Abstract
Tracheal bronchus (TB) is a very rare condition, which is often associated with some other pathologies. This study was designed to characterize the morphology of tracheal bronchus and associated pathologies in Vietnamese individuals using multidetector-row computed tomography (MDCT). From August 2016 to February 2021, 16, 64-, and 128-detector-row computed tomography scanners were used to perform chest scans of 3663 patients, of whom 32 had tracheal bronchus and associated pathologies. The prevalence of tracheal bronchus was 0.9%, of which 0.6% were male and 0.3% were female. We found that one patient had bilateral tracheal bronchus (3.1%) and 31 patients (96.9%) had right-sided tracheal bronchus. Most patients (75.1%) had type II tracheal bronchus, whereas 15.6% and 6.2% had type III and type I tracheal bronchus, respectively. The average distance from the tracheal bronchus to the carina was 6.6 ± 6.4 mm. The average diameter of the tracheal bronchus was 4.4 ± 2.2 mm; the group with 2–4-mm tracheal bronchus accounted for the highest proportion (46.9%). Associated pathologies included congenital heart diseases (i.e., valvular heart disease, tetralogy of Fallot, cyanotic congenital heart disease-APSO, and aortic coarctation) (43.7%), stenosis of the bilateral pulmonary arteries (15.6%), absent left pulmonary artery (6.2%), stenosis of the right pulmonary artery (3.1%), anomalous pulmonary venous connection (3.1%), stenosis of the trachea (3.1%), stenosis of the left main bronchus (3.1%), bronchogenic cyst (3.1%), and bronchial atresia (3.1%), and the remaining 12.5% had no abnormalities. tracheal bronchus is a very rare abnormality among Vietnamese and is often accompanied by other pathologies. MDCT with a high spatial resolution and a good tissue contrast, along with contrast agent and appropriate scanning protocols, is efficient in detecting tracheal bronchus and associated pathologies.
Keywords: Tracheal bronchus, Multidetector-row computed tomography, Bronchus, Trachea, Associated pathologies
INTRODUCTION
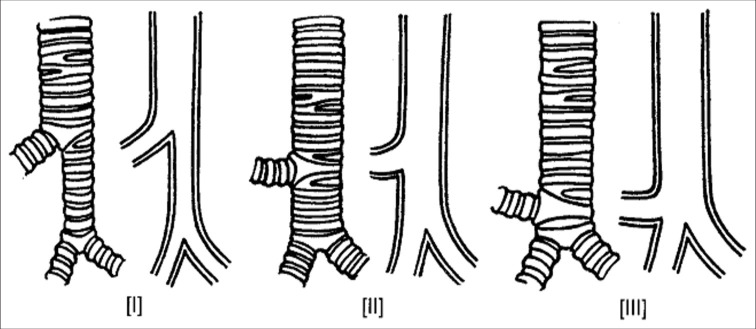
Tracheal bronchus (TB) is a very rare pathological condition, affecting approximately 1% of the world’s population, and it is classified as either “displaced” or “supernumerary.”[1-3] The essence of this pathology is the appearance of a bronchial branch growing mainly from the right side of the trachea, at the site of the carina, or approximately 2 cm above the carina.[3] This bronchial branch governs the right upper lobe or additionally a part of the middle lobe; however, it mostly remains in the apical segment of the upper lobe.[1,3,4] The disease was first described by Sandifort in 1785.[2] In some cases, all bronchi of the upper lobe originate directly from the trachea, while the right main bronchus will become an intermediate bronchus, directing the air to the middle and lower lobes; this abnormality is called “true tracheal bronchus” or “bronchus suis” (common in pigs and other even-toed ungulate animals).[5] Abnormalities in the left side are rarer than that in the right side, and this tracheal bronchus usually dominates the second segment of the upper lobe of the left lung.[1] According to Conacher (2000), tracheal bronchus is classified into three types [Figure 1]: (1) type I: The tracheal bronchus has traces of bronchial diverticulum, and its diameter is nearly equal to the diameter of the trachea above the carina; (2) type II: The bronchus for the apical segment originates at a high altitude; and (3) type III: The tracheal bronchus is fully developed at the site of the carina.[6] In the treatment, special attention should be paid during anesthesia, because type I abnormality may make intubation difficult. Type II abnormality easily causes bronchial obstruction. Meanwhile, type III abnormality, similar to type II, can cause unilateral ventilation disorders, particularly in the upper lobe.[3,6,7]
Figure 1:
Classification of tracheal bronchus according to Conacher (2000).
In fact, the aforementioned abnormalities often cause clinical symptoms; however, in some cases, we cannot explain the symptoms. Some patients have repeated pneumonia, cough, shortness of breath, and even hemoptysis; in infants or children, respiratory failure may occur.[5,7,8] For cases, where the cause is difficult to determine, a comprehensive examination, including medical history; clinical examination; hematological, biochemical, microbiological tests; and exploration of respiratory function, is performed. In addition, most patients undergo bronchoscopy, echocardiography, and chest computed tomography (CT).[8,9] Multidetector-row CT (MDCT) is a diagnostic modality with high spatial resolution and good tissue contrast, allowing the visualization of the pathologies on multiple planes using reconstruction software; therefore, it can detect tracheal bronchus and abnormalities of the lobes or segments that are dominated by tracheal bronchus. Furthermore, with contrast injection and appropriate scanning protocols, it can show the associated pathologies, such as congenital heart diseases and abnormal heart and blood vessels. For this pathology, CT may be the most dominant imaging tool.[8-11] This study was designed to characterize the morphology of tracheal bronchus and associated pathologies among Vietnamese using MDCT.
CASE SERIES
A cross-sectional study was conducted involving 32 patients of 3663 who were examined and treated at National Lung Hospital and Hanoi Heart Hospital, Hanoi, Vietnam, from August 2016 to February 2021. Of the 32 patients, 21 were male and 11 were female, with a male/female ratio of 1.9:1 (P < 0.05); the age of the patients ranged from 7 days to 75 years.
In the two hospitals, we used six MDCT scanners: 64- and 128-detector row CT Scenaria (Hitachi, Japan); 16- and 64-detector row CT Somatom Perspective (Siemens, Germany); and 16-detector row CT LightSpeed Ultra and LightSpeed Plus (GE, USA). All patients underwent routine chest CT using a contiguous slice thickness of 0.6–1.25 mm, a pitch of 1.5, a matrix size of 512 × 512, a tube voltage of 120 kV, and a tube current of 300 mA. For children, the tube voltage was reduced to 80 kV and the tube current was altered to 110 mA.
To detect associated pathologies, a contrast agent was administered with a dose of 1 mL/kg for adults and 1.5 mL/kg for children through a peripheral venous access route using an automatic injector through an 18- or 22-gauge needle through an antecubital vein at a rate of 3–5 mL/s. The moment of acquisition scanning was determined using the test bolus, which means that the contrast agent was injected first, and then, the CT scanner started scanning one slice continuously at the region of interest, which was placed on the main pulmonary artery or descending aorta. When the contrast agent concentration reached the threshold of 120 HU, the acquisition scanning automatically started so that the contrast agent spread most strongly into the heart chambers and major blood vessels of the heart, which could help doctors recognize the lesions and other associated pathologies; this delayed time was usually approximately 20–30 s after the injection. The post-scanned images were saved as DICOM files and viewed and processed on the workstation. Multiplanar reformation (MPR), multi-projection volume reconstruction, volume rendering (VR), and virtual endoscopy were used to help observe and access the lesions better.[11-13]
The clinical symptoms and imaging characteristics of tracheal bronchus are shown in [Table 1].
Table 1:
Clinical symptoms and imaging characteristics of tracheal bronchus (n=32).
| Number | Percentage | |
|---|---|---|
| Clinical symptoms | ||
| Cough | 23 | 71.9 |
| Hemoptysis | 4 | 12.5 |
| Shortness of breath | 19 | 59.4 |
| Wheezing | 13 | 40.6 |
| Chest pain | 17 | 53.1 |
| No symptoms | 4 | 12.5 |
| Tracheal bronchus type (Conacher) | ||
| Bilateral | 1 | 3.1 |
| Right side (Type I) | 2 | 6.2 |
| Right side (Type II) | 24 | 75.1 |
| Right side (Type III) | 5 | 15.6 |
| Anomalies of bronchial tree | ||
| Displaced | 10 | 31.3 |
| Supernumerary | 18 | 56.3 |
| Pig bronchus | 4 | 12.4 |
| Tracheal bronchus site (distance to the carina) | ||
| At the site of carina (0 mm) | 6 | 18.8 |
| <11 mm | 19 | 59.4 |
| 11–20 mm | 5 | 15.6 |
| >20 mm | 2 | 6.2 |
| Absolute tracheal bronchus diameter | ||
| <2 mm | 4 | 12.5 |
| 2–4 mm | 15 | 46.9 |
| 4–6 mm | 8 | 25.0 |
| >6 mm | 5 | 15.6 |
| Relative tracheal bronchus diameter (compared with the tracheal diameter) (%) | ||
| <25 | 13 | 40.6 |
| 25–50 | 13 | 40.6 |
| 50–75 | 4 | 12.5 |
| >75 | 2 | 6.2 |
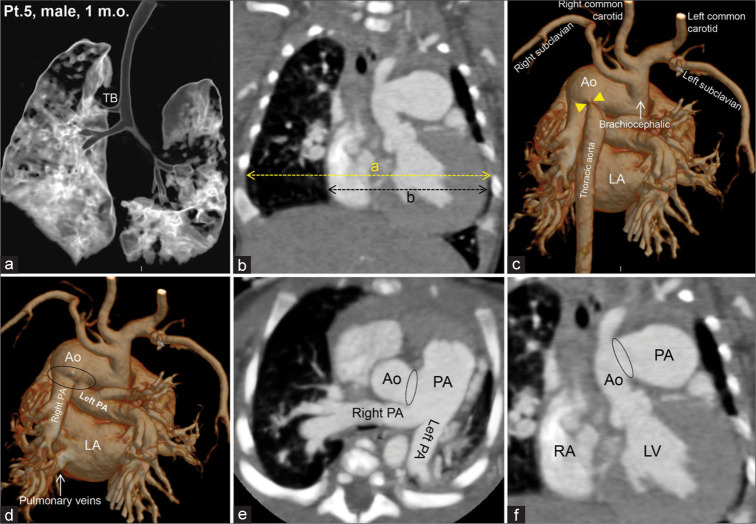
The three most common clinical symptoms were cough, shortness of breath, and chest pain. The most common tracheal bronchus abnormality was type II (75.1%) [Figure 2]. Only one patient had bilateral tracheal bronchus (3.1%). The average distance from the tracheal bronchus to the carina was 6.6 mm; most patients (93.8%) had a distance of ≤20 mm. The average diameter of the tracheal bronchus was 4.4 ± 2.2 mm, ranging from 1.7 mm to 12 mm. The group with a diameter of 2–4 mm accounted for the highest proportion (46.9%). Moreover, 81.2% of the patients had a tracheal bronchus diameter of >50% of the tracheal diameter. Most tracheal bronchi belong to the supernumerary group (56.3%).
Figure 2:
Chest computed tomography images of a 53-year-old man with a tracheal bronchus (TB) on the right side (Type II), approximately 2 cm above the carina (a-d). This bronchial branch governed the right upper lobe. No lesions were observed in the lung parenchyma (a). TB was discovered incidentally during routine health check.
The pathologies associated with tracheal bronchus and treatment methods are shown in [Table 2].
Table 2:
The pathologies associated with tracheal bronchus and treatment methods (n=32).
| Associated pathologies | Number (%) | Treatment (%) | |
|---|---|---|---|
| Drugs | Surgery | ||
| Cardiovascular diseases | 24 (75.0) | 14 (43.7) | 19 (59.3) |
| Stenosis of the bilateral pulmonary arteries | 5 | 5 | 5 |
| Stenosis of the right pulmonary artery | 2 | 2 | 2 |
| Absent left pulmonary artery | 2 | 2 | 2 |
| Pulmonary veins drain into the coronary sinus | 1 | 1 | |
| Ventricular septal defect, atrial septal defect, and heart valve diseases | 8 | 4 | 4 |
| Tetralogy of Fallot | 1 | 1 | |
| Cyanotic congenital heart disease – APSO (types II, III, and IV) | 3 | 3 | |
| Aortic coarctation | 2 | 2 | |
| Other pathologies | 4 (12.5) | 4 (12.5) | 0 |
| Tracheal stenosis | 1 | 1 | |
| Bronchial atresia | 1 | 1 | |
| Bronchogenic cyst | 1 | 1 | |
| Stenosis of the left main bronchi | 1 | 1 | |
| No associated abnormalities | 4 (12.5) | 0 | 0 |
Some patients had more than one associated abnormality or pathology. Cardiovascular diseases accounted for the majority (75.0%), they were quite diverse; however, most of them were congenital heart diseases (14/32 = 43.7%), followed by stenosis of the bilateral pulmonary arteries, accounting for 15.6% (5/32) [Figure 3]; other pathologies and no associated abnormalities accounted for 12.5% each. Nineteen patients (59.3%) underwent surgery or first underwent medical treatment with drugs, followed by surgery. The surgery was mainly related to treating abnormalities of congenital heart disease. Five patients (15.6%) received conservative treatment only. The remaining four patients received no treatment.
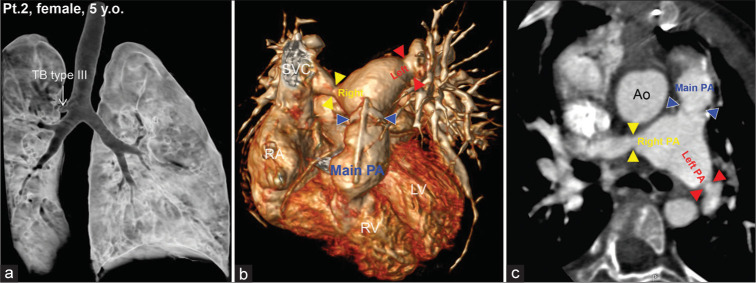
Figure 3:
Chest computed tomography images of a 5-year-old girl with a tracheal bronchus on the right side, at the site of the carina (type III) (a). There was stenosis at the main (blue arrow heads), right (yellow arrow heads), and left (red arrow heads) pulmonary arteries (b and c). right atrium, right ventricle, left ventricle, Ao, aorta, pulmonary artery, and superior vena cava.
DISCUSSION
Incidence, age, and sex
In this study, in the past 5 years (2016–2021), we have detected 32 cases of tracheal bronchus of 3663 patients (0.9%) in two specialized hospitals in Hanoi, Vietnam. The youngest patient was 7 days old and the oldest was 75 years old; among them, males had a higher proportion than females (1.9:1). Similar to some other countries,[3,10,14] tracheal bronchus is a very rare disease in Vietnam; our patients’ age fluctuated in a wide range, because we had randomly selected patients undergoing chest MDCT in the two aforementioned hospitals, most of whom had clinical symptoms related to the heart and lungs.
Clinical symptoms
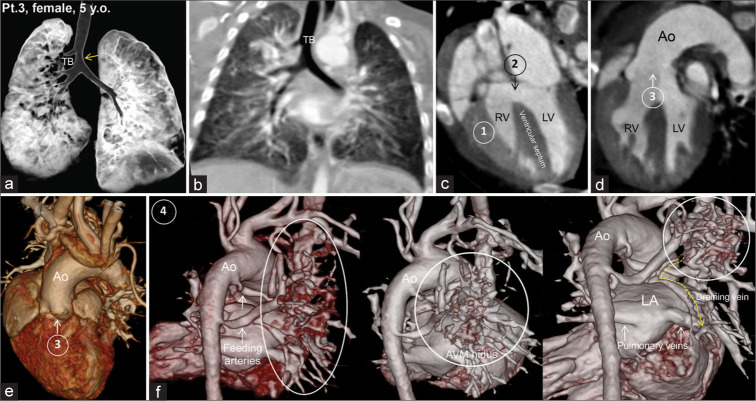
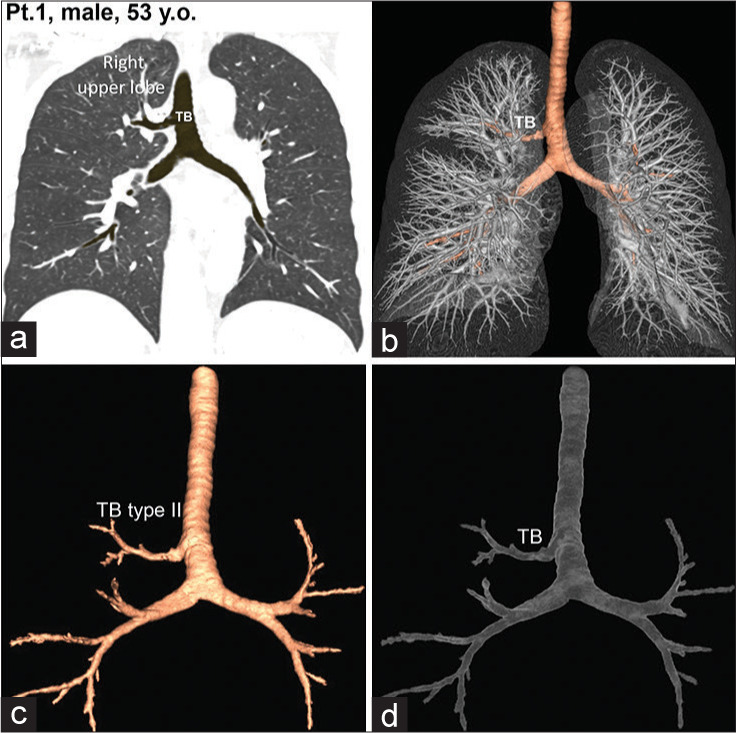
In this study, the three most common clinical symptoms were cough, shortness of breath, and chest pain. All children (100%) had serious clinical manifestations, such as coughing, hemoptysis, wheezing, shortness of breath, and chest pain, due to congenital cardiovascular abnormalities; stagnation could cause stenosis, obstruction of the airways leading to atelectasis, or even severe respiratory failure due to heart abnormalities, such as cyanotic congenital heart disease, tetralogy of Fallot [Figure 4], valvular heart diseases, patent ductus arteriosus, aortic coarctation, and anomalous pulmonary venous connection, and tracheal and bronchial abnormalities, such as tracheal stenosis, bronchogenic cyst, and bronchial obstruction. Most patients underwent surgery (59.3%). The clinical manifestations of tracheal bronchus often vary, depending on the diameter of the tracheal bronchus and the associated pathologies.[15,16] In this study, four patients were asymptomatic, which could be explained by the small diameter of the tracheal bronchus, without ventilation disturbances, stagnation, and associated pathologies. The clinical symptoms caused by tracheal bronchus and associated diseases often overlap; sometimes, determining the root cause of the disease is difficult.
Figure 4:
Computed tomography images of a 1-month-old boy with a tracheal bronchus (TB) on the right side (Type II), approximately 2.3 cm above the carina. There was a tracheal stenosis just below the TB site (yellow arrow) (a). The lung parenchyma was opaque, with congestion in both lungs (b). In addition to TB, the patient had tetralogy of Fallot (c-f) including (1) thickened right ventricular wall (hypertrophy), (2) ventricular septal defect, (3) the aorta overriding the septal defect, and (4) absent pulmonary artery; instead, there was a large arteriovenous malformation – AVM (oval or round circle) on the right side of the heart, in which two feeding arteries originated from the descending aorta, and the draining vein (dotted arrows) drained into one of the four pulmonary veins.
Characteristics of tracheal bronchus
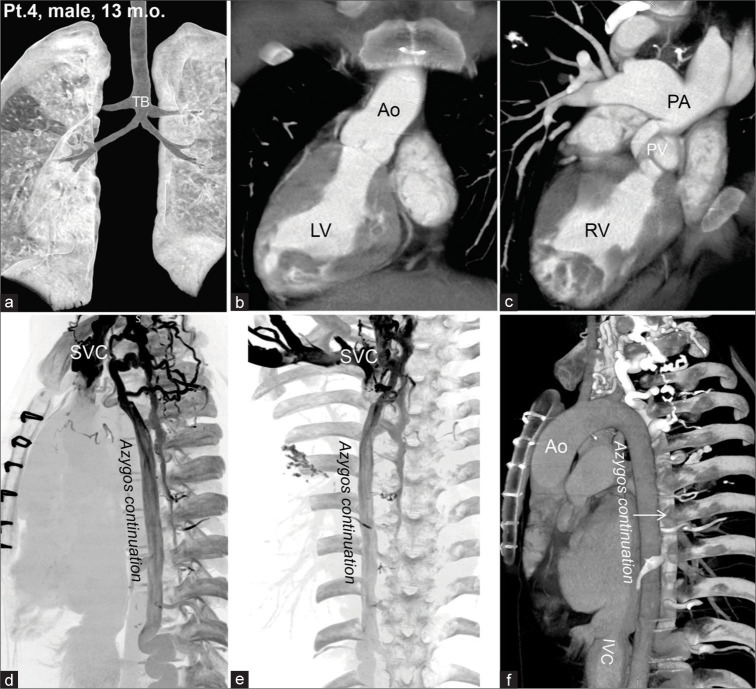
According to our data, all abnormalities were located on the right side. We did not have any cases with the left-sided abnormalities; only one patient had bilateral tracheal bronchus [Figure 5]. The most common type of tracheal bronchus was type II (75.1%), which is the tracheal bronchus that dominates the apical segment with the size of trachea being completely normal. Most abnormalities were within the distance of 0–2 cm from the carina (93.8%), as described in the literature;[3,8] however, in this study, we noticed abnormalities with a mean distance from the carina of 6.5 mm. Most tracheal bronchi had a diameter of >2 mm (87.5%), with an average of 4.4 ± 2.2 mm, ranging from 1.7 mm to 12 mm. The group of patients with tracheal bronchus diameters ranging from 2 mm to 4 mm accounted for the highest proportion (46.9%). Most tracheal bronchi have a diameter of <50% of the tracheal diameter (81.2%). Many studies have attempted to classify tracheal bronchus according to the method of Conacher (2000); however, each author provided different numbers in terms of the tracheal bronchus type, diameter, and distance from the tracheal bronchus to the carina.[7] Dave et al. (2014) reported that all of their cases had tracheal bronchus on the right side and had type III tracheal bronchus. One patient had near-carina tracheal stenosis. Before detecting tracheal bronchus, seven of 11 patients were intubated during the surgery for congenital heart disease.[15] Wang et al. (2016) found that the tracheal bronchus distance to the carina of <1 cm accounted for 25%, 1–2 cm accounted for 50%, and 2–3 cm accounted for 25%.[5] Moreno et al. (2019) reported that 76% of tracheal bronchus cases were type I, and 24% were type III.[7] Pérez Ruiz et al. (2018) reported that the type of tracheal bronchus was primarily ectopic lobar of the right upper lobe (73%), followed by apical supernumerary (11.5%). The tracheal bronchus that originated from the lower third of the trachea accounted for 96.0% and those that originated from the carina accounted for 4.0%.[14] According to RuchonnetMetrailler et al. (2015), patients with type I, II, III accounted for 56%, 31%, and 13%, respectively.[3] The determination of the tracheal bronchus type, diameter, and distance to the carina is important to clinicians, particularly when preparing to apply therapeutic interventions, such as intubation under anesthesia and treatment of respiratory failure. In these cases, there is always a question of whether the end of the endotracheal tube obstructs the exit of the tracheal bronchus; moreover, considering the possibility of secondary respiratory complications, such as atelectasis, respiratory failure, or pneumonia after tube placement is necessary.
Figure 5:
Computed tomography images of a 13-month-old boy with bilateral tracheal bronchus and bilateral main bronchial stenosis (a). This patient had a right-sided heart (b), abnormalities in the pulmonary valve (PV), main pulmonary artery stenosis, and dilatation of the right and left pulmonary arteries (c). An azygos continuation (d-f) was observed due to interrupted inferior vena cava (IVC), commonly associated with the left isomerism. PV, (pulmonary valve)
Associated pathologies
In the literature, many abnormalities have been reported to be associated with tracheal bronchus.[1,2,4,14] However, these abnormalities can be divided into two main groups: (1) cardiovascular diseases and (2) other pathologies. The incidence of these abnormalities varied widely among studies, depending on the patient group selected for the study and what diagnostic modality was used; however, generally, bronchopulmonary and cardiovascular abnormalities were easier to detect, because patients often had clinical manifestations.[14] In this study, MDCT was used to investigate the patients with cardiovascular and respiratory symptoms; therefore, we could only detect the lesions in the lungs, trachea, bronchi, heart, and major blood vessels [Table 2], but not genetic abnormalities in other organs. To sum up our point, we found that 75.0% of the patients had associated cardiovascular diseases [Figure 6] and 12.5% had other pathologies.
Figure 6:
Computed tomography images of a 1-month-old boy with a tracheal bronchus on the right side (Type II) (a). The patient had an enlarged heart (b), in which the cardiac–thoracic index = the maximum transverse diameter of the heart/the maximum internal diameter of the thorax = b/a >0.6 (for newborns). A brachiocephalic trunk arising from the aortic arch was observed, from which the bilateral subclavian and common carotid arteries arose. The thoracic aorta was severely narrow (yellow arrow heads) at the origin, emerging from the aortic arch (c). The root of the pulmonary artery has a large opening (oval circle) to the aorta (d-f).
Earlier, Sen et al. (2010) conducted a more comprehensive examination and found many types of lesions in the body; for example, tracheal bronchus can be combined with other congenital abnormalities, such as rib abnormalities, chest concave, congenital esophageal obstruction, tracheal– esophageal ventilation, tracheal stenosis, congenital cystic malformation, spine abnormalities, Down syndrome, and Klippel Feil’s syndrome.[17] Moreno et al. (2019) reported that 33% of patients with tracheal bronchus had tracheomalacia, 32% had congenital cardiovascular abnormalities, 28% had a combination of gastroesophageal reflux disease, 22.5% had congenital tracheal stenosis, and 8.3% had symptoms associated with Down syndrome.[7] Pérez Ruiz et al. (2018) found that 92.3% of tracheal bronchus cases were related to congenital diseases (i.e., heart disease accounted for 69%, of which diseases of the ventricular septum accounted for 22.2%, diseases of the atrial septum accounted for 16.7%, patent ductus arteriosus accounted for 16.7%, pulmonary valve stenosis accounted for 11.1%, aortic stenosis accounted for 5.5%, chromosomal abnormality accounted for 35%, and spinal defects accounted for 11%). Other abnormalities included tracheomalacia, accounting for 26.9%; bronchomalacia, accounting for 26.9%; tracheal stenosis, accounting for 19.2%; and bronchial stenosis, accounting for 7.7%.[14]
Based on Ruchonnet-Metrailler et al. (2015)’s study, tracheal bronchus was also associated with other abnormalities, such as cardiac abnormalities (19.2%) that include tetralogy of Fallot, ventricular septal, aortic and pulmonary vascular abnormalities, and abnormalities of other major blood vessels. The related syndromes accounted for 21%, including three tracheal bronchus cases related to Down syndrome and two tracheal bronchus cases related to CHARGE syndrome; congenital tracheal stenosis accounted for 14%; and 38.5% of the patients had no associated abnormalities.[3]
As mentioned above, tracheal bronchus is often associated with congenital heart diseases; therefore, patients with a primary diagnosis of congenital heart disease must also be concerned about whether they have tracheal bronchus.
Differential diagnosis
Several bronchial anomalies require differential diagnosis with tracheal bronchus. (1) The first is accessory cardiac bronchus – according to Webb and Higgins, this is a phenomenon of bronchial growth that originates from the edge of the intermediate bronchus or bronchus of the right lower lobe, spreading downward and toward the mediastinum or heart, often found by chance in approximately 0.1% of patients.[18] In some cases, the accessory cardiac bronchus is short; the bronchial tip ends, which is not related to the alveoli and may also end in the mediastinum. Others may have long bronchial branches, associated with a portion of lung tissue. Most cases are asymptomatic; some cases present with hemoptysis or chronic pneumonia. (2) The second is bronchial isomerism – bronchial isomerism is used to refer to the symmetrical anatomy of the right and left bronchi. It may be independent or in combination with other abnormalities, particularly congenital heart disease.[9,18] In our patients, all anomalies originated from the trachea, of which almost all protruded from the right side; only one case had bilateral and symmetrical tracheal bronchus that ventilated the upper lobes of both lungs. Based on bronchial morphology, the patient with bilateral tracheal bronchi appeared to have left isomerism with an azygos continuation [Figure 5] observed in cases of interrupted inferior vena cava, again commonly associated with the left isomerism.
Role of MDCT in detecting tracheal bronchus and associated pathologies
Two common modalities are used to investigate tracheal bronchus, namely, MDCT and flexible bronchoscopy. Flexible bronchoscopy has the advantage of allowing the direct visualization of the surface of the airways (bronchi); it is good for evaluating a lobe bronchus and is a useful tool in assessing the extent and length of the narrowing, determining whether the cause of the stenosis is the absence of bronchial cartilage.[8-12]
However, MDCT has many advantages over flexible bronchoscopy and is considered the gold standard in determining tracheal bronchus due to the following reasons: MDCT is a noninvasive investigation method with a wide field of view, from the central region (trachea) to the periphery of the lung;[11] has thin slice thickness;[9] and can be performed quickly and easily, even in children, without the need of sedation or anesthesia.[11] The detection of tracheal bronchus using MDCT without a contrast agent is not difficult because the air in the trachea and bronchus has a very different density as compared with the lung parenchyma and other chest structures. Axial images along with 2D renderings (i.e., MPR and MIP) on sagittal, coronal, oblique, and curved sections and 3D rendering (VR) allow the localization of tracheal bronchus and the assessment of its stenosis, obstruction, dilation, morphology (type), and size (diameter) and other tracheal bronchus – associated abnormalities at any desired angle, including the distal portion of the narrowed or obstructed area, when endoscopic hose cannot pass through.[8,10,12] This information will help clinicians avoid treatment accidents and complications. Moreover, MDCT also allows the observation of lung parenchymal lesions and the consequences of having tracheal bronchus, such as pneumonia, lung tumors, bronchogenic cysts, and lung hypoventilation.[9,10] Furthermore, virtual endoscopic software allows for the superficial assessment of the trachea and preliminary evaluation of the tracheal cartilage. When heart and blood vessel diseases or lung tumors are suspected, contrast-enhanced 3D CT is an excellent tool in assessing the relationship between the bronchial tree, heart, and blood vessels, which plays a particularly important role in patients with indications of surgery; 3D CT can also be used to evaluate lymph nodes, the stage of cancer, and invasion of the tumor into the airways.[12] Furthermore, CT helps physicians plan interventional techniques, such as respiratory endoscopy, stenting, surgery, and monitoring. At present, dynamic MDCT with thin slice thickness, taken during both inspiration and expiration (4D CT taken in one respiratory cycle), with MPR, VR, and virtual endoscopy software helps comprehensively assess the airways and is today’s most powerful diagnostic tool.[11]
Although MDCT has many advantages over flexible bronchoscopy, the combination of both modalities remains the optimal choice in diagnosing tracheal bronchus and associated diseases;[11] besides, ultrasound and magnetic resonance imaging can also be added.
The disadvantage of MDCT is the use of ionizing radiation; therefore, it is contraindicated in pregnant women and limited in children. Virtual endoscope software allows the visualization of the surface of the trachea; however, this is only a virtual image.
Treatment
Of the 32 patients (59.3%), 19 received treatment, of whom three adults and 16 children received surgery or the combination of drugs and surgery. The surgery was mainly related to solving the abnormalities associated with congenital heart disease. Five patients (15.6%) received conservative treatment only. The remaining four patients received no treatment at all. In surgical cases, during anesthesia, the anesthesiologist paid special attention to the tracheal bronchus to avoid the endotracheal tubes obstructing the airways. In adults, the disease is often associated with other lung diseases, such as repeated pneumonia, which could cause bronchiectasis, chronic obstructive bronchopulmonary disease, and even lung tumors. For these cases, we administered treatment early to avoid dangerous complications. In the case of repeated pneumonia, hemoptysis due to bronchiectasis, segmentectomy, or lobectomy was performed. In this study, three patients underwent lobectomy, including two adults and a 10-month-old child, due to hemoptysis and repeated pneumonia.
CONCLUSION
Our initial results showed that tracheal bronchus is also a very rare (0.9%) abnormality among Vietnamese and is often associated with other pathologies (mainly cardiovascular diseases). The airways should be evaluated carefully in all cases of congenital heart defect to look for such anomalies. MDCTs of ≥16 detector rows with high spatial resolution and good tissue contrast, along with contrast agent and appropriate scanning protocols, are efficient in detecting tracheal bronchus and associated pathologies.
Footnotes
How to cite this article: Lam K, Hoang LV, Anh LV. Tracheal bronchus and associated pathologies detected by multidetector-row computed tomography in the Vietnamese population. J Clin Imaging Sci 2022;12:56.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Doolittle AM, Mair EA. Tracheal bronchus: Classification, endoscopic analysis, and airway management. Otolaryngol Head Neck Surg. 2002;126:240–3. doi: 10.1067/mhn.2002.122703. [DOI] [PubMed] [Google Scholar]
- 2.Ghaye B, Szapiro D, Fanchamps JM, Dondelinger RF. Congenital bronchial abnormalities revisited. Radiographics. 2001;21:105–19. doi: 10.1148/radiographics.21.1.g01ja06105. [DOI] [PubMed] [Google Scholar]
- 3.Ruchonnet-Metrailler I, Abou Taam R, de Blic J. Presence of tracheal bronchus in children undergoing flexible bronchoscopy. Respir Med. 2015;109:846–50. doi: 10.1016/j.rmed.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Zheng YJ, Deng JK, Zhang DZ, Gen YG. Diagnosis of tracheal bronchus in children. World J Pediatr. 2007;3:286–9. [Google Scholar]
- 5.Wang S, Zhang H, Zhu L, Zhen J, Liu J, Xu Z. Surgical management of congenital tracheal stenosis associated with tracheal bronchus and congenital heart disease. Eur J Cardiothorac Surg. 2016;49:1201–6. doi: 10.1093/ejcts/ezv317. [DOI] [PubMed] [Google Scholar]
- 6.Conacher ID. Implications of a tracheal bronchus for adult anaesthetic practice. Br J Anaesth. 2000;85:317–20. doi: 10.1093/bja/85.2.317. [DOI] [PubMed] [Google Scholar]
- 7.Moreno M, Castillo-Corullón S, Pérez-Ruiz E, Luna MC, Antón-Pacheco JL, Mondejar-Lopez P, et al. Spanish multicentre study on morbidity and pathogenicity of tracheal bronchus in children. Pediatr Pulmonol. 2019;54:1610–6. doi: 10.1002/ppul.24435. [DOI] [PubMed] [Google Scholar]
- 8.Kim H, Kim YT, Jou SS, Lee WH. True tracheal bronchus: Classification and anatomical relationship on multi-detector computed tomography. J Korean Soc Radiol. 2017;76:264–72. doi: 10.3348/jksr.2017.76.4.264. [DOI] [Google Scholar]
- 9.Jamil A, Soos MP. StatPearls. Treasure Island, FL: StatPearls Publishing; 2021. Tracheal bronchus. [Google Scholar]
- 10.Chen SJ, Lee WJ, Wang JK, Wu MH, Chang CI, Liu KL, et al. Usefulness of three-dimensional electron beam computed tomography for evaluating tracheobronchial anomalies in children with congenital heart disease. Am J Cardiol. 2003;92:483–6. doi: 10.1016/S0002-9149(03)00676-3. [DOI] [PubMed] [Google Scholar]
- 11.Baden W, Schaefer J, Kumpf M, Tzaribachev N, Pantalitschka T, Koitschev A, et al. Comparison of imaging techniques in the diagnosis of bridging bronchus. Eur Respir J. 2008;31:1125–31. doi: 10.1183/09031936.00045907. [DOI] [PubMed] [Google Scholar]
- 12.Jugpal TS, Garg A, Sethi GR, Daga MK, Kumar J. Multi-detector computed tomography imaging of large airway pathology: A pictorial review. World J Radiol. 2015;7:459–74. doi: 10.4329/wjr.v7.i12.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Suzuki M, Matsui O, Kawashima H, Takemura A, Matsubara K, Hayashi N, et al. Radioanatomical study of a true tracheal bronchus using multidetector computed tomography. Jpn J Radiol. 2010;28:188–92. doi: 10.1007/s11604-009-0405-5. [DOI] [PubMed] [Google Scholar]
- 14.Pérez Ruiz E, Caro Aguilera P, Valdivielso AI, Sanchís Cárdenas S, Martínez García Y, Pérez Frías J. Tracheal bronchus diagnosed in children undergoing flexible bronchoscopy. Paediatr Respir Rev. 2018;28:26–30. doi: 10.1016/j.prrv.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 15.Dave MH, Gerber A, Bailey M, Gysin C, Hoeve H, Hammer J, et al. The prevalence of tracheal bronchus in pediatric patients undergoing rigid bronchoscopy. J Bronchol Interv Pulmonol. 2014;21:26–31. doi: 10.1097/LBR.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 16.Shih FC, Lee WJ, Lin HJ. Tracheal bronchus. CMAJ. 2009;180:783. doi: 10.1503/cmaj.080280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sen S, Sentürk E, Pabusçu E, Sen S. Upper lobectomy for lung cancer with true tracheal bronchus: A unique presentation. J Arch Bronconeumol. 2010;46:332–4. doi: 10.1016/S1579-2129(10)70076-8. [DOI] [PubMed] [Google Scholar]
- 18.Webb WR, Higgins BC. 2nd ed. Philadelphia, PA: Wolters Kluwer; 2002. Thoracic Imaging: Pulmonary and Cardiovascular Radiology; pp. 1–2. [Google Scholar]