Abstract
Aims
The transition from analogue to digital pathology (DP) is underway in Switzerland. To assess relevant experiences of pathologists with DP and gauge their outlook towards a digital future, a national survey was conducted by the Swiss Digital Pathology Consortium. Similar surveys were conducted in other countries, enabling a meta-analysis of DP experiences.
Methods
Pathologists and residents were asked to complete a survey containing 12 questions. Results were compared with similar studies conducted in the United Kingdom, Sweden, Canada, and India.
Results
The estimated response rate among practicing pathologists and trainees nationwide was 39.5%. Of these, 89% have experience with digital slides, mainly for education (61%) and primary diagnostics (20%). Further, 32% have worked with an image analysis programme and 26% use computer-based algorithms weekly. Interestingly, 66% would feel comfortable making a primary diagnosis digitally, while 10% would not. Most respondents believe more standards and regulations are necessary for the clinical employment of DP. Noted advantages include ease of access to slides and the resulting connectivity benefits, namely collaboration with experts across disciplines, off-site work, training purposes, and computational image analysis. Perceived disadvantages include implementation costs and issues associated with IT infrastructure and file formats.
Conclusion
The survey results suggest that experiences and perspectives of Swiss pathologists concerning DP is comparable to that of the other reporting countries undergoing transitions to digital workflows. Although more standards and regulations are needed to ensure the safe usage of these technologies, pathologists in Switzerland appear welcoming of this new digital era.
INTRODUCTION
The transformation of clinical workflows from glass to digitised slides is already underway in histopathology labs worldwide.1–4 This transformation is likely driven in part by the numerous proven advantages of going digital: increased precision in measurements of areas and distances, more reliable counting of events and more objective evaluation of therapeutic and prognostic biomarkers.5 Further, digital archives created from these slides support: (i) rapid retrieval of cases for diagnostic comparisons, (ii) access to a variety of cases for educational purposes and (iii) the development of data-hungry computational algorithms by providing large retrospective cohorts.6 Moreover, diagnostic slide sharing in the context of tele-pathology and working remotely is expected to help grapple with the universal shortage of pathologists.7 Despite these advantages, there are a number of important implementation challenges associated with digitisation; ‘going digital’ coincides with more than simply installing a slide scanner.8 Laboratory work-flows likely need to be re-evaluated to address any emerging bottlenecks resulting from the digital transition. Challenges with the implementation of IT components, such as high-volume storage, should not be underestimated. For example, the integration of various components of a digital pathology (DP) workflow, such as the image management systems (IMS) and laboratory information systems (LIS), can be difficult and typically requires extensive cooperation between vendors/partners. In Switzerland, slide scanners are becoming increasingly commonplace and some institutes have already undergone the complete integration between their scanners, pathology information system, and IMS. Other institutes are in the process of validating computational image analysis algorithms to aid in their routine work. The Swiss Digital Pathology Consortium (SDiPath) has conducted a national survey of pathologists to gain deeper insights into the current landscape of their experiences with DP and gauge perspectives on many issues surrounding this topic.
METHODS
A survey was developed consisting of 12 questions evaluating four topics: (1) personal experience and working environment, (2) current experience with digital slides and image analysis programmes, (3) the pathologists’ opinion on the future implications of DP and (4) general advantages and disadvantages of DP. The answers were requested in the form of either yes/no or multiple-choice questions with the possibility to add a free-text answer, if the desired option was absent. The survey was created in English and subsequently translated into German and French by native speakers. A copy of the survey is shown in the online supplementary table 1.
To reduce bias in the participants of the survey, a non-DP related venue was targeted for the initial distribution of the printed version of the survey. The February 2019 immunohistochemistry (IHC) slide seminar organised by the Swiss Society of Pathology (SSPath) was selected. It was attended by 159 pathologists spanning a number of different subspecialties. After the seminar, an invitation to participate in the survey was sent out to all SSPath members in the subsequent online newsletter.
Members were also encouraged to distribute the survey invitation to pathologists or residents who are not SSPath members. The invitation contained a link to the online version of the survey, which was developed and executed using Google Forms. Data collection then took place over a 2-month time period. At the end of March, the data collection phase was determined to be completed. χ2 tests were performed using SAS V.9.4 (the SAS Institute, Cary, North Carolina, USA). All p-values were two-sided and considered significant when p<0.05.
RESULTS
A total of 134 survey responses were received, including 99 from the slide seminar (64% of the participants) and the remaining 35 from the online survey. Thereof, 100 respondents were staff pathologists and 34 were residents. According to Swiss federal statistics, 485 staff pathologists are registered in Switzerland, including 398 who are members of the SSPath. The overall response rate for all pathologists in the country is 21% and of all SSPath members is 29.6%. Additionally, there are 87 pathology positions for residents in Switzerland, yielding a response rate among residents of 39%. Taken together, the national response rate for the targeted audience was 39.5%. Employees of a university institute (52%), hospital pathology department (25%) or private pathology institute (16%) completed the majority of surveys.
Current experience with digital slides
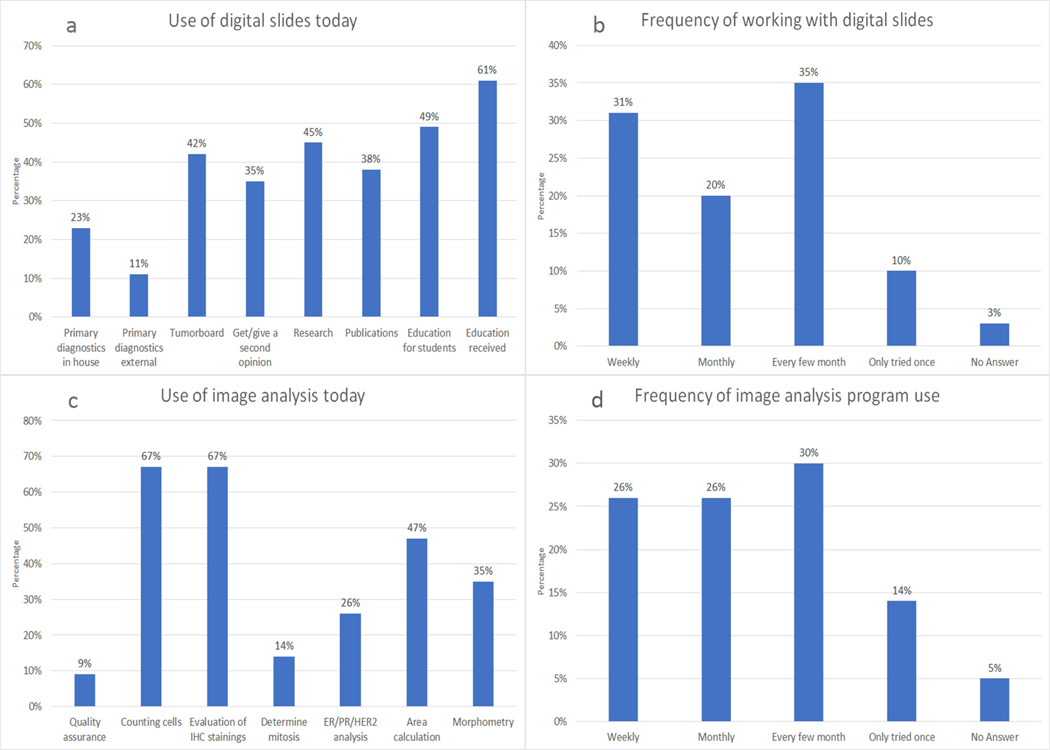
To date, 89% of respondents have experience in the use of digital slides: 61% state that they received an education in pathology at least in part supported by digital slides and 49% named digital slides as an instrument for education of students and interns. Further, digital slides were frequently cited for use in interdisciplinary work such as tumour boards, second reader consultations, research and publications. Further, 22% of respondents have used digital slides for a primary diagnosis, with 11% having performed such a diagnosis remotely (ie, from a location outside their own pathology institute) (figure 1A), whereas 31% of pathologist work with digital slides every week and 37% only every few months (figure 1B). There was no difference in experience with digital images between less (residents and pathologists with <5 years of experience) or more experienced pathologists (p=0.8713).
Figure 1.
(A) Results of the question on the current use of digital slides in Switzerland. (B) Results of the frequency of digital slide usage in Switzerland. (C) Results of the question on the current use of image analysis programmes in Switzerland. (D) Results of the frequency of image analysis programme usage in Switzerland. IHC, immunohistochemistry.
Current experience with image analysis
Experience with the utilisation of image analysis programs is limited to 32% of the respondents. The software used most frequently included the open source image analysis programme ‘QuPath’9 with nine counts, followed by ‘HALO’ from Indica Labs10 with seven counts and ‘Visiopharm’11 with five counts. A variety of other applications were mentioned once or twice (see online supplementary table 2). Image analysis programs were mainly used for cell counting (67%) and IHC marker quantification (67%) (figure 1C). In regards to frequency, 26% of responses indicated weekly work and again 26% with monthly work regarding such programs. There was no statistically significant difference between less (residents of pathologists with <5 years experience) and more experienced pathologists (p=0.7048). About a half of participants reported less frequent work, with 35% using an application every few months and the remaining 14% having tried such software only once (figure 1D).
Opinion on the future of digital pathology
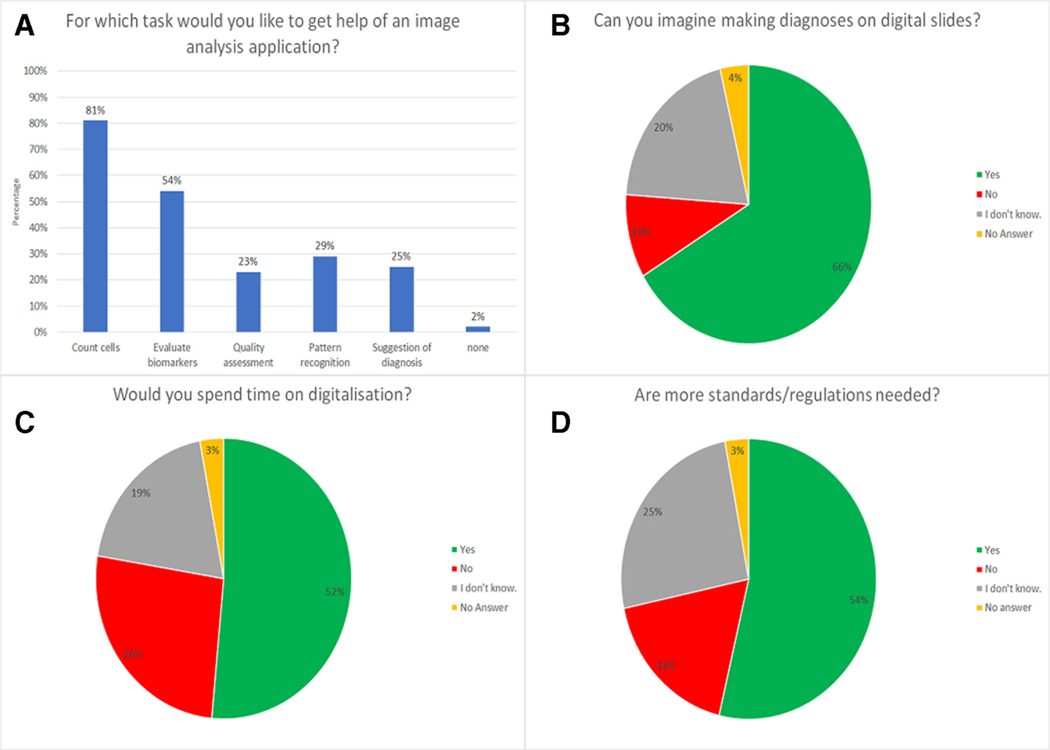
When asked in what way DP will change the pathologists’ work in the future, 82% chose ‘Computer-based diagnostics will enrich and facilitate work’. Notably, only 5% selected DP ‘will replace the pathologist in the long run’ and 2% that it ‘will make work boring and monotonous’. The rest believe that computer-based diagnostics will not have a significant impact on their work. More so, 81% indicated a desire to have an image analysis program for counting cells in their daily routine and 54% requested help for the evaluation of biomarkers. An application suggesting diagnosis was indicated by 25% of the participating pathologists as being potentially useful. Only 2% indicated that they did not want assistance in any form (figure 2A).
Figure 2.
(A) For which task do Swiss pathologists wish help by an image analysis programme? (B) Willingness for making diagnosis digital. (C) Willingness to invest time into digitalisation. (D) Is there a need for more standards and regulations?
In the context of primary diagnostics, 66% of pathologists could imagine making diagnoses on a digital slide with only 10% completely refusing (figure 2B). Interestingly, there was no difference found by comparing less versus more experienced pathologists (p=0.6046). Further, 52% would spend time to help implement digitalisation (figure 2C). Results show 66% of younger interviewees such as residents and pathologists with up to 5 years’ experience are willing to invest time on this front compared with 46% of more experienced pathologists, yet the difference was not statistically significant (p=0.4471). There are too few standards and regulations according to 54% of the respondents and 25% do not know if more standards are needed (figure 2D). On a scale intended to measure innovation advantage from 0 (no advantage) to 5 (very big advantage), participants responded as follows: no score of 0 was given, score 1: 3.7%, score 2: 19.4%, score 3: 23.1%, score 4: 28.4% and score 5: 20.9%. There was no answer available for six surveys. The median value across all survey was score 4.
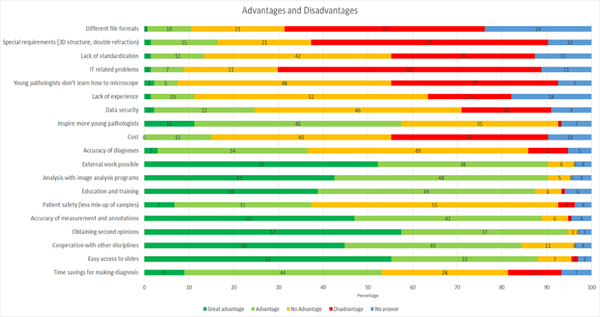
Advantages and disadvantages
The following topics are perceived as advantages or great advantages of DP in general: (1) accuracy of measurement and annotations, (2) obtaining second opinions, (3) cooperation with other disciplines, (4) easy access to the slides, (5) remote access/ work possibilities, (6) analysis with image analysis programmes and (7) education and training. The exact percentages can be found in figure 3. A contentious topic discovered by this survey is in regards to time management: 53% see a potential in saving time, whereas 12% are concerned about additional time expenditure. For patient safety and the accuracy of diagnosis, there is no change anticipated by respondents. In this light, only 9% indicated they were afraid of less accurate diagnoses when made digitally versus a microscope. Major downsides are anticipated in terms of (1) IT-related problems, (2) special requirements (eg, Congo red, macro sections, immunofluorescence), (3) different file formats, (4) young pathologists not being properly trained to use a microscope, (5) costs and (6) the lack of standardisation. Overall, 20% suspect a disadvantage in data security by digital processing of slides.
Figure 3.
The opinion on general advantages and disadvantages of digital pathology.
DISCUSSION
This survey aimed to discover the views of pathologists in Switzerland with regard to the current state (2019) and future of DP. One potential limitation of this study is the limited response rate of 21%. According to the Swiss federal register, 485 pathologists are presently registered in Switzerland. However, data from the Swiss Medical Association FMH (Foederatio Medicoroum Helvetcorum) indicate that only 253 of them are currently actively practicing in the country, suggesting a considerably higher response rate of 39.5%. Several surveys on a similar topic were carried out in different countries.12–15 In Canada, 17% of Canadian Association of Pathologists-registered pathologists as well as 27% of practicing pathologists and residents answered a similar national survey, while only 18% of participants answered in the USA. In Sweden, 37% of all residents partook in a similar survey. Our response rate is therefore similar, if not considerably higher in comparison to these prior surveys. To counteract the potential bias of an online-only survey on this technology -related topic, an IHC seminar attended by all levels of technophile pathologists was chosen with a printed paper survey distribution. A potential limitation identified after execution of the summary was in regards to the reported vague verbalisation of some final items in Question 12. This oversight came from merging two questions shortly before dissemination of the survey and the error was brought to our attention during the slide seminar. For these last points, we intended to gauge the degree of perceived severity of these different issues. The responses to these four items should be interpreted with caution.
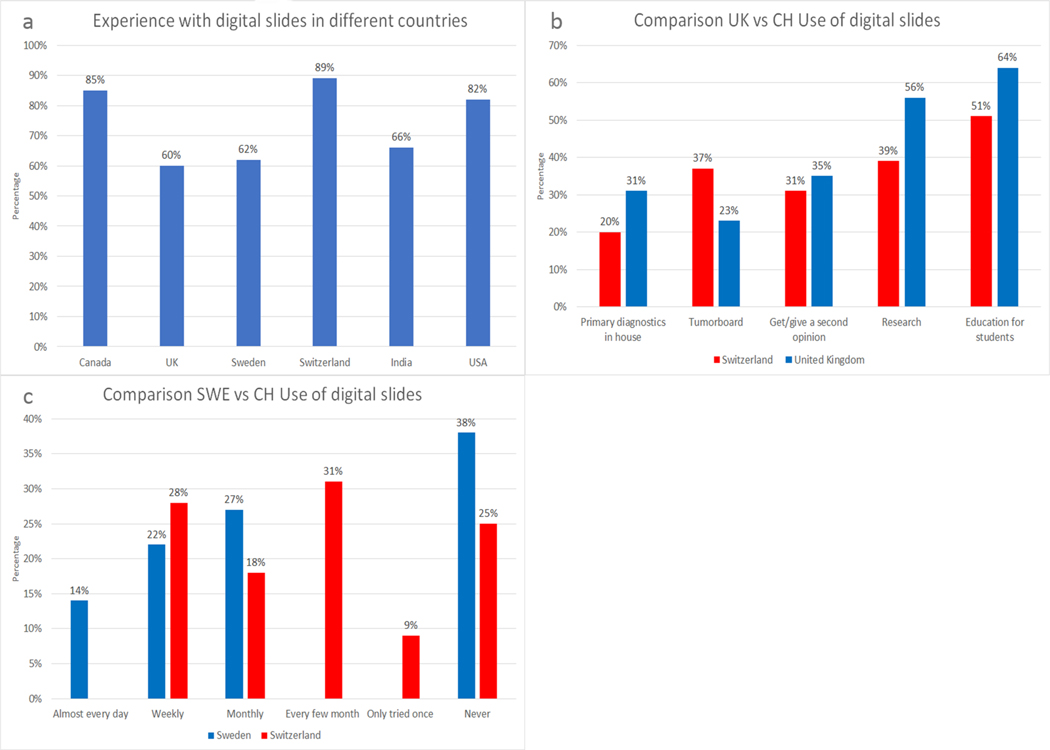
To aid in a comparison between countries, we were kindly provided with results from a survey in 2017 among residents conducted by Dr Sofia Jarkman and colleagues for the Linköping University Hospital in Sweden.14 A similar study was also conducted in the UK, which interestingly targeted institutions and not single individuals.15 This difference implies that the true number of pathologists would probably be higher in their case than the results reported there. The surveys in Canada12 and India13 were conducted in 2013 and 2014, respectively, which in this rapidly moving field may already be considered outdated. In Sweden and in the USA14 16 only residents were considered for their surveys. The 89% of pathologists who reported working with digital slides during our survey is on par with the 85% in Canada,12 60% in the UK,15 62% in Sweden, 66% in India13 and 82% in the USA16 (figure 4A). The experience with image analysis programmes is similar between countries with 31% in Switzerland, 37% in Canada and 31% in the UK. One can conclude that one-third of pathologists have already experienced work with computer-based algorithms to evaluate slides.
Figure 4.
(A) Comparison of Canada, the UK, Sweden, Switzerland, India and the USA for experience with digital slides. (B) Comparison of the UK and Switzerland for the form of digital slide usage. (C) Comparison of Sweden and Switzerland for the frequency of digital slide usage.
Our study was designed with insights from the surveys in the UK and in Sweden and therefore, a more detailed comparison was possible between the three. The UK is reportedly more advanced in routine DP work: 31% use digital slides for primary diagnostics15 compared with 20% in Switzerland. Only in collaboration with other specialties such as the tumour board (multidisciplinary conference) does Switzerland have a higher rate than that of the UK, 37% vs 23%, respectively. In both countries, education is the leading reason for digital slide use with 51% Switzerland and 64% in the UK15 (figure 3B). In Sweden, digital slides are used more frequently than in Switzerland: 36% of Swedish residents use digital slides at least once a week in contrast to 28% of Swiss pathologists.14 Interestingly, there are more residents without any experience using digital slides in Sweden (38%) than in Switzerland (25%, figure 4C). Since publication of these results, the UK has become a world leader in the implementation of DP workflows. Publications by the team at Leeds present guidelines for (1) the management of DP projects, (2) ISO 15189 accreditation in a digital setting and (3) numerous practical tips for building a business plan along with a smooth integration of DP into lab and diagnostic workflows.17 Other groups have also fully transitioned to digital workflow. For example, van Dienst and Baidoschvili in the Netherlands reported on the time saving aspects and benefits of their DP implementations.1 18 Additionally, they shared their experiences with the tender process and approach towards setting up their laboratory, infrastructure and pathologists’ workstations.19 A survey of 23 participants from their department with various amounts of exposure to DP systems indicated that after working digitally for 6 months: 43.5% felt very confident, 30.4% rather confident and only 4.3% slightly confident or not at all.19 In Sweden, DP implementation began in 2006 with Thorstenson et al reporting their experiences over a 7-year period along with the results of a survey including 10 pathologists.3 The focus was on digital tools along with aspects of the experienced digital diagnostic work. At that time, almost 40% of surveyed pathologists reported using automatic algorithms in their daily work.3 Fraggetta et al also share their experiences with a 100% digital diagnostic workflow in Catania, Italy.2 They underline that the effective adoption of whole slide imaging for primary diagnostic use was more dependent on preimaging variables and integration with the LIS than on IT infrastructure.
The advantages frequently mentioned in the surveys from Canada, Sweden, the UK and Switzerland are the easy access to the slides in digital archives. This access is seen to facilitate collaboration with other specialties, the possibility of working externally, and the potential for education.12 14 15 Unsurprisingly, the digitisation of slides is seen as promising for the application of computer-based approaches for image quantification and analysis. Although image analysis programmes will change the pathologists’ work in some way, the interviewees are not afraid of replacement by such tools. In the Swedish survey, residents strongly disagree with the statement, ‘the pathologist will be replaced in the future’. Similarly, in Switzerland only 5% envision such a scenario.
A contentious question relates to the potential time savings afforded by DP. While scanning glass slides requires time and effort, sending a link to receive a second opinion is much faster than a glass slide. Therefore, without stricter on-site measurements of these tasks, it is difficult to determine overall potential savings or expenditure of time. Even though reducing the risk of patient misidentification has been identified as an advantage of digital slides5 only one-third (37%) of Swiss pathologists consider it as beneficial. Canadian pathologists had major concerns about the accuracy of a diagnosis made on digital slides due to image quality12 in contrast to the Swiss pathologist where only 9% have concerns regarding this aspect. Hanna et al showed in their study that diagnoses performed on glass slides and digital slides are concordant.20 The most severe disadvantage identified across countries is the cost for DP implementation, that is, associated hardware and software.12 15 The proprietary file formats of each scanner manufacturer also do not allow a seamless exchange of data and can potentially lead to time consuming conversions. These concerns are well founded given the large investments needed to have institutes push digital integration forward.
Another anticipated disadvantage is the current lack of experience and standards in the DP realm. In the UK, 78% indicated that they would like more guidance in DP usage.15 A similar perceived lack of standardisation is also a problem in Switzerland: 54% indicated a desire for more standards and regulations regarding digital slide usage. Although guidelines for DP diagnosis and computational pathology definitions/best practices from various countries are already established,21–23 the dissemination of its knowledge has not yet appeared to reach the global community. This is potentially one of the most important findings of this study, further motivating the SDiPath to help facilitate the awareness of DP in Switzerland.
CONCLUSION
This survey provides an overview for the first time on the situation and experiences of pathologists with DP in Switzerland. Most Swiss pathologists have some experience with digital slides and one-third have experience with image analysis. The current status of Switzerland is comparable to other countries who have conducted similar surveys. The pathologists appear to be open-minded to the evolution towards a more digital future, with only a small minority believing DP will result in job loss. While there appears to be minimal concerns associated with the quality of diagnoses after migrating to digital slides, more standards and regulations are requested. There appears to be agreement that DP is a fast growing emerging field, with a number of opportunities for future innovation and integration. As such, the repetition of a similar survey in 5 years’ time to monitor progress and changes in perception would likely yield different conclusions. Taken together, these results strongly suggest that a new era in Swiss pathology is on the way.
Supplementary Material
Take home messages.
The notion of going digital appears to be well-received in the Swiss pathology community.
Most Swiss pathologists already have at least some experience with digital slides.
Many pathologists are unaware of guidelines already in existence and the need for standardisation and regulations needs to be addressed.
It will be the role of the Swiss Consortium for Digital Pathology to provide a durable venue for the necessary discussions and dissemination of national guidelines.
Acknowledgements
We would like to thank the Swiss Society of Pathology for helping us with the distribution of the survey and all respondents who took the time to participate. We also are indebted to Dr Sofia Jarkman for allowing us to reference her work here.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Handling editor Dhirendra Govender.
data availability statement
Data are available on reasonable request.
REFERENCES
- 1.Baidoshvili A, Bucur A, van Leeuwen J, et al. Evaluating the benefits of digital pathology implementation: time savings in laboratory logistics. Histopathology 2018;73:784–94. [DOI] [PubMed] [Google Scholar]
- 2.Fraggetta F, Garozzo S, Zannoni GF, et al. Routine digital pathology workflow: the Catania experience. J Pathol Inform 2017;8:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thorstenson S, Molin J, Lundström C. Implementation of large-scale routine diagnostics using whole slide imaging in Sweden: digital pathology experiences 2006–2013. J Pathol Inform 2014;5:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams BJ, Jayewardene D, Treanor D. Digital immunohistochemistry implementation, training and validation: experience and technical notes from a large clinical laboratory. J Clin Pathol 2019;72:373–8. [DOI] [PubMed] [Google Scholar]
- 5.Grobholz R. [Digital pathology : The time has come!]. Pathologe 2018;39:228–35. [DOI] [PubMed] [Google Scholar]
- 6.Madabhushi A, Le Image analysis and machine learning in digital pathology: challenges and opportunities. Med Image Anal 2016;33:170–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koelzer V, Zlobec I, Willi N, et al. Digitale Pathologie – vom Objektträger zum Datenträger. Swiss Medical Forum – Schweizerisches Medizin-forum 2019;19:49–51. [Google Scholar]
- 8.Zlobec I, Grobholz R, Janowczyk A. Going digital: more than just a scanner! Der Pathologe. In Press 2019.
- 9.Bankhead P, Loughrey MB, Fernández JA, et al. QuPath: open source software for digital pathology image analysis. Sci Rep 2017;7:16878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Labs I. Halo pathology illiminated, 2018. Available: http://www.indicalab.com/halo/
- 11.Visiopharm. Pathcore and Visiopharm provide a powerful image analysis, 2016. Available: https://healthcare-in-europe.com/en/news/pathcore-visiopharm-provide-a-powerful-image-analysis.html
- 12.Bellis M, Metias S, Naugler C, et al. Digital pathology: attitudes and practices in the Canadian pathology community. J Pathol Inform 2013;4:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chordia TD, Vikey A, Choudhary AB, et al. Current status and future trends in telepathology and digital pathology. J Oral Maxillofac Pathol 2016;20:178–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Global Engage-Digital Pathology Congress. The Native Digital Pathologist - Experience from a Pathology Trainee. London, 2017. [Google Scholar]
- 15.Williams BJ, Lee J, Oien KA, et al. Digital pathology access and usage in the UK: results from a national survey on behalf of the National cancer research Institute’s CM-Path initiative. J Clin Pathol 2018;71:463–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vallangeon BD, Hawley JS, Sloane R, et al. An assessment of pathology resident access to and use of technology: a nationwide survey. Arch Pathol Lab Med 2017;141:431–6. [DOI] [PubMed] [Google Scholar]
- 17.Williams BJ, Knowles C, Treanor D. Maintaining quality diagnosis with digital pathology: a practical guide to iso 15189 accreditation. J Clin Pathol 2019. [DOI] [PubMed]
- 18.Baidoshvili A, Stathonikos N, Freling G, et al. Validation of a whole-slide image-based teleconsultation network. Histopathology 2018;73:777–83. [DOI] [PubMed] [Google Scholar]
- 19.Stathonikos N, Nguyen TQ, Spoto CP, et al. Being fully digital: perspective of a Dutch academic pathology laboratory. Histopathology 2019;75:621–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanna MG, Reuter VE, Hameed MR, et al. Whole slide imaging equivalency and efficiency study: experience at a large academic center. Mod Pathol 2019;32:916–28. [DOI] [PubMed] [Google Scholar]
- 21.Abels E, Pantanowitz L, Aeffner F, et al. Computational pathology definitions, best practices, and recommendations for regulatory guidance: a white paper from the digital pathology association. J Pathol 2019;249:286–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.García-Rojo M. International clinical guidelines for the adoption of digital pathology: a review of technical aspects. Pathobiology 2016;83:99–109. [DOI] [PubMed] [Google Scholar]
- 23.García-Rojo M, De Mena D, Muriel-Cueto P, et al. New European Union regulations related to whole slide image scanners and image analysis software. J Pathol Inform 2019;10:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request.