Purpose of review
The coronavirus disease 2019 (COVID-19) pandemic has posed great challenges to intensive care units (ICUs) across the globe. The objective of this review is to provide an overview on how ICU surging was managed during COVID-19 pandemic, with a special focus on papers published in the last 18 months.
Recent findings
From the onset of the COVID-19 pandemic, it was apparent that the biggest challenge was the inequity of access to an adequately equipped and staffed ICU bed. The first wave was overwhelming; large surge of patients required critical care, resources were limited and non-COVID-19 care processes were severely compromised. Various approaches were used to address ICU staffing shortage and to expand the physical ICU space capacity. Because of restrictions to family visitations in most ICUs, the pandemic posed a threat to communication and family-centered ICU care. The pandemic, especially during the first wave, was accompanied by a high level of apprehension in the community, many uncertainties about clinical course and therapy and an influx of speculations and misinformation.
Summary
Although healthcare systems learned how to face some of the challenges with subsequent waves, the pandemic had persistent effects on healthcare systems.
Keywords: coronavirus disease 2019, intensive care, pandemic, staff, surge capacity
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has posed great challenges to intensive care units (ICUs) across the globe. The first wave was overwhelming; large surge of patients required critical care, resources for patient management such as personal protective equipment and ventilators were limited and non-COVID-19 care processes were severely compromised. This was accompanied by a high level of apprehension in the community, many uncertainties about clinical course and therapy and an influx of speculations and misinformation. (Table 1). Although healthcare systems learned how to face some of the challenges with subsequent waves, the pandemic had persistent effects on healthcare systems.
Table 1.
The evolution of ICU response during COVID-19 pandemic
| First wave | Subsequent waves | |
| Healthcare system level | Large surge of patients that overwhelmed healthcare systems | Healthcare systems became more prepared |
| Non-COVID-19 care processes were severely compromised | Non-COVID-19 care was resumed | |
| High level of apprehension in the community at large | Level of apprehension in the country about COVID-19 eased with time | |
| Limited availability of resources for patient management, such as personal protective equipment, ventilators and medications | Better availability of resources | |
| Family visitation were restricted, and communication was compromised | Family visitation became less restrictive, with improvement in communication | |
| Major staffing shortages, the employment of non-ICU staff | ICU staffing shortages were better managed | |
| Patient level | Disease severity was high | Disease severity reduced, associated with better outcomes |
| Many uncertainties about clinical course and therapy | More information about the clinical course and therapy | |
| Early reports from observational studies were often incomplete | More comprehensive and complete observational datasets | |
| No data from clinical trials | Clinical trials results became available | |
| No vaccines | Healthcare professionals and patients became increasingly vaccinated | |
| Reliance on invasive respiratory support | Common use of noninvasive respiratory support | |
| No data on effective therapeutics | Emerging data on effective therapeutics |
COVID-19, coronavirus disease 2019; ICU, intensive care unit.
The objective of this review is to highlight how ICU surging managed during COVID-19 pandemic, with a special focus on papers published in the last 18 months.
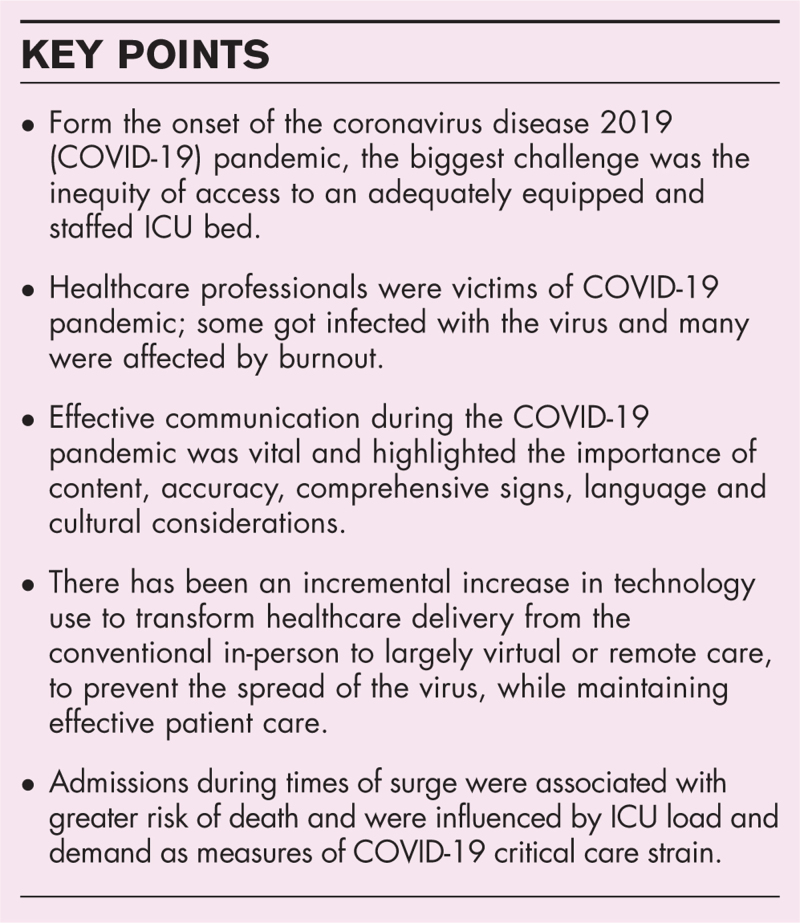
Box 1.
no caption available
ICU STAFFING
It was apparent from the onset of COVID-19 pandemic that ICU staffing was a limiting factor in the surge response; lack of staffed ICU beds has resulted in increased mortality [1]. Critical care staff capacity was augmented by noncritical staff during the initial COVID-19 surges. A multicenter international point-prevalence study during the pandemic surge between February 15 and May 15, 2020, showed that non-ICU nurses and physicians were employed in 85% and 58% of the participating ICUs, respectively [2▪▪]. In a survey of US hospitals about the preparedness for the first COVID-19 surge, almost all hospitals (n = 169) canceled or postponed elective surgeries (96.7%) and nonsurgical procedures (94.8%) [3▪]. In semi-structured interviews of intensivists from hospitals in the United States between August and November 2020, clinicians believed that ICU staff was the most limited resource; staff shortages were improved by the use of tiered staffing models, just-in-time training for non-ICU clinicians, designated treatment teams, and deployment of trainees [4]. In a study from United States, 48% of sites implemented tiered staffing models, 49% adding temporary physicians, nurses, or respiratory therapists, and 30% changed the ratios of physicians or nurses to patients [5]. In the tiered staffing models, non-ICU skilled physicians and advanced practice providers provided care under the supervision or in collaboration with an intensivist [6]. Nursing workforce has also been expanded by teaming ICU-trained nurses with other nurses to assist in non-ICU aspects of care. The use of procedure teams (e.g., intubations, central venous catheterization and mobility teams) and telemedicine coverage has been used to expand ICU staffing workforce. However, there have been concerns about the lower-quality care provided as a result the repurposing and augmenting staff [6]. Additionally, cancelling time-sensitive care to avail staff to work in the ICU has been associated with adverse consequences on the outcome of other patients with non-COVID-19 conditions.
Healthcare professionals were also victims of COVID-19 pandemic. According to an estimate from the World Health Organization (WHO), between 80 000 and 180 000 healthcare professionals could have died from COVID-19 in the period between January 2020 and May 2021 [7]. Burnout added further stain to the critical care workforce. A cross-sectional study (October 30−December 1, 2020) of healthcare professionals in 16 ICUs during the second wave in France, demonstrated high prevalence of anxiety (60%), depression (36%), posttraumatic stress disorder (28%), and burnout (45%). The highest tiers of hospital management urgently need to provide psychological support, peer-support groups, and a communication structure that ensure the well being of healthcare professionals [8▪▪]. The following modifiable determinants of symptoms of mental health disorders have been identified: fear of being infected, inability to rest, inability to care for family, struggling with difficult emotions, regret about the restrictions in visitation policies, and witnessing hasty end-of-life decisions [9]. A quantitative study demonstrated that such major individual-level concerns intersected with institutional-level challenges, such as feeling or being valued within the healthcare setting. Transparency and trust in the institutional setting were identified as key for successful leadership through such uncertain times [10].
MANAGING ICU SPACE AND EQUIPMENT STRAIN
Various approaches were used to expand the physical space capacity for managing critically ill patients with COVID-19. In a survey of US hospitals (n = 169) about the preparedness for a potential surge of the COVID-19, 63% of hospitals dedicated specific ICUs for patients with COVID-19, 51% repurposed existing step-down units as ICUs, 33% repurposed other clinical care space not typically dedicated to inpatient care as ICUs, 24% repurposed existing medical/surgical units as ICUs, 13% created new medical units in areas not typically dedicated to clinical care [3▪]. A multicenter point-prevalence study during the pandemic surge between February 15 and May 15, 2020, showed that 40% patients were admitted to surge capacity beds [2▪▪]. Shortages of ventilators, supplies and medications were a prominent challenge during COVID-19 pandemic. In the above survey of US hospitals, 71% bought or borrowed additional mechanical ventilators, 30% used noninvasive ventilators, continuous positive airway pressure (CPAP) machines, or anesthesia machines for mechanical ventilation. Almost no hospitals actually developed protocols for rationing ventilators (5.6%) or connecting multiple patients to a single ventilator (4.8%), although a majority were prepared to do both (64.4% and 61.3%, respectively) [3▪]. The lack of adequate personal protective equipment for frontline healthcare professionals, including respirators, gloves, face shields, gowns, and hand sanitizer resulted from problems with the global supply chain [11].
COMMUNICATION
Communication with caregivers is one of the most highly valued aspects of care. Effective communication during the COVID-19 pandemic was vital and highlighted the importance of content, accuracy, comprehensive signs, language and cultural considerations. Ignorance with sociocultural, economic, psychological, and health factors can jeopardize effective communication at all levels [12,13]. The pandemic posed a threat to communication and family-centered ICU care. Visitations were prohibited in most ICUs to prevent transmission of infection. With the family was no longer at the patient's bedside, structured communication, involvement in decision-making and support to the family by the ICU team could not adequately be provided [14]. The use of personal protective equipment by healthcare professionals further increased the barriers to communication due to fogging, incoherent speech and inability to view the facial expressions of the caregiver by the patient. Practicing alternative communication strategies therefore became a necessity for healthcare professionals to communicate with patients and their families.
Recognizing the value of staying in touch, guidance for communication with patients and families in the COVID-19 has been published [15]. This includes providing clear explanations, provided directly or over the phone and on institutional websites, concerning the imposed restrictive policy and the justification for the same, maintaining continuity of communication through proactive routine telephone calls and providing information about the patient's health status and comfort along with a follow up plan [16,17]. In addition, the ICU team should encourage the patient and family to call, text, and use videoconferencing with each other as often as they desire [15]. When visitation in the ICU is forbidden, one should try to make it possible at least during end-of-life care to arrange for end-of-life family videoconferences to help the family prepare for bereavement [17].
Effective communication, if ignored, may generate gaps especially in vulnerable populations, increasing the difficulty in combating the healthcare challenges faced during the pandemic [13]. One of the major factors for developing Post-ICU syndrome-Family (PICS-F) is poor communication with an ICU team. Communication that is perceived as inconsistent, unsatisfactory or uncomforting is associated with higher risk of post-ICU burden [14]. Healthcare professionals have faced significant burnout during the pandemic [17]. Addressing the psychology of the individual and providing psychological support is vital during a pandemic and can be achieved by establishing an effective communication network. As the pandemic evolved, recognizing these challenges and concerns, ICU teams made their visitation policies more flexible to facilitate effective communication, adapting to the inflow of patients, while using specific protocols to limit the transmission of infection.
THE USE OF TECHNOLOGY
There has been an incremental increase in technology use to transform healthcare delivery from the conventional in-person to largely virtual or remote care, to prevent the spread of the virus, while maintaining effective patient care. A systematic review of the use of 20 technology-based methods for the provision of remote healthcare services suggested that they could help control the spread of the disease [18]. The pandemic brought the realization of the benefits of digital transformation and the value of remote monitoring technologies for the critically ill [19]. The use of technology facilitated setting up of centralized ‘command centers’ for rapid response and optimal distribution of patients across hospital and ICUs based on bed and resource availability. In addition, high-risk patients could be monitored in areas outside the ICU using wireless systems [20].
Tele-communications tools allow health-care workers to assess, monitor, council and treat patients remotely. Telemedicine additionally helps in conserving health-care resources, especially personal protective equipment, and free ICU beds [21]. Use of telemedicine can be advantageous to individuals with underlying health conditions who are particularly susceptible to COVID-19 [22]. Systematic reviews have demonstrated the usefulness of telemedicine based services used during the pandemic [23▪,24]. The concept of “live-streamed ICU rounds” were developed to limit the physical presence of ICU staff, by allowing medical staff to communicate to provide multidisciplinary care and education [25,26]. However, this approach is limited by lack of direct patient contact. Communication with patients and families were often facilitated through virtual ICU visits, web-based family conferences, video calls and through media groups.
In some ICUs, patient equipment, including infusion pumps, monitors and ventilator control boards were moved outside the patient rooms and connected to the patient by extension cords or tubes or were controlled remotely using Wi-Fi or Bluetooth. Artificial intelligence (AI) has been studied as a diagnostic tool, an epidemiological instrument, and for drug-selection and for managing vasopressor infusions. Whether AI can provide effective timely solutions to help during a pandemic needs to be investigated. Additionally, technology enabled developing large registries, rapid large scale global data collection and facilitated developing platform trials [27]. Nevertheless, the effectiveness of the individual technologies needs to be investigated further for their impact on patient-centered outcomes.
RESEARCH AND KNOWLEDGE DISSEMINATION
The pace of COVID-19 research was extraordinary. There were many success stories, with large clinical trials and international registries completed in months. The International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) has reported data on over 800 000 hospitalized patients in more than 54 countries, and addressed multiple aspects of clinical characterization of COVID-19 [28]. Platform clinical trials have proven highly efficient in evaluating multiple treatments. The Randomized, Embedded, Multifactorial Adaptive Platform for Community-acquired Pneumonia (REMAP-CAP) [29], the Randomized Evaluation of COVID-19 Therapy (RECOVERY) [30], and the World Health Organization SOLIDARITY trial [31] have generated high-quality data on a spectrum of therapeutics within relatively a short period.
However, there were multiple challenges, especially during the first wave of COVID-19 pandemic. A large number of trials that could not be completed or were underpowered, duplicated, or of poor quality. Conduction of clinical trials, in many parts of the world, was complicated by lengthy regulatory rules and bureaucracy. A small percentage of eligible patients have been enrolled in clinical trials while large numbers of patients have been treated with off-label, unproven therapies. There was an “infodemic” of low-quality medical information, amplified by social media.
PATIENTS OUTCOMES DURING COVID-19 SURGES
In many ICUs, the response to the COVID-19 surges required almost doubling ICU bed capacity and changing multiple aspects of ICU workflow [32▪]. Mortality for critically ill patients with COVID-19 seems to be associated with the extent of ICU burden. A study in 88 Veteran Affairs hospitals evaluating ICU load and demand as measures of COVID-19 critical care strain found an adjusted hazard ratio for mortality of 1.94 (95% confidence interval of 1.46−2.59) when demand was >75−100% [33▪▪]. The effects of COVID-19 surges on patient outcomes were evaluated in 144 116 in-patients with a surge index to capture the quantitative and volume-outcome relationship [34]. Mortality risk increased with escalating severity-weighted COVID-19 caseload with approximately one in every four COVID-19 deaths potentially attributable to surges. In another multicenter study, admissions during times of surge were associated with 21−49% increased odds of death [35]. The percentage of hospital beds occupied by COVID-19 patients was independently and inversely associated with survival during the early COVID-19 pandemic in a retrospective study [36]. Hospitals performed better when the prevalence of COVID-19 in their surrounding communities was lower, possibly by not being overwhelmed [37]. Nonetheless, the odds of being discharged alive increased over time suggesting a learning curve [37,38▪,39].
Based on data from the delta surge in the US, a regression model predicted that if ICU bed use nationwide reached 75% or exceeded 100% of ICU bed capacity, an estimated 12 000 and 80 000 excess deaths, respectively, would occur nationally over the following 2 weeks [40▪▪]. During the shutdown periods, the delivery of hospital services, ICU utilization and outcomes changed significantly. Increase in in-hospital mortality was recorded in six capitals within the Brazilian Unified Health System with the pandemic, including or excluding COVID-19 hospitalizations [41]. A large cohort study on the impact of pandemic on outcomes of non-COVID-19 patients admitted to 165 Brazilian ICUs demonstrated a reversal of the trend toward a decrease in overall and risk-adjusted mortality consistently observed between 2011 and 2020 that coincided with the beginning of COVID-19 pandemic [42▪▪].
LESSONS LEARNED
There is insufficient evidence on the impact of critical sector's preparedness for pandemics; nonetheless countries with more recent prior experiences with public health crises were better prepared to implement effective responses to COVID-19 threat [43]. Learning from our responses will help ICUs to be more resilient to confront future health crises. We learned from this pandemic that the biggest challenge was the inequity of access to an adequately equipped and staffed ICU bed. Developing contingency plans that anticipate how to gain immediate access to additional staff and hospital areas while providing stress management and resilience trainings for the frontline workers must be among the priorities [44]. Optimization and diversification for biomedical supplies and equipment as well as preparedness at all levels of supply chain might prevent or mitigate shortages. Institutions, policymakers and governments must do all they can to prevent the scarcity of resources. Coordination all levels of government as well as between public and private services is essential to this end [43]. If resources do become scarce, triage guidelines can alleviate system burden and ensure equal treatment [45,46]. At the same time, the pace of surges must be controlled in the community by flattening the curve as no healthcare system can sustain uncontrolled outbreaks without significantly exceeding its total ICU capacity with major human lives costs [47]. Transparent local metrics and benchmarking are important to driving changes in contingency plans.
Strategies for rapid and effective communication are of utmost importance to sustain the response for the duration of the pandemic while maintaining standard of care. The COVID-19 pandemic has emphasized the importance of the rapid implementation of well designed clinical trials with more representation of low-income countries. We have learned that interventions without evidence should be avoided for their potential to harm and rather rapidly learn, share and adaptively apply the best stand of care and evidence-based treatments.
CONCLUSION
The COVID-19 pandemic has posed great challenges to ICUs involving ICU staffing, ICU space and equipment, communication, technology, research and knowledge dissemination. Although healthcare systems learned how to face some of the challenges with subsequent waves, the pandemic had persistent effects on healthcare systems.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
Y.A. is an investigator on the REMAP-CAP trial and is a board member of the International Severe Acute Respiratory and emerging Infection Consortium (ISARIC).
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.French G, Hulse M, Nguyen D, et al. Impact of hospital strain on excess deaths during the COVID-19 pandemic − United States, July 2020−July 2021. MMWR Morbid Mortal wkly Rep 2021; 70:1613–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2▪▪.Greco M, De Corte T, Ercole A, et al. Clinical and organizational factors associated with mortality during the peak of first COVID-19 wave: the global UNITE-COVID study. Intensive Care Med 2022; 48:690–705. [DOI] [PMC free article] [PubMed] [Google Scholar]; This was multicenter, international, point prevalence study of adult patients with COVID-19 admitted to ICUs between February 15th and May 15th, 2020. 4994 patients from 280 ICUs in 46 countries were included. The study demonstrated that ICUs increased their total capacity from 4931 to 7630 beds, deploying personnel from other areas. Overall, 1986 (39.8%) patients were admitted to surge capacity beds. In this study, admission to surge capacity beds was not associated with mortality, even after controlling for other factors. Older age, invasive mechanical ventilation, and AKI were identified as the strongest predictors of mortality.
- 3▪.Kerlin MP, Costa DK, Davis BS, et al. Actions taken by US hospitals to prepare for increased demand for intensive care during the first wave of COVID-19: a national survey. Chest 2021; 160:519–528. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study evaluated what actions did US hospitals take to prepare for a potential surge in demand for critical care services in the context of the COVID-19 pandemic.
- 4.Vranas KC, Golden SE, Mathews KS, et al. The influence of the COVID-19 pandemic on ICU organization, care processes, and frontline clinician experiences: a qualitative study. Chest 2021; 160:1714–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathews KS, Seitz KP, Vranas KC, et al. Variation in initial U.S. hospital responses to the coronavirus disease 2019 pandemic. Crit Care Med 2021; 49:1038–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dichter JR, Devereaux AV, Sprung CL, et al. Mass critical care surge response during COVID-19: implementation of contingency strategies − a preliminary report of findings from the task force for mass critical care. Chest 2022; 161:429–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. The impact of COVID-19 on health and care workers: a closer look at deaths. Geneva: World Health Organization; 2021. [Google Scholar]
- 8▪▪.Azoulay E, Pochard F, Reignier J, et al. Symptoms of mental health disorders in critical care physicians facing the second COVID-19 wave: a cross-sectional study. Chest 2021; 160:944–955. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this cross-sectional study of 1203 healthcare providers, 845 responded (70%) (66% nursing staff, 32% medical staff, 2% other professionals); 487 (57.6%) had treated more than 10 new patients with COVID-19 in the previous week. Insomnia affected 320 (37.9%), and 7.7% were taking a psychotropic drug daily. Symptoms of anxiety, depression, posttraumatic stress disorder, and burnout were reported in 60.0% (95% CI, 56.6−63.3%), 36.1% (95% CI, 32.9−39.5%), 28.4% (95% CI, 25.4−31.6%), and 45.1% (95% CI, 41.7−48.5%) of respondents, respectively.
- 9.Azoulay E, Cariou A, Bruneel F, et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19. A cross-sectional study. Am J Respir Crit Care Med 2020; 202:1388–1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berkhout SG, Sheehan KA, Abbey SE. Individual- and institutional-level concerns of healthcare workers in Canada during the COVID-19 pandemic: a qualitative analysis. JAMA Netw Open 2021; 4:e2118425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ranney ML, Griffeth V, Jha AK. Critical supply shortages − the need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med 2020; 382:e41. [DOI] [PubMed] [Google Scholar]
- 12.Communicating during an outbreak or public health investigation. Available at: https://www.cdc.gov/eis/field-epi-manual/chapters/Communicating-Investigation.html [Accessed 23 June 2022]. [Google Scholar]
- 13.Reddy BV, Gupta A. Importance of effective communication during COVID-19 infodemic. J Fam Med Prim Care 2020; 9:3793–3796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robert R, Kentish-Barnes N, Boyer A, et al. Ethical dilemmas due to the COVID-19 pandemic. Ann Intensive Care 2020; 10:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hart JL, Oppenheim TA, Courtright KR IM. Family-centered care during the COVID-19 era. J Pain Symptom Manage 2020; 60:e93–e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azoulay E, Kentish-Barnes N. A 5-point strategy for improved connection with relatives of critically ill patients with COVID-19. Lancet Respir Med 2020; 8:e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azoulay E, De Waele J, Ferrer R, et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care 2020; 10:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehraeen E, Mehrtak M, SeyedAlinaghi S, et al. Technology in the era of COVID-19: a systematic review of current evidence. Infect Disord Drug Targets 2022; 22:e240322202551. [DOI] [PubMed] [Google Scholar]
- 19.Arabi YM, Azoulay E, Al-Dorzi HM, et al. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med 2021; 47:282–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Michard F, Saugel B, Vallet B. Rethinking the post-COVID-19 pandemic hospital: more ICU beds or smart monitoring on the wards? Intensive Care Med 2020; 46:1792–1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu R, Sundaresan T, Reed ME, et al. Telehealth in oncology during the COVID-19 outbreak: bringing the house call back virtually. JCO Oncol Pract 2020; 16:289–293. [DOI] [PubMed] [Google Scholar]
- 22.Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26:309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23▪.Garfan S, Alamoodi AH, Zaidan BB, et al. Telehealth utilization during the COVID-19 pandemic: a systematic review. Comput Biol Med 2021; 138:104878. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a systematic review of telehealth utilization during COVID-19. The paper addresses challenges, motivations and recommended solutions are identified for telehealth and describes different applications of telehealth during the COVID-19 pandemic.
- 24.Shanbehzadeh M, Kazemi-Arpanahi H, Kalkhajeh SG, Basati G. Systematic review on telemedicine platforms in lockdown periods: lessons learned from the COVID-19 pandemic. J Educ Health Promot 2021; 10:211–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hagana A, Behranwala R, Aojula N, Houbby N. Digitalising medical education: virtual ward rounds during COVID-19 and beyond. BMJ Simul Technol Enhanc Learn 2021; 7:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pennell CE, Kluckow H, Chen SQ, et al. Live-streamed ward rounds: a tool for clinical teaching during the COVID-19 pandemic. Med J Aust 2020; 213:306–308. e301. [DOI] [PubMed] [Google Scholar]
- 27.Berry SM, Connor JT, Lewis RJ. The platform trial: an efficient strategy for evaluating multiple treatments. JAMA 2015; 313:1619–1620. [DOI] [PubMed] [Google Scholar]
- 28.Reyes LF, Murthy S, Garcia-Gallo E, et al. Clinical characteristics, risk factors and outcomes in patients with severe COVID-19 registered in the International Severe Acute Respiratory and Emerging Infection Consortium WHO clinical characterisation protocol: a prospective, multinational, multicentre, observational study. ERJ Open Res 2022; 8:552–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Investigators REMAP-CAP, Bradbury CA, Lawler PR, et al. Effect of antiplatelet therapy on survival and organ support-free days in critically ill patients with COVID-19: a randomized clinical trial. JAMA 2022; 327:1247–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.RECOVERY Collaborative Group. Aspirin in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet 2022; 399:143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO Solidarity Trial Consortium. Remdesivir and three other drugs for hospitalised patients with COVID-19: final results of the WHO Solidarity randomised trial and updated meta-analyses. Lancet 2022; 399:1941–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32▪.Al-Dorzi HM, Aldawood AS, Almatrood A, et al. Managing critical care during COVID-19 pandemic: the experience of an ICU of a tertiary care hospital. J Infect Public Health 2021; 14:1635–1641. [DOI] [PMC free article] [PubMed] [Google Scholar]; This case study describes the response of an Intensive Care Department at a tertiary-care hospital to COVID-19 pandemic. The ICU response required almost doubling ICU bed capacity and changing multiple aspects of ICU workflow to be able to care for high numbers of affected patients.
- 33▪▪.Bravata DM, Perkins AJ, Myers LJ, et al. Association of intensive care unit patient load and demand with mortality rates in US Department of Veterans Affairs hospitals during the COVID-19 pandemic. JAMA Netw Open 2021; 4:e2034266. [DOI] [PMC free article] [PubMed] [Google Scholar]; The study evaluated whether greater coronavirus disease 2019 (COVID-19) intensive care unit (ICU) strain was associated with increased COVID-19 mortality. This was a cohort study of 8516 patients with COVID-19 admitted to 88 US Veterans Affairs hospitals. Patients with COVID-19 treated during periods of peak COVID-19 ICU demand had a nearly 2-fold increased risk of mortality compared with those treated during periods of low demand.
- 34.Kadri SS, Sun J, Lawandi A, et al. Association between caseload surge and COVID-19 survival in 558 U.S. hospitals, March to August 2020. Ann Intern Med 2021; 174:1240–1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keene AB, Admon AJ, Brenner SK, et al. Association of surge conditions with mortality among critically ill patients with COVID-19. J Intensive Care Med 2022; 37:500–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dale CR, Starcher RW, Chang SC, et al. Surge effects and survival to hospital discharge in critical care patients with COVID-19 during the early pandemic: a cohort study. Crit Care 2021; 25:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Asch DA, Sheils NE, Islam MN, et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med 2021; 181:471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38▪.Anesi GL, Jablonski J, Harhay MO, et al. Characteristics, outcomes, and trends of patients with COVID-19-related critical illness at a learning health system in the United States. Ann Intern Med 2021; 174:613–621. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated that among patients with COVID-19-related critical illness admitted to ICUs of a learning health system in the United States, mortality seemed to decrease over time.
- 39.Roth GA, Emmons-Bell S, Alger HM, et al. Trends in patient characteristics and COVID-19 in-hospital mortality in the United States during the COVID-19 pandemic. JAMA Netw Open 2021; 4:e218828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪▪.French G HM, Nguyen D, et al. Impact of hospital strain on excess deaths during the COVID-19 pandemic — United States, July 2020–July 2021. MMWR Morb Mortal Wkly Rep 2021; 70:1613–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study predicted, based on the conditions of hospital strain during July 2020–July 2021, which included the presence of SARS-CoV-2 B.1.617.2 (Delta) variant, that ICU bed use at 75% capacity is associated with an estimated additional 12,000 excess deaths 2 weeks later.
- 41.Portela MC, de Aguiar Pereira CC, Lima SML, et al. Patterns of hospital utilization in the Unified Health System in six Brazilian capitals: comparison between the year before and the first six first months of the COVID-19 pandemic. BMC Health Serv Res 2021; 21:976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42▪▪.Zampieri FG, Bastos LSL, Soares M, et al. The association of the COVID-19 pandemic and short-term outcomes of non-COVID-19 critically ill patients: an observational cohort study in Brazilian ICUs. Intensive Care Med 2021; 47:1440–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]; This large cohort study on the impact of pandemic on outcomes of non-COVID-19 patients admitted to 165 Brazilian ICUs demonstrated a reversal of the trend toward a decrease in overall and risk-adjusted mortality consistently observed between 2011 and 2020 that coincided with the beginning of COVID-19 pandemic.
- 43.Pearson C, Britt H, Schapiro L. Adapting healthcare delivery in response to COVID-19: international lessons for the United States (commonwealth fund, Sept. 2021). 2021. Available at: 10.26099/nr66-tn77. [DOI] [Google Scholar]
- 44.Wei EK, Long T, Katz MH. Nine lessons learned from the COVID-19 pandemic for improving hospital care and healthcare delivery. JAMA Intern Med 2021; 181:1161–1163. [DOI] [PubMed] [Google Scholar]
- 45.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med 2020; 382:2049–2055. [DOI] [PubMed] [Google Scholar]
- 46.Aziz S, Arabi YM, Alhazzani W, et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med 2020; 46:1303–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gilardino RE. Does “flattening the curve” affect critical care services delivery for COVID-19? A global health perspective. Int J Health Policy Manag 2020; 9:503–507. [DOI] [PMC free article] [PubMed] [Google Scholar]