Abstract
Study Design
Systematic review and meta-analysis.
Objective
To evaluate systematically the complications of prolonged cervical immobilisation in a hard collar.
Methods
Following registration with PROSPERO, a systematic search of electronic databases (MEDLINE, EMBASE) was conducted. Two reviewers independently screened the search results according to pre-determined search criteria. Data was extracted and tabulated. Joanna Briggs Institute checklists were used for assessing the quality of included studies.
Results
The search identified 773 articles. A total of 25 studies were selected for final inclusion. The results largely comprised a mixture of case reports/series, cohort studies and reviews. The most commonly reported complications were pressure ulcers, dysphagia and increased intracranial pressure. A pressure ulcer pooled prevalence of 7% was calculated. There was insufficient data for quantitative analysis of any other complication.
Conclusions
There is significant morbidity from prolonged hard collar immobilisation, even amongst younger patients. Whilst based upon limited and low-quality evidence, these findings, combined with the low-quality evidence for the efficacy of hard collars, highlights a knowledge gap for future research.
Keywords: cervical, vertebrae, trauma, post-operative, hard collar, orthosis, complications, pressure ulcers, dysphagia, systematic review, meta-analysis
Introduction
The prolonged use of rigid cervical collars is common, either as part of non-operative management of spinal trauma, but also as an adjunct to cervical spine surgery. 1 It is estimated 13/100,000 patients undergo non-operative management of a cervical spine fracture each year. 2 The frequency of their use following cervical spine surgery is less well defined. 3 When used for either indication, immobilisation is often for at least 4 weeks.3-5
Prolonged periods of hard collar use were defined in this study as ≥2 days of wear, to distinguish from emergency immobilisation. Prolonged use can lead to a range of adverse effects, including pressure ulceration, raised intracranial pressure (ICP) and dysphagia. 6 These complications, which can occur in both inpatients and outpatients, can cause morbidity which may be avoidable.6,7
Recent studies have questioned the effectiveness of using hard collars post-operatively.8,9 Compounded by a lack of recognition of the potential complications, this has resulted in inconsistent guidance from surgeons. 3
Although some reviews have been published detailing adverse events and quality improvement protocols,6,10-12 there is no systematic review providing a comprehensive analysis of the complications of prolonged use.
The objective of this systematic review is to characterise the frequency and factors associated with complications the results of which should support decision-making by healthcare professionals.
Method
A systematic review of the literature was performed, compliant with the preferred reporting items of systematic reviews and meta-analysis (PRISMA) guidelines (Supplementary Data 1) and prospectively registered with PROSPERO (CRD42021247869).
Search Strategy and Search Criteria
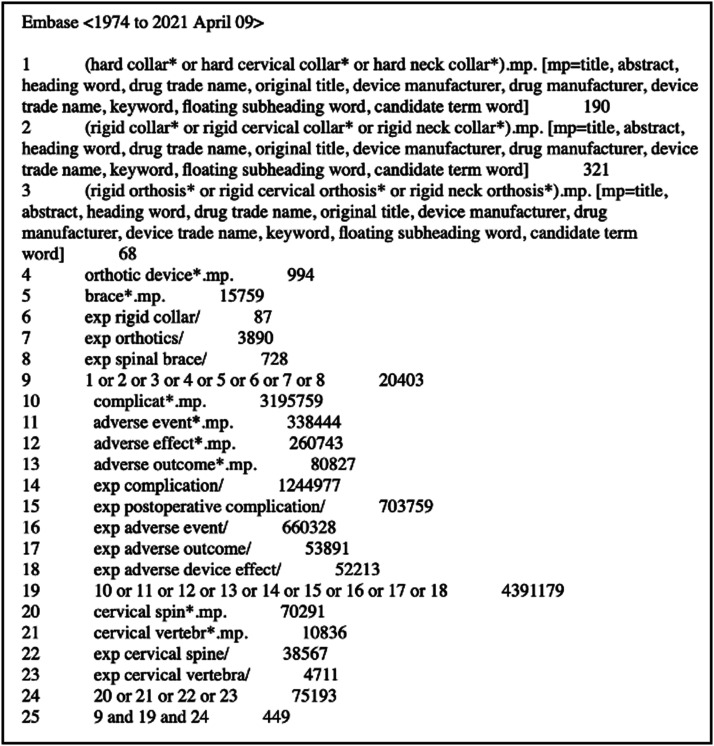
A sensitive search strategy (Supplementary Data 2) was developed with a medical librarian for EMBASE and MEDLINE. Searches were performed using Ovid (Wolters Kluwer, Netherlands) from inception to 9th April 2021. An example of the terms used in the Embase search is shown in Figure 1.
Figure 1.
Embase search strategy.
Articles in English, of any nature, reporting on the complications related to prolonged hard collar use were included (Table 1). For the purpose of this study, ‘prolonged use’ was defined as the wearing of a hard collar on at least two consecutive days, thereby distinguishing from cases of emergency immobilisation. Two reviewers (J.B and E.D) independently performed title and abstract screening with blinding, using Rayyan. 13 A pilot screen of 50 publications was first done to ensure concordance and any disagreements following unblinding were resolved by discussion.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| English, full text | Other forms of orthosis (e.g., Halo, SOMI, soft collar) in isolation |
| Adults (18 years and above) | |
| Reporting on complications of orthosis related to prolonged use of a rigid collar, where prolonged is defined as wear on at least two consecutive days | Animal studies |
| Cadaveric studies | |
| Children and youths (up to and including 17 years) | |
| Where the primary focus is acute care with no follow-up | |
| Editorials, letters, replies |
Screening for eligibility occurred in accordance with the criteria in Table 1.
Data Extraction and Critical Appraisal
Articles were retrieved for full-text screening and data extraction using a piloted table.
The Joanna Briggs Institute (JBI) critical assessment tools were chosen on the basis of wide variations in study design, the absence of large randomised control trials and the inclusion of case reports. 14 JBI checklists were completed to assess the quality of the included articles (Supplementary Data 3).
Full-text screening and data extraction were performed by the same two reviewers. Any differences were reconciled through discussion and consensus.
Quantitative Analysis
Meta-analysis was performed where two or more primary studies reported on the prevalence of the same complication. Analysis was performed using R (v4.0.5; R Core Team, 2020) and RStudio (v1.4.1106; RStudio Team, 2021). The R packages ‘meta’ (v4.18-0) 15 and ‘ggplot2’ (v3.3.3) 16 were used to generate pooled prevalence estimates and explore associations using bivariate regression, respectively.
Results
Search Strategy
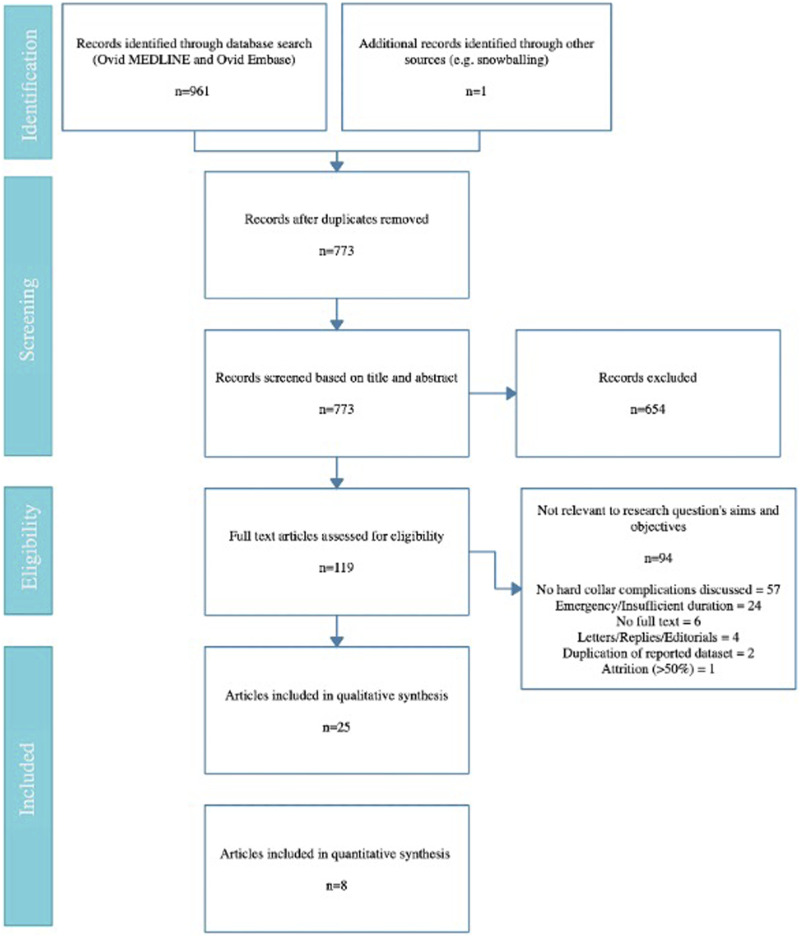
After removing duplicates, the initial search identified 773 articles. Subsequent abstract and title screening eliminated 654 articles, leaving 119 shortlisted for full text review. Of these, 25 were included in this study (Figure 2). A meta-analysis was performed on a subsection of the included articles (n = 8).
Figure 2.
PRISMA flow diagram of the search strategy.
A kappa (κ) value of .69 was calculated for title and abstract screening and a value of .95 for full text screening. There was thus a substantial degree of inter-rater reliability. Furthermore, there was complete concordance for data extraction and quality assessment.
Study Characteristics
Alongside 5 narrative reviews and 1 systematic review, 19 primary clinical studies were identified. This included 13 cohort studies, 4 case reports/series, 1 randomised trial and 1 economic evaluation. Of the primary clinical studies, the mean patient age ranged from 26.8 to 84 and publication years were between 1991 and 2020.
The majority (12/19) of the primary research included was conducted entirely in an inpatient setting. The exceptions were 2 studies involving volunteers17,18 and 5 studies with outpatient follow up.5,7,19-21 Three studies exclusively recruited patients from critical care.22-24 Most studies reported on skin breakdown/ulceration (17/25), and to lesser extent dysphagia (6/25) and increased ICP (4/25).
An evidence summary for the included cohort studies is shown in Table 2. The evidence summary table for the remaining studies can be found in Supplementary Data 4.
Table 2.
Evidence summary table of the included cohort studies.
| Authors | Year | Country | Mean Patient Age, yrs | Collar Indication | Collar Type | Reported Complications | Frequency of Complications | Mean Duration of Wear, Days |
|---|---|---|---|---|---|---|---|---|
| Moran et al. | 2013 | Australia | NR | Trauma | Aspen | Dysphagia Delirium LRTI Falls | 4/8 (50%) 3/8 (38%) 5/8 (63%) 3/8 (38%) | NR d |
| Molinari et al. | 2012 | USA | 84 | Trauma | Miami J | Skin breakdown/ulceration | 2/34 (6%) | 84 (SD = 0) |
| Powers et al. | 2006 | USA | 37.8 | Trauma | Aspen | Skin breakdown/ulceration | 33/484 (7%) | 10.3 (SD = 11.4) |
| Molano et al. | 2004 | Spain | 35.5 | Trauma | NR | Skin breakdown/ulceration | 22/92 (24%) | NR e |
| Nakanishi et al. | 2019 | Australia | 81.9 | Trauma | Philadelphia | Skin breakdown/ulceration HAP | 11/90 (12%) 10/90 (11%) | NR |
| Hylton et al. | 2016 | UK | 74 | Trauma | Miami J | Psychosocial issues Skin breakdown/ulceration Skin erythema | 6/51 (12%) 2/51 (4%) 10/51 (20%) | 50.8 |
| Ham et al. | 2014 | USA | 43.7 | Trauma | Various | Skin breakdown/ulceration | 1/88 (1%) | 3.5 (SD = 3.4) |
| Lewis et al. | 2011 | Australia | NR | Trauma | NR | Skin breakdown/ulceration | 2/32 (6%) | NR f |
| Ackland et al. | 2007 | Australia | 40.9 a | Trauma | Philadelphia | Skin breakdown/ulceration | 27/299 (9%) | NR g |
| Karlberg et al. | 1991 | Sweden | 26.8 | Volunteer | Philadelphia | Impaired voluntary saccades | NR | 5 |
| Borders et al. | 2018 | USA | NR b | Trauma | NR | Dysphagia | 104/113 (92%) | NR |
| Kalb et al. | 2012 | USA | 51 | Post-operative | NR | Dysphagia | NR c | NR |
| Iizuka et al. | 2005 | Japan | 61.4 | Post-operative | Philadelphia | Reduced cervical ROM | NR | 42 h |
aMean male age = 38.2 yrs and mean female age = 43.5 yrs; assumption of equal proportion.
bA majority (58%) of patients were under 65 yrs.
cThere were 27 cases of dysphagia reported, with no significant increase in the hard collar group.
dDuration of immobilisation = 2–12 weeks.
eMedian day of ulcer detection = 7.
fMean duration of all patients = 94.5 days.
gMedian duration = 1 day (IQR = 2).
hOne group 8 weeks in collar and the other 4 weeks in collar.
NR = not reported, LRTI = lower respiratory tract infection, HAP = hospital acquired pneumonia, ROM = range of motion
Pressure Ulceration
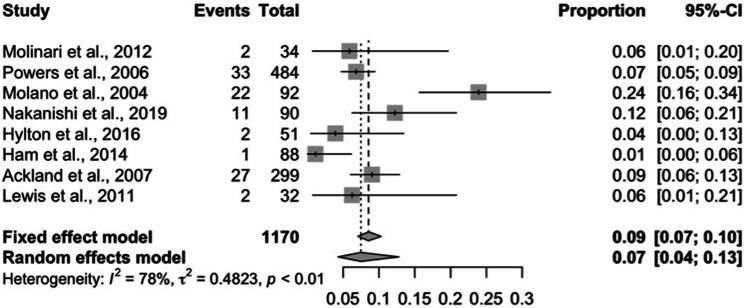
Eight primary clinical studies reported on the occurrence of skin breakdown/ulceration. These studies cumulatively include 1,170 patient outcomes and the mean duration of hard collar immobilisation ranged from 3.5 days to 84 days. A more detailed description of these studies is shown in in Table 3.
Table 3.
A subgroup evidence table of studies reporting on pressure ulcer frequency.
| Authors | Year | Mean Patient Age, Years | Specific Trauma Indication | Collar Type | Skin Breakdown Frequency | Outpatient Follow up | Mean Duration of Wear, Days | Nursing Measures |
|---|---|---|---|---|---|---|---|---|
| Molinari et al. | 2012 | 84 (Range = 71–99) | Type II odontoid fracture | Miami J | 2/34 (6%) | Yes | 84 (SD = 0) | NR |
| Powers et al. | 2006 | 37.8 (Range = 2–94) | Confirmed cervical injury, ICU | Aspen | 33/484 (7%) | No | 10.3 (SD = 11.4) | Pad change every 24 hrs, skin clean every 12 hrs |
| Molano et al. | 2004 | 35.5 (SD = 13.8) | Suspected cervical injury, ICU | NR | 22/92 (24%) | No | NR c | NR |
| Nakanishi et al. | 2019 | 81.9 (SD = 8.6) | Suspected cervical injury | Philadelphia | 11/90 (12%) | No | NR | Removed, cleaned and dried every 4–8 hrs |
| Hylton et al. | 2016 | 74 (Range = 21–95) | Confirmed cervical injury | Miami J | 2/51 (4%) | Yes | 50.8 | Removed and adjusted weekly (outpatient) |
| Ham et al. | 2014 | 43.7 (SD = 19.6; Range = 18–91) | Suspected cervical injury, ICU | Various | 1/88 (1%) | No | 3.5 (SD = 3.4) | Pressure relieving mattress, turning every 2 hrs, occipital foam ring |
| Lewis et al. | 2011 | NR | Type II odontoid fracture | NR | 2/32 (6%) | Yes | NR d | NR |
| Ackland et al. | 2007 | 40.9 (SD = 18.6) a | Suspected cervical injury | Philadelphia | 27/299 (9%) | No | NR e | Patient position changed every 8 hrs. Removed, cleaned and dried every 4–8 hrs |
aMean male age = 38.2 ± 16.7 years and mean female age = 43.5 ± 20.4 years; assumption of equal proportion.
bA majority (58%) of patients were under 65 years.
cMedian day of ulcer detection = 7.
dMean duration of all patients = 94.5 days.
eMedian duration = 1 day (IQR = 2).
SD = standard deviation, NR = not reported, ICU = intensive care unit, hrs = HoursGrey = excluded from age regression analysis.
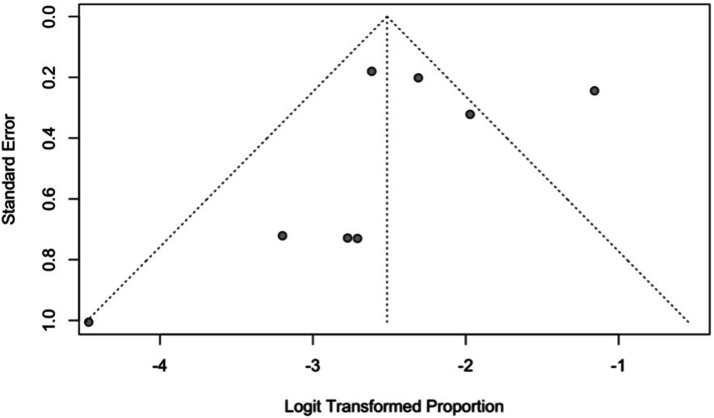
Reported incidence across studies displayed high heterogeneity (I 2 = 78%; Figure 3).
Figure 3.
An asymmetric funnel plot displaying study heterogeneity.
Using a random effects model, the pooled prevalence was estimated as 7% [95% CI: 4–13%] (Figure 4).
Figure 4.
A pooled prevalence analysis of pressure ulcers in cases of prolonged hard collar immobilisation; random effects model.
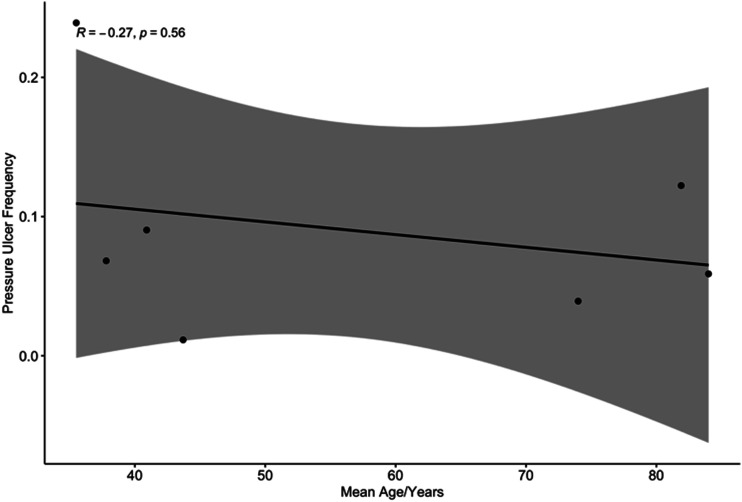
In order to explore potential sources of heterogeneity, factors associated with pressure ulceration were explored based on data reported. Seven studies reported on both mean patient age and the frequency of pressure ulceration in patients immobilised with hard collars. A bivariate regression analysis was undertaken to establish if there was a correlation between increased age and pressure ulceration. In the context of wide confidence intervals, there was no significant correlation observed between the variables (Figure 5; Spearman rank correlation coefficient, R, was −.27).
Figure 5.
Bivariate regression analysis of pressure ulcer frequency as a function of mean patient age.
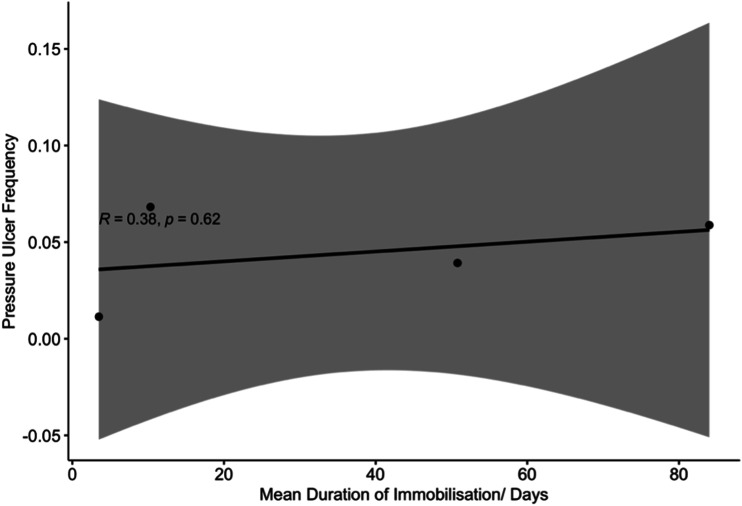
A mean duration of immobilisation was disclosed in 4 studies reporting pressure ulcers.7,20,22,24 Bivariate regression analysis revealed no significant correlation between these variables (Figure 6; Spearman rank correlation coefficient, R, was .38). A positive association between length of stay and collar-related pressure ulceration was reported in 1 study. 25
Figure 6.
Bivariate regression analysis of pressure ulcer frequency as a function of mean duration of immobilisation.
Dysphagia
A total of 3 primary studies described dysphagia as a complication of prolonged use of a hard collar.19,26,27 Kalb et al. (2012) 26 found no significant association compared to a group with no collar. However, Borders et al. (2018) 27 reported that cervical bracing was both a significant predictor of dysphagia and associated with greater dysphagia severity. In a cohort study without a non-immobilised group, Moran et al. (2013) 19 observed a prevalence of dysphagia of 50%.
Increased Intracranial Pressure
A single randomised trial spanning 5 days 17 demonstrated evidence of increased ICP each day, measured indirectly via optic nerve sheath diameter.
Miscellaneous
The frequency of respiratory infections was assessed in 2 of the included studies.19,25 Lower respiratory tract infection (LRTI) was observed in 5/8 participants in a small cohort study, 19 while hospital acquired pneumonia was diagnosed in 11/90 patients in a larger study. 25 There was no control population without cervical immobilisation in either case. In both studies, all recruited patients were hospital inpatients aged over 65.
One study investigated the effects of hard collar immobilisation on postural control and voluntary eye movements in healthy volunteers. 18 Measures of postural control were not significantly altered, however, there was a significant reduction in the velocity of voluntary saccades.
A single retrospective study with 24–48 month follow-up recorded a significant reduction in mean cervical range of motion following immobilisation for 8 weeks (46%), compared to 4 week immobilisation (25%). 5
Psychosocial issues associated with prolonged hard collar use were examined in one study with outpatient follow up. 7 Mood swings and/or low self-esteem were reported by 6/51 of the participants. The mean immobilisation duration was 7.25 weeks and there was again no control arm.
Discussion
This is the first systematic review and meta-analysis studying adverse events associated with prolonged hard collar immobilisation. Current evidence is largely of low quality and based on inpatients with trauma. It is apparent that complications can occur. Pressure ulceration was the most frequently studied and suitable for meta-analysis, occurring in 7% (95% CI: 4%, 13%) of cases.
In trauma hard collars are used to immobilise the cervical spine in order to reduce pain and reduce the risk of displacement or deformity. Use of a hard collar is considered to be a safe therapy with low morbidity.
The findings of this review highlight the risk and incidence of complications. Hard collars double the occurrence of pressure sores above what is expected for inpatients in general 28 and increase the risk of dysphagia. 27 Moreover, there could be implications for co-existent injuries with one study using healthy volunteers showing that hard collars increase intracranial pressure. 17 This corroborates an extensive literature of direct measurements. 29 Management of raised intracranial pressure is a key component of the treatment of head injury, which co-exists with spinal trauma in up to 60% of cases. 30
Due to the limited scope and length of observation, the incidence of complications is likely to be an under-estimate. Most of the reported evidence relates to inpatients following trauma with outpatient follow up only conducted in 4 studies.7,19-21 Much of the patient timeline is unaccounted for, omitting those patients with prolonged hard collar immobilisation. This leads to underreporting of complications. Constraints on the type of complication reported were imposed in each study. For instance, the two large cohort studies of dysphagia prevalence failed to report on pressure ulceration.26,27
Lastly, some complications cited in the literature were not discussed in the cohort studies, such as nerve compression palsies. 31
How these findings apply to an elective and/or outpatient setting remains uncertain. The morbidity associated with immobilisation in a hard collar should be taken into account in decision making around the risks and benefits. The National Institute for Health Research, United Kingdom, has recently commissioned the DENS Trial. This study of the duration of external neck stabilisation following odontoid fracture in older or frail adults is a randomised controlled trial of collar vs no collar (DENS RCT). 32 Whilst this population represents a subgroup of hard collar use, it will collect the first high-quality prospective data on hard collar morbidity.
One of the surprising findings of this review was that morbidity was not associated with age. In the context of study limitations, this should be interpreted cautiously, as skin fragility and therefore pressure sore risk increases with age. 33 One potential explanation for this, would be the recognition of this risk, with planned interventions, such as selective use of hard collars and/or routine collar care for elderly patients, to mitigate it.
Another surprising finding was the absence of an association between length of stay and pressure ulceration. This is at odds with our existing understanding for the pathophysiology of pressure ulcers, 34 whereby an increased time of immobilisation increases the risk of small ischaemic events of the skin. Again, this must therefore be interpreted cautiously, largely due to the limited reporting of duration and length of follow up (Figure 6).
Limitations
The included studies had inconsistent methodologies, outcome measures and reporting style. An important limitation is the sparse and haphazard nature of the literature. This was offset, at least in part, by using a random effects model in the meta-analysis.
The identification of pressure ulcers is inconsistent, as evidenced by the lower inter-observer reliability using the European Pressure Ulcer Advisory Panel (EPUAP) classification system. 35 This was minimised in the prospective cohort studies by experienced observers. More generally, distinguishing between EPUAP scores was not relevant to this meta-analysis and confusion with other lesions is unlikely in the cervical region.
Omissions in data limited the power of some analyses, such as the infrequent reporting of the duration of immobilisation and the absence of reporting the time at which complications occurred. Similarly, there was little data in middle-aged adults, illustrated in Figure 4. This was likely a consequence of the bimodal age distribution of cervical injuries in young adults and the elderly. Absent data was recognised both in the interpretation and graphically by confidence intervals.
Whilst Borders et al. (2018) 27 established a positive dysphagia association with videofluoroscopic swallowing studies, Kalb et al. (2012) 26 found no association in subjective clinician and patient reports. It can be argued that subjective dysphagia is more clinically relevant. Nonetheless, image-confirmed dysphagia suggests there might exist a greater risk of aspiration.
Implications for Practice and Future Investigation
The rates of surgery for age-related (degenerative) indications are rising 36 and an ageing population is at greater risk of low-velocity cervical spine fragility injuries. 37 Hard collar immobilisation may be used increasingly in the future despite uncertainty about effectiveness and the incidence of adverse events.
Of the few examples we identified, both the collar design and co-existent care were implicated in modifying adverse events. For example, Spark et al. (2013) 38 reported that Miami J and Aspen collars were more favourable for features such as reduced tissue interface pressure and reduced skin humidity, whilst Powers (1997) 39 used a nursing protocol to reduce the occurrence of pressure sores.
Although mentioned in patient advice leaflets as a complication, 40 this review did not capture any direct studies of cervical muscle atrophy consequent to hard collar use. Just one included study alludes to this, 5 with subtle range of motion deficits measured following longer immobilisation. It is suggested that cervical muscle atrophy may be responsible. This represents a further knowledge gap in the literature.
A growing body of evidence suggests that hard collars are often used following cervical spine surgery. This comprises both the decision whether to use a hard collar and the duration of immobilisation. For some common procedures, neither clinical outcome nor fusion are different with or without the use of a hard collar.5,8,9
Evidence is needed to allow informed and cost-effective decision making between surgeons and patients. The shifting cost-benefit analysis lends itself to randomised controlled trial with a specific focus on hard collar complications. The aforementioned DENS trial is therefore a welcome start.
Conclusion
Prolonged immobilisation with hard collars causes a range of morbidity, including pressure sores, dysphagia, increased ICP and peripheral nerve palsies. However, the current data reporting on incidence is of low quality, and high-quality prospective studies are needed to decide on the merits and risks of using hard collar in patients with cervical spine injuries and following cervical spine surgery.
Supplementary Material
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: BMD is supported by a Royal College of Surgeons Research Fellowship and an NIHR Clinical Doctoral Research Fellowship.
Disclaimer: The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Jamie F.M. Brannigan https://orcid.org/0000-0003-1697-403X
Benjamin M. Davies https://orcid.org/0000-0003-0591-5069
References
- 1.Agabegi SS, Asghar FA, Herkowitz HN. Spinal orthoses. J Am Acad Orthop Surg. 2010;18(11):657-667. doi: 10.5435/00124635-201011000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Fredø HL, Bakken IJ, Lied B, Rønning P, Helseth E. Incidence of traumatic cervical spine fractures in the Norwegian population: a national registry study. Scand J Trauma Resuscitation Emerg Med. 2014;22:78. doi: 10.1186/s13049-014-0078-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bible JE, Biswas D, Whang PG, Simpson AK, Rechtine GR, Grauer JN. Postoperative bracing after spine surgery for degenerative conditions: A questionnaire study. Spine J. 2009;9(4):309-316. doi: 10.1016/j.spinee.2008.06.453. [DOI] [PubMed] [Google Scholar]
- 4.Robinson AL, Schmeiser G, Robinson Y, Olerud C. Surgical vs. non-surgical management of displaced type-2 odontoid fractures in patients aged 75 years and older: Study protocol for a randomised controlled trial. Trials. 2018;19(1):452. doi: 10.1186/s13063-018-2690-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iizuka H, Nakagawa Y, Shimegi A, et al. Clinical results after cervical laminoplasty. Clinical Spine Surgery. 2005;18(6):489-491. doi: 10.1097/01.bsd.0000154447.83084.b2. [DOI] [PubMed] [Google Scholar]
- 6.Webber-Jones JE, Thomas CA, Bordeaux REJ. The management and prevention of rigid cervical collar complications. Orthop Nurs. 2002;21(4):19-27. [DOI] [PubMed] [Google Scholar]
- 7.Hylton B, Lidder S, Armitage A, James S. Eastbourne Miami-J Protocol: A pilot study for the care of cervical injuries in the community. Acta Chir Orthop Traumatol Cech. 2016;83(3):186-188. [PubMed] [Google Scholar]
- 8.Campbell MJ, Carreon LY, Traynelis V, Anderson PA. Use of cervical collar after single-level anterior cervical fusion with plate. Spine. 2009;34(1):43-48. doi: 10.1097/BRS.0b013e318191895d. [DOI] [PubMed] [Google Scholar]
- 9.Hida T, Sakai Y, Ito K, et al. Collar fixation is not mandatory after cervical laminoplasty. Spine. 2017;42(5):E253-E259. doi: 10.1097/BRS.0000000000001994. [DOI] [PubMed] [Google Scholar]
- 10.Waqar M, Van-Popta D, Barone DG, Sarsam Z. External immobilization of odontoid fractures: A systematic review to compare the halo and hard collar. World Neurosurg. 2017;97:513-517. doi: 10.1016/j.wneu.2016.10.035. [DOI] [PubMed] [Google Scholar]
- 11.Peck GE, Shipway DJH, Tsang K, Fertleman M. Cervical spine immobilisation in the elderly: A literature review. Br J Neurosurg. 2018;32(3):286-290. doi: 10.1080/02688697.2018.1445828. [DOI] [PubMed] [Google Scholar]
- 12.Zarghooni K, Beyer F, Siewe J, Eysel P. The orthotic treatment of acute and chronic disease of the cervical and lumbar spine. Dtsch Arztebl int. 2013;110(44):737-742. doi: 10.3238/arztebl.2013.0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zeng X, Zhang Y, Kwong JSW, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J Evid Base Med. 2015;8(1):2-10. doi: 10.1111/jebm.12141. [DOI] [PubMed] [Google Scholar]
- 15.Schwarzer G, Carpenter JR, Rücker G. An Introduction to Meta-Analysis in R. In: Schwarzer G, Carpenter JR, Rücker G, eds. Meta-Analysis with R. Use R!. Springer International Publishing; 2015:3-17. doi: 10.1007/978-3-319-21416-0_1. [DOI] [Google Scholar]
- 16.Wickham H. Programming with ggplot2. In: Wickham H, ed. Ggplot2: Elegant Graphics for Data Analysis. Use R! Springer International Publishing; 2016:241-253. doi: 10.1007/978-3-319-24277-4_12. [DOI] [Google Scholar]
- 17.Ladny M, Smereka J, Ahuja S, Szarpak L, Ruetzler K, Ladny JR. Effect of 5 different cervical collars on optic nerve sheath diameter. Medicine. 2020;99(16):e19740. doi: 10.1097/MD.0000000000019740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karlberg M, Magnusson M, Johansson R. Effects of restrained cervical mobility on voluntary eye movements and postural control. Acta Otolaryngol. 1991;111(4):664-670. [DOI] [PubMed] [Google Scholar]
- 19.Moran C, Kipen E, Chan P, et al. Understanding post-hospital morbidity associated with immobilisation of cervical spine fractures in older people using geriatric medicine assessment techniques: A pilot study. Injury. 2013;44(12):1838-1842. doi: 10.1016/j.injury.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 20.Molinari RW, Khera OA, Gruhn WL, McAssey RW. Rigid cervical collar treatment for geriatric type II odontoid fractures. Eur Spine J. 2012;21(5):855-862. doi: 10.1007/s00586-011-2069-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewis E, Liew S, Dowrick A. Risk factors for non-union in the non-operative management of type II dens fractures. ANZ J Surg. 2011;81(9):604-607. [DOI] [PubMed] [Google Scholar]
- 22.Powers J, Daniels D, McGuire C, Hilbish C. The incidence of skin breakdown associated with use of cervical collars. J Trauma Nurs. 2006;13(4):198-200. [DOI] [PubMed] [Google Scholar]
- 23.Molano Alvarez E, Murillo Perez MA, Salobral Villegas MT, Dominguez Caballero M, Cuenca Solanas M, Garcia Fuentes C. Úlceras por presión secundarias a la inmovilización con collarín cervical: Una complicación de la lesión cervical aguda. Enfermería Intensiva. 2004;15(3):112-122. [DOI] [PubMed] [Google Scholar]
- 24.Ham HWW, Schoonhoven LL, Galer AA, Shortridge-Baggett LLM. Cervical collar-related pressure ulcers in trauma patients in intensive care unit. J Trauma Nurs. 2014;21(3):94-102. doi: 10.1097/JTN.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 25.Nakanishi T, Mitra B, Ackland H, O’Reilly G, Cameron P. Time in collars and collar-related complications in older patients. World Neurosurg. 2019;129(101528275):e478-e484. doi: 10.1016/j.wneu.2019.05.187. [DOI] [PubMed] [Google Scholar]
- 26.Kalb S, Reis MT, Cowperthwaite MC, et al. Dysphagia after anterior cervical spine surgery: Incidence and risk factors. World Neurosurg. 2012;77(1):183-187. doi: 10.1016/j.wneu.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 27.Borders JC, Gibson AL, Grayev A, Thibeault S. Predictors of dysphagia in critically injured patients with neck trauma. J Crit Care. 2018;44:312-317. doi: 10.1016/j.jcrc.2017.12.004. [DOI] [PubMed] [Google Scholar]
- 28.Kayser SA, VanGilder CA, Lachenbruch C. Predictors of superficial and severe hospital-acquired pressure injuries: A cross-sectional study using the international pressure ulcer prevalence survey. Int J Nurs Stud. 2019;89:46-52. doi: 10.1016/j.ijnurstu.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 29.Dunham CM, Brocker BP, Collier BD, Gemmel DJ. Risks associated with magnetic resonance imaging and cervical collar in comatose, blunt trauma patients with negative comprehensive cervical spine computed tomography and no apparent spinal deficit. Crit Care. 2008;12(4):R89. doi: 10.1186/cc6957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Macciocchi S, Seel RT, Thompson N, Byams R, Bowman B. Spinal cord injury and co-occurring traumatic brain injury: Assessment and incidence. Arch Phys Med Rehabil. 2008;89(7):1350-1357. doi: 10.1016/j.apmr.2007.11.055. [DOI] [PubMed] [Google Scholar]
- 31.Rodgers JA, Rodgers WB. Marginal mandibular nerve palsy due to compression by a cervical hard collar. J Orthop Trauma. 1995;9(2):177-179. doi: 10.1097/00005131-199504000-00015. [DOI] [PubMed] [Google Scholar]
- 32.NIHR Funding and Awards Search Website . Accessed October 10, 2021. https://fundingawards.nihr.ac.uk/award/NIHR131118
- 33.Jaul E, Barron J, Rosenzweig JP, Menczel J. An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr. 2018;18(1):305. doi: 10.1186/s12877-018-0997-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anders J, Heinemann A, Leffmann C, Leutenegger M, Pröfener F, von Renteln-Kruse W. Decubitus Ulcers. Dtsch Arztebl Int. 2010;107(21):371-382. doi: 10.3238/arztebl.2010.0371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beeckman D, Schoonhoven L, Fletcher J, et al. EPUAP classification system for pressure ulcers: European reliability study. J Adv Nurs. 2007;60(6):682-691. doi: 10.1111/j.1365-2648.2007.04474.x. [DOI] [PubMed] [Google Scholar]
- 36.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy. Spine. 2015;40(12):E675-E693. doi: 10.1097/BRS.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 37.Jabbour P, Fehlings M, Vaccaro AR, Harrop JS. Traumatic spine injuries in the geriatric population. Neurosurg Focus. 2008;25(5):E16. doi: 10.3171/FOC.2008.25.11.E16. [DOI] [PubMed] [Google Scholar]
- 38.Sparke A, Voss S, Benger J. The measurement of tissue interface pressures and changes in jugular venous parameters associated with cervical immobilisation devices: A systematic review. Scand J Trauma Resuscitation Emerg Med. 2013;21:81. doi: 10.1186/1757-7241-21-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Powers J. A multidisciplinary approach to occipital pressure ulcers related to cervical collars. J Nurs Care Qual. 1997;12(1):46-52. [DOI] [PubMed] [Google Scholar]
- 40.Guide to Wearing Your Cervical Hard Collar . Hull University Teaching Hospitals NHS Trust. 2021. https://www.hey.nhs.uk/patient-leaflet/guide-wearing-cervical-hard-collar/ Accessed October 10, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.