Abstract
Background
Mental health of college students has become a public health issue of common concern worldwide. Especially during the COVID-19 pandemic, the problem has become even more acute. The aim of this study was to assess the association between sugar-sweetened beverages (SSB) consumption and psychological symptoms among Chinese college students in order to promote their mental health.
Methods
The study population was 6,120 college students aged 19–22 years from Anhui, Henan and Xinjiang, China. Basic demographic information, covariates and SSB Consumption data were collected through a self-assessment questionnaire. The “Multidimensional Sub-health Questionnaire of Adolescents” was used to assess the psychological symptoms of college students. The Chi-square test, one-way ANOVA and logistic regression analysis were used to investigate the differences and associations between SSB consumption and psychological symptoms among Chinese college students.
Results
The detection rate of psychological symptoms among Chinese college students was 8.1%. The detection rate of boys students was 9.4% and that of girls students was 7.1%, and the difference was statistically significant in comparison (χ2-value was 11.08, p < 0.001). After controlling for covariates, Model 2 analysis showed that compared to SSB consumption <2 time/week, college students with SSB consumption ≥2 time/week (OR = 2.96, 95% CI: 2.36, 3.70) had a higher risk of psychological symptoms (p < 0.001). The same trend was found for emotional symptoms, behavioral symptoms, and social adaptation difficulties dimensions.
Conclusion
There is an association between SSB consumption and the occurrence of psychological symptoms among Chinese college students. Future measures should be taken to reduce both SSB consumption and the incidence of psychological symptoms.
Keywords: SSB consumption, psychological symptoms, college students, association analysis, COVID-19
Introduction
Over the past 2 years or so, the COVID-19 pandemic has become a major public health emergency of international concern all over the world (Chilamakuri and Agarwal, 2021). Evidence suggested that, college students are more vulnerable to sudden changes in COVID-19 pandemic compared to the general population (Stangier et al., 2021). Mental health among college students is a significant public health concern (Mackenzie et al., 2011; Beiter et al., 2015). Several meta-analysis presented that the prevalence of psychological symptoms (e.g., depression, anxiety) among college students greatly increased during the COVID-19 pandemic (Li et al., 2021; Liyanage et al., 2021; Mulyadi et al., 2021; Santabarbara et al., 2021), including in China (Ma et al., 2020; Wang et al., 2021; Wu et al., 2021).
An emerging body of evidence has suggested that diet plays an important role in mental health (Huang et al., 2019). Current evidence also supported that healthy eating patterns that meet food-based dietary recommendations and nutrient requirements may assist in the prevention and treatment of depression and anxiety (Kris-Etherton et al., 2021). Constituting a large part of the energy intake, sugar-sweetened beverages (SSB) has been considered to be an important risk factor for obesity, type 2 diabetes mellitus, cardiovascular disease. The SSB consumptions per person are still increasing (Popkin and Hawkes, 2016). In China, the percentage of SSB consumption in children increased from 72.6 to 90.3% in 2004–2011 (Guo et al., 2021). During the COVID-19 pandemic and lockdown, changes in dietary behavior factors include increased total food consumption, decreased adherence to healthy diets, and increased snack and SSB intake (Chew and Lopez, 2021). It has also been reported that due to emotional As a way of comforting and feeling better in an anxious state, snacking and SSB intake have increased markedly during the COVID-19 pandemic (Di Renzo et al., 2020; Scarmozzino and Visioli, 2020).
A meta-analysis including 10 observational studies involving 365,289 participants indicated that SSB consumption might be associated with a modestly higher risk of depression (Hu et al., 2019). It was reported that consuming SSB 1 or more times per day versus consuming none was associated with a 26% greater prevalence of poor mental health (95% CI: 1.11–1.43) among US adults (Freije et al., 2021). Similar results were also found in Korean (Kim et al., 2022), Canada (Yu et al., 2017) and Chinese (Yu et al., 2015) adults and children and adolescents from Iranian (Zahedi et al., 2014) and China (Liu et al., 2022). A prospective data suggested that high consumption of SSB during adolescence were associated with psychological distress in young adulthood (Kleppang et al., 2021). A study of Tibetan adolescents at high altitudes in China showed an association between SSB consumption and executive function (Zhang et al., 2022). A study of Australian women during the COVID-19 pandemic showed a strong positive association between SSB consumption days and psychological distress, and SSB consumption days were higher during the COVID-19 pandemic (Grieger et al., 2022). However, there are few such studies on Chinese college students.
There is evidence to show that, 9 months after initiation of the outbreak of COVID-19, More than half of Chinese college students have depressive and anxiety symptoms (Xiao et al., 2021). In contrast, a large proportion of college students consumed SSB (82.0, 95%CI, 81.4, 82.6; Rahman et al., 2022). This study hypothesized that there is an association between SSB consumption and psychological symptoms of Chinese college students. Our study focuses on exploring whether there is an association between SSB consumption and psychological symptoms among Chinese college students during the COVID-19 pandemic. To provide reference for Chinese college students to control SSB consumption and reduce the incidence of psychological symptoms.
Materials and methods
Study design and population
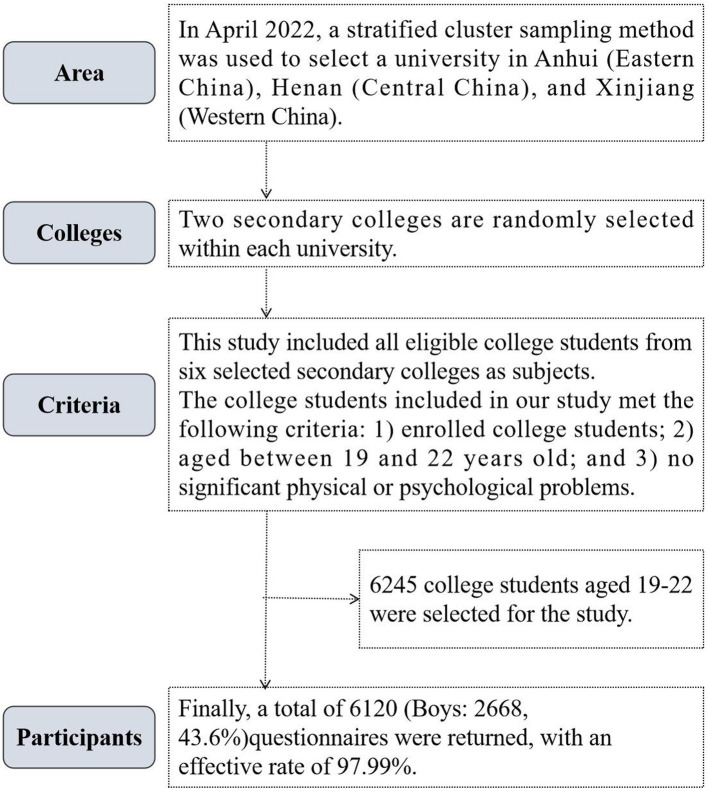
Our study was a cross-sectional original study. In April 2022, a stratified whole-group sampling method was used to sample subjects in two steps. First, one university in Anhui (Eastern China), one in Henan (Central China) and one in Xinjiang (Western China) were selected. Second, two colleges were randomly selected from each school through communication with the school administration. All eligible students participated in the survey. The college students included in our study met the following criteria: (1) enrolled college students; (2) aged between 19 and 22 years old; (3) by asking the head teacher, the included subjects had no significant physical or psychological problems. Finally, 6,245 college students aged 19–22 were selected for the study, and 6,120 (boys: 2668, 43.6%) questionnaires were returned, with an effective rate of 97.99%. The specific sampling process of the subjects is shown in Figure 1.
Figure 1.
Sampling process of Chinese college students’ subjects.
The written informed consent of the student was obtained prior to the survey, which was conducted anonymously and encoded. This research survey was approved by the Human Ethics Committee of Chizhou University (202201051).
Procedure
Under the cooperation of teachers and accompanied by graduate students majoring in human movement science, college students completed the questionnaire independently. An electronic questionnaire containing basic information, sugary drinks, and psychological symptoms was distributed to the students in the classroom. Students obtained the electronic questionnaire by scanning a QR code and submitted it on the spot when finished.
SSB consumption
Data on SSB consumption were obtained using the following question: In the past 7 days, how many time did you drink SSB. SSB include milk tea, carbonated beverages, non-carbonated sugar-sweetened non-alcoholic beverages, sports beverages, fruit juice beverages, sweetened milk and yogurt beverages, vitamin water, and sweetened iced tea that are common in our daily lives, such as Natural fruit juices, Coke, Sprite, Nutrition Express, Red Bull etc.?” (0, 1, 2, 3, 4, ≥5)? About 250 ml is consumed each time. To ensure an adequate number of participants in each group, the frequency of SSB consumption was categorized into two groups (<2 time/week, and ≥2 times/week).
Psychological symptoms
The Multidimensional Sub-health Questionnaire of Adolescents (MSQA) is a psychological symptoms designed specifically for a group of children and adolescents (including college students) and has been used in several studies (Yao et al., 2015; Yang et al., 2019; Mahara et al., 2021; Huang et al., 2022). In this paper, the survey of psychological symptoms was completed using a simple version of the MSQA with good reliability and validity. The short version of the questionnaire contains 15 items to investigate emotional symptoms (7 items, e.g., “often blaming yourself”), behavioral symptoms (4 items, e.g., “always feeling like people are working against you”), and social adaptation difficulties (4 items, e.g., “unwilling to ask for help when in trouble”). There are six response options for each items: “more than 3 months,” “more than 2 months,” “more than 1 month,” “more than 2 weeks,” “more than 1 week,” “never or less than 1 week.” Participants choose one option that can best describe their situations. The score is recorded as 1 if the response was “more than 1 month,” “more than 2 months,” and “more than 3 months” and recorded as 0 for the other responses. Scores for the three dimensions (emotional symptoms, behavioral symptoms, and social adaptation difficulties) were obtained by summing the scores for the corresponding items. Psychological symptoms were calculated by summing the scores of the all the 15 items. The cutoff points for emotional symptoms, behavioral symptoms, and social adaptation difficulties were ≥4, ≥1, and ≥2, respectively; the cutoff for psychological symptoms was ≥7.
Covariates
Covariates investigated in our study included siblings, parental education, body mass index (BMI), Socioeconomic Status (SES), sleep duration, screen time and Moderate and Vigorous Physical Activity (MVPA). Parental education is divided into primary school and below, junior high school and high school, college and above. BMI is calculated as weight (kg)/height (m)2. The SES survey includes surveys of parents’ occupations, educational attainment, and household facilities, and a composite score is calculated. According to the final score of the survey, SES defines the low grade according to the percentile <15th percentile, 15–85th percentile as the middle grade, and >85th percentile as the high grade. Sleep duration is divided into ≥8 h/days, <8 h/days. Screen time is divided into <2 h/days, ≥2 h/days. MVPA was calculated based on the time and frequency of moderate-to-high-intensity exercise that participants filled out each day for the past week. MVPA is defined as an activity performed with moderate or high effort while exercising, and one feels short of breath. Such as cycling, brisk running, playing football, lifting heavy objects, skating, etc.
Statistical analysis
Descriptive language was used to express the SSB status of different categories of Chinese college students. The description of continuous variables was expressed as mean ± standard deviation (M ± SD). Categorical variables are expressed as percentages (%). The detection rate of psychological symptoms and its three dimensions for Chinese college students with different SSB was analyzed by Chi-squares test. The relationship between SSB consumption and psychological symptoms and its three dimensions was analyzed by logistic regression using three models (Crude Model, Model 1, Model 2). Crude Model was conducted without adjustment; Model 1 was conducted after adjusting age, siblings, parental education, BMI, SES; Based on Model 1, Model 2 included sleep duration, screen time and MVPA as additional control variables. α = 0.05 was used as the two-sided test level.
Results
We conducted the SSB consumption survey on 6,120 (boys: 2668, 43.6%) Chinese college students, with an average age of (20.16 ± 1.03) years. In China, 12.2% (748/6120) of college students had SSB consumption ≥2 time/week.
The results showed that the detection rate of psychological symptoms among Chinese college students was 8.1% (495/6120). The detection rate of psychological symptoms problems was 9.4% (251/2668) in boys students and 7.1% (244/3452) in girls students, and the difference was statistically significant in comparison (χ2-value of 11.08, p < 0.01).
Overall, among college students with SSB consumption <2 time/week and SSB consumption ≥2 time/week, the detection rate of psychological symptoms was similar in terms of sex, only child, father’s education, mother’s education, sleep duration, screen time, and socioeconomic status, the differences were statistically significant. The detection rate of psychological symptoms of college students with SSB consumption ≥2 time/week was higher than that of college students with SSB consumption<2 time/week (Table 1).
Table 1.
Comparison of SSB consumption status of college students with different characteristics in China.
| Characteristics | Psychological symptoms | χ 2-value | p-value | ||
|---|---|---|---|---|---|
| Total | SSB consumption <2 time/week | SSB consumption ≥2 time/week | |||
| Sex | |||||
| Boys | 251 (9.4) | 179 (7.8) | 72 (19.5) | 50.925 | <0.001 |
| Girls | 244 (7.1) | 165 (5.4) | 79 (20.9) | 123.620 | <0.001 |
| Only child | |||||
| Yes | 90 (6.1) | 43 (3.4) | 47 (22.4) | 113.961 | <0.001 |
| No | 405 (8.7) | 301 (7.3) | 104 (19.3) | 85.825 | <0.001 |
| Father’s education | |||||
| Primary school and below | 207 (11.8) | 143 (9.9) | 64 (20.9) | 29.522 | <0.001 |
| Junior high school and above | 288 (6.6) | 201 (5.1) | 87 (19.7) | 136.759 | <0.001 |
| Mother’s education | |||||
| Primary school and below | 166 (6.1) | 104 (4.5) | 62 (16.4) | 80.092 | <0.001 |
| Junior high school and above | 329 (9.6) | 240 (7.9) | 89 (24.1) | 99.419 | <0.001 |
| Sleep duration | |||||
| ≥8 h/days | 40 (2.4) | 34 (2.2) | 6 (5.2) | 4.319 | 0.038 |
| <8 h/days | 455 (10.3) | 310 (8.2) | 145 (22.9) | 128.153 | <0.001 |
| Screen time | |||||
| <2 h/days | 53 (3.8) | 44 (3.4) | 9 (9.6) | 9.329 | 0.002 |
| ≥2 h/days | 442 (9.4) | 300 (7.4) | 142 (21.7) | 136.128 | <0.001 |
| Socioeconomic status (SES) | |||||
| Low | 97 (10.1) | 81 (9.8) | 16 (11.7) | 0.455 | 0.500 |
| Medium | 305 (7.1) | 210 (5.5) | 95 (19.5) | 129.131 | <0.001 |
| High | 93 (11.0) | 53 (7.4) | 40 (32.3) | 67.013 | <0.001 |
Descriptive statistics are presented as mean (standard deviation) and number (percentage) for continuous and categorical. SSB consumption is calculated in 250 ml bottles for each calculation. SES, low (<15th percentile), medium (15–85th percentile), high (>85th percentile). SES, socioeconomic status; BMI, body mass index; MVPA, moderate and vigorous physical activity; SSB, sugar-sweetened beverages.
Overall, the detection rate of psychological symptoms was 20.2% among college students with SSB consumption ≥2 time/week, which was higher than that of those with SSB consumption <2 time/week (6.4%). Regarding the different dimensions, emotional symptoms, behavioral symptoms, and social adaptation difficulties were detected at the highest rates among college students with SSB consumption ≥2 time/week, 26.3, 30.6, and 26.5% respectively, the differences were statistically significant (χ2-value was 302.786, 354.593, 272.343, respectively; p < 0.001; Table 2).
Table 2.
Comparison of the detection rate of psychological symptoms among college students with different SSB consumption in China.
| Psychological symptoms | SSB Consumption | No psychological symptoms | Have psychological symptoms | χ 2-value | p-value | ||
|---|---|---|---|---|---|---|---|
| N | Percentage | N | Percentage | ||||
| Boys | |||||||
| Emotional symptoms | <2 time/week | 2,117 | 92.1 | 181 | 7.9 | 75.733 | <0.001 |
| ≥2 time/week | 287 | 77.6 | 83 | 22.4 | |||
| Behavioral symptoms | <2 time/week | 2091 | 91.0 | 207 | 9.0 | 127.664 | <0.001 |
| ≥2 time/week | 261 | 70.5 | 109 | 29.5 | |||
| Social adaptation difficulties | <2 time/week | 2,122 | 92.3 | 176 | 7.7 | 69.120 | <0.001 |
| ≥2 time/week | 291 | 78.6 | 79 | 21.4 | |||
| Psychological symptoms | <2 time/week | 2,119 | 92.2 | 179 | 7.8 | 50.925 | <0.001 |
| ≥2 time/week | 298 | 80.5 | 72 | 19.5 | |||
| Girls | |||||||
| Emotional symptoms | <2 time/week | 2,892 | 94.1 | 182 | 5.9 | 252.252 | <0.001 |
| ≥2 time/week | 264 | 69.8 | 114 | 30.2 | |||
| Behavioral symptoms | <2 time/week | 2,856 | 92.9 | 218 | 7.1 | 231.641 | <0.001 |
| ≥2 time/week | 258 | 68.3 | 120 | 31.7 | |||
| Social adaptation difficulties | <2 time/week | 2,853 | 92.8 | 221 | 7.2 | 223.707 | <0.001 |
| ≥2 time/week | 259 | 68.5 | 119 | 31.5 | |||
| Psychological symptoms | <2 time/week | 2,909 | 94.6 | 165 | 5.4 | 123.620 | <0.001 |
| ≥2 time/week | 299 | 79.1 | 79 | 20.9 | |||
| Total | |||||||
| Emotional symptoms | <2 time/week | 5,009 | 93.2 | 363 | 6.8 | 302.786 | <0.001 |
| ≥2 time/week | 551 | 73.7 | 197 | 26.3 | |||
| Behavioral symptoms | <2 time/week | 4,947 | 92.1 | 425 | 7.9 | 354.593 | <0.001 |
| ≥2 time/week | 519 | 69.4 | 229 | 30.6 | |||
| Social adaptation difficulties | <2 time/week | 4,975 | 92.6 | 397 | 7.4 | 272.343 | <0.001 |
| ≥2 time/week | 550 | 73.5 | 198 | 26.5 | |||
| Psychological symptoms | <2 time/week | 5,028 | 93.6 | 344 | 6.4 | 167.798 | <0.001 |
| ≥2 time/week | 597 | 79.8 | 151 | 20.2 | |||
After controlling for covariates, Model 2 analysis showed that compared to SSB consumption <2 time/week, college students with SSB consumption ≥2 time/week (OR = 2.96, 95% CI: 2.36, 3.70) had a higher risk of psychological symptoms (p < 0.001). The same trend was found for emotional symptoms, behavioral symptoms, and social adaptation difficulties dimensions. And the trends were consistent for college boys and girls (Table 3).
Table 3.
Logistic regression analysis of SSB consumption and psychological symptoms among Chinese college students (n = 6,120).
| Psychological symptoms | SSB Consumption | Odds ratio (95% confidence interval) | ||
|---|---|---|---|---|
| Crude Model | Model 1 | Model 2 | ||
| Boys | ||||
| Emotional symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 3.38 (2.54, 4.51)a | 2.82 (2.05, 3.88)a | 2.82 (2.05, 3.89)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Behavioral symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 4.22 (3.24, 5.50)a | 3.94 (2.96, 5.25)a | 3.61 (2.70, 4.83)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Social adaptation difficulties | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 3.27 (2.44, 4.39)a | 2.92 (2.12,4.01)a | 2.86 (2.07,3.96)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Psychological symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 2.86 (2.12,3.86)a | 2.20 (1.59,3.05)a | 1.90 (1.37,2.64)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Girls | ||||
| Emotional symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 6.86 (5.26,8.95)a | 8.06 (6.00,10.83)a | 6.98 (5.18,9.40)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Behavioral symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 6.09 (4.71, 7.88)a | 6.83 (5.17, 9.02)a | 5.92 (4.47, 7.85)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Social adaptation difficulties | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 5.93 (4.59, 7.67)a | 7.42 (5.58, 9.85)a | 6.44 (4.83, 8.58)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Psychological symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 4.66 (3.47, 6.25)a | 5.49 (3.98, 7.56)a | 4.70(3.40,6.50)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Total | ||||
| Emotional symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00(Reference) |
| ≥2 time/week | 4.93 (4.06,5.99)a | 4.62 (3.75,5.69)a | 4.31 (3.49,5.31)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Behavioral symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 5.14 (4.27,6.18)a | 5.08 (4.18,6.17)a | 4.55(3.73,5.54)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Social adaptation difficulties | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 4.51 (3.72,5.47)a | 4.36 (3.57, 5.34)a | 3.99 (3.26, 4.91)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
| Psychological symptoms | <2 time/week | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| ≥2 time/week | 3.70 (3.00, 4.56)a | 3.42 (2.74, 4.27)a | 2.96 (2.36, 3.70)a | |
| p for trend | <0.001 | <0.001 | <0.001 | |
Model 1 controlled for age, only child, parental education, BMI, and SES; Model 2 controlled for Sleep duration, screen time, and MVPA on top of Model 1. SES, socioeconomic status; BMI, body mass index; MVPA, moderate and vigorous physical activity; SSB, sugar-sweetened beverages.
p < 0.001.
Discussion
Our study investigated SSB consumption and psychological symptoms of Chinese college students, and analyzed the association between the two. Our results showed a strong association between SSB consumption and psychological symptoms among Chinese college students. After controlling for relevant demographic factors and confounders, compared to SSB consumption <2 time/week, college students with SSB consumption ≥2 time/week had a higher risk of psychological symptoms.
More and more studies have confirmed that SSB consumption among children and adolescents is increasing rapidly year by year, and college students are an important stage of SSB consumption and an important group of SSB consumption (Sharma et al., 2020). The Scientific Research Report on Dietary Guidelines for Chinese Residents (2021) shows that the sales of sugary beverages are increasing year by year, and children and adolescents have the highest consumption rate of sugary beverages at more than 30 and 25%, which should draw sufficient attention (Residents, 2021). In addition, 42.1% of free sugar intake in urban population comes from sugary drinks and dairy beverages. Studies have confirmed that excessive SSB consumption will have more adverse effects on the physical and mental health of children and adolescents (Russo et al., 2020; Roesler et al., 2021). Studies have shown that during the COVID-19 pandemic lockdown, lifestyle changes such as decreased physical activity and increased SSB consumption have led to increased obesity (Sanchez et al., 2021; Pulvera et al., 2022). The occurrence of obesity due to excessive consumption of SSB is also an important factor to further increase the occurrence of psychological symptoms, which has adverse effects on mental health. This is an important reason for the higher detection rate of psychological symptoms in college students with higher SSB consumption.
Previous studies have tended to analyze the relationship between SSB consumption and physical function, while relatively few studies have addressed the relationship between SSB consumption and mental health, especially in college student populations with high and unstable psychological burdens. Our study analyzed the association between SSB consumption and psychological symptoms among Chinese college students. The results showed the association between SSB consumption and psychological symptoms. Our research also showed that the detection rate of psychological symptoms was significantly higher among Chinese college boys (9.4%) than girls (7.1%), which is consistent with the findings of related studies (Sagar-Ouriaghli et al., 2020).One of the main reasons is that, influenced by the traditional Chinese educational ideology, families and society give college boys greater hopes and responsibilities, which invariably increases the psychological burden of college boys, resulting in higher psychological symptoms than girls. Secondly, compared with girls students, boys college students have more bad life and eating habits, such as smoking, alcoholism, staying up late, drinking too many sugary drinks, obesity, etc. These bad life or eating habits are risk factors for the occurrence of psychological symptoms problems.
There are also some research explanations on the reciprocal mechanism of SSB consumption and psychological symptoms. Studies have confirmed that excessive intake of SSB in children and adolescents promotes the secretion of dopamine in the brain, which makes the body feel pleasure and stimulates the increase of appetite, leading to the occurrence of overweight and obesity, thus leading to the occurrence of psychological symptoms (Anjum et al., 2018). It was also confirmed that high sugar consumption groups (>100 g/days) were significantly associated with higher fatigue, social activity distress, and depression compared to low sugar consumption groups (<100 g/days) (Maaz et al., 2020). Potential deleterious effects of low to moderate intake of SSBs on cardiovascular risk markers such as low-density lipoprotein particles, fasting glucose and high sucrose C-reactive protein that contribute to an increased risk of psychological symptoms (Aeberli et al., 2011). In addition to fructose intake that promotes insulin resistance, hypertension, and dyslipidemia, leading to metabolic dysregulation, fructose intake stimulates the hypothalamic–pituitary–adrenal (HPA) axis, leading to elevated glucocorticoids, which in turn Elevated hormones are often associated with serious psychiatric consequences, such as suicide, psychotic disorders, depression, mania, and panic disorder (Harrell et al., 2015).
There are several advantages of this study. First, the study has a larger sample size, which can better represent the situation of SSB consumption and psychological symptoms among Chinese college students, and the results are more convincing. Second, the study is the first to analyze the association between SSB consumption and psychological symptoms among Chinese college students, which provides a reference and help for the development of education and public health policies by Chinese educational and administrative authorities (Farsad-Naeimi et al., 2020; Yin et al., 2021). Our study also has some limitations. For one, this study was a cross-sectional survey study, and it was only able to analyze the association between SSB consumption and psychological symptoms, but not to understand the causal causality between the two. Second, the investigation of covariates in this study was limited, only family factors, parental education, SES, diet, sleep, and physical activity were investigated, and more factors, such as video screen time and academic stress, should be investigated in future studies to better analyze the association that exists between SSB consumption and psychological symptoms. Third, it is difficult to accurately measure SSB consumption due to the influence of the subjects’ recall ability; at the same time, questionnaires assessing mental health may underreport results because students may be ashamed to answer certain questions.
Conclusion
In conclusion, there was an association between SSB consumption and psychological symptoms among Chinese college students. Future measures should be taken to reduce both SSB consumption and the incidence of psychological symptoms. The results of this study will provide a reference for the primary and secondary prevention of mental health among Chinese university students. It will also provide a reference and help for the development of education and public health policies by Chinese university education and government departments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Human Ethics Committee of Chizhou University (202201051). This study was conducted in accordance with the Declaration of Helsinki. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YW and CB: Conceptualization. HL: Data curation. CB: Formal analysis. HL: Funding acquisition. RC: Investigation. JZ: Methodology. YW: Project administration. YW: Resources. CB: Software. RC: Supervision. JZ: Validation. HL: Visualization. YW and CB: Writing – original draft. YW and CB: Writing – review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This project is funded by the Anhui Provincial Department of Education “Anhui Province Higher Education Provincial Quality Engineering Major Project“ (2021jyxm1013).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank the students and parents who participated in this study, as well as the staff who participated in the data testing of this study.
References
- Aeberli I., Gerber P. A., Hochuli M., Kohler S., Haile S. R., Gouni-Berthold I., et al. (2011). Low to moderate sugar-sweetened beverage consumption impairs glucose and lipid metabolism and promotes inflammation in healthy young men: a randomized controlled trial. Am. J. Clin. Nutr. 94, 479–485. doi: 10.3945/ajcn.111.013540, PMID: [DOI] [PubMed] [Google Scholar]
- Anjum I., Jaffery S. S., Fayyaz M., Wajid A., Ans A. H. (2018). Sugar beverages and dietary sodas impact on brain health: a mini literature review. Cureus 10:e2756. doi: 10.7759/cureus.2756, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beiter R., Nash R., Mccrady M., Rhoades D., Linscomb M., Clarahan M., et al. (2015). The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J. Affect. Disord. 173, 90–96. doi: 10.1016/j.jad.2014.10.054, PMID: [DOI] [PubMed] [Google Scholar]
- Chew H., Lopez V. (2021). Global impact of COVID-19 on weight and weight-related behaviors in the adult population: a scoping review. Int. J. Environ. Res. Public Health 18:1876. doi: 10.3390/ijerph18041876, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilamakuri R., Agarwal S. (2021). COVID-19: characteristics and therapeutics. Cells 10:206. doi: 10.3390/cells10020206, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Renzo L., Gualtieri P., Cinelli G., Bigioni G., Soldati L., Attina A., et al. (2020). Psychological aspects and eating habits during COVID-19 home confinement: results of EHLC-COVID-19 Italian online survey. Nutrients 12:2152. doi: 10.3390/nu12072152, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsad-Naeimi A., Asjodi F., Omidian M., Askari M., Nouri M., Pizarro A. B., et al. (2020). Sugar consumption, sugar sweetened beverages and attention deficit hyperactivity disorder: a systematic review and meta-analysis. Complement. Ther. Med. 53:102512. doi: 10.1016/j.ctim.2020.102512, PMID: [DOI] [PubMed] [Google Scholar]
- Freije S. L., Senter C. C., Avery A. D., Hawes S. E., Jones-Smith J. C. (2021). Association between consumption of sugar-sweetened beverages and 100% fruit juice with poor mental health among US adults in 11 US states and the District of Columbia. Prev. Chronic Dis. 18:E51. doi: 10.5888/pcd18.200574, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grieger J. A., Habibi N., O'Reilly S. L., Harrison C. L., Moran L. J., Vo H., et al. (2022). Psychological distress and its association with intake of sugar-sweetened beverages, discretionary foods, and alcohol in women during the COVID-19 pandemic in Australia. Nutrition 103-104:111794. doi: 10.1016/j.nut.2022.111794, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo H., Phung D., Chu C. (2021). Sociodemographic, lifestyle, behavioral, and parental factors associated with sugar-sweetened beverage consumption in children in China. PLoS One 16:e0261199. doi: 10.1371/journal.pone.0261199, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell C. S., Burgado J., Kelly S. D., Johnson Z. P., Neigh G. N. (2015). High-fructose diet during periadolescent development increases depressive-like behavior and remodels the hypothalamic transcriptome in male rats. Psychoneuroendocrinology 62, 252–264. doi: 10.1016/j.psyneuen.2015.08.025, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu D., Cheng L., Jiang W. (2019). Sugar-sweetened beverages consumption and the risk of depression: a meta-analysis of observational studies. J. Affect. Disord. 245, 348–355. doi: 10.1016/j.jad.2018.11.015, PMID: [DOI] [PubMed] [Google Scholar]
- Huang Q., Liu H., Suzuki K., Ma S., Liu C. (2019). Linking what we eat to our mood: a review of diet, dietary antioxidants, and depression. Antioxidants (Basel) 8:376. doi: 10.3390/antiox8090376, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Yuan Q., Ge M., Sheng X., Yang M., Shi S., et al. (2022). Childhood trauma and non-suicidal self-injury among Chinese adolescents: the mediating role of psychological sub-health. Front. Psych. 13:798369. doi: 10.3389/fpsyt.2022.798369, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Hong C., Lee G. (2022). Association between sugar-sweetened beverage consumption and depression and suicidal ideation among Korean adults: a cross-sectional study from the 2014 and 2016 Korean National Health and nutrition examination survey (KNHANES). Nutr. Res. Pract. 16, 194–204. doi: 10.4162/nrp.2022.16.2.194, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleppang A. L., de Ridder K., Haugland S. H., Stea T. H. (2021). Physical activity, sugar-sweetened beverages, whole grain bread and insomnia among adolescents and psychological distress in adulthood: prospective data from the population-based HUNT study. Int. J. Behav. Nutr. Phys. Act. 18:143. doi: 10.1186/s12966-021-01215-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kris-Etherton P. M., Petersen K. S., Hibbeln J. R., Hurley D., Kolick V., Peoples S., et al. (2021). Nutrition and behavioral health disorders: depression and anxiety. Nutr. Rev. 79, 247–260. doi: 10.1093/nutrit/nuaa025, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang A., Wu Y., Han N., Huang H. (2021). Impact of the COVID-19 pandemic on the mental health of college students: a systematic review and meta-analysis. Front. Psychol. 12:669119. doi: 10.3389/fpsyg.2021.669119, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Chen T., Chen M., Ma Y., Ma T., Gao D., et al. (2022). Sugar-sweetened beverages and depressive and social anxiety symptoms among children and adolescents aged 7-17 years, stratified by body composition. Front. Nutr. 9:888671. doi: 10.3389/fnut.2022.888671, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liyanage S., Saqib K., Khan A. F., Thobani T. R., Tang W. C., Chiarot C. B., et al. (2021). Prevalence of anxiety in university students during the COVID-19 pandemic: a systematic review. Int. J. Environ. Res. Public Health 19:62. doi: 10.3390/ijerph19010062, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., Zhao J., Li Y., Chen D., Wang T., Zhang Z., et al. (2020). Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 29:e181. doi: 10.1017/S2045796020000931, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maaz A., Filippos K., Ramos R. C. (2020). 25 association of added dietary sugar and worse mental health status in inflammatory bowel disease. Gastroenterology 158, 23–26. doi: 10.1016/S0016-5085(20)30705-8 [DOI] [Google Scholar]
- Mackenzie S., Wiegel J. R., Mundt M., Brown D., Saewyc E., Heiligenstein E., et al. (2011). Depression and suicide ideation among students accessing campus health care. Am. J. Orthopsychiatry 81, 101–107. doi: 10.1111/j.1939-0025.2010.01077.x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahara G., Liang J., Zhang Z., Ge Q., Zhang J. (2021). Associated factors of suboptimal health status among adolescents in China: a cross-sectional study. J. Multidiscip. Healthc. 14, 1063–1071. doi: 10.2147/JMDH.S302826, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulyadi M., Tonapa S. I., Luneto S., Lin W. T., Lee B. O. (2021). Prevalence of mental health problems and sleep disturbances in nursing students during the COVID-19 pandemic: a systematic review and meta-analysis. Nurse Educ. Pract. 57:103228. doi: 10.1016/j.nepr.2021.103228, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin B. M., Hawkes C. (2016). Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 4, 174–186. doi: 10.1016/S2213-8587(15)00419-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulvera R., Altman E., Avina L., Thompson H., Schillinger D., Madsen K. (2022). Pandemic-related financial hardship and disparities in sugar-sweetened beverage consumption and purchasing among San Francisco Bay Area residents during COVID-19. Prev. Med. Rep. 26:101759. doi: 10.1016/j.pmedr.2022.101759, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman H. A., Amornsriwatanakul A., Abdul-Mumin K. H., Agustiningsih D., Chaiyasong S., Chia M., et al. (2022). Prevalence of health-risk behaviors and mental well-being of ASEAN university students in COVID-19 pandemic. Int. J. Environ. Res. Public Health 19:8528. doi: 10.3390/ijerph19148528, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Residents W. G. O. S. (2021). A brief version of scientific report on dietary guidelines for Chinese Residents (2021). J. Nutr. 43:1. doi: 10.13325/j.cnki.acta.nutr.sin.2021.02.001 [DOI] [Google Scholar]
- Roesler A., Rojas N., Falbe J. (2021). Sugar-sweetened beverage consumption, perceptions, and disparities in children and adolescents. J. Nutr. Educ. Behav. 53, 553–563. doi: 10.1016/j.jneb.2021.04.004, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo R. G., Northridge M. E., Wu B., Yi S. S. (2020). Characterizing sugar-sweetened beverage consumption for US children and adolescents by race/ethnicity. J. Racial Ethn. Health Disparities 7, 1100–1116. doi: 10.1007/s40615-020-00733-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagar-Ouriaghli I., Godfrey E., Graham S., Brown J. (2020). Improving mental health help-seeking Behaviours for male students: a framework for developing a complex intervention. Int. J. Environ. Res. Public Health 17:4965. doi: 10.3390/ijerph17144965, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez E., Lecube A., Bellido D., Monereo S., Malagon M. M., Tinahones F. J., et al. (2021). Leading factors for weight gain during COVID-19 lockdown in a Spanish population: a cross-sectional study. Nutrients 13:894. doi: 10.3390/nu13030894, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabarbara J., Ozamiz-Etxebarria N., Idoiaga N., Olaya B., Bueno-Novitol J. (2021). Meta-analysis of prevalence of depression in dental students during COVID-19 pandemic. Medicina (Kaunas) 57:1278. doi: 10.3390/medicina57111278, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarmozzino F., Visioli F. (2020). Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods 9:675. doi: 10.3390/foods9050675, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma A., Jain M., Nahar V. K., Sharma M. (2020). Determining predictors of change in sugar sweetened beverage consumption behaviour among university students in India. Int. J. Adolesc. Med. Health 34:1. doi: 10.1515/ijamh-2019-0078, PMID: [DOI] [PubMed] [Google Scholar]
- Stangier U., Kananian S., Schuller J. (2021). Perceived vulnerability to disease, knowledge about COVID-19, and changes in preventive behavior during lockdown in a German convenience sample. Curr. Psychol. 41, 7362–7370. doi: 10.1007/s12144-021-01456-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Wen W., Zhang H., Ni J., Jiang J., Cheng Y., et al. (2021). Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: a systematic review and meta-analysis. J. Am. Coll. Heal., 1–8. doi: 10.1080/07448481.2021.1960849, PMID: [DOI] [PubMed] [Google Scholar]
- Wu X., Tao S., Zhang Y., Li S., Ma L., Yu Y., et al. (2021). Geographic distribution of mental health problems among Chinese college students during the COVID-19 pandemic: Nationwide, web-based survey study. J. Med. Internet Res. 23:e23126. doi: 10.2196/23126, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao P., Chen L., Dong X., Zhao Z., Yu J., Wang D., et al. (2021). Anxiety, depression, and satisfaction with life among college students in China: nine months after initiation of the outbreak of COVID-19. Front. Psych. 12:777190. doi: 10.3389/fpsyt.2021.777190, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang R., Li D., Wang J., Wan Y., Tao F., Zhang S. (2019). Association of health literacy and physical sub-health among Chinese middle school students. Wei Sheng Yan Jiu 48, 711–716. doi: 10.19813/j.cnki.weishengyanjiu.2019.05.003 [DOI] [PubMed] [Google Scholar]
- Yao Y., Wang L., Chen Y., Kang Y., Gu Q., Fang W., et al. (2015). Correlation analysis of anxiety status and sub-health status among students of 13-26 years old. Int. J. Clin. Exp. Med. 8, 9810–9814. [PMC free article] [PubMed] [Google Scholar]
- Yin J., Zhu Y., Malik V., Li X., Peng X., Zhang F. F., et al. (2021). Intake of sugar-sweetened and low-calorie sweetened beverages and risk of cardiovascular disease: a meta-analysis and systematic review. Adv. Nutr. 12, 89–101. doi: 10.1093/advances/nmaa084, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B., He H., Zhang Q., Wu H., Du H., Liu L., et al. (2015). Soft drink consumption is associated with depressive symptoms among adults in China. J. Affect. Disord. 172, 422–427. doi: 10.1016/j.jad.2014.10.026, PMID: [DOI] [PubMed] [Google Scholar]
- Yu Z. M., Parker L., Dummer T. (2017). Associations of coffee, diet drinks, and non-nutritive sweetener use with depression among populations in eastern Canada. Sci. Rep. 7:6255. doi: 10.1038/s41598-017-06529-w, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahedi H., Kelishadi R., Heshmat R., Motlagh M. E., Ranjbar S. H., Ardalan G., et al. (2014). Association between junk food consumption and mental health in a national sample of Iranian children and adolescents: the CASPIAN-IV study. Nutrition 30, 1391–1397. doi: 10.1016/j.nut.2014.04.014, PMID: [DOI] [PubMed] [Google Scholar]
- Zhang F., Yin X., Liu Y., Li M., Gui X., Bi C. (2022). Association between sugar-sweetened beverage consumption and executive function among Chinese Tibetan adolescents at high altitude. Front. Nutr. 9:939256. doi: 10.3389/fnut.2022.939256, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.