ABSTRACT
The aim of this study was to review the available literature on the efficacy and safety of the Rezum system for the treatment of symptomatic benign prostatic hyperplasia (BPH). A revision of literature up to January 2021 was carried out. Medline, Scopus, Web of Science, and PubMed archives were screened to identify all the relevant studies investigating the role of Rezum in the treatment of BPH. Randomized controlled trial (RCT), retrospective, prospective, observational, and comparative studies were included. Finally, 17 studies were included, five of which reporting data of a double blind Rezum RCT. Overall, 1,451 patients underwent Rezum procedure. All the studies performed a minimum of 3 months follow-up. Preoperatively, the mean International Prostate Symptom Score (IPSS) score was 19.8, mean Qmax was 9.2 mL s−1, and mean PVR was 142 cc. At 3 months after surgery, the mean IPSS score was 1.5, mean Qmax was 13.7 mL s−1, and mean PVR was 74 cc. Six studies investigated sexual function, most of them using the International Index of Erectile Function (IIEF)-5 questionnaire and a few also the Male Sexual Health Questionnaire (MSHQ). Preoperative mean IIEF-5 score was 18.5, and the mean MSHQ score was 7.4. At the 3 months follow-up, the mean IIEF-5 score was 16.4, and the mean MSHQ score was 9.62. None of the studies reported intraoperative complications. Rezum system is a novel minimally invasive treatment for symptomatic BPH using transurethral water vapor thermal energy. It represents a cost-effective and safe procedure with durable relief of lower urinary tract symptom, preservation of sexual function, low complications rate, and short recovery time.
Keywords: Lower urinary tract symptoms, prostatic hyperplasia, Rezum, therapeutics.
Main Points
New promising minimally invasive surgical therapies (MISTs) for the management of symptomatic BPH have increased to reduce the risk of adverse events, particularly with regard to sexual function preservation.
Rezum system is a novel minimally invasive treatment for symptomatic BPH using transurethral water vapor thermal energy.
It represents a safe and effective procedure with durable relief of LUTS, preservation of sexual function, low complications rate, and short recovery time.
Introduction
Symptomatic benign prostatic hyperplasia (BPH) presents clinically when the benign prostatic enlargement (BPE) compresses the prostatic urethra with bladder outlet obstruction leading to lower urinary tract symptoms (LUTSs), ranging from urinary storage to voiding issues. Urinary obstruction can cause acute urinary retention (AUR), urinary tract infection (UTI), bladder stones, and renal failure with impairment of health-related quality of life and significant socioeconomic problems to public health systems worldwide.1
BPH represents one of the most important clinical challenges that urologists will need to face in upcoming times.2 Due to high prevalence of this disease in aging males, accumulation of postponed elective surgeries caused by the COVID-19-related pandemic era, and potential worsening of the underlying clinical condition, more BPH surgeries will need to be performed given the increasing waiting lists.3
According to the European Association of Urology guidelines and other international societies, the management of BPH includes conservative approach, pharmacotherapy (i.e., alpha blockers and 5-alpha reductase inhibitors), and surgical treatment focusing on patient relief from LUTS secondary to BPE.
In this regard, pharmacological treatments could provide unsatisfactory LUTS relief, with potential side effects such as orthostatic hypotension, asthenia, and sexual dysfunction. Nowadays, minimally invasive surgical therapies (MISTs) are increasingly offered as a mainstay treatment for BPH, and several options are available. The gold standard for small/moderate prostate sizes is still considered as the transurethral resection of the prostate (TURP).4 However, this can have relatively high rates of intraoperative and postoperative complication, including moderate risk of bleeding, readmissions, retrograde ejaculation, and longer operative and anesthetic time.5
Consequently, over the last decades, new promising MISTs for the management of symptomatic BPH have increased to reduce the risk of adverse events, particularly with regard to sexual function preservation.6 The introduction of these techniques could be relevant especially in the COVID-19 period, when the need to further reduce operating time, hospital stay, and risks of general anesthesia is more important than ever for the patients.6
In this context, the recently developed Rezum System (Rezum®, Boston Scientific Company Inc., Marlborough, MA, USA) represents the unique transurethral MIST that uses convective water vapor energy by radiofrequency. The procedure provides water vapor thermal energy to rapidly ablate the obstructive prostatic tissue, including the median lobe, while preserving sexual function (anterograde ejaculation).
Thermodynamically, this approach contrasts with the conductive characteristics of other MISTs, such as transurethral microwave and radiofrequency modalities. Convection is the movement of heated gas or liquid within a defined space,7 without a discernible thermal gradient with quick disruption of membrane cells.
Whereas conduction is the transfer of heat through a nonmoving material from the area of higher to lower temperature that requires long treatment times and considerable energy deposition, to imply tissue destruction with an obligatory temperature gradient.7–9
The Rezum system, which involves an endoscopic approach, consists of injecting water vapor (generated via inductive coil heater) into the transition zone of the prostate, at approximately 103°C.
Rezum thermal therapy can also be performed under local anesthesia in most cases, or with oral sedation as well as prostate block, and intravenous sedation followed by post-treatment analgesic, limiting the risks related to general or spinal anesthesia in anticoagulated patients and with other comorbidities.10
Thus, the aim of this study was to perform a literature review in order to assess the efficacy and safety of the Rezum system for the treatment of BPH.
Methods
Evidence Acquisition
We performed a review of English-language literature available up until January 2021. Medline, Scopus, Web of Science, and Embase archives were screened using a single query to identify all the relevant studies investigating the role of Rezum in the treatment of BPH. The following terms were included: (benign prostate hyperplasia) OR (bph) OR (LUTS) AND (Rezum) OR (Water vapor) OR (Steam). Randomized clinical trials, retrospective, prospective, observational, and comparative studies on human adults were included in the review. Case reports, commentaries, letters to the editor, reviews, and non-English articles were excluded a priori. Two different authors did independently the data extraction, and subsequently, they crosschecked it. Conflicts were resolved by discussion or with an independent arbiter.
Titles and abstracts were examined, and manuscripts were classified. Then, full-text articles were examined. References from the selected studies were also hand investigated to identify additional reports. An excel file was created respecting the following criteria: participants, interventions, comparators, outcomes, and study design. The median patient age was collected. The baseline characteristics of population were recorded, including Charlson Comorbidity Index, body mass index, and previous or current drugs. Preoperatively, the LUTSs were explored using the uroflowmetry with postvoid residual volume, the International Prostate Symptom Score (IPSS) questionnaire, the Male Sexual Health Questionnaire (MSHQ), the Overactive Bladder symptoms score, and the International Continence Society “male” questionnaires. Sexual activity was scored by the International Index of Erectile Function (IIEF-5). The biometric assessment of the prostate (volume) was ultrasonographical determined. Data on the Rezum technique were included, such as operative time, median number of lobe injections, and occurrence of intraoperative complications. Outcomes were then evaluated postoperatively. The median follow-up period was included, focusing on short- and long-term complications.
For descriptive data, medians with range (minimum and maximum values) were used. All collected data were evaluated using Statistical Package for Statistical Sciences, version 25.0 (IBM SPSS Corp.; Armonk, NY, USA).
Technical Details
The Rezum system consists of injecting water vapor into the transition zone of the prostate, at approximately 103°C. When heated to steam, water expands approximately 1,700 times its liquid volume and carries up to 540 calories of energy per gram.7 This stored thermal energy is released when the steam phase shifts or condenses from vapor to liquid upon contact with tissue.7
This water vapor (0.5 mL) is convectively delivered in a 9-second site injection reaching temperatures between 70°C and 80°C, which disperses circumferentially in the tissue interstices creating a 1.5-2.0 cm confined thermal lesion.7 , 9
The needle is retracted after each treatment and repositioned in 1 cm increments distal from the previous site to the end of the prostatic tissue just proximal to the verumontanum.9 The objective of the treatment is to create contiguous, overlapping lesions running parallel to the natural slope of the urethra9 that will result in tissue necrosis and shrinkage in the transition zone of the prostate over a few months.
Results
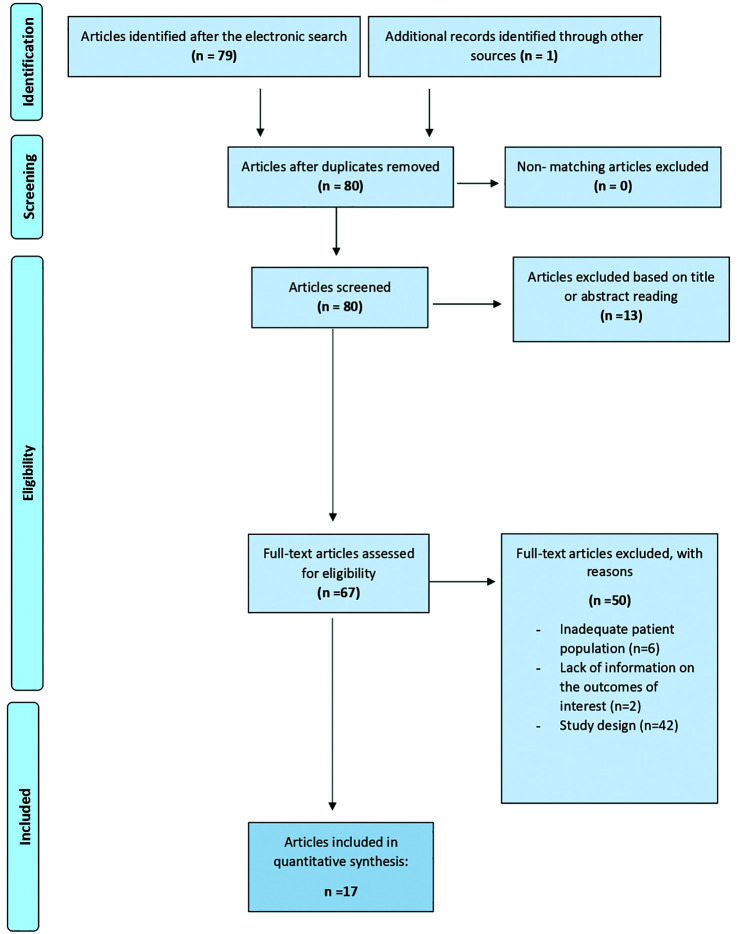
Seventeen studies were finally selected for the review (Figure 1). Among these, five studies reported data of a double blind randomized controlled trial (RCT) study with a 4-year follow-up,11–15 six were retrospective studies,16–21 four were prospective studies,5,22–24 and two were preliminary reports of which one compared the Rezum System with the Urolift system.6,25 Overall, 1,481 patients underwent the surgical procedure. The mean age was 67.9 years (range: 66-76 years). Postoperatively, the mean follow-up period was 13 months (range: 2-48 months).
Figure 1.
Flow chart of the identified studies (Medline, Scopus, Web of Science, and Embase archives).
All of the studies included in the review compared preoperative clinical data to the postoperative outcomes in terms of urinary function and complications, while six studies also explored sexual function.
Overall, 1,451 patients underwent Rezum procedure, and 91 patients underwent other techniques included in two case/control studies. The mean prostate volume was 52 g (range: 30-140 g); large glands (>80 g) were included in a study that investigated the outcomes in Rezum system considering small versus large glands.
Urinary Function
Most of the studies investigated the urinary function using IPSS, post void residual (PVR), and flow rate (Qmax) at the uroflowmetry, recorded preoperatively and during the follow-up. All of the studies performed a minimum of 2 months follow-up, others reached 6 and 12 months, and one study performed a follow-up of 48 months. Preoperatively, the mean IPSS score was 19.8, the mean Qmax was 9.2 mL s−1, and the mean PVR was 142 cc. At 3 months after surgery, the mean IPSS score was 1.5, mean Qmax was 13.7 mL s−1, and mean PVR was 74 cc.
The average improvement of IPSS, Qmax, and PVR outcomes at 3 and 12 months follow-up was summarized in Table 1.
Table 1.
Urinary Function Outcomes After Rezum, at 3 and 12 Months Follow-Up
| Year | Study Design | Author | Number of Participants | Duration of Follow-Up (Months) | IPSS (%Reduction) 3 Months | IPSS (%Reduction) 12 Months | Qmax mL s–1 (%Improvement) 3 Months | Qmax mL s–1 (%Improvement) 12 Months | PVR (%Reduction) 3 Months | PVR (%Reduction) 12 Months | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | Multicenter double blinded RCT (4 years data) | McVary et al.11 | 197 | 48 | 52 | 53 | 64 | 55 | 13 | 5 | |
| 2020 | Multicenter retrospective study | Alegorides et al.16 | 62 | 12 | 60 | 62 | 31 | 47 | 68 | 79 | |
| 2017 | Multicenter retrospective study | Darson et al.17 | 131 | 12 | 50 | 48 | 34 | 16 | 60 | 64 | |
| 2015 | Multicenter prospective pilot study (1 year data) | Dixon et al.22 | 65 | 12 | 62 | 57 | 62 | 62 | 35 | 31.70 | |
| 2020 | Comparative retrospective study | Bole et al.21 | 182 | 3 | n/a | n/a | 40 | n/a | 48 | n/a | |
| 2020 | Preliminary comparative report | Tutrone et al.25 | 53 | 2 | 46 | n/a | n/a | n/a | n/a | n/a | |
| 2017 | Retrospective study | Mollengarden et al.19 | 129 | 12 | 54 | n/a | 54 | n/a | 33 | n/a | |
| 2020 | Multicenter Retrospective study | McVary et al.18 | 38 | 27 | n/a | n/a | n/a | n/a | n/a | n/a | |
| 2021 | Pilot study prospective | Haroon et al.5 | 10 | 3 | 75 | n/a | 45 | n/a | 74 | n/a | |
| 2016 | Multicenter prospective pilot study (2 year data) | Dixon et al.23 | 65 | 24 | 62 | 57 | 62 | 62 | 35 | 32 | |
| 2021 | Retrospective study | Garden et al.20 | 204 | 3 | 32 | n/a | 55 | n/a | 30 | n/a | |
| 2020 | Preliminary report | Johnston et al.6 | 210 | 12 | 71 | 79 | 72 | 96 | 41 | 37 | |
| 2021 | Multicenter prospective study | Siena et al.24 | 135 | 6 | 80 | n/a | n/a | n/a | n/a | n/a | |
| %Improvement | 59 | 59 | 52 | 56 | 44 | 41 |
Sexual Function
Six studies investigated sexual function in patients who underwent Rezum treatment. Most of them used the IIEF-5 questionnaire and a few also used the MSHQ. The presence of ejaculatory disorders in the postoperative period was also assessed in four different studies.
The preoperative mean IIEF-5 score was 18.5, and the mean MSHQ score was 7.4. At 3 months follow-up, this improved to a mean IIEF-5 score of 16.4 and a mean MSHQ score of 9.62. As regard to the ejaculatory disorders in the postoperative period, one study reported an ejaculatory volume reduction in 2% of patients at 3/6 months after surgery, one study reported ex novo anejaculation at 1 year follow-up in 10.8% of patients and reduction of ejaculatory volume in 10.8%, with one study which described ex novo both anejaculation and erectile disfunction in 3.1% of patients.
The average improvement of IIEF scores at 3 and 12 months follow-up was summarized in Table 2.
Table 2.
Sexual Function Outcomes After Rezum, at 3 and 12 Months Follow-Up
| Year | Study Design | Author | Number of Participants | Duration of Follow-Up (Months) | IIEF (%Improvement) 3 Months | IIEF (%Improvement) 12 Months | |
|---|---|---|---|---|---|---|---|
| 2019 | Multicenter double blinded RCT (4 years data) | McVary et al.11 | 197 | 48 | 0 | 1.30 | |
| 2020 | Multicenter retrospective study | Alegorides et al.16 | 62 | 12 | 2 | 0 | |
| 2017 | Multicenter retrospective study | Darson et al.17 | 131 | 12 | n/a | n/a | |
| 2015 | Multicenter prospective pilot study (1 year data) | Dixon et al.22 | 65 | 12 | n/a | n/a | |
| 2020 | Comparative retrospective study | Bole et al.21 | 182 | 3 | n/a | n/a | |
| 2020 | Preliminary comparative report | Tutrone et al.25 | 53 | 2 | n/a | n/a | |
| 2017 | Retrospective study | Mollengarden et al.19 | 129 | 12 | n/a | n/a | |
| 2020 | Multicenter retrospective study | McVary et al.18 | 38 | 27 | n/a | n/a | |
| 2021 | Pilot study prospective | Haroon et al.5 | 10 | 3 | n/a | n/a | |
| 2016 | Multicenter prospective pilot study (2 year data) | Dixon et al.23 | 65 | 24 | n/a | n/a | |
| 2021 | Retrospective study | Garden et al.20 | 204 | 3 | –9 | n/a | |
| 2020 | Preliminary report | Johnston et al.6 | 210 | 12 | 16 | 36 | |
| 2021 | Multicenter prospective study | Siena et al.24 | 135 | 6 | –37.50 | n/a | |
| %Improvement | –6 | 12 |
Complications
All the procedures were successfully performed with no intraoperative complications. Early postoperative complications included clot retention (2-4%), AUR (11-32%), and blood transfusion in two patients, who were involved in a specific case/control study with large prostate glands (>80 g). Late complications comprised AUR (5%), UTI, and LUTS such as dysuria, urinary urgency, hematuria, and nocturia (10-20% of all patients). The mean time of postoperative catheterization was 8.8 days. There are no readmissions rates reported in the studies.
Reoperation Rates
Overall, the average retreatment rate in the studies during follow-up with a surgical or minimally invasive procedure was 1.0935%; specifically, patients retreated with Rezum system were 1.075%, patients retreated with TURP were 0.0185%, and those receiving other surgical treatments were 0.006%.
Discussion
The first transurethral ablative surgery for BPH was performed in 1926, becoming over a next few decades the gold standard treatment in patients not responding to medical therapy.
Although TURP proved to be effective for reducing LUTS symptoms, this technique has several reported limitations, mainly due to the notable side effects in elderly patients with comorbidities.
In the last decade, novel MISTs-like Rezum System has been developed to offer an effective and safer procedure for BPH-related LUTS management.
The main outcome measures have been published by McVary et al.11 in the only double blind Rezum RCT, reporting a significant and long-term mean IPSS score improvement. After unblinding at 3 months, IPSS was reduced by 50% compared to 20% in the control group (P < .0001); thus, control subjects were requalified for the crossover study, and mean IPSS improvement from baseline remained significant from the early response at 3 months (49.9%) to 1 year (52.2%), 2 year (50.7%), 3 year (49.7%), and 4 year (46.7%), P < .0001. These data were in accordance with other significant improvements in IPSS quality of life (QoL) (42.9%, P < .0001) and in Qmax (49.5%, P < .0001) at a 4-year follow-up.11 These data on urinary outcomes are confirmed also in the largest European multicenter series recently reported by Siena et al.24 on 680 patients. They report a median Qmax of +8.9 mL s−1 (IQR 5-13), median IPSS of –12 (P < .01), and a median PVR of –65.6 cc (P < .001).
Dixon et al.23 in their multicenter prospective pilot study highlighted the long-term efficacy of Rezum, with 2 years follow-up. At the 12-month follow-up, IPSS score was reduced by 56%, durable at 24 months (55%), P < .001. Also, QoL and Qmax significantly improved.
The targeted prostate tissue ablation may be applied to all zones of the gland including an enlarged central zone and median lobe with similar symptom improvement, as reported in most of the studies.
To date, only two studies investigated the efficacy of Rezum specifically in large prostate glands (≥80 cc).
Bole et al.21 published the first preliminary report to compare the use of Rezum in large prostate glands (≥80 cc) to small prostate glands (<80 cc), demonstrating its short-term safety and efficacy with statistically significant improvement at 3 months, of IPSS, peak flow, and PVR. Moreover, in a subgroup of catheter-dependent patients, the postoperative catheter free rate was 83% for men with glands >80 cc, which was comparable to 88% in the smaller gland group,21 suggesting another valid application of Rezum.
Garden et al.20 also compared the successful outcomes of Rezum between men with small (<80) and large prostates (≥80 cc). Similar to previous findings, for selected patients with sufficient longitudinal follow-up, Rezum effectively improved Qmax and PVR in large prostates, offering short-term symptomatic relief. Conversely, Rezum did not significantly reduce the rates of intermittent catheterization.
In a recent study, McVary et al.18 conducted a retrospective analysis of 38 catheter-dependent men with complete urinary retention, showing that Rezum can be an effective and a safe surgical option, with 70% catheter free patients in a median of 26 days after the procedure.
As regards the safety profile of Rezum, the early complications reported were transient and mild, typical of endoscopic procedures. The most represented were dysuria, AUR, UTI, hematuria, urgency, and frequency. Furthermore, the mean period of postoperative catheterization was 8.8 days, and this could also be related to early adverse events.
Johnston et al.6 reported a feedback in the form of free text comments from patients and noted that the duration of a catheter postoperatively and irritative symptoms in the initial recovery period was the main drawbacks of Rezum. Even so, patients’ satisfaction rates were high.
Only two patients needed blood transfusions, and they were included in a specific case/control study with a large prostate gland (≥80), but postoperative complication rate was not significantly different between large and small glands.21
Although Garden et al.20 reported no difference in UTI rates, in their case series, patients with a large prostate gland were at higher risk of urosepsis after Rezum.
The rate of Rezum retreatment or additional BPH surgery seems to be <5% at 4 years.6,10–17,19,20,22,23,25
In the Rezum RCT study, the retreatment rate with a surgical or minimally invasive procedure was 4.4% (6 of 135 subjects) over 4 years of follow-up. Six patients underwent a secondary treatment for LUTS (one open prostatectomy, three plasma-button transurethral vaporization of the prostate, and two retreated with the Rezum procedure), four of these secondary interventions were related to the presence of a median lobe that was identified but nontreated.11
The same authors updated their data at 5 years follow-up, and the retreatment rate remained unchanged (4.4%), while 11.1% of the treatment-arm subjects initiated BPH medication.26
As far as sexual function is concerned, McVary et al.11 assessed data of RCT for a change in MSHQ function and IIEF-EF scores. MSHQ did not change significantly from the baseline at 12-month and 24-month follow-up. However, MSHQ declined significantly to 13.6% (P = .0046) and 14.2% (P = .0038) at 36 and 48 months, respectively. Meanwhile, the MSHQ bother score had a significant decline (12 months P = .0017, 24 months P = .0118, and 36 months P = .0153) until the 48-months follow-up (P = .6495). There was no significant declining in the IIEF-EF score from 12 months (P = .7054) to 48 months follow-up (P = .0333). No treatment or device-related de novo ED was reported during the 12-month period after treatment.11
Dixon et al.23 did not report a significant increase in the IIEF and MSHQ scores at the 3 month to 24 month follow-up. Even then, no sexually related adverse events were reported.
Alegorides et al.16 assessed the rates of sexually active patients, showing identical results preoperatively (90.7%) and at 1 year (90.2%). The IIEF-5 score was not different postoperatively and remained stable throughout the duration of the 12 month follow-up. At 1 year, the MSHQ score had increased by an average of two points (P = .056).16 Their study showed the higher rate of ex novo anejaculation (10.8%)16 against lower rates (3.1%) reported by Mollengarden et al.19
Cost effectiveness analysis was not considered in all these studies. Recently, Ulchaker et al.27 provided a pre- and postoperative cost-effectiveness analysis of six treatments for BPH. Rezum system was cheaper than TURP ($2,489 vs $4,821), having favorable cost-effectiveness and excellent safety/tolerability profile.27 Indeed, it was superior in terms of cost and efficacy to other MISTs such as Urolift and Prostiva (interstitial laser ablation).27 Future studies need to do more head to head comparisons of different form of MISTs, ideally in a randomized fashion, taking into account the QoL and cost of these treatments.
Conclusion
Rezum System is a novel minimally invasive treatment for benign prostate enlargement using transurethral water vapor thermal therapy. It seems to be an effective, safe, and cost-effective procedure. Recent data show its versatility even in catheter-dependent patients with large prostates or median lobe, preserving sexual function. This procedure can be performed in an office or ambulatory setting under local anesthesia reducing anesthetic risks and recovery time.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - A.E., O.S.; Design - A.E., O.S.; Supervision - A.E., A.D., G.I.R., L.E., S.B., O.S.; Materials - A.E.B., G.C.; Data Collection and/or Processing - A.E.B., G.C., A.L., F.E., F.V.; Analysis and/or Interpretation - A.E.B., G.C., A.L., F.E., F.V.; Literature Search - A.E.B., G.C.; Writing Manuscript - A.E., A.E.B., G.C.; Critical Review - A.D., G.I.R., L.E., S.B., O.S.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1. Suarez-Ibarrola R, Miernik A, Gratzke C, Schoeb DS. Reasons for new MIS. Let’s be fair: ITIND, urolift and rezūm. World J Urol . 2021;39:2315–2327.. 10.1007/s00345-020-03453-z) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ficarra V, Novara G, Abrate A.et al. Urology practice during the COVID-19 pandemic. Minerva Urol Nefrol . 2020;72:(3):369–375.. 10.23736/S0393-2249.20.03846-1) [DOI] [PubMed] [Google Scholar]
- 3. Amparore D, Campi R, Checcucci E.et al. Forecasting the future of urology practice: A comprehensive review of the recommendations by international and European associations on priority procedures during the COVID-19 pandemic. Eur Urol Focus . 2020;6:(5):1032–1048.. 10.1016/j.euf.2020.05.007) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Arezki A, Sadri I, Couture F.et al. Reasons to go for Rezum steam therapy: An effective and durable outpatient minimally invasive procedure. World J Urol . 2021;39:2307–2313.. 10.1007/s00345-020-03457-9) [DOI] [PubMed] [Google Scholar]
- 5. Haroon UM, Khan JS, McNicholas D, Forde JC, Davis NF, Power RE. Introduction of Rezum system technology to Ireland for treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: a pilot study on early outcomes and procedure cost analysis. Ir J Med Sci . 2021. 10.1007/s11845-021-02552-z) [DOI] [PubMed] [Google Scholar]
- 6. Johnston MJ, Noureldin M, Abdelmotagly Y.et al. Rezum water vapour therapy: Promising early outcomes from the first UK series. BJU Int . 2020;126:(5):557–558.. 10.1111/bju.15203) [DOI] [PubMed] [Google Scholar]
- 7. Dixon CM, Rijo Cedano E, Mynderse LA.et al. Transurethral convective water vapor as a treatment for lower urinary tract symptomatology due to benign prostatic hyperplasia using the rezūm(®) system: Evaluation of acute ablative capabilities in the human prostate. Res Rep Urol . 2015;7:13–18.. 10.2147/RRU.S74040) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mynderse LA, Hanson D, Robb RA.et al. Rezum system water vapor treatment for lower urinary tract symptoms/benign prostatic hyperplasia: Validation of convective thermal energy transfer and characterization with magnetic resonance imaging and 3-dimensional renderings. Urology . 2015;86:(1):122–127.. 10.1016/j.urology.2015.03.021) [DOI] [PubMed] [Google Scholar]
- 9. McVary KT, Rogers T, Mahon J, Gupta NK. Is sexual function better preserved after water vapor thermal therapy or medical therapy for lower urinary tract symptoms due to benign prostatic hyperplasia?. J Sex Med . 2018;15:(12):1728–1738.. 10.1016/j.jsxm.2018.10.006) [DOI] [PubMed] [Google Scholar]
- 10. Cantrill CH, Zorn KC, Elterman DS, Gonzalez RR. The Rezum system—A minimally invasive water vapor thermal therapy for obstructive benign prostatic hyperplasia. Can J Urol . 2019;26:(3):9787–9793.. [PubMed] [Google Scholar]
- 11. McVary KT, Rogers T, Roehrborn CG. Rezum water vapor thermal therapy for lower urinary tract symptoms associated with benign prostatic hyperplasia: 4-Year results from randomized controlled study. Urology . 2019;126:171–179.. 10.1016/j.urology.2018.12.041) [DOI] [PubMed] [Google Scholar]
- 12. McVary KT, Roehrborn CG. Three-year outcomes of the prospective, randomized controlled rezūm system study: Convective radiofrequency thermal therapy for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Urology . 2018;111:1–9.. 10.1016/j.urology.2017.10.023) [DOI] [PubMed] [Google Scholar]
- 13. McVary KT, Gange SN, Gittelman MC.et al. Minimally invasive prostate convective water vapor energy ablation: A multicenter, randomized, controlled study for the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia. J Urol . 2016;195:(5):1529–1538.. 10.1016/j.juro.2015.10.181) [DOI] [PubMed] [Google Scholar]
- 14. McVary KT, Gange SN, Gittelman MC.et al. Erectile and ejaculatory function preserved with convective water vapor energy treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: Randomized controlled study. J Sex Med . 2016;13:(6):924–933.. 10.1016/j.jsxm.2016.03.372) [DOI] [PubMed] [Google Scholar]
- 15. Roehrborn CG, Gange SN, Gittelman MC.et al. Convective thermal therapy: Durable 2-Year results of randomized controlled and prospective crossover studies for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. J Urol . 2017;197:(6):1507–1516.. 10.1016/j.juro.2016.12.045) [DOI] [PubMed] [Google Scholar]
- 16. Alegorides C, Fourmarier M, Eghazarian C, Lebdai S, Chevrot A, Droupy S. Treatment of benign prostate hyperplasia using the Rezum® water vapor therapy system: Results at one year. Prog Urol . 2020;S1166-7087:(20):30166–4.. 10.1016/j.purol.2020.05.004) [DOI] [PubMed] [Google Scholar]
- 17. Darson MF, Alexander EE, Schiffman ZJ.et al. Procedural techniques and multicenter postmarket experience using minimally invasive convective radiofrequency thermal therapy with Rezum system for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Res Rep Urol . 2017;9:159–168.. 10.2147/RRU.S143679) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McVary KT, Holland B, Beahrs JR. Water vapor thermal therapy to alleviate catheter-dependent urinary retention secondary to benign prostatic hyperplasia. Prostate Cancer Prostatic Dis . 2020;23:(2):303–308.. 10.1038/s41391-019-0187-5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mollengarden D, Goldberg K, Wong D, Roehrborn C. Convective radiofrequency water vapor thermal therapy for benign prostatic hyperplasia: A single office experience. Prostate Cancer Prostatic Dis . 2018;21:(3):379–385.. 10.1038/s41391-017-0022-9) [DOI] [PubMed] [Google Scholar]
- 20. Garden EB, Shukla D, Ravivarapu KT.et al. Rezum therapy for patients with large prostates (≥ 80 g): Initial clinical experience and postoperative outcomes. World J Urol . 2021;39:3041–3048.. 10.1007/s00345-020-03548-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bole R, Gopalakrishna A, Kuang R.et al. Comparative postoperative outcomes of rezūm prostate ablation in patients with large versus small glands. J Endourol . 2020;34:(7):778–781.. 10.1089/end.2020.0177) [DOI] [PubMed] [Google Scholar]
- 22. Dixon C, Cedano ER, Pacik D.et al. Efficacy and safety of rezūm system water vapor treatment for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Urology . 2015;86:(5):1042–1047.. 10.1016/j.urology.2015.05.046) [DOI] [PubMed] [Google Scholar]
- 23. Dixon CM, Cedano ER, Pacik D.et al. Two-year results after convective radiofrequency water vapor thermal therapy of symptomatic benign prostatic hyperplasia. Res Rep Urol . 2016;8:207–216.. 10.2147/RRU.S119596) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Siena G, Cindolo L, Ferrari G.et al. Water vapor therapy (rezūm) for lower urinary tract symptoms related to benign prostatic hyperplasia: Early results from the first Italian multicentric study. World J Urol . 2021. 10.1007/s00345-021-03642-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tutrone RF, Schiff W. Early patient experience following treatment with the UroLift prostatic urethral lift and rezum steam injection. Can J Urol . 2020;27:(3):10213–10219.. [PubMed] [Google Scholar]
- 26. McVary KT, Roehrborn CG. Five year results of the prospective, randomized controlled trial of water vapor thermal therapy for treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Late-Breaking Abstract. J Urol . 2020;203:(4):e1021. [Google Scholar]
- 27. Ulchaker JC, Martinson MS. Cost-effectiveness analysis of six therapies for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Clinicoecon Outcomes Res . 2017;10:29–43.. 10.2147/CEOR.S148195) [DOI] [PMC free article] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a