Abstract
Background
Community-based Health Insurance (CBHI) is a voluntary prepayment mechanism that guarantees the provision of basic healthcare services without financial barriers to underserved segments of the population in developing countries. The Government of Ethiopia launched the CBHI program to protect the community from high out-of-pocket health expenditure and improve health service utilization a decade ago. However, to improve the quality of healthcare services delivery in health facilities and cover the changing costs of healthcare, the government should revise the contribution of the CBHI scheme. Therefore, we determined the willingness to pay for a CBHI scheme and associated factors among rural households of Lemu and Bilbilo district, South Central Ethiopia.
Methods
We conducted a community-based cross-sectional study design to assess willingness to pay for the CBHI scheme and its associated factors among households in Lemu and Bilbilo districts, South Central Ethiopia. We used a double bounded contingent valuation method to elicit households’ willingness to pay for the CBHI scheme. Data were coded, cleaned, entered into Statistical Package for Social Science (SPSS) version 25, and exported to STATA 16 for analysis. A logistic regression analysis was conducted to determine the presence of statistically significant associations between the willingness to pay for the CBHI scheme and independent variables at a p-value <0.05 and Adjusted odds ratio (AOR) values with 95% CI. Finally, we checked the fitness of the model using Hosmer and Lemeshow’s goodness-of-fit test.
Results
Of the 476 study participants, 82.9% (95% CI: 79.2%, 86.01%) were willing to pay for the CBHI scheme and only 62% of them can afford the average amount of 358.32ETB ($7.68) per household per annum. Primary education (AOR = 3.17; 95% CI: 1.74–5.80), secondary and above education (AOR = 4.13; 95% CI: 1.86–9.18), large family size (AOR = 2.75; 95% CI: 1.26–5.97), monthly income of 500-1000ETB (AOR = 3.75; 95% CI: 1.97–7.13) and distance to public health facilities (AOR = 2.14, 95% CI: 1.04–4.39 were significantly associated with willingness to pay for the CBHI scheme.
Conclusion
In this study, around 83% of respondents were willing to pay for the CBHI and meet the government expectation for 2020. The study also revealed that educational status, family size, monthly income, and distance from the health facilities were significant factors associated with WTP for the CBHI scheme. In addition, we found that a large number of the respondents couldn’t afford the average amount of money that the participants were willing to pay for the CBHI scheme. So, the government should consider the economic status of the communities while revising the CBHI scheme premium not to miss those who cannot afford the contribution.
Introduction
Financial protection during obtaining health care services is an important dimension of universal health coverage (UHC) [1–3]. However, the proportion of catastrophic health expenditure increased by 5.3% at a 25% threshold until 2015, from 100 million people to about 200 million people every year [2]. Despite the availability of prepayment mechanisms, out-of-pocket payment (OOP) remained the major means of financing the health system in low and middle-income countries (LMIC) [4]. In sub-Saharan African countries, OOP accounted for 40% of total health expenditures and exposed a significant number of communities to financial burdens that limit access to healthcare services at the point of service delivery [5]. Besides, high OOP, poor quality of healthcare services at public facilities, and low coverage of prepayment means were the major challenges of the health system of Ethiopia for a decade [6, 7]. In Ethiopia, OOP expenditures constitute 34% of total health expenditures and exposed a huge financial hardship to communities for a decade [8]. But the WHO recommends moving away from direct OOP to prepayment means and pool risks through health care financing strategies to mobilize resources for health [1]. In addition, there is an increased advocacy for the CBHI schemes as a viable option for catastrophic health expenditure in LMIC for a decade [9]. Currently, CBHI is a widely known prepayment mechanism in LMIC including Ethiopia. It helps communities to manage their healthcare costs and provides access to equitable healthcare services for the poor and other vulnerable groups [4, 10]. The government of Ethiopia has launched the CBHI program a decade ago with a nominal contribution from households, and it is highly subsidized by the government. The introduction of the CBHI scheme in the health financing reforms of 2005 generated a remarkable change in the public health facilities [11, 12].
After the reform, the introduction of the CBHI scheme has reduced catastrophic OOP expenditure, increased health care utilization, availability of drugs, and quality of services through retaining mobilized resources at health facilities [12–15]. For instance, in North-west Ethiopia, around 50.5% of insured households utilized healthcare services from public health facilities when compared to non-insured individuals (29.3%) [16]. Besides, according to the Federal Ministry of Health report during the evaluation of the CBHI scheme in piloted districts, 72.3% of the CBHI scheme members have visited health facilities [11]. Moreover, studies in Ethiopia revealed that the implementation of the CBHI scheme has reduced catastrophic health expenditure by 23.2%, increased the annual outpatient visits by 111%, and annual revenues of the facilities by 47% [10, 17, 18]. Even though the government of Ethiopia proposed to enroll more than 80% of households in the CBHI scheme by 2020, there is still a low enrollment rate in the program [11]. Currently, the households uptake of the CBHI scheme was 73%, in West Arsi zone [19], 78%, in Bench Maji zone [20], and 12.8% in Sidama Zone [21]. In addition, previous studies found that 74.8% of residents in Gemmachis district [22], 83.9% of households in Bugna district [23], and 90% of households in Jimma Zone [24] were willing to pay for the CBHI scheme. The previous findings reported that households’ willingness to pay (WTP), renew their CBHI membership, and enroll in the CBHI program depends on the affordability of premium, quality of care, waiting time to get services, and availability of basic logistics and supplies in health facilities [21, 25–28]. But to improve the quality of healthcare services in health facilities and cover the changing costs of healthcare, the government should revise the contribution of the CBHI scheme. Currently, as the previous CBHI scheme contribution and 25% government subsidies for all members were inadequate to cover the costs of healthcare services, the government of Ethiopia has revised the scheme premium from 240 Ethiopian Birr (ETB) to 410 ETB per household per annum [13]. Additionally, households’ WTP for the projected CBHI scheme played a crucial role in achieving the UHC and delivering high-quality healthcare services despite budget cuts and institutional challenges [29]. Therefore, we determined the willingness to pay for the CBHI scheme and associated factors among rural households of Lemu and Bilbilo district, South Central Ethiopia.
Method and material
Study setting, design, and period
This community-based cross-sectional study was conducted in Lemu and Bilbilo districts, South Central Ethiopia from September 10–30, 2021. Lemu and Bilbilo districts have 32 kebele (the smallest administrative unit) with a total population of 180,695 (89,352 men and 91,343 women) according to a 2007 Ethiopian center statistical agency report. Lemu and Bilbilo district is located 175 km from Addis Ababa, the capital city of Ethiopia, and 56 km from Asella, the zonal town of the Arsi zone. It is bordered on the South by the Hasasa district, on the West by Munesa District, on the North by Digelu and Tijo district, and on the East by the Shirka district. Besides, the district has 7 health centers and one primary hospital, which serves around 250,000 communities in nearby districts.
Study population and eligibility criteria
All rural households in Lemu and Bilbilo districts who were not a member of the CBHI scheme were the source population, whereas all households in the randomly selected kebele were the study population. The heads of households (i.e. Mother/Father) that have stayed for more than six months in the selected kebele and who were aged 18 and above years old were included in the study. We considered heads of the households primarily for interviews from the selected households and interviewed the senior adults aged 18 and above where the households’ headswere not available. Respondents who were government workers or who were unable to respond due to their health conditionswere excluded from the study.
Sample size determination and sampling technique procedure
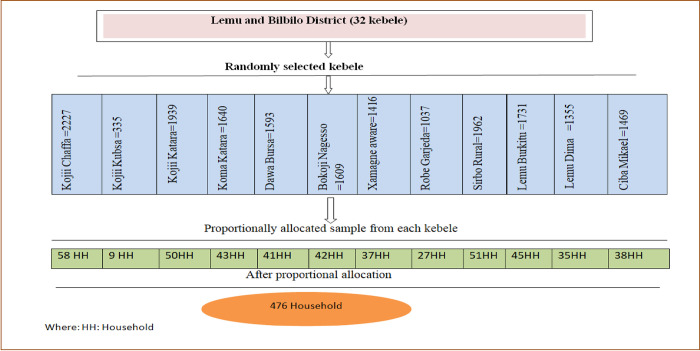
We calculated a sample size of 476 using a single population proportion formula, taking the proportion of households WTP for the CBHI scheme (P = 74.8%) [22], 95% level of confidence, 5% marginal error, considering a design effect of 1.5 and an anticipated non-response rate of 10%. We used a two-stage sampling technique to recruit the participating households. In the first stage, we selected Lemu and Bilbilo districts from the Arsi zone as the district had a high number of households that didn’t uptake the CBHI scheme and planned to improve the CBHI scheme enrollment rate. In the second stage, we randomly selected twelve kebele out of thirty-two kebele and allocated proportionally to each kebele using the number of households residing in that administrative unit (Fig 1). A systematic random sampling method was employed to recruit the participants after we prepared a sampling frame based on the current enrollment status of the CBHI scheme.
Fig 1. Number of sample sizes from selected kebele in Lemu and Bilbilo district, South-Central, Ethiopia, 2021.
Variables of the study
Willingness to pay for the CBHI scheme among households in the Lemu and Bilbilo districts was the dependent variable, while factors such as socio-demographic (age, sex, family size, and marital status), socioeconomic variables (monthly income, occupation, and education status), health and health-care utilization (illness experience within the past three months, chronic illness and distance to health facilities) and awareness about the CBHI scheme were independent variables.
Operational definition
Willingness to pay for the CBHI scheme
Was defined as the maximum (non-zero) amount that households heads are willing to pay for the community-based health insurance scheme, assessed using a double bounded contingent valuation method through applying a bidding game.
Benefits package
Was defined as the type of healthcare services provided or covered by the CBHI scheme for all eligible members of the households that had enrolled in the CBHI scheme.
Route of access to health facilities
Was also defined as the process through which the member of the CBHI scheme should pass to get services from high-level health facilities if other facilities existed nearby to their residential area.
Data collection procedures and quality management
We used a pre-tested, semi-structured, interviewer-administered questionnaire to collect data from participants from September 10th to 30th, 2021. The questionnaire was adapted from previous studies [22, 24], translated into Afan Oromo, and retranslated back into English by language experts. The questionnaire comprises socio-demographic and economic characteristics, health and healthcare utilization-related factors, awareness and perception about the CBHI scheme, and WTP for the CBHI scheme. We collected data using four trained health professionals experts who were fluent speakers of the local language. We described the hypothetical CBHI scheme in detail to the respondent including the benefits package, the criteria for membership, the potential benefits, and the terms of conditions before assessing their WTP. Thereafter the respondents were asked for their WTP for the proposed CBHI using the dichotomous choice Contingent Valuation Method (CVM). Those participants who responded “no” to the dichotomous CMV were asked for the reasons why they were refused to pay for the CBHI scheme. However, if the respondent’s response was “yes” to the dichotomous choice CVM, the bidding game was employed to ascertain the premium each respondent would willing to pay for the hypothetical scheme. In the bidding game, the respondents were asked if they would pay an initial bid amount (410 ETB) and probed the questions depending on their response to this bid. If the study participants agreed to pay the initial bid (410ETB), the interviewer would raise the bid amount to 450ETB and again question their WTP. Next, if the respondents agreed to pay for the first higher bid, the interviewer would raise the bid amount to 500ETB andagain question their WTP. Finally, if the respondents still agreed to pay for the bid, they were asked to indicate the maximum amount that they would be willing to pay using open CVM. However, if the respondent expressed unwillingness to pay the initial bid, the interviewer would lower the bid amount (350 ETB) and again question their WTP. In case the study participants disagreed to pay the first lowered bid, the interviewer would lower the bid (300ETB) andrepeat the inquiry. Lastly, if the participants still expressed unwillingness to pay for the second lowered bid, they were asked to state the maximum amount that they were willing to pay using open CVM. The principal investigator monitored and supervised the overall data collection activities and checked for completeness and consistency of data daily.
Data analysis
The collected data were entered into SPSS version 25 and exported to STATA 16 for analysis. We utilized descriptive statistics such as frequencies and percentages for categorical variables whereas mean with standard deviation (SD) was used for summarizing continuous variables. All variables with a p-value ≤0.25 in the bivariate logistic regression analysis were fitted to a multivariate logistic regression model to determine their association with the WTP for the CBHI scheme. Odds ratios with a 95% confidence interval (CI) and a P-value less than 0.05 were reported to determine the associations between independent variablesand WTP for the CBHI scheme. Finally, the fitness of the model was assessed by using Hosmer and Lemeshow’s goodness-of-fit test.
Ethical consideration
We obtained Ethical clearance from the Institutional Review Board of Paradise Valley University College (Ref.no.pvuc/1021/2021). We also obtained informed written consent from respondents before interviewing by explaining the purpose of the study. We assured the confidentiality of the participants’ information using a coding system and by removing any potential personal identifiers.
Result
Socio-demographic characteristics of the respondents
Out of the 476 study participants, 473 were included in the study with a response rate of 99.4%. Among 473 respondents, 384 (81.2%) were males and 269 (56.9%) of them were in the age category of 30–44 years old. A majority (39.5%) of the respondents attended primary education, 411 (86.9%) were married, 441 (93.2%) were Oromo by ethnicity, and 328 (69.3%) were Orthodox religious followers. More than three-fifths (67.4%) of the respondents had a family size of less than or equal to five (Table 1).
Table 1. Sociodemographic characteristics of respondents in South Central, Ethiopia, 2021.
| Variables | Categories | Frequency (%) |
|---|---|---|
| Sex | Male | 384 (81.2) |
| Female | 89 (18.8) | |
| Age | 18–29 years | 127 (26.8) |
| 30–44 years | 269 (56.9) | |
| Above 44 years | 77 (16.3) | |
| Marital status | Married | 411 (86.9) |
| Others a | 62 (13.1) | |
| Religion | Muslim | 115 (24.3%) |
| Orthodox | 328 (69.3%) | |
| Other b | 30 (6.4%) | |
| Education | Non-formal | 195 (41.2) |
| Primary | 187 (39.5) | |
| Secondary | 91 (19.2) | |
| Ethnicity | Oromo | 441 (93.2) |
| Other c | 32 (6.8) | |
| Occupation | farmer | 322 (68.1) |
| Merchants | 66 (14) | |
| Others d | 85 (18) | |
| Monthly income | <500 birr | 115 (24.3) |
| 500–1000 birr | 212 (44.8) | |
| above 1000 birr | 146 (30.9) | |
| Family size | ≤ 5 | 319 (67.4) |
| >5 | 154 (32.6) |
Note
a = widowed/divorced
b = Protestant, Catholic, Wakefta
c = Amhara, Gurage
d = daily labor, housewife
Accesses to care and health-seeking behavior of respondents
Out of 473 study participants, 49 (10.4%) had chronic illnesses and 111 (23.5%) of them had experienced illnesses in the last three months. Among those who encountered illnesses in the last three months, 103 (92.8%) sought medical treatment whereas 8 (7.2%) of them didn’t seek treatment due to the difficulty of covering the cost of medical treatment. A majority (87.7%) of the respondents reside at a distance of below 11km from nearby public health facilities (Table 2).
Table 2. Healthcare characteristics of respondents in Lemu and Bilbilo Woreda, 2021.
| Variables | Categories | Frequency (%) |
|---|---|---|
| Chronic illness | Yes | 49 (10.4) |
| No | 424 (89.6) | |
| Experienced illness in the last three months | Yes | 111 (23.5) |
| No | 362 (76.5) | |
| Seek treatment | Yes | 103 (92.8) |
| No | 8 (7.2) | |
| Place of treatment | Private clinic | 20 (19.4%) |
| Government health center | 49 (47.6%) | |
| Government hospital | 34 (33%) | |
| Distance from public health facility | ≤ 10km | 415 (87.7) |
| >10km | 58 (12.3) |
Resident’s knowledge about community based health insurance scheme
Regarding respondents’ awareness of the CBHI scheme, 369 (78%) of them heard about the CBHI scheme whereas 237 (64.2%), 199 (53.9%), and 273 (74%) of the participants knew about the benefit packages, route of access and principle of the CBHI scheme. Of those who heard about the CBHI scheme, 200 (54.2%) of them reported health workers as a source of information while 72 (19.5%) of the respondents got information from family members and friends (Table 3).
Table 3. Respondents’ knowledge of a community-based health insurance scheme.
| Variables | Categories | Frequency (%) |
|---|---|---|
| Heard about the CBHI scheme | No | 104 (22%) |
| Yes | 369 (78%) | |
| Source of information | Health workers | 200 (54.2%) |
| Radio and TV | 73 (19.8%) | |
| Family and friends | 72 (19.5%) | |
| Other | 24 (6.5%) | |
| Know benefit package | Yes | 237 (64.2%) |
| No | 132 (35.8%) | |
| Know Principles of CBHI | Yes | 273 (74.0%) |
| No | 96 (26.0%) | |
| Know the route of access | Yes | 199 (53.9%) |
| No | 170 (46.1%) |
Respondent’s perception of community-based health insurance scheme
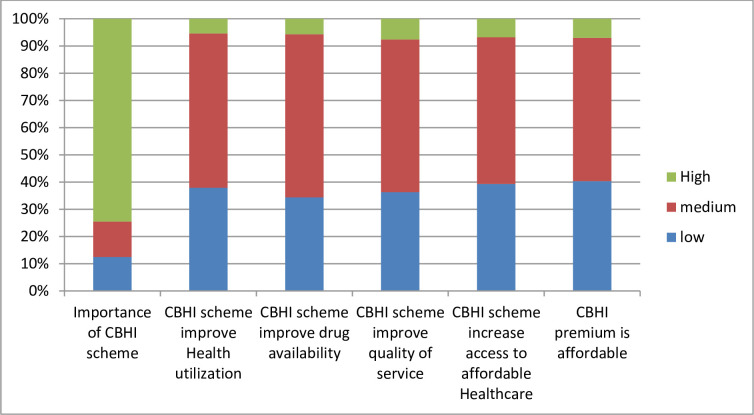
Around 275 (74.5%) respondents think that the CBHI scheme has high importance whereas 194 (52.6%) of them perceived that the potential of affordability of the current CBHI premium was medium. The perceived potential of the CBHI scheme to increase access to affordable healthcare was medium among 199 (53.9%) of participants. Moreover, around 56.6% and 59.9% of respondents perceived the potential of the CBHI scheme to improve the healthcare utilization and drug availability as a medium respectively. Besides, the perception of households towards the potential of the CBHI scheme to improve the quality of health services was medium in 56.1% of the participants (Fig 2).
Fig 2. Respondents’ perception towards community based health insurance scheme, 2021.
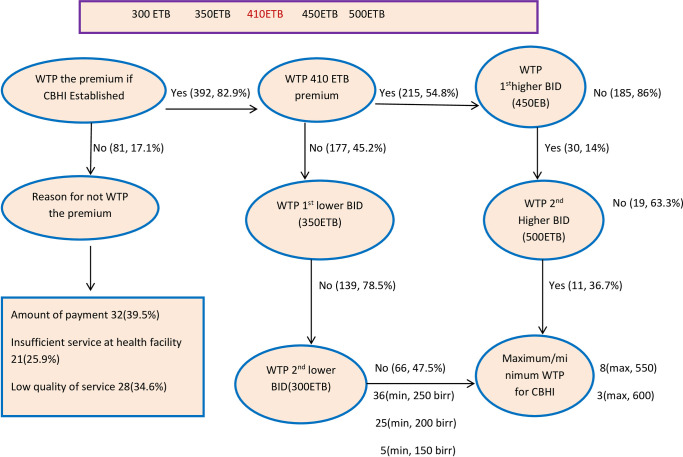
Willingness to pay for the community based health insurance scheme
Of the 473 study participants, 82.9% (95% CI: 79%, 85.9%) of them were willing to pay for the proposed community-based health insurance scheme. The mean (SD) amount of contribution the respondents were willing to pay per household per annum was 358.32 (82.13) ETB or (7.68USD) [30]. Out of 392 study participants, 215 (54.8%) of them were willing to pay the national stated premium of 410 ETB (8.78USD). Additionally, of the respondents who were willing to pay the initial bid, 30 (14%) of them were also prepared to pay the first higher bid of 450ETB (9.64USD), and 11 (36.7%) of those who were willing to pay the first higher bid were also willing to pay the 500ETB (10.71USD) bidding amount. Besides, out of the participants who were not willing to pay the initial bid, 139 (78.5%) of them were not willing to pay the lower bid of 350ETB (7.49USD) whereas 66 (47.5%) of those who were not willing to pay the first lower bid were also not willing to pay the second lower bid of 300ETB (6.42USD) bidding amount. Out of 81 study participants who were not willing to pay for the CBHI scheme; 32 (39.5%), 21 (25.9%), and 28 (34.6%) of them were not willing to pay due to amount of payment, insufficient services, and poor perceived quality of healthcare at public health facilities respectively (Fig 3).
Fig 3. Participants’ willingness to pay for community based health insurance scheme, 2021.
Respondents’ ability to pay for the annual CBHI premium
To calculate the respondent’s ability to pay the WTP amount of 358.32ETB, the health expenditure-income ratio technique was employed. Based on data from developing countries, we used a 5% health expenditure-to-income ratio, which suggests that a household that spends less than 5% of their income does not push into poverty because of healthcare costs [31–33]. Using this approach, we found that only 62% of the study participant could afford to pay for the CBHI scheme premium (Table 4).
Table 4. Respondents’ ability to pay for the annual CBHI premium using expenditure to the income approach.
| <5% of household income | ≥5% of household income | |
|---|---|---|
| Frequency | 243 | 149 |
| Percentage | 62.0% | 38.0% |
Factors associated with respondents’ willingness to pay for CBHI scheme
We found age, marital status, sex, educational status, occupation, family size, monthly income, experiences of an illness in the last three months and distance to the health facilities were eligible for multivariate logistic regression analysis (p-value of <0.25). In multivariate logistic regression, family size, monthly income, distance from public health facilities, and educational status of the respondents remained to have an association with WTP for the CBHI scheme. The odds of willingness to pay for the CBHI scheme among families who had a family member of greater than five was almost 3 times higher than a family member of five or less (AOR = 2.75; 95% CI: 1.26–5.97). In addition, those respondents who attended primary and above education were almost 3 times more likely to pay for the CBHI scheme than those who had informal education (AOR = 3.17; 95% CI: 1.74–5.80). Besides, the odds of willingness to pay for the CBHI scheme among individuals who had secondary and above education were 4.13 times higher than those with no formal education (AOR = 4.13; 95% CI: 1.86–9.18). Participants who had a monthly income of 500-1000ETB were almost four times more likely to pay for the CBHI scheme compared to those who had a monthly income of less than 500 ETB (AOR = 3.75; 95% CI: 1.97–7.13). Similarly, the odds of willingness to pay for the CBHI scheme among respondents who live at a distance of less than 11km from public health facilities were almost 2 times higher than those who live at a distance of 11km and above from health facilities (AOR = 2.14, 95% CI: 1.04–4.39) (Table 5).
Table 5. Factors associated with respondents’ Willingness to pay for CBHI scheme, 2021.
| Categories | Willingness to pay | COR(95%CI) | AOR(95%CI) | |
|---|---|---|---|---|
| Yes (%) | No (%) | |||
| Age categories | ||||
| 18–29 years | 101 (79.5) | 26 (20.5) | 1 | 1 |
| 30–44 years | 225 (83.6) | 44 (16.4) | 1.35 (.79, 2.29) | 1.42 (.75, 2.70) |
| Above 44 years | 66 (85.7) | 11 (14.3) | 1.62 (0.75, 3.49) | 0.95 (0.31, 2.95) |
| Marital status | ||||
| Married | 338 (82.2) | 73 (17.8) | 1 | 1 |
| Other | 54 (87.1) | 8 (12.9) | 1.51 (0.69,3.30) | 1.29 (0.52,3.18) |
| Sex | ||||
| Male | 315 (82) | 69 (18) | 0.69 (0.36,1.33) | 0.77 (0.33,1.83) |
| female | 77 (86.5) | 12 (13.5) | 1 | 1 |
| educational status | ||||
| Non-formal | 149 (76.4) | 46 (23.6) | 1 | 1 |
| Primary | 163 (87.2) | 24 (12.8) | 2.06 (1.21, 3.51) | 3.17 (1.74, 5.80)* |
| Secondary and above | 80 (87.9) | 11 (12.1) | 2.31 (1.14, 4.70) | 4.13 (1.86, 9.18)* |
| Occupational status | ||||
| Farmer | 268 (83.2) | 54 (16.8) | 1 | 1 |
| merchant | 53 (80.3) | 13 (19.7) | 0.86 (0.44,1.68) | 1.06 (0.46,2.45) |
| Other | 71 (83.5) | 14 (16.5) | 1.07 (0.56,2.03) | 1.25 (0.52,3.05) |
| Monthly income | ||||
| Less than 500 birr | 84 (73) | 31 (27) | 1 | 1 |
| 500–1000 birr | 190 (89.6) | 22 (10.4) | 3.48 (1.91,6.32) | 3.75 (1.97,7.13)* |
| Above 1000 birr | 118 (80.8) | 28 (19.2) | 1.7 (0.95,3.02) | 1.66 (0.81,3.41) |
| Distance to Health facility | ||||
| ≤10km | 349 (84.1) | 66 (15.9) | 1.78 (0.94,3.39) | 2.14 (1.04,4.39)* |
| >10km | 43 (74.1) | 15 (25.9) | 1 | 1 |
| Family size | ||||
| ≤ 5 | 256 (20.2) | 63 (19.8) | 1 | 1 |
| > 5 | 136 (88.3) | 18 (11.7) | 1.94 (1.10,3.39) | 2.75 (1.26,5.97)* |
| Illness in last 3 months | ||||
| Yes | 91 (82) | 20 (18) | 1.22 (0.71,2.10) | 0.75 (0.42,1.34) |
| No | 301 (83.1) | 61 (16.9) | 1 | 1 |
Note
* p-value < 0.05
Discussion
The Ethiopian health care system is under tremendous reform to protect its citizens from catastrophic out-of-pocket health expenditure by introducing voluntary health insurance [12]. The overall aim of this study was to determine WTP for the CBHI scheme and associated factors among households in the Lemu and Bilbilo districts of Ethiopia. In this study, we found that 82.9% of the participants were willing to pay for the CBHI scheme. This finding is almost comparable with the study done in Nigeria,82% [34], Kewiot and EfratanaGedem districts, 79% [35], and Oromia Region,83.9% [36]. However, it is less than studies done in Bangladesh, 86.7% [37], Jimma Zone, 90% [24], and higher than studies in Pakistan, 64% [38], Nepal, 71.3% [39], Nigeria,74.52% [40], Bugna district,77.8% [23] and Gemmachis district, 74.8% [22]. This variation might be due to differences in the sample size, study period, socioeconomic status, and level of awareness of the participants towards the CBHI scheme. The affordability of the CBHI scheme premium had a significant influence on households’ enrolment and retention in the scheme [27, 31, 41–43]. In this study, we found that only 62% of respondents have ability to pay (ATP) the average amount of money that the participants were willing to pay for the CBHI scheme. The implication of low level of ATP of respondents despite high WTP is that there is uncertainty in improving the coverage of the schemes and attaining the goal of UHC unless there is external financial support. Therefore, the government should consider involvement of domestic donors and small microfinance in subsidising the CBHI scheme premiums as observed in other African countries [44–46]. Besides, the government should improve domestic resource mobilization to subsidize the premium so as to allow the some segment of communities to enroll in the scheme without facing further financial hardship. In addition, the mean amounts of money participants were willing to pay was 358.32ETB ($7.68) per household per annum. This is consistent with the currently proposed payment of 8.53USD [47], a study in Gemmachis district, $7.76 [22], and Jimma Zone, $8.27 [24]. However, it is higher than report from Fogera district of Ethiopia,$1.95 [48] and lower than studies from Saudi Arabia, $13.33 [49], Nigeria, $20.4 [50], Cameron, 103.44$ [51], Bugna district, $11.12 [23], Amhara Region, $10.5 [35] and Oromia Region, $17.9 [36]. The discrepancy might be due to the difference in the study period, economic growth, and socioeconomic status of study participants.
We found that study participants with large family members were more likely to pay for the CBHI scheme than those with few family members. This finding was supported by the study conducted in Nigeria [34, 52], Saudi Arabia [49], Bugna district, Ethiopia [23], Amhara Region, Ethiopia [35], and Jimma zone, Ethiopia [24]. This possible explanation might be households with large family members suffer from financial risks due to unanticipated illnesses, particularly in low-income families. So, they might have chosen to pay for the CBHI scheme to avoid the risk of catastrophic OOP health expenditure during the time of illness. The probability of willingness to pay for the CBHI scheme was higher among respondents who were more educated than those who had no formal education. This finding was supported by the study conducted in Bangladesh [37], Nigeria [50], Fogera District [48], and Gemmachis district, Ethiopia [22]. This could be because those individuals with better educational levels might have a better understanding of the concepts, benefits package, and principles of the CBHI scheme, which can ease their decision to pay for the scheme. In addition, educated respondents have a better awareness of the benefit of making regular insurance payments to avoid the risk of catastrophic healthcare expenditures at the time of unpredictable illness.
We found that respondents’ monthly income had a significant association with WTP for the CBHI scheme. Those individuals who had high monthly income were more likely to pay for the CBHI scheme than those who had low monthly income (less than 500ETB). This finding is similar with studies done in Malaysia [53], India [54], Pakistan [38], Bangladesh [37], Cameron [51], and Sierra Leone [55]. This could be because respondents with high income might have enough resources to pay for the requested CBHI scheme premium to protect their family members from unpredictable illnesses [24, 38]. We found that the distance respondents reside from the public facility had a significant effect on WTP for the CBHI scheme. The odds of willingness to pay for the CBHI scheme were almost 2 times higher among those who reside at a distance of less than 11kilometres from nearby health facilities than their counterparts. This finding was supported by the study conducted in Bangladesh [42], Nigeria [52], and Eastern Ethiopia [22]. The possible reason might be those respondents who were very close to the health facilities have less travel time and non-medical costs such as transportation, and food expenses and are more likely the use healthcare service. Even though our study had a high response rate, it has a few drawbacks. First, the use of dichotomous double bounded CVM to assess the WTP for the CBHI scheme might not indicate the actual contribution that the respondents can pay for the proposed CBHI scheme based on their own choice. Second, a significant number of study participants have no awareness ofthe route of access, principle, and benefits packages of the CBHI scheme and this might affects the respondents’ level of WTP for the proposed health insurance scheme. Third, since we included only the participants from rural area, the findings of this study cannot be generalized to households residing in urban areas.
Conclusion
In this study, around 83% of respondents were willing to pay for the CBHI and meet the government expectation of 2020. The study also revealed that educational status, family size, monthly income, and distance from the health facilities were significant factors associated with WTP for the CBHI scheme. In addition, we found that a large number of the respondents couldn’t afford the average amount of money that the participants were willing to pay for the CBHI scheme. So, the government should consider the economic status of the communities while revising the CBHI scheme premium not to miss those who cannot afford the contribution.
Supporting information
(DTA)
(DOC)
(DOCX)
Acknowledgments
Our deepest gratitude goes to the Department of Public Health, College of Medicine and Health Science, Dilla University and Paradise Valley University College for their continuous effort and support. Our appreciation also goes to Lemu and Bilbilo district Health office and data collectors for their genuine support during data collection.
Abbreviations
- AOR
Adjusted Odd Ratio
- CBHI
Community Based Health Insurance
- CI
Confidence Interval
- COR
Crude Odd Ratio
- ETB
Ethiopian Birr
- IRB
Institutional Review Board
- LMIC
Low and Medium-Income Countries
- OR
Odd Ratio
- USD
United State Dollar
- WHO
World Health Organization
- WTP
Willingness to Pay
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Karen A. Grépin, Bridget R. Irwin, Trakinsky BS. On the Measurement of Financial Protection: An Assessment of the Usefulness of the Catastrophic Health Expenditure Indicator to Monitor Progress Towards Universal Health Coverage. Health Systems & Reform. 2020;6(1). Epub e1744988. doi: 10.1080/23288604.2020.1744988 [DOI] [PubMed] [Google Scholar]
- 2.WHO, Bank W. Global Monitoring Report on Financial Protection in Health 2019. 2019.
- 3.Voorhoeve A, Ottersen T, Norheim OF. Making fair choices on the path to universal health coverage: a précis. Health Economics, Policy and Law. 2016;11(1):71–7. doi: 10.1017/S1744133114000541 [DOI] [PubMed] [Google Scholar]
- 4.Chukwuemeka A Umeh, Feeley FG. Inequitable Access to Health Care by the Poor in Community-Based Health Insurance Programs: A Review of Studies From Low- and Middle-Income Countries. Global Health: Science and Practice 2017;5(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leive A, K. X. Coping with out-of-pocket health payments: empirical evidence from 15 African countries. Bull World Health Organ. 2008;86:849–56C. doi: 10.2471/blt.07.049403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panda Iddo Dror, K TP. What factors affect the take up of voluntary and community-based health insurance programs in low and middle-income countries? Institute of Education. 2013. [Google Scholar]
- 7.Saumya Misra a, Shally Awasthi, Jai V. Singh, Monica Agarwal, Kumar V. Assessing the magnitude, distribution, and determinants of catastrophic health expenditure in urban Lucknow, North India. Clinical Epidemiology and global health 2015;3(16). [Google Scholar]
- 8.FMOH. Ethiopia health accounts, 2013/2014. Addis Ababa, Ethiopia2017.
- 9.Sara Bennett, Bethesda, USA and Health Policy Unit, Medicine LSoHaT. The role of community-based health insurance within the health care financing system: a framework for analysis. Health Policy and Planning 2004;19(3). doi: 10.1093/heapol/czh018 [DOI] [PubMed] [Google Scholar]
- 10.Bekele Demissie, Negeri KG. Effect of Community-Based Health Insurance on Utilization of Outpatient Health Care Services in Southern Ethiopia: A Comparative Cross-Sectional Study. Risk Management and Healthcare Policy. 2020:13 13:141–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.FMOH. Evaluation of community-based health insurance pilot schemes in Ethiopia: Final report. Addis Ababa: Ethiopian Health Insurance Agency, 2015. [Google Scholar]
- 12.Ali EE. Health Care Financing in Ethiopia: Implications on Access to Essential Medicines. Value in Health Regional issues. 2014;4C:37–40. doi: 10.1016/j.vhri.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 13.Solomon Feleke, Workie Mitiku, Hailu Zelelew, Ashagari TD. Ethiopia’s Community-based Health Insurance: A Step on the Road to Universal Health Coverage. Health Finance & Governance. 2014. [Google Scholar]
- 14.Tesfay G. The impact of community-based health insurance in health service utilization in Tigray; (Case of kilte Awlaelo woreda: Mekelle; 2014. [Google Scholar]
- 15.Darius Erlangga, Marc Suhrcke, Shehzad Ali, Bloor K. The impact of public health insurance on health care utilization, financial protection and health status in low- and middle-income countries: A systematic review. PLoS ONE. 2019;14(8). 10.1371/journal.pone.0219731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Desta Debalkie Atnafu, Hiwot Tilahun, Alemu YM. Community-based health insurance and healthcare service utilization, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. 2018;8. e019613. doi: 10.1136/bmjopen-2017-019613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mekonen AM, Gebregziabher MG, AS T. The effect of community-based health insurance on catastrophic health expenditure in Northeast Ethiopia: A cross-sectional study. PLoS ONE 2018;13(10). doi: 10.1371/journal.pone.0205972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zemzem Shigute, Anagaw D. Mebratie, Robert Sparrow, Getnet Alemu, Bedi AS. The Effect of Ethiopia’s Community-Based Health Insurance Scheme on Revenues and Quality of Care. International Journal of Environmental Research and Public Health. 2020;12(8558). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kasim Ebrahim, Fanos Yonas, Kaso M. Willingness of community to enroll in community-based health insurance and associated factors at household Level in Siraro District, West Arsi Zone, Ethiopia. Journal of Public Health and Epidemiology. August 2019;11(6):137–44. [Google Scholar]
- 20.Melaku Haile, Shimeles Ololo, Megersa B. Willingness to join community-based health insurance among rural households of Debub Bench District, Bench Maji Zone, Southwest Ethiopia. BMC Public Health 2014;14(591). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dawit Nageso, Kebede Tefera, Gutema K. Enrollment in community-based health insurance program and the associated factors among households in Boricha district, Sidama Zone, Southern Ethiopia; a cross-sectional study. PLoS ONE. 2020;15(6). doi: 10.1371/journal.pone.0234028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abishu Kado, Bedasa Taye Merga, Hassen Abdi Adem, Yadeta Dessie, Biftu Geda. Willingness to Pay for Community-Based Health Insurance Scheme and Associated Factors Among Rural Communities in Gemmachis District, Eastern Ethiopia. ClinicoEconomics and Outcomes Research. 2020;12:609–18. doi: 10.2147/CEOR.S266497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amare Minyihun, Measho Gebreslassie Gebregziabher, Gelaw YA. Willingness to pay for community‑based health insurance and associated factors among rural households of Bugna District, Northeast Ethiopia. BMC Res Notes 2019;12(55). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muluneh Getachew Garedew, Shimeles Ololo Sinkie, Dejene Melese Handalo, Waju Beyene Salgedo, Kidus Yitebarek Kehali, Feyera Gebissa Kebene, et al. Willingness to Join and Pay for Community-Based Health Insurance Among Rural Households of Selected Districts of Jimma Zone, Southwest Ethiopia. ClinicoEconomics and Outcomes Research. 2020;12:45–55. doi: 10.2147/CEOR.S227934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Esther F. Adebayo, Olalekan A. Uthman, Charles S. Wiysonge, Erin A. Stern, Kim T. Lamont, Ataguba JE. A systematic review of factors that affect the uptake of community-based health insurance in low-income and middle-income countries. BMC Health Services Research 2015;15(543). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kindie Mitiku Kebede, Geberetsadik SM. Household satisfaction with community-based health insurance scheme and associated factors in piloted Sheko district; Southwest Ethiopia. PLoS ONE 2019;14(5). Epub e0216411. doi: 10.1371/journal.pone.0216411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mecthilde Mukangendo, Manasse Nzayirambaho, Regis Hitimana, Yamuragiye A. Factors Contributing to Low Adherence to Community-Based Health Insurance in Rural Nyanza District, Southern Rwanda. Journal of Environmental and Public Health. 2018;2018:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Racha Fadlallah, Fadi El-Jardali, Nour Hemadi, Rami Z. Morsi, Clara Abou Abou Samra, Ali Ahmad, et al. Barriers and facilitators to implementation, uptake and sustainability of community based health insurance schemes in low and middle-income countries: a systematic review. International Journal for Equity in Health (2018) 17:13. 2018;17(13). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Organization WH. The World Health Report. Health Systems Financing: The Path to Universal Coverage. Geneva: WHO; 2010. Contract No: WHO Report ISBN. 2018;978(92):4. [Google Scholar]
- 30.Exchange rate of Ethiopian birr to foreign currency [Internet]. October 15, 2021. Available from: https://www.combanketh.et/en/exchange-rate#exchangerate.
- 31.Ogundeji YK, Akomolafe B, Ohiri K, Butawa NN. Factors influencing willingness and ability to pay for social health insurance in Nigeria. PloS one. 2019;14(8):e0220558. doi: 10.1371/journal.pone.0220558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wagstaff A, Doorslaer Ev. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. Health economics. 2003;12(11):921–33. [DOI] [PubMed] [Google Scholar]
- 33.Wagstaff A, Flores G, Smitz M-F, Hsu J, Chepynoga K, Eozenou P. Progress on impoverishing health spending in 122 countries: a retrospective observational study. The Lancet Global Health. 2018;6(2):e180–e92. doi: 10.1016/S2214-109X(17)30486-2 [DOI] [PubMed] [Google Scholar]
- 34.Christie Divine Akwaowo, Idongesit Umoh, Olugbemi Motilewa, Bassey Akpan, Edidiong Umoh, Edidiong Frank, et al. Willingness to Pay for a Contributory Social Health Insurance Scheme: A Survey of Rural Residents in Akwa Ibom State, Nigeria. Front Public Health. 2021;9(654362). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eshetu Mamo, Bekele G. Households’ Willingness to Pay for Community Based Health Insurance Scheme: in Kewiot and EfratanaGedem Districts of Amhara Region, Ethiopia. Business and Economic Research. 2017;7(2). [Google Scholar]
- 36.Alem Deksisa, Meyrema Abdo, Ebrahim Mohamed, Daniel Tolesa, Sileshi Garoma, Abate Zewdie, et al. Willingness of community based health insurance uptake and associated factors among urban residents of Oromia regional state, Oromia, Ethiopia, a cross-sectional study. BMC Health Services Research 2020;20(864). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahmed Sayem, Mohammad Enamul Hoque Abdur Razzaque Sarker, Sultana Marufa, Islam Ziaul, Gazi Rukhsana, et al. Willingness-to-Pay for Community-Based Health Insurance among Informal Workers in Urban Bangladesh. PLoS ONE. 2016;11(2). Epub e0148211. doi: 10.1371/journal.pone.0148211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Akhtar Sana, Fatima Rida, Ishaq Tayyaba, Mehmood Masooma, Zulfqar Ayesha AK. Willingness to Pay for Community-Based Healthcare Insurance Schemes in Developing Countries: A Case of Lahore, Pakistan. Ethiop J Health Sci. 2020;30(1):135. doi: 10.4314/ejhs.v30i1.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhawana Khatiwada, Saruna Ghimire, Naveen Shrestha, Khadga Bhadur Shrestha, Dahal PK. Willingness to pay for health insurance in the Mangalbare village development committee of Illam district. MOJ Public Health. 2017;5 (2). [Google Scholar]
- 40.Oyekale AS. Factors Influencing Households’ Willingness to Pay for National Health Insurance Scheme (NHIS) in Osun State, Nigeria. Ethno Med. 2012;6(3):167–72. [Google Scholar]
- 41.Berhanu Bifato, Amanuel Ayele, Muse Rike, Dangura D. Community Based Health Insurance Enrollment and Associated Factors in Sidama Region, Ethiopia. Journal of Tropical Disease and Public Health. 2021;9(8):297. [Google Scholar]
- 42.Dror DM, Hossain SAS, Majumdar A, Pérez Koehlmoos TL, John D, PK P. What Factors Affect Voluntary Uptake of Community-Based Health Insurance Schemes in Low- and Middle-Income Countries? A Systematic Review and Meta-Analysis. PLoS ONE. 2016;11(8). e0160479. doi: 10.1371/journal.pone.0160479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Negash B, Dessie Y, Gobena T. Community Based Health Insurance Utilization and Associated Factors among Informal Workers in Gida Ayana District, Oromia Region, West Ethiopia. East African Journal of Health and Biomedical Sciences. 2019;3(2):13–22. [Google Scholar]
- 44.Peterson L, Comfort A, Omasanjuwa E, Ambrose K, Hatt L. Extending health insurance to informal sector workers in urban settings: findings from a micro-insurance pilot in Lagos, Nigeria. 2015;[39] p. [Google Scholar]
- 45.Mtei G, Mulligan J. Community health funds in Tanzania: A literature review. Ifakara Health Research and Development Centre, Ifakara. 2007. [Google Scholar]
- 46.Saha S, Kermode M, Annear P. Effect of combining a health program with a microfinance-based self-help group on health behaviors and outcomes. Public Health. 2015;129(11):1510–8. doi: 10.1016/j.puhe.2015.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.ORHB. Notification of the Revised Community-based Health Insurance. 2021.
- 48.Adane Kebede, Measho Gebreslassie, Yitayal M. Willingness to pay for community-based health insurance among households in the rural community of Fogera District, North West Ethiopia. International Journal of Economics, Finance and Management Sciences. 2014;2(4):263–9. [Google Scholar]
- 49.Mohammed Khaled Al-Hanawi, Kirit Vaidya, Omar Alsharqi, Obinna Onwujekwe. Investigating the Willingness to Pay for a Contributory National Health Insurance Scheme in Saudi Arabia: A Cross-sectional Stated Preference Approach. Appl Health Econ Health Policy. 2018;16:259–71. doi: 10.1007/s40258-017-0366-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Obinna Onwujekwe, Ekechi Okereke, Chima Onoka, Benjamin Uzochukwu, Joses Kirigia, Petu A. Willingness to pay for community-based health insurance in Nigeria: do economic status and place of residence matter? Health Policy and Planning 2010;25:155–61. doi: 10.1093/heapol/czp046 [DOI] [PubMed] [Google Scholar]
- 51.Rosine Wafo Cheno, William Tchabo, Tchamy J. Willingness to join and pay for community-based health insurance and associated determinants among urban households of Cameroon: a case of Douala and Yaounde. Heliyon. 2021;7. Epub e06507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Usman Bukola A. Willingness to Pay For Community Based Health Care Financing Scheme: A Comparative Study among Rural and Urban Households in Osun State, Nigeria. IOSR Journal of Dental and Medical Sciences. 2013;5(6):27–40. [Google Scholar]
- 53.Shafie A.A., Hassali MA. Willingness to pay for voluntary community-based health insurance: Findings from an exploratory study in the state of Penang, Malaysia. Social Science & Medicine 2013;96: 272–6. doi: 10.1016/j.socscimed.2013.02.045 [DOI] [PubMed] [Google Scholar]
- 54.Ghosh M. Awareness and Willingness to Pay for Health Insurance: A Study of Darjeeling District. IOSR Journal Of Humanities And Social Science 2013;12(1):41–7. [Google Scholar]
- 55.Agyei-Baffour P, Isiaka Jimmy A TP, Larbie D, Anarfi Boateng K, Kwaku Duah I, Bangura A, et al. Socio-Demographic Predictors of Willingness to Pay for Premium of National Health Insurance: A Cross-sectional Survey of Six Districts in Sierra Leone. Int J Health Policy Manag. 2021;x(x):1–8. doi: 10.34172/ijhpm.2021.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DTA)
(DOC)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.