Abstract
Study Design:
Prospective cohort.
Objective:
To prospectively evaluate PROs up to 5-years after complex ASD surgery.
Methods:
The Scoli-RISK-1 study enrolled 272 ASD patients undergoing surgery from 15 centers. Inclusion criteria was Cobb angle of >80°, corrective osteotomy for congenital or revision deformity, and/or 3-column osteotomy. The following PROs were measured prospectively at intervals up to 5-years postoperative: ODI, SF36-PCS/MCS, SRS-22, NRS back/leg. Among patients with 5-year follow-up, comparisons were made from both baseline and 2-years postoperative to 5-years postoperative. PROs were analyzed using mixed models for repeated measures.
Results:
Seventy-seven patients (28.3%) had 5-year follow-up data. Comparing baseline to 5-year data among these 77 patients, significant improvement was seen in all PROs: ODI (45.2 vs. 29.3, P < 0.001), SF36-PCS (31.5 vs. 38.8, P < 0.001), SF36-MCS (44.9 vs. 49.1, P = 0.009), SRS-22-total (2.78 vs. 3.61, P < 0.001), NRS-back pain (5.70 vs. 2.95, P < 0.001) and NRS leg pain (3.64 vs. 2.62, P = 0.017). In the 2 to 5-year follow-up period, no significant changes were seen in any PROs. The percentage of patients achieving MCID from baseline to 5-years were: ODI (62.0%) and the SRS-22r domains of function (70.4%), pain (63.0%), mental health (37.5%), self-image (60.3%), and total (60.3%). Surprisingly, mean values (P > 0.05) and proportion achieving MCID did not differ significantly in patients with major surgery-related complications compared to those without.
Conclusions:
After complex ASD surgery, significant improvement in PROs were seen at 5-years postoperative in ODI, SF36-PCS/MCS, SRS-22r, and NRS-back/leg pain. No significant changes in PROs occurred during the 2 to 5-year postoperative period. Those with major surgery-related complications had similar PROs and proportion of patients achieving MCID as those without these complications.
Keywords: adult spinal deformity, patient reported outcomes, deformity, spinal deformity surgery, adult idiopathic scoliosis
Introduction
Adult spinal deformity (ASD) impedes the ability to perform activities of daily living and maintain an acceptable quality of life. Surgical intervention has been shown to correct spinal alignment and provide durable improvement in several patient-reported outcomes (PROs).1,2 While ASD outcomes at 2 years are commonly reported, less is known about outcomes in this surgical population beyond this time point.
The Scoli-Risk-1 study was a prospective, international, multicenter, observational study assessing neurologic and non-neurologic complications in patients undergoing surgical correction of complex spinal deformities. 3 Patient-reported outcomes (PROs) were an equally important measure obtained prospectively in this study to assess post-surgical success and provide insight into the patient’s opinion of their own quality of life, function, disability, pain, and satisfaction. 4 Postoperative changes in PROs can be evaluated with statistical significance or a minimum clinically important difference (MCID) analysis. Understanding the long-term nature of PROs after complex ASD surgery may allow surgeons to better educate patients preoperatively and assist in the discussion of the value equation of these type of spinal reconstructions.
We sought to further study long-term PROs in the prospective Scoli-Risk-1 study at 5-years postoperative. The current objectives were to: 1) report 5-year PROs, 2) conduct an MCID analysis of 5-year PROs, and 3) determine the impact of major surgery-related complications on 5-year PROs.
Methods
Study Design and Patient Population
The Scoli-RISK-1 study was a prospective, international, multicenter, observational study evaluating neurologic complications following surgical correction of complex ASD. Inclusion criteria were: ages 18-80 years, deformity apex between C7-L2, major sagittal/coronal Cobb angle ≥80°, congenital or revision deformity undergoing corrective spinal osteotomy, patient undergoing three-column spinal osteotomy (3CO) (i.e. pedicle subtraction osteotomy or vertebral column resection) from C7 to L5, reconstruction or decompression for preoperative myelopathy secondary to their deformity, or reconstruction or decompression due to deformity and ossification of the ligamentum flavum or posterior longitudinal ligament. Exclusion criteria were: unlikely to comply with follow-up, substance dependency or psychiatric disturbance in ≤ 3 from operation, active malignancy/infection, spinal trauma/injury/fracture/malignancy in ≤ 3 months from operation, long-term paraplegia, pregnancy, or those incarcerated/instituitnalized. 5
Fifteen international centers enrolled patients—North America (9), Europe (3), and Asia (3)—and all centers obtained institutional review board approval. Forty-three experienced spinal deformity surgeons participated. Decisions about surgical approach, instrumentation, corrective maneuvers, and use of bone grafts or substitutes were at the discretion of the primary surgeon. The study was registered with ClinicalTrials.gov (NCT01305343). Institutional Review Board (IRB) approval was received at each respective institution (protocol number AAAR2375 for the lead author’s institution) and informed consent was obtained from every participant. Funding for the Scoli-Risk-1 study was obtained from AOSpine, the Scoliosis Research Society, and Norton Healthcare, although no funding was used in this secondary analysis.
Data Collection
Basic demographic and surgical data were collected, including but not limited to comorbidities, prior spine procedures, surgical indication, levels fused, operative time, estimated blood loss (EBL), osteotomies, 3CO performed, and radiographic measurements. All patients had an ASIA-certified neurologic exam at all follow-up time points.
PRO data was collected before surgery and postoperatively at 6-weeks, 6-months, 1-year, 2-years, and 5-years. Given emphasis on 5-year outcomes data, preoperative values were compared to 5-year PRO information. PROs included: Numerical Rating Scale for back/leg pain (NRS-back/leg pain), Oswestry Disability Index (ODI) version 2.1a,6,7 Short Form-36 v2 Physical and Mental Component Score (SF36-PCS/MCS),8,9 and Scoliosis Research Society (SRS-22r) Instrument. 10 Complications were categorized in accordance with prior studies as major vs. minor, and surgery-related or not surgery-related. 11 Classifications were made by a panel of experts involved in the study, and discrepancies were resolved by 2 authors (LGL/SLZ).
Statistical Analysis
Descriptive statistics were used to summarize patients’ demographics and surgery details. Categorical data was presented using frequencies and percentages, continuous data was presented with mean, standard deviations (SD) and range for normally distributed data, or median and range for non-normally distributed data. Change of PROs over follow-up were analyzed using mixed models for repeated measures (MMRM) with an unstructured covariance. The number and proportion of patients improving from baseline to 5-year follow-up by at least the minimum clinically important difference (MCID) were calculated for ODI and SRS-22r. MCID threshold values were set in accordance with prior studies: −12.8 for ODI, +0.587 for SRS-pain, 0.375 for SRS-activity, +0.800 for SRS-appearance, +0.420 for SRS-mental, and +0.710 for SRS-total.12-16 The impact of major surgery-related complications on ODI and SRS-22r were assessed by comparing mean values derived by MMRM analyses. The proportion of patients achieving MCID for PROs at 5-years was compared for patients with and without any major surgery-related complication using Chi-Square tests. Two-sided P values below 0.05 were considered statistically significant. All statistical analyses were performed using SAS (version 9.4, SAS Institute Inc., Cary, NC, US).
Results
Demographic and Operative Data
A total of 77 (28.3%) patients had 5-year follow-up (Table 1). The mean age was 57.8 years with 80.5% female and 64.9% Caucasian. Smoking among these patients was rare (5.2%) and the majority of patients had previous spine surgery (57.1%). A significant majority underwent 3CO (74.0%) and had posterior only surgery (77.9%). Median number of level involved in surgery was 10 (range 9 to 14). Due to the follow-up rate, a sensitivity analysis compared the 77 patients with 5-year follow-up to the 195 patients without 5-year follow-up (Supplementary Tables 1-4.) The only significant differences between those with and without 5-year follow-up were gender (more females in the 5-year group), race (less Caucasians in the 5-year group), comorbidities (more comorbidities in the 5-year group), with no differences in surgical details or adverse events.
Table 1.
Demographics of Patient Sample.
| N = 77 | |
|---|---|
| Age, mean (SD); range | 57.8 (15.5); 19.0–80.0 |
| Female, n (%) | 62 (80.5) |
| Race, n (%) | |
| White | 50 (64.9) |
| East Asian | 26 (33.8) |
| Other | 1 (1.3) |
| Smoker, n (%) | 4 (5.2) |
| BMI, mean (SD); range | 26.4 (5.7); 17.0–39.7 |
| Previous spine surgery, n (%) | 44 (57.1) |
| Preoperative neuro deficit, n (%) | 20 (26.0) |
| Number of documented comorbidities, median; range | 2; 0–12 |
| Operative time in minutes*, mean (SD); range | 426 (149); 159–1023 |
| Total estimated blood loss in ml*, median; range | 2026; 250–12 000 |
| Three-column osteotomy, n (%) | 57 (74.0) |
| Surgical approach, n (%) | |
| Posterior only | 60 (77.9) |
| Anterior-posterior combined | 17 (22.1) |
| Levels involved in surgery, median; range | 10; 9–14 |
| ASA Grade**, n (%) | |
| I | 2 (2.6) |
| II | 44 (57.1) |
| III | 31 (40.3) |
* for staged procedures the sum over the stages was calculated.
** for staged procedures worst ASA grade was used.
Patient-Reported Outcomes
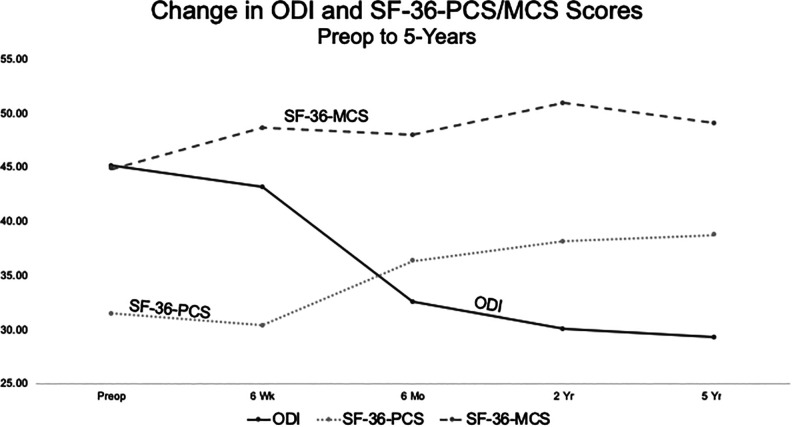
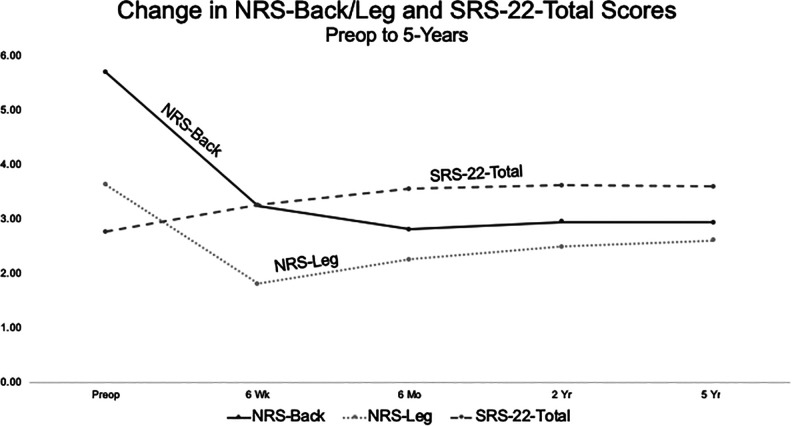
Mean values for NRS-back/leg, ODI, and SF36-PCS/MCS are seen (Table 2). Comparing baseline to 5-year data, significant improvement was seen in NRS-back pain, NRS-leg pain, ODI, and SF36-PCS/MCS. During the 2 to 5-year period, no significant changes were seen in any PROs, indicating stability over this mid to long-term follow-up period. Additionally, significant improvement from baseline to 5-years was observed for the SRS-22r total mean score and individual mean domain scores (Table 3). Similarly, no significant changes were seen during the 2 to 5-year period. Graphical summary of all mean PROs at each time point is seen in Figures 1 and 2.
Table 2.
NRS-Back/Leg Pain, ODI, SF36-PCS/MCS in Patients With 5-Year Follow-Up; Results From Mixed Effects Model for Repeated Measurements (Patients Who Participated in Extension Study, Including Unpunctual Assessments).
| Outcome | Visit | n | Mean (95% CI) | Change from baseline (95%CI) | P value | Change from 2 to 5-years (95%CI) | P value |
|---|---|---|---|---|---|---|---|
| NRS-back pain | Enrollment | 75 | 5.70 (5.04; 6.36) | ||||
| 6 weeks | 75 | 3.25 (2.69; 3.80) | −2.45 (−3.07; −1.83) | <.001 | |||
| 6 months | 76 | 2.82 (2.24; 3.41) | −2.87 (−3.55; −2.19) | <.001 | |||
| 24 months | 73 | 2.96 (2.30; 3.62) | −2.74 (−3.49; −1.99) | <.001 | |||
| 5 years | 75 | 2.95 (2.33; 3.57) | −2.75 (−3.48; −2.02) | <.001 | −0.01 (−0.63; 0.61) | 0.977 | |
| NRS-leg pain | Enrollment | 73 | 3.64 (2.85; 4.42) | ||||
| 6 weeks | 73 | 1.82 (1.29; 2.34) | −1.82 (−2.55; −1.10) | <.001 | |||
| 6 months | 76 | 2.26 (1.64; 2.89) | −1.38 (−2.20; −0.55) | 0.001 | |||
| 24 months | 73 | 2.50 (1.80; 3.20) | −1.14 (−1.99; −0.28) | 0.010 | |||
| 5 years | 74 | 2.62 (2.00; 3.24) | −1.02 (−1.84; −0.19) | 0.017 | 0.12 (−0.59; 0.83) | 0.737 | |
| Oswestry Disability Index (ODI) | Enrollment | 75 | 45.2 (40.1; 50.3) | ||||
| 6 weeks | 69 | 43.2 (38.9; 47.5) | −2.0 (−7.3; 3.3) | 0.456 | |||
| 6 months | 74 | 32.6 (28.6; 36.6) | −12.6 (−17.1; −8.1) | <.001 | |||
| 24 months | 74 | 30.1 (25.3; 34.9) | −15.1 (−19.5; −10.8) | <.001 | |||
| 5 years | 73 | 29.3 (24.2; 34.3) | −15.9 (−20.7; −11.2) | <.001 | −0.8 (−4.4; 2.8) | 0.659 | |
| SF36-Physical Component Summary (PCS) | Enrollment | 72 | 31.5 (29.1; 34.0) | ||||
| 6 weeks | 69 | 30.4 (28.4; 32.3) | −1.2 (−4.0; 1.7) | 0.419 | |||
| 6 months | 76 | 36.4 (34.6; 38.1) | 4.8 (2.4; 7.3) | <.001 | |||
| 24 months | 72 | 38.2 (35.8; 40.7) | 6.7 (3.9; 9.5) | <.001 | |||
| 5 years | 70 | 38.8 (36.4; 41.2) | 7.2 (4.2; 10.3) | <.001 | 0.5 (−1.7; 2.8) | 0.638 | |
| SF36-Mental Component Summary (MCS) | Enrollment | 72 | 44.9 (41.8; 47.9) | ||||
| 6 weeks | 69 | 48.7 (45.6; 51.7) | 3.8 (0.3; 7.3) | 0.034 | |||
| 6 months | 76 | 48.0 (45.0; 51.0) | 3.2 (0.1; 6.2) | 0.040 | |||
| 24 months | 72 | 51.0 (48.0; 53.9) | 6.1 (3.1; 9.1) | <.001 | |||
| 5 years | 70 | 49.1 (46.3; 52.0) | 4.3 (1.1; 7.4) | 0.009 | −1.8 (−4.5; 0.9) | 0.183 |
Table 3.
SRS-22r in Patients With 5-Year Follow-Up; Results From Mixed Effects MODEL for Repeated Measurements (Patients Who Participated in Extension Study, Including Unpunctual Assessments).
| Outcome | Visit | n | Mean (95% CI) | Change from baseline (95%CI) | P value | Change from 2 to 5-years (95%CI) | P value |
|---|---|---|---|---|---|---|---|
| SRS-22-Total | Enrollment | 61 | 2.78 (2.64; 2.93) | ||||
| 6 weeks | 73 | 3.26 (3.14; 3.38) | 0.48 (0.35; 0.60) | <.001 | |||
| 6 months | 76 | 3.56 (3.42; 3.70) | 0.78 (0.62; 0.93) | <.001 | |||
| 24 months | 74 | 3.63 (3.47; 3.79) | 0.85 (0.67; 1.02) | <.001 | |||
| 5 years | 74 | 3.61 (3.45; 3.77) | 0.82 (0.66; 0.98) | <.001 | −0.02 (−0.15; 0.10) | 0.731 | |
| SRS-22-Function | Enrollment | 74 | 2.71 (2.51; 2.91) | ||||
| 6 weeks | 74 | 2.53 (2.37; 2.69) | −0.18 (−0.38; 0.03) | 0.093 | |||
| 6 months | 77 | 3.05 (2.84; 3.25) | 0.34 (0.12; 0.55) | 0.002 | |||
| 24 months | 74 | 3.40 (3.18; 3.61) | 0.69 (0.48; 0.90) | <.001 | |||
| 5 years | 74 | 3.42 (3.21; 3.62) | 0.71 (0.49; 0.92) | <.001 | 0.02 (−0.13; 0.16) | 0.793 | |
| SRS-22-Pain | Enrollment | 75 | 2.52 (2.28; 2.76) | ||||
| 6 weeks | 74 | 2.75 (2.52; 2.99) | 0.23 (0.03; 0.44) | 0.028 | |||
| 6 months | 77 | 3.38 (3.17; 3.60) | 0.86 (0.64; 1.09) | <.001 | |||
| 24 months | 74 | 3.48 (3.25; 3.71) | 0.96 (0.70; 1.22) | <.001 | |||
| 5 years | 75 | 3.47 (3.24; 3.70) | 0.95 (0.70; 1.21) | <.001 | −0.01 (−0.20; 0.19) | 0.944 | |
| SRS-22-Mental Health | Enrollment | 74 | 3.54 (3.34; 3.74) | ||||
| 6 weeks | 73 | 3.63 (3.43; 3.84) | 0.09 (−0.10; 0.28) | 0.329 | |||
| 6 months | 77 | 3.78 (3.59; 3.96) | 0.23 (0.05; 0.42) | 0.014 | |||
| 24 months | 74 | 3.84 (3.64; 4.03) | 0.29 (0.10; 0.48) | 0.003 | |||
| 5 years | 75 | 3.86 (3.66; 4.05) | 0.31 (0.11; 0.52) | 0.003 | 0.02 (−0.15; 0.19) | 0.816 | |
| SRS-22-Appearance | Enrollment | 75 | 2.35 (2.18; 2.51) | ||||
| 6 weeks | 74 | 3.71 (3.55; 3.86) | 1.36 (1.17; 1.55) | <.001 | |||
| 6 months | 77 | 3.71 (3.54; 3.88) | 1.37 (1.15; 1.58) | <.001 | |||
| 24 months | 74 | 3.64 (3.44; 3.85) | 1.30 (1.06; 1.53) | <.001 | |||
| 5 years | 75 | 3.45 (3.25; 3.65) | 1.10 (0.90; 1.31) | <.001 | −0.19 (−0.40; 0.02) | 0.071 | |
| SRS-22-Satisfaction | Enrollment | 61 | 3.09 (2.80; 3.39) | ||||
| 6 weeks | 73 | 4.27 (4.09; 4.45) | 1.18 (0.84; 1.52) | <.001 | |||
| 6 months | 76 | 4.20 (4.01; 4.39) | 1.11 (0.76; 1.46) | <.001 | |||
| 24 months | 74 | 4.05 (3.82; 4.27) | 0.96 (0.56; 1.36) | <.001 | |||
| 5 years | 75 | 4.07 (3.85; 4.28) | 0.98 (0.62; 1.33) | <.001 | 0.02 (−0.18; 0.22) | 0.856 |
Figure 1.
Mean ODI and SF36-PCS/MCS scores from preoperative to 5-years postoperatively.
Figure 2.
Mean NRS-back/leg pain and SRS-22r total from preoperative to 5-years postoperatively.
MCID Analysis
For ODI and SRS-22r, an MCID analysis was conducted (Table 4). The majority of patients achieved MCID at 5-years in all categories, except for SRS-mental health, with 37.5% of patients achieving an MCID.
Table 4.
Patients Meeting Minimum Clinical Important Difference (MCID) Between Baseline and 5 Years for ODI and SRS-Subscales.
| Variable | N = 77 |
|---|---|
| ODI Δ from preop to 5yr ≥ MCID, n (%) | 71 |
| No | 27 (38.0) |
| Yes | 44 (62.0) |
| SRS-22-function Δ from preop to 5yr ≥ MCID, n (%) | 71 |
| No | 21 (29.6) |
| Yes | 50 (70.4) |
| SRS-22-pain Δ from preop to 5yr ≥ MCID, n (%) | 73 |
| No | 27 (37.0) |
| Yes | 46 (63.0) |
| SRS-22-mental health Δ from preop to 5yr ≥ MCID, n (%) | 72 |
| No | 45 (62.5) |
| Yes | 27 (37.5) |
| SRS-22-self-image Δ from preop to 5yr ≥ MCID, n (%) | 73 |
| No | 29 (39.7) |
| Yes | 44 (60.3) |
| SRS-22-total Δ from preop to 5yr ≥ MCID, n (%) | |
| No | 23 (39.7) |
| Yes | 35 (60.3) |
Impact of Complications
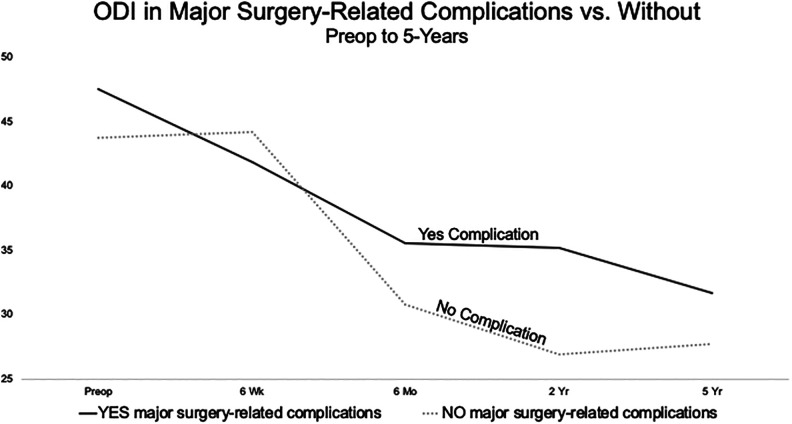
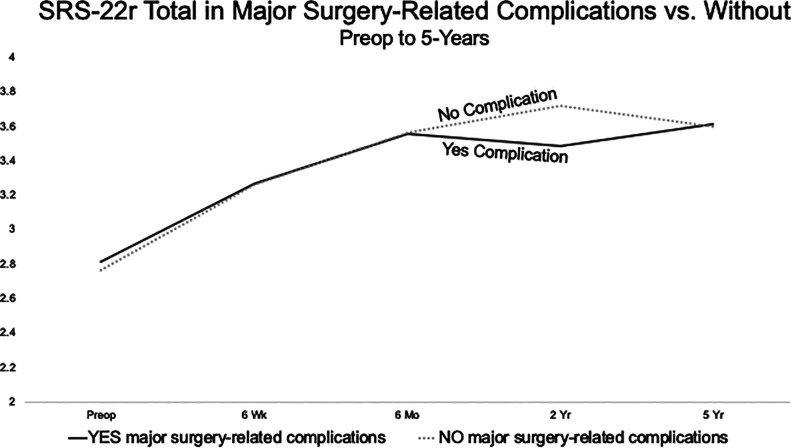
Patients with major surgery-related complication (N = 30) were compared to those without major surgery-related complications (N = 47), for ODI and SRS-22r. Using mean values, no significant difference was seen between both groups at each follow-up time point and 5-years for ODI (27.7 for patients with major surgery-related complications versus 31.7 for patients without P = 0.448) (Figure 3) and SRS-22r-total (3.62 versus 3.62, P = 0.937) (Figure 4). Comparing the proportion of patients that achieved an MCID with and without major surgery-related complications, surprisingly, no significant differences were seen (Table 5).
Figure 3.
Mean ODI in patients with major surgery-related complications compared to those without from preoperative to 5-years postoperatively.
Figure 4.
Mean SRS-22r total score in patients with major surgery-related complications compared to those without from preoperative to 5-years postoperatively.
Table 5.
Patients Meeting Minimum Clinical Important Difference (MCID) With Major Surgery-Related Complication Versus Those Without, Between Baseline and 5 Years for ODI and SRS-22.
| Variable | YES Major Surgery-Related Complication* | NO Major Surgery-Related Complication | P-value |
|---|---|---|---|
| N = 30 | N = 47 | ||
| ODI Δ from preop to 5yr ≥MCID, n (%) | 27 | 44 | 0.253† |
| No | 8 (29.6) | 19 (43.2) | |
| Yes | 19 (70.4) | 25 (56.8) | |
| SRS-22-function Δ from preop to 5yr ≥ MCID, n (%) | 28 | 43 | 0.225† |
| No | 6 (21.4) | 15 (34.9) | |
| Yes | 22 (78.6) | 28 (65.1) | |
| SRS-22-pain Δ from preop to 5yr ≥ MCID, n (%) | 29 | 44 | 0.392† |
| No | 9 (31.0) | 18 (40.9) | |
| Yes | 20 (69.0) | 26 (59.1) | |
| SRS-22-mental health Δ from preop to 5yr ≥ MCID, n (%) | 28 | 44 | 0.803† |
| No | 17 (60.7) | 28 (63.6) | |
| Yes | 11 (39.3) | 16 (36.4) | |
| SRS-22-self-image Δ from preop to 5yr ≥ MCID, n (%) | 29 | 44 | 0.799† |
| No | 11 (37.9) | 18 (40.9) | |
| Yes | 18 (62.1) | 26 (59.1) | |
| SRS-22-total Δ from preop to 5yr ≥ MCID, n (%) | 24 | 34 | 0.778† |
| No | 9 (37.5) | 14 (41.2) | |
| Yes | 15 (62.5) | 20 (58.8) |
* Any major surgery-related complication with onset before SRS-22 completion at 5 years FU.
†Chi-Square test.
Discussion
Given both the importance and shortage of long-term outcomes after complex ASD surgery, we prospectively evaluated PROs 5-years after ASD surgery. From baseline to 5-years postoperative, nearly all PROs significantly improved. In the 2 to 5-year period, no significant changes in any PROs occurred. Surprisingly, and importantly, the impact of a major surgery-related complication did not significantly alter either the absolute PRO values or the proportion achieving MCID. Despite the challenges of patients being lost to follow-up, these results represent rare 5-year outcomes of prospectively accrued data after complex ASD surgery.
Patient-Reported Outcomes at 5-Years
While 5-year outcome data after ASD surgery is sparse, 5-year PRO data is even rarer. 17 Significant improvement was seen in all PROs from preoperative to 5-years. Kryola et al. 18 retrospectively evaluated 79 ASD patients from a single institution and found that ODI and visual analog (VAS) back/leg pain were significantly improved at 4-5 years compared to baseline. In 541 ASD patients, Terran et al. 19 retrospectively showed improvement in preoperative to 5-year ODI (38.7 vs. 22.3), although their average preoperative ODI was lower than our value of 45.2, signifying less preoperative disability.
With respect to changes occurring during the follow-up period, Bridwell et al. 20 reported minimal changes in SRS (3.89 to 3.88) and ODI (19 to 18) during the 2 to 5-year follow-up period. A second study of 118 patients also showed that 2-year PRO accurately predicted 5-year PRO data, though inclusion criteria was undergoing ≥5 level fusion, which may not represent a true complex ASD population. Jain et al. 21 found 1-year PROs predicted 3-year PROs, and the greatest improvements occurred between 6 weeks and 1-year. These studies confirm our findings that little meaningful PRO change occurs from 2 to 5-years.
Though patients significantly improved in NRS-leg pain, the magnitude was only half that of back pain. Especially with a small sample size, providing clinical context to significant findings is important, and the smaller magnitude of improvement in NRS-leg has several potential explanations. Interestingly, an earlier study of 113 ASD patients found a similar phenomenon, that NRS-leg pain worsened slightly from 2 to 3-5-year follow-up (1.45 to 1.81). 20 Our population, along with the prior study, represents a back-pain dominated population, with mean preoperative NRS-back pain score of 5.70 compared to NRS-leg pain score of 3.64. LEGACY measures can be susceptible to floor/ceiling effects, where improvement cannot be measured due to an already high/low starting point.22,23 The current baseline NRS-leg pain score of 3.64 is similar to the earlier study of 3.35, both of which leave little room for improvement. 20 Despite achieving statistical significance, it is possible that similar studies may not obtain significance, which would not be surprising. Alternative explanations for worsening leg pain may be from spine-related conditions, such as worsening central or foraminal stenosis, or unrelated conditions, such as degenerative hip or knee arthritis, neuropathy, or inflammatory conditions. A previous Scoli-Risk-1 publication reported that at 5-years, 20 of 44 non-surgery-related adverse events were musculoskeletal and non-spine in nature, with 5 hip/knee joint replacement performed and 2 orthopedic trauma surgeries performed. 24
MCID Analysis
While MCID analyses have gained favor in the spinal deformity literature, long-term MCID outcomes are lacking. Except for SRS-22-mental health scores, approximately two-thirds of patients achieved MCID (range 60.3% to 70.4%). The most successful domain was in the SRS-22-function domain, with 70.4% achieving MCID. An additional prospective study of lumbar scoliosis comparing operative to nonoperative treatment found more operative patients achieved MCID in SRS-22 (85.7% vs. 38.7%; P < 0.001) and ODI (77.4% vs. 38.3%; P < 0.001), though outcomes halted at 2-years. Furthermore, a retrospective analysis of 240 ASD patients reported that 60% achieved MCID for ODI, though outcomes were also only up to 2-years postoperatively and ASD definitions were less restrictive than ours. 25
Prior studies have suggested that patients undergoing more complex surgeries may have lower rates of achieving MCID. In 94 patients undergoing deformity surgery with a PSO, 62.3% achieved an MCID in SRS-22-pain, yet only 26.5% of patients achieved MCID in ODI. 26 Nearly 3 in 4 patients in our sample underwent a 3CO, and except for SRS-22 mental health, all patients achieved 60% or greater MCID. The low rate of MCID change in SRS-22 mental health has been seen in prior studies, 27 likely due to the higher than average starting point of the mental health domain (3.54) compared to domains of pain, function, appearance, and satisfaction (all under 3.0). Similarly in the present analysis, our baseline mental health score was 3.6 resembling the baseline values of the earlier study 27 likely representing a high baseline starting point and ceiling effect.22,23 Alternatively, the high mental health score may also represent a clustering effect of the disease state and disability. The low MCID percentage for SRS-22-mental health scores may have been due to the high baseline score of 3.54, leaving less room for improvement, compared to the other domains that were mostly under 3.00, except SRS-satisfaction (3.09). Moreover, the elevated scores in this domain could be associated with the design of the study, as the exclusion criteria included any recent substance dependency or psychological disturbance. Overall, to our knowledge, there are very few studies reporting MCID outcomes at 5-years postoperatively after complex ASD surgery.
Impact of Complications
The current results showed little variation in PROs—both mean values and MCID analysis—in those with major surgery-related complications compared to those without. Due to a limited sample size, we must be judicious and not equate a lack of significance with equivalent outcomes. That said, more patients reached MCID in the complication group in 3 out of 6 outcome domains in ODI, SRS-22-function, SRS-22-total), and <10% difference was see in SRS-22-pain, further emphasizing similar outcomes regardless of complications, and our results are consistent with prior reports in the literature. In a study of 126 patients undergoing 3CO with 5-year follow-up, O’Neill and colleagues 28 found that although 36% had major surgical complications, 5-year ODI and SRS scores were similar between those with and without major surgical complications, predicated that the complication was adequately treated. A single institution cohort of 41 patients undergoing ASD surgery with prophylactic vertebroplasty at both the UIV and UIV+1 found that at 5-years, no significant differences in SRS-22, ODI, or SF36 scores between the PJK and non-PJK group were seen. Similarly, Kim et al. 29 found that SRS outcome scores did not differ in patients with PJK vs. without except for the self-image domain when PJK exceeded 20°. Additional studies have showed limited impact on perioperative complications after ASD surgery, 30 yet these were not restricted to major surgery-related complications. Conversely, some prior reports have shown the opposite. In a study of 134 ASD patients followed to 5-years, Falloon and colleagues 31 found that unplanned reoperation negatively impacted ODI and SRS-22-pain/function/satisfaction/total scores. Moreover, Bridwell et al. 20 reported that ODI and SRS were significantly worse in 9 of 113 ASD patients with complications. It is possible that our results showed a more favorable impact of major surgery-related complications because the long-term follow-up allowed ample time to recover. Alternatively, the number of patients lost to follow-up may represent a skewed sample of patients happier with their care. 32
Strengths and Limitations
The prospective and long-term nature of the current study represent 2 important strengths. While many multicenter studies of ASD surgery exist from large, collaborative registries,33-35 the majority of these studies are retrospective. Furthermore, the threshold for complex ASD surgery is defined differently throughout the literature, yet our current inclusion was fairly strict, evidenced by nearly 3 in 4 patients undergoing 3CO. Other studies define ASD as a Cobb angle of ≥20º, SVA ≥5 cm, pelvic tilt ≥25º, and minimum ODI ≥30,35,36 compared to the Scoli-Risk-1 inclusion criteria of Cobb angle ≥80º, among others. 5 Moreover, having 5-year outcomes is unique. While many other impactful ASD studies have led to important findings and accurate predictive scores, follow-up is limited to 2-years postoperative,13,36 which may potentially miss important long-term changes. We also analyzed PROs with statistical significance and an MCID analysis. With respect to MCID, some authors have suggested that when conducting MCID analyses, the minimum detectable measurement difference (MDMD) in a PRO should be considered, such that the MCID is greater than the MDMD. 37 MDMD values for the SRS-22 have been reported at 0.3 for SRS-22-activity/mental health and 0.2 SRS-22-total, which were both less than our MCID values for SRS-22r domains, which were all greater than 0.3.
Important limitations of the current manuscript must be mentioned. Despite its prospective, multicenter design, many patients were unfortunately lost to follow-up in the 2 to 5-year window. Only 28.3% of patients had data complete enough to perform the 5-year analysis. Furthermore, the less than ideal follow-up rate was likely due to the long-term nature of the study and surgeon institutional changes. The significant loss of patients speaks to the difficulty of long-term follow-up in a surgical population. It is unknown whether patients happier or less satisfied with care returned to clinic, which makes the current data vulnerable to bias. Second, significant heterogeneity existed in each patient and surgical decision-making. That said, the strict enrollment criteria promoted homogenous collection of patients undergoing the most complicated spine surgeries, offering high internal validity. Third, due to small sample sizes, we could not conduct a predictive analysis of patient and surgical factors associated with improved or worsened PROs. Previous studies have outlined valuable predictor studies of PROs, 4 and unfortunately, this was not possible in our analysis. Fourth, some authors have suggested that using the substantial clinical benefit (SCB) marker rather than MCID,26,38 and only MCID values were used here.
Conclusions
After complex ASD surgery, durable improvement in PROs were seen at 5-year follow-up in all PROs including ODI, SF36-PCS/MCS, SRS-22r, and NRS-back/leg pain. No significant changes occurred during the 2 to 5-year follow-up period. Surprisingly, those with major surgery-related complications had similar PROs and proportion achieving MCID than those without such complications, further validating the benefit of these type of spinal reconstructive procedures performed in the complex ASD patient population.
Supplemental Material
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220988276 for Patient-Reported Outcomes After Complex Adult Spinal Deformity Surgery: 5-Year Results of the Scoli-Risk-1 Study by Scott L. Zuckerman, Meghan Cerpa, Lawrence G. Lenke, Christopher I. Shaffrey, Leah Y. Carreon, Kenneth M. C. Cheung, Michael P. Kelly, Michael G. Fehlings, Christopher P. Ames, Oheneba Boachie-Adjei, Mark B. Dekutoski, Khaled M. Kabeaish, Stephen J. Lewis, Yukihiro Matsuyama, Ferran Pellisé, Yong Qiu, Frank J. Schwab, Justin S. Smith and AO Spine Knowledge Forum Deformity and SRS Scoli-RISK-1 Study Group in Global Spine Journal
Footnotes
Authors’ Note: This work has been presented at the SRS 2020 Conference.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by AO Spine through the AO Spine Knowledge Forum Deformity, the Scoliosis Research Society (SRS), and Norton Healthcare. AO Spine Knowledge Forum Deformity is a focused group of international deformity experts. AO Spine is a clinical division of the AO Foundation, which is an independent medically-guided not-for-profit organization. Study support was provided directly through the AO Spine Research Department and the AO Innovation Translation Center, Clinical Evidence.
ORCID iD: Scott L. Zuckerman, MD, MPH  https://orcid.org/0000-0003-2951-2942
https://orcid.org/0000-0003-2951-2942
Meghan Cerpa, MPH  https://orcid.org/0000-0002-5931-7067
https://orcid.org/0000-0002-5931-7067
Michael P. Kelly, MD, MS  https://orcid.org/0000-0001-6221-7406
https://orcid.org/0000-0001-6221-7406
Michael G. Fehlings, MD, PhD  https://orcid.org/0000-0002-5722-6364
https://orcid.org/0000-0002-5722-6364
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Smith JS, Shaffrey CI, Berven S, et al. Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine (Phila Pa 1976). 2009;34(16):1693–1698. [DOI] [PubMed] [Google Scholar]
- 2.Smith JS, Shaffrey E, Klineberg E, et al. Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine. 2014;21(6):994–1003. [DOI] [PubMed] [Google Scholar]
- 3.Cerpa M, Lenke LG, Fehlings MG, Shaffrey CI, Cheung KMC, Carreon LY. Evolution and advancement of adult spinal deformity research and clinical care: an overview of the Scoli-RISK-1 study. Global Spine J. 2019;9(1):8S–14S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carreon LY, Glassman SD, Shaffrey CI, et al. Predictors of health-related quality-of-life after complex adult spinal deformity surgery: a Scoli-RISK-1 secondary analysis. Spine Deform. 2017;5(2):139–144. [DOI] [PubMed] [Google Scholar]
- 5.Lenke LG, Shaffrey CI, Carreon LY, et al. Lower extremity motor function following complex adult spinal deformity surgery: two-year follow-up in the scoli-RISK-1 prospective, multicenter, international study. J Bone Joint Surg Am. 2018;100(8):656–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273. [PubMed] [Google Scholar]
- 7.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25(22):2940–2952; discussion 2952. [DOI] [PubMed] [Google Scholar]
- 8.Ware JE, Jr. SF-36 health survey update. Spine (Phila Pa 1976). 2000;25(24):3130–3139. [DOI] [PubMed] [Google Scholar]
- 9.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 10.Asher MA, Lai SM, Glattes RC, Burton DC, Alanay A, Bago J. Refinement of the SRS-22 Health-Related Quality of Life Questionnaire function domain. Spine (Phila Pa 1976). 2006;31(5):593–597. [DOI] [PubMed] [Google Scholar]
- 11.Kelly MP, Lenke LG, Shaffrey CI, et al. Evaluation of complications and neurological deficits with three-column spine reconstructions for complex spinal deformity: a retrospective Scoli-RISK-1 study. Neurosurg Focus. 2014;36(5): E17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Crawford CH, Glassman SD, Bridwell KH, Berven SH, Carreon LY. The minimum clinically important difference in SRS-22 R total score, appearance, activity and pain domains after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976). 2015;40(6):377–381. [DOI] [PubMed] [Google Scholar]
- 13.Kelly MP, Lurie JD, Yanik EL, et al. Operative versus nonoperative treatment for adult symptomatic lumbar scoliosis. J Bone Joint Surg Am. 2019;101(4):338–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu S, Diebo BG, Henry JK, et al. The benefit of nonoperative treatment for adult spinal deformity: identifying predictors for reaching a minimal clinically important difference. Spine J. 2016;16(2):210–218. [DOI] [PubMed] [Google Scholar]
- 15.Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY. Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study Questionnaire Short Form 36, and pain scales. Spine J. 2008;8(6):968–974. [DOI] [PubMed] [Google Scholar]
- 16.Yuksel S, Ayhan S, Nabiyev V, et al. Minimum clinically important difference of the health-related quality of life scales in adult spinal deformity calculated by latent class analysis: is it appropriate to use the same values for surgical and nonsurgical patients? Spine J. 2019;19(1):71–78. [DOI] [PubMed] [Google Scholar]
- 17.Ploumis A, Simpson AK, Cha TD, Herzog JP, Wood KB. Coronal spinal balance in adult spine deformity patients with long spinal fusions: a minimum 2- to 5-year follow-up study. J Spinal Disord Tech. 2015;28(9):341–347. [DOI] [PubMed] [Google Scholar]
- 18.Kyrola K, Kautiainen H, Pekkanen L, Makela P, Kiviranta I, Hakkinen A. Long-term clinical and radiographic outcomes and patient satisfaction after adult spinal deformity correction. Scand J Surg. 2019;108(4):343–351. [DOI] [PubMed] [Google Scholar]
- 19.Terran J, McHugh BJ, Fischer CR, et al. Surgical treatment for adult spinal deformity: projected cost effectiveness at 5-year follow-up. Ochsner J. 2014;14(1):14–22. [PMC free article] [PubMed] [Google Scholar]
- 20.Bridwell KH, Baldus C, Berven S, et al. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976). 2010;35(20):1849–1854. [DOI] [PubMed] [Google Scholar]
- 21.Jain A, Kebaish KM, Sciubba DM, et al. Early patient-reported outcomes predict 3-year outcomes in operatively treated patients with adult spinal deformity. World Neurosurg. 2017;102:258–262. [DOI] [PubMed] [Google Scholar]
- 22.Hung M, Stuart AR, Higgins TF, Saltzman CL, Kubiak EN. Computerized adaptive testing using the PROMIS physical function item bank reduces test burden with less ceiling effects compared with the short musculoskeletal function assessment in orthopaedic trauma patients. J Orthop Trauma. 2014;28(8):439–443. [DOI] [PubMed] [Google Scholar]
- 23.Boody BS, Bhatt S, Mazmudar AS, Hsu WK, Rothrock NE, Patel AA. Validation of patient-reported outcomes measurement information system (PROMIS) computerized adaptive tests in cervical spine surgery. J Neurosurg Spine. 2018;28(3):268–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cerpa MZSLLEa. Non-neurologic complications after complex adult spinal deformity surgery: what happens during long-term follow-up? Paper Presented at: SRS2020; Virtual. [Google Scholar]
- 25.Yoshida G, Hasegawa T, Yamato Y, et al. Minimum clinically important differences in Oswestry disability index domains and their impact on adult spinal deformity surgery. Asian Spine J. 2019;13(1):35–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fakurnejad S, Scheer JK, Lafage V, et al. The likelihood of reaching minimum clinically important difference and substantial clinical benefit at 2 years following a 3-column osteotomy: analysis of 140 patients. J Neurosurg Spine. 2015;23(3):340–348. [DOI] [PubMed] [Google Scholar]
- 27.Riley MS, Bridwell KH, Lenke LG, Dalton J, Kelly MP. Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine. 2018;28(2):194–200. [DOI] [PubMed] [Google Scholar]
- 28.O’Neill KR, Lenke LG, Bridwell KH, et al. Clinical and radiographic outcomes after 3-column osteotomies with 5-year follow-up. Spine (Phila Pa 1976). 2014;39(5):424–432. [DOI] [PubMed] [Google Scholar]
- 29.Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008;33(20):2179–2184. [DOI] [PubMed] [Google Scholar]
- 30.Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976). 2007;32(24):2764–2770. [DOI] [PubMed] [Google Scholar]
- 31.Faloon MJ, Essig D, Cho W, et al. Unplanned reoperations affect long-term outcomes in adult spinal deformity patients undergoing long fusions to the sacrum. Spine Deform. 2015;3(4):367–371. [DOI] [PubMed] [Google Scholar]
- 32.Adogwa O, Karikari IO, Elsamadicy AA, Sergesketter AR, Galan D, Bridwell KH. Correlation of 2-year SRS-22r and ODI patient-reported outcomes with 5-year patient-reported outcomes after complex spinal fusion: a 5-year single-institution study of 118 patients. J Neurosurg Spine. 2018;29(4):422–428. [DOI] [PubMed] [Google Scholar]
- 33.Agarwal N, Angriman F, Goldschmidt E, et al. Relationship between body mass index and sagittal vertical axis change as well as health-related quality of life in 564 patients after deformity surgery. J Neurosurg Spine. 2019:1–6. [DOI] [PubMed] [Google Scholar]
- 34.Takemoto M, Boissiere L, Novoa F, et al. Sagittal malalignment has a significant association with postoperative leg pain in adult spinal deformity patients. Eur Spine J. 2016;25(8):2442–2451. [DOI] [PubMed] [Google Scholar]
- 35.Pellise F, Vila-Casademunt A, Nunez-Pereira S, et al. The Adult Deformity Surgery Complexity Index (ADSCI): a valid tool to quantify the complexity of posterior adult spinal deformity surgery and predict postoperative complications. Spine J. 2018;18(2):216–225. [DOI] [PubMed] [Google Scholar]
- 36.Scheer JK, Osorio JA, Smith JS, et al. Development of a preoperative predictive model for reaching the Oswestry Disability Index minimal clinically important difference for adult spinal deformity patients. Spine Deform. 2018;6(5):593–599. [DOI] [PubMed] [Google Scholar]
- 37.Kelly MP, Kim HJ, Ames CP, et al. Minimum detectable measurement difference for health-related quality of life measures varies with age and disability in adult spinal deformity: implications for calculating minimal clinically important difference. Spine (Phila Pa 1976). 2018; 43(13): E790–E795. [DOI] [PubMed] [Google Scholar]
- 38.Carreon LY, Kelly MP, Crawford CH III, et al. SRS-22 R minimum clinically important difference and substantial clinical benefit after adult lumbar scoliosis surgery. Spine Deform. 2018;6(1):79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220988276 for Patient-Reported Outcomes After Complex Adult Spinal Deformity Surgery: 5-Year Results of the Scoli-Risk-1 Study by Scott L. Zuckerman, Meghan Cerpa, Lawrence G. Lenke, Christopher I. Shaffrey, Leah Y. Carreon, Kenneth M. C. Cheung, Michael P. Kelly, Michael G. Fehlings, Christopher P. Ames, Oheneba Boachie-Adjei, Mark B. Dekutoski, Khaled M. Kabeaish, Stephen J. Lewis, Yukihiro Matsuyama, Ferran Pellisé, Yong Qiu, Frank J. Schwab, Justin S. Smith and AO Spine Knowledge Forum Deformity and SRS Scoli-RISK-1 Study Group in Global Spine Journal