Abstract
Glenoid articular cartilage lesion is a rare complication following traumatic anterior dislocation of the shoulder. We report the case of a 14-year-old male rugby player with traumatic anterior shoulder instability, an extensively flapped lesion on the glenoid articular cartilage, and an osseous Bankart lesion. Arthroscopic findings revealed that the glenoid cartilage was flap-detached, extending from the anteroinferior to the center. Repair of the osseous Bankart lesion using suture anchors and resection of the unstable peripheral part of the cartilage was performed arthroscopically. The main region of the injured articular surface was left untouched. During postoperative follow-up, absorption of the glenoid articular surface near the suture anchor holes was identified. Arthroscopic examination three months post-surgery showed that the flap detached lesion of the residual cartilage was stable and appeared adapted on the glenoid surface. The resected area was covered by fibrous tissue. A follow-up computed tomography scan revealed that the osseous lesion was united. The patient returned to his previous sports capacity eight months following the operation. At the 2-year-follow-up, magnetic resonance imaging revealed that the glenoid surface was remodeled to a flattened round shape with no signs of osteoarthritis, exhibiting proper conformity of the joint surfaces to the humeral head. Arthroscopic Bankart repair using suture anchors may cause bone resorption at the glenoid surface, leading to remodeling of the glenoid surface from the damaged glenoid cartilage lesion in young patients.
Keywords: Bankart lesion, Shoulder injuries, Articular cartilage lesion, Arthroscopy
Highlights
Glenoid articular cartilage lesion is a rare complication following traumatic anterior dislocation of the shoulder.
We reported on a 14-year-old rugby player with traumatic anterior instability, with an extensive glenoid labral tear and articular cartilage flap lesion and osseous Bankart lesion. The patient was treated by arthroscopic osseous Bankart repair
The follow-up arthroscopy at 3rd postoperative month revealed that the flap lesion had healed with fibrous soft tissue covering the area of resected cartilage. The patient was able to return to his pre-injury capacity after 8 months.
In young patients, arthroscopic osseous Bankart repair may lead to remodeling of the glenoid surface from the damaged glenoid cartilage lesion.
Introduction
Traumatic anterior shoulder dislocation is frequently associated with osseous Bankart lesions in collision sports such as rugby.1 Treatment includes arthroscopic repair of the osseous Bankart lesion, which may lead to glenoid remodeling.1 Contrarily, glenoid labral articular disruption (GLAD) is uncommon in cases of traumatic anterior dislocation.2 Arthroscopic findings indicate that there is a variant of the cartilage lesion, an avulsion of the anteroinferior glenoid labrum, and flap tear of the adjacent articular cartilage, called a glenoid labral tear and articular cartilage flap (GLAF) lesion.3 To our knowledge, there have been no reports on GLAF lesions associated with osseous Bankart lesions.
We report a rare case of traumatic anterior instability with an extensive GLAF lesion and osseous Bankart lesion treated by arthroscopic osseous Bankart repair for glenohumeral stabilization.
Case Presentation
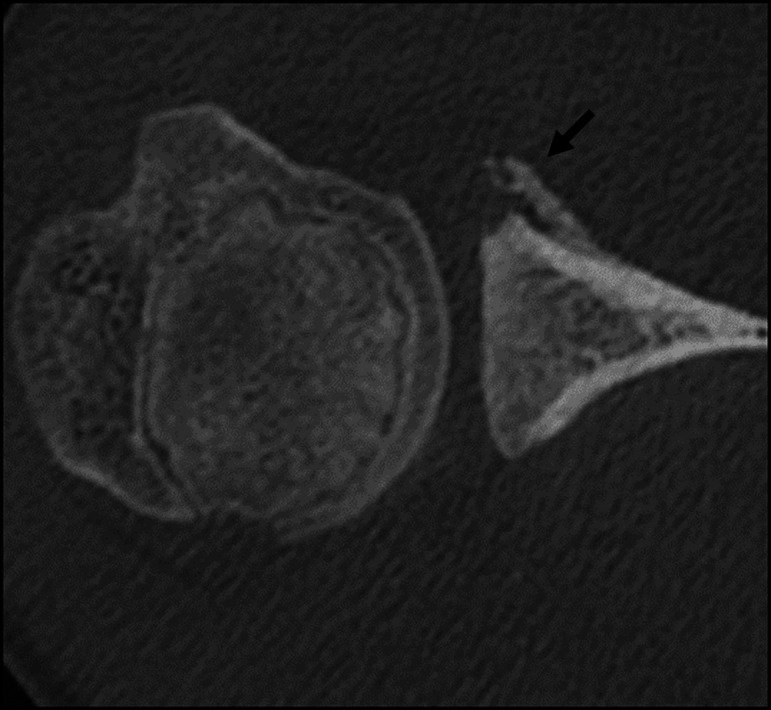
A 14-year-old male rugby player tackled an opponent and suffered a subluxation of the right shoulder due to forced abduction and external rotation of his arm. Although he returned to play after conservative treatment by a local physician for 2 months, he experienced multiple subluxations but never had a complete dislocation that required closed reduction in a hospital. He was referred to our hospital, and on physical examination, had no limitation in the range of motion (ROM) in the right shoulder or apparent muscle weakness in any direction. The anterior apprehension test was positive, and the Beighton score was 1, which excluded hypermobility.4 The patient had an Oxford shoulder instability score of 27 points.5 Plain radiography showed a residual epiphyseal line in the humerus and an avulsed bone fragment below the glenoid (Figure 1). A glenoid osseous lesion was confirmed in the anteroinferior part by computed tomography (CT),6 with a 3.1 mm osseous Bankart lesion, 14.3% glenoid defect, and 6.2 mm Hill-Sachs lesion width (Figure 2). Preoperative magnetic resonance imaging (MRI) was not performed as the CT findings sufficed in indicating the primary cause of the condition.
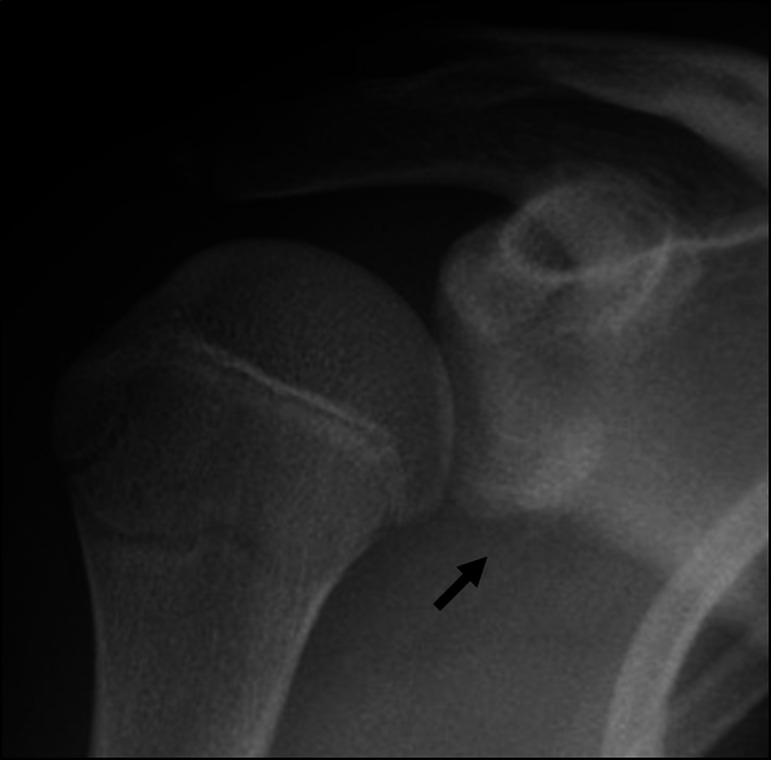
Figure 1.
Preoperative images. Plain radiograph of the anteroposterior view; arrow shows osseous Bankart lesion.
Figure 2.
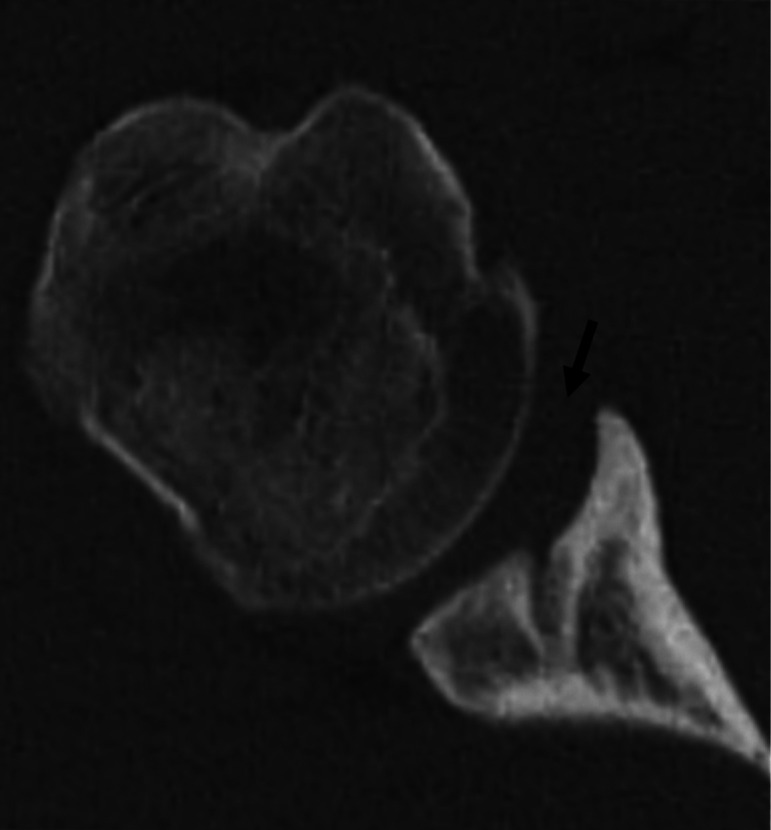
CT image of axial view. An osseous bony lesion was observed in the anteroinferior part of the glenoid. CT, computed tomography.
Arthroscopic surgery was performed in the beach-chair position, 4 months after the injury. The glenohumeral joint was observed from the posterior portal using a 45° arthroscope to have a clear visualization of the edge of the anteroinferior part of the glenoid. An extensive flap-detached cartilage lesion in the anteroinferior quarter part of the glenoid with osseous Bankart lesion (3 to 6 o’clock) was observed (Figure 3). Partial resection of the anterior flap-detached lesion was performed. Meanwhile, the posterior part of the flap-detached cartilage lesion, which connected with the normal articular cartilage was left as is because we expected the lesion to reattach by spontaneous healing. Therefore, only the osseous Bankart lesion was repaired using 4 suture anchors (Gryphon BR Anchor; Mitek Sports Medicine, Boston, MA, USA).7 The anteroinferior rim of the glenoid cartilage was partially resected at a width of 5 mm to enable accurate placement of the suture anchors during the procedure (Figure 4). The 2 sutures in the middle penetrated through the substantial bone of the osseous Bankart lesion using a Bone Stitcher (Smith and Nephew, MA, USA).8
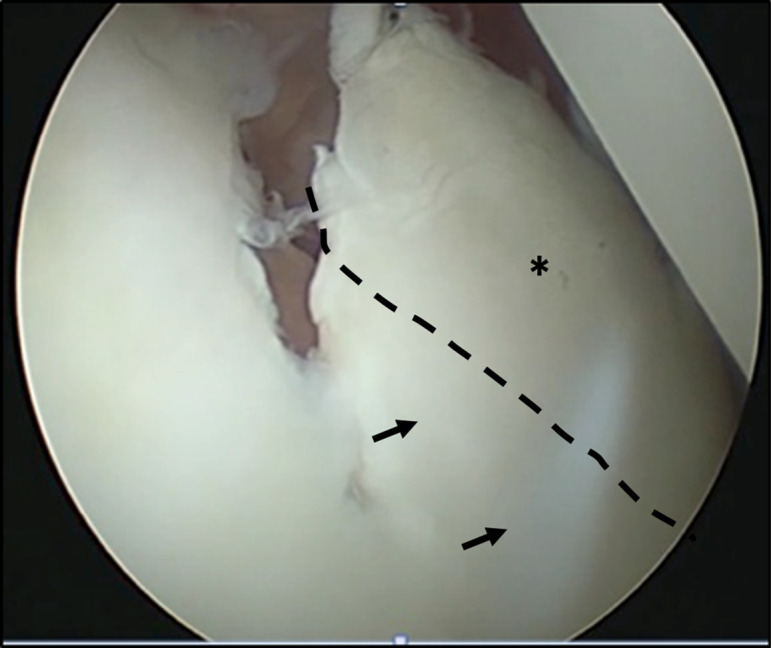
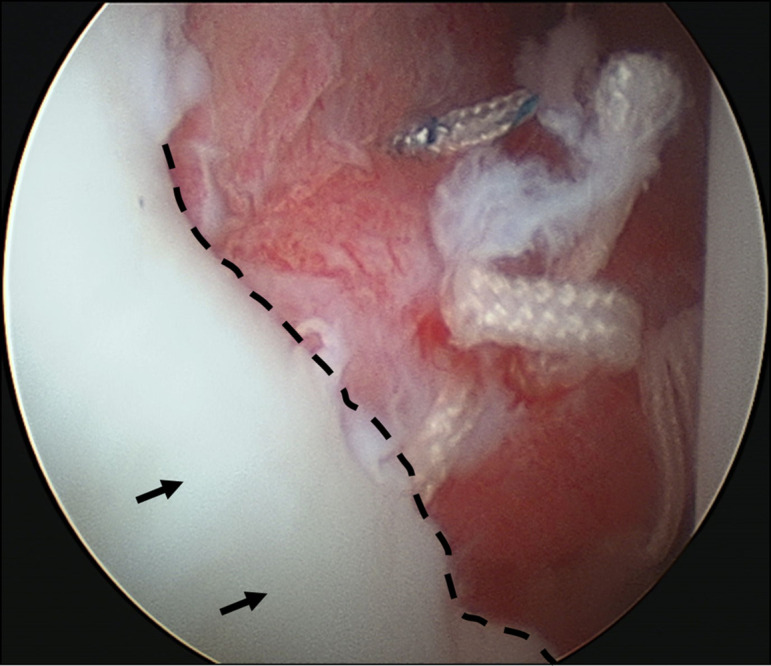
Figure 3.
Arthroscopic view of the anterior part from the posterior portal at the initial surgery. An extensively flap-detached cartilage lesion (asterisk) in the anteroinferior part of the glenoid. The dotted line indicates the trimming line of the anterior edge of the articular cartilage. Arrows show the unmoved cartilage lesion after partial resection.
Figure 4.
Post-repair of the osseous Bankart lesion at the initial surgery. The dotted line and arrows represent the same locations as shown in Figure 3.
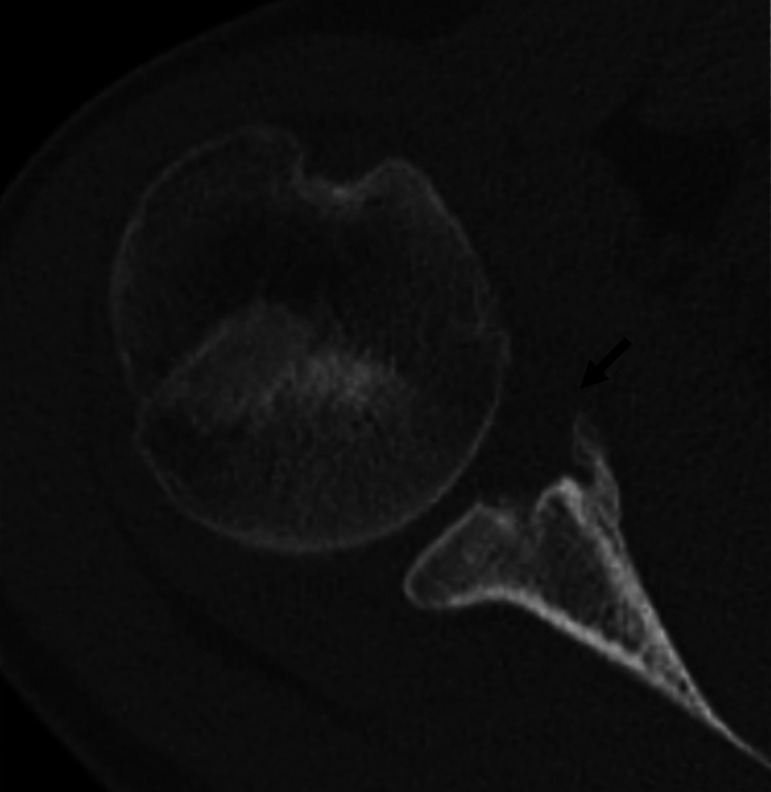
A standard postoperative rehabilitation protocol for the arthroscopic Bankart repair was implemented, with 3 weeks of immobilization using an abduction brace followed by gradual passive ROM exercises. One-month post-operation, a plain x-ray indicated partial bone resorption in the glenoid, and this change progressed for the following 2 months. 3 months post-operation, a CT scan revealed a healed osseous Bankart lesion and significant bone loss at the anterior glenoid surface near the area of the suture anchor (Figure 5). We suggested a second surgery to re-evaluate the situation despite the patient having no complaints or any apparent symptoms for 2 reasons. First, additional surgical treatment such as resection of the remaining flap-detached cartilage lesion or microfracture might be needed if the cartilage lesion was unperturbed and unstable. Second, the postoperative CT findings suggested deterioration of the glenoid surface caused by the cartilage lesion. The patient’s parents provided informed consent for performing arthroscopy 3 months following the initial surgery.
Figure 5.
CT images 3 months post-operation at the axial view. The osseous Bankart lesion that had not been fully reduced was united after 3 months although osteolytic changes in the glenoid were observed. CT, computed tomography.
The follow-up arthroscopy performed 3 months after the initial surgery revealed that the flap-detached lesion of the residual cartilage was flattened and stabilized with fibrous soft tissue covering the area of the resected cartilage with the healed osseous Bankart lesion (Figure 6). The patient was allowed to begin muscle strength training, running, and ball-handling 3 months after the initial surgery, just after the second-look arthroscopy, in accordance with our rehabilitation protocol for rugby players.1
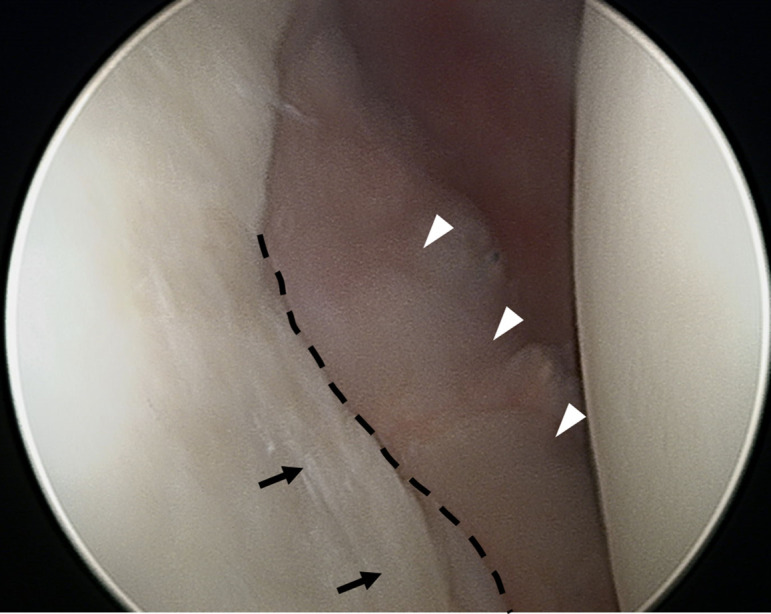
Figure 6.
Arthroscopic view of the anterior part from the posterior portal at the second surgery. The dotted line and arrows represent the same locations as shown in Figures 3 and 4. The white arrowheads show the detached lesion of the residual cartilage, flattened and stable with fibrous soft tissue covering the area of the healed osseous Bankart lesion.
At 6 months, a three-dimensional (3D) CT showed flattened remodeling of the anterior glenoid. The patient returned to his pre-injury capacity after 8 months. The patient reported no recurrent instability for 2 years post-operation and had an Oxford shoulder instability score of 48. A CT 2 years post-operation showed a united osseous Bankart lesion and a reasonably flattened glenoid surface (Figure 7). An MRI 2 years post-operation (Figure 8) showed osteosclerotic changes of the subchondral bone revealing fibrocartilaginous tissue on the surface that appeared to have good conformity with the humeral head.
Figure 7.

CT images at 2 years post-operation at the axial view. Arrows show the peripheral flattening of the osteolytic lesion as remodeling was noted. CT, computed tomography.
Figure 8.
MRI at the 2-year follow-up at the proton axial view. Sclerotic changes in the subchondral bone and fibrocartilaginous tissue formation on top of it were noted. Proper conformity with the humeral head was observed. MRI, magnetic resonance imaging.
Discussion
To our knowledge, this is the first report of an operative case of traumatic anterior instability with extensive glenoid articular cartilage lesion accompanied by an osseous Bankart lesion with a 2-year follow-up. Although the damaged cartilage was not directly repaired, arthroscopic follow-up after 3 months revealed that the lesion had been stabilized following glenohumeral stabilization and osseous reconstruction of the glenoid by arthroscopic osseous Bankart repair.8 Although postoperative bone resorption was also observed at the anterior part of the glenoid surface where the suture anchors were inserted, there was improvement during the subsequent healing of the osseous glenoid lesion with an eventual return to pre-injury capacity.
Galano et al9 reported that GLAD lesions could be treated by either removal of an irreparable fragment and microfracture, or by reattachment of the cartilage flap to the glenoid with a chondral fixation device. Page et al3 reported a case in which a GLAF lesion was treated with a meniscal repair device to place a mattress suture in the cartilage periphery after reconstruction of a labral tear with suture anchors to form a neo-labrum in an attempt to overlap and stabilize the flap-detached cartilage lesion. In our case, the removal of the cartilage lesion was not considered because the lesion was extensive. To prioritize the treatment of the shoulder instability, only the peripheral cartilage overlying the bony fragment was resected and the osseous Bankart lesion repaired. Arthroscopy at the 3-month follow-up revealed that the resected cartilage periphery was remodeled and covered by soft tissue. The glenoid subchondral bone was not seen but was well preserved based on the MRI findings at the 2-year follow-up. There are prior studies on cartilage flap tears in association with hip labral tears which suggest high vascularity to the cartilage flap.10 The patient, in this case, was young, and the osseous involvement was continuous with the cartilage flap tear. Therefore, these factors may have contributed to the flap healing without surgical stabilization. Other treatment options, for example, the removal of an unstable cartilage fragment and microfracture, could also have been successful. However, resecting the flap-detached cartilage and microfracture would have resulted in the glenoid surface being covered with fibrocartilage, which is different from the normal hyaline cartilage.11
Postoperative diagnostic imaging results revealed bone resorption anteroinferior to the glenoid where the suture anchors were placed, suggesting progression of bone resorption at the anterior margin of the glenoid by the suture anchors. Previous reports indicated the risks of bone resorption due to suture anchors, especially with materials such as poly-l-lactic and polyglycolic acids.12 However, the anchors used in this case were a complex of glycolic–lactic acid polyester and beta-tricalcium phosphate, which have not been reported to cause bone resorption. There have been reports on the risk of heat necrosis while drilling bone.13 Some groups have suggested that lower blood perfusion could cause bone resorption.14 Anatomical studies have shown low vasculature in the peripheral part of the glenoid.15
It is assumed that the repair of the glenoid osseous lesion led to the improvement of the subchondral bone morphology, which in turn facilitated the repair of the damaged cartilage. Even if the bony fragment was not fully reduced, remodeling of the morphology of the glenoid surface can be expected by bony healing.7 It was critical to repair the osseous Bankart lesion and to avoid resection of the damaged cartilage fragment to reduce the risk of osteoarthritis in the future.1
A secondary center for ossification in the scapular glenoid usually appears at 11 years of age and disappears at around 17 or 18 years of age. As the epiphyseal line is located in the upper third of the glenoid, the areas of separated cartilage and the osseous Bankart lesion were expected to have high healing potential because of the patient’s age, which was indicated by the residual epiphyseal plate.16,17 Therefore, in cases of cartilage injury and osseous Bankart lesion in an adolescent patient, it is important to consider the mechanism of injury, reconstruction of the main lesion, and avoiding resection of the cartilage and osseous lesions.
There are several limitations to this study. First, we did not perform an osteochondral biopsy during the second surgery. Second, we did not use preoperative MRI since the osseous Bankart lesion was identified as the essential lesion by CT scan prior to MRI. Except for economical reasons, preoperative MRI is suggested as it helps identify concomitant lesions. Even if surgical repair for the cartilage lesion was attempted for the patient’s age, there was no consensus that repair was better than excision and what device and procedure were best. Third, regarding the evaluation of the glenoid bone morphology, we have consistently performed 3D CT. However, considering the problems such as radiation exposure, a CT 2 years after the surgery may not have been necessary and an MRI alone would have been sufficient. Fourth, a third-look arthroscopy at the 2-year follow-up would be meaningful. However, the patient had already returned to playing rugby without any complaints. Also, ideal remodeling of the glenoid surface had been revealed by CT examination and all imaging studies showed no osteoarthritic change on the glenoid surface. Therefore, we did not push forward with a third-look arthroscopy 2 years after the surgery.
Conclusion
We reported on a 14-year-old rugby player with an extensive GLAF lesion and osseous Bankart lesion treated by arthroscopic osseous Bankart repair. The remaining cartilage was stabilized on the glenoid surface with glenoid osseous remodeling. The patient was able to return to his pre-injury capacity of playing rugby.
Footnotes
Informed Consent:
The patient’s parents provided informed consent for performing arthroscopy three months following the initial surgery.
Author Contributions: Concept - A.T.; Design - A.T.; Supervision - T.N., T.M.; Materials - M.S.; Data Collection and/or Processing - M.S., T.N., T.M.; Analysis and/or Interpretation - M.S.; Literature Review - M.S.; Writing - M.S.; Critical Review - A.T.
Acknowledgments We express our sincere thanks to Dr. Nobuto Kitamura, Dr. Wataru Morita, and Dr. Tomoshige Tamaki for helpful discussions and comments on the manuscript.
Declaration of Interests: The authors have no conflicts of interest to declare.
Funding: The authors declared that this study has received no financial support.
References
- 1. Tasaki A, Morita W, Yamakawa A.et al. Combined arthroscopic Bankart repair and coracoid process transfer to anterior glenoid for shoulder dislocation in rugby players: evaluation based on ability to perform sport-specific movements effectively. Arthroscopy. 2015;31(9):1693 1701. 10.1016/j.arthro.2015.03.013) [DOI] [PubMed] [Google Scholar]
- 2. Neviaser TJ. The GLAD lesion: another cause of anterior shoulder pain. Arthroscopy. 1993;9(1):22 23. 10.1016/s0749-8063(05)80339-1) [DOI] [PubMed] [Google Scholar]
- 3. Page R, Bhatia DN. Arthroscopic repair of a chondrolabral lesion associated with anterior glenohumeral dislocation. Knee Surg Sports Traumatol Arthrosc. 2010. ;18(12):1748 1751. 10.1007/s00167-010-1095-3) [DOI] [PubMed] [Google Scholar]
- 4. Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969;51(3):444 453. 10.1302/0301-620X.51B3.444) [DOI] [PubMed] [Google Scholar]
- 5. Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br. 1999;81(3):420 426. 10.1302/0301-620x.81b3.9044) [DOI] [PubMed] [Google Scholar]
- 6. Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85(5):878 884. 10.2106/00004623-200305000-00016) [DOI] [PubMed] [Google Scholar]
- 7. Kitayama S, Sugaya H, Takahashi N.et al. Clinical outcome and glenoid morphology After arthroscopic repair of chronic osseous Bankart lesions: a five to eight-year follow-up study. J Bone Joint Surg Am. 2015;97(22):1833 1843. 10.2106/JBJS.N.01033) [DOI] [PubMed] [Google Scholar]
- 8. Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. Surgical technique. J Bone Joint Surg Am. 2006;88(suppl 1 Pt 2):159 169. 10.2106/JBJS.F.00319) [DOI] [PubMed] [Google Scholar]
- 9. Galano GJ, Weisenthal BM, Altchek DW. Articular shear of the anterior-inferior quadrant of the glenoid: a glenolabral articular disruption lesion variant. Am J Orthop (Belle Mead NJ). 2013;42(1):41 43. [PubMed] [Google Scholar]
- 10. Wright VJ, McCrum CL, Li H, Tranovich MJ, Huard J. Significant chondrocyte viability is present in acetabular chondral flaps associated with femoroacetabular impingement. Am J Sports Med. 2018;46(1):149 152. 10.1177/0363546517732751) [DOI] [PubMed] [Google Scholar]
- 11. Saltzman BM, Leroux T, Cole BJ. Management and surgical options for articular defects in the shoulder. Clin Sports Med. 2017;36(3):549 572. 10.1016/j.csm.2017.02.009) [DOI] [PubMed] [Google Scholar]
- 12. Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ. Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med. 2012;40(6):1424 1430. 10.1177/0363546511417573) [DOI] [PubMed] [Google Scholar]
- 13. Mediouni M, Schlatterer DR, Khoury A.et al. Optimal parameters to avoid thermal necrosis during bone drilling: a finite element analysis. J Orthop Res. 2017;35(11):2386 2391. 10.1002/jor.23542) [DOI] [PubMed] [Google Scholar]
- 14. Cooper DE, Arnoczky SP, O’Brien SJ, Warren RF, DiCarlo E, Allen AA. Anatomy, histology, and vascularity of the glenoid labrum. An anatomical study. J Bone Joint Surg Am. 1992;74(1):46 52. 10.2106/00004623-199274010-00007) [DOI] [PubMed] [Google Scholar]
- 15. Abrassart S, Stern R, Hoffmeyer P. Arterial supply of the glenoid: an anatomic study. J Shoulder Elbow Surg. 2006;15(2):232 238. 10.1016/j.jse.2005.07.015) [DOI] [PubMed] [Google Scholar]
- 16. Wall EJ, Vourazeris J, Myer GD.et al. The healing potential of stable juvenile osteochondritis dissecans knee lesions. J Bone Joint Surg Am. 2008;90(12):2655 2664. 10.2106/JBJS.G.01103) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zember JS, Rosenberg ZS, Kwong S, Kothary SP, Bedoya MA. Normal skeletal maturation and imaging pitfalls in the pediatric shoulder. RadioGraphics. 2015;35(4):1108 1122. 10.1148/rg.2015140254) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a