Abstract
Study design:
Retrospective cohort study.
Objective:
Respiratory compromise (RC) is a rare but catastrophic complication of anterior cervical spine surgery (ACSS) commonly due to compressive fluid collections or generalized soft tissue swelling in the cervical spine. Established risk factors include operative duration, size of surgical exposure, myelopathy, among others. The purpose of this current study is to identify the incidence and clinical course of patients who develop RC, and identify independent predictors of RC in patients undergoing ACSS for cervical spondylosis.
Methods:
A large, prospectively-collected registry was used to identify patients undergoing ACSS for spondylosis. Patients with posterior cervical procedures were excluded. Baseline patient characteristics were compared using bivariate analysis, and multivariate analysis was employed to compare postoperative complications and identify independent predictors of RC.
Results:
298 of 52,270 patients developed RC (incidence 0.57%). Patients who developed RC had high rates of 30-day mortality (11.7%) and morbidity (75.8%), with unplanned reoperation and pneumonia the most common. The most common reason for reoperations were hematoma evacuation and tracheostomy. Independent patient-specific factors predictive of RC included increasing patient age, male gender, comorbidities such as chronic cardiac and respiratory disease, preoperative myelopathy, prolonged operative duration, and 2-level ACCFs.
Conclusion:
This is among the largest cohorts of patients to develop RC after ACSS identified to-date and validates a range of independent predictors, many previously only described in case reports. These results are useful for taking preventive measures, identifying high risk patients for preoperative risk stratification, and for surgical co-management discussions with the anesthesiology team.
Keywords: ACDF, respiratory, complications, cervical spine, intubation
Introduction
Anterior cervical spine surgery (ACSS) including anterior cervical discectomy and fusion (ACDF), corpectomy and fusion (ACCF), and cervical disc arthroplasty (CDA) offer a robust variety of treatment options for cervical spondylosis with anterior pathology such as disc herniation and disc-osteophyte complexes. 1 ACDF remains the most commonly performed anterior-based procedure with over 100,000 cases performed in 2013, 2 and is a well-tolerated procedure with high reports of patient satisfaction and improvements in functional scores. 3 However, there are a number of rare but potentially catastrophic complications that can occur in the immediate perioperative period, including injury to the dura, vertebral artery, laryngeal nerve, esophagus, and trachea.4-7 These injuries can lead to fluid collections (hematoma, cerebrospinal fluid), generalized soft tissue swelling, and more rarely, direct injury to the phrenic nerve or instrumentation failure resulting in airway compression.8-11 As a result, patients undergoing ACSS may experience respiratory compromise (RC), manifesting as failure to wean from the ventilator postoperatively or emergent, unplanned reintubations. The reported incidence of RC ranges from 0% to 6.1%, with studies ranging from retrospective single-surgeon reports to multi-institutional studies.12-14 Numerous risk factors for RC have been previously described, for instance, Sagi et al. reported on 19 patients who developed RC and identified exposure of ≥ 3 vertebral bodies, blood loss ≥ 500 milliliters, operative duration > 5 hours, and upper cervical spine exposure as risk factors. In contrast, a case report by Emery et al. on 7 myelopathic patients who developed RC identified corpectomies, smoking history, and preoperative respiratory disease as risk factors. 8
Current literature regarding RC consists primarily of retrospective, single-institution studies that are likely underpowered given the infrequent rate at which RC occurs, and often with various studies finding contradictory predictors of RC. Larger studies utilizing national registries are also lacking as they either focus on one particular type of anterior cervical spine surgery (e.g. only ACDF) or do not fully assess the breadth of variables that may be associated with RC. The purpose of this current study is to utilize a large, national, prospectively-collected registry to identify the incidence and clinical course of patients who develop RC, as well as identify independent patient-specific and operative predictors of RC in patients undergoing ACSS for cervical spondylosis.
Methods
Data Source
This study was a retrospective cohort of prospectively collected data by the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) between 2011-8. In 2018, there were over one million unique surgical procedures collected in this registry from 722 clinical sites and consisting of over 270 variables. 15 Participating clinical sites range from community centers to academic hospitals, and procedures at these sites are randomly selected for inclusion in the registry. Patients are followed prospectively from hospital admission up to 30-days after their procedure, regardless of the date of discharge. All data is collected by trained surgical clinical reviewers that manually enter and periodically audit the data to ensure accuracy. As a result, the ACS-NSQIP has high data accuracy and inter-rater reliability,16-18 and has been used extensively in orthopedics outcomes-based research.19-22
Patient Identification
All patients who underwent ACSS were identified using Current Procedural Terminology (CPT codes). Patients who underwent a single-level ACDF were identified using CPT code 22551, and multi-level ACDF with the addition of CPT code 22552. Those who underwent single- and multi-level ACCF were identified using CPT code 63081 and 63082, and those who underwent a CDA were identified using CPT code 22856 with or without 22858 (SDC I). CDA cases were not stratified by number of levels performed due to a limited sample size with multi-level procedures. Only patients with a surgical indication of cervical spondylosis were included in this study by manually screening postoperative International Classification of Disease (ICD) Codes to identify a diagnosis of spondylosis with or without myelopathy (SDC II). Any patient who underwent a hybrid procedure (e.g. one-level ACDF and one-level CDA) were excluded. Patients who underwent any posterior cervical procedures including fusion, discectomy, un-instrumented, or instrumented fusion were excluded (Figure 1). Finally, patients with missing baseline patient-specific or operative characteristics were excluded. Anterior plate utilization was identified by using CPT code 22845-7.
Figure 1.
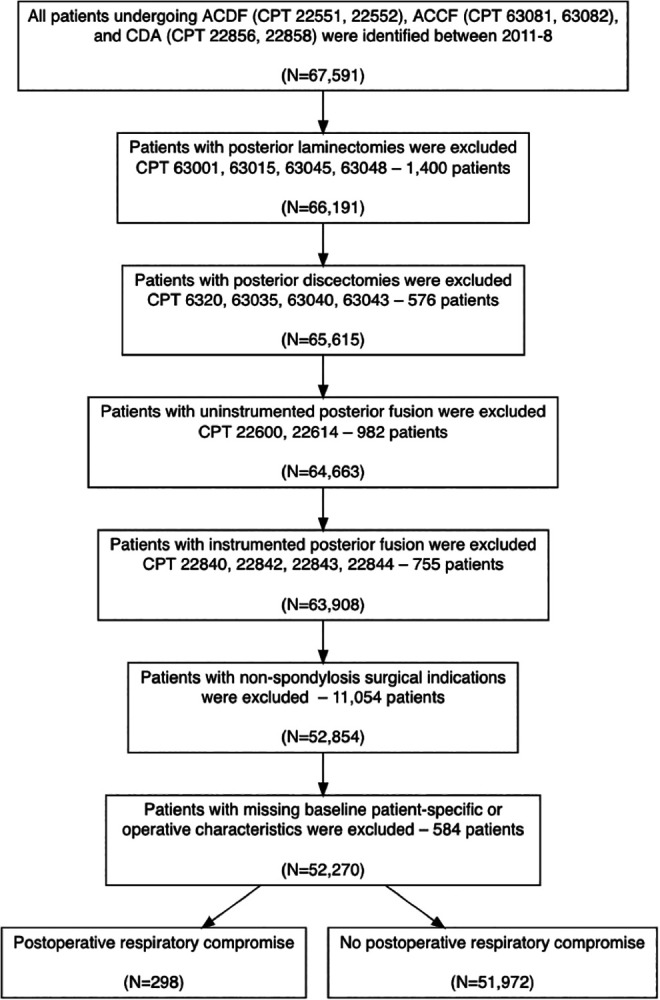
STROBE diagram of included patients. ACDF: Anterior cervical discectomy and fusion; ACCF: Anterior cervical corpectomy and fusion; CDA: Cervical disc arthroplasty.
Preoperative Characteristics and Postoperative Outcomes
RC was defined as failure to extubate from ventilator within 48 hours of surgery or emergent, unplanned reintubation within 30 days after surgery. Baseline patient-specific and operative characteristics were identified for each patient. Patient-specific characteristics included patient age, gender, ethnicity (white, black, other), body mass index (BMI, calculated from patient height and weight), medical comorbidities (hypertension, smoking history, diabetes mellitus, dyspnea, chronic obstructive pulmonary disease [COPD], preoperative corticosteroid use, bleeding disorders, congestive heart failure), baseline functional status, and a diagnosis of preoperative myelopathy. Operative characteristics included operative duration, procedure performed (ACDF [1-, 2-, and 3-levels], ACCF [1- and 2-levels], and CDA), anterior plate instrumentation, ambulatory surgery (defined as a length of stay of zero days), and American Society of Anesthesiologists (ASA) classification. Postoperative outcomes included any complication, which was an aggregate of the following complications: death, cardiac or renal complications, pneumonia, unplanned return to the operating room, deep vein thrombosis, stroke, sepsis, wound infection or dehiscence, and urinary tract infection. Additional outcome variables assessed included perioperative blood transfusions, unplanned hospital readmission, and non-home discharge.
Statistical Analysis
Statistical analysis was performed using SPSS version 25 (IBM Corp., Armonk, NY) and R version 3.6.3 (R Core Team, 2020). 23 Baseline patient-specific/operative characteristics and postoperative complications were compared using bivariate analysis. Any baseline patient-specific/operative characteristic with P < 0.200 was adjusted for in a multivariate analysis. Binary logistic multivariate models were used to compare postoperative complications and to identify independent predictors of RC. Statistical significance was defined as P < 0.050.
Results
298 patients developed RC after ACSS and 51,972 did not develop RC, with a total incidence of 0.57% (Table 1). Patients who developed RC were more likely to be older, male, non-white or non-black ethnicity, have a history of hypertension, diabetes mellitus, preoperative dyspnea or corticosteroid use (P = 0.006), COPD, bleeding disorders, and congestive heart failures. They had higher rates of preoperative myelopathy, longer operative duration, were more likely to undergo 2-level ACCFs, had higher ASA classifications, and were less likely to have had an ambulatory surgery (P < 0.001 for all comparisons, unless otherwise noted). 171 patients remained intubated >48 hours after surgery and 113 of these patients (66.1%) required subsequent reintubation after extubation. 127 patients who were extubated <48 hours after surgery also required unplanned re-intubation.
Table 1.
Comparison of Patient-Specific Characteristics by Postoperative Respiratory Complication Status.
| All patients | Postoperative respiratory complication | |||
|---|---|---|---|---|
| Yes | No | P-value | ||
| Number of patients | 52,270 | 298 | 51,972 | |
| Patient-Specific Characteristics | ||||
| Age | < 0.001 † | |||
| < 50 | 37.3% | 12.8% | 37.5% | |
| 51-60 | 32.5% | 28.5% | 32.5% | |
| 61-70 | 20.9% | 31.2% | 20.9% | |
| > 70 | 9.2% | 27.5% | 9.1% | |
| Female % | 50.1% | 34.9% | 50.2% | < 0.001 † |
| Ethnicity | < 0.001 † | |||
| White | 80.1% | 70.8% | 80.2% | |
| Black | 1.8% | 1.0% | 1.8% | |
| Other or not reported | 18.1% | 28.2% | 18.0% | |
| Body mass index (kg/m2) | 0.033 | |||
| Non-obese (< 30) | 53.9% | 53.7% | 53.9% | |
| Obese I (30-34.9) | 25.7% | 20.8% | 25.7% | |
| Obese II (35-39.9) | 12.5% | 13.8% | 12.5% | |
| Obese III (> 40) | 7.9% | 11.7% | 7.9% | |
| Comorbidities | ||||
| Hypertension | 45.3% | 71.8% | 45.1% | < 0.001 † |
| Smoking history | 27.3% | 31.5% | 27.3% | 0.102 |
| Diabetes mellitus | 16.0% | 34.2% | 15.9% | < 0.001 † |
| Dyspnea | 5.1% | 12.4% | 5.1% | < 0.001 † |
| COPD | 4.5% | 14.1% | 4.5% | < 0.001 † |
| Preoperative corticosteroid use | 3.2% | 6.0% | 3.2% | 0.006 † |
| Bleeding disorder | 1.1% | 4.4% | 1.1% | < 0.001 † |
| Congestive heart failure | 0.2% | 2.0% | 0.0% | < 0.001 † |
| Dependent functional status | 1.7% | 14.8% | 1.6% | < 0.001 † |
| Preoperative myelopathy | 38.1% | 54.7% | 38.0% | < 0.001 † |
| Operative Characteristics | ||||
| Operative duration (hours) | < 0.001 † | |||
| < 2 | 56.2% | 35.2% | 56.3% | |
| 2-3 | 28.0% | 29.5% | 28.0% | |
| > 3 | 15.8% | 35.2% | 15.7% | |
| Procedure | < 0.001 † | |||
| ACDF (# of levels) | ||||
| One | 45.0% | 35.9% | 45.0% | |
| Two | 37.1% | 35.9% | 37.1% | |
| Three or more | 5.8% | 9.7% | 5.7% | |
| ACCF (# of levels) | ||||
| One | 3.7% | 8.1% | 3.7% | |
| Two or more | 3.3% | 9.1% | 3.2% | |
| CDA | 5.2% | 1.3% | 5.3% | |
| Anterior plate instrumentation | 68.1% | 69.5% | 68.1% | 0.620 |
| Ambulatory surgery | 8.4% | 2.0% | 8.4% | < 0.001 † |
| ASA classification | < 0.001 † | |||
| I or II | 57.6% | 23.8% | 57.7% | |
| III or IV | 42.4% | 76.2% | 42.3% | |
† Significance defined as p < 0.05, significant values are in bold.
COPD: Chronic Obstructive Pulmonary Disease, ASA: American Society of Anesthesiologists; ACDF: Anterior cervical discectomy and fusion; ACCF: Anterior cervical corpectomy and fusion; CDA: Cervical disc arthroplasty.
Postoperative Complications
Patients who developed RC after ACSS had significantly higher rates of total complications (75.8%) relative to those who did not (2.66%) (Table 2). On multivariate, all assessed comparisons of postoperative outcomes, with the exception of wound dehiscence, remained significantly higher in the RC relative to the non-RC cohort. The most common complications were unplanned return to the operating room (43.6%, Odds ratio [OR] 40.1, 95% confidence interval [CI] 30.9-52.0), pneumonia (35.9%, OR 68.8, 95%CI 50.7-93.2), sepsis (14.8%, OR 15.8, 95%CI 9.0-27.7), and death (11.7%, OR 51.5, 95%CI 30.6-86.9). Additionally, patients who developed RC had higher rates of perioperative blood transfusions (11.1%, OR 18.5, 95% CI 11.7-29.3), unplanned hospital readmission (26.7%, OR 5.4, 95%CI 4.1-7.3), and non-home discharge (45.6%, OR 8.5, 95%CI 6.4-11.1; P < 0.001 for all comparisons unless otherwise noted).
Table 2.
Comparison of 30-Day Complications by Postoperative Respiratory Complication Status.
| All Patients | Postoperative respiratory complication | Bivariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|---|
| Yes | No | ||||||
| 52,270 | 298 | 51,972 | P-value | OR | 95% CI | P-value | |
| Any complication | 3.07% | 75.8% | 2.66% | < 0.001 † | 73.4 | 55.3-97.4 | < 0.001 † |
| Death | 0.15% | 11.7% | 0.08% | < 0.001 † | 51.5 | 30.6-86.9 | < 0.001 † |
| Cardiac complications | 0.22% | 19.5% | 0.11% | < 0.001 † | 105.8 | 68.3-164.0 | < 0.001 † |
| Renal complications | 0.07% | 4.36% | 0.05% | < 0.001 † | 32.4 | 14.7-71.5 | < 0.001 † |
| Pneumonia | 0.59% | 35.9% | 0.39% | < 0.001 † | 68.8 | 50.7-93.2 | < 0.001 † |
| Unplanned return to operating room | 1.45% | 43.6% | 1.21% | < 0.001 † | 40.1 | 30.9-52.0 | < 0.001 † |
| Deep vein thrombosis | 0.25% | 5.37% | 0.22% | < 0.001 † | 13.20 | 7.3-23.8 | 0.011 † |
| Stroke/cerebrovascular accident | 0.07% | 3.02% | 0.05% | < 0.001 † | 26.7 | 11.2-63.9 | < 0.001 † |
| Sepsis | 0.20% | 14.8% | 0.16% | < 0.001 † | 15.8 | 9.0-27.7 | < 0.001 † |
| Wound infection | 0.40% | 2.01% | 0.39% | < 0.001 † | 4.7 | 2.0-11.0 | < 0.001 † |
| Wound dehiscence | 0.04% | 0.00% | 0.04% | 0.729 | -- | -- | -- |
| Urinary tract infection | 0.50% | 6.71% | 0.46% | < 0.001 † | 7.1 | 4.2-11.8 | < 0.001 † |
| Perioperative blood transfusion | 0.30% | 11.1% | 0.24% | < 0.001 † | 18.5 | 11.7-29.3 | < 0.001 † |
| Unplanned readmission | 3.55% | 26.7% | 3.42% | < 0.001 † | 5.4 | 4.1-7.3 | < 0.001 † |
| Non-home discharge | 4.40% | 45.6% | 4.16% | < 0.001 † | 8.5 | 6.4-11.1 | < 0.001 † |
† Significance defined as p < 0.05, significant values are in bold.
OR: Odds ratio; CI: Confidence interval
Of the 130 reoperations that occurred in the RC cohort, 52 (40.0%) were for hematoma evacuation and 18 (13.8%) were for tracheostomy (Table 3). Of the 69 RC patients who required readmission, 26 (37.7%) were for respiratory complications (including pneumonia, tracheostomy complications, and respiratory failure) and 13 (18.8%) were hematoma related.
Table 3.
Reasons for Reoperation and Readmission in Patients With Respiratory Compromise.
| Reoperation reason | Number (% of total) |
|---|---|
| Hematoma evacuation | 52 (40.0%) |
| Tracheostomy | 18 (13.8%) |
| Revision procedure (repeat arthrodesis, decompression) | 14 (10.8%) |
| Unrelated to cervical spine | 10 (7.7%) |
| Infectious (abscess, soft tissue debridement) | 5 (3.8%) |
| Wound dehiscence | 3 (2.3%) |
| Reason for reoperation unknown | 28 (21.5%) |
| Total reoperations | 130 (100.0%) |
| Readmission reason | Number (% of total) |
| Respiratory (pneumonia, tracheostomy complication, respiratory failure) | 26 (37.7%) |
| Hematoma | 13 (18.8%) |
| Unrelated to cervical spine | 8 (11.6%) |
| Non-surgical site infection (sepsis, Clostridium difficile) | 6 (8.7%) |
| Recurrence of neck pain or myelopathic symptoms | 4 (5.8%) |
| Surgical site infection | 4 (5.8%) |
| Dysphagia | 4 (5.8%) |
| Hardware failure | 1 (1.4%) |
| Reason for readmission unknown | 3 (4.3%) |
| Total readmissions | 69 (100.0%) |
Independent Predictors of RC
On multivariate analysis, patient age 61 to 70 (OR 2.3, 95%CI 2.5-6.1), age >70 (OR 3.9, 95%CI 2.5-6.1), non-white ethnicity (OR 1.4, 95%CI 1.1-1.8, P = 0.011), medical comorbidities including hypertension (OR 1.4, 95%CI 1.1-1.9, P = 0.018), smoking history (OR 1.4, 95% 1.1-1.9, P = 0.009), diabetes mellitus (OR 1.4, 95%CI 1.1-1.8, P = 0.009), COPD (OR1.6, 95%CI 1.2-2.4, P = 0.007), congestive heart failure (OR 3.0, 95%CI 3.1-6.2, P = 0.019), and dependent functional status (OR 4.4, 95%CI 3.1-6.2) were independent predictors of developing RC (Table 4). Operative factors that were predictive of RC included preoperative myelopathy (OR 1.3, 95%CI 1.1-1.7, P = 0.018), operative duration >3 hours (OR 2.3, 95%CI 1.7-3.1), 2-level ACCF (OR 2.3, 95%CI 1.5-3.6), and ASA classification III or IV (OR 1.9, 95%CI 1.4-2.5; P < 0.001 for all comparisons unless otherwise noted).
Table 4.
Independent Predictors of Postoperative Respiratory Complications.
| OR | 95% CI | P-value | |
|---|---|---|---|
| Age | |||
| < 50 | Reference | - | - |
| 51-60 | 1.7 | 1.1-2.5 | 0.011 † |
| 61-70 | 2.3 | 1.5-3.5 | < 0.001 † |
| > 70 | 3.9 | 2.5-6.1 | < 0.001 † |
| Male gender | 1.7 | 1.3-2.2 | < 0.001 † |
| Ethnicity | |||
| White | Reference | - | - |
| Black | 0.6 | 0.2-1.8 | 0.345 |
| Other or not reported | 1.4 | 1.1-1.8 | 0.011 † |
| Body mass index (kg/m2) | |||
| Non-obese (< 30) | Reference | - | - |
| Obese I (30-34.9) | 0.7 | 0.5-1.1 | 0.053 |
| Obese II (35-39.9) | 0.9 | 0.6-1.3 | 0.581 |
| Obese III (> 40) | 1.2 | 0.8-1.8 | 0.350 |
| Comorbidities | |||
| Hypertension | 1.4 | 1.1-1.9 | 0.018 † |
| Smoking history | 1.4 | 1.1-1.9 | 0.009 † |
| Diabetes mellitus | 1.4 | 1.1-1.8 | 0.009 † |
| Dyspnea | 1.4 | 0.9-2.0 | 0.108 |
| COPD | 1.6 | 1.2-2.4 | 0.007 † |
| Bleeding disorder | 1.8 | 1.0-3.2 | 0.058 |
| Congestive heart failure | 3.0 | 1.2-7.3 | 0.019 † |
| Dependent functional status | 4.4 | 3.1-6.2 | < 0.001 † |
| Preoperative myelopathy | 1.3 | 1.1-1.7 | 0.018 † |
| Operative duration (hours) | |||
| < 2 | Reference | - | - |
| 2-3 | 1.3 | 1.0-1.8 | 0.059 |
| > 3 | 2.3 | 1.7-3.1 | < 0.001 † |
| Procedure | |||
| ACDF (# of levels) | |||
| One | Reference | - | - |
| Two | 0.9 | 0.7-1.3 | 0.738 |
| Three or more | 1.2 | 0.8-1.9 | 0.370 |
| ACCF (# of levels) | |||
| One | 1.5 | 1.0-2.5 | 0.068 |
| Two or more | 2.3 | 1.5-3.6 | < 0.001 † |
| CDA | 1.1 | 0.3-1.9 | 0.463 |
| Ambulatory surgery | 0.5 | 0.2-1.1 | 0.070 |
| ASA classification | |||
| I or II | Reference | - | - |
| III or IV | 1.9 | 1.4-2.5 | < 0.001 † |
† Significance defined as p < 0.05, significant values are in bold.
COPD: Chronic Obstructive Pulmonary Disease, ASA: American Society of Anesthesiologists; ACDF: Anterior cervical discectomy and fusion; ACCF: Anterior cervical corpectomy and fusion; CDA: Cervical disc arthroplasty.
Discussion
This study identified 298 patients who developed RC, which occurred in 0.57% of all anterior cervical spine surgeries. Patients who develop RC have extremely high 30-day mortality (11.7%) and morbidity (75.8%) including pneumonia, return to the operating room, among others. We established a variety of patient-specific and operative predictors of developing RC after ACS, including increasing patient age, a history of preoperative cardiac or pulmonary comorbidities, dependent functional status, preoperative myelopathy, 2-level ACCF procedures, and prolonged operative duration. This is one of the largest RC cohorts described to date in the literature that identified the most comprehensive independent predictors of RC. These findings are useful for patient counseling, risk stratification, and surgical co-management in conjunction with the anesthesiology team for patients who are undergoing ACSS.
Given the low incidence of RC after ACSS, Marquez-Lara et al. was the first to leverage a large, national registry, the National Inpatient Sample (NIS), to query patients undergoing ACDF between 2002-11. 24 In total, the authors identified 1,464 cases of RC, which they defined as unplanned reintubations, with a total incidence of 0.56%. This incidence is concordant with the findings from our study; however, it does not include patients who had prolonged postoperative intubation. The authors identified age ≥ 65, 3-level or more ACDF, medical comorbidities such as congestive heart failure, chronic lung disease, neurological disorders, paralysis as predictors of RC in their cohort. This current study identified similar predictors of RC (with the exception of variables not available in the ACS-NSQIP such as neurological disorders), in addition to identifying relevant and potentially modifiable operative characteristics not described by Marquez-Lara et al., including preoperative myelopathy, operative duration, multi-level corpectomies, and ASA classification. Furthermore, the NIS is limited to outcomes only through the inpatient stay, and does not track patients after discharge which is a weakness relative to the ACS-NSQIP. To date, only small case studies discussed an association between myelopathy and RC, with conflicting results.8,14 It is possible that prior studies have been too underpowered to identify an association between myelopathy and RC, as patients with cervical myelopathy have been shown previously to have abnormal spirometry findings with decreased vital capacity, peak expiratory flow rate, increased respiratory rate,25,26 and with one case report even identifying myelopathy as a cause of bilateral phrenic nerve palsies. 27
Prior studies have utilized the ACS-NSQIP to identify the incidence and predictors of RC. Lim et al. in 2017 also utilized this registry to identify patients between 2011-2013 who underwent single- or multi-level (defined as two or more) ACDF. 28 In total they identified 73 patients who developed RC (total incidence of 0.60%), with independent predictors including increasing patient age, male gender, respiratory comorbidities, higher ASA class, and operative duration. The authors did not assess for the association between preoperative myelopathy and RC, and also did not find corpectomy as a predictor of RC. This is in contrast to our current study which identified a 2-level ACCF as having 2.3-fold higher odds of developing RC, relative to a one-level ACDF. This discrepancy may be due to the fact that the Lim et al. study had significantly fewer RC patients than this current study, or because they grouped all corpectomies together and did not sub-stratify by the number of corpectomies that were performed. 28 Of note, our current study also did not find an increased risk of RC with a single-level corpectomy. One prior case report did note an association between multi-level corpectomies and upper airway obstruction requiring reintubation, however, it was not sufficiently powered to perform a formal statistical analysis. 8 Corpectomies are typically reserved for cases that require substantial decompression, often in the setting of myelopathy.29,30 The increased rates of RC in our 2-level corpectomy cohort may have been due to an increased rate of preoperative myelopathy in this cohort, which impacts respiratory function. Additionally, the exposure for a corpectomy is typically more extensive than that of an ACDF or CDA in order to adequately visualize the lateral wall of the vertebral body to ensure adequate and complete decompression has occurred. Prior studies have demonstrated increased pre-vertebral soft tissue swelling as a function of number of levels fused, corpectomies, and upper cervical spine surgery.31,32
While previous studies have identified the incidence and risk factors for RC,24,28,33 none have fully defined the short-term clinical course of patients who develop RC. This study demonstrates that patients who develop RC have high rates of both morbidity and mortality. The high morbidity in this study (75.8%) is primarily driven by high rates of unplanned reoperations (43.6%) within 30-days of index surgery—most commonly for hematoma evacuation, presumably the etiology of RC in these patients, and for tracheostomy, illustrating the dismal prognosis for many patients who develop RC. A compressive hematoma may be the most common etiology of RC, reported between 0.6% and 1.3% in ACSS,34,35 and may be due to vascular injury, inadequate hemostasis, or for unknown etiologies.36,37 Interestingly, we did not find a statistical association between preoperative bleeding disorders and the development of RC. A case study by Song et al. corroborates this association as they had 9 patients develop compressive hematomas with respiratory symptoms at an average of 33 hours after index ACSS, however, none had preoperative coagulopathy. 38 In 3 patients who underwent hematoma evacuation in that case report, the sources of bleeding were identified as the jugular vein, an intramuscular vessel, and the superior thyroid artery.
This study has a number of limitations that are primarily inherent to national registry outcomes-based analyses. First, we were only able to identify short-term, 30-day outcomes and are unable to elucidate the medium- and long-term clinical courses, such as morbidity, mortality, and instrumentation failure, in patients who develop RC. Next, we identified myelopathy as an independent predictor of developing subsequent RC, however, we were not able to assess the relationship between the severity of myelopathy and the development of RC. Our classification of preoperative myelopathy was also predicated on postoperative ICD coding, which may be prone to misclassification or error. Additionally, drain utilization postoperatively may impact the development of compressive hematomas which may be a cause of RC. Unfortunately, we are unable to identify drain utilization information including number and type of drains used, duration of utilization, and drain output volume. Finally, we lacked a number of relevant variables that may have proven to be independent predictors of RC, such as preoperative anti-coagulant consumption, history of anesthetic related complications, utilization of steroid preparations during surgery to reduce swelling, among others.
In spite of these limitations, this current study identified one of the largest cohorts of patients to develop RC after ACSS and identified a range of independent predictors, some of which have only been previously described in case reports. RC is an extremely rare complication after ACSS with significant short-term morbidity and mortality. High risk patients, such as elderly males with cardiac and pulmonary comorbidities, a history of myelopathy, undergoing a lengthy ACSS procedure such as multi-level ACCF should be counseled on the risk for catastrophic complications such as RC. This data also is useful for preoperative risk stratification and surgical co-management discussions with the anesthesiology team.
Supplemental Material
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220984469 for Respiratory Compromise After Anterior Cervical Spine Surgery: Incidence, Subsequent Complications, and Independent Predictors by Venkat Boddapati, Nathan J. Lee, Justin Mathew, Michael B. Held, Joel R. Peterson, Meghana M. Vulapalli, Joseph M. Lombardi, Marc D. Dyrszka, Zeeshan M. Sardar, Ronald A. Lehman and K. Daniel Riew in Global Spine Journal
Supplemental Material, sj-docx-2-gsj-10.1177_2192568220984469 for Respiratory Compromise After Anterior Cervical Spine Surgery: Incidence, Subsequent Complications, and Independent Predictors by Venkat Boddapati, Nathan J. Lee, Justin Mathew, Michael B. Held, Joel R. Peterson, Meghana M. Vulapalli, Joseph M. Lombardi, Marc D. Dyrszka, Zeeshan M. Sardar, Ronald A. Lehman and K. Daniel Riew in Global Spine Journal
Footnotes
Authors’ Note: This study utilized national, de-identified data and is exempt from IRB review. This study does not have any prior or duplicate submissions or publications elsewhere of any part of the work. No funding sources, including from the National Institutes of Health; Wellcome Trust; or Howard Hughes Medical Institute, were utilized to complete this study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Venkat Boddapati, MD  https://orcid.org/0000-0002-3333-2234
https://orcid.org/0000-0002-3333-2234
Justin Mathew, MD  https://orcid.org/0000-0002-7699-780X
https://orcid.org/0000-0002-7699-780X
Meghana M. Vulapalli, BS  https://orcid.org/0000-0003-1197-0400
https://orcid.org/0000-0003-1197-0400
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Findlay C, Ayis S, Demetriades AK. Total disc replacement versus anterior cervical discectomy and fusion: a systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short- and medium- to long-term outcomes. Bone Joint J. 2018;100(8):991–1001. doi:10.1302/0301-620x.100b8.Bjj-2018-0120.R1 [DOI] [PubMed] [Google Scholar]
- 2.Saifi C, Fein AW, Cazzulino A, et al. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine J. 2018;18(6):1022–1029. doi:10.1016/j.spinee.2017.10.072 [DOI] [PubMed] [Google Scholar]
- 3.McAfee PC, Reah C, Gilder K, et al. A meta-analysis of comparative outcomes following cervical arthroplasty or anterior cervical fusion: results from 4 prospective multicenter randomized clinical trials and up to 1226 patients. Spine. 2012;37(11):943–952. doi:10.1097/BRS.0b013e31823da169 [DOI] [PubMed] [Google Scholar]
- 4.Wang T, Ma L, Yang DL, et al. Factors predicting dysphagia after anterior cervical surgery: a multicenter retrospective study for 2 years of follow-up. Medicine (Baltimore). 2017;96(34):e7916. doi:10.1097/md.0000000000007916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Obermüller T, Wostrack M, Shiban E, et al. Vertebral artery injury during foraminal decompression in “low-risk” cervical spine surgery: incidence and management. Acta Neurochir (Wien). 2015;157(11):1941–1945. doi:10.1007/s00701-015-2594-2 [DOI] [PubMed] [Google Scholar]
- 6.Fountas KN, Kapsalaki EZ, Nikolakakos LG, et al. Anterior cervical discectomy and fusion associated complications. Spine. 2007;32(21):2310–2317. doi:10.1097/BRS.0b013e318154c57e [DOI] [PubMed] [Google Scholar]
- 7.Tasiou A, Giannis T, Brotis AG, et al. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg. 2017;3(3):444–459. doi:10.21037/jss.2017.08.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emery SE, Smith MD, Bohlman HH. Upper-airway obstruction after multilevel cervical corpectomy for myelopathy. J Bone Joint Surg Am Vol. 1991;73(4):544–551. [PubMed] [Google Scholar]
- 9.Fujibayashi S, Shikata J, Yoshitomi H, Tanaka C, Nakamura K, Nakamura T. Bilateral phrenic nerve palsy as a complication of anterior decompression and fusion for cervical ossification of the posterior longitudinal ligament. Spine. 2001;26(12):E281–286. doi:10.1097/00007632-200106150-00029 [DOI] [PubMed] [Google Scholar]
- 10.Penberthy A, Roberts N. Recurrent acute upper airway obstruction after anterior cervical fusion. Anaesth Intensive Care. 1998;26(3):305–307. doi: 10.1177/0310057x9802600314 [DOI] [PubMed] [Google Scholar]
- 11.Riew KD, Sethi NS, Devney J, Goette K, Choi K. Complications of buttress plate stabilization of cervical corpectomy. Spine. 1999;24(22):2404–2410. doi:10.1097/00007632-199911150-00019 [DOI] [PubMed] [Google Scholar]
- 12.Kim M, Rhim SC, Roh SW, Jeon SR. Analysis of the risk factors associated with prolonged intubation or reintubation after anterior cervical spine surgery. J Korean Med Sci. 2018;33(17):e77. doi:10.3346/jkms.2018.33.e77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagoshi N, Fehlings MG, Nakashima H, et al. Prevalence and outcomes in patients undergoing reintubation after anterior cervical spine surgery: results from the AOSPINE North America Multicenter study on 8887 patients. Global Spine J. 2017;7(1):96s–102s. doi:10.1177/2192568216687753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sagi HC, Beutler W, Carroll E, Connolly PJ. Airway complications associated with surgery on the anterior cervical spine. Spine. 2002;27(9):949–953. doi:10.1097/00007632-200205010-00013 [DOI] [PubMed] [Google Scholar]
- 15.ACS-NSQIP. Program Specifics. https://www.facs.org/quality-programs/acs-nsqip/program-specifics. Published 2019. Accessed July 1, 2020.
- 16.Davis CL, Pierce JR, Henderson W, et al. Assessment of the reliability of data collected for the Department of Veterans Affairs national surgical quality improvement program. J Am Coll Surg. 2007;204(4):550–560. doi:10.1016/j.jamcollsurg.2007.01.012 [DOI] [PubMed] [Google Scholar]
- 17.Ingraham AM, Richards KE, Hall BL, Ko CY. Quality improvement in surgery: The American College of Surgeons National Surgical Quality Improvement Program approach. Adv Surg. 2010;44(1):251–267. [DOI] [PubMed] [Google Scholar]
- 18.Trickey AW, Wright JM, Donovan J, et al. Interrater reliability of hospital readmission evaluations for surgical patients. Am J Med Qual. 2017; 32(2):201–207. doi:10.1177/1062860615623854 [DOI] [PubMed] [Google Scholar]
- 19.Boddapati V, Fu MC, Nwachukwu BU, et al. Procedure length is independently associated with overnight hospital stay and 30-day readmission following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthros. 2020;28(2):432–438. doi:10.1007/s00167-019-05622-z [DOI] [PubMed] [Google Scholar]
- 20.Boddapati V, Grosso MJ, Sarpong NO, Geller JA, Cooper HJ, Shah RP. Early morbidity but not mortality increases with surgery delayed greater than 24 hours in patients with a periprosthetic fracture of the hip. J Arthroplast. 2019;34(11):2789–2792. e2781. doi:10.1016/j.arth.2019.06.027 [DOI] [PubMed] [Google Scholar]
- 21.Fu MC, Boddapati V, Dines DM, et al. The impact of insulin dependence on short-term postoperative complications in diabetic patients undergoing total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(12):2091–2096. doi:10.1016/j.jse.2017.05.027 [DOI] [PubMed] [Google Scholar]
- 22.Sarpong NO, Boddapati V, Herndon CL, Shah RP, Cooper HJ, Geller JA. Trends in length of stay and 30-day complications after total knee arthroplasty: an analysis from 2006 to 2016. J Arthroplast. 2019;34:1575–1580. doi:10.1016/j.arth.2019.04.027 [DOI] [PubMed] [Google Scholar]
- 23.[Anonymous]. R Core Team (2020). R: A language and environment for statistical computing. In. 3.6.3 ed. Vienna, Austria: R Foundation for Statistical Computing. https://www.R-project.org/. Published 2020. Accessed July 1, 2020.
- 24.Marquez-Lara A, Nandyala SV, Fineberg SJ, Singh K. Incidence, outcomes, and mortality of reintubation after anterior cervical fusion. Spine. 2014;39(2):134–139. doi:10.1097/brs.0000000000000098 [DOI] [PubMed] [Google Scholar]
- 25.Toyoda H, Nakamura H, Konishi S, Terai H, Takaoka K. Does chronic cervical myelopathy affect respiratory function? J Neurosurg Spine. 2004;1(2):175–178. doi:10.3171/spi.2004.1.2.0175 [DOI] [PubMed] [Google Scholar]
- 26.Bhagavatula ID, Bhat DI, Sasidharan GM, et al. Subclinical respiratory dysfunction in chronic cervical cord compression: a pulmonary function test correlation. Neurosurg Focus. 2016;40(6):E3. doi:10.3171/2016.3.Focus1647 [DOI] [PubMed] [Google Scholar]
- 27.Fregni F, Conceicao Souza GE, Taricco MA, Mutarelli EG. Phrenic paresis and respiratory insufficiency associated with cervical spondylotic myelopathy. Acta Neurochir (Wien). 2004;146(3):309–312; discussion 312. doi:10.1007/s00701-003-0201-4 [DOI] [PubMed] [Google Scholar]
- 28.Lim S, Kesavabhotla K, Cybulski GR, Dahdaleh NS, Smith ZA. Predictors for airway complications following single- and multilevel anterior cervical discectomy and fusion. Spine. 2017;42(6):379–384. doi:10.1097/brs.0000000000001737 [DOI] [PubMed] [Google Scholar]
- 29.Medow JE, Trost G, Sandin J. Surgical management of cervical myelopathy: indications and techniques for surgical corpectomy. Spine J. 2006;6(6):233s–241s. doi:10.1016/j.spinee.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 30.Salvatore C, Orphee M, Damien B, Alisha R, Pavel P, Bernard G. Oblique corpectomy to manage cervical myeloradiculopathy. Neurol Res Int. 2011;2011:734232. doi:10.1155/2011/734232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Song KJ, Choi BW, Kim HY, Jeon TS, Chang H. Efficacy of postoperative radiograph for evaluating the prevertebral soft tissue swelling after anterior cervical discectomy and fusion. Clin Orthop Surg. 2012;4(1):77–82. doi:10.4055/cios.2012.4.1.77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thomas SG, Joseph V, Rajshekhar V. Temporal progression and spatial distribution of “normal” prevertebral soft tissue swelling following central corpectomy for cervical spondylotic myelopathy. Neurol India. 2012;60(2):217–223. doi:10.4103/0028-3886.96405 [DOI] [PubMed] [Google Scholar]
- 33.Wilson LA, Zubizarreta N, Bekeris J, et al. Risk factors for reintubation after anterior cervical discectomy and fusion surgery: evaluation of three observational data sets. Can J Anaesth. 2020;67(1):42–56. doi:10.1007/s12630-019-01492-8 [DOI] [PubMed] [Google Scholar]
- 34.Bertalanffy H, Eggert HR. Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien). 1989;99(1-2):41–50. [DOI] [PubMed] [Google Scholar]
- 35.Marotta N, Landi A, Tarantino R, Mancarella C, Ruggeri A, Delfini R. Five-year outcome of stand-alone fusion using carbon cages in cervical disc arthrosis. Eur Spine J. 2011;20(1):S8–12. doi:10.1007/s00586-011-1747-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Debkowska MP, Butterworth JF, Moore JE, Kang S, Appelbaum EN, Zuelzer WA. Acute post-operative airway complications following anterior cervical spine surgery and the role for cricothyrotomy. J Spine Surg. 2019;5(1):142–154. doi:10.21037/jss.2019.03.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Palumbo MA, Aidlen JP, Daniels AH, Thakur NA, Caiati J. Airway compromise due to wound hematoma following anterior cervical spine surgery. Open Orthop J. 2012;6:108–113. doi:10.2174/1874325001206010108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song KJ, Choi BW, Lee DH, Lim DJ, Oh SY, Kim SS. Acute airway obstruction due to postoperative retropharyngeal hematoma after anterior cervical fusion: a retrospective analysis. J Orthop Surg Res. 2017;12(1):19. doi:10.1186/s13018-017-0517-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-gsj-10.1177_2192568220984469 for Respiratory Compromise After Anterior Cervical Spine Surgery: Incidence, Subsequent Complications, and Independent Predictors by Venkat Boddapati, Nathan J. Lee, Justin Mathew, Michael B. Held, Joel R. Peterson, Meghana M. Vulapalli, Joseph M. Lombardi, Marc D. Dyrszka, Zeeshan M. Sardar, Ronald A. Lehman and K. Daniel Riew in Global Spine Journal
Supplemental Material, sj-docx-2-gsj-10.1177_2192568220984469 for Respiratory Compromise After Anterior Cervical Spine Surgery: Incidence, Subsequent Complications, and Independent Predictors by Venkat Boddapati, Nathan J. Lee, Justin Mathew, Michael B. Held, Joel R. Peterson, Meghana M. Vulapalli, Joseph M. Lombardi, Marc D. Dyrszka, Zeeshan M. Sardar, Ronald A. Lehman and K. Daniel Riew in Global Spine Journal


