Brief report of 13 eyes with blunt trauma secondary to recoil from elastic cord exercise equipment, and review of the literature.
Key words: blunt trauma, elastic band, exercise band, injury, recoil, resistance band
Purpose:
To discuss the mechanism of injury and characterize the clinical features of ocular trauma associated with elastic cord exercise equipment band injuries in a consecutive series of patients seen at a single vitreoretinal surgery practice.
Methods:
We performed a retrospective review of all patients who were treated for blunt trauma from 2013 to 2020 at a single vitreoretinal practice.
Results:
Thirteen eyes from 11 patients met the inclusion criteria of possessing ocular trauma secondary to recoil from exercise bands. Presenting visual acuity ranged from 20/16 to HM (median: 20/32). The most frequently observed anterior segment pathologies were traumatic iritis (54%) and angle recession (31%). The most common posterior segment findings were vitreous hemorrhage (54%) and peripheral commotio retinae (54%). Three eyes (23%) required surgical intervention. Follow-up intervals ranged from 0 to 10 months (median: 1.75 months). Visual acuity at last examination ranged from 20/13 to 20/400 (median: 20/40).
Conclusion:
A wide spectrum of serious ocular injuries requiring medical and surgical intervention can result from this form of blunt ocular trauma. The frequency of this event would be decreased by the use of sports goggles and careful inspection of equipment for wear and over use.
Traumatic ocular injuries from recoil of bungee cords have been well documented.1 Recently, there have been case reports describing trauma associated with exercise equipment using elastic cords.2–6 Users of exercise bands strength train by generating the force necessary to overcome the resistance of the synthetic rubber. Ocular trauma may result from the accidental recoil of the elastic cord. Whereas impact from recoil of bungee cords is incurred by a metal hooked end, blunt trauma from exercise bands resulted from the band itself. Traumatic iritis,2,3 traumatic mydriasis,4 iris sphincter tear,5 angle recession,5 hyphema,3–5 iridodonesis,3 anterior vitreous prolapse,3 vitreous hemorrhage,3 commotio retinae,2 retinal detachment,2,6 retinal dialysis,6 vitreous base avulsion,6 and lens dislocation3 have been previously reported. In this case series, we describe our experience with consecutive cases of elastic exercise band ocular injuries.
Methods
This study was approved by the Institutional Review Board of California Pacific Medical Center. We performed a retrospective review for all patients who were treated for blunt trauma from 2013 to 2020 at a single vitreoretinal practice. Thirteen eyes from 11 patients met the inclusion criteria of possessing ocular trauma secondary to recoil from exercise bands.
For each subject, we recorded demographic information, mechanism of injury, presenting visual acuity and intraocular pressure (IOP), previous ocular history, anterior segment findings, posterior segment findings, diagnostic imaging obtained, intervention, duration of follow-up, maximum IOP, final visual acuity and IOP, and final anatomic status.
Results
Patient demographics, clinical findings, and final anatomical dispositions are summarized in Table 1. There were five men and six women. Age at presentation ranged from 16 to 76 years (median: 43 years). Nine patients (82%) had unilateral involvement. Two patients (18%), both men, had bilateral involvement. No patient had a history of prior ocular trauma. Lattice degeneration, treated retinal tear, and pseudophakia were noted in one eye each. Two eyes possessed posterior vitreous detachments. All were without safety glasses at the time of injury. All 11 (100%) patients described slippage of the elastic band from the anchoring point followed by impact from the recoiling the elastic band as the cause of their blunt ocular trauma. Four (36%) patients described use of a flat elastic loop and two (18%) used an elastic cord with terminal handles. Five patients (45%) were documented as using an unspecified resistance band, but could not be reached for further clarification. Six (55%) patients sustained injury at the gym or an exercise class, three (27%) while strength training at home, and two (18%) were at an unspecified location. Presenting visual acuity ranged from 20/16 to HM (median: 20/32). Initial IOP ranged from 7 to 30 mmHg (Median: 14 mmHg). Follow-up intervals ranged from 0 to 10 months (median: 1.25 months); four eyes (31%) lacked further visits after initial examination. Visual acuity at last examination ranged from 20/13 to 20/400 (median: 20/40), maximum IOP ranged from 14 to 48 mmHg (median: 26 mmHg), and final IOP ranged from 8 to 20 mmHg (median: 14 mmHg) for the nine eyes (69%) with follow-up visits.
Table 1.
Summary of Individual Clinical Findings, Interventions, and Outcomes
| Case | Age (years) | Sex | Eye | Initial Vision (Snellen) | Initial IOP (mmHg) | Type of Elastic Band | Mechanism | Setting | Anterior Segment Findings | Posterior Segment Findings | Intervention | Duration of Follow-up | Final Vision (Snellen) | Maximum IOP (mmHg) | Final IOP (mmHg) | Final Anatomic Disposition |
| 1 | 33 | M | OD | 20/200-2 | 10 | Flat loop | Slipped | Home | Traumatic iritis, iris sphincter tears, corneal abrasion, angle recession, inferior zonular dialysis, inferior iridodonesis | VH, mac-CR, SRH, CR, CHR | IOP lowering, corticosteroid, and atropine drops | 10 minutes | 20/40-2 | 48 | 12 | Attached, peripheral subretinal fibrosis, mac-RPE disruption |
| 2 | 33 | M | OS | HM | 7 | Flat loop | Slipped | Home | Traumatic iritis, corneal abrasion, angle recession | VH, mac-CR, CR, MH | IOP lowering, corticosteroid, and atropine drops | 10 minutes | 20/250-3 | 26 | 17 | Attached, MH closed, mac-RPE disruption, peripheral RPE disruption, peripheral subretinal fibrosis |
| 3 | 42 | F | OS | 20/32 | 14 | Flat loop | Slipped | Gym* | None | None | Observation | 0 | ||||
| 4 | 34 | F | OD | 20/25 | 14 | Flat loop | Slipped† | Gym | Traumatic iritis | None | Observation | 0 | ||||
| 5 | 62 | M | OS | 20/32-1 | 13 | Unspecified | Slipped | Unspecified | Subconjunctival hemorrhage | CR | Observation | 2 weeks | 20/25 | 14 | 14 | Attached, resolved CR |
| 6 | 76 | M | OD | 20/32 | 12 | Unspecified | Slipped | Unspecified | None | VH, CR, RH | Observation | 7 weeks | 20/20-1 | 14 | 14 | Attached, resolved VH and CR |
| 7 | 47 | F | OS | 20/16-2 | 14 | Cord with handles | Slipped | Home | Eyelid ecchymosis | None | Observation | 0 | ||||
| 8 | 67 | F | OS | 20/63 | 30 | Flat loop | Slipped | Exercise class | Traumatic iritis, dislocated lens, vitreous prolapse, angle recession, traumatic mydriasis | VH | 1. IOP lowering and corticosteroid drops 2. PPV/lensectomy/SF-PCIOL |
4 minutes | 20/40 | 40 | 20 | Attached, SF-PCIOL, traumatic mydriasis |
| 9 | 16 | F | OS | 20/16-1 | 15 | Unspecified | Slipped | Gym | None | CR | Observation | 0 | ||||
| 10 | 43 | F | OD | 20/20 | 16 | Unspecified | Slipped | Exercise class | Traumatic iritis | VH, SRH, CR | Observation | 5 weeks | 20/16-1 | 17 | 17 | Attached, resolved SRH and CR |
| 11 | 67 | M | OS | 20/100 | 10 | Unspecified | Slipped | Gym | None | VH, RRD, PVR | 1. SB/PPV/MP/AFx/EL/Gas 2. PPV/MP/AFx/EL/SiO 3. SOR/MP/inferior relaxing retinotomy/AFx/SIO 4. Intravitreal methotrexate ×3 |
6 minutes | 20/400 | 26 | 8 | Attached |
| 12 | 19 | M | OD | 20/25 | 9 | Cord with handles | Slipped | Home | Traumatic iritis, hyphema, angle recession | Initially: Avulsed vitreous base, CR, VH, PH 3m: RRD, PVR |
1. Topical steroids, cyclopentolate, IOP lowering drops 2. SB/PPV/AFx/EL/Gas |
5m | 20/63 | 26 | 12 | Attached |
| 13 | 19 | M | OS | 20/20 | 16 | Cord with handles | Slipped | Home | Traumatic iritis | RH | Corticosteroid and cyclopentolate drops | 5 minutes | 20/13 | 16 | 14 | Attached, resolved RH |
Injured by another user.
Injury occurred while supervised by personal trainer.
AFx, air fluid exchange; CHR, choroidal rupture; CR, commotio retinae; EL, endolaser; F, female; HM, hand motion; M, male; mac, macular; MH, traumatic macular hole; MP, membrane peel; OD, right eye; OS, left eye; PH, preretinal hemorrhage; PPV, pars plana vitrectomy; PVR, proliferative vitreoretinopathy; RH, retinal hemorrhage; RPE, retinal pigment epithelium; RRD, rhegmatogenous retinal detachment; SB, scleral buckle; SF-PCIOL, scleral fixated posterior chamber intraocular lens; SiO, silicone oil; SOR, silicone oil removal; SRH, subretinal hemorrhage; VH, vitreous hemorrhage.
We found seven eyes (54%) with traumatic iritis, four eyes (31%) with angle recession, two eyes (15%) with corneal abrasion, and traumatic mydriasis, iris sphincter tears, hyphema, lens dislocation, anterior vitreous prolapse, and zonular dialysis in one eye each. Meanwhile, four eyes (31%) had unremarkable anterior segment examinations. We encountered no globe ruptures in our cohort. Regarding the posterior segment, we encountered seven eyes (54%) with vitreous hemorrhage and seven eyes (54%) with peripheral commotio retinae. Macula-involving commotio retinae, peripheral subretinal hemorrhage, peripheral retinal hemorrhages, rhegmatogenous retinal detachment, and proliferative vitreoretinopathy were observed in two eyes (15%) each, respectively. Vitreous base avulsion, peripheral choroidal rupture, and traumatic macular hole (Figure 1) were observed in one eye (8%) each, respectively. Three eyes (23%) had unremarkable funduscopic examinations. Seven eyes (54%) were observed without intervention, five eyes (38%) were treated with prescription eye drops, and three eyes (23%) required surgical intervention for retinal detachment or dislocated lens. For the nine eyes with serial examinations, five (56%) had unremarkable final fundoscopic exams, two (22%) developed macular atrophy as the result of traumatic pigment epitheliopathy, one (11%) possessed peripheral retinal atrophy, and another (11%) peripheral subretinal fibrosis (Figure 1).
Fig. 1.
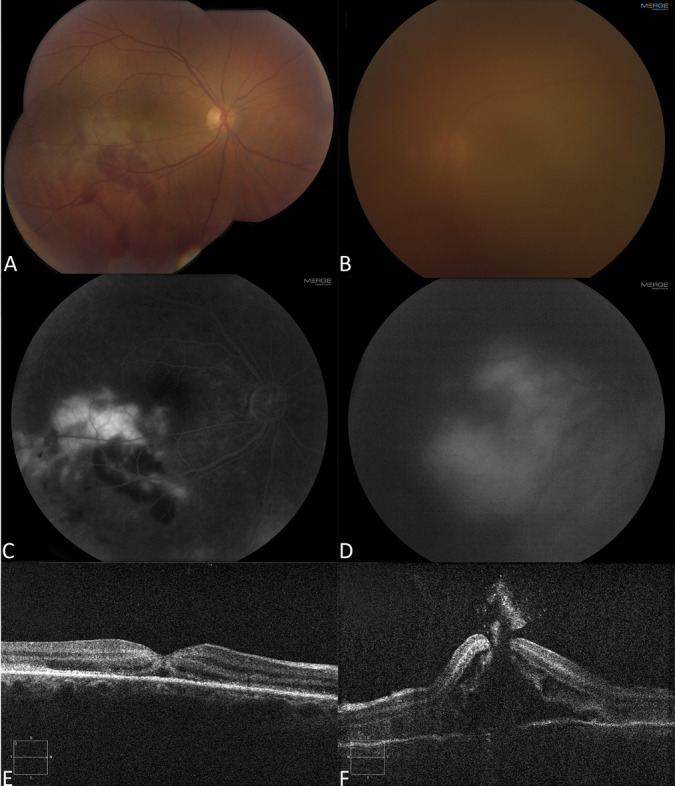
Thirty-three-year-old man who sustained injury to both eyes from recoil of ruptured elastic exercise band. A. Fundus photo of the right eye showing mild vitreous hemorrhage, macular commotio retinae, and subretinal hemorrhage. B. Fundus photo of the left eye showing significant vitreous hemorrhage obscuring details of the posterior segment. C. Fluorescein angiography of the right eye with hyperfluorescence in the area affected by commotio retina indicating traumatic retinal pigment epitheliopathy and hypofluoresence due to blockage from subretinal hemorrhage. D. Late fluorescein angiography of the left eye with diffuse hyperfluorescence in the macula suggestive of traumatic retinal pigment epitheliopathy, and a faint outline of a macular hole. E. Spectral domain-optical coherence tomography of the right eye showing temporal hyperreflectivity in the outer retina and subretinal fluid at the fovea. F. Spectral domain-optical coherence tomography of the left eye showing traumatic macular hole with intraretinal and subretinal fluid.
Discussion
Although exercise band injuries are well known in the world of litigation and have led to multiple product recalls,1 they have only been infrequently described in the medical literature. To the best of our knowledge, there are five case reports detailing unilateral exercise band injuries in seven eyes (Table 2).2–6 Elastic exercise band injury is similar in mechanism to the well-reported cases of bungee cord associated trauma, wherein elastic cords that were stretched to high tension and anchored by a metal hook were inadvertently released with resultant recoil that caused blunt ocular trauma.7 The clinical manifestations of elastic band injury were markedly less severe than what has been reported with bungee cord associated ocular trauma.7 This distinction is most likely because of the absence of a metal hook on elastic exercise bands. The relatively milder sequelae of elastic band injuries may explain why there are only few reported cases. Still, they are not without unexpected danger.
Table 2.
Summary of Previously Reported Cases
| Authors | Age (years) | Sex | Eye | Best Corrected Initial Vision (Snellen) | Type of Elastic Band | Mechanism | Setting of Injury | Initial IOP (mmHg) | Previous Ocular History | Anterior Segment Findings | Posterior Segment Findings | Intervention | Duration of Follow-up (months) | Final Vision (Snellen) | Max IOP (mmHg) | Final IOP (mmHg) | Final Anatomic Status |
| Ducharme and To2 | 43 | F | OS | 20/60 | Cord with handles | Slipped | Aerobics class | 24 | Undisclosed | Subconjunctival hemorrhage, hyphema, traumatic mydriasis | None | IOP lowering, corticosteroid, and cyclopentolate drops. | 1 | “Normal” | 24 | “Normal” | Attached |
| Kollbaum et al3 | 26 | M | OS | HM | Unspecified | Slipped* | Gym | Undisclosed | None | Traumatic iritis, hyphema, iris sphincter tear, angle recession | PH, RH | IOP lowering, corticosteroid, and homatropine drops | 0.5 | Undisclosed | Undisclosed | Undisclosed | Undisclosed |
| Joondeph SA and Joondeph BC4 | 25 | M | OD | 20/30 | Flat loop | Snapped | Crossfit class | Undisclosed | None | None | Retinal dialysis, avulsed vitreous base, RRD | SB | 4 | 20/25 | Undisclosed | Undisclosed | Attached |
| Wangsathaporn and Tsui5 | 7 | F | OS | 20/200 | Unspecified | Snapped* | Home | Undisclosed | None | Traumatic iritis | Mac-CR, CR, RRD | SB | 12 | 20/30 | Undisclosed | Undisclosed | Attached, outer retinal atrophy in macula |
| Rosignoli et al6 | 48 | F | OD | LP | Unspecified | Unspecified recoil | Home | 40 | 1. RRD OD s/p SB/PPV/AFx/EL/Gas 19 days prior | Hyphema, dislocated lens | None | 1. IOP lowering drops and oral acetazolamide. 2. PPV/lensectomy |
3.5 | 20/20† | 40 | “Normal” | Attached |
| Rosignoli et al6 | 72 | M | OD | LP | Unspecified | Unspecified recoil | Exercise class | 49 | 1. Pseudophakia OD. 2. Advanced glaucoma. 3. RRD OD s/p PPV/AFx/EL/Gas 14 days prior |
Hyphema, iridodonesis, traumatic iritis, dislocated PCIOL | None | 1. IOP lowering drops and oral acetazolamide. 2. PPV, removal of dislocated IOL. 3. SF-PCIOL |
6 | 20/100 | 49 | “Normal” | Attached |
| Rosignoli et al6 | 74 | M | OD | HM | Unspecified | Unspecified recoil | Home | 35 | 1. Pseudophakia OD 2. Primary open angle glaucoma s/p trabeculectomy |
Hyphema, vitreous prolapse into AC, dislocated PCIOL | VH | 1. IOP lowering drops. 2. PPV with peripheral iridectomy and repositioning of IOL into AC. 3. IOL exchange with SF-PCIOL |
7 | 20/30 | 35 | “Normal” | Attached |
Injured by close proximity to another user.
Best corrected vision with contact lens.
AC, anterior chamber; AFx, air fluid exchange; CR, commotio retinae; EL, endolaser; F, female; HM, hand motion; LP, light perception; M, male; mac, macular; OD, right eye; OS, left eye; PH, preretinal hemorrhage; PPV, pars plana vitrectomy; RH, retinal hemorrhage; RRD, rhegmatogenous retinal detachment; SB, scleral buckle; SF-PCIOL, scleral fixated posterior chamber intraocular lens; VH, vitreous hemorrhage.
Exercise bands are generally manufactured as flat, tubular rubber straps or rubber cords with handles at the ends. They are a popular form of strength training because of their affordability, portability, and ease of use. Exercise band users strength train by repeatedly generating the force required to overcome the resistance of and then elongate the band. The bands are generally anchored under feet, toes, or to a heavy, immobile fixture. The user then maintains baseline tension by grasping a terminal loop or handle and stretching the band until it is taut. Next, the elastic band is further elongated through extremity flexion or extension. The degree of resistance encountered can be adjusted based on altering the thickness of the band or baseline tension. The elasticity of exercise bands is created by use of synthetic rubber that is, augmented by plasticizers, substances added during the manufacturing process to increase flexibility, workability, or distensibility.8
All of the patients in this report sustained injury when the resistance band slipped from the anchoring point at high tension and resulted in high velocity recoil. Breakage of elastic bands has also been reported as a cause of recoil (Table 2).4,5 Degradation of the rubber and incorporated plasticizers from exposure to high temperature, light, and ozone, and repeated high tension stretching may have resulted in the rupture of the elastic bands.9 Patients were generally performing arm flexion, deltoid flexion, deltoid abduction, seated or standing rows, or a “rear-deltoid fly” exercise, which entails deltoid abduction in the transverse plane. In all described scenarios, the anchoring points of the resistance bands were under or anterior to the user, creating a trajectory towards the user's face and eyes during exercise band recoil. Of note, two previously described patients and one individual in this series were injured by being in close proximity to an elastic band user (Tables 1 and 2).3,5 Blunt ocular trauma from recoiling resistance bands can result in significant coup and contrecoup mechanical injury. The compressive mechanical forces can also cause equatorial expansion of the globe and exert traction on vitreous attachment points at the vitreous base, optic nerve, and macula, which can result in retinal tears, traumatic macular holes, and acute posterior vitreous detachment.10 We suspect the equatorial expansion of the globe and resultant centrifugal forces led to the development of zonular dehiscence and iris sphincter rupture in some patients.
Temporary vision loss was observed in injured eyes that possessed lens dislocation, vitreous hemorrhage, mild macular commotio retinae, and a traumatic macular hole that closed spontaneously. More permanent vision loss resulted from macular damage associated with severe macular commotio retina with traumatic pigment epitheliopathy or retinal detachment. Four eyes (31%) also developed traumatic angle recession, and possess risk of permanent vision loss from glaucomatous optic neuropathy. Overall, three eyes (23%) required surgical intervention. Of the eyes with follow-up, five (56%) have final vision worse than 20/40. Blunt trauma with elastic exercise bands should be considered a serious ocular injury with significant potential to result in irreparable vision loss.
Patients who were men or possessed bilateral eye injuries from recoiling elastic bands were found to have more severe ocular trauma. The final visual acuity for male eyes ranged from 20/13 to 20/400 (median: 20/40-2), and from 20/16 to 20/40 (median: 20/20) for female eyes. When compared with those who suffered unilateral injuries, patients with bilateral trauma were found to have higher incidence of angle recession glaucoma (75% vs 11%), macular atrophy from traumatic macular pigment epitheliopathy (50% vs 0%), traumatic macular hole (25% vs 0%), avulsed vitreous base (25% vs 0%), rhegmatogenous retinal detachment (25% vs 11%), and proliferative vitreoretinopathy (25% vs 11%). Male patients likely used exercise bands with more resistance or stretched the bands to higher tension, resulting in recoil with relatively greater force compared with their female counterparts. The nasal bridge would be expected to protect patients from sustaining bilateral injury, but occasionally the recoiling band possesses sufficient force to rapidly conform around the bridge of the nose and then strike both eyes. The greater force of impact most likely explains the worse outcomes in patients with bilateral injury. Variations in facial anatomy, such as the flatter nasal bridges of Asian races, may also determine frequency of bilateral injury, but both men (Caucasian and Middle Eastern) in this series who sustained bilateral injury possessed prominent nasal bridges.
Users of elastic exercise bands should regard them as an exercise tool with a limited service life. Exercise bands should be stored in a cool, dry, and shaded location to minimize degradation, and inspected carefully for signs of compromise before use. Manufacturers can make their product safer by indicating an expiration date, or provide complementary pairs of safety glasses with every purchase of exercise bands. Although none of the patients with ocular injuries caused by exercise bands wore protective eyewear at the time of injury, it is not an unreasonable safety precaution.
Footnotes
Supported by San Francisco Retina Foundation.
None of the authors has any financial/conflicting interests to disclose.
Contributor Information
William Carrera, Email: wmc16@case.edu.
Michelle Y. Peng, Email: michypeng@gmail.com.
Anita Agarwal, Email: anita.agarwal@vanderbilt.edu.
Judy J. Chen, Email: Judyjchen@gmail.com.
Robert N. Johnson, Email: bj.johnson@comcast.net.
James M. Jumper, Email: jmichaeljumper@gmail.com.
Henry R. McDonald, Email: hrichardmcdonald@gmail.com.
References
- 1.Resistance Band Injury Lawsuit|Lawyer, Attorney [Internet]. 2020. Schmidtlaw.com. Available at: https://www.schmidtlaw.com/resistance-band-injury-lawsuit/. Accessed July 9, 2020. [Google Scholar]
- 2.Ducharme J, To KW. Exercise band-induced hyphema. Arch Ophthalmol 1995;113:142. [DOI] [PubMed] [Google Scholar]
- 3.Kollbaum E, Henderson P, Hitzeman S. Multiple ocular consequences to blunt trauma injury: poster# 70. Optom Vis Sci 2001;78:171. [Google Scholar]
- 4.Joondeph SA, Joondeph BC. Retinal detachment due to CrossFit training injury. Case Rep Ophthalmologic Med 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wangsathaporn K, Tsui I. Commotio retinae resulting from rubber band injury in two girls. Ophthalmic Surg Lasers Imaging Retina 2019;50:309–313. [DOI] [PubMed] [Google Scholar]
- 6.Rosignoli LM, Regan KA, Gray MJ, et al. Exercise band-induced lens dislocations: a case series. Am J Ophthalmol Case Rep 2019;15:100496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hollander DA, Aldave AJ. Ocular bungee cord injuries. Curr Opin Ophthalmol 2002;13:167–170. [DOI] [PubMed] [Google Scholar]
- 8.Brazel CS, Rosen SL. Fundamental principles of polymeric materials. 3rd ed. Hoboken: John Wiley & Sons, 2012. Chapter 7.11: Concentrated solutions: Plasticizers. p. 122–124. [Google Scholar]
- 9.Li GY, Koenig JL. A review of rubber oxidation. Rubber Chem Technol 2005;78:355–390. [Google Scholar]
- 10.Johnson RN, McDonald HR, Lewis H, et al. Traumatic macular hole: observations, pathogenesis, and results of vitrectomy surgery. Ophthalmology 2001;108:853–857. [DOI] [PubMed] [Google Scholar]


