remains the epicentre with more than half of TB patients co-infected with HIV, of which, many die either before diagnosis or early during treatment(7). Similarly, TB/HIV co-infection has emerged as a public health challenge in resource-rich regions, including the United States of America and Eastern Europe(8,9).
During the last two decades, there has been a substantial improvement in outcomes of TB/HIV co-infected patients due to the implementation of several public health interventions. The universal access to antiretroviral therapy (ART) by PLWH, regardless of CD4 T-cell count has significantly reduced TB rates (10). Additionally, TB prophylaxis therapy with isoniazid for six to twelve months or a joint isoniazid and rifampicin regimen for three months has decreased the likelihood of TB in PLWH by an estimated 32% to 64%(11). The revolutionary impact of ART in reducing HIV-associated TB risk was underscored in recent observational cohort studies (12).
Despite the significant progress in combating TB/HIV, successful treatment of HIV-associated TB remains a daunting mission. This review discusses recent developments in management approaches ranging from novel diagnostic techniques to revised and newly approved drug regimens as well as future strategies aimed at improving treatment outcomes of TB in PLWH. While the new approaches will improve the management of HIV-associated TB worldwide, their impact will be greatest in low- and middle-income settings where there are limited healthcare resources and a high prevalence of TB and HIV.
New approaches to TB diagnosis
Early diagnosis and prompt initiation of treatment are important prerequisites for good TB treatment outcomes, limit transmission of infection and are integral pillars of the World Health Organization (WHO) End TB Strategy (13). Despite the scale-up of ART, TB remains a significant cause of hospital admission and patient mortality in resource-limited settings with a high prevalence of HIV infection. This problem is in part, due to the low detection rates by sub-standard diagnostics for HIV-related TB, with delayed and missed diagnoses contributing to fatal outcomes(14,15).
Sputum smear microscopy using direct Ziehl–Neelsen staining remains the primary diagnostic tool in resource-limited settings. While this technique is rapid, specific and cheap, it is operator dependent (16). Moreover, sputum smear microscopy performs poorly in patients with advanced HIV, detecting 22% to 43% of active disease(6). This is mainly attributed to a low bacterial load in sputum from patients with advanced HIV; thus, the optimal bacterial concentration for visual detection by microscopy is not attainable(16,17). For PLWH with suspected TB despite negative sputum smear microscopy, mycobacterial culture has been the solitary diagnostic option(17). However, this test is expensive, complex and has a long turnaround time for results; therefore, it is seldomly available in resource-limited settings(18,19). Furthermore, there is limited access to rapid liquid culture methods such as Mycobacterium Growth Indicator Tube (MGIT), which have been shown to accelerate the turnaround time to diagnosis (20,21). These challenges undermine TB control efforts by prolonging patient agony and sustaining transmission(15,22). We urgently need simple, rapid, accurate and affordable point-of-care diagnostic tools to overcome these challenges.
Recent developments in TB diagnostics have transformed case detection and treatment of patients with HIV-associated TB. First, nucleic acid amplification tests (NAATs) such as Xpert® MTB/RIF and Xpert® MTB/RIF Ultra, have facilitated rapid detection of Mtb and resistance to rifampicin, expedited TB diagnosis and initiation of treatment compared to microscopy and culture-based diagnostic methods(23). A previous study reported that in PLWH with high clinical suspicion of TB, Xpert® MTB/RIF outperformed sputum smear microscopy and detected 97.8% versus 68.9%; p=0.0002, of pulmonary TB cases against a composite reference standard Löwenstein-Jensen (LJ) and liquid culture(24). While Xpert® MTB/RIF has outstanding sensitivity in smear-positive sputum samples, it is less sensitive in smear-negative sputum (25). For this reason, the next-generation Xpert® MTB/RIF Ultra is particularly suited for the analysis of specimens with low bacillary load, such as those from PLWH. In a recent comparative analysis, Xpert® MTB/RIF Ultra had a sensitivity of 78.9% (95% CI, 70.0–86.1) compared to 66.1% (95%CI,56.4–74.9) for Xpert® MTB/RIF in smear negative-culture positive sputum samples. This represents an estimated 13% increase in sensitivity. For smear and culture-positive samples, Xpert® MTB/RIF Ultra and Xpert® MTB/RIF had comparable sensitivities of 97.8% (95% CI, 92.3–99.7) and 98.9% (95% CI, 94.0–100), respectively (25). Similarly, the diagnostic accuracy of Xpert® MTB/RIF Ultra was evaluated in PLWH in a recent multicentre diagnostic accuracy study(26). Xpert® MTB/RIF Ultra had superior pulmonary TB case detection in patients with culture-positive sputum compared to Xpert® MTB/RIF, with sensitivities of 90% (95% CI, 83–95) and 77% (95% 68–84), respectively(26).
Additionally, Xpert® MTB/RIF Ultra had higher sensitivity for the detection of tuberculous meningitis in PLWH than Xpert® MTB/RIF. In one study, Xpert® MTB/RIF Ultra and Xpert® MTB/RIF had sensitivities of 95% (95% CI, 77–99) and 45% (95% CI, 24–68; p=0.0010), respectively, against a composite reference standard of any positive cerebrospinal fluid (CSF) tuberculous test (27). Similar findings were reported by another study in which Xpert® MTB/RIF Ultra and Xpert® MTB/RIF had sensitivities of 92.9% (95% CI, 80.5–98.5) and 65.8% (95% CI, 48.6–80.4; p=0.0063), respectively, for detection of HIV-associated tuberculous meningitis against the composite microbiological standard(28). Importantly, simultaneous detection of rifampicin resistance by Xpert® MTB/RIF and Xpert® MTB/RIF Ultra at the time of TB diagnosis allows early identification of patients at risk of multidrug-resistant TB (MDR-TB) or extensively drug-resistant TB (XDR-TB) and initiation of appropriate treatment(17). Moreover, Xpert® MTB/RIF and Xpert® MTB/RIF Ultra require limited training/expertise and have relatively high sensitivity for paucibacillary TB(17,29). Consequently, the WHO and the Centers for Disease Control and Prevention (CDC) have approved the use of these diagnostic assays in individuals suspected of having HIV-associated TB or MDR-TB(23,30,31).
Secondly, the introduction of the urine-based lateral flow lipoarabinomannan assay (urine LAM, Alere Determine TB LAM Ag [AlereLAM]) for the diagnosis and screening of active TB in PLWH has shown great promise as a point-of-care test (POC) (6,15). Urine LAM produces a result in less than 25 minutes, using an estimated 60 μL of urine to detect lipoarabinomannan, an Mtb glycolipid antigen present in the mycobacterial cell wall(15). Several studies have reported the excellent performance of urine LAM and associated mortality reduction in hospitalised PLWH with advanced immunosuppression resulting in a decrease in mortality(15,32,33). In addition, The sensitivity of medical and chest X-ray diagnosis is increased by the urine LAM test, subsequently facilitating early initiation of treatment in vulnerable patient populations, thereby contributing to favourable outcomes(15). Furthermore, urine LAM is not reliant on obtaining sputum samples, making it a useful test in HIV-infected patients with extrapulmonary or disseminated TB (15,33).
The AlereLAM assay is limited by reduced sensitivity when the patient’s CD4 count is above 100 cells per μl and in patients with extrapulmonary TB (EPTB)(23,34). To overcome these limitations, a novel Fujifilm SILVAMP TB LAM (FujiLAM) assay has been developed and detects lipoarabinomannan on an instrument-free platform, producing results in less than one hour (35–39). A recent study assessed the diagnostic accuracy of the FujiLAM assay compared with the AlereLAM assay for the detection of TB in hospitalised PLWH. The study reported that FujiLAM has superior sensitivity than AlereLAM. The overall sensitivities were 70.4% (95% CI, 53.0–83.1) and 42.3% (95% CI, 31.7–51.8) for FujiLAM and AlereLAM, respectively (difference 28.1%), compared with the microbiological reference standard. The estimated specificities were 90.8% (95% CI,86.0–94.4) and 95.0% (95% CI, 87.7–98.8) for FujiLAM and AlereLAM, respectively. In patients with CD4 count <100 cells/μL, the FujiLAM sensitivity was 84.2% (95% CI, 71.4–91.4) versus 57.3% (95% CI, 42.2–69.6) for AlereLAM (difference 26.9%). Although the sensitivities of both assays were suboptimal in patients with CD4 count >200 cells/μL, FujiLAM had superior sensitivity of 44.0% (95% CI, 29.7–58.5) compared with 12.2% (95% CI, 4.6–23.7) for AlereLAM (difference 31.8%) (40). The superior sensitivity of FujiLAM over AlereLAM was also seen in patients with EPTB and those with TB mycobacteraemia(34).
The availability of simple, rapid, point-of-care urine tests for TB represents a significant breakthrough in TB control(15). The advent of AlereLAM prompted the WHO to endorse the assay as the diagnostic and screening tool for active TB disease in two specific populations. These include HIV-infected adults manifesting signs and symptoms of pulmonary/extrapulmonary TB (EPTB) and a CD4+ T cell count of less than 100 cells per μl, and critically ill HIV-infected patients irrespective of their CD4+ T cell count or if CD4+ T cell count is not known(6). Furthermore, combining LAM with Xpert® MTB/RIF/ Xpert® MTB/RIF Ultra testing of the urine offers an intriguing opportunity to improve the diagnosis of active TB in PLWH as reported by recent publications(28,41). The use of FujiLAM as a screening and diagnostic test for TB in PLWH is likely to increase the already known survival benefit of point-of-care urine tests for TB(14,32,33,39)
Thirdly, in recent times, ultrasonography has been shown to aid the diagnosis of EPTB, which occurs more frequently in PLWH (42,43). The emergence of focused assessment with sonography for HIV-associated TB (FASH) has garnered attention as a potential point-of-care diagnostic tool. FASH detects sonographic signs of EPTB such as effusions in the pleural and pericardial spaces, enlarged intra-abdominal lymph nodes and micro-abscesses, particularly in the spleen and liver. The FASH protocol has been adopted as an integral diagnostic tool in some extremely resource-limited settings(42,43). There is growing interest to implement the FASH protocol throughout these settings because of its many advantages, including expedient time to diagnosis, inexpensive, radiation-free and less reliance on a conventional electric power source. Additionally, clinicians with little or no previous experience in ultrasonography can be trained to perform FASH. Despite underlying concerns of inter-observer variability and misdiagnosis, further studies should explore the role of FASH in expediting treatment of HIV-associated TB(43).
Advances in TB treatment
TB treatment in PLWH is identical to the therapy in HIV-uninfected patients(44).
Standard guidelines for drug-susceptible TB include an intensive phase of two months with isoniazid (INH), rifampicin (RIF), ethambutol (EMB), and pyrazinamide (PZA). This is followed by a minimum of four months continuation phase with INH and RIF(45,46). While we have drugs to treat TB, prolonged treatment with multi-drug regimens is fraught with issues of compliance, toxicity and drug resistance. Consequently, successful treatment outcomes are only achieved in an estimated 80% of patients with drug-susceptible TB (47). To reduce the toxicity of the current standard quadruple drug regimen, a recent study observed that the addition of methionine and vitamin B complex to the standard regimen reduced liver toxicity(48).
Despite expanded access to ART in regions with a high prevalence of HIV and TB, mortality within the first 6 months after ART initiation remains high, particularly among patients with advanced HIV. Undiagnosed TB is a common cause of this excess mortality(49). To address this challenge, three recent clinical trials (STATIS ANRS 12290, REMEMBER and TB Fast Track) investigated whether starting empirical TB treatment at ART initiation would reduce mortality among severely immunosuppressed PLWH with CD4+ T cell count <150 cells/μL. Although the comparator arms and CD4+ T cell cut-offs were different across the trials, empirical TB treatment did not reduce mortality at 24 weeks(50–52), suggesting that other factors also contribute to excess mortality during the early phase of ART. Patients with advanced HIV infection and TB are at a higher risk of opportunistic infections, TB treatment failure, overlapping drug toxicities, development of immune reconstitution inflammatory syndrome (IRIS) and the emergence of TB drug resistance compared to HIV-uninfected TB patients(47,53,54). These factors are likely to contribute to early mortality following ART initiation.
Treatment of MDR-TB and XDR-TB
Previous MDR-TB and XDR-TB treatment guidelines recommended prolonged use of expensive multi-drug regimens with serious side effects which resulted in unfavourable outcomes, particularly in PLWH(55). The recent introduction of new and repurposed effective, less toxic oral drugs has, however, revolutionised the MDR-TB and XDR-TB treatment landscape and improved treatment outcomes(56). Of the approved new drugs, bedaquiline and delamanid have been recommended by WHO and CDC for treatment of MDR-TB based on accumulating evidence for efficacy and reduced mortality when included in MDR-TB treatment regimens, even amongst PLWH(56,57). Pretomanid is another promising new drug for TB, which was recently evaluated in a multicentre, open-label, partially randomised, Phase 2b trial as part of a combinatory regimen comprising bedaquiline, pyrazinamide and moxifloxacin for the treatment of patients with drug-resistant pulmonary TB. In patients with pyrazinamide-susceptible rifampicin-resistant disease, this regimen had superior bactericidal activity at day 56 of treatment compared with the standard first-line quadruple regimen of isoniazid, rifampicin, pyrazinamide and ethambutol. Furthermore, this regimen has a lower pill burden than the currently recommended WHO rifampicin-resistant TB treatment options and does not include injectable drugs (47).
While the availability of new drugs for TB is a long-awaited and welcome development, the addition of linezolid and clofazimine to treatment regimens for drug-resistant TB represents a paradigm shift in TB drug discovery(47). Linezolid and clofazimine, antimicrobial agents, initially discovered for the treatment of other infections, have shown novel modes of action against Mtb(58). Consequently, the repurposing of drugs with known safety profiles is an attractive and innovative approach to treat drug-resistant TB(58). The Food and Drug Administration (FDA) has approved bedaquiline and linezolid for treatment of adults with XDR-TB, treatment intolerant or non-responsive MDR-TB(59).
The WHO has also updated its treatment guidelines and recommends treating both multidrug-resistant and rifampicin-resistant TB with either an 18-month regimen in patients with confirmed fluoroquinolone resistance or a shorter 9–12-month regimen for patients with fluoroquinolone and aminoglycosides sensitivity(60–62). The short regimen entails an intensive phase comprising moxifloxacin, amikacin or kanamycin, ethionamide or prothionamide, clofazimine, isoniazid, ethambutol, and pyrazinamide for a duration of four to six months. This is followed by a continuation phase of moxifloxacin, clofazimine, ethambutol, and pyrazinamide for five months(63,64). The efficacy of the short-course regimen was initially demonstrated in observational studies in South Asia and in Central and West Africa, where it had high success rates, including in HIV-infected patients(44,57,65). Additionally, PLWH may be at increased risk of adverse events associated with new and repurposed TB drugs. For instance, linezolid has been associated with cytopenias, peripheral neuropathy, and optic neuropathy among PLWH. Clofazimine, delamanid, and bedaquiline lengthen the QT interval; therefore, their use is not recommended if the QT interval is above 500 ms(66). Several ongoing trials listed in Table 1 are assessing the efficacy and safety of new regimens for the treatment of drug-resistant tuberculosis and are grounds for optimism.
Table 1:
Ongoing clinical trials of treatment of multidrug-resistant TB in PLWH and HIV-uninfected individuals
| Name of trial | Study population | Study groups | Description | Status |
|---|---|---|---|---|
| NiX-TB (NCT02333799) | 109 participants enrolled, HIV− and HIV + adults (aged ≥18 years) | 6 months bedaquiline (400 mg daily for 2 weeks then 200 mg three times weekly), pretomanid (200 mg daily), linezolid (600 mg twice daily), | Phase 3 trial assessing the safety and efficacy of bedaquiline, pretomanid as well as linezolid in subjects with pulmonary infection of either XDR-TB, treatment-intolerant tuberculosis, or pre-XDR non-responsive MDR-TB | Active but not recruiting. Expected completion July 2020 |
| NC-008 SimpliciTB (NCT03338621) | 455 participants enrolled, HIV− and HIV + adults (aged ≥18 years) | 6 months bedaquiline, pretomanid, moxifloxacin, pyrazinamide daily, single arm study | Phase 2 trial evaluating the efficacy, safety and tolerability of bedaquiline, pretomanid, moxifloxacin Plus Pyrazinamide (BPaMZ) compared to a 6-month Treatment of HRZE/HR (Control) in Adult Participants With Drug-Sensitive Smear-Positive Pulmonary Tuberculosis (DS-TB) and a 6-month Treatment of BPaMZ in Adult Participants With Drug Resistant, Smear-Positive Pulmonary Tuberculosis (DR-TB) | Active but not recruiting. results expected February 2022 |
| IMPAACT 2005 (NCT03141060) | 48 participants enrolled, HIV− and HIV + children (aged <18 years) | Pharmacokinetics, safety 6 months delamanid (100 mg twice daily) plus Optimised multi-drug background regimen (OBR), single arm study | This phase 1–2 study will evaluate the pharmacokinetics, safety, and tolerability of the anti-tuberculosis (TB) drug delamanid (DLM) in combination with an optimised multi-drug background regimen (OBR) for MDR-TB in HIV-infected and HIV-uninfected children with MDR-TB. | Recruitment ongoing. Completion date November 2022 |
| endTB (NCT02754765) | 750 participants enrolled, HIV− and HIV + adults (aged ≥18 years) | 9 months bedaquiline, linezolid, moxifloxacin, pyrazinamide daily, or 9 months of bedaquiline, linezolid, clofazimine, levofloxacin, pyrazinamide daily, or 9 months of bedaquiline, linezolid, delamanid, levofloxacin, pyrazinamide daily, or 9 months of delamanid, linezolid, clofazimine, levofloxacin, pyrazinamide daily, or 9 months of delamanid, clofazimine, moxifloxacin, pyrazinamide daily vs local regimen as per WHO guidelines |
This Phase 3 trial will evaluate the efficacy and safety of five new, all-oral, shortened regimens for MDR-TB. | Recruitment ongoing. Estimated completion date April 2021 |
| TB-PRACTECAL (NCT02589782) | 630 participants enrolled, HIV− and HIV + adults (aged ≥18 years) | 6 months bedaquiline, pretomanid, moxifloxacin, linezolid daily,or 6 months bedaquiline, pretomanid, linezolid, clofazimine daily,or 6 months bedaquiline, pretomanid, linezolid daily (all oral) vs local regimen | This phase 2–3 trial evaluating short treatment regimens containing bedaquiline and pretomanid in combination with existing and repurposed anti-TB drugs for the treatment of biologically confirmed pulmonary MDR-TB. | Recruitment ongoing. Estimated date of completion March 2021 |
| NExT 5001 (NCT02454205) | 154 participants enrolled, HIV− and HIV + adults (aged ≥18 years) | 6–9 months bedaquiline, linezolid, levofloxacin, pyrazinamide and either high-dose isoniazid or ethionamide or terizidone daily (all oral) vs 6–8 months kanamycin, moxifloxacin, pyrazinamide, ethionamide, terizidone daily, and 16–18 months moxifloxacin | phase 2–3 trial investigating a new treatment regimen for patients with MDR-TB | Active, not recruiting. Estimated date of completion December 2020 |
New ART approaches in HIV associated TB treatment
TB-associated mortality in HIV-infected patients is highest in the early stages of TB therapy(4). However, several clinical trials have demonstrated the benefits of early initiation of effective ART during TB therapy, including improved survival of severely immune-suppressed patients(67–70). Consequently, these findings informed the decision by the CDC, American Thoracic Society (ATS), Infectious Disease Society of America (IDSA), and the WHO to recommend the immediate initiation of ART in all patients with drug-susceptible TB and HIV (23,71).
The interactions between ART and TB medications complicate the management of dually-infected patients, particularly in low-income settings, where there is a limited range of ART drugs(44,72). These interactions occur predominantly during the metabolism of the drugs. The drug-drug interactions involving the first-line TB drug, rifampicin, are of particular clinical relevance. Rifampicin significantly reduces plasma concentrations of some concurrently administered ART drugs, resulting in sub-optimal plasma levels and poor ART outcomes(44,73). ART drugs that are substrates of P-glycoprotein and CYP3A4, such as the protease inhibitors (PIs) and the non-nucleoside reverse transcriptase inhibitor (NNRTI) nevirapine are significantly affected by rifampicin(44,73). To overcome this problem, ART regimens containing another NNRTI, efavirenz, are preferred for concurrent use with rifampicin-containing TB treatment, especially in low- and middle-income countries (LMICs)(74). However, increasing rates of resistance to NNRTIs in LMICs underscore the need for alternative ART drugs (75).
The use of the integrase strand transfer inhibitor (INSTI), dolutegravir (DTG), has increased rapidly in TB-endemic LMICs following the recent WHO recommendation to include DTG in first- and second-line ART regimens based on its efficacy and good safety profile(74). However, it is important to note that when co-administered with rifampicin, DTG exposure is decreased by 54%(44). Hence, the dose of DTG should be increased to 50 mg twice daily when it is given together with rifampicin(74). A recent addition to the INSTI class, bictegravir, is also perturbed by rifampicin. Despite using the twice-daily regimen that included emtricitabine, tenofovir, and bictegravir, rifampicin reduced bictegravir plasma concentrations by 80% compared to once-daily dosing without rifampicin. Therefore, bictegravir should not be given with rifampicin(57).
Future perspectives
While there have been momentous advances in the last decade in combating TB, including new TB drugs and rapid diagnostics, the management of HIV-associated TB remains nevertheless complicated. There is persisting need for optimal oral TB treatment regimens that are short, effective and less toxic to treat drug-susceptible and drug-resistant TB in PLWH(47,76). Figure 1 summarizes recently introduced approaches and those under evaluation to improve management of TB in PLWH. During the last 60 years, TB drug discovery has focused predominantly on identifying compounds that target the pathogen, Mtb. However, recent efforts have expanded to include investigation of a series of adjunct therapeutic strategies known as host-directed therapies (HDTs) that target the host response to infection instead(77). HDTs target specific pathways involved in the pathogenesis of TB in the host(78). By enhancing cellular antibacterial mechanisms as well as directly limiting inflammation, HDTs avert lung injury and increase chemotherapy effectiveness (79). In addition, HDTs can be used concurrently with antimicrobial treatment regimens against drug-resistant TB with minimal risk of therapeutic resistance. They also provide the additional benefit of potentially decreasing the number of drugs required in combination treatment, mainly when toxicity is a problem as well as reducing the duration of TB treatment(78).
Figure 1. A summary of recent approaches and approaches under evaluation to improve the management of TB in people living with HIV.
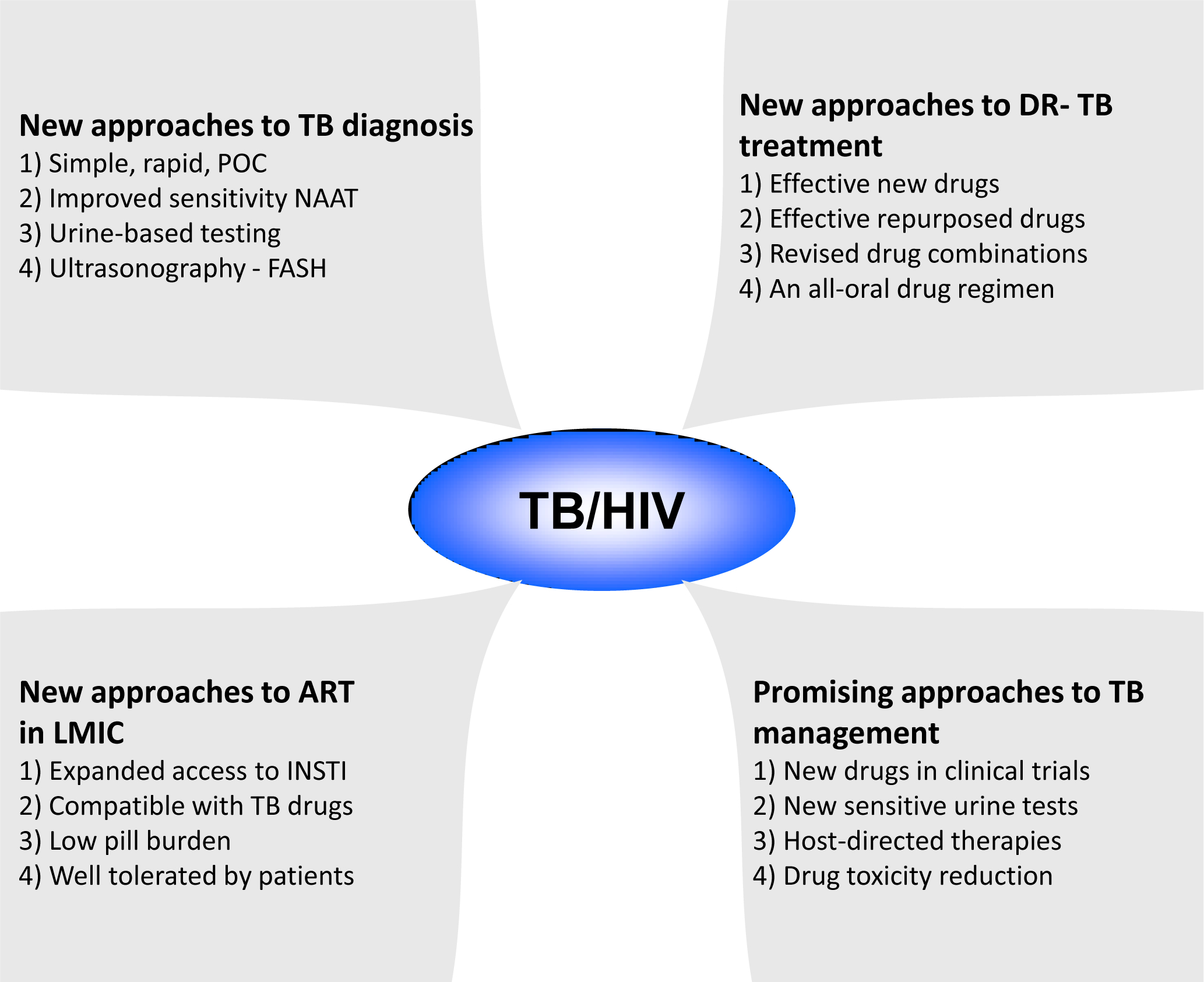
ART – antiretroviral therapy; DR-TB – drug-resistant tuberculosis; FASH- focused assessment with sonography for HIV-associated tuberculosis; HIV – human immunodeficiency virus; LMICs – low- and middle-income countries; NAAT – nucleic acid amplification test; POC – point-of-care; TB – tuberculosis.
Currently, there are several HDTs drugs under investigation. Firstly, rapamycin, a known immunosuppressive used in organ transplantation, inhibits the mammalian target rapamycin (mTOR), a negative regulator of autophagy(79). The selective form of autophagy known as xenophagy directly tags intracellular pathogens for lysosomal degradation and is crucial in host control of TB(78,80–82). Recent studies have reported that the Stimulator of IFN genes (STING)-dependent cytosolic sensing pathway recognises Mtb DNA released into the cytosol and facilitates marking of the bacteria with ubiquitin for delivery to the autophagic machinery(83). However, Mtb manipulates xenophagy by inhibiting maturation of autophagosomes(84) and through the action of its enhanced intracellular survival (EIS) protein, which mediates AKT/mTOR pathway via activation of IL-10(85). Whilst rapamycin is a promising HDT drug for TB; it has been reported to cause interstitial pneumonitis, which may complicate the management of patients with pre-existing lung disease. Another drug currently in clinical trials as a potential HDT for TB is metformin, which enhances autophagy by promoting phagolysosome maturation and augments mitochondrial reactive oxygen species production(79).
Additionally, vitamin D, whose active metabolite, 1,25-dihydoxyvitamin D, has long been known to enhance the immune responses to mycobacteria in vitro, is a candidate HDT. In a recent study, vitamin D was shown to limit intracellular Mtb growth in macrophages by enhancing innate immune responses through Toll-like receptors and IFN-γ, overturning Mtb-induced phagosome maturation arrest, increased expression of antimicrobial peptides and subsequent induction of autophagy in infected cells(86). HDTs may have additional benefits in HIV and TB co-infected patients by minimising drug-drug interactions with ART as well as limiting the risk of developing IRIS and death (77).
Conclusion
TB and HIV coinfection remains a global public health concern responsible for high morbidity and mortality. While rapid, sensitive tests for TB screening and diagnosis have simplified case detection and accelerated access to TB treatment among TB/HIV co-infected patients, further work is required to shorten the duration of TB treatment and minimise the emergence of TB and ART drug resistance, drug-drug interactions between TB and HIV therapies and overlapping drug toxicities.
Key points.
The introduction and scaling-up of simple, rapid and sensitive TB diagnostics have promoted early access to TB treatment by PLWH.
New and repurposed TB drugs have transformed the treatment of drug-resistant HIV-associated TB, particularly MDR- and XDR-TB, by enhancing the potency and reducing toxicity of new TB treatment regimens.
Integrase inhibitor-based ART is effective and well-tolerated by HIV-infected patients receiving rifampicin-based TB treatment in resource-limited settings.
Host-directed therapies as adjunct therapeutic approaches to augment antimicrobial TB treatment and improve treatment outcomes warrant further exploration.
2. Acknowledgements
Financial support and sponsorship: HCM and KCJ are supported by African Research Leader Awards MR/P020526/1 and MR/T008822/1, respectively, jointly funded by the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordant agreement and are part of the EDCTP2 programme supported by the European Union. HCM is also supported by the Bill and Melinda Gates Foundation and the National Institutes of Health through grant numbers OPP1108452 and AI155319, respectively. A core grant from the Wellcome Trust supports the Malawi Liverpool Wellcome Trust Clinical Research Programme.
Footnotes
Conflict of interest: All authors declare no conflict of interest.
References
- 1.Pawlowski A, Jansson M, Sköld M, Rottenberg ME, Källenius G. Tuberculosis and HIV co-infection. PLoS pathogens. 2012;8(2):e1002464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Narayanasamy P, Switzer BL, Britigan BE. Prolonged-acting, multi-targeting gallium nanoparticles potently inhibit growth of both HIV and mycobacteria in co-infected human macrophages. Scientific Reports. 2015;5:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bell LCK, Noursadeghi M. Pathogenesis of HIV-1 and mycobacterium tuberculosis co-infection. Nature Reviews Microbiology. 2018;16(2):80–90. [DOI] [PubMed] [Google Scholar]
- 4.Manosuthi W, Wiboonchutikul S, Sungkanuparph S. Integrated therapy for HIV and tuberculosis. AIDS Research and Therapy. 2016;13(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Global Tuberculosis Report 2020. 2020.
- 6.Pai M, Behr MA, Dowdy D, Dheda K, Divangahi M, Boehme CC, et al. Tuberculosis. Vol. 2, Nature Reviews Disease Primers; 2016. p. 1–23. [DOI] [PubMed] [Google Scholar]
- 7.Lawn SD, Meintjes G, Mcilleron H, Harries AD, Wood R. Management of HIV-associated tuberculosis in RLS. BMC Medicine. 2013;11(253):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montales MT, Chaudhury A, Beebe A, Patil S, Patil N. HIV-Associated TB Syndemic: A Growing Clinical Challenge Worldwide. Frontiers in Public Health. 2015;3:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Efsen AMW, Schultze A, Post FA, Panteleev A, Furrer H, Miller RF, et al. Major challenges in clinical management of TB/HIV coinfected patients in Eastern Europe compared with Western Europe and Latin America. PLoS ONE. 2015;10(12):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawn SD, Wilkinson RJ. ART and prevention of HIV-associated tuberculosis. The Lancet HIV. 2015;2(6):e221–2. [DOI] [PubMed] [Google Scholar]
- 11.Martinson NA, Barnes GL, Moulton LH, Msandiwa R, Hausler H, Ram M, et al. New Regimens to Prevent Tuberculosis in Adults with HIV Infection. New England Journal of Medicine. 2011. Jul 7;365(1):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawn SD, Wood R, De Cock KM, Kranzer K, Lewis JJ, Churchyard GJ. Antiretrovirals and isoniazid preventive therapy in the prevention of HIV-associated tuberculosis in settings with limited health-care resources. The Lancet Infectious Diseases. 2010;10(7):489–98. [DOI] [PubMed] [Google Scholar]
- 13.Al Abri S, Kasaeva T, Migliori GB, Goletti D, Zenner D, Denholm J, et al. Tools to implement the World Health Organization End TB Strategy: Addressing common challenges in high and low endemic countries. International Journal of Infectious Diseases. 2020;92:S60–8. [DOI] [PubMed] [Google Scholar]
- 14.Gupta-Wright A, Corbett EL, van Oosterhout JJ, Wilson D, Grint D, Alufandika-Moyo M, et al. Rapid urine-based screening for tuberculosis in HIV-positive patients admitted to hospital in Africa (STAMP): a pragmatic, multicentre, parallel-group, double-blind, randomised controlled trial. Lancet. 2018;392(10144):292–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peter JG, Zijenah LS, Chanda D, Clowes P, Lesosky M, Gina P, et al. Effect on mortality of point-of-care, urine-based lipoarabinomannan testing to guide tuberculosis treatment initiation in HIV-positive hospital inpatients: A pragmatic, parallel-group, multicountry, open-label, randomised controlled trial. The Lancet. 2016;387(10024):1187–97. [DOI] [PubMed] [Google Scholar]
- 16.Lawn SD, Wood R. Tuberculosis in antiretroviral treatment services in resource-limited settings: Addressing the challenges of screening and diagnosis. Journal of Infectious Diseases. 2011;204(SUPPL. 4):1159–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO. Xpert MTB / RIF increases timely TB detection among people living with HIV and saves lives - Information note. World Health Organisation. 2013;(1):1–4. [Google Scholar]
- 18.Méndez-Samperio P Diagnosis of Tuberculosis in HIV Co-infected Individuals: Current Status, Challenges and Opportunities for the Future. Scandinavian Journal of Immunology. 2017;86(2):76–82. [DOI] [PubMed] [Google Scholar]
- 19.Lawn SD, Brooks SV., Kranzer K, Nicol MP, Whitelaw A, Vogt M, et al. Screening for HIV-associated tuberculosis and rifampicin resistance before antiretroviral therapy using the Xpert MTB/RIF assay: A prospective study. PLoS Medicine. 2011;8(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao P, Yu Q, Zhang Y. Evaluation of a manual identification system for detection of Mycobacterium tuberculosis in a primary tuberculosis laboratory in China. Journal of International Medical Research. 2019;47(6):2666–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diriba G, Kebede A, Yaregal Z, Getahun M, Tadesse M, Meaza A, et al. Performance of Mycobacterium Growth Indicator Tube BACTEC 960 with Lowenstein-Jensen method for diagnosis of Mycobacterium tuberculosis at Ethiopian National Tuberculosis Reference Laboratory, Addis Ababa, Ethiopia. BMC Research Notes. 2017;10(1):181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmad R, Xie L, Pyle M, Suarez MF, Broger T, Steinberg D, et al. A rapid triage test for active pulmonary tuberculosis in adult patients with persistent cough. Science Translational Medicine. 2019;11(515). [DOI] [PubMed] [Google Scholar]
- 23.Wilson JW, Nilsen DM, Marks SM. Multidrug-resistant tuberculosis in patients with human immunodeficiency virus management considerations within high-resourced settings. Vol. 17, Annals of the American Thoracic Society. American Thoracic Society; 2020. p. 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carriquiry G, Otero L, González-Lagos E, Zamudio C, Sánchez E, Nabeta P, et al. A Diagnostic Accuracy Study of Xpert®MTB/RIF in HIV-Positive Patients with High Clinical Suspicion of Pulmonary Tuberculosis in Lima, Peru. PLoS ONE. 2012;7(9):3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chakravorty S, Simmons AM, Rowneki M, Parmar H, Cao Y, Ryan J, et al. The new Xpert MTB/RIF ultra: Improving detection of Mycobacterium tuberculosis and resistance to Rifampin in an assay suitable for point-of-care testing. mBio. 2017;8(4):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dorman SE, Schumacher SG, Alland D, Nabeta P, Armstrong DT, King B, et al. Xpert MTB/RIF Ultra for detection of Mycobacterium tuberculosis and rifampicin resistance: a prospective multicentre diagnostic accuracy study. The Lancet Infectious Diseases. 2018;18(1):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bahr NC, Nuwagira E, Evans EE, Cresswell FV., Bystrom PV, Byamukama A, et al. Diagnostic accuracy of Xpert MTB/RIF Ultra for tuberculous meningitis in HIV-infected adults: a prospective cohort study. The Lancet Infectious Diseases. 2018;18(1):68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.**.Cresswell FV, Tugume L, Bahr NC, Kwizera R, Bangdiwala AS, Musubire AK, et al. Xpert MTB/RIF Ultra for the diagnosis of HIV-associated tuberculous meningitis: a prospective validation study. The Lancet Infectious Diseases. 2020;20(3):308–17. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reports the superior sensitivity of Xpert 409 ® MTB/RIF Ultra in detecting TB meningitis compared with Xpert MTB/RIF and MGIT culture in HIV-infected adults with suspected meningitis, but it cannot reliably exclude TB meningitis due to its insufficient negative predictive value. These observations have important implications for the diagnosis and treatment of TB meningitis in HIV-infected patients.
- 29.Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, Dendukuri N. Xpert® MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Vol. 2014, Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.WHO. Automated Real-Time Nucleic Acid Amplification Technology for Rapid and Simultaneous Detection of Tuberculosis and Rifampicin Resistance: Xpert MTB/RIF Assay for the Diagnosis of Pulmonary and Extrapulmonary TB in Adults and Children: Policy update. World Health Organisation. 2013;1–79. [PubMed] [Google Scholar]
- 31.World Health Organization. Meeting Report of a Technical Expert Consultation : Non-inferiority analysis of Xpert MTB / RIF Ultra compared to Xpert MTB / RIF. 2017;1–11. [Google Scholar]
- 32.**.Huerga H, Mathabire Rucker SC, Cossa L, Bastard M, Amoros I, Manhiça I, et al. Diagnostic value of the urine lipoarabinomannan assay in HIV-positive, ambulatory patients with CD4 below 200 cells/μl in 2 low-resource settings: A prospective observational study. Denkinger CM, editor. PLOS Medicine. 2019;16(4):e1002792. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study describes the diagnostic value and reduction in mortality risk of including urine LAM in TB diagnostic algorithms of HIV-positive, ambulatory patients with CD4<200 cells/μl. These findings may have important implications for use of LAM in HIV-positive patients with CD4 100–200 cells/μl, and may inform revision of current guidelines.
- 33.*.Cresswell FV, Ellis J, Kagimu E, Bangdiwala AS, Okirwoth M, Mugumya G, et al. Standardized Urine-Based Tuberculosis (TB) Screening With TB-Lipoarabinomannan and Xpert MTB/RIF Ultra in Ugandan Adults With Advanced Human Immunodeficiency Virus Disease and Suspected Meningitis. Open Forum Infectious Diseases. 2020;7(4). [DOI] [PMC free article] [PubMed] [Google Scholar]; This paper describes the systematic screening of hospitalised patients with advanced HIV disease and suspected meningitis using urine LAM and Xpert® MTB/RIF Ultra assays. The finding of a high prevalence of urine TB test positivity, particularly among patients with TB meningitis, underscores the role of urine LAM as useful screening and diagnostic test for disseminated TB in patients with advanced HIV disease.
- 34.Kerkhoff AD, Sossen B, Schutz C, Reipold EI, Trollip A, Moreau E, et al. Diagnostic sensitivity of SILVAMP TB-LAM (FujiLAM) point-of-care urine assay for extra-pulmonary tuberculosis in people living with HIV. European Respiratory Journal. 2020;55:1901259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sigal GB, Pinter A, Lowary TL, Kawasaki M, Li A, Mathew A, et al. A novel sensitive immunoassay targeting the 5-methylthio-ᴅ-xylofuranose–lipoarabinomannan epitope meets the WHO’s performance target for tuberculosis diagnosis. Journal of Clinical Microbiology. 2018;56(12):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choudhary A, Patel D, Honnen W, Lai Z, Prattipati RS, Zheng RB, et al. Characterization of the Antigenic Heterogeneity of Lipoarabinomannan, the Major Surface Glycolipid of Mycobacterium tuberculosis, and Complexity of Antibody Specificities toward This Antigen. The Journal of Immunology. 2018;200(9):3053–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zheng Q, Lavis LD. Development of photostable fluorophores for molecular imaging. Vol. 39, Current Opinion in Chemical Biology. Elsevier Ltd; 2017. p. 32–8. [DOI] [PubMed] [Google Scholar]
- 38.Mitamura K, Shimizu H, Yamazaki M, Ichikawa M, Nagai K, Katada J, et al. Clinical evaluation of highly sensitive silver amplification immunochromatography systems for rapid diagnosis of influenza. Journal of Virological Methods. 2013;194(1–2):123–8. [DOI] [PubMed] [Google Scholar]
- 39.Bjerrum S, Broger T, Székely R, Mitarai S, Opintan JA, Kenu E, et al. Diagnostic accuracy of a novel and rapid lipoarabinomannan test for diagnosing tuberculosis among people with human immunodeficiency virus. Open Forum Infectious Diseases. 2020. Jan 1;7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Broger T, Sossen B, du Toit E, Kerkhoff AD, Schutz C, Ivanova Reipold E, et al. Novel lipoarabinomannan point-of-care tuberculosis test for people with HIV: a diagnostic accuracy study. The Lancet Infectious Diseases. 2019;19(8):852–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shah M, Hanrahan C, Wang ZY, Dendukuri N, Lawn SD, Denkinger CM, et al. Lateral flow urine lipoarabinomannan assay for detecting active tuberculosis in HIV-positive adults. Vol. 2016, Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Heller T, Mtemang’ombe EA, Huson MAM, Heuvelings CC, Bélard S, Janssen S, et al. Ultrasound for patients in a high HIV/tuberculosis prevalence setting: a needs assessment and review of focused applications for Sub-Saharan Africa. International Journal of Infectious Diseases. 2017;56:229–36. [DOI] [PubMed] [Google Scholar]
- 43.*.Bobbio F, Di Gennaro F, Marotta C, Kok J, Akec G, Norbis L, et al. Focused ultrasound to diagnose HIV-Associated tuberculosis (FASH) in the extremely resource-limited setting of South Sudan: A cross-sectional study. BMJ Open. 2019;9(4):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reports the yield of the FASH protocol in detecting extrapulmonary TB in HIV infected patients in an extremely resourse-limited setting. The performance of the protocol was good, particularly among severely immunosuppressed patients and should be investigated in larger studies in different settings.
- 44.Meintjes G, Brust JCM, Nuttall J, Maartens G. Review Management of active tuberculosis in adults with HIV. The Lancet HIV. 2019;6(7):e463–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Caño-muñiz S, Anthony R, Niemann S, Alffenaar JC. New Approaches and Therapeutic Options for Mycobacterium. Clinical microbiology reviews. 2018;31(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Horsburgh CR, Barry CE, Lange C. Treatment of Tuberculosis. New England Journal of Medicine. 2015;373(22):2149–60. [DOI] [PubMed] [Google Scholar]
- 47.*.Tweed CD, Dawson R, Burger DA, Conradie A, Crook AM, Mendel CM, et al. Bedaquiline, moxifloxacin, pretomanid, and pyrazinamide during the first 8 weeks of treatment of patients with drug-susceptible or drug-resistant pulmonary tuberculosis: a multicentre, open-label, partially randomised, phase 2b trial. The Lancet Respiratory Medicine. 2019;7(12):1048–58. [DOI] [PMC free article] [PubMed] [Google Scholar]; This phase 2b trial reports the outcome of different TB treatment regimens containing old and new anti-TB drugs for treatment of drug-susceptible and drug-resistant pulmonary TB. The observation that regimens containing bedaquiline and pretomanid may simplify dosing and shorten duration of treatment of drug-susceptible pulmonary TB is encouraging and warrants further evaluation.
- 48.Amagon KI, Awodele O, Akindele AJ. Methionine and vitamin B-complex ameliorate antitubercular drugs-induced toxicity in exposed patients. Pharma Res Per. 2017;5(5):360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lawn SD, Kranzer K, Edwards DJ, McNally M, Bekker LG, Wood R. Tuberculosis during the first year of antiretroviral therapy in a South African cohort using an intensive pretreatment screening strategy. AIDS. 2010;24(9):1323–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hosseinipour MC, Bisson GP, Miyahara S, Sun X, Moses A, Riviere C, et al. Empirical tuberculosis therapy versus isoniazid in adult outpatients with advanced HIV initiating antiretroviral therapy (REMEMBER): A multicountry open-label randomised controlled trial. The Lancet. 2016;387(10024):1198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.**.Blanc FX, Badje AD, Bonnet M, Gabillard D, Messou E, Muzoora C, et al. Systematic or test-guided treatment for tuberculosis in HIV-infected adults. New England Journal of Medicine. 2020;382(25):2397–410. [DOI] [PubMed] [Google Scholar]; This study describes the lack of a survival benefit associated with initiating empirical TB treatment to reduce early mortality after ART initiation in severely immunocompromised HIV-infected patients. This observation has important clinical implications for the management of severely immunosuppressed patients during the early phase of ART.
- 52.*.Grant AD, Charalambous S, Tlali M, Karat AS, Dorman SE, Hoffmann CJ, et al. Algorithm-guided empirical tuberculosis treatment for people with advanced HIV (TB Fast Track): an open-label, cluster-randomised trial. The Lancet HIV. 2020;7(1):e27–37. [DOI] [PubMed] [Google Scholar]; In this study, algorithm-guided empirical TB treatment recommended by clinic nurses for severely immunosuppressed HIV-infected patients increased coverage of TB treatment but did not reduce early mortality after ART initiation. This paper highlights the need for a better understanding of the causes of high mortality among patients with advanced HIV disease during the early phase of ART.
- 53.Lai RPJ, Meintjes G, Wilkinson RJ. HIV-1 tuberculosis-associated immune reconstitution inflammatory syndrome. Seminars in Immunopathology. 2016;38(2):185–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mesfin YM, Hailemariam D, Biadglign S, Kibret KT. Association between HIV/AIDS and Multi-Drug Resistance Tuberculosis: A Systematic Review and Meta-Analysis. Shukla D, editor. PLoS ONE. 2014;9(1):e82235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shah NS, Auld SC, Brust JCM, Mathema B, Ismail N, Moodley P, et al. Transmission of Extensively Drug-Resistant Tuberculosis in South Africa. New England Journal of Medicine. 2017;376(3):243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.**.Franke MF, Khan P, Hewison C, Khan U, Huerga H, Seung KJ, et al. Culture Conversion in Patients Treated with Bedaquiline and/or Delamanid: A Prospective Multi-country Study. American Journal of Respiratory and Critical Care Medicine. 2020. 1–39 p. [DOI] [PMC free article] [PubMed] [Google Scholar]; This large multicountry study reports that HIV-infected patient with rifampicin-resistant or MDR pulmonary TB, treated with bedaquiline and/or delamanid-containing regimens in routine care, had lower probability of sputum culture conversion within six months of treatment initiation compared with patients without HIV. This observation may have important implications for the duration of treatment of HIV-infected patients with MDR and XDR-TB.
- 57.Tornheim JA, Dooley KE. Challenges of TB and HIV co-treatment: updates and insights. Current opinion in HIV and AIDS. 2018;13(6):486–91. [DOI] [PubMed] [Google Scholar]
- 58.Patil K, Bagade S, Bonde S, Sharma S, Saraogi G. Recent therapeutic approaches for the management of tuberculosis: Challenges and opportunities. Biomedicine & Pharmacotherapy. 2018. Mar;99:735–45. [DOI] [PubMed] [Google Scholar]
- 59.Nahid P, Mase SR, Migliori GB, Sotgiu G, Bothamley GH, Brozek JL, et al. Treatment of drug-resistant tuberculosis an official ATS/CDC/ERS/IDSA clinical practice guideline. Vol. 200, American Journal of Respiratory and Critical Care Medicine. 2019;200:93–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.WHO | WHO consolidated guidelines on drug-resistant tuberculosis treatment. WHO. 2019; [PubMed] [Google Scholar]
- 61.World Health Organization. Rapid Communication : key changes to treatment of multidrug- and rifampicin-resistant tuberculosis. World Health Organization. 2018;1–7. [Google Scholar]
- 62.WHO. Rapid Communication: Key changes to the treatment of drug-resistant tuberculosis. World Health Organization. 2019;6. [Google Scholar]
- 63.Tiberi S, du Plessis N, Walzl G, Vjecha MJ, Rao M, Ntoumi F, et al. Tuberculosis: progress and advances in development of new drugs, treatment regimens, and host-directed therapies. The Lancet Infectious Diseases. 2018;3099(18):1–16. [DOI] [PubMed] [Google Scholar]
- 64.Nunn AJ, Phillips PPJ, Meredith SK, Chiang CY, Conradie F, Dalai D, et al. A trial of a shorter regimen for rifampin-resistant tuberculosis. New England Journal of Medicine. 2019;380(13):1201–13. [DOI] [PubMed] [Google Scholar]
- 65.Trebucq A, Schwoebel V, Kashongwe Z, Bakayoko A, Kuaban C, Noeske J, et al. Treatment outcome with a short multidrug-resistant tuberculosis regimen in nine African countries. International Journal of Tuberculosis and Lung Disease. 2018;22(1):17–25. [DOI] [PubMed] [Google Scholar]
- 66.Hurtado RM, Meressa D, Goldfeld AE. Treatment of drug-resistant tuberculosis among people living with HIV. Current Opinion in HIV and AIDS. 2018;13(6):478–85. [DOI] [PubMed] [Google Scholar]
- 67.Blanc F-X, Sok T, Laureillard D, Borand L, Rekacewicz C, Nerrienet E, et al. Earlier versus Later Start of Antiretroviral Therapy in HIV-Infected Adults with Tuberculosis. New England Journal of Medicine. 2011. Oct;365(16):1471–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray A, et al. Timing of initiation of antiretroviral drugs during tuberculosis therapy. New England Journal of Medicine. 2010;362(8):697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Havlir DV, Kendall MA, Ive P, Kumwenda J, Swindells S, Qasba SS, et al. Timing of antiretroviral therapy for HIV-1 infection and tuberculosis. New England Journal of Medicine. 2011;365(16):1482–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Abdool Karim SS, Naidoo K, Grobler A, Padayatchi N, Baxter C, Gray AL, et al. Integration of Antiretroviral Therapy with Tuberculosis Treatment. New England Journal of Medicine. 2011;365(16):1492–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nahid P, Dorman SE, Alipanah N, Barry PM, Brozek JL, Cattamanchi A, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clinical Infectious Diseases. 2016;63:e147–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Estill J, Ford N, Salazar-Vizcaya L, Haas AD, Blaser N, Habiyambere V, et al. The need for second-line antiretroviral therapy in adults in sub-Saharan Africa up to 2030: A mathematical modelling study. The Lancet HIV. 2016;3(3):e132–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.JK K, NG K. Highly Active Antiretroviral Therapy and Anti-tuberculosis Drug Interactions with Associated Clinical Implications: A Review. Journal of Drug Metabolism & Toxicology. 2016;7(2). [Google Scholar]
- 74.World Health Organisation (WHO). Policy Brief: Update of Recommendations on First-and Second-Line Antiretroviral Regimens. WHO Library Cataloguing-in-Publication Data. 2019;(July). [Google Scholar]
- 75.Gupta-Wright A, Corbett EL, Fielding K, Grint DJ, International D, J van Oosterhout MJ, et al. Virological failure, HIV-1 drug resistance, and early mortality in adults admitted to hospital in Malawi: an observational cohort study. The Lancet HIV. 2020;7:e620–628.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hatherill M, Chaisson RE, Denkinger CM. Addressing critical needs in the fight to end tuberculosis with innovative tools and strategies. PLOS Medicine. 2019;16(4):e1002795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zumla A, Maeurer M, Chakaya J, Hoelscher M, Ntoumi F, Rustomjee R, et al. Towards host-directed therapies for tuberculosis. Nature Reviews Drug Discovery. 2015;14:511–2. [DOI] [PubMed] [Google Scholar]
- 78.Palucci I, Delogu G. Host Directed Therapies for Tuberculosis: Futures Strategies for an Ancient Disease. Chemotherapy. 2018;63(3):172–80. [DOI] [PubMed] [Google Scholar]
- 79.Wallis RS, Hafner R. Advancing host-directed therapy for tuberculosis. Nature Reviews Immunology. 2015;15(4):255–63. [DOI] [PubMed] [Google Scholar]
- 80.Hawn TR, Matheson AI, Maley SN, Vandal O. Host-Directed Therapeutics for Tuberculosis: Can We Harness the Host? Microbiology and Molecular Biology Reviews. 2013;77(4):608–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gomes LC, Dikic I. Autophagy in antimicrobial immunity. Molecular Cell. 2014;54(2):224–33. [DOI] [PubMed] [Google Scholar]
- 82.Chandra P, Kumar D. Selective autophagy gets more selective: Uncoupling of autophagy flux and xenophagy flux in Mycobacterium tuberculosis-infected macrophages. Autophagy. 2016;12(3):608–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Watson RO, Bell SL, MacDuff DA, Kimmey JM, Diner EJ, Olivas J, et al. The Cytosolic Sensor cGAS Detects Mycobacterium tuberculosis DNA to Induce Type I Interferons and Activate Autophagy. Cell Host and Microbe. 2015;17(6):811–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chandra P, Ghanwat S, Matta SK, Yadav SS, Mehta M, Siddiqui Z, et al. Mycobacterium tuberculosis Inhibits RAB7 Recruitment to Selectively Modulate Autophagy Flux in Macrophages. Scientific Reports. 2015;5:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Duan L, Yi M, Chen J, Li S, Chen W. Mycobacterium tuberculosis EIS gene inhibits macrophage autophagy through up-regulation of IL-10 by increasing the acetylation of histone H3. Biochemical and Biophysical Research Communications. 2016;473(4):1229–34. [DOI] [PubMed] [Google Scholar]
- 86.Cervantes JL, Oak E, Garcia J, Liu H, Lorenzini PA, Batra D, et al. Vitamin D modulates human macrophage response to Mycobacterium tuberculosis DNA. Tuberculosis. 2019;116:S131–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


