Abstract
Background
Existing studies of patient-reported outcomes (PRO) following total knee arthroplasty (TKA) based on fixation methods (cemented vs cementless) are limited to single centers with small sample sizes. Using multicentered data,, we compared baseline and early post-operative global and condition-specific PROs between patients undergoing cemented versus cementless TKA.
Methods
With PROs prospectively collected through Comparative Effectiveness Pulmonary Embolism Prevention After Hip and Knee Replacement (PEPPER) trial (ClinicalTrials.gov: NCT02810704), we examined pre- and post-operative (1, 3, and 6-months) outcomes in 5,961 patients undergoing primary TKA enrolled by 28 medical centers between December 2016 and August 2021. Outcomes included the short-form of the Knee Injury and Osteoarthritis Outcome Score (KOOS-Jr.), the Patient-Reported Outcomes Measurement Information System Physical Health (PROMIS-PH), and the Numeric Pain Rating Scale (NPRS). To minimize selection bias, we performed a 1-to-1 propensity score matched analysis to assess relative pre- to post-operative change in outcomes within and between cemented and cementless TKA groups.
Results
With greater than 90% follow-up, significant pre to- post-operative improvements were observed in both groups. At 6 months, the cemented TKA group achieved a 3.3 point (55% of the Minimum Clinically Important Difference) greater improvement in the mean KOOS-Jr. (95%CI: 0.36, 6.30; P = 0.028) than did the cementless group with no significant between-group differences in PROMIS-PH and NPRS.
Conclusions
In a large cohort of primary TKAs, patients with cemented fixation reported early incremental benefit in KOOS-Jr. over those with cementless TKA. Future studies are warranted to capture longer follow-up of PROs.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-022-05899-1.
Keywords: Knee arthroplasty, Cemented TKA, Cementless TKA, Patient-Reported outcomes
Background
There has been a large increase in the rate of total knee arthroplasty (TKA) over the past decade in the United States. Among the Medicare population, roughly 351,000 TKA were performed in 2010, more than doubling to 738,000 in 2020 [1]. TKA provides relief of pain and recovery of functional status for patients with knee osteoarthritis [2, 3]. Two types of fixation of TKA implants can be utilized, with either the use of polymethyl-methacrylate (PMMA) bone cement or cementless implants which most often utilize a porous or textured surface to promote direct osseous integration of the implant.
Previous studies have attempted to determine the superiority of these two implant fixation methods. Based on early studies demonstrating their superiority, cemented TKA has been widely used in the United States as the gold standard [4–7]. However, recent papers have challenged the superiority of cement. Some show that there are no statistically significant differences in clinical and cost outcomes [8–16], while others suggest that cementless TKA achieves greater survivorship and long-term functional recovery [17, 18] and lower procedure cost [19]. While cement provides immediate fixation, cementless fixation requires the biologic process of osseous integration to occur, and some reports show higher early rates of subtle radiolucencies, implant migration, aseptic loosening and higher early pain scores in cementless TKA [6, 20–23]. Because of the importance of pain relief and early function to our patients following TKA [24], the relevance of early outcomes following TKA should not be underestimated.
Lacking from the current body of evidence are rigorous comparisons of pre-and early post-operative patient-reported measures of pain and functional disability from a large multicenter cohort. Researchers have only recently focused on patient-reported outcomes (PRO) as a valuable tool to assess patient recovery, pain and function following TKA [12–18, 25, 26]. With few exceptions [18, 26], most studies have found no statistically significant differences in PROs between cemented and cementless TKA [12–17, 25]. However, these studies have been focused on the experience of a single surgeon or single institution, with limited generalizability. Further, many prior studies cited in the literature compare outcomes of older cemented and cementless TKA technologies [27], and recent design improvements with more modern designs remain to be investigated in a contemporary dataset.
In order to improve the understanding of early patient recovery after TKA, we analyzed global and condition-specific PROs between patients who received cemented TKA compared with cementless implants using prospectively collected data from the multicenter Patient-Centered Outcomes Research Institute (PCORI) funded Comparative Effectiveness of Pulmonary Embolism Prevention after Hip and Knee Replacement (PEPPER) trial.
Methods
Study design
PROs were prospectively collected through the PEPPER trial (NCT02810704 at ClinicalTrials.gov), a large, multi-centered, randomized clinical trial evaluating safety and effectiveness of prophylactic antithrombotic medication after total hip and knee arthroplasty [28]. A central (single) human subjects review board from the Medical University of South Carolina provided regulatory review of the study (Approval Number: Pro00053742). All procedures were performed in accordance with the ethical standards of the institution.
While PEPPER is an ongoing randomized trial for antithrombotic drug safety, assignment to cement or cementless TKA was at the discretion of participating surgeons. Furthermore, the primary safety outcomes of venous thromboembolism, bleeding, and death in PEPPER are currently blinded until the trial ends due to data integrity protocols, and as such, are not available for our analysis. Nevertheless, PEPPER provides data on 6 month longitudinal PROs (global and condition-specific), patient characteristics (age, Body Mass Index (BMI), gender, race, ethnicity, education, working status, drinking, smoking, and comorbidity), and implant fixation methods (cemented and cementless), collected from study participants enrolled by 28 North American hospitals (among a total of 31 participant centers). This enabled us to analyze prospectively collected data to evaluate the influence of implant fixation method of TKA on short term PROs. Specifically, we included participants enrolled in the PEPPER trial between 12/19/2016 and 8/31/2021 and performed 1-to-1 propensity score matched analysis to compare outcomes between cemented and cementless TKA.
Data outcomes
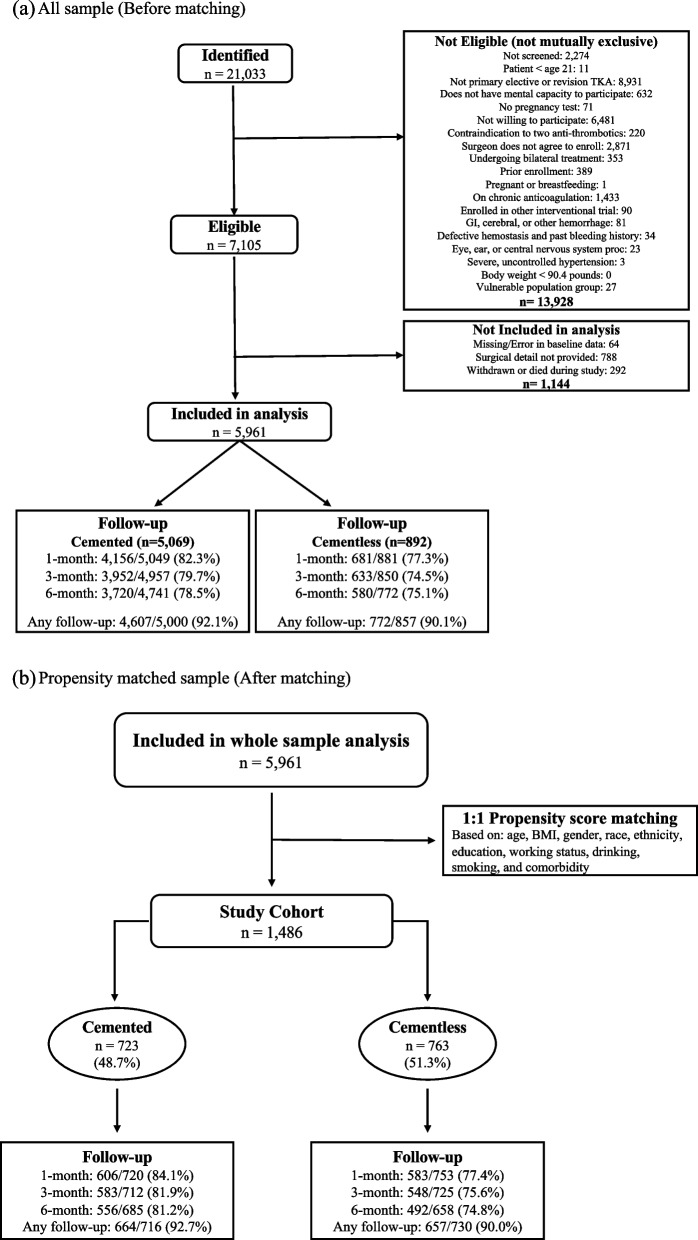
We included adult patients undergoing elective primary TKA who provided an informed consent, excluding those on chronic anticoagulation or who had comorbidities that confounded the assessment of antithrombotic medication safety. We categorized patients by two treatment subgroups, which were utilized at the discretion of the surgeon: (1) cemented TKA and (2) cementless TKA. Even though PEPPER enrolled subjects with knee revision or unicompartmental knee replacement procedures, they were excluded from our analysis in order to focus on the question of cemented vs cementless fixation in a more homogenous cohort of primary TKA. We also excluded those who died or withdrew from the study because they lacked complete PRO’s. Detailed inclusion and exclusion criteria for study participation can be found in Fig. 1-(a).
Fig. 1.
Study cohort and follow-up by implant fixation methods (a) All sample (Before matching) Note: PROs were collected at 1-month, 3-month, and 6-month using centralized telephone interviews, web-based surveys, and postage-paid reply mail surveys. (b) Propensity matched sample (After matching) Note: PROs were collected at 1-month, 3-month, and 6-month using centralized telephone interviews, web-based surveys, and postage-paid reply mail surveys
Using centralized telephone interviews, web-based surveys, and postage-paid reply mail surveys, PROs were collected pre-operatively and at 1-month (37 days post-operative, -7/ + 10 days), 3-month (90 days post-operative, -10/ + 14 days), and 6-months (180 days post-operative, -28/ + 28 days). Patients were contacted for follow-up regardless of complication, or if they changed or discontinued antithrombotic medications. In addition to PROs, patient demographic information and comorbidities were collected preoperatively, and operative characteristics, including the use of cement, were specifically reported by the enrolling center.
Primary outcomes include validated measure of patient-reported knee function, general physical health, and pain. Knee function was evaluated using the short form version of the Knee Injury and Osteoarthritis Outcome Score (KOOS-Jr.), which contains 7 questions to assess pain, function, and quality of daily living within the past week [29]. The KOOS-Jr. is scored on a 0–100 scale with a larger value representing a higher knee function [30]. The Patient-Reported Outcomes Measurement Information System Physical Health (PROMIS-PH) Summary was used to assess global pain and general (physical) health. The PROMIS-PH is a 10-item measure, calculated using a T-score in which distributions are standardized with a mean (standard deviation) of 50 (10), with greater scores indicating better health [31]. The Numeric Pain Rating Scale (NPRS) is scored on a 0–10 scale with a lower score representing less pain [32]. We also report the proportion of patients who achieved a Minimum Clinically Important Difference (MCID) using threshold for KOOS-Jr., PROMIS-PH, and NPRS of 6, 7.9, and 2 points respectively [30, 32].
Statistical analysis
One of the challenges in comparing PROs between cemented and cementless TKA is that even after adjusting for observable characteristics of patients, there might still be confounders that lead to biased estimates of the association between implant fixation methods and PROs. For example, if many surgeons tend to use cementless fixation in younger patients and use cemented fixation in older patients due to the fact that younger patients are more likely to have better bone quality, then there would be a concern for potential bias due to extrapolation even after controlling for age. Also, if surgeons’ motivation and surgical skills, which are hard to observe, are correlated with decision on cemented/cementless fixation, accounting for observable characteristics could not help reduce bias.
To minimize these biases, we conducted a propensity score matched analysis. Specifically, we employed single nearest-neighbor matching (also known as 1-to-1 matching) in which each cementless case is matched to a cemented participant that most closely resembles their observed patient characteristics. We matched cases to control based on age, BMI, gender, race, ethnicity, education, working status, drinking, smoking, and comorbidity. Participants who are outside the “region of common support” were dropped from the analysis. There are several reasons why we used 1-to-1 matching. First, on average, discordant matches can lead to biased estimates in multiple nearest neighbor matching than in 1-to-1 matching [33]. Despite excluding unmatched observations, the overall power is not compromised because the improved quality of matches from 1-to-1 matching can lead to increased power [34]. Based on our propensity matched sample size, our analysis was sufficiently powered to detect a 2.0 point between-group difference in KOOS-Jr., a 1.2-point difference in PROMIS-PH, and a 0.35-point difference in NPRS, with at least 85% power. These differences compare favorably with the previously mentioned MCIDs for each measure. We also imposed a replacement as well as a caliper (0.25 standard deviation) to increase the average quality of matches, further reducing bias [35]. We estimated the Average Treatment Effect (ATE) for the sample within the range of common support [36]. Stata-17.0-MP (StataCorp, College Station, TX) was used to conduct all analyses.
Results
Study population
Among 5,961 TKA patients who were eligible for this analysis, there were 5,069 (85.0%) cemented and 892 (15.0%) cementless procedures. Patients undergoing bilateral procedures or second side surgery were excluded from PEPPER. Before constructing a propensity score matched sample, patients with cemented TKA had a lower BMI, were more likely to be white, non-Hispanic, and college graduates. They were also more likely to be a former smoker compared to patients with cementless TKA (Appendix A1). Excluded cases who died or withdrew from the study were older (66.1 compared to 64.2; p < 0.001) and more likely to be white (89.2% compared to 77.9%; p = 0.021) compared to those included in the analysis.
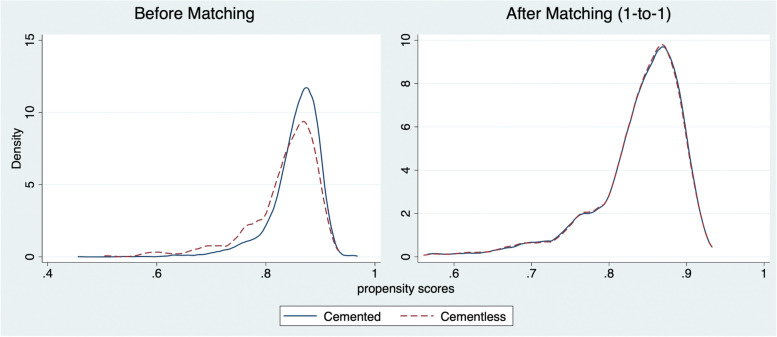
Following propensity-matching, the sample size reduced to 1,486 (cemented: 723, cementless: 763). There were no significant differences in observable patient characteristics or comorbidities between cemented and cementless TKA (Table 1). The distributions of estimated propensity scores for both groups before and after matching confirm that our propensity score matching approach achieved balance between groups with respect to observed covariates (Fig. 2).
Table 1.
Descriptive statistics from Propensity matched sample (1:1 matching)
| Baseline Characteristic | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| Cemented | Cementless | All | p-value | |
| AGE | ||||
| Age (mean) | 64.5 | 64.3 | 64.4 | 0.691 |
| Body Mass Index (BMI) | ||||
| BMI (mean) | 33.1 | 33.2 | 33.1 | 0.731 |
| Gender | ||||
| Female (%) | 57.7 | 56.1 | 56.9 | 0.538 |
| Male (%) | 42.3 | 43.9 | 43.1 | |
| Race | ||||
| White (%) | 78.7 | 76.3 | 77.5 | 0.536 |
| Black (%) | 13.6 | 15.1 | 14.3 | |
| Other/Multiple (%) | 7.7 | 8.6 | 8.2 | |
| Ethnicity | ||||
| Hispanic (%) | 4.6 | 3.7 | 4.1 | 0.385 |
| Non-Hispanic (%) | 95.4 | 96.3 | 95.9 | |
| Education | ||||
| Less than college (%) | 60.2 | 64.5 | 62.4 | 0.086 |
| College graduate (%) | 39.8 | 35.5 | 37.6 | |
| Work | ||||
| Working (%) | 36.2 | 36.6 | 36.4 | 0.877 |
| Unemployed (%) | 2.2 | 2.1 | 2.2 | |
| Sick leave or maternity leave (%) | 14.3 | 15.6 | 14.9 | |
| Disabled due to hip or knee pain (%) | 47.3 | 45.7 | 46.5 | |
| Alcohol | ||||
| Never (%) | 29.3 | 31.3 | 30.4 | 0.614 |
| Monthly or less (%) | 26.0 | 26.1 | 26.0 | |
| 2–4 times a month (%) | 16.1 | 16.4 | 16.2 | |
| 2–3 times a week (%) | 14.5 | 14.8 | 14.7 | |
| 4 or more times a week (%) | 14.1 | 11.4 | 12.7 | |
| Smoke | ||||
| Never (%) | 58.9 | 58.6 | 58.8 | 0.981 |
| Current (%) | 7.3 | 7.2 | 7.3 | |
| Former (%) | 33.8 | 34.2 | 33.9 | |
| Comorbidity count | ||||
| 0 (%) | 60.0 | 59.0 | 59.5 | 0.589 |
| 1 (%) | 25.9 | 28.1 | 27.0 | |
| 2 + (%) | 14.1 | 12.9 | 13.5 | |
| N (% of total) | 723 (48.7) | 763 (51.3) | 1,486 | |
Note: Descriptive statistics are from 1 to 1 nearest matching within caliper (0.25 SD)
Significance tests were based on Chi-square comparisons for categorical variables and based on analysis of variance (ANOVA) for continuous variables
Fig. 2.
Balance plot of study cohort before and after the propensity score matching. Note: Distribution of the propensity scores before and after 1:1 matching between cemented and cementless TKA groups
Among the matched cohort, 91.3% of patients who passed through the 6-month follow-up window at the time of analysis (92.7% for cemented TKA; 90.0% for cementless TKA) completed at least one post-operative PRO collection survey (at either 1-month, 3-months, or 6-months.). Follow-up rates were similar between the two groups of patients (Fig. 1-(b)). The baseline characteristic for ethnicity was the most frequently unanswered response, but was only missing in less than 1% of cases.
The effects of TKA on PROs in the propensity matched sample
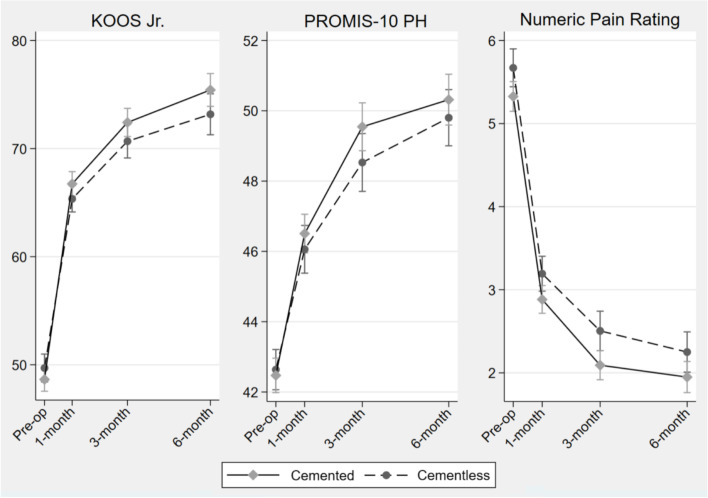
Overall, for both fixation methods, there were statistically significant pre- to post-operative improvements in mean knee function, physical health, and pain by 6-months (Fig. 3). Specifically, the mean adjusted KOOS-Jr., PROMIS-PH, and NPRS improved by 26.2 (95%CI: 24.9, 27.4), 7.7 (95%CI: 7.1, 8.2), and -3.3 (95%CI: -3.5, -3.1) points in the cemented TKA and by 25.3 (95%CI: 24.0, 26.6), 7.4 (95%CI: 6.8, 8.0), and -3.5 (95%CI: -3.7, -3.3) points in the cementless group, respectively (Table 2). Both Table 2 and Fig. 3 show that improvements increased over time, with the largest improvement appearing from pre-operative to 1 month, and slower improvements at 3 and 6 months, suggesting stabilization of the effects of TKA on PROs over time.
Fig. 3.
PROs following TKA between cemented and cementless fixation in the propensity-matched cohort. Note: Patient-reported outcomes following cemented and cementless total knee arthroplasty. Estimated coefficients were adjusted for age, BMI, gender, race, ethnicity, education, working status, drinking, smoking, and comorbidity
Table 2.
Adjusted Mean Patient-Reported Outcomes and Improvements by Month (1:1 matching)
| Total Knee Arthroplasty | Cemented | Cementless | |||||
|---|---|---|---|---|---|---|---|
| N | Mean | 95% CI | N | Mean | 95% CI | ||
| KOOS-Jr | Baseline | 723 | 48.9 | (47.8 – 50.0) | 763 | 48.7 | (47.5 – 49.8) |
| 1-month | 723 | 66.6 | (65.4 – 67.8) | 763 | 65.0 | (63.7 – 66.2) | |
| 3-month | 723 | 72.3 | (71.1 – 73.6) | 763 | 70.9 | (69.6 – 72.2) | |
| 6-month | 723 | 75.1 | (73.8 – 76.3) | 763 | 73.9 | (72.6 – 75.3) | |
| 1-mon-Base | 723 | 17.7 | (16.5 – 18.9) | 763 | 16.3 | (15.1 – 17.5) | |
| 3-mon-Base | 723 | 23.4 | (22.1 – 24.6) | 763 | 22.3 | (21.0 – 23.5) | |
| 6-mon-Base | 723 | 26.2 | (24.9 – 27.4) | 763 | 25.3 | (24.0 – 26.6) | |
| PROMIS-PH | Baseline | 723 | 42.6 | (42.0 – 43.2) | 763 | 42.2 | (41.6 – 42.9) |
| 1-month | 723 | 46.5 | (45.9 – 47.1) | 763 | 45.8 | (45.1 – 46.4) | |
| 3-month | 723 | 49.6 | (49.0 – 50.2) | 763 | 48.4 | (47.7 – 49.1) | |
| 6-month | 723 | 50.2 | (49.6 – 50.9) | 763 | 49.6 | (49.0 – 50.3) | |
| 1-mon-Base | 723 | 3.9 | (3.4 – 4.5) | 763 | 3.5 | (3.0 – 4.0) | |
| 3-mon-Base | 723 | 7.0 | (6.5 – 7.6) | 763 | 6.2 | (5.6 – 6.7) | |
| 6-mon-Base | 723 | 7.7 | (7.1 – 8.2) | 763 | 7.4 | (6.8 – 8.0) | |
| NPRS | Baseline | 723 | 5.3 | (5.1 – 5.5) | 763 | 5.7 | (5.6 – 5.9) |
| 1-month | 723 | 2.9 | (2.7 – 3.1) | 763 | 3.2 | (3.0 – 3.4) | |
| 3-month | 723 | 2.1 | (1.9 – 2.3) | 763 | 2.5 | (2.3 – 2.7) | |
| 6-month | 723 | 2.0 | (1.8 – 2.2) | 763 | 2.3 | (2.1 – 2.5) | |
| 1-mon-Base* | 723 | -2.4 | (-2.6 – -2.2) | 763 | -2.5 | (-2.7 – -2.3) | |
| 3-mon-Base* | 723 | -3.2 | (-3.4 – -3.0) | 763 | -3.2 | (-3.4 – -3.0) | |
| 6-mon-Base* | 723 | -3.3 | (-3.5 – -3.1) | 763 | -3.5 | (-3.7 – -3.3) | |
* Lower scores are better, so that negative signs represent improvement
Note: Baseline, 1-month, 3-month, and 6-month represent absolute score at each time point, while 1-mon-Base, 3mon-Base, and 6-mon-Base represent changes at1,3,6 months from baseline
PROs between cemented and cementless fixation in TKA
We compared pre-operative to post-operative changes in PROs between cemented and cementless TKA using a propensity score matched analysis (Table 3). Only the observed differences in the mean adjusted KOOS-Jr. were statistically significant between groups, while no statistically significant differences were found between groups in the adjusted measures for PROMIS-PH and NPRS at any time point. Specifically, at 6 months, cemented TKA achieved a 3.3 point greater improvement in KOOS-Jr. (95%CI: 0.36, 6.30; P = 0.028) compared to cementless TKA (Table 3).
Table 3.
Results from Propensity Score Matching (1-to-1 matching)
| Outcomes | KOOS-Jr | PROMIS-PH | NPRS | |||
|---|---|---|---|---|---|---|
| P | P | P | ||||
| Surgical approach (ref = cementless) | ||||||
| Cemented | -1.37 | .113 | -0.11 | .766 | -0.34 | .022 |
| Follow-up (ref = baseline) | ||||||
| 1-month | 15.7 | .000 | 3.43 | .000 | -2.48 | .000 |
| 3-month | 21.0 | .000 | 5.90 | .000 | -3.17 | .000 |
| 6-month | 23.5 | .000 | 7.17 | .000 | -3.42 | .000 |
| Approach interaction (ref = cementless) | ||||||
| Cemented *1-month | 2.46 | .042 | 0.61 | .303 | 0.04 | .862 |
| Cemented *3-month | 2.80 | .037 | 1.19 | .076 | -0.07 | .740 |
| Cemented *6-month | 3.33 | .028 | 0.69 | .302 | 0.05 | .836 |
| AGE | ||||||
| Age (mean) | 0.27 | .000 | 0.09 | .000 | -0.03 | .000 |
| Sex (ref = male) | ||||||
| Female | -1.48 | .023 | -1.09 | .001 | 0.20 | .058 |
| Body Mass Index | -0.08 | .091 | -0.16 | .000 | 0.002 | .813 |
| Race (ref = white) | ||||||
| Black | -3.41 | .004 | -1.86 | .000 | 1.11 | .000 |
| Other or multiple | -1.39 | .271 | -1.91 | .000 | 0.58 | .001 |
| Hispanic (ref = no) | ||||||
| Yes | 2.51 | .106 | 1.28 | .064 | 0.43 | .077 |
| Education (ref = less than college) | ||||||
| College or higher | 0.61 | .392 | 0.93 | .008 | -0.20 | .074 |
| Working status (ref = working) | ||||||
| Unemployed | -0.68 | .728 | -0.81 | .337 | 0.03 | .945 |
| Sick leave or maternity leave | -2.69 | .036 | -4.13 | .000 | 0.90 | .000 |
| Disabled due to hip or knee pain | 0.55 | .497 | -0.84 | .038 | -0.02 | .904 |
| Alcohol use (ref = never) | ||||||
| Monthly or less | -1.10 | .227 | 0.52 | .213 | 0.06 | .652 |
| 2–4 times a month | -2.11 | .061 | 0.48 | .329 | 0.04 | .798 |
| 2–3 times a week | -0.01 | .995 | 1.64 | .000 | -0.19 | .229 |
| 4 or more times a week | 0.79 | .502 | 1.72 | .001 | -0.25 | .135 |
| Smoke (ref = never) | ||||||
| Current | -3.69 | .029 | -1.43 | .078 | 0.59 | .015 |
| Former | -0.57 | .411 | -1.00 | .003 | 0.11 | .339 |
| Comorbidity (ref = no) | ||||||
| COPD | -2.18 | .152 | -1.54 | .009 | 0.07 | .746 |
| Paralysis | 15.9 | .028 | 15.2 | .000 | -1.69 | .173 |
| Heart attack | 0.22 | .863 | -0.09 | .888 | 0.36 | .149 |
| Carotid artery disease | -1.28 | .621 | -0.24 | .858 | -0.23 | .626 |
| Stroke | 2.00 | .279 | 0.53 | .507 | -1.60 | .680 |
| Rheumatoid arthritis | -1.73 | .243 | -1.64 | .004 | 0.41 | .038 |
| Diabetes | 1.98 | .022 | -0.72 | .108 | 0.03 | .827 |
| Cancer | 1.46 | .210 | 0.45 | .374 | -0.11 | .493 |
| Liver disease | -0.34 | .876 | 0.66 | .507 | -0.48 | .142 |
| Peripheral vascular disease | 3.13 | .133 | -1.26 | .192 | -0.48 | .149 |
| Kidney disease | -6.15 | .000 | -4.04 | .000 | 0.53 | .077 |
| Ulcer disease | -6.90 | .007 | -2.92 | .000 | 0.81 | .023 |
| HIV or AIDS | -5.50 | .289 | -4.44 | .084 | 1.12 | .194 |
| Constant | 37.3 | .000 | 43.5 | .000 | 7.17 | .000 |
Note: The estimated coefficients were from 1 to 1 nearest matching within caliper (0.25 SD)
A responder analysis shows the proportion of patients within each group who achieved the MCID in each outcome over time (Fig. 4). Overall, the proportion of patients who achieved the MCID increased over time. By 6 months, 90.5%, 49.5%, and 76.9% of patients who underwent TKA achieved the MCID in KOOS-Jr., PROMIS-PH, and NPRS respectively, with no statistically significant differences in the proportion of patients who achieved the MCID between cemented and cementless groups in each time point.
Fig. 4.
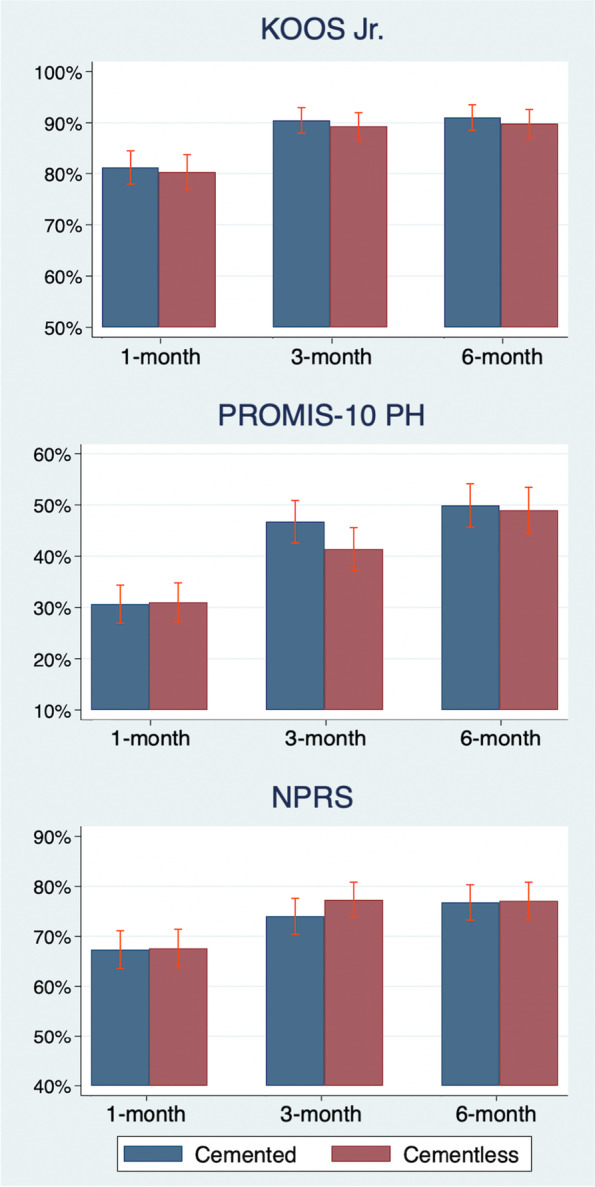
Proportion of patients achieving MCID at 1, 3, and 6 months among the propensity-matched cohort. Note: Proportion of patients within each group (cemented vs cementless) who achieved the Minimum Clinically Important Difference (MCID) in each patient-reported outcomes (KOOS Jr., PROMIS-10 PH, and NPRS)
Comparison between propensity matched sample and whole sample
Between-group effects in the PROMIS-PH or NPRS were similar for the propensity matched sample and the entire unmatched sample (based on a linear mixed-effects regression). However, the magnitude of the effect coefficients for KOOS-Jr. were decreased by half in the entire, unmatched sample (Appendix A2,) but did not change the overall trend of the results or conclusions. For example, in both samples, the differences in KOOS-Jr. between cemented and cementless TKA were mostly significant and increased over time. This suggests a low likelihood of bias after adjusting for observable characteristics.
Discussion
Our study demonstrated significant improvements in patient-reported pain and functional outcomes among all patients enrolled in the PEPPER trial who underwent either cemented or cementless TKA. Patients who underwent cemented TKA had a statistically significant greater improvement in knee function scores (KOOS-Jr.) than did those having a cementless procedure, but the effect difference (3.3 points; 55% of the MCID) was small from a clinical perspective. There were no other significant relative differences in general physical health or pain based on implant fixation methods. While group-mean differences in specific knee function did not reach MCID, the findings that patients undergoing cemented TKA achieved better improvement in KOOS-Jr. compared to those with cementless TKA may be of substantial importance to both patients and surgeons in discussing expectations for early recovery outcomes. Surgeons and patients may appropriately use this information to inform pre-operative counseling and shared decision-making.
The finding of a between-group treatment effect less than the MCID in the present study broadly aligns with several smaller studies from single centers that found no or little significant differences in PROs between cemented and cementless TKA [12–17, 25, 26]. A notable exception is the meta-analysis by Liu et al. [18] which reported better long term functional benefit for cementless patients (mean difference: 1.70; p = 0.004). Their finding was based on the Knee Society function scores of 652 subjects in cementless TKA and 656 subjects in cemented TKA from 9 studies with at least 2-year of follow-up. Notably, our analysis was based on larger overall sample size with a propensity-matched sample that still exceeded that the size of that included in the studies analyzed by Liu et al. Specifically, in our study, longitudinal PROs were collected prospectively from a large cohort of TKA patients enrolled by 28 medical centers among 31 total centers participating in PEPPER. This larger sample size enabled us to perform a propensity-matched analysis, which helps address any selection-by-indication bias, and increased external validity (generality of findings). In addition, our study focused on commonly used and validated instruments for both global and condition-specific measures.
This study has several limitations. First, while PROs were prospectively collected from the PEPPER trial, it is important to acknowledge that the randomization in the PEPPER trial is unrelated to our analysis; specifically, patients were not randomized to receive cemented or cementless TKA. Even though we employed a propensity score matching approach to reduce selection-by-indication bias, we cannot fully discount the potential for unobserved confounders that could weaken the validity of our findings. Second, because PEPPER is focused on safety surrounding anti-thrombotic drugs, long-term PRO’s (beyond the 6-month window) were not available. While it is known that most improvement in PROs after TKA occurs in the first 3 months, and PROs tend to stabilize after 6 months [37, 38], the extrapolation of our finding of a higher KOOS Jr after cemented compared with cementless might not be sustained in the longer term. PEPPER patients were enrolled by multiple (mostly academic) institutions with highly developed research and clinical trials infrastructures, which may limit our generalizability to other settings. Differences in safety, such as antithrombotic events, infections, or readmissions were not available for this analysis because they remain blinded until the PEPPER trial has been completed. The PEPPER trial did not collect all potentially confounding clinical details such as the type of TKA implant, kinematic alignment, type of porous metal coating, use of robot surgery. The degree to which these factors are disproportionately related to patient reported outcome is unknown and are thus a potential source of unobserved confounding. Lastly, although single nearest-neighbor matching approach could increase quality of matches, it also increased the variance of sample estimates by dropping many observations, which may lead to less precise parameter estimates.
Conclusion
While further studies with longer-term follow-up of PROs are required to definitively compare outcomes between cemented and cementless TKA, our findings suggest that cemented TKA potentially affords a slight benefit in patient-reported physical function during the first 6 months following surgery. Such an early advantage in physical function after cemented TKA could provide a benefit to patient pain, function, morale, and satisfaction following a major surgical procedure and may represent an important addition to pre-operative patient counseling and shared decision-making prior to total knee replacement.
Supplementary Information
Additional file 1: Appendix A1. Descriptive statistics from all sample Appendix A2. Results for regression models from all sample (Mixed effects).
Abbreviations
- PRO
Patient-reported outcomes
- TKA
Total knee arthroplasty
- PEPPER
Comparative Effectiveness of Pulmonary Embolism Prevention after Hip and Knee Replacement
- KOOS-Jr.
Short-form of the Knee Injury and Osteoarthritis Outcome Score
- PROMIS-PH
Patient-Reported Outcomes Measurement Information System Physical Health
- NPRS
Numeric Pain Rating Scale
- PMMA
Polymethyl-methacrylate
- PCORI
Patient-Centered Outcomes Research Institute
- BMI
Body Mass Index
- MCID
Minimum Clinically Important Difference
- ATE
Average Treatment Effect
Authors’ contributions
HK has given substantial contributions to the conception, design, and drafting of the manuscript. CP, BM, and VP contributed to the study concept, design, and interpretation of the data. All authors participated in revising of the manuscript. All authors read and approved the final version of manuscript.
Funding
This study was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (PCS-1402–09328) for the PEPPER trial, and by grant R01HS024714, from the Agency for Healthcare Research and Quality (AHRQ). The study sponsors had no role in the design or conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript. The statements in this article are solely the responsibility of the authors and do not necessarily represent the views of PCORI, AHRQ or their Board of Governors or Methodology Committees.
Availability of data and materials
The data that support the findings of this study are available from Vincent D. Pellegrini, Professor of Orthopaedics, Dartmouth-Hitchcock Medical Center but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Vincent D. Pellegrini, Professor of Orthopaedics, Dartmouth-Hitchcock Medical Center.
Declarations
Ethics approval and consent to participate
(a) All procedures were performed in accordance with the relevant ethical guidelines and regulations. (b) This study was approved by the central (single) human subjects review board from the Medical University of South Carolina (Pro00053742). Written informed consent was obtained from all participants.
Consent for publication
Not Applicable.
Competing interests
One or more of the authors (HK, CP, BM) have received funding from Agency for Healthcare Research and Quality (AHRQ). CP received royalties from Total Joint Orthopedics and research support from Zimmer Biomet. CP served as a paid consultant for Simith & Nephew, Total Joint Orthopedics, Zimmer Biomet, 3 M, Haereus, and Immunis. CP holds stock in Joint Development LLC. BM served as a paid consultant on the PEPPER trial, through ownership in STATIX, LLC. VP has nothing to disclose. The PEPPER INVESTIGATORS do have any competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hyunkyu Ko, Email: hyunkyu.ko@utah.edu.
Christopher E. Pelt, Email: Chris.Pelt@hsc.utah.ed
Brook I. Martin, Email: BROOK.MARTIN@hsc.utah.edu
Vincent D. Pellegrini, Jr., Email: Vincent.D.Pellegrini.JR@dartmouth.edu
The PEPPER Investigators:
James A. Browne, Antonia F. Chen, Eric M. Cohen, Charles M. Davis, III, Navin D. Fernando, Kevin B. Fricka, Richard J. Friedman, Kevin L. Garvin, Richard Iorio, Michael S. Kain, Stephen L. Kates, Brent A. Lanting, Brock A. Lindsey, William J. Maloney, Robert M. Molloy, Michael A. Mont, Wayne E. Moschetti, James Nace, Charles L. Nelson, Kevin I. Perry, James D. Slover, Mark J. Spangehl, Lawrence M. Specht, Scott M. Sporer, Robert S. Sterling, and Zeke J. Walton
References
- 1.Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. JBJS. 2014;96(8):624–630. doi: 10.2106/JBJS.M.00285. [DOI] [PubMed] [Google Scholar]
- 2.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: a meta-analysis. JAMA. 1994;271(17):1349–1357. doi: 10.1001/jama.1994.03510410061034. [DOI] [PubMed] [Google Scholar]
- 3.Hawker G, Wright J, Coyte P, Paul J, Dittus R, Croxford R, Katz B, Bombardier C, Heck D, Freund D. Health-related quality of life after knee replacement. Results of the knee replacement patient outcomes research team study. JBJS. 1998;80(2):163–173. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79–86. doi: 10.1097/00003086-199712000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Duffy, Gavan P., Daniel J. Berry, and James A. Rand. "Cement versus cementless fixation in total knee arthroplasty." Clinical Orthopaedics and Related Research (1976–2007) 356 (1998): 66–72. [DOI] [PubMed]
- 6.Carlsson Å, Björkman A, Besjakov J, Önsten I. Cemented tibial component fixation performs better than cementless fixation: a randomized radiostereometric study comparing porous-coated, hydroxyapatite-coated and cemented tibial components over 5 years. Acta Orthop. 2005;76(3):362–369. doi: 10.1080/00016470510030832. [DOI] [PubMed] [Google Scholar]
- 7.Metsovitis SR, Ploumis AL, Chantzidis PT, Terzidis IP, Christodoulou AG, Dimitriou CG, Tsakonas AC. Rotaglide total knee arthroplasty: a long-term follow-up study. JBJS. 2011;93(9):878–884. doi: 10.2106/JBJS.I.01702. [DOI] [PubMed] [Google Scholar]
- 8.Matassi F, Carulli C, Civinini R, Innocenti M. Cemented versus cementless fixation in total knee arthroplasty. Joints. 2013;1(3):121. doi: 10.11138/jts/2013.1.3.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prudhon, Jean-Louis, and Régis Verdier. "Cemented or cementless total knee arthroplasty?: Comparative results of 200 cases at a minimum follow-up of 11 years." Sicot-j 3 (2017). [DOI] [PMC free article] [PubMed]
- 10.Batailler C, Malemo Y, Demey G, Kenney R, Lustig S, Servien E. Cemented vs uncemented femoral components: a randomized, controlled trial at 10 years minimum follow-up. J Arthroplasty. 2020;35(8):2090–2096. doi: 10.1016/j.arth.2020.03.043. [DOI] [PubMed] [Google Scholar]
- 11.Prasad, Anoop K., Jaimee HS Tan, Hany S. Bedair, Sebastian Dawson-Bowling, and Sammy A. Hanna. "Cemented vs. cementless fixation in primary total knee arthroplasty: a systematic review and meta-analysis." EFORT open reviews 5, no. 11 (2020): 793–798. [DOI] [PMC free article] [PubMed]
- 12.Denis Nam, Lawrie Charles M, Salih Rondek, Nahhas Cindy R, Nunley Robert L, Nunley Ryan M. Cemented versus cementless total knee arthroplasty of the same modern design: a prospective, randomized trial. J Bone Joint Surg Am. 2019;101(13):1185. doi: 10.2106/JBJS.18.01162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Ooij Bas, Sierevelt Inger N, van der Vis Harm M, Hoornenborg Daniël, Haverkamp Daniël. What is the role of cemented fixation in total knee arthroplasty? The two-year results of a randomized RSA controlled trial. Bone Joint J. 2021;103(1):98–104. doi: 10.1302/0301-620X.103B1.BJJ-2020-0788.R1. [DOI] [PubMed] [Google Scholar]
- 14.Yazdi H, Choo KJ, Restrepo C, Hammad M, Sherman M, Parvizi J. Short-term results of triathlon cementless versus cemented primary total knee arthroplasty. Knee. 2020;27(4):1248–1255. doi: 10.1016/j.knee.2020.05.010. [DOI] [PubMed] [Google Scholar]
- 15.Pacoret, Victor, Etienne Kalk, Ludovic Labattut, Guillaume Girardot, Emmanuel Baulot, and Pierre Martz. "Survival rate of cemented versus cementless tibial component in primary total knee arthroplasty over 5 years of follow-up: comparative study of 109 prostheses." SICOT-J 6 (2020). [DOI] [PMC free article] [PubMed]
- 16.Rassir R, Nolte PA, van der Lugt JCT, Nelissen RGHH, Sierevelt IN, Verra WC. No differences in cost-effectiveness and short-term functional outcomes between cemented and uncemented total knee arthroplasty. BMC Musculoskelet Disord. 2020;21(1):1–7. doi: 10.1186/s12891-020-03477-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Newman JM, Sodhi N, Dekis JC, Khlopas A, Piuzzi NS, Sultan AA, Levin JM, Mont MA. Survivorship and functional outcomes of cementless versus cemented total knee arthroplasty: a meta-analysis. J Knee Surg. 2020;33(03):270–278. doi: 10.1055/s-0039-1678525. [DOI] [PubMed] [Google Scholar]
- 18.Liu Y, Zeng Yi, Yuangang Wu, Li M, Xie H, Shen B. A comprehensive comparison between cementless and cemented fixation in the total knee arthroplasty: an updated systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):1–14. doi: 10.1186/s13018-021-02299-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lawrie, C. M., M. Schwabe, A. Pierce, R. M. Nunley, and R. L. Barrack. "The cost of implanting a cemented versus cementless total knee arthroplasty." The bone & joint journal 101, no. 7_Supple_C (2019): 61–63. [DOI] [PubMed]
- 20.Fricka KB, Sritulanondha S, McAsey CJ. To cement or not? Two-year results of a prospective, randomized study comparing cemented vs. cementless total knee arthroplasty (TKA) J Arthroplasty. 2015;30(9):55–58. doi: 10.1016/j.arth.2015.04.049. [DOI] [PubMed] [Google Scholar]
- 21.Beaupré LA, Al-Yamani M, Huckell JR, Johnston DWC. Hydroxyapatite-coated tibial implants compared with cemented tibial fixation in primary total knee arthroplasty: a randomized trial of outcomes at five years. JBJS. 2007;89(10):2204–2211. doi: 10.2106/00004623-200710000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Nilsson KG, Kärrholm J, Carlsson L, Dalén T. Hydroxyapatite coating versus cemented fixation of the tibial component in total knee arthroplasty: prospective randomized comparison of hydroxyapatite-coated and cemented tibial components with 5-year follow-up using radiostereometry. J Arthroplasty. 1999;14(1):9–20. doi: 10.1016/S0883-5403(99)90196-1. [DOI] [PubMed] [Google Scholar]
- 23.Ryd, L. E. I. F., A. N. D. E. R. S. Lindstrand, A. N. D. E. R. S. Stenström, and G. Ö. R. A. N. Selvik. "Porous coated anatomic tricompartmental tibial components. The relationship between prosthetic position and micromotion." Clinical orthopaedics and related research 251 (1990): 189–197. [PubMed]
- 24.Trousdale, Robert T., Brian J. McGrory, Daniel J. Berry, Michael W. Becker, and William S. Harmsen. "Patients' concerns prior to undergoing total hip and total knee arthroplasty." In Mayo Clinic Proceedings, vol. 74, no. 10, pp. 978–982. Elsevier, 1999. [DOI] [PubMed]
- 25.Dubin JA, Westrich GH. A matched cohort study between cementless TKA and cemented TKA shows a reduction in tourniquet time and manipulation rate. J Orthop. 2020;21:532–536. doi: 10.1016/j.jor.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kagan R, Anderson MB, Bailey T, Hofmann AA, Pelt CE. Ten-year survivorship, patient-reported outcomes, and satisfaction of a fixed-bearing unicompartmental knee arthroplasty. Arthroplasty today. 2020;6(2):267–273. doi: 10.1016/j.artd.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prasad, Anoop K., Jaimee HS Tan, Hany S. Bedair, Sebastian Dawson-Bowling, and Sammy A. Hanna. "Cemented vs. cementless fixation in primary total knee arthroplasty: a systematic review and meta-analysis." EFORT open reviews 5, no. 11 (2020): 793–798. [DOI] [PMC free article] [PubMed]
- 28.Comparative Effectiveness of Pulmonary Embolism Prevention after Hip and Knee Replacement (PEPPER). https://clinicaltrials.gov/ct2/show/NCT02810704 Accessed 22 Apr 2021. [DOI] [PMC free article] [PubMed]
- 29.KOOS-Jr. outcome survey https://www.hss.edu/hoos-jr-koos-jr-outcomes-surveys.asp Accessed 22 Apr 2021.
- 30.Hung M, Bounsanga J, Voss MW, Saltzman CL. Establishing minimum clinically important difference values for the Patient-Reported Outcomes Measurement Information System Physical Function, hip disability and osteoarthritis outcome score for joint reconstruction, and knee injury and osteoarthritis outcome score for joint reconstruction in orthopaedics. World journal of orthopedics. 2018;9(3):41. doi: 10.5312/wjo.v9.i3.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lam Ka Hoo, Kwa Vincent IH. Validity of the PROMIS-10 Global Health assessed by telephone and on paper in minor stroke and transient ischaemic attack in the Netherlands. BMJ open. 2018;8(7):e019919. doi: 10.1136/bmjopen-2017-019919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Farrar John T, Young James P, Jr, LaMoreaux Linda, Werth John L, Poole Michael R. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 33.Smith JA, Todd PE. Does matching overcome LaLonde's critique of nonexperimental estimators? Journal of econometrics. 2005;125(1–2):305–353. doi: 10.1016/j.jeconom.2004.04.011. [DOI] [Google Scholar]
- 34.Snedecor, George W., and William G. Cochran. "Statistical methods." (1980).
- 35.Stuart, Elizabeth A. "Matching methods for causal inference: A review and a look forward." Statistical science: a review journal of the Institute of Mathematical Statistics 25, no. 1 (2010): 1. [DOI] [PMC free article] [PubMed]
- 36.Garrido Melissa M, Kelley Amy S, Paris Julia, Roza Katherine, Meier Diane E, Morrison R. Sean, Aldridge Melissa D. Methods for constructing and assessing propensity scores. Health services research. 2014;49(5):1701–1720. doi: 10.1111/1475-6773.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kagan R, Anderson MB, Christensen JC, Peters CL, Gililland JM, Pelt CE. The recovery curve for the patient-reported outcomes measurement information system patient-reported physical function and pain interference computerized adaptive tests after primary total knee arthroplasty. J Arthroplasty. 2018;33(8):2471–2474. doi: 10.1016/j.arth.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 38.Liddle AD, Pandit H, Judge A, Murray DW. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14 076 matched patients from the National Joint Registry for England and Wales. The bone & joint journal. 2015;97(6):793–801. doi: 10.1302/0301-620X.97B6.35155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix A1. Descriptive statistics from all sample Appendix A2. Results for regression models from all sample (Mixed effects).
Data Availability Statement
The data that support the findings of this study are available from Vincent D. Pellegrini, Professor of Orthopaedics, Dartmouth-Hitchcock Medical Center but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Vincent D. Pellegrini, Professor of Orthopaedics, Dartmouth-Hitchcock Medical Center.