Abstract
Study design
This is a meta-analysis and systematic review of the available literature.
Objective
In the case of severe foraminal stenosis, conducting uncinate process resection (UPR) during ACDF could achieve complete nerve root decompression and significant relief of neurological symptoms for CR. However, there is some controversy regarding its necessity and safety. This study aims to compare the safety and efficacy of ACDF with UPR and ACDF.
Methods
The following electronic databases were searched: Medline, PubMed, Embase, the Cochrane Central Register of Controlled Trials, Evidence Based Medicine Reviews, VIP, and CNKI. And the following data items were considered: baseline demographics, efficacy evaluation indicators, radiographic outcome, and surgical details.
Results
10 studies were finally identified, including 746 patients who underwent ACDF with UPR compared to 729 patients who underwent ACDF. The group of ACDF with UPR had statistically longer intraoperative time (95% CI: 4.83, 19.77, P = .001) and more intraoperative blood loss (95% CI: 12.23, 17.76, P < .001). ACDF with UPR obtained a significantly better improvement of Arm VAS at postoperative first follow-up (95% CI: −1.85, −.14 P = .02). There was no significant difference found in improvement of Neck VAS at postoperative latest follow-up (95% CI: −.88, .27, P = .30), improvement of Arm VAS at postoperative latest follow-up (95% CI: −.59, −.01, P = .05), improvement of NDI (95% CI: −2.34, .33, P = .14), JOA (95% CI: −.24, .43, P = .56), change of C2-C7 lordosis (95% CI: −.87, 1.33, P = .68), C2-C7 SVA (95% CI: −.73, 5.08, P = .14), T1 slope (95% CI: −2.25, 1.51, P = .70), and fusion rate (95% CI: .83, 1.90 P = .29).
Conclusion
ACDF with UPR is an effective and necessary surgical method for CR patients with severe foraminal stenosis.
Keywords: cervical radiculopathy, ACDF, uncinate process resection, foraminal stenosis, meta-analysis
Introduction
Cervical radiculopathy (CR) is a degenerative spinal disorder associated with radicular arm pain and sensory disturbances caused by compression of a cervical nerve root.1,2 Although nonsurgical treatment is preferentially recommended, surgical treatment is inevitable and necessary when conservative therapy fails or the symptoms worsen.3,4 In cervical radiculopathy, the major pathology is the disc herniation and the impingement of nerve root from the osteophytes projecting from the uncinate process (UP) anteriorly. 5 In such a case, it is difficult to get the bony decompression thorough posterior approach. Anterior cervical discectomy and fusion (ACDF) was firstly introduced by Smith and Robinson in 1958 and was regarded as the gold-standard procedure for CR patients. 6 By decompression of neural elements and fusion, ACDF aiming to improve the stability of vertebral and its clinical efficacy and radiologic results has been proved superior.
Since ACDF was described over a half century ago, the technique has been evolving. In recent years, an increasing number of scholars have been focused on the complete decompression of intervertebral foramen with the wide application of anterior cervical approach. For the proximity of the nerve to the posterior edge of the uncinate process, osteophytes of the UP usually compress the cervical nerve root directly in CR, which can develop foraminal stenosis. On this ground, ACDF could not achieve complete nerve root decompression and significant relief of neurological symptoms without UPR for patients with severe foraminal stenosis. With the development of surgical instruments and techniques (high speed burr, ultrasonic dissector, et al), UPR has become relatively feasible and simple. Nevertheless, UPR is a technically demanding procedure due to the proximity of the UP to the vertebral artery and nerve roots. Vascular structure or nerve root injury may occur in this additional surgical procedure. On the other hand, the presence of UP is a unique anatomic feature of the cervical spine, which can limit the lateral flexion and posterior translation of the cervical spine. Kotani’s biomechanical study indicated that the foraminal part of UP provided the most stability of cervical spine. 7 Meanwhile, there had been a worry that UPR may decrease the stability of resected segment and affect the fusion rate. 8 Efficacy and safety were two factors that should be considered collectively in choosing the surgery method.
No consensus was reached on removal or retention of UP in previous studies. Cloward advocated direct decompression with removal of all factors that compressed nerve roots including uncovertebral osteophytes. 9 In Safaee MM’s study, 52 patients received ACDF with UPR, the results showed a significant effectiveness as well as an acceptable safety profile. 10 However, the initial surgical philosophy of ACDF was to increase the foraminal canal diameter (indirect decompression) by disc space distraction. Robinson believed that osteophytes can spontaneously be absorbed with release of abnormal stress stimuli. In Smith and Robinson’s first clinical study of ACDF, 9 of 14 patients’ outcome were good by indirect decompression. Shen et al in 2004 made the comparison of the fusion rate and relief of neck and arm pain in 109 patients who received these two anterior approaches (ACDF with UPR VS ACDF). 11 There was no significant difference in both pain relief and fusion rate, which meant that UPR was non-essential. These aforementioned said leads us to a question which has been controversial : Whether additional UPR during ACDF is needed?
The above-mentioned studies were low-grade evidence-based medical evidence. There is still no comprehensive review regarding the comparative analysis on outcomes between these two cervical spine procedures. The current study is the first meta-analysis to compare the safety and efficacy of ACDF with UPR with ACDF in the respects of patient-rated scores, sagittal alignment, and fusion rate. We aim to answer the following 3 questions: whether additional UPR during ACDF is necessary? Whether UPR is safe? What is the indication of UPR? We hope this study could have a number of implications for this controversial issue and provide clinicians with an evidence base for their clinical decision making.
Methods
Search Strategy
This meta-analysis was executed in accordance with the PRISMA guidelines. 12 We searched the following electronic databases from their inception dates to December 2021: Medline, PubMed, Embase, the Cochrane Central Register of Controlled Trials, Evidence Based Medicine Reviews, VIP, and CNKI. The following search terms were combined: “cervical,” “uncinate process,” “uncinectomy,” “resection,” “removal” as either keywords or MESH terms. We reviewed all reference lists of all retrieved articles and searched manually to identify additional relevant articles. According to inclusion and exclusion criteria, we assessed identified articles systematically.
Selection Criteria
All included articles should meet all of the following inclusion criteria: (1) adults (over 18 years of age); (2) ACDF with UPR (anterior cervical discectomy and fusion with uncinate process resection) and ACDF without UPR; (3) cervical radiculopathy; (4) outcome was patient-rated scores (VAS or NDI or JOA) and/or radiographic outcome (sagittal alignment or fusion rate). Studies were excluded in the following situations: (1) with subjects who had cervical spine surgery due to ossification of posterior longitudinal ligaments, fractures, or tumors; (2) no specific data on the clinical effect and information about complications; (3) basic research reports including biomechanics and basic science studies; (4) no control group (ACDF) for comparison;
Data Extraction
Two investigators independently reviewed each retrieved article and extracted data from article texts, tables, and figures. From the studies, the following data items were considered: study design (author, year, and prospective or retrospective), study population (diagnosis, patient number, and age), efficacy evaluation indicators (visual analogue scale [VAS], neck disability index [NDI], and Japanese Orthopaedic Association [JOA] grade), radiographic outcome (sagittal alignment or fusion rate), and surgical details (intraoperative time and intraoperative blood loss). A third reviewer (WM) participated in discussion and consensus to resolve discrepancies between the two reviewers.
Methodological Quality and Risk of Bias
Newcastle-Ottawa Scale was adopted to assess the methodological quality by two reviewers while modifying it to match the needs of this study. 3 items: selection, comparability, and exposure composed the assessment of methodological quality of included articles. NOS scores higher indicated better quality of studies.
We assessed risks of bias of included trials through the criteria of the Cochrane Handbook for Systematic Reviews based on six different domains, which were graded as “low” or “high” risk of bias, or “unclear.”13,14
Statistical Analysis
We used the I2 statistics to evaluate the heterogeneity of all the studies. If the I2 value was ≥50 %, the assumption of homogeneity was rejected and a random-effects model was used. Otherwise, it was considered to be of good homogeneity and adopt a fixed-effects model. We used odds ratio (OR) as the summary statistic to analyze binary data such as fusion rate. Continuous data like decrease of JOA score was presented in terms of mean and standard deviation (SD). Asymmetry of funnel plots for each outcome was evaluated by Eggers' test. In case of sufficient evidence of funnel plot asymmetry, the trim and fill method were used to evaluate the influence of publication bias. P-values less than .05 was considered statistically significant, and all P-values were 2-sided. All meta-analyses were performed in the Review Manager version 5.3.
Results
Database Results
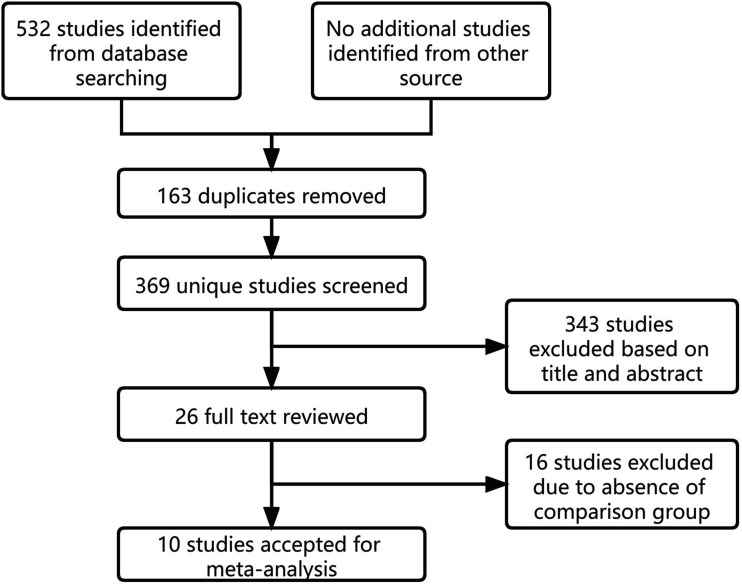
A total of 532 articles were identified from electronic database searches. After removal of 163 duplicated articles, 369 articles were screened on title and abstract. 343 irrelevant studies were excluded with a remaining of 26 articles. After full text review, we excluded 16 articles. Ultimately, 10 articles were selected for the meta-analysis.11,15-23 Figure 1 showed the selection process. NOS was adopted to assess the methodological quality of identified articles. The studies with the score of 7 were considered good quality. According to this method, all identified articles’ quality was showed to be superior (Table 1).
Figure 1.
Selection of Articles.
Table 1.
Study Characteristics and Demographics
| Author | Study type | Diagnosis | Age | Segment | Gender(male/female) | Resection tool | Follow-up(year) | |||
|---|---|---|---|---|---|---|---|---|---|---|
| UA | A | UA | A | UA | A | |||||
| Noh SH 2020 | R, RCT | CR | 49.1 ± 9.67 | 47.9 ± 9.78 | 24 | 24 | 8/16 | 9/15 | B+O | 2 |
| Mella P 2021 | P, RCT | CR | 57.7 ± 10.3 | 54.1 ± 10.4 | 523 | 596 | 153/122 | 195/136 | O | 2 |
| Sun B 2021 | R, RCT | CR | 58.2 ± 10.2 | 58.8 ± 10.9 | 78 | 192 | 30/25 | 67/59 | / | 1 |
| Abudouaini H 2021 | R, OS | CR | 51.46 ± 9.47 | 53.47 ± 10.36 | 37 | 50 | 17/20 | 22/28 | B | 1 |
| Lee DH 2018 | R, OS | CR | 57.7 ± 10.4 | 59.0 ± 10.5 | 180 | 57 | 66/55 | 23/23 | B | 2 |
| Huang JW 2019 | R, OS | CR | 46.9 ± 3.0 | 48.1 ± 4.2 | 73 | 39 | 26/23 | 17/10 | B | 1.5 |
| Wang XP 2020 | R, OS | CR | 56.2 ± 6.4 | 54.3 ± 9.2 | 23 | 33 | 9/8 | 12/14 | C | 3 |
| Lin D 2018 | R, OS | CR | 47.0 ± 3.32 | 45 + 2.34 | 83 | 41 | 33/24 | 18/11 | C | 1 |
| Liu SG 2019 | R, OS | CR | 42.97 ± 3.78 | 43.34 ± 3.67 | 54 | 44 | 23/17 | 18/14 | C | 2 |
| Shen FH 2004 | R, RCT | CR | 46 ± 10.6 | 47 ± 11.3 | 105 | 75 | 44/27 | 21/17 | B | 1 |
R retrospective; P prospective; OS observational study; RCT randomized controlled trial; CR cervical radiculopathy; UA UPR with ACDF; A simple ACDF; B burr; O osteotome; C curette
Risk of Bias
Concealment of randomization and allocation was not described in any included studies, as well as the blinding of outcome assessment, participants, and personnel. On the other hand, 9 of 10 included studies were retrospective studies. Outcome data was retained completely and selective reporting was avoided in all studies. All included studies were assessed at high risk of performance bias consequently. Through Eggers' test, we did not find significant publication bias in all of the statistical results of identified studies.
Study Characteristics and Demographics
In these 10 included studies, there were 746 patients who underwent ACDF with UPR compared to 729 patients who underwent ACDF. Only 1 study was prospective study and other 9 ones were retrospective studies. The publication years of 9 included studies ranged from 2018 to 2021 and the remaining one was published in 2004. All studies specified the indication as CR. The summary age was 53.7 ± 10.68 years for group of ACDF with UPR compared to 53.5 ± 10.78 years for ACDF group. In the group of ACDF with UPR, 409 of them were males while 337 were females. In the ACDF group, 402 of them were males while 327 were females. In the case of demographics information, there was no significant difference between 2 groups. The detailed study characteristics and demographics are shown in Table 2.
Table 2.
Newcastle–Ottawa Scale
| Author | Representativeness of exposed cohort | Selection of non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts based on basis of design or analysis | Assessment of outcomes | Was follow-up long enough for outcomes to occur(2 years) | Adequacy of follow-up of cohorts(80%) | Total scores |
|---|---|---|---|---|---|---|---|---|---|
| Noh SH 2020 | * | * | * | * | ** | * | * | 8 | |
| Mella P 2021 | * | * | * | * | ** | * | * | 8 | |
| Sun B 2021 | * | * | * | * | ** | * | 7 | ||
| Abudouaini H 2021 | * | * | * | * | ** | * | 7 | ||
| Lee DH 2018 | * | * | * | * | ** | * | * | 8 | |
| Huang JW 2019 | * | * | * | * | ** | * | 7 | ||
| Wang XP 2020 | * | * | * | * | ** | * | * | * | 9 |
| Lin D 2018 | * | * | * | * | ** | * | 7 | ||
| Liu SG 2019 | * | * | * | * | ** | * | * | 8 | |
| Shen FH 200 | * | * | * | * | ** | * | 7 |
Surgical Details
Intraoperative Time
Intraoperative time was reported in 4 included studies, involved 833 patients. In the group of ACDF with UPR, the pooled intraoperative time was 97.67 ± 22.23 min compared to 87.30 ± 17.71 min in the ACDF group. A significantly longer intraoperative time was found for ACDF with UPR compared to ACDF. (WMD 12.30, 95% CI: 4.83, 19.77, I2 = 81%, P = .001) (Figure 2).
Figure 2.
Forest Plot of Intraoperative Time.
Intraoperative Blood Loss
Intraoperative blood loss was reported in 4 included studies, involved 784 patients. In the group of ACDF with UPR, the pooled intraoperative blood loss was 46.86 ± 31.28 ml compared to 34.28 ± 36.28 ml in the ACDF group. A significantly more intraoperative blood loss was found for ACDF with UPR compared to ACDF. (WMD 14.99, 95% CI: 12.23, 17.76, I2 = 0%, P < .001) (Figure 3).
Figure 3.
Forest Plot of Intraoperative Blood Loss.
Clinical Outcome
Decrease of Neck VAS score (last follow-up)
We compared the decrease of neck pain from preoperative to the time of latest follow-up. The severity of neck pain was scored via the visual analogue scale (VAS), with 0 being no pain and 10 being the worst pain imaginable. Neck VAS was reported in 4 included studies, involved 908 patients. In the group of ACDF with UPR, the pooled decrease of Neck VAS score was 4.72 ± 2.19 compared to 4.06 ± 2.45 in the ACDF group. We could not find statistical difference between ACDF with UPR and ACDF in the improvement of preoperative Neck VAS and postoperative Neck VAS at the time of latest follow-up (WMD −.30, 95% CI: −.88, .27, I2 = 86%, P = .30) (Figure 4).
Figure 4.
Forest Plot of Neck VAS Score (Last Follow-Up).
Decrease of Arm VAS score (last follow-up)
We compared the decrease of arm pain from preoperative to the time of latest follow-up. The severity of arm pain was scored via the visual analogue scale (VAS). Arm VAS was reported in 7 included studies, involved 1113 patients. In the group of ACDF with UPR, the pooled decrease of Neck VAS score was 5.54 ± 1.81 compared to 5.31 ± 2.29 in the ACDF group. The result indicated that ACDF with UPR achieved seemingly better results than ACDF in improvement of arm pain at the time of latest follow-up. However, the difference was not statistically significant (WMD −.30, 95% CI: −.59, -.01, I2 = 71%, P = .05) (Figure 5).
Figure 5.
Forest Plot of Arm VAS Score (Last Follow-Up).
Decrease of Arm VAS score (early postoperative period)
We compared the decrease of neck pain from preoperative to the time of postoperative first follow-up (immediately after surgery or 1 week after surgery). Arm VAS of early postoperative period was reported in 4 included studies, involved 378 patients. In the group of ACDF with UPR, the pooled decrease of Arm VAS score was 3.22 ± 2.15 compared to 1.84 ± 2.16 in the ACDF group. A significantly more decrease of Arm Vas in the early postoperative follow-up was found for ACDF with UPR compared to ACDF (WMD −1.00, 95% CI: −1.85, -.14, I2 = 89%, P = .02) (Figure 6).
Figure 6.
Forest Plot of Arm VAS Score (Early Postoperative Period).
Improvement of NDI
We compared the decrease of NDI score from preoperative to the time of latest follow-up. NDI score was reported in 8 included studies, involved 1156 patients. In the group of ACDF with UPR, the pooled decrease of NDI score was 16.23 ± 5.48 compared to 14.34 ± 5.22 in the ACDF group. We could not find statistical difference between ACDF with UPR and ACDF in the improvement of preoperative NDI and postoperative NDI at the time of latest follow-up (WMD −1.01, 95% CI: −2.34, .33, I2 = 88%, P = .14) (Figure 7).
Figure 7.
Forest Plot of NDI.
Improvement of JOA
We compared the decrease of JOA from preoperative to the time of latest follow-up. JOA was reported in 4 included studies, involved 259 patients. In the group of ACDF with UPR, the pooled improvement of JOA was 5.66 ± 2.70 compared to 5.07 ± 2.54 in the ACDF group. We could not find statistical difference between ACDF with UPR and ACDF in the improvement of preoperative JOA and postoperative JOA at the time of latest follow-up (WMD −.1, 95% CI: −.24, .43, I2 = 18%, P = .56) (Figure 8).
Figure 8.
Forest Plot of JOA.
Radiographic Outcome
Change of C2-C7 Lordosis
We compared the change of C2-C7 lordosis from preoperative to the time of latest follow-up. C2-C7 lordosis was reported in 4 included studies, involved 378 patients. In the group of ACDF with UPR, the pooled modification of C2-C7 lordosis was .57 ± 6.65° compared to −.92 ± 7.02 in the ACDF group. We could not find statistical difference between ACDF with UPR and ACDF in the modification of C2-C7 lordosis and postoperative C2-C7 lordosis at the time of latest follow-up (WMD .23, 95% CI: −.87, 1.33, I2 = 0%, P = .68) (Figure 9).
Figure 9.
Forest Plot of C2-C7 Lordosis.
Change of C2-C7 SVA
We compared the change of C2-C7 SVA from preoperative to the time of latest follow-up. C2-C7 SVA was reported in 3 included studies, involved 302 patients. In the group of ACDF with UPR, the pooled modification of C2-C7 SVA was −.54 ± 6.04 mm compared to −1.64 ± 7.40 mm in the ACDF group. We could not find statistical difference between ACDF with UPR and ACDF in the modification of C2-C7 SVA and postoperative C2-C7 SVA at the time of latest follow-up (WMD 2.18, 95% CI: −.73, 5.08, I2 = 71%, P = .14) (Figure 10).
Figure 10.
Forest Plot of C2-C7 SVA.
Change of T1 Slope
We compared the change of T1 slope from preoperative to the time of latest follow-up. T1 slope was reported in 3 included studies, involved 302 patients. In the group of ACDF with UPR, the pooled modification of T1 slope was .23 ± 5.55° compared to .59 ± 5.53° in the ACDF group. We could not find statistical difference between ACDF with UPR and ACDF in the modification of T1 slope and postoperative T1 slope at the time of latest follow-up (WMD −.37, 95% CI: −2.25, 1.51, I2 = 58%, P = .70) (Figure 11).
Figure 11.
Forest Plot of T1 Slope.
Fusion Rate
We compared the fusion rate at the time of latest follow-up. Fusion rate was reported in 7 included studies, involved 1274 patients. In the group of ACDF with UPR, the pooled OR was 91.93% compared to 90.81% in the ACDF group. We could not find statistical difference between ACDF with UPR and ACDF in the fusion rate at the time of latest follow-up (OR 1.25, 95% CI: .83, 1.90, I2 = 0%, P = .29) (Figure 12).
Figure 12.
Forest Plot of Fusion Rate.
Discussion
Based on the results of meta-analysis, two group’s postoperative patient-rated disability outcomes were similar. We could not find statistical difference in JOA and NDI scores. However, patients who underwent ACDF with UPR could get better improvement of arm pain in the early postoperative period compared to ACDF. At the time of latest follow-up, the group of ACDF with UPR obtained seemingly better results than ACDF in the relief of arm pain as well. (P = .05) Some scholars believed that ACDF could obtain a satisfactory effect of decompression and UPR was nonessential for additional surgical risks. Some studies indicated that symptomatic relief could be achieved through disc space distraction and resorption of the osteophytes after solid fusion. 24 However, more previous studies’ findings were consistent with results of current meta-analysis, in which patients got rapid and significant relief of radicular pain after UPR. Clifton W reviewed 37 cases of ACDF with UPR in 10 years, 95% patients obtained pain-free outcome rate for radiculopathy which was defined as VAS 0 at latest follow-up. In Pakzaban’s study, the group of ACDF with UPR’s mean improvement in VAS scores for arm pain was 4.7 ± 2.3 during the follow-up period of 14-37 weeks. For symptomatic CR, the osteophytes of UP could narrow the foramen and cause damage to the exiting nerve. The hypertrophy of the UP could also extend lateral to the edge of the cervical disc space and make ACDF difficult in decompressing foraminal completely, trajectory of which is deep-to-superficial from within the disc space. 25 During UPR, the anterior wall of foramen was destructed and outlet space of nerve root was increased obviously, which relieved patients’ radicular pain significantly.
As for radiographic outcome, change of C2-C7 lordosis, C2-C7 SVA, T1 slope, and fusion rate showed similar results in both groups. Based on this finding, we found additional UPR did not have a more pronounced impact on cervical sagittal balance and segmental stability compared to ACDF. Clausen indicated the significant biomechanical implications of UP and found the reduction of cervical motion in all loading modes made by UP, especially in lateral bending and axial rotation. 26 So there were some concerns that UPR might cause hypermobility of the resected segment and added more load on load-bearing structures. Meanwhile, lateral limitation of UP to the intervertebral fusion was sacrificed for the UPR, which might cause the displacement of fusion and presence of pseudarthrosis.
However, a recent biomechanical study showed that UPR just slightly affected the sagittal kinematics, the range of motion lateral bending and axial rotation could be increased by UPR and the load on other structures was slightly increased. 27 From all included studies, the single UPR had less than 2 resected segments. In our opinion, the UPR with a lower number of resected segments was insufficient to influence global cervical sagittal balance. Interestingly, Lee DH found that ACDF with UPR group obtained a higher fusion rate (94.2%) than ACDF group (86.9%) in 2 years follow-up. 19 The authors interpreted this finding as the result of UPR’s compression effect to the upper and lower vertebra. We failed to find similar findings and description of this effect in other literature, which remained to be tested in future studies. Based on the existing studies, few clinical studies have described UPR’s impact on subsidence. Noh SH’s study did not find a significant adverse effect of subsidence during the 2-year follow-up. To the best of our knowledge, type of cage and size is a significant factor of subsidence. We were inclined to believe that ACDF with UPR did not pose extra requirements on the size of cage. This remained to be determined in future studies.
We noticed the statistical difference in surgical details between 2 groups. ACDF with UPR had a longer intraoperative time and more intraoperative blood loss than ACDF. Pakzaban reported that each UPR segment added an estimated 15 min to surgery time with an ultrasonic dissector. 28 This is not surprising. Although surgical techniques were different in different studies, UPR needed additional time to operate as an additional surgical step. On the other hand, as a bony structure, UP is composed of cortical bone and cancellous bone. UPR itself did not increase intraoperative bleeding significantly. Bleeding could occur from lateral epidural veins and the paravertebral venous plexus after the removal of UP. The pooled intraoperative blood loss in current meta-analysis was 46.86 ± 31.28 ml in group of ACDF with UPR, which was acceptable and expected. There was no report of vertebral artery injury or nerve root injury in all 746 patients of this group. In fact, for safety considerations, several techniques of UPR have been introduced including using high-speed burr, ultrasonic bone dissector, and osteotome. Notably, the presence of arterial variations of the V2 segment within the cervical intervertebral foramen is the contraindication of complete UPR, which was reported by Gitkind AI, and could be identified by preoperative imaging.
As a surgical procedure of direct decompression, UPR could be performed independently or combined with ACDF. In Verbiest H’s initial report, UP resect by a lateral approach, which was modified by Jho in 1996.29-31 This modified technique for standalone anterior cervical foraminotomy aimed to spare intervertebral discs and avoid fusion. However, operation visual field and operating space of UP were limited in this surgical procedure. Compared to this standalone resection, ACDF with UPR had a better stability of resected segment for the fusion. On the other hand, the operative vision of UP was clearer and broader through the disc space with the completion of an anterior diskectomy. 28 This surgical procedure combined the advantages of two surgeries, which balanced the easy manipulability and completeness of decompression.
It was in agreement with multiple studies that the indication of ACDF with UPR was CR with foraminal stenosis caused by osteophytes of hypertrophied UP.17,18,27,28,32,33 In accordance with Sun B’s study, the width of the intervertebral foramen (wIVF) was found to be significantly associated with the improvement in post-operative outcomes. 17 The author reported that patients with pre-operative wIVF<3mm who underwent ACDF with UPR had significantly better improvement of post-operative clinical symptoms than those who underwent ACDF alone, which quantified the severity of foraminal stenosis in the indication. Besides clinical study, a biomechanical study indicated that degenerative UP decreased cervical spine’s range of motion and shields other load-bearing structures. In summary, UPR was targeted and necessary for CR patients with severe foraminal stenosis. But regrettably, the quantified indication was not described in any other studies, which we hope could be standardized and quantified in more future research studies.
In most studies, UPR defaulted to the resection of the complete UP. Only a few of scholars focused on the resected areas of the UP. SH Lee reported that bilateral UPR over 38% during ACDF increased the risk of subsidence during follow-up. 34 Technique of minimal oblique UPR was adopted in Lee BH’s study with good clinical and radiological outcomes. 35 The posteromedial part of the hypertrophied UP was partially resected and the mean resected areas of the UP were 17.4 ± 8.7 mm 2 on the right and 17.3 ± 11.2 mm 2 on the left. However, some issues were still unresolved: Should UP be resected completely or partially? How much of the UP should be resected?
The feasibility and safety of ACDF with UPR were supported by the results of current meta-analysis. However, as a novel combination of two procedures, the number of studies investigated in this field was insufficient and the existing research was not deep enough. As is mentioned above, there are many aspects which are not yet been defined. These issues are expected to be explored and analyzed in future clinical studies.
In terms of surgical operation, complete exposure of the UP was a key step before attempting UPR and a thorough understanding of the pertinent anatomy was the precondition of this procedure. On average, the UP is 4.8 mm tall, 8 mm deep, and 4.9 mm wide at the base. The distance between the tip of the UP and the vertebral artery is between .6 and 2.5 mm. 36 Several techniques of UPR have been reported in previous studies. From Table 2, we could find that the major resection tools were osteotome, curette, and burr in the included studies. There were reports that burr could cause thermal injury to the VA, nerve root, and even the spinal cord. 37 On the other hand, burr could slip and entrap soft tissue for its rotating nature. From the 2 above-mentioned aspects, high speed burr might cause additional negative affect on intraoperative blood loss and clinical outcome compared to osteotome. However, using osteotome might prolong intraoperative time for a high requirement in surgical skills. During the ACDF with UPR, the posterior longitudinal ligament (PLL) could be identified after complete discectomy. Whether the PLL was taken down before or after UPR was based on the surgeon’s preferences. Leaving the PLL intact provided some protection to the nerve root and dura, and finding the plane behind the PLL was easier once the UP was removed.
We noticed some limitations of our study. Only 10 clinical trials with a relatively small sample size were included. Except Shen’s study, all of other included articles were published from 2018 to 2021, which reflected that ACDF with UPR had received little attention from researchers until recent years. As a result, the number of existing research was limited. Most of included studies were retrospective, non-randomized observational studies. Therefore, in future clinical work, high-quality, large-sample, and prospective randomized clinical trials should be conducted as far as possible to provide doctors with the best evidence-based information. Across these studies, there were also variations in the technical nuances of the surgical procedure with UPR and ACDF being performed with different techniques. These factors all add uncontrollable bias to our findings. Ideally, to minimize bias the operative technique, defined outcomes, and follow-up period should be standardized across all cases.
Conclusions
From the existing low-quality evidence, we found similar improvements of sagittal alignment, fusion rate, patient-rated disability outcomes, and neck pain in ACDF with UPR and ACDF. However, ACDF with UPR could obtain a significantly better relief in arm pain in the early postoperative period. Furthermore, ACDF with UPR had longer intraoperative time and more intraoperative blood loss. Notably, posterior-lateral disc herniation could cause nerve roots compression as well. In the case of disc herniation, ACDF alone can achieve a satisfactory outcome. Thus, the preoperative imaging examination (cervical X-rays with oblique views and CT) is essential for evaluating foraminal stenosis severity to judge whether or not to perform UPR. In summary, ACDF with UPR is an effective and necessary surgical method for CR patients with severe foraminal stenosis. No matter in intraoperative complications and cervical sagittal balance, ACDF with UPR is safe and reliable. Regrettably, there are currently no standardized and quantified surgical indications for ACDF with UPR. Larger sample-size prospective and randomized studies are required for further validation and analysis in the future.
Acknowledgments
We would like to thank the reviewers for their thorough review of our manuscript, especially under the severe circumstance of worldwide epidemic COVID-19, and we wish that everybody pulls through safe and sound.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data Availability: All supporting data can be provided upon request to the authors.
Abbreviation: CR: cervical radiculopathy; ACDF: anterior cervical discectomy and fusion; UP: uncinate process; UPR: uncinate process resection
ORCID iDs
Mengchen Yin https://orcid.org/0000-0001-7404-1495
References
- 1.Civelek E, Kiris T, Hepgul K, Canbolat A, Ersoy G, Cansever T. Anterolateral approach to the cervical spine: major anatomical structures and landmarks. J Neurosurg Spine. 2007;7(6):669-678. [DOI] [PubMed] [Google Scholar]
- 2.Uğur HC, Uz A, Attar A, Tekdemir I, Egemen N, Elhan A. Anatomical projection of the cervical uncinate process in ventral, ventrolateral, and posterior decompressive surgery. J Neurosurg. 2000;93(2 Suppl):248-251. [DOI] [PubMed] [Google Scholar]
- 3.Tracy JA, Bartleson JD. Cervical spondylotic myelopathy. Neurologist. 2010;16(3):176-187. [DOI] [PubMed] [Google Scholar]
- 4.Vanek P, Bradac O, DeLacy P, Saur K, Belsan T, Benes V. Comparison of 3 fusion techniques in the treatment of the degenerative cervical Spine disease. Is stand-alone autograft really the “Gold Standard?.” Spine. 2012;37(19):1645-1651. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka N, Fujimoto Y, An HS, Ikuta Y, Yasuda M. The anatomic relation among the nerve roots, intervertebral foramina, and intervertebral discs of the cervical spine. Spine. 2000;25(3):286-291. [DOI] [PubMed] [Google Scholar]
- 6.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am.40-A(3). 1958;40:607-624. [PubMed] [Google Scholar]
- 7.Kotani Y, McNulty PS, Abumi K, Cunningham BW, Kaneda K, McAfee PC. The role of anteromedial foraminotomy and the uncovertebral joints in the stability of the cervical Spine. Spine. 1998;23(14):1559-1565. [DOI] [PubMed] [Google Scholar]
- 8.Ishihara H, Kanamori M, Kawaguchi Y, Nakamura H, Kimura T. Adjacent segment disease after anterior cervical interbody fusion. Spine J. 2004;4(6):624-628. [DOI] [PubMed] [Google Scholar]
- 9.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15(6):602-617. [DOI] [PubMed] [Google Scholar]
- 10.Safaee MM, Nichols NM, Yerneni K, Zhang Y, Riew KD, Tan LA. Safety and efficacy of direct nerve root decompression via anterior cervical discectomy and fusion with uncinectomy for cervical radiculopathy. J Spine Surg. 2020;6(1):205-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS. Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J. 2004;4(6):629-635. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Noteboom EA, May AM, van der Wall E, de Wit NJ, Helsper CW. Patients' preferred and perceived level of involvement in decision making for cancer treatment: A systematic review. Psychooncology. 2021;30(10):1663-1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280-286. [DOI] [PubMed] [Google Scholar]
- 15.Noh SH, Park JY, Kuh SU, et al. Association of complete uncinate process removal on 2-year assessment of radiologic outcomes: Subsidence and sagittal balance in patients receiving one-level anterior cervical discectomy and fusion. BMC Musculoskelet Disord. 2020;21(1):439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mella P, Suk KS, Kim HS, et al. ACDF with total en bloc resection of uncinate in foraminal stenosis of the cervical Spine. Clin Spine Surg. 2021;34(4):E237-E242. [DOI] [PubMed] [Google Scholar]
- 17.Sun B, Xu C, Zhang Y, et al. Intervertebral foramen width is an important factor in deciding additional uncinate process resection in ACDF-a retrospective study. Front Surg. 2021;8:626344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abudouaini H, Wu T, Liu H, et al. Partial uncinatectomy combined with anterior cervical discectomy and fusion for the treatment of one-level cervical radiculopathy: Analysis of clinical efficacy and sagittal alignment. BMC Musculoskelet Disord. 2021;22(1):777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee DH, Cho JH, Baik JM, et al. Does additional uncinate resection increase pseudarthrosis following anterior cervical discectomy and fusion? Spine. 2018;43(2):97-104. [DOI] [PubMed] [Google Scholar]
- 20.Huang JW GW, Ding Z, et al. Application of anterior cervical decompression and fusion combined with partial resection of the uncinate joint in the treatment of cervical spondylotic radiculopathy. Orthopaedics. 2019;10(6):492-498. [Google Scholar]
- 21.Wang XP GL, Jia W, et al. Efficacy comparison of preservation and removal of the uncinate process in anterior cervical discectomy and intervertebral bone grafting and fusion surgery. Chin J Bone Joint Injury. 2020;35(1):32-34. [Google Scholar]
- 22.Lin D CC, Lin D, et al. Clinical efficacy comparison of retention and removal of the uncinate process in anterior cervical surgery. Orthopedic Journal of China. 2018;26(1):11-16. [Google Scholar]
- 23.SG L. Feasibility analysis of uncinate process retention in anterior decompression with intervertebral bone grafting and internal fixation for cervical spondylosis. The journal of Cervicodynia and Lumbodynia. 2019;40(3):326-329. [Google Scholar]
- 24.Bayley JC, Yoo JU, Kruger DM, Schlegel J. The role of distraction in improving the space available for the cord in cervical spondylosis. Spine. 1995;20(7):771-775. [DOI] [PubMed] [Google Scholar]
- 25.Tan LA, Riew KD. Anterior cervical foraminotomy: 2-dimensional operative video. Operative Neurosurgery. 2018;15(5):E66. [DOI] [PubMed] [Google Scholar]
- 26.Clausen JD, Goel VK, Traynelis VC, Scifert J. Uncinate processes and Luschka joints influence the biomechanics of the cervical spine: Quantification using a finite element model of the C5-C6 segment. J Orthop Res. 1997;15(3):342-347. [DOI] [PubMed] [Google Scholar]
- 27.Wang Z, Zhao H, Liu JM, Tan LW, Liu P, Zhao JH. Resection or degeneration of uncovertebral joints altered the segmental kinematics and load-sharing pattern of subaxial cervical spine: A biomechanical investigation using a C2-T1 finite element model. J Biomech. 2016;49(13):2854-2862. [DOI] [PubMed] [Google Scholar]
- 28.Pakzaban P. Ultrasonic total uncinectomy: A novel technique for complete anterior decompression of cervical nerve roots. Operative Neurosurgery. 2014;10:535-541.10discussion 541 [DOI] [PubMed] [Google Scholar]
- 29.Jho HD. Microsurgical anterior cervical foraminotomy for radiculopathy: A new approach to cervical disc herniation. J Neurosurg. 1996;84(2):155-160. [DOI] [PubMed] [Google Scholar]
- 30.Verbiest H. A lateral approach to the cervical spine: Technique and indications. J Neurosurg. 1968;28(3):191-203. [DOI] [PubMed] [Google Scholar]
- 31.Gitkind AI, Olson TR, Downie SA. Vertebral artery anatomical variations as they relate to cervical transforaminal epidural steroid injections. Pain Med. 2014;15(7):1109-1114. [DOI] [PubMed] [Google Scholar]
- 32.Clifton W, Williams D, Pichelmann M. How I do it: total uncinatectomy during anterior diskectomy and fusion for cervical radiculopathy caused by uncovertebral joint hypertrophy. Acta Neurochirurgica. 2019;161(10):2229-2232. [DOI] [PubMed] [Google Scholar]
- 33.Segar AH, Riccio A, Smith M, Protopsaltis TS. Total uncinectomy of the cervical spine with an osteotome: Technical note and intraoperative video. Neurosurg Spine. 2019;31:1-4. [DOI] [PubMed] [Google Scholar]
- 34.Lee SH, Lee JS, Sung SK, Son DW, Lee SW, Song GS. The effect of uncinate process resection on subsidence following anterior cervical discectomy and fusion. J Korean Neurosurg Soc. 2017;60(5):550-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee BH, Park JH, Lee JY, Jeon HJ, Park SW. Efficiency of minimal oblique resection of the uncinate process during an anterior cervical discectomy and fusion. Medicine. 2021;100(31):e26790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tubbs RS, Rompala OJ, Verma K, et al. Analysis of the uncinate processes of the cervical spine: An anatomical study. J Neurosurg Spine. 2012;16(4):402-407. [DOI] [PubMed] [Google Scholar]
- 37.Tarazi N, Munigangaiah S, Jadaan M, McCabe JP. Comparison of thermal spread with the use of an ultrasonic osteotomy device: Sonopet ultrasonic aspirator versus misonix bonescalpel in spinal surgery. J Craniovertebr Junction Spine. 2018;9(1):68-72. [DOI] [PMC free article] [PubMed] [Google Scholar]