Abstract
Background:
A neuroendoscope is a technical advance that allows surgeons to visualize certain regions of the brain that was previously inaccessible through the use of a surgical microscope. Several neuroendoscope designs have been implemented by other neurosurgeons over the past 5 years. The advantage of a neuroendoscope is the addition of a flexible and narrow tip that allows for safe entry into intracranial structures for clinical observation. However, there are some limitations to this approach. Here, we report the use of a modified angioscope as a newly developed neuroendoscope to be employed in observing intracranial structures.
Methods:
We report the use of an angioscope that is 1.8 mm in diameter and has both a thin and flexible tip. In this study, the angioscope was inserted into the lumen of an aspirator tube, and the tip of the device was placed at the intracranial area of intended observation area. Image findings were evaluated using an established in vivo goat brain model.
Results:
The angioscope was light in weight and maneuverable and could be reached and observed in the blind spot using a surgical microscope. From the cerebellopontine angle, the lower cranial nerves and trigeminal nerve could be observed, and from the cisterna magna, the floor of the fourth ventricle and the aqueduct could be seen.
Conclusion:
The angioscope is a useful instrument to observe intracranial locations safely and effectively even within a limited surgical field. Further modifications will be required to use the angioscope in various craniotomy procedures.
Keywords: Angioscope, Intracranial, Neuroendoscope, Neurosurgery

INTRODUCTION
When patients suffer from aneurysm, a procedure known as cerebral aneurysm neck clipping must be performed to prevent ischemia. At present, neurosurgeons must perform microsurgical clipping, where a small metal clip is used to obstruct the ruptured aneurysm and to prevent rebleeding.[9,10] For neurosurgeons, the ability to observe the intracranial area around the neck of an aneurysm is crucial to prevent ischemic complications.[9,10] Of particular concern, the region of the branch of vessels originating behind the parent artery is difficult to observe using a standard surgical microscope.[3,5] In addition, in the cases of microvascular decompression for trigeminal neuralgia, it may also be difficult to observe the responsible vessels on the dorsal cranial surface containing the trigeminal nerve.[8,15] The neuroendoscope, due to its higher magnification, better observation, and additional illumination, can provide us information that may not be obtained using the microscope in aneurysm surgery.[1,3,5,12,13] The neuroendoscope assists in capturing blind spots with the surgical microscope.[1,3,5,12,13] However, using a neuroendoscope may be difficult in a narrow surgical field without advanced technique for safe and reliable use.[2]
An angioscope is utilized to observe and evaluate the degree of atherosclerosis within the lumen of blood vessels.[4,6,7,15] A unique feature of the angioscope is that the retractable tip is thin and flexible, approximately 1.83 mm in width. Therefore, we considered that it could be applied as a neuroendoscope to capture deep and narrow areas of the brain that cannot be observed with a surgical microscope. In this report, the angioscope was examined to determine its potential for use as a new neuroendoscope that is safer and easier to handle than conventional neuroendoscopic manipulation using an in vivo goat brain model.[11]
MATERIALS AND METHODS
Animal models
In vivo goat brain model that we recently reported was employed to the present study. Three male goats, which weighed 17.5, 26.5, and 27.5 kg, were considered. We ensured that the study was performed under the conformity of the international, national, and institutional rules considering animal experiments, clinical studies, and biodiversity rights. All manipulations and protocols were performed according to the Guidelines for Animal Experiments at the International University of Health and Welfare and in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH publications no. 85–23) revised in 1996.
Surgery
Animals were initially anesthetized with xylazine 0.4 mg/0.02/kg and atropine 0.5 mg injected intramuscularly, and maintained on 5% isoflurane and 95% O2 at 1.5–2.0 ml/min to control breathing. Anesthesia was maintained with 2% isoflurane and 100% O2 at 1.5–2.0 ml/min.[11] Craniotomies were performed by placing the animals in the prone position and orientating the head such that midline skin incisions of the scalp could be safely carried out. The craniotomy was carried out in a size of 6 cm × 6 cm with an air tome. After incision of the dura mater, a right retrosigmoid approach was performed under a surgical microscope. An additional surgical approach was made from the lateral side of the cerebellum to reach the cerebellopontine angle, and an angioscope was inserted to investigate whether it is possible to observe trigeminal nerves and lower cranial nerves. Next, the tonsil was retracted and the floor of the fourth ventricle was observed, and an angioscope was inserted ventral to the brainstem to observe the anterior surface of the brainstem and cervical spinal cord.
In vivo recordings
The angioscope used in this study was a Zemporshe videovascular endoscopic catheter with an outer diameter of 1.83 mm, length of 180 cm, a focal range of 2–3 mm, a viewing angle of 92.6°, and a pixel count of 48000 (OVALIS, Osaka, Japan). The angioscope was inserted into a suction tube (Fujita Medical Instruments Co., Ltd Tokyo, Japan) with an inner diameter of 2.5 mm to guide it safely to the deep and narrow areas of the brain.
RESULTS
The angioscope is extremely light in weight, easy to handle, and allows rapid access to the area under observation [Figure 1a]. Furthermore, by inserting the angioscope into the lumen of the suction tube, it could be safely and rapidly introduced into the optimal site [Figure 1b]. In evaluation through the retrosigmoid approach, the angioscope inserted into the cerebellopontine angle allowed us to clearly observe the lower cranial nerves, such as the glossopharyngeal and vagus nerves, as well as the trigeminal nerve [Figure 2a]. In addition, the entrance to the Meckel’s cave, which is difficult to detect with a surgical microscope, could be clearly observed [Figure 2b]. The cerebellar tonsil was retracted and the floor of the fourth ventricle was clearly observed, and the central sulcus and aqueduct could be identified [Figure 3a]. Angioscope was inserted ventral to the brainstem through the foramen magnum. The anterior surface of the brainstem and cervical spinal cord could be clearly observed [Figure 3b]. In vivo goat brain model has a brain texture similar to that of humans, and the cranial nerves have a gross anatomical structure similar to that of humans, making it useful for research to evaluate the neuroendoscope.
Figure 1:
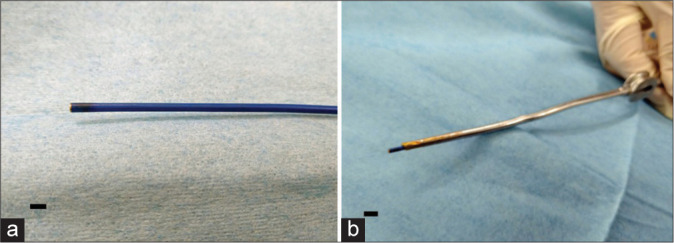
Observations of the angioscope. Panel a depicts an angioscope that has a thin and flexible tip. Panel b depicts the use of the angioscope into the lumen of the aspirator tube allowing for safe observation of the intracranial cavity. The scale bar is 2 mm.
Figure 2:
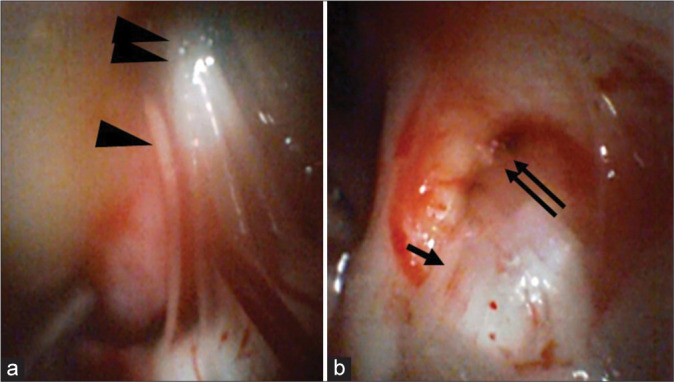
Observations of an angioscope inserted into the cerebellopontine angle Panel (a) depicts the use of the angioscope to observe the glossopharyngeal (arrow head) and vagus nerves (double arrow heads) in the cerebellopontine angle. Panel (b) indicates the use of the angioscope to observe the trigeminal nerve (arrow) and Meckel’s cavity (double arrows).
Figure 3:
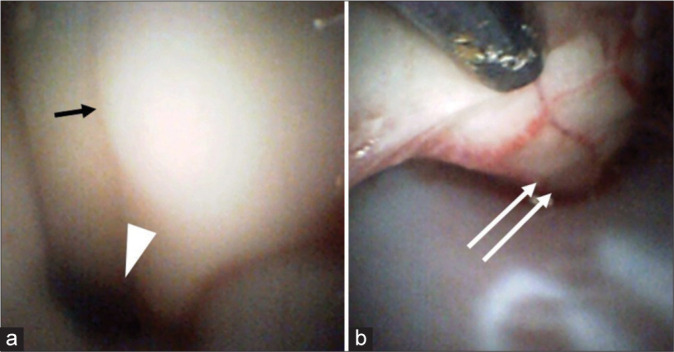
Observations of an angioscope inserted into the cisterna magna Panel (a) depicts the use of the angioscope to observe the floor of the fourth ventricle of the central sulcus (arrow), as well as the cerebral aqueduct (arrow head). Panel (b) indicates the use of the angioscope inserted through the foramen magnum to observe the anterior surface of the spinal cord (double arrow), which could be evaluated up to the C3 vertebrae.
DISCUSSION
The angioscope is primarily used for observations of the coronary artery. Normal intima of the endothelium is white and smooth, but the lipid deposition provides a yellowish tinting of the endothelial cell wall, allowing angioscope to detect early atherosclerotic lesions that do not cause stenosis.[6] In addition, it is expected that angioscope will be able to provide diagnosis of unstable plaques with a high risk of developing acute coronary syndromes and selective treatment of localized lesions under endoscopic guidance.[7,14] Angioscope is also used to follow peripheral arteries of the extremities to observe the patient after stenting.[4,7,14] When angioscope is performed to observe a lesion inside an artery, the complexities of stopping blood flow and flushing the lumen with saline solution are involved.[7,14] However, in the case of craniotomy surgery, it is possible to simply insert an angioscope into the surgical field for any sites in the brain. Here, we report the angioscope as a light weight device that is thin and flexible enough, making it sufficiently maneuverable for intravascular observations. Therefore, we decided to evaluate the potential of the angioscope as a new neuroendoscope that can be introduced into various intracranial regions that are difficult to observe with other devices.
Neuroendoscopes are usually used to observe pituitary tumors,[13] skull base tumors,[1] intraventricular manipulations,[12] and areas that are blind spots in the surgical microscope.[1,3,5,12,13] Neuroendoscope allows direct observation of branches from the parent artery around the neck of a cerebral aneurysm, even in areas where a surgical microscope would have a blind spot.[3,5] In fact, it has been reported that aneurysm surgery using the neuroendoscope is associated with fewer complications than conventional aneurysm surgery.[5] In microvascular decompression for trigeminal neuralgia, the neuroendoscope also allows direct observation of the responsible vessel for compressing the trigeminal nerve, even if it is located behind the trigeminal nerve and is difficult to observe with a surgical microscope.[8,15] Since both are used in a limited narrow surgical field, advanced skills are required to perform the observations safely and confidently.[2] In a narrow surgical field, a neuroendoscope can be an obstacle to surgical microscope manipulation because it obstructs the field of view.[2]
In this study, a thin, light, and flexible angioscope was inserted into the suction in the present study. The angioscope can be used in the same motion as a suction manipulation, because no particular skill is required to handle it. In addition, double-tube suction may be useful in the fact that it does not interfere with the suction function. We are currently preparing a study of angioscope as neuroendoscope with double-tube suction. The major difference with existing neuroendoscope is that the angioscope can be manipulated in fine movements to intend to observe the optimum site and does not interfere with the surgical manipulations in the limited narrow surgical field because of its thinness. Further refinement of the angioscope for use as a new neuroendoscope has the potential to provide a significant benefit in craniotomy surgery.
There have been no reports of this neurosurgical technique training using live goat brains. We recently reported the usefulness of in vivo goat brain model in neurosurgical training.[11] The goat brain has a human-like brain texture and anatomical structures such as blood vessels and nerves that are similar to those of humans. Since in vivo goat brain model is not a cadaveric brain, it allows for realistic training such as a hemostatic manipulation in a pulsating brain and blood vessel.[11] In addition, it was indicated that the interhemispheric and the retrosigmoid approaches are possible.[11] The present study used an in vivo goat model and indicated the usefulness of this model not only for neurosurgical technique training but also for neuroendoscopic research.
CONCLUSION
The angioscope could be very useful as a neuroendoscope to safely and simply observe any site in craniotomy that cannot be reached by the field of view of a surgical microscope. The angioscope is expected to be developed and refined as a new neuroendoscope through further improvements based on the accumulation of more cases.
Acknowledgments
We would like to express our gratitude to OVARIS K.K., led by Mr. Hori and Integra Japan K.K., led by Mr. Ito and Mr. Shibakawa, for their cooperation with goat brain model.
Footnotes
How to cite this article: Onoda K, Sashida R, Hirokawa Y, Fujiwara R, Wakamiya T, Michiwaki Y, et al. The development of a new, ultra-fine, and flexible neuroendoscope for intracranial observation. Surg Neurol Int 2022;13:460.
Contributor Information
Keisuke Onoda, Email: onoda3883@gmail.com.
Ryohei Sashida, Email: sashidaryohei@gmail.com.
Yu Hirokawa, Email: yuhirokawa13@gmail.com.
Ren Fujiwara, Email: renfujiwara9@gmail.com.
Tomihiro Wakamiya, Email: twakamiya@iuhw.ac.jp.
Yuhei Michiwaki, Email: y.michiwaki@iuhw.ac.jp.
Tatsuya Tanaka, Email: s96047@hotmail.com.
Kazuaki Shimoji, Email: shimoji@iuhw.ac.jp.
Eiichi Suehiro, Email: esuehiro@iuhw.ac.jp.
Fumitaka Yamane, Email: fyamane@iuhw.ac.jp.
Masatou Kawashima, Email: mkawashima@iuhw.ac.jp.
Akira Matsuno, Email: akira.dr.ruby@gmail.com.
Ethical approval
All procedures used in this research were approved by the Ethical Committee of International University of Health and Welfare.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Almeida JP, de Albuquerque LA, Fabbro MD, Sampaio M, Medina R, Chacon M, et al. Endoscopic skull base surgery: Evaluation of current clinical outcomes. J Neurosurg Sci. 2019;63:88–95. doi: 10.23736/S0390-5616.16.03386-5. [DOI] [PubMed] [Google Scholar]
- 2.Azab WA, Abdelrahman AY, Alsheikh TM, Najibullah M. Neuroendoscopy in Kuwait: Evolution, current status and future directions. World Neurosurg. 2016;92:298–302. doi: 10.1016/j.wneu.2016.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Fischer G, Oertel J, Perneczky A. Endoscopy in aneurysm surgery. Neurosurgery. 2012;70(Suppl 2):184–91. doi: 10.1227/NEU.0b013e3182376a36. [DOI] [PubMed] [Google Scholar]
- 4.Hatada A, Takagaki Y, Yamamoto S, Okamura Y, Nishimura Y. High-resolution angioscopic observation of deep vein thrombosis after catheter-directed venous thrombolysis. Circ J. 2020;84:1885. doi: 10.1253/circj.CJ-20-0461. [DOI] [PubMed] [Google Scholar]
- 5.Ho CL, Peter Y Hwang PY. Endoscope-assisted transorbital keyhole surgical approach to ruptured supratentorial aneurysms. J Neurol Surg A Cent Eur Neurosurg. 2015;76:376–83. doi: 10.1055/s-0035-1547358. [DOI] [PubMed] [Google Scholar]
- 6.Ihara M, Nojima Y, Koh N, Adachi H, Kurimoto T, Okayama K, et al. Angioscopic findings of neovascularization around yellow plaque. Circ J. 2021;85:1400. doi: 10.1253/circj.CJ-21-0102. [DOI] [PubMed] [Google Scholar]
- 7.Ikeoka K, Okayama K, Watanabe T, Nanto S, Sakata Y, Hoshida S. Refractory vascular wall healing after paclitaxel-coated nitinol stent implantation in the femoropopliteal artery: A high-resolution angioscopic assessment. Ann Vasc Dis. 2018;11:373–6. doi: 10.3400/avd.cr.18-00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kher Y, Yadav N, Yadav YR, Parihar V, Ratre S, Bajaj J. Endoscopic vascular decompression in trigeminal neuralgia. Turk Neurosurg. 2017;27:998–1006. doi: 10.5137/1019-5149.JTN.17046-16.1. [DOI] [PubMed] [Google Scholar]
- 9.Lee HS, Kim M, Park JC, Ahn JS, Lee S, Park W. Clinical features of ischemic complications after unruptured middle cerebral artery aneurysm clipping: Patients and radiologically related factors. Neurosurg Rev. 2021;44:2819–29. doi: 10.1007/s10143-021-01475-8. [DOI] [PubMed] [Google Scholar]
- 10.Matsukawa H, Kamiyama H, Miyazaki T, Kinoshita Y, Ota N, Noda K, et al. surgical treatment of middle cerebral artery aneurysms: Aneurysm location and size ratio as risk factors for neurologic worsening and ischemic complications. World Neurosurg. 2018;117:e563–70. doi: 10.1016/j.wneu.2018.06.077. [DOI] [PubMed] [Google Scholar]
- 11.Onoda K, Fujiwara R, Sashida R, Hirokawa Y, Wakamiya T, Michiwaki Y, et al. In vivo goat brain model for neurosurgical training. Surg Neurol Int. 2022;13:344. doi: 10.25259/SNI_494_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rocque BG. Neuroendoscopy for intraventricular tumor resection. World Neurosurg. 2016;90:619–20. doi: 10.1016/j.wneu.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rutkowski M, Zada G. Management of pituitary adenomas invading the cavernous sinus. Neurosurg Clin N Am. 2019;30:445–55. doi: 10.1016/j.nec.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Tsujimura T, Ishihara T, Iida O, Hata Y, Toyoshima T, Higashino N, et al. Arterial healing 10 months after implantation of an ultrathin-strut, biodegradable-polymer, sirolimus-eluting stent an angioscopic study. Circ Rep. 2021;3:316–23. doi: 10.1253/circrep.CR-21-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang P, Li Q, Wang C, Li C. Complete neuroendoscopic versus microscopical trigeminal neuralgia microvascular decompression (MVD) in primary trigeminal neuralgia (PTN) Am J Transl Res. 2021;13:12905–12. [PMC free article] [PubMed] [Google Scholar]


