Abstract
Study Design
Systematic Review and Meta-Analysis.
Objectives
The elderly have an increased risk of perioperative complications for Adult Spinal Deformity (ASD) corrections. Stratification of these perioperative complications based on risk type and specific risk factors, however, remain unclear. This paper will systematically review perioperative risk factors in the elderly undergoing ASD correction stratified by type: medical, implant-related, proximal junctional kyphosis (PJK), and need for revision surgery.
Methods
A systematic review was performed using the PRISMA guidelines. A query of PubMed was performed to identify publications pertinent to ASD in the elderly. Publications included in this review focused on patients ≥65 years old who underwent operative management for ASD to assess for risk factors of perioperative complications.
Results
A total of 734 unique citations were screened resulting in ten included articles for this review. Pooled incidence of perioperative complications included medical complications (21%), implant-related complications (16%), PJK (29%), and revision surgery (13%). Meta-analysis calculated greater preoperative PT (WMD 2.66; 95% Cl .36–4.96; P = .02), greater preoperative SVA (WMD 2.24; 95% Cl .62–3.86; P = .01), and greater postoperative SVA (WMD .97; 95% Cl .03–1.90; P = .04) to significantly correlate with development of PJK with no evidence of publication bias or concerns in study heterogeneity.
Conclusions
There is a paucity of literature describing perioperative complications in the elderly following ASD surgery. Appropriate understanding of modifiable risk factors for the development of medical and implant-related complications, proximal junctional kyphosis, and revision surgeries presents an opportunity to decrease morbidity and improve patient outcomes.
Keywords: adult spinal deformity, spinal deformity
Introduction
Although spinal deformity can affect any age group, the elderly are disproportionally impacted with the prevalence of adult spinal deformity (ASD) being as high as 68% in those over the age of 60. 1 ASD may present with a multitude of symptoms, including intractable axial back pain due to sagittal, and/or coronal plane imbalances, symptoms due to stenosis such as neurogenic claudication or radiculopathy, among others. As a result, ASD patients report lower health-related quality of life (HRQoL) scores on patient-reported outcome measures. 2 ASD is heterogeneous in clinical presentation and characterized by both clinical and radiographic parameters with treatment guided toward improvement of HRQoL. Aging is frequently associated with de-novo or degenerative scoliosis and accounts for up to 53% of pathology in ASD patients ≥65 years old, where asymmetric degeneration of the intervertebral discs and facet joints can lead to spinal column instability, spinal stenosis, or nerve root impingement.3-5 This contrasts with younger adults (<65 years old) where adult idiopathic scoliosis and degenerative scoliosis account for 43% and 29% of ASD pathology, respectively. 5
Degenerative ASD patients typically present with higher comorbidity indices compared to idiopathic, congenital, and other ASD subgroups due to advanced age. 6 With an increase in the proportion of elderly patients being seen in developed countries and the resultant increase in ASD prevalence, more knowledge pertaining to the treatment challenges that this population faces will be necessary.
Compared to conservative management of ASD, surgical treatment has been previously shown to result in superior clinical outcomes. In a study by Smith et al., 7 ASD surgical treatment of an aged patient cohort (65–85 years old) was found to result in a significant improvement in HRQoL similar to that seen in younger patients. Despite improved clinical outcomes, surgical correction of ASD has the potential for increased risk of complications in the elderly. 8 The incidence of perioperative complications in the elderly have been reported to be anywhere from 19.7% to 71%.5-7,9-15 Ambiguity in the exact risk factors that predispose the elderly to perioperative complications (whether from comorbidities, age-associated reserve, surgical correction techniques employed, etc.) necessitates further study in order for appropriate complication mitigation strategies to be devised.
The current literature regarding perioperative complications in the elderly is vague. Complications is an umbrella term which can include anything from medical complications to surgical or implant-related complications to the need for revision surgeries. Grouping of these categories has resulted in some ambiguity in the literature, as well as some uncertainty about true estimates regarding complication rates. Here, we evaluate each of these complications separately and their associated risk factors in the current literature.
Methods
A systematic review of the literature was performed using PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines to report risk factors for perioperative complications for ASD corrections. 16
Data Sources and Search
A query of PubMed was performed to identify publications pertinent to ASD in older aged individuals (age ≥65 years) published between 2005 and 2021. We searched for articles that reported on outcomes following surgical correction for ASD. The following keywords were used to search the database: “adult spinal deformity” and “adult spinal deformity surgery.” The AND, OR, and MeSH terms were used to improve search results.
Eligibility Criteria
Inclusion criteria for studies were as follows: (1) mean population of patients age ≥65, (2) studies in English, (3) studies published between 2005 and 2021, (4) study populations which received surgical correction for ASD, (5) studies with original patient data, (6) articles where postoperative complications were characterized, and (7) independent risk factors were identified. Exclusion criteria included (1) articles published prior to 2005, (2) systematic reviews, meta-analyses and reported case series without original patient data, and (3) corrective surgery for trauma or tumor.
Study Selection and Data Collection
Studies were initially screened by title and abstract for relevance. Full-text review for eligibility and data extraction was then performed. Screening, selection for eligibility, and data extraction was performed independently by 2 authors with any dispute being resolved through discussion between the 2 reviewers. All articles searched within PubMed were exported into Endnote X7 software for deduplication. Risk factors in the reported data were pooled from the studies stratified by type of complication. All available data from included studies was included for analysis. Levels of evidence were assigned to each individual study using the Oxford Centre for Evidence-Based Medicine Table. 17
Statistical Analysis
Studies were pooled to calculate crude incidence. Meta-analysis was performed using mean differences with 95% Cl Z-test values to describe continuous variables and odds ratios to describe dichotomous variables. A random-effects model was employed where there was significant heterogeneity otherwise, a fixed-effects model was utilized. Heterogeneity was significant when P < .10 for the Chi-squared test and when I2 >50%. Statistical analyses were performed using STATA 17.0 (Stata Corp, College Station, TX). To evaluate risk factors where there were no similarly reported variables between studies, we describe the results narratively presenting findings in the original research.
Risk of Bias Across Studies
Egger’s test was used to detect publication bias when meta-analyses were performed using at least 3 studies. Significance was defined using the alpha threshold of .05 unless otherwise specified.
Results
Study Selection
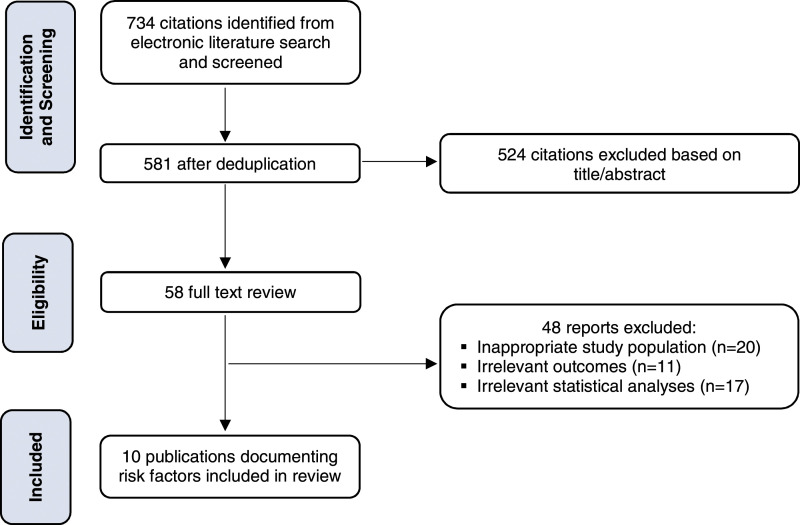
The search result in the database identified 734 articles in English during the 16-year study period. Additional screening and review narrowed the search to 58 articles. Forty-eight of these articles were excluded based on the age of the study population, extraneous outcome measures, and lack of complication risk-stratification. Ten publications were included in this review. The selection process included in this review is shown in Figure 1.
Figure 1.
Schematic depicting search algorithm for systematic literature review.
Study Characteristics
Baseline characteristics of the articles included in this review are presented in Table 1. The pooled demographics of the ten studies included 3893 patients with a mean age of 67 ± 7.50. Patients had 8.56 ± 2.8 levels fused on average. All studies were retrospective and classified as level IV evidence.
Table 1.
Study characteristics of articles included in review.
| Study | Total N | Age Mean ± SD | PSO N (%) | 3CO N (%) | Levels Fused Mean ± SD | Medical Complications N (%) | Implant-Related Complications N (%) | PJK N (%) | Revision N (%) |
|---|---|---|---|---|---|---|---|---|---|
| Daubs et al. 2007 | 46 | 66.8 ± 6.2 | 19 (41.3%) | NR | 9.1 ± 3.2 | 17 (37%) | NR | NR | 12 (26%) |
| Puvanesarajah et al. 2016 | 2293 | range: 65-84 | NR | NR | NR | NR | NR | NR | 241 (10.5%) |
| Park et al. 2017 | 160 | 67.6 ± 6.1 | 24 (15%) | NR | 6 ± 2.4 | NR | NR | 27 (16.9%) | NR |
| Wang et al. 2018 | 226 | 65.5 ± 8.1 | 3 (1.33%) | NR | NR | 44 (19.5%) | NR | NR | NR |
| Nguyen et al. 2019 | 260 | 65.2 ± 9.8 | 59 (22.7%) | 70 (26.9%) | 10.5 ± 3.2 | NR | 20 (7.7%) | NR | 83 (32%) |
| Jung et al. 2019 | 76 | 68.3 | NR | 28 (36.8%) | 9.9 ± 3.2 | NR | 9 (11.8%) | NR | NR |
| Im et al. 2020 | 83 | 70.3 ± 5.7 | 68 (82%) | NR | 8 | NR | NR | 30 (36.1%) | NR |
| Lau et al. 2020 | 405 | 64.5 | — | 405 (100%) | NR | 81 (20%) | 35 (7.7%) | NR | NR |
| Kawabata et al. 2020 | 230 | 72.2 ± 8.5 | NR | 95 (46.8%) | 7.9 ± 2 | NR | 91 (45%) | 51 (25.24%) | 35 (17.3%) |
| Xi et al. 2021 | 114 | 65.51 ± 8.05 | NR | NR | NR | NR | NR | 63 (55.3%) | NR |
| 3893 | 67 ± 7.50 | 173/775 (22%) | 598/971 (62%) | 8.56 ± 2.8 | 142/677 (21%) | 155/971 (16%) | 171/587 (29%) | 371/2829 (13%) |
Risk Factors for Medical Complications
The crude incidence of medical complications in 3 studies was 21%. There were no similarly reported variables across studies for the development of medical complications. Individually reported independent risk factors for medical complications included increased age, age >69 years old, patients who underwent a pedicle subtraction osteotomy, American Society of Anesthesiologists (ASA) grade >2, and operative duration.9,15
Risk Factors for Implant-Related Complications
The crude incidence of implant-related complications in 4 studies was 16%. Meta-analyses of 3 studies18-20 revealed no significant relationship between body mass index (BMI), bone mineral density (BMD), fused number of instrumented vertebrae and development of implant-related complications (data not shown). Meta-analyses of 2 studies reported no relationship between uppermost instrumented vertebrae (UIV) above T6, UIV below T6, lower instrumented vertebrae (LIV) to the sacrum and relationship to the development of implant-related complications (data not shown).19,20 Individually reported independent risk factors for implant-related complications included increased age at surgery, greater postoperative global tilt, greater preoperative thoracolumbar kyphosis, and pedicle subtraction osteotomy at S1.19,21
Risk Factors for PJK
The crude incidence of PJK in 3 studies was 29%. Commonly reported variables across all studies included spinopelvic parameters on radiographs including thoracic kyphosis (TK), pelvic tilt (PT), sagittal vertical axis (SVA), and pelvic incidence minus lumbar lordosis (PI-LL). Meta-analyses of 3 studies22-24 resulted in greater preoperative PT (WMD 2.66; 95% Cl .36–4.96; P = .02), greater preoperative SVA (WMD 2.24; 95% Cl .62–3.86; P = .01), and greater postoperative SVA (WMD .97; 95% Cl .03–1.90; P = .04) to significantly correlate with development of PJK (Figures 2–4). Preoperative, postoperative, and change in TK had no significant correlation with development of PJK. Pre- and postoperative measures of PI-LL had no statistically significant correlation with development of PJK on meta-analyses (data not shown). Individually reported independent risk factors for the development of PJK included greater postoperative thoracic kyphosis, dorsal displacement of the L1 plumb line measured as the L1 to gravity line distance, and greater BMI.23,24
Figure 3.
Forest plot showing relationship between preoperative SVA and PJK.
Figure 2.
Forest plot showing relationship between preoperative pelvic tilt and PJK.
Figure 4.
Forest plot showing relationship between postoperative SVA and PJK.
Risk Factors for Revision Surgery
The crude incidence of revision surgeries in 4 studies was 13%. There were no similarly reported variables across studies for the risk of revision surgery. The individually reported risk factors for revision surgery included greater time to clinical follow-up and presence of osteoporosis.18,25
Risk of Bias Across Studies
For variables exploring implant-related complications, Egger’s test showed no evidence of publication bias (BMI t = −.05, P = .97; fused number of instrumented vertebrae t = 2.11, P = .28). Heterogeneity was low and not significant in the meta-analyses for variables exploring risk of PJK preoperative PT (p for heterogeneity = .90, I2 = 0%), preoperative SVA (p for heterogeneity = .36, I2 = 3%), and postoperative SVA (p for heterogeneity = .92, I2 = 0%). The test for heterogeneity was significant in the meta-analyses for preoperative, postoperative and change in TK (preoperative TK p for heterogeneity = .004, I2 = 82%; postoperative TK p for heterogeneity = .01, I2 = 79%; change in TK p for heterogeneity = .13, I2 = 51%). Egger’s test revealed no evidence of publication bias (preoperative TK t = −2.17, P = .27; postoperative TK t = −.61, P = .65; change in TK t = −1.97, P = .30; preoperative PT t = −.44, P = .74; preoperative SVA t = −1.22, P = .44; postoperative SVA t = −.28, P = .83).
Discussion
Current Management
When adjusted by extent of spinal deformity and surgical treatment, Oswestry Disability Index (ODI) and Scoliosis Research Society-22 (SRS-22) pain scores are markedly worse in older individuals compared to a younger matched cohort following ASD correction. 10 In a study by Smith et al., older patients were found to have more disability (worse ODI scores) at baseline compared to younger patients. However, the older patient cohort was also then found to have a similar postoperative improvement as the younger patient cohort in the study at the 2-year follow-up timepoint. Despite potential for perioperative complications, older patients stand to benefit from surgical intervention for ASD. 7
Surgical treatment for ASD has increased linearly over time, with interbody fusions and three-column osteotomies becoming more common. 26 In a paper by Sing et al., between 2004 and 2011 the incidence of ASD correction surgery was found to be increasing most for patients aged 65–69 years old, followed by those aged 70–74. 27 Another smaller study found that use of decompression and osteotomy for ASD correction are more often used in the elderly (65–85 years old), as opposed to patients aged 25-64 where the use of Smith-Petersen osteotomies is much more common. Furthermore, pelvic fixation is also more commonplace in older patients. 7
Radiographic Correction
The SRS-Schwab classification correlates spinopelvic radiographic parameters with HRQoL outcomes which include the following: (1) pelvic incidence minus lumbar lordosis, (2) pelvic tilt, (3) sagittal vertical axis (SVA). This classification serves as a framework for alignment goals in ASD. 28 The most widely used radiographic parameter to measure extent of sagittal malignment is assessed through the SVA, which is defined by the distance from a vertical line drawn from the middle of the C7 vertebral body (C7 vertical tilt/plumb line) to the posterosuperior endplate of S1.
Correcting ASD by radiographic spinopelvic parameters has traditionally been done by applying average threshold values to all patients. Correcting sagittal alignment based on age has recently gained traction in the literature. A retrospective study of 903 patients with ASD reported that the average/optimal spinopelvic alignment goals traditionally used (PI-LL < 10, PT < 20, SVA < 4 cm) is less applicable to patients with high pelvic incidence and increased age. 29 This is because patient compensation tends to increase over time in order to adapt to age-related changes in sagittal alignment (such as an increased sagittal vertical axis, increased pelvic tilt due to loss of lumbar lordosis, spinopelvic mismatch, and an increased T1 pelvic angle). Patients >65 years old with ASD demonstrate age-related increases in lower-body compensatory mechanisms reaching ideal spinopelvic alignment 1 year after surgery with greater compensation in patients who were under corrected for ASD. 30 Moreover, aggressive overcorrection of ASD can contribute to complications such as proximal junctional kyphosis. 31 For example, the ideal PI-LL mismatch for a younger patient (45–54 years old) is .5° which gradually increases to 17° in those at least 74 years old (Table 2). Similarly, SVA is ideal when close to 1 cm in patients <54 years old, whereas that number gradually increases to almost 8 cm in those at least 74 years old. Essentially, an age-appropriate achievement of PI-LL and SVA correction exists where overcorrection past these points may be associated with complications and worse outcomes.
Table 2.
PT: pelvic tilt, LL: lumbar lordosis, SVA: sagittal vertical axis. Ideal age-specific alignment parameters correlate to HRQoL and patient-reported outcomes. This table was taken from an article published by Lafage et al. (DOI: 10.1097/BRS.0000000000002146).
| Ideal age-specific alignment criteria | |||
|---|---|---|---|
| Patient population (age) | PT (°) | PI-LL (°) | SVA (mm) |
| <35 | 11.0 | −10.5 | −30.5 |
| 35–44 | 15.4 | −4.6 | −5.5 |
| 45–54 | 18.8 | 0.5 | 15.1 |
| 55–64 | 22.0 | 5.8 | 35.8 |
| 65–74 | 25.1 | 10.5 | 54.5 |
| ≥74 | 28.8 | 17.0 | 79.3 |
Medical Complications
A very well-established risk factor for medical complications is increased age with patients >69 years old being 9 times more likely to develop medical complications. 9 Interestingly, 1 retrospective review of 300 patients found that increased age did not significantly predict development of medical complications compared to those aged 50–64, 65–79, and ≥80 years old. However, this study did find that older patients presented with higher complication rates. The authors attributed this discrepancy to the extrapolation of data from databases vs single-institution cohorts. 12 Inclusion of studies solely reported from databases may give rise to certain biases due to the limited amount of information one can extrapolate from databases. The medical complication rates in elderly patients ≥65 for the studies included in this review range from 20% to 37%.9,21
Daubs et al. reported that for every year-increase in a patient’s age, there is a 23% increased risk of developing a postoperative complication. Patients with and without postoperative complications were compared in the study and demonstrated significant improvement in ODI scores with no correlation in change in ODI scores with age. This suggests that while increased age is associated with the development of complications, it may have little impact on HRQoL. 9 Soroceanu et al. also reported that medical complications ultimately do not affect clinical outcome. Despite medical complications, patients experience significant improvement in HRQoL similar to that of patients without medical complications. 32
Patients who undergo a PSO are at an increased risk of medical complications. 9 Rigid spinal deformities often require spinal osteotomies for correction. Three-column osteotomies such as pedicle subtraction osteotomy (PSO) or vertebral column resection can be used to achieve appropriate spinal column correction. Anticipation of these risks may be a way to mitigate medical complications. Therefore, other correction strategies and techniques such as multiple lateral interbody fusions in order to release lateral osteophytes or aggressive posterior transforaminal interbodies should each be considered. Performing a PSO in the elderly should only be performed when absolutely necessary given its association with increased EBL, operative time, etc. and subsequent hardware and/or medical complications.
Implant-Related Complications
Late surgical complications are typically due to continuous mechanical stress that can result in implant-related complications. Implant-related complications encompass a wide variety of pathologies including proximal junction kyphosis, distal junction kyphosis, pseudoarthrosis, rod breakage, vertebral fracture, among others.
The incidence of implant-related complications is reported to be anywhere from 4.2% to 45% in the elderly.12,19 Kawabata et al. 19 reported the following types of mechanical failure in an elderly patient cohort: vertebral fracture (20%), rod fracture (13%), pseudarthrosis (7%), and distal junctional kyphosis (4%).
Other studies report screw loosening to be more prevalent in patients ≥75 years old compared to rod breakage. 33 These can have poor outcomes as Yamato et al. 34 reported an 18% incidence of rod fracture (mean age 68.5) in a cohort of 304 patients with 66.7% of these patients requiring revision surgeries.
Increased postoperative global tilt was an independent risk factor for implant-related complications in the elderly. Global tilt was defined as the sum of the pelvic tilt and the C7 vertical tilt. Interestingly, there was no significant association in postoperative sagittal vertical axis or postoperative pelvic tilt between patients who developed implant-related failure vs those who did not. 19 This brings up a salient point in determining which radiographic parameters are most predictive of complication risks. One can infer that overcorrection of spinopelvic parameters leading to an increased postoperative global tilt can result in complications. Cautious determination of age-appropriate thresholds for ASD correction should be performed to mitigate these risks.
Proximal Junctional Kyphosis
PJK most commonly occurs above UIV and is defined as kyphosis of 10 or more degrees greater than preoperative measurements. Progression from PJK to proximal junctional failure (PJF) necessitates revision surgery. PJF is defined by both kyphosis and structural failure of the vertebral body.
Lafage et al. 31 reported increased age at surgery as a risk factor for development of PJK. Incidence of PJK was reported at 50.2% in those >65 years old. This retrospective cohort study involving 679 patients with ASD demonstrated that patients >65 years old who developed PJK were overcorrected compared to non-PJK patients when comparing 1-year postoperative PI-LL mismatch to age-adjusted alignment criteria.
Revision Surgeries
A cohort study evaluating the risk of revision surgeries in 553 patients who were surgically treated for ASD found an incidence of 19.9% revision surgeries at a 2-year follow-up period and an incidence of 7.2% patients who underwent more than 1 single revision surgery. When stratified by age, revision risk was at 25.4% for 60–70 year olds and 23.3% for patients over the age of 70. 35 Another study reported a 47.3% revision rate in age ≥70. This study reported comparable rates of revisions in age ≥70 compared to age 41–55, as well as nonsignificant differences between the amount of hardware failures, pseudarthrosis, PJK, or sagittal malalignment indicated for the revisions. 13 Puvanesarajah et al 25 reported the following revision rates in 2293 patients aged 65–84: 10.5% at 1 year, 15.4% at 2 years, 17.2% at 3 years, 18.2% at 4 years, and 18.5% at 5 years.
In a propensity score-matched analysis, there was no significant difference in the amount of revision surgeries in advanced age when comparing cohorts aged 50–65 and >70 years old. 10
Indications for revision risks appear to be similar across age groups. Puvanesarajah et al. found the following indications for revisions in a cohort age 65–84: instrument failure accounted for 53.5% for revisions at 1 year and 62.3% of revisions at 5 years. Infections accounted for 24.1% of revisions at 1 year and 21.2% of revisions at 5 years. 25 Pitter et al. 35 found the following indications for revisions in a younger cohort with a median age of 53: implant failure 38.2%, infection 11.8%, curve progression 10.9%, pseudarthrosis 10.9%, neurologic deficit 10.9%, and PJK 7.3%.
Osteoporosis increases revision risk in the elderly. 25 Osteoporotic compression fractures can result in kyphotic deformities typically within the thoracic and lumbar spine. Osteoporosis is exceedingly common in patients with ASD age ≥65. 5 In a retrospective cohort study of 110 patients (age 73.86 ± 5.20), fragility vertebral fractures of ≥10 degrees of kyphosis presented with worse global spinal alignment (measured via the T1 pelvic angle) and increased disability indices. 36 In terms of mitigation strategies, perioperative daily teriparatide treatment when compared to bisphosphonate treatment, has shown decreased amounts of adjacent vertebral fractures in patients ≥75 years of age with both ASD and osteoporosis. 33
BMP use is associated with lower risk of revision surgery reported at both 4- and 5-year follow-up in the elderly. 25 A prospective clinical trial reported increased rates of fusions in ASD patients treated with recombinant human bone morphogenetic-protein-2 without graft supplementation. 37
Mortality
Elderly patients (age >65) with ASD present with increased mortality postoperatively when compared to ages 25–64. 6 Jain et al. 38 reported the perioperative mortality rate to be .9% in a 3519-patient sized cohort of >65 year olds at 6 weeks postoperatively and to be 1.8% at 2 years follow-up.
Summary of Evidence
In our systematic review with meta-analysis, we have reported the incidence of medical complications, implant-related complications, PJK, and incidence of revision surgery in the elderly. We have reported the individual risk factors stratified by risk type. Despite lack of high-level evidence studies included in this review, our meta-analyses demonstrate that increased preoperative pelvic tilt, increased preoperative and postoperative SVA significantly correlates with development of PJK.
Limitations
Several limitations exist in our study. The paucity of literature regarding perioperative complications in the elderly limited the power and stability of our meta-analysis. Subsequently, a single study can influence the sensitivity of the meta-analysis, which is especially the case for analyses stemming from unadjusted variables. Ultimately our review is novel as it remains the first to discuss perioperative complications in the elderly stratified by risk type.
Conclusion
Current literature has established that surgical correction for ASD in the elderly is associated with increased risk of complications. Despite these risks, the elderly demonstrate improved HRQoL measures postoperatively similar to younger patients. 7 There is ambiguity in the literature regarding independent risk factors for perioperative complications in the elderly. There is a need for appropriate stratification of complications to assess for true measures of risks. Appropriate understanding of modifiable risk factors for the development of medical complications, implant-related complications, proximal junctional kyphosis, and revision surgeries presents an opportunity to decrease morbidity and improve patient outcomes. Elderly ASD patients represent a challenging demographic that require a unique set of skills. An appropriate perioperative risk assessment should be performed to mitigate development of complications and need for additional surgery. Elderly patients should be counseled on risks prior to surgical intervention to guide expectations and management.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Angelica Alvarez Reyes https://orcid.org/0000-0002-6708-1365
Andrew S. Jack https://orcid.org/0000-0001-9620-4734
References
- 1.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. 2005;30(9):1082-1085. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 2.Kyrölä K, Repo J, Mecklin JP, Ylinen J, Kautiainen H, Häkkinen A. Spinopelvic changes based on the simplified SRS-schwab adult spinal deformity classification: relationships with disability and health-related quality of life in adult patients with prolonged degenerative spinal disorders. Spine. 2018;43(7):497-502. doi: 10.1097/brs.0000000000002370. [DOI] [PubMed] [Google Scholar]
- 3.Youssef JA, Orndorff DO, Patty CA, et al. Current status of adult spinal deformity. Global Spine J. 2013;3(1):51-62. doi: 10.1055/s-0032-1326950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diebo BG, Shah NV, Boachie-Adjei O, et al. Adult spinal deformity. Lancet. 2019;394(10193):160-172. doi: 10.1016/s0140-6736(19)31125-0. [DOI] [PubMed] [Google Scholar]
- 5.Yamato Y, Matsuyama Y, Hasegawa K, et al. A Japanese nationwide multicenter survey on perioperative complications of corrective fusion for elderly patients with adult spinal deformity. J Orthop Sci. 2017;22(2):237-242. doi: 10.1016/j.jos.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Worley N, Marascalchi B, Jalai CM, et al. Predictors of inpatient morbidity and mortality in adult spinal deformity surgery. Eur Spine J. 2016;25(3):819-827. doi: 10.1007/s00586-015-4104-x. [DOI] [PubMed] [Google Scholar]
- 7.Smith JS, Shaffrey CI, Glassman SD, et al. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine. 2011;36(10):817-824. doi: 10.1097/BRS.0b013e3181e21783. [DOI] [PubMed] [Google Scholar]
- 8.Yagi M, Rahm M, Gaines R, et al. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine. 2014;39(10):E607-E614. doi: 10.1097/brs.0000000000000266. [DOI] [PubMed] [Google Scholar]
- 9.Daubs MD, Lenke LG, Cheh G, Stobbs G, Bridwell KH. Adult spinal deformity surgery: complications and outcomes in patients over age 60. Spine. 2007;32(20):2238-2244. doi: 10.1097/BRS.0b013e31814cf24a. [DOI] [PubMed] [Google Scholar]
- 10.Yagi M, Fujita N, Okada E, et al. Clinical outcomes, complications, and cost-effectiveness in surgically treated adult spinal deformity over 70 years: a propensity score-matched analysis. Clin Spine Surg. 2020;33(1):E14-E20. doi: 10.1097/bsd.0000000000000842. [DOI] [PubMed] [Google Scholar]
- 11.Miller EK, Neuman BJ, Jain A, et al. An assessment of frailty as a tool for risk stratification in adult spinal deformity surgery. Neurosurg Focus. 2017;43(6):E3. doi: 10.3171/2017.10.Focus17472. [DOI] [PubMed] [Google Scholar]
- 12.Lau D, Osorio JA, Deviren V, Ames CP. The relationship of older age and perioperative outcomes following thoracolumbar three-column osteotomy for adult spinal deformity: an analysis of 300 consecutive cases. J Neurosurg Spine. 2018;28(6):593-606. doi: 10.3171/2017.10.Spine17374. [DOI] [PubMed] [Google Scholar]
- 13.Challier V, Henry JK, Liu S, et al. Complication rates and maintenance of correction after 3-column osteotomy in the elderly: report of 55 patients with 2-year follow-up. Neurosurgery. 2018;83(5):973-980. doi: 10.1093/neuros/nyx580. [DOI] [PubMed] [Google Scholar]
- 14.Yagi M, Hosogane N, Fujita N, et al. Predictive model for major complications 2 years after corrective spine surgery for adult spinal deformity. Eur Spine J. 2019;28(1):180-187. doi: 10.1007/s00586-018-5816-5. [DOI] [PubMed] [Google Scholar]
- 15.Wang H, Zhang Z, Qiu G, Zhang J, Shen J. Risk factors of perioperative complications for posterior spinal fusion in degenerative scoliosis patients: a retrospective study. BMC Musculoskelet Disord. 2018;19(1):242. doi: 10.1186/s12891-018-2148-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.OCEBM Levels of Evidence Working Group . The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence. [Google Scholar]
- 18.Nguyen JH, Buell TJ, Wang TR, et al. Low rates of complications after spinopelvic fixation with iliac screws in 260 adult patients with a minimum 2-year follow-up. J Neurosurg Spine. 2019;30(5):1-9. doi: 10.3171/2018.9.Spine18239. [DOI] [PubMed] [Google Scholar]
- 19.Kawabata A, Yoshii T, Sakai K, et al. Identification of predictive factors for mechanical complications after adult spinal deformity surgery: a multi-institutional retrospective study. Spine. 2020;45(17):1185-1192. doi: 10.1097/brs.0000000000003500. [DOI] [PubMed] [Google Scholar]
- 20.Jung JM, Hyun SJ, Kim KJ, Jahng TA. Rod fracture after multiple-rod constructs for adult spinal deformity. J Neurosurg Spine. 2019;32:1-8. doi: 10.3171/2019.9.Spine19913. [DOI] [PubMed] [Google Scholar]
- 21.Lau D, Haddad AF, Deviren V, Ames CP. Complication profile associated with S1 pedicle subtraction osteotomy compared with 3-column osteotomies at other thoracolumbar levels for adult spinal deformity: series of 405 patients with 9 S1 osteotomies. J Neurosurg Spine. 2020;33(5):1-11. doi: 10.3171/2020.4.Spine20239. [DOI] [PubMed] [Google Scholar]
- 22.Im SK, Lee JH, Kang KC, et al. Proximal junctional kyphosis in degenerative sagittal deformity after under- and overcorrection of lumbar lordosis: does overcorrection of lumbar lordosis instigate PJK? Spine. 2020;45(15):E933-E942. doi: 10.1097/brs.0000000000003468. [DOI] [PubMed] [Google Scholar]
- 23.Xi Z, Duan PG, Mummaneni PV, et al. Posterior displacement of L1 may be a risk factor for proximal junctional kyphosis after adult spinal deformity correction. Global Spine J. 2021:21925682211015651. doi: 10.1177/21925682211015651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH. Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery. 2017;80(2):279-286. doi: 10.1227/neu.0000000000001240. [DOI] [PubMed] [Google Scholar]
- 25.Puvanesarajah V, Shen FH, Cancienne JM, et al. Risk factors for revision surgery following primary adult spinal deformity surgery in patients 65 years and older. J Neurosurg Spine. 2016;25(4):486-493. doi: 10.3171/2016.2.Spine151345. [DOI] [PubMed] [Google Scholar]
- 26.Passias PG, Poorman GW, Jalai CM, et al. Morbidity of adult spinal deformity surgery in elderly has declined over time. Spine. 2017;42(16):E978-E982. doi: 10.1097/brs.0000000000002009. [DOI] [PubMed] [Google Scholar]
- 27.Sing DC, Berven SH, Burch S, Metz LN. Increase in spinal deformity surgery in patients age 60 and older is not associated with increased complications. Spine J. 2017;17(5):627-635. doi: 10.1016/j.spinee.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 28.Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine. 2012;37(12):1077-1082. doi: 10.1097/BRS.0b013e31823e15e2. [DOI] [PubMed] [Google Scholar]
- 29.Protopsaltis TS, Soroceanu A, Tishelman JC, et al. Should sagittal spinal alignment targets for adult spinal deformity correction depend on pelvic incidence and age? Spine. 2020;45(4):250-257. doi: 10.1097/brs.0000000000003237. [DOI] [PubMed] [Google Scholar]
- 30.Passias PG, Horn SR, Frangella NJ, et al. Full-body analysis of adult spinal deformity patients' age-adjusted alignment at 1 year. World Neurosurg. 2018;114:e775-E784. doi: 10.1016/j.wneu.2018.03.079. [DOI] [PubMed] [Google Scholar]
- 31.Lafage R, Schwab F, Glassman S, et al. Age-adjusted alignment goals have the potential to reduce PJK. Spine. 2017;42(17):1275-1282. doi: 10.1097/brs.0000000000002146. [DOI] [PubMed] [Google Scholar]
- 32.Soroceanu A, Burton DC, Oren JH, et al. Medical complications after adult spinal deformity surgery: incidence, risk factors, and clinical impact. Spine. 2016;41(22):1718-1723. doi: 10.1097/brs.0000000000001636. [DOI] [PubMed] [Google Scholar]
- 33.Seki S, Hirano N, Kawaguchi Y, et al. Teriparatide versus low-dose bisphosphonates before and after surgery for adult spinal deformity in female Japanese patients with osteoporosis. Eur Spine J. 2017;26(8):2121-2127. doi: 10.1007/s00586-017-4959-0. [DOI] [PubMed] [Google Scholar]
- 34.Yamato Y, Hasegawa T, Kobayashi S, et al. Treatment strategy for rod fractures following corrective fusion surgery in adult spinal deformity depends on symptoms and local alignment change. J Neurosurg Spine. 2018;29(1):59-67. doi: 10.3171/2017.9.Spine17525. [DOI] [PubMed] [Google Scholar]
- 35.Pitter FT, Lindberg-Larsen M, Pedersen AB, Dahl B, Gehrchen M. Revision Risk after primary adult spinal deformity surgery: a nationwide study with two-year follow-up. Spine Deform. 2019;7(4):619. doi: 10.1016/j.jspd.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 36.Langella F, Balestrino A, Damilano M, et al. The aging spine: the effect of vertebral fragility fracture on sagittal alignment. Arch Osteoporos. 2021;16(1):109. doi: 10.1007/s11657-021-00975-w. [DOI] [PubMed] [Google Scholar]
- 37.Luhmann SJ, Bridwell KH, Cheng I, Imamura T, Lenke LG, Schootman M. Use of bone morphogenetic protein-2 for adult spinal deformity. Spine. 2005;30(17 suppl l):S110-S117. doi: 10.1097/01.brs.0000175184.27407.6a. [DOI] [PubMed] [Google Scholar]
- 38.Jain A, Hassanzadeh H, Puvanesarajah V, et al. Incidence of perioperative medical complications and mortality among elderly patients undergoing surgery for spinal deformity: analysis of 3519 patients. J Neurosurg Spine. 2017;27(5):534-539. doi: 10.3171/2017.3.Spine161011. [DOI] [PubMed] [Google Scholar]