Abstract
Study Design:
Retrospective cohort study conducted at tertiary spinal trauma referral center.
Objective:
We aimed to determine if early definitive management of spine fractures in patients admitted to the Intensive Care Unit (ICU) shortens the intubation time and the length of stay (LOS), without increasing mortality.
Methods:
The medical records of all patients admitted to the ICU and submitted to surgical stabilization of spine fractures were reviewed over a 10-year period. Time to surgery, number of fractured vertebrae, degree of neurological injury, Simplified Acute Physiology Score (SAPS II), ASA score and associated trauma were evaluated. Surgeries performed on the first 72 hours after trauma were defined as “early surgeries.” Intubation time, LOS on ICU, overall LOS and mortality rate were compared between patients operated early and late.
Results:
Fifty patients were included, 21 with cervical fractures, 23 thoracic and 6 lumbar. Baseline characteristics did not differ between patients in both groups. Patients with early surgical stabilization had significantly shorter intubation time, ICU-LOS and overall LOS, with no differences in terms of mortality rate. After multivariate adjustments overall LOS was significantly shorter in patients operated earlier.
Conclusions:
Early spinal stabilization (<72 hours) of severely injured patients is beneficial and shortens the intubation time, ICU-LOS and overall LOS, with no differences in terms of mortality rate. Although some patients may require a delay in treatment due to necessary medical stabilization, every reasonable effort should be made to treat patients with unstable spinal fractures as early as possible.
Level of Evidence of the Study:
Level III.
Keywords: polytrauma, early treatment, spine fractures, timing of surgery, spinal trauma, length of stay
Introduction
Spinal injuries are reported in up to 46% of patients experiencing major trauma.1,2
Despite this high incidence of unstable spinal fractures in polytrauma patients, the optimal timing for spine surgical stabilization remains controversial. The benefits of an early surgery have to be weighed against the risks that this surgery entails in this specific population.
Most of the current literature focuses on the optimal timing of surgical intervention for acute spinal cord injury.3-5 Although improved neurologic recovery has been associated to early intervention,3-5 there is little information available regarding the effect of the timing of surgery in polytrauma patients with spinal fractures, regardless of the presence of neurologic injury.
Mechanically unstable spine fractures require bedrest until surgical intervention. This immobilization and recumbency predisposes patients to pulmonary complications, urinary tract infection, sepsis, deep venous thrombosis and immune dysfunction.6-11 Early intervention of those fractures allows patients for expeditious mobilization and may consequently reduce these complications. Furthermore, these benefits seem more pronounced in multiply injured patients in comparison to those with isolated orthopaedic injuries.3,6
On the other hand, advocates of delayed surgical treatment argue that, in the initial phase after trauma, patients with multiple injuries may be too sick to withstand the additional stress caused by a surgical intervention. This “second-hit” theory, suggests that the aggression of an early definitive surgery, combined with the initial trauma (“first-hit”), may entail an exuberant inflammatory response, leading to a higher mortality and a poorer outcome.11-13
Early surgical intervention has been accepted into the standard of care for patients with isolated long-bone fractures 14 and polytrauma patients with long-bone fractures. 15 However, the early total care (ETC) philosophy versus the damage-control orthopaedics (DCO) attitude is still a controversial topic in spine fractures.
In the present study, we sought to analyze the effect of early stabilization of spinal fractures in severely injured patients. The hypothesis for this study was that early definitive management of spine fractures in patients admitted to the Intensive Care Unit (ICU) shortens the intubation time, the length of stay (LOS) in the ICU and the overall LOS, without increasing mortality.
Methods
This study was approved by the local ethics committee and was conducted in compliance with the standards of the Declaration of Helsinki.
All patients who underwent surgical stabilization of spine fractures were retrospectively reviewed over a 10-year period (January 2007 and April 2017) in a single institution, which is a tertiary spinal trauma referral center. Our hospital has a 24 hour on-call spine surgeon to respond to urgent spine fractures and all fractures requiring surgical treatment are operated on the same day or as soon as possible, independently of the presence or absence of spinal cord injury.
From a total of 371 cases identified during the analyzed period, only the severely injured requiring organ support therapies and direct admission to an intensive care unit (ICU) were included in the study.
All selected patients were characterized in terms of age, gender, trauma mechanism, localization and number of fractured vertebrae, degree of spine cord injury (ASIA—American Spinal Injury Association Impairment Scale), 16 time to surgery, length of surgery and number of spinal segments fixed.
The Simplified Acute Physiology Score (SAPS II), the American Society of Anaesthesiologists (ASA) score, Glasgow Coma Scale (GCS), need for chest tube, need for intubation, hemoglobin and hematocrit at admission, need for transfusion and associated trauma were also analyzed. SAPS II score, 17 is a severity score and mortality estimation score for patients admitted to intensive care units that is routinely evaluated at our institution by the senior intensivist at the ICU who was blind to the patient results and surgical strategy. It consists of 17 variables (age, heart rate, systolic blood pressure, temperature, Glasgow Coma Scale, mechanical ventilation or CPAP, PaO2, FiO2, urine output, blood urea nitrogen, sodium, potassium, bicarbonate, bilirubin, white blood cell count, chronic diseases and type of admission) and its results range from 0 and 163 points, with the lowest values indicating 0% mortality and highest values indicating 100% mortality.
Time to surgery was defined as the number of hours between patient’s arrival at the emergency department and the time at which the spine surgery was initiated. Seventy-two hours was defined as the cut-off between early and late surgery. This time frame was chosen since it is the most commonly used in previous studies2,3,5,10,18,19 so that we could obtain comparable data. As such, surgeries performed in the first 72 hours after admission were defined as “early” and those occurring latter than 72 hours after trauma were defined as “late surgeries.”
The main outcomes compared between groups were intubation time, length of stay (LOS) in the ICU, overall LOS and mortality rate.
Statistical Analysis
The IBM Statistical Package for Social Sciences (SPSS), version 23, was used for statistical analysis. Descriptive statistics were calculated and Kolmogorov-Smirnov test was used for assessing normal distribution. Depending on the variable analyzed, Chi-square, Fisher’s exact test, t-test and Mann-Whitney U-test were used to compare early versus late groups.
Pearson product-moment correlation was run to determine the relationship between surgery delay and the outcomes.
Multivariate analysis (logistic regression) was performed to explore the effects of potential confounders on the outcomes measured.
All P values ≤ 0.05 were considered statistically significant. Variables included in the logistic regression model were based on clinical indication or P value < 0.05 on univariate analysis. Odds ratios and 95% confidence intervals were calculated when appropriate.
Results
Of the initial 371 cases of surgical spine fractures identified, 50 patients were severely injured and admitted to an intensive care unit (ICU) and were included in the final study.
Of these 50 patients, 40 were male and 10 were female, with a mean age of 53 ± 18 years (20-86).
In terms of anatomical distribution, 21 patients had cervical fractures, 23 thoracic and 6 lumbar, with a mean of 2 fractured vertebrae per patient. All patients with a cervical fracture were treated by an isolated anterior approach and those with thoracic and lumbar fractures were submitted to open pedicle screw instrumentation with or without decompression.
The most frequent mechanism of injury was fall from height above 3 meters (n = 26), followed by motorcycle vehicles (n = 10).
Forty nine percent of patients had some degree of spinal cord injury at admission (ASIA A-D).
Mean SAPS II score was 42 ± 12 (24-72) which translates an average predicted mortality rate of 30% at 24 h. Sixty percent of patients had an ASA IV score.
In average, patients had 2 fractured vertebrae/ spinal segments requiring surgical fixation. In 35% of patients another surgical procedure was performed at the same surgical time. Median operation time (which included those additional surgeries) was 3 hours (range: 57 to 465 minutes).
The median delay to surgery was 13 hours (range 3 to 672 hours, average 88 hours). In the “early surgery” group the median delay to surgery was 9 hours. Conversely, the “late surgery” group had a median delay to surgery of 14 days (range 78 to 672 hours, average 338 hours).
Baseline characteristics (including SAPS II and ASA scores, injured spinal region, neurologic injury and mortality rate) did not differ between patients in both groups (P > 0.05; Table 1).
Table 1.
Baseline Data in Severely Injured Patients With Different Surgical Timings.
| Early 72h | Late 72h | P value | |
|---|---|---|---|
| n = 38 | n = 12 | ||
| Male Sex | 29 (76%) | 11 (92%) | 0.416 |
| Mean Age, years (range) | 52 ± 18(28-81) | 55 ± 18(20-86) | 0.578 |
| Cervical | 17 (45%) | 4 (33%) | 0.880 |
| Thoracic | 17 (45%) | 6 (50%) | |
| Lumbar | 4 (10%) | 2 (17%) | |
| Number of segments fractured | 2.08 (1-4) | 1.42 (1-4) | 0.134 |
| Number of segments involved | 4.24 (2-8) | 3.75 (2-8) | 0.444 |
| Spinal cord injury | 20 (53%) | 4 (36%) | 0.496 |
| Chest tube | 15 (40%) | 6 (50%) | 0.658 |
| GCS ≤ 14 | 19 (50%) | 5 (42%) | 0.787 |
| Hemoglobin at admission (g/dL) | 11.7 ± 4.2 | 12.4 ± 4.7 | 0.645 |
| Hematocrit at admission (vol%) | 35.1 ± 8.8 | 35.7 ± 8.7 | 0.813 |
| Transfusion (unit) | 3.1 ± 2.2 | 2.4 ± 3 | 0.457 |
| Operating time, min | 187 ± 71 | 159 ± 111 | 0.449 |
| SAPS II score | 42 ± 14 | 36 ± 9 | 0.178 |
| ASA score III | 12 (32%) | 4 (33%) | 0.892 |
| ASA score IV | 21 (58%) | 7 (55%) | |
| Mortality Rate | 4 (11%) | 2 (17%) | 0.621 |
SAPS II Score: Simplified Acute Physiology Score; ASA: American Society of Anesthesiologists; GCS: Glasgow Coma Scale.
Twenty of the 24 patients with spinal cord injury were stabilized early, ideally within the first 6-12 hours. Patients with spinal cord injury had higher ICU-LOS (P = 0.043).
Patients submitted to early surgical stabilization had significantly shorter intubation time, shorter ICU-LOS and shorter overall LOS (Table 2), with no differences in terms of mortality rate (Table 1).
Table 2.
Outcome Parameters With Different Surgical Timings.
| Early 72h | Late 72h | P value | |
|---|---|---|---|
| n = 34* | n = 10* | ||
| Intubation time, days | 7.2 ± 6.7 | 14.2 ± 9.2 | <0.05 (0.036) |
| ICU length of stay, days | 20 ± 15.1 | 29 ± 9.6 | <0.05 (0.011) |
| Overall length of stay, days | 34 ± 15 | 60 ± 24 | <0.001 |
* Patients that died during hospital stay were not included in this analysis.
Greater advantages were seen in patients with an associated thoracic trauma (n = 34). In this subgroup patients, those treated within the first 72 h had shorter mechanical ventilation time (7,7 days versus 14,6 days in those operated after the first 72 h (P = 0.03)).
After multivariate adjustments for all baseline characteristics evaluated (Table 1) overall LOS was significantly shorter in patients operated earlier and delay to surgery significantly predicted length of stay (F (9, 23) = 5.317, P < 0.001, R2 = 0.675). There was also a strong, statistically significant, positive correlation between time to surgery and hospital stay (r = 0.594, n = 44, P < 0.001) (Figure 1).
Figure 1.
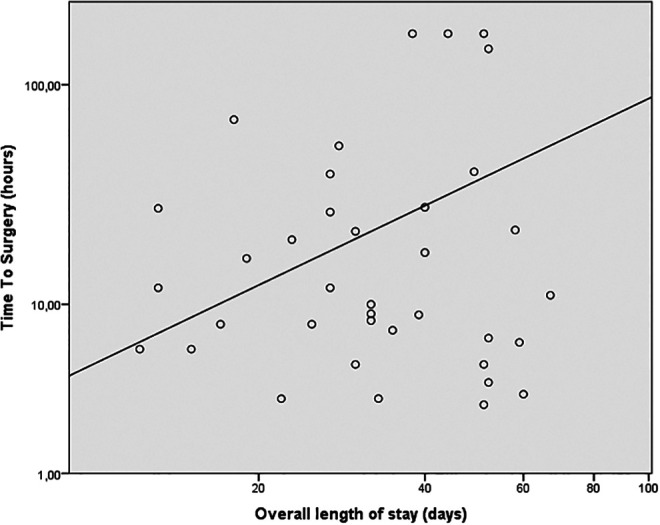
Delay to surgery correlates strongly with hospital stay (r = 0.594, n = 44, P < 0.001).
Discussion
The concept of early spine fixation for polytrauma patients without neurological deficits remains a controversial topic. Indeed, the process of decision making for spinal fractures in such specific population is complex and lacks a consensual standard of care. Polytrauma patients present a great number of associated injuries and frequently are in critical condition. These conditions make the decision about timing and type of surgical treatment very difficult, as well as how to prioritize the treatment of the numerous injuries.
Many authors in the past were advocates of delayed surgical treatment. This, as above-mentioned, would potentially render the patients more stable to then withstand the additional stress caused by a spine surgery.11-13 Nonetheless, others, as supported by this study, have clearly questioned this classic delayed philosophy.3,19-22
One of the major studies with 229 polytrauma patients that underwent early spine fixation within 72 h22 revealed that these patients had a shorter ICU, shorter overall LOS and a lower rate of respiratory complications compared to patients who underwent delayed treatment. These better outcomes were even seen in patients with associated thoracic trauma or with neurological injury. 22 These results were further confirmed by other study, 18 that reported a lower incidence of venous thrombosis, respiratory distress syndrome and overall LOS with early spine fixation. In another study analyzing only thoracic fractures, 23 the delayed surgical treatment after 72 h was also associated with an increased risk of pneumonia and also an increased need for prolonged mechanical ventilation.
Patients with thoracic fractures or with an associated thoracic trauma showed in our cohort the greatest advantages. This is very important in the decision making about these patients, because thoracic fractures are the most common fractures in polytrauma patients and thoracic trauma has major incidence in this population. 24
In a single-cohort prospective study, 25 polytrauma patients with spinal fractures were evaluated to determine whether urgent (< 24 hours) surgical stabilization of the spine fractures increased the risk compared with early (24–72 hours) treatment. They found no complications in either group, and no revisions were needed in the urgent group. They concluded that urgent stabilization is safe in polytrauma patients, particularly in the setting of neurological deficit or fracture instability.
In a recent study. 8 with data from the Trauma Registry of the German Trauma Society, it was also analyzed early (< 72 hours) versus late (> 72 hours) surgical treatment in polytrauma patients with spinal injuries. They found that early stabilization was associated with a shorter LOS, shorter ICU stay, and reduced rate of sepsis compared with those with late stabilization. In our study, patients treated within 72 hours also had shorter ICU stay (20 versus 29 days), overall LOS (34 versus 60 days) and need for mechanical ventilation (7.2 versus 14.2 days). Furthermore, patients not operated in the first 72 hours, often went through a long worsening period (lasting between 7 and 21 days in our study) before being stabilized for surgery.
In our study we found that patients with worse mean SAPS score were more likely to be treated with early stabilization (42 vs 36, although without statistical difference, P = 0.178). However, our study differs from previous reports8,25 since here, logistic regression was used in order to mitigate potential confounding factors of the independent effect of early treatment. This allowed us to conclude that early surgical stabilization is independently and significantly associated with reduced LOS. The similar results showed in other studies aforementioned, further validates our findings.
The eligibility of a polytrauma patient to early surgical treatment is largely influenced by their hemodynamic stability. While, some studies 26 have reported an increased blood loss in these patients, this was not found in our study.
There are several limitations to this study worthy of discussion. Firstly, as in most part of the studies in the literature, our population is heterogeneous with a variety of spinal injuries; various associated neurological, thoracic, and abdominal injuries; different injury severities and a mix of baseline patient health status and comorbidities. Secondly, it is a retrospective study with a relatively low population number from a single institution. Additionally, and one of the most important limitations is that patients could not be randomized in early or delayed operative groups. Nevertheless, we, unlike others, have used logistic regression to account for baseline confounders and mortality rate in order to reduce this bias. Further research should be made to identify clear and specific criteria in these severe polytrauma patients that make them candidates for early surgeries.
In conclusion, this study demonstrates that early spinal stabilization (<72 hours) of severely injured patients is beneficial and shortens the intubation time, ICU-LOS and overall LOS, with no differences in terms of mortality rate. Although some patients may require delay due to necessary medical stabilization, every reasonable effort should be made to treat patients with unstable spinal fractures as early as possible. If an early surgical treatment is feasible, severely injured patients may benefit from a shorter period of hospital stay.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Arnaldo Sousa, MD  https://orcid.org/0000-0003-1934-6821
https://orcid.org/0000-0003-1934-6821
Ricardo Rodrigues-Pinto, MD, PhD, FEBOT  https://orcid.org/0000-0002-6903-348X
https://orcid.org/0000-0002-6903-348X
References
- 1.Heyde CE, Ertel W, Kayser R. Management of spine injuries in polytraumatized patients [in German]. Orthopade. 2005;34(9):889–905. doi:10.1007/s00132-005-0847-0 [DOI] [PubMed] [Google Scholar]
- 2.Schinkel C, Frangen TM, Kmetic A, Andress HJ, Muhr G. Spinal fractures in multiply injured patients: an analysis of the German Trauma Society’s trauma register. Unfallchirurg. 2007;110(11):946–952. doi:10.1007/s00113-007-1351-2 [DOI] [PubMed] [Google Scholar]
- 3.Konieczny MR, Strüwer J, Jettkant B, et al. Early versus late surgery of thoracic spine fractures in multiple injured patients: is early stabilization always recommendable? Spine J. 2015;15(8):1713–1718. doi:10.1016/j.spinee.2013.07.469 [DOI] [PubMed] [Google Scholar]
- 4.Cengiz ŞL, Kalkan E, Bayir A, Ilik K, Basefer A.Timing of thoracolomber spine stabilization in trauma patients; impact on neurological outcome and clinical course. A real prospective (RCT) randomized controlled study. Arch Orthop Trauma Surg. 2008;128(9):959–966. doi:10.1007/s00402-007-0518 -1 [DOI] [PubMed] [Google Scholar]
- 5.Mirza SK, Krengel WF, Chapman JR, et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop Relat Res. 1999;(359):104–114. doi:10.1097/00003086-199902000-00011 [DOI] [PubMed] [Google Scholar]
- 6.Dimar JR, Carreon LY, Riina J, Schwartz DG, Harris MB. Early versus late stabilization of the spine in the polytrauma patient. Spine (Phila Pa 1976). 2010;35(21 suppl):187–192. doi:10.1097/BRS.0b013e3181f32bcd [DOI] [PubMed] [Google Scholar]
- 7.McHenry TP, Mirza SK, Wang J, et al. Risk factors for respiratory failure following operative stabilization of thoracic and lumbar spine fractures. J Bone Joint Surg Am. 2006;88(5):997–1005. doi:10.2106/JBJS.E.00560 [DOI] [PubMed] [Google Scholar]
- 8.Bliemel C, Lefering R, Buecking B, et al. Early or delayed stabilization in severely injured patients with spinal fractures? Current surgical objectivity according to the trauma registry of DGU: treatment of spine injuries in polytrauma patients. J Trauma Acute Care Surg. 2014;76(2):366–373. doi:10.1097/TA.0b013e3182aafd7a [DOI] [PubMed] [Google Scholar]
- 9.Pakzad H, Roffey DM, Knight H, Dagenais S, Yelle JD, Wai EK. Delay in operative stabilization of spine fractures in multitrauma patients without neurologic injuries: effects on outcomes. Can J Surg. 2011;54(4):270–276. doi:10.1503/cjs.008810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Boynick CP, Kurd MF, Darden BV, Vaccaro AR, Fehlings MG. Timing of surgery in thoracolumbar trauma: is early intervention safe? Neurosurg Focus. 2014;37(1):1–7. doi:10.3171/2014.5.FOCUS1473 [DOI] [PubMed] [Google Scholar]
- 11.Stahel PF, VanderHeiden T, Flierl MA, et al. The impact of a standardized “spine damage-control” protocol for unstable thoracic and lumbar spine fractures in severely injured patients: a prospective cohort study. J Trauma Acute Care Surg. 2013;74(2):590–596. doi:10.1097/TA.0b013e31827d6054 [DOI] [PubMed] [Google Scholar]
- 12.Stahel PF, Smith WR, Moore EE. Role of biological modifiers regulating the immune response after trauma. Injury. 2007;38(12):1409–1422. doi:10.1016/j.injury.2007.09.023 [DOI] [PubMed] [Google Scholar]
- 13.Schmidt OI, Gahr RH, Gosse A, Heyde CE. ATLS ® and damage control in spine trauma. World J Emerg Surg. 2009;4(1):1–11. doi:10.1186/1749-7922-4-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bone LB, Johnson KD, Weigelt J SR. Early versus delayed stabilization of femoral fractures. A prospective randomized study. J Bone Jt Surg Am. 1989;71(3):336–340. https://www.ncbi.nlm.nih.gov/pubmed/2925704 [PubMed] [Google Scholar]
- 15.Beckman SB, Scholten DJ BB. Long bone fractures in the polytrauma patient. Am Surg. 1989;55(6):356–358. [PubMed] [Google Scholar]
- 16.Roberts TT, Leonard GR, Cepela DJ. Classifications in brief: American Spinal Injury Association (ASIA) Impairment Scale. Clin Orthop Relat Res. 2017;475(5):1499–1504. doi:10.1007/s11999-016-5133-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agha A, Bein T, Fröhlich D, Höfler S, Krenz D, Jauch KW. “Simplified Acute Physiology Score” (SAPS II) in the assessment of severity of illness in surgical intensive care patients. Chirurg. 2002;73(5):439–442. doi:10.1007/s00104-001-0374-4 [DOI] [PubMed] [Google Scholar]
- 18.Croce MA, Bee TK, Pritchard E, Miller PR, Fabian TC. Does optimal timing for spine fracture fixation exist? Ann Surg. 2001;233(6):851–858. doi:10.1097/00000658-200106000-00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scaramuzzo L, Tamburrelli FC, Piervincenzi E, Raggi V, Cicconi S, Proietti L. Percutaneous pedicle screw fixation in polytrauma patients. Eur Spine J. 2013;22(suppl 6):933–938. doi:10.1007/s00586-013-3011-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kerwin AJ, Frykberg ER, Schinco MA, et al. The effect of early surgical treatment of traumatic spine injuries on patient mortality. J Trauma. 2007;63(6):1308–1313. doi:10.1097/TA.0b013e31815b8361 [DOI] [PubMed] [Google Scholar]
- 21.Lubelski D, Tharin S, Como JJ, Steinmetz MP, Vallier H, Moore T. Surgical timing for cervical and upper thoracic injuries in patients with polytrauma. J Neurosurg Spine. 2017;27(6):633–637. doi:10.3171/2017.4.SPINE16933 [DOI] [PubMed] [Google Scholar]
- 22.Kerwin AJ, Frykberg ER, Schinco MA, Griffen MM, Murphy T TJ. The effect of early spine fixation on non-neurologic outcome. J Trauma. 2005;58(1):15–21. [DOI] [PubMed] [Google Scholar]
- 23.Schinkel C, Frangen TM, Kmetic A, Andress HJ, Muhr G.Timing of thoracic spine stabilization in trauma patients: impact on clinical course and outcome. J Trauma. 2006;61(1):156–160. doi:10.1097/01.ta.0000222669.09582.ec [DOI] [PubMed] [Google Scholar]
- 24.Leucht P, Fischer K, Muhr G, Mueller EJ. Epidemiology of traumatic spine fractures. Injury. 2009;40(2):166–172. doi:10.1016/j.injury.2008.06.040 [DOI] [PubMed] [Google Scholar]
- 25.McLain RF BD. Urgent surgical stabilization of spinal fractures in polytrauma patients. Spine (Phila Pa 1976). 1999;24(16):1646–1654. [DOI] [PubMed] [Google Scholar]
- 26.Rutges JPHJ, Oner FC, Leenen LPH. Timing of thoracic and lumbar fracture fixation in spinal injuries: a systematic review of neurological and clinical outcome. Eur Spine J. 2007;16(5):579–587. doi:10.1007/s00586-006-0224-7 [DOI] [PMC free article] [PubMed] [Google Scholar]


