Abstract
The education of health professionals substantially changed before, during, and after the COVID-19 pandemic. A 2010 Lancet Commission examined the 100-year history of health-professional education, beginning with the 1910 Flexner report. Since the publication of the Lancet Commission, several transformative developments have happened, including in competency-based education, interprofessional education, and the large-scale application of information technology to education. Although the COVID-19 pandemic did not initiate these developments, it increased their implementation, and they are likely to have a long-term effect on health-professional education. They converge with other societal changes, such as globalisation of health care and increasing concerns of health disparities across the world, that were exacerbated by the pandemic. In this Health Policy, we list institutional and instructional reforms to assess what has happened to health-professional education since the publication of the Lancet Commission and how the COVID-19 pandemic altered the education process.
Introduction
The education of health professionals is currently at a crucial moment for potential change. After 10 years of innovations, an example of which is massive open online courses (free online courses available for anyone to enrol), the COVID-19 pandemic disrupted education systems everywhere, increased the use of online technologies, led to major institutional rearrangements to accommodate teaching models that combine online and in-person teaching, and revealed pre-existing inequalities in access to educational resources within and between countries. By starting economic and social crises, the pandemic has generated many disruptions that will probably have long-term implications for both education and health-care systems. As a subsystem between these two systems, but related to both, health-professional education can be a leader in innovation to improve the integration of emerging competencies and technologies. This Health Policy examines important developments in the past 10 years to assess potential progress and issues with the education of health professionals after the COVID-19 pandemic.
In 2010, the Lancet Commission1 on the education of health professionals for the 21st century recommended a global, interdisciplinary, and evidence-based approach to review the Flexner century (the century between 1910 when the Flexner report2 was published and 2010 when the Lancet Commission was published) and establish a way to encourage interdisciplinary and global integration of health-professional education. The Commission identified three types of reforms: science-based reforms promoting scientific curricula in universities, problem-based learning in academic medical centres, and systems-based reforms aimed at developing competencies for effective interprofessional practice in complex health-care systems. Based on an integrative framework, the Commission offered a comprehensive set of recommendations. This Health Policy assesses the education of health professionals in the past 10 years, analysing the main developments before, during, and after the COVID-19 pandemic. Although the 2010 Lancet Commission is the basis for this Health Policy, we do not reiterate its points. Instead, we assess any further developments in the education of health professionals, how the COVID-19 pandemic affected the education of health professionals, and the implications of these developments in the long term (panel 1 ).
Panel 1. Summary.
Globally, the annual number of medical and nursing graduates has substantially increased in the past 10 years; it has almost doubled for doctors and tripled for nurses and midwives. Increases in graduate numbers were more substantial in high-income countries than in low-income countries, and in private schools than public schools. Health professional education costs students and governments approximately US$110 billion per year. International collaboration and communication are increasing, facilitated by the worldwide capabilities of the internet.
COVID-19 has had both direct and indirect effects on the education of health professionals. The COVID-19 pandemic directly restricted face-to-face teaching in classrooms, which led to an increase in online learning. The pandemic also increased demand for health services, prompting the use of information technology and expanding the use of telehealth (the provision of health care by use of telecommunications technology), thus indirectly affecting the required competencies of medical graduates. Some of these changes to health professional education are substantially different to previous teaching methods; many have not yet stabilised but are likely to be sustained, creating new challenges and opportunities to enhance teaching and learning in the health professions.
We posit that after the COVID-19 pandemic, new educational technologies based on developments in cognitive sciences and health-care systems will lead to future innovations. Developments in competency-based education, interprofessional education, and information technology-facilitated education will increase to balance the Flexnerian2 emphasis on excellence in the life sciences with other perspectives. The digital sciences will use information technology to develop health-professional education while overcoming its issues. The COVID-19 pandemic showed the limitations of only learning online, highlighting the need for imaginative blended models of teaching that respond to the pedagogical imperatives of the three types of learning (informative, formative, and transformative) identified in a 2010 Lancet Commission.1
Information technology innovations in big data, augmented reality, mixed reality, simulation, and artificial intelligence are transforming both education and health-care systems. These changes might be the start of a new generation of reforms to methods of teaching. Current models of closed educational systems that distribute most of the content and costs at the beginning of the education process will be improved and eventually superseded by an open, longitudinal model that better meets the changing educational needs of professionals throughout their careers.
The COVID-19 pandemic has encouraged health professional education to transition into sustainable strategies of technology-infused blended learning. The education of health-care professionals will be challenged to respond to societal concerns about health equity and to encourage professionalism that incorporates concern for the individual and the community. Overcoming these challenges while maintaining the values of health-care professions is a crucial goal for health educators.
Developments since the 2010 Lancet Commission
We examined developments in the education of health professionals since the 2010 Lancet Commission according to both institutional and instructional aspects, as was done in the Commission. Analysis of the institutional aspect is based on quantitative data tabulating the global number and characteristics of schools, graduates, and financing. We examined the instructional aspect by first focusing on papers citing the 2010 Lancet Commission, then using additional publications from the past 10 years for a comprehensive perspective. There were fewer papers reporting on institutional reforms than papers describing instructional innovations.
We also examined the effects of COVID-19 on health-professional education. The effects of the COVID-19 pandemic were seen most clearly in the increase of the acceptance of information technology-facilitated education. We assessed this type of education in relation to the pandemic by reviewing the literature and doing an online survey of a convenience sample of 67 schools of medicine and nursing in the USA, Canada, Mexico, Costa Rica, Brazil, sub-Saharan Africa, China, Spain, and Thailand. We categorised the findings from the literature according to the conceptual framework proposed by the Lancet Commission: criteria for admissions, competencies, channels of instruction, and career pathways.
An estimation of country-level health-professional education costs and the number of schools and graduates (appendix pp 2–28), a description of the citation analysis and the literature review before COVID-19 (appendix pp 29–35), examples from the literature review before COVID-19 (appendix pp 44–46), the online survey on information technology usage before and during the COVID-19 pandemic (appendix pp 47–51), and reviewed literature about the effects of COVID-19 on health education and practice (appendix pp 52–58) are all available.
Before the COVID-19 pandemic
Institutional changes
Based on official data sources, we tabulated the number and characteristics of medical and public health schools3, 4, 5, 6, 7 and of graduates in medicine, nursing, or midwifery8, 9 by country or region (table 1 ). Because of reporting practices, nursing and midwifery graduates were combined in our analysis, despite the distinctive features of these groups. For public health, we only reported the number of schools as there are no consistent global data on number of graduates, potentially because of heterogeneity among countries in the professional categories included. We estimated costs for the education of doctors and nurses directly from the literature (56 estimates across 47 countries) or indirectly via a regression analysis.
Table 1.
The number of medical institutions, graduates, and individuals in the health-care workforce by region
|
Population (millions)* |
Estimated number of schools |
Estimated graduates per year (thousands) |
Workforce (thousands) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Medical |
Public health |
Doctors |
Nurses and midwives† |
Doctors |
Nurses and midwives† |
||||||||||
| 2008 | 2018 | 2008 | 2018‡ | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | ||
| World | 7036 | 7585 | 2420 | 3384 | 467 | 723 | 289 | 542 | 541 | 1424 | 8401 | 11 752 | 17 684 | 28 798 | |
| Asia | |||||||||||||||
| China | 1371 | 1393 | 188 | 157 | 72 | 153 | 76 | 93 | 29 | 99 | 1861 | 2767 | 1259 | 3721 | |
| India | 1230 | 1353 | 300 | 457 | 4 | 60 | 30 | 128 | 36 | 323 | 646 | 1171 | 1372 | 2360 | |
| Other | 1075 | 1142 | 241 | 488 | 33 | 65 | 18 | 46 | 55 | 155 | 494 | 879 | 1300 | 2195 | |
| Central | 82 | 89 | 51 | 71 | 2 | 3 | 6 | 12 | 15 | 31 | 235 | 275 | 603 | 723 | |
| High-income Asia-Pacific | 227 | 250 | 168 | 161 | 26 | 54 | 10 | 20 | 56 | 143 | 409 | 565 | 1543 | 2354 | |
| Europe | |||||||||||||||
| Central | 122 | 82 | 64 | 72 | 19 | 17 | 8 | 10 | 28 | 19 | 281 | 223 | 670 | 525 | |
| Eastern | 212 | 209 | 100 | 124 | 15 | 9 | 22 | 28 | 48 | 21 | 840 | 806 | 1798 | 1705 | |
| Western | 435 | 436 | 282 | 283 | 52 | 70 | 42 | 60 | 119 | 180 | 1350 | 1644 | 3379 | 4328 | |
| The Americas | |||||||||||||||
| North America | 361 | 364 | 173 | 212 | 65 | 99 | 19 | 29 | 74 | 227 | 793 | 955 | 2997 | 5149 | |
| Latin America and the Caribbean | 602 | 637 | 513 | 776 | 82 | 80 | 35 | 56 | 33 | 126 | 827 | 1454 | 1099 | 3263 | |
| Africa | |||||||||||||||
| North Africa and the Middle East | 450 | 533 | 206 | 330 | 46 | 51 | 17 | 41 | 22 | 106 | 540 | 767 | 925 | 1403 | |
| Sub-Saharan Africa | 868 | 1099 | 134 | 253 | 51 | 62 | 6 | 18 | 26 | 89 | 125 | 246 | 739 | 1072 | |
Detailed data sources and regional distribitions are available (appendix pp 2–28).
Population estimates were sourced from The World Bank.10
The sum of nurses and midwives was used to estimate the numbers in the nurses and midwives columns.
Estimated number of medical schools does not include non-operational schools
Schools and graduates
Between 2008 and 2018, there was a substantial increase in the number of medical and public health schools. The annual number of medical graduates almost doubled and the number of nursing graduates tripled in this timeframe; these numbers are more than the global population growth of 8% (table 1). Nurses are the majority (59%) of health professionals in the workforce—more than all other professional groups combined.11 Global distribution of the health-care workforce continued to show imbalances related to skewed numbers of health-care workers graduating among countries, with high-income countries having more graduates than low-income countries (appendix p 25). A systematic analysis of the availability of health professionals in 204 countries from 1990 to 2019 produced results that are consistent with ours, including wide variations in human resource density across nations. The analysis concluded that to achieve universal health-care coverage, the global health-care workforce would require “considerable expansion”.12
Despite having a higher density of health-care workers and more professionals graduating than low-income countries, high-income countries (and high-income regions within countries) continue to attract and retain professionals from low-income countries and regions. This migration of trained health professionals both across and within countries exacerbates imbalances in the ratio of health professionals to population, and increases disparities in access and quality of health care. A 2022 report from the International Centre on Nurse Migration13 estimates that 7 million nurses are needed worldwide to achieve pre-pandemic-quality health care and recommends amounts of staff sufficient to ensure patient safety, expansion of domestic nurse training systems, and adherence to ethical international recruitment standards to ensure that low-income and middle-income countries continue to retain an adequate number of nurses for the health-care needs of their populations.13
Many institutional collaborations, partnerships, and networks, as recommended by the Lancet Commission, were reported in the literature. An increasing number of international projects have been facilitated by worldwide access to the internet. Changes and developments in institutions seemed to be especially clear in nursing. As well as an increase in the number of schools, types of nursing programmes have diversified, adding more certificate programmes that are 1–3 years in duration and various postgraduate programmes.
Costs and financing
Approximately US$110 billion was invested globally in medical and nursing education in 2018; $60·9 billion was invested in doctors and $48·8 billion was invested in nurses and midwives (table 2 ). This estimate is similar to the $100 billion estimate made by the Lancet Commission in 2010, which was based on scarce data. Mean costs in 2018 were $114 000 per doctor and $32 000 per nurse. Expenditures for educating doctors and nurses were highest in North America ($21·4 billion), then in western Europe ($8 billion; table 2). Per capita expenditures for training doctors and nurses were ten times more in North America than in Africa.
Table 2.
Financing of medical and nursing graduates by region
|
Doctors |
Nurses and midwives |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated number of graduates per year (thousands) |
Estimated expenditure per graduate (US$ thousands) |
Total expenditure (US$ billions) |
Estimated number of graduates per year (thousands) |
Estimated expenditure per graduate (US$ thousands) |
Total expenditure (US$ billions) |
||||||||
| 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | 2008 | 2018 | ||
| World | 289 | 542 | 122 | 114 | 46·2 | 60·9 | 541 | 1518 | 50 | 32 | 27·2 | 48·8 | |
| Asia | |||||||||||||
| China | 76 | 93 | 14 | 41 | 1·1 | 3·8 | 29 | 99 | 3 | 8 | 0·1 | 0·8 | |
| India | 30 | 128 | 35 | 70 | 1·0 | 8·9 | 36 | 323 | 7 | 14 | 0·2 | 4·5 | |
| Other | 18 | 46 | 85 | 54 | 1·6 | 2·5 | 55 | 155 | 20 | 11 | 1·1 | 1·7 | |
| Central | 6 | 12 | 74 | 63 | 0·4 | 0·8 | 15 | 31 | 13 | 13 | 0·2 | 0·4 | |
| High-income Asia-Pacific | 10 | 20 | 381 | 223 | 3·8 | 4·5 | 56 | 143 | 75 | 39 | 4·2 | 5·5 | |
| Europe | |||||||||||||
| Central | 8 | 10 | 181 | 80 | 1·4 | 0·8 | 28 | 19 | 39 | 17 | 1·1 | 0·3 | |
| Eastern | 22 | 28 | 151 | 77 | 3·4 | 2·1 | 48 | 21 | 29 | 13 | 1·4 | 0·3 | |
| Western | 42 | 60 | 400 | 204 | 17·0 | 12·2 | 119 | 180 | 82 | 44 | 9·8 | 8·0 | |
| The Americas | |||||||||||||
| North America | 19 | 29 | 497 | 469 | 9·7 | 13·5 | 74 | 227 | 101 | 94 | 7·5 | 21·4 | |
| Latin America and the Caribbean | 35 | 56 | 132 | 77 | 4·6 | 4·3 | 33 | 126 | 26 | 16 | 0·9 | 2·0 | |
| Africa | |||||||||||||
| North Africa and the Middle East | 17 | 41 | 113 | 166 | 1·9 | 6·9 | 22 | 106 | 24 | 30 | 0·5 | 3·2 | |
| Sub-Saharan Africa | 6 | 18 | 52 | 32 | 0·3 | 0·6 | 26 | 89 | 11 | 7 | 0·3 | 0·6 | |
Detailed data sources and regional distribitions are available (appendix pp 2–28).
56% of medical schools were public and 39% of medical schools were private (appendix p 18). However, the increase in the number of private schools is more than the increase in the number of public schools, showing that public financing is not enough to fulfil demand for health-care workers.
Instructional changes
We identified papers published in the past 10 years about the education of health professionals that cited the 2010 Lancet Commission. Because of the large number of publications (n=2164), a random sample of 1000 eligible papers was reviewed. We only reviewed 1000 papers because the literature showed a consistent pattern of key themes in this random sample. Of the 1000 reviewed papers, 437 required further examination (appendix p 30). In these 437, the most cited recommendations from the Commission were competency-based education (24%), interprofessional education (19%), and information technology-facilitated education (8·5%). For a more comprehensive perspective than articles citing the Lancet Commission only, we reviewed additional publications about these three recommendations from the past 10 years and examined the 50 most cited papers for each recommendation. The main findings and some examples from the literature are available (panel 2 ; appendix pp 44–46).
Panel 2. A sample of innovations in the education of health professionals between 2010 and 2019.
Competency-based education
Teaching:
-
•
Entrustable professional activities (EPAs) as requirements for graduation14, 15, 16
-
•
New frameworks of professional activities and markers of progress, such as the EPAs used by the Association of American Medical Colleges17 or the markers used by the American Board of Internal Medicine18
-
•
Emphasis on the implementation of competency-based education across all disciplines, particularly medicine and nursing15, 16, 18, 19
Development stages:
-
•
Difficulty in balancing generic versus specialised competencies throughout education20, 21
-
•
Recognition of interprofessionalism and teamwork as important competencies22, 23, 24, 25, 26
Important entities:
- •
- •
-
•
US Federal Government for Graduate Medical Education Funding24
Implementation challenges:
- •
- •
- •
- •
- •
Interprofessional education
Competencies for interprofessional collaborative practice:
-
•
Collaboration among disciplines to develop important competencies53
-
•
Need for efficient and multidisciplinary health-care teams to address population health54, 55, 56
-
•
Interprofessional collaboration between health and non-health students, such as the Praboromarajchanok Institute (Nonthaburi, Thailand) doing activities with both nursing and engineering students57
Settings:
-
•
Experiential engagement in authentic, real-world settings that are crucial for learning, development of professional identity, and social responsibility58, 59, 60
Critical skills, training, and identity:
- •
-
•
Uniprofessional versus interprofessional identity (ie, identity as a health-care worker vs identity as a team)63,64
Implementation challenges:
-
•
Emergence of strategies to develop, implement, and assess interprofessional education65, 66
-
•
Small amount of evidence of successful implementation67
-
•
Structural, cultural, financial, and curricular barriers61, 68, 69, 70, 71, 72
Information technology-facilitated education
Knowledge management:
-
•
Repository for knowledge and data analytics, such as Coursera73, 74
-
•
Wearable technology, such as smartwatches, and electronic health records linkages
Pedagogic changes:
Distance and outreach:
- •
-
•
Vodcasts (video podcasts), podcasts, and microvideos80
Simulation and artificial intelligence:
Competency-based education
24% (105/437) of the publications that were reviewed focused on the use and improvement of competency-based education, showing that use of competency-based education pre-dates the 2010 Lancet Commission. Competencies for professional work have increasingly become accepted as the optimal outcome of health-professional education. The concept of competency encompasses a broad range of abilities, integrating complex cognitive capabilities with specific skills. In health care, competency has been defined as “an observable ability of a health professional, integrating multiple components such as knowledge, skills, values and attitudes”.88 Competency-based education “de-emphasizes time-based training and promises a greater accountability, flexibility, and learner-centeredness”.89
Entrustable professional activities (EPAs) facilitate assessments of competencies as they are crucial tasks in professional practice that students are entrusted to perform once sufficient competence is attained (panel 2).14, 15, 16 EPAs enable outcome-oriented curriculum reforms based on how well students can do important professional tasks. There is increasing recognition of interprofessionalism and teamwork as important competencies, as well as the need for collaborations across multiple private, public, and community-based entities. Use of competency-based education and EPAs is done globally across multiple professions, such as dentistry, pharmacy,16, 90 nursing, public health, and medicine. Most of the published articles focused on nursing and medical education.
Health equity is increasingly recognised as a neglected curricular theme amid substantial health disparities among population subgroups, defined by urban or rural residence, race, ethnicity, income, housing, and education. The literature highlighted health inequities both domestically and globally. As these disparities and their solutions are global, the topic of global health has become popular with students who are part of international networks and educational consortia. For example, the Association of Pacific Rim Universities Global Health Program48 has established 19 important competencies in five areas of global health training. Many students from high-income countries are engaged in global health education, and increasing numbers are becoming engaged in low-income and middle-income countries.49, 50 Within global health, there is a decolonialisation movement that recognises that, like other areas of study, global health has been affected by the geopolitical context in which it originated and operated.
Interprofessional education
Interprofessional education encourages collaborative practices in multiple health-care-related disciplines. It was mentioned in 19% (84/437) of the reviewed publications. Several papers define interprofessional education as an “occasion when two or more professions learn with, from and about each other to improve collaboration and quality of care”.91, 92
Inspired by the idea that interprofessional collaboration could be crucial for high-quality, safe, and patient-centred care in the USA, the Interprofessional Education Collaborative (IPEC) published competencies for this practice in 2011.53 IPEC emphasised four broad competency areas: values and ethics, roles and responsibilities, interprofessional communication, and teamwork and team-based care. After 6 years of implementation of the Affordable Care Act, these competencies were updated in 2016 with a renewed focus on improving the experience of care for the patient, improving the health of populations in the USA, and reducing the per capita cost of health care, as recommended by the Institute of Health Care Improvement.53
Many papers highlight the need for efficient, multidisciplinary teams to meet the increasingly complex health-care needs of a population.54, 55, 56 The Africa Interprofessional Education Network56 is an example of a consensus-based partnership between institutions working to establish interprofessional education and collaborative practice as part of workforce training to “promote effective functioning of [a] healthcare system”.56 Most interprofessional education studies focus on nurses and doctors in clinical settings; other health professions and non-clinical settings are less frequently covered. Some authors have reported that particular topics, such as palliative care, pain management, and patient safety, are easily amenable to developing interprofessional educational experiences. Some believe that students and health professionals should directly and experientially engage in collaborative opportunities in authentic, real-world settings, such as communities, homeless shelters, teaching hospitals, and primary health units. These interprofessional experiences can increase recognition of health disparities and encourage the development of student and professional identities that have a shared sense of social responsibility.58, 59, 60
Development of teaching staff is essential to high-quality interprofessional education and collaborative practice. Trained as uniprofessionals who practice in one profession, most medical and nursing staff have little experience in collaborative practice. Some students are exposed to interprofessional education during their studies, but have few opportunities in laboratory or clinical placements to practise interprofessional education61 or even become familiar with the concept.59 Among the few publications that provide strategies for development of teaching staff was a partnership between eight universities that tested a 1-year programme to train a group of interprofessional faculty leaders (those who are skilled in effectively facilitating interprofessional education).62 It aimed to prepare participating staff to lead interprofessional education activities at their own institutions.
A balance between uniprofessional and interprofessional identity is crucial. Khalili and colleagues63 proposed an interprofessional socialisation framework to promote collaborative, person-centred practice and facilitate dual identity formation. Joynes64 introduces the concept of interprofessional responsibility, describing how professional identity is conceptualised and how professionals should integrate professional identity and collaborative practice.
Several publications provide guidance for development, delivery, and assessment of interprofessional education.65, 66 Kahaleh and colleagues65 provided strategies for implementing an interprofessional education curriculum and effective assessment tools specifically intended for pharmaceutical schools. However, there is little published evidence of successful implementation. One exception is the Collaborative Competencies Model at the University of Toronto,67 with common competencies across eleven health professions leading to longitudinal relationships between these professions, while supporting uniprofessional curricular objectives. However, many structural, cultural, financial, and curricular issues, such as the need for financial investments in educational programmes and a lack of organisational support, prevent effective interprofessional education implementation.61, 68, 69, 70, 71, 72
Information technology-facilitated education
Information technology innovations were being used in educational programmes before the 2010 Lancet Commission was published. These innovations helped ensure that nurses in rural areas could access medical centres in Australia.93 For example, the Aga Khan University (Nairobi, Kenya; Dar es Salaam, Tanzania; Kampala, Uganda)94 introduced information technology-facilitated education curricula in Kenya, Tanzania, and Uganda. The development of information technology-facilitated education and its scope increased in the 10 years after the Lancet Commission. Novel approaches in areas such as big data, augmented reality, mixed reality, simulation, and artificial intelligence are changing both health-care and education systems. To analyse these innovations, we classified information technology-facilitated functions into four categories: knowledge management, pedagogic changes, distance and outreach, and simulation and artificial intelligence.
Knowledge management
As the amount of health care-related data have increased, new technologies have enhanced opportunities for curricular innovation and evaluation. Rapid retrieval of information and practice standards alongside increased use of hand-held devices, such as smartphones and electronic tablets, allow for prompt and reliable access to clinical guidelines. Internet-based platforms use data mining, data analysis, and visualisation methods for curriculum assessment.73, 74 Information technology-based knowledge management offers the best opportunity to make learning time available to accommodate the increasing list of important competencies necessary for professional practice. Internet access to information has reduced the dependence on memorisation by students and practitioners. Computer-supported collaborative learning systems have been proposed as an effective strategy to help students manage large amounts of information, particularly for medical curricula.95, 96 Some internet platforms have been specific to medicine,74, 97 although many educational tools have also developed outside of medical education, such as the Khan Academy (Mountain View, CA, USA).
Pedagogic changes
Digital technology has increased the number of pedagogic approaches—blended, hybrid, and fully online learning. Blended learning allows for so-called flipped classrooms, in which online and in-person learning is available for both individual and group activities. Hybrid learning allows in-person and online student audiences synchronous access to the same materials. Early introduction of technology into classroom education used multimedia (eg, Prezi), computer-assisted instruction, electronic audience response systems (eg, iClicker), and polling systems (eg, Poll Everywhere) in real time. E-learning and blended learning (with both in-person and asynchronous curricular activities) became popular in the early 2010s.
Distance and outreach
Technology reduces distance between students and health educators across the globe through virtual proximity, potentially bringing expertise to rural regions and isolated health-care workers. The literature highlights an expansion of telemedicine (the diagnosis and treatment of patients by use of telecommunications technology). For instance, the Haiti Medical Education project98 connected rural primary care clinicians in Haiti to international experts. Another example is Project ECHO,77, 78 a telemedicine model connecting community health-care providers with experts through telementoring (mentoring and guidance of junior or community staff offered virtually by experts or senior faculty). Video live streaming, podcasts, and videocasts have become popular ways of communicating information to personal digital assistants and hand-held devices. Information technology has also reduced the challenges that occur due to geographical and spatial separation regarding access to open educational resources. Within 2 years of the 2010 Lancet Commission being published, massive open online courses began to be introduced via online platforms, such as EdX, Coursera, and Udacity. Although the initial business models of online learning have improved, massive open online courses provide large numbers of students worldwide with low-cost access to high-quality educational materials. However, many low-income countries have low participation in massive open online courses because of a lack of access and capacity to use digital technologies, or lack of awareness of these courses.99 In 2019, only 28·2% of the African population were internet users, compared with 77·2% in the Americas.100
Simulation and artificial intelligence
Some of the most promising applications of novel technologies to the education of health professionals have occurred in simulation and artificial intelligence. Beginning with virtual patients and mannequins and subsequently incorporating serious games (gamification of major educational concepts) and augmented reality, many medical and nursing schools have increased their reliance on simulation and artificial intelligence for clinical skills training. Simulation offers safe and authentic learning across multiple patient-care contexts, such as inpatient, emergency, outpatient, and home care. Virtual patients have been implemented in 130 medical schools in the USA and Canada.81 Information technology enables students to do virtual dissections, participate in standardised case studies, and join procedures (eg, surgery). The applications of this information technology-facilitated education are expected to increase as substantial investments in the Metaverse (an immersive virtual world) begin to provide specific products and services. For example, ten US universities are participating in a pilot project to become so-called metaversities through a model that combines in-person, online, and simulated environments.101
The effect of COVID-19 on health-professional education during the pandemic
To understand the initial effects of COVID-19 on the use of information technology-facilitated education in medical and nursing schools, we did a survey that aimed to identify technological applications that have supported learning outside of the classroom via online platforms. The survey included a convenience sample of 67 schools of medicine and nursing in the USA, Canada, Mexico, Costa Rica, Brazil, sub-Saharan Africa, China, Spain, and Thailand.
Additionally, we did an early landscaping analysis to assess the effects of the COVID-19 pandemic on the education of health professionals; we reviewed three sources of information. The Association of Medical Educators in Europe102, 103 published two Best Evidence in Medical Education (BEME) guides on pandemic-related changes in health-professional education: a systematic review in May, 2020, with 49 final articles, and a scoping review in January, 2021, with 127 final articles. The third source of data was a collection of 186 articles compiled by Academic Medicine as of Feb 10, 2022, about changes in health education and practice as a direct result of the COVID-19 pandemic.
We classified the themes identified in this analysis according to the four domains proposed in the 2010 Lancet Commission: criteria for admission, which includes achievement variables, such as previous academic performance, and adscription variables, such as race, ethnicity, sex, nationality, and socioeconomic status; competencies, as they are defined in the process of establishing the curriculum; methods of teaching, such as didactic methods, teaching technologies, and communication media; and career pathways, the options graduates have when they finish their professional studies as a result of the knowledge and skills they have attained, the process of professional socialisation they have been exposed to as students, and their perceptions of opportunities in local or global labour markets.1
COVID-19 global survey of schools for health professionals
COVID-19 has increased the use of information technology-facilitated education globally. Restricted physical access to classrooms and health-care facilities led to an immediate increase in the use of digital platforms to meet the training needs of students in all health-care disciplines. 80% of the institutions surveyed reported regular use of some information technology-facilitated education before the COVID-19 pandemic. Common tools included hand-held devices, such as computer tablets or smartphones, and the internet. 39% (26/67) of the schools used completely online education, and 60% (40/67) used blended or hybrid approaches. Many new courses were designed for or adapted to information technology-facilitated education. Designing or implementing digital education, availability of appropriate technology, infrastructure, costs, and technology competence of teachers and students were reported as common issues. 67% of the schools reported that they anticipate information technology-facilitated education will improve, be implemented in a larger number of institutions than it is currently, and be integrated into future curricula. A 2021 international survey of nursing education and graduates from nursing schools during the pandemic, involving more than 130 nursing associations globally, reported widespread educational disruption, delays in nursing student graduation, and increasing numbers of applications to nursing schools.104
COVID-19-related educational changes
Between the first and second BEME guides there was a substantial increase in the number of publications, coordinated developments, and collaborative developments regionally, nationally, and internationally in health-professional education. Most publications referred to undergraduate medical education, with many focusing on disruptions to medical practice and clinical training programmes. The main areas of development included increasing the use of online learning (both synchronous and asynchronous) and simulation, especially in the surgical specialties. 50% (23/49) came from the USA, 25% (12/49) came from Asia, and 20% (10/49) came from Europe.
Criteria for admissions
The COVID-19 pandemic meant medical schools had to use virtual interviews for admissions, residency positions, and fellowship positions. Although this might have allowed applicants to access a larger number of programmes than they would have had access to in in-person interviews, the possible effects of virtual environments on equity of access are not yet fully known. Several educational institutions have revised their admissions procedures in innovative ways. For example, the University of Houston College of Medicine (Houston, TX, USA)105 converted its in-person multiple mini-interview process for admission into an online format. The University of Toronto106 started using semisynchronous, video-based modified personal interviews instead of in-person interviews. Adjustments to non-cognitive skill assessments were also reported, such as the development of centralised management processes, safety protocols, and communication systems.107 Studies reported positive reactions about virtual interviewing opportunities from students regarding the ease of interaction, time savings, and cost savings.108, 109, 110 However, this virtual process could introduce potential new biases and issues with access among applicants from low socioeconomic status backgrounds and under-represented minority groups, as they might be disproportionally affected by the changes due to the COVID-19 pandemic.111, 112 The challenge, therefore, is to ensure that virtual interviews do not negatively affect diversity and equity in student recruitment.
The opportunity for students to apply to multiple institutions causes considerable operational and management challenges for individuals reviewing and processing admissions. Some studies have proposed enforcing a limit to the number of interviews that applicants can attend to ensure genuine interest.113 A persistent theme in early literature about the effects of the pandemic was the need for flexibility in testing requirements, admission criteria, and licensing requirements in medical education.
Competencies
As part of the COVID-19 pandemic-induced restrictions, clinical placements in surgery were replaced with a combination of asynchronous and synchronous virtual learning by use of video reviews and surgical simulators.114, 115 Training in ultrasound,116 safe endotracheal intubation,117, 118 and appropriate donning and doffing procedures for gowns119 are examples of specific doctor competencies that required additional attention to deal with the multiple increases in COVID-19-related hospitalisations. An example of a multi-institutional collaborative effort in training paediatricians to care for adults with COVID-19 was the Pediatric Overflow Planning Contingency Response Network,120 which was reviewed positively by students for its practicality. Assessment of competencies was done by use of virtual objective structured clinical evaluations (OSCEs) and in person with physical distancing. Virtual OSCEs were partly successful.121 Online clinical vignettes, use of open-book examinations, and multiple-choice examinations based on short clinical scenarios were all used for assessment.122, 123, 124 COVID-19 required teachers to teach and assess more crucial competencies than before the COVID-19 pandemic.125 Several authors suggested additional competencies should be developed in areas such as public health, social justice, advocacy, telehealth, and leadership.126, 127, 128, 129, 130
Channels of instruction
Globally, there were many online platforms and techniques that met the unprecedented need to continue teaching without being in person. Planned conferences, boot camps that prepare students for their next phase of training, and grand rounds were delivered via video conferencing platforms;131 clinical electives and clinical clerkships became virtual learning opportunities.132 Digital clinical placements, virtual rounds, telemedicine, online OSCEs, and telesimulation (simulation training done without physical presence) were widely reported.133, 134, 135 Features of videoconferencing that allow learner engagement, such as hand raising, online chats, polling, and break-out rooms, were used extensively.136, 137, 138 In Mexico, an online curriculum with 8000 students, 18 000 junior doctors, and 5000 staff members was delivered successfully using a new, digital, distance-learning platform.139 Other innovations include virtual ward rounds using a computer tablet on wheels to learn about COVID-19 patients,140 experiential learning without physical presence by supervised telephone or video consultations, and the integration of online students into patient encounters. Active learning methods of teaching, such as case-based, team-based, and problem-based learning, were attempted online. Synchronous online sessions used several tactics to ensure ongoing learner engagement, such as break-out rooms for small group work, a chat function while videoconferencing, virtual whiteboards, and games.
In addition to multiple reports on the challenges of using online teaching, the scoping review involved many articles on in situ and laboratory-based simulation projects.141, 142 Simulation-based stress testing of clinical systems was used to inform management guidelines for COVID-19 in the USA.143 The Alberta Health Service144 provided simulation training to approximately 30 000 health-care workers across Alberta. Yale School of Medicine (New Haven, CT, USA)145 developed a novel curriculum converting high-fidelity, mannequin-based simulation into a fully online virtual telesimulation format. As part of a renewed commitment to improving health-professional education, Massachusetts General Hospital (Boston, MA, USA)146 announced a new simulation facility for comprehensive training of health professionals in hospital functions. Some surgical training programmes reported online procedural skill development (eg, knot tying, suturing, and microsurgical skills).147, 148, 149 Most of the simulation training involved multidisciplinary teams. A collaborative curriculum to teach point-of-care ultrasound involved 15 different institutions and a rotating group of 30 instructors to teach synchronous skill-development sessions.150
A technology integration framework has been proposed to evaluate online learning programmes. The framework is called PICRAT, which refers to both the methods of learner engagement (passive, interactive or creative) and the use of technology by the teacher (replaces, amplifies, or transforms the in-person learning experience).151 This comprehensive framework was used to rate reports of online learning developments in postgraduate medical education in response to the COVID-19 pandemic. A systematic review revealed strong preferences of students for online instruction and a preponderance of reports from the specialisation of emergency medicine.152
Innovations include the development of online communities of practice for trainee wellness and learning or improving skills via social media platforms. Virtual cafés have become venues for discussions about educational, clinical, and wellbeing topics.153 A rigorous iterative process was used in the development and deployment of a practical, digital learning system for handling the effects of COVID-19 on mental health.154 Although it is too early to ascertain the effects of the diverse adaptive strategies of education that the COVID-19 pandemic caused, there are already some initial evaluations of student perceptions of online learning that show generally positive responses. However, so-called Zoom fatigue (watching a computer screen for extended periods of time without human interaction), insufficient engagement, and concerns about the effectiveness of online learning are all issues that will require long-term assessment by teaching staff.
Career pathways
The COVID-19 pandemic prompted the early graduation of many medical and nursing students worldwide to meet clinical demands, thus increasing the number of staff entering into professional practice.155, 156 Other than this short-term change, there are few reports that explicitly focus on the effects of the pandemic on the career pathways of graduates, as such effects will probably take several years to happen. The extensive virtual training during COVID-19 will probably have a differential effect on medical students and junior doctors. Deficits in professional identity formation and competencies related to virtual training will probably be evident in the next few years. Recommendations have been made to make use of the increase in virtual education to maximise career advancement for postgraduate trainees.157
Health-professional education after the COVID-19 pandemic
COVID-19 presented an unexpected opportunity to increase innovation in higher education systems (eg, universities and accrediting organisations), health-care systems, and the interaction between these systems. As well as the short-term disruptions the COVID-19 pandemic caused, it is likely to have societal consequences with long-term effects. These consequences will take some time to understand, but institutions can use the energy and passion of individuals and communities as a result of the pandemic to rectify structural deficits and overcome limitations that the pandemic revealed. Institutions should not merely adapt to a new normal way of training, but proactively establish an improved normal way of training. The first part of this would be to develop novel ways of conceptualising models that could change health-professional education after the COVID-19 pandemic.
A conceptual framework
The transformation imperative in higher education is led by two inter-related concepts that the COVID-19 pandemic has encouraged: the development of new educational technologies based on improvements in the cognitive sciences and the unprecedented amount of change in health-care systems because of increased technological and organisational complexity. The amount of change in health-care systems happens more quickly than conventional instructional processes can teach. During the time a student is in an educational institution, existing jobs are being disrupted and new jobs are being created, so it is impossible for new graduates to completely learn all competencies required in the workplace. Therefore, initial teaching is not sufficient to ensure successful ability, either in professional proficiency or personal wellbeing. Furthermore, new educational technologies make it possible to increase competency development to include more than traditional, formal, full-time teaching. As a result, the previously separate life stages of learning and work become connected. These two concepts of change require higher education to use the so-called education for life model that has implications for both instructional and institutional design.
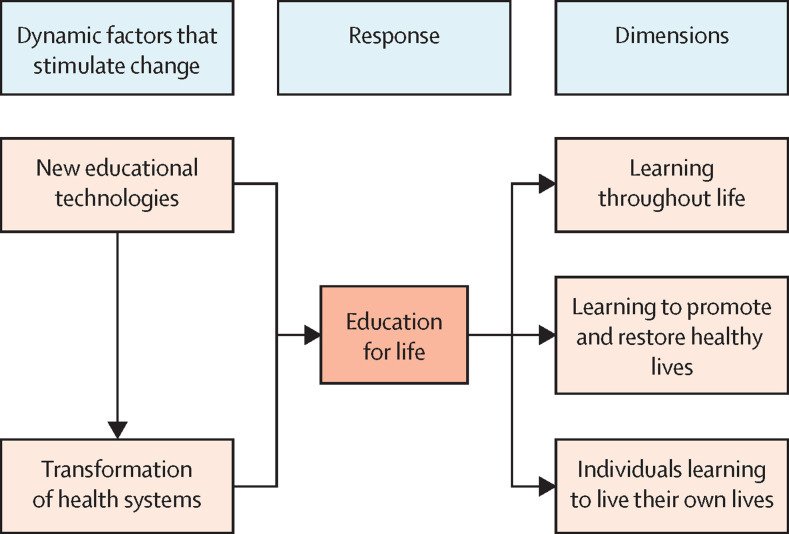
Education for life encompasses three parts (figure 1 ). The first is learning throughout life, which refers to education that lasts for a lifetime rather than a specific timeframe. Traditional educational models separate the life course into stages for learning, work, and retirement. Closed educational systems that distribute most of the content and costs at the beginning of the education process should be improved and eventually superseded by open systems that are designed to meet the constant needs for new competencies throughout the careers of health professionals.
Figure 1.
An adaptive response to disruption of the education of health professionals
Learning to promote and restore healthy lives
The second part of education for life refers to the substantive content of the education of health professionals, which focuses on developing competencies to preserve and improve the lives and wellbeing of individuals, families, and communities. In other words, it is education that aims to help other individuals via the technical expertise and service ethics of health professionals.
Learning to live one's own life
Part of education should enable students to preserve their sense of purpose and mental wellbeing. This part involves learning to balance work life and life in areas other than work, as well as learning to cope with stress and adversity. Preventing occupational burnout, however, is not only a matter of developing these individual capabilities but of learning how to change the organisation of work to support the wellbeing of all team members while supporting equity among the different categories of the health-care workforce. Due to increasing workloads, adequate staffing is essential to manage stress and pressure that can negatively affect wellbeing.158, 159
Health-professional educational institutions should overcome challenges and use opportunities from technological innovations and health system disruptions to effectively implement the three parts of education for life.
Technology and global outreach
The effects of the COVID-19 pandemic have been most clear in the widespread use of information technology-facilitated education, which offers a common platform for the other two teaching innovations, competency-based education and interprofessional education. The same information technology innovations that are changing education are also being used in health care, and therefore lead to changes in the workplaces students will join after they graduate. To succeed in the workplace, health professionals will have to be conversant with the uses and limitations of these technological innovations, including telemedicine and artificial intelligence. Information technology is both a pedagogical tool and an increasingly important area of substantive competency for health professionals.
Education was one of the few areas of society that did not have a technological revolution during the 20th century, unlike health care. The start of the technological revolution in education might have happened in the 10 years after the publication of the Lancet Commission. Although the Commission highlighted the promise of information technology, it could not have anticipated the speed, scope, breadth, and depth of innovation. Soon after its introduction in 2008, the New York Times declared 2012 the year of the massive open online course. Since 2012, there have been many new approaches to education based on development in information technology, including artificial intelligence, augmented reality, mixed reality, and simulation. Information technology in health care and health-professional education has changed from a desktop computer to hand-held devices and from classrooms to direct patient care. The COVID-19 pandemic substantially increased the need for these pre-existing technological developments.
Many adaptations to the COVID-19 pandemic based on online technologies were short-term accommodations that were not high-quality enough for a long-term transformation of health-professional education. Distinguishing between hybrid and blended models of online teaching helps to clarify this point. In hybrid courses, the same material is delivered in person or remotely, depending on the circumstances of different groups of students. For example, during the pandemic, students who had pre-existing health conditions, had tested positive for COVID-19, were in quarantine, or had travel restrictions had to attend classes online while other students were in the classroom. By contrast, blended instruction combines in-person and online methods based on the pedagogical requirements of different types of educational material. For example, the 2010 Lancet Commission distinguished between three types of learning: informative, formative, and transformative (appendix p 59).1 The combination of online and in-person teaching varies for each type. For informative learning to obtain factual knowledge, high-quality online platforms can replace traditional in-person lectures.160 As educational processes change to include formative and transformative learning, the need for team-based and immersive in-person teaching formats increases. Rather than being separated based on their circumstances, all students benefit from the optimal blend of pedagogical approaches.
Artificial intelligence also has potential to improve health-professional education. As the applications of artificial intelligence develop, they might reduce costs and improve standardisation in both education and health care. For example, artificial intelligence can power algorithms to assist with differential diagnoses, and machine learning tools can validate diagnoses, read x-rays, and examine pathology specimens.161 These abilities provide the opportunity to adjust educational competencies to increase free space and time for the patient–provider interaction. Paradoxically—and optimistically—integration of artificial intelligence tools into the daily practice of medicine can be adapted to increase humane and compassionate care. In education, new technologies will provide the necessary platforms to implement the three parts of so-called education for life in practice.
The disruption of traditional methods of education by the increase of applications of information technology has been so large that it could be the start of a new generation of reforms in the education of health professionals. The three generations of reforms identified by the 2010 Lancet Commission (science-based, problem-based, and systems-based) were all launched during the Flexner century. This new generation of reforms is encouraged by technological innovations that exploit developments in learning and teaching, and will improve upon the accomplishments of the previous three generations of reform.
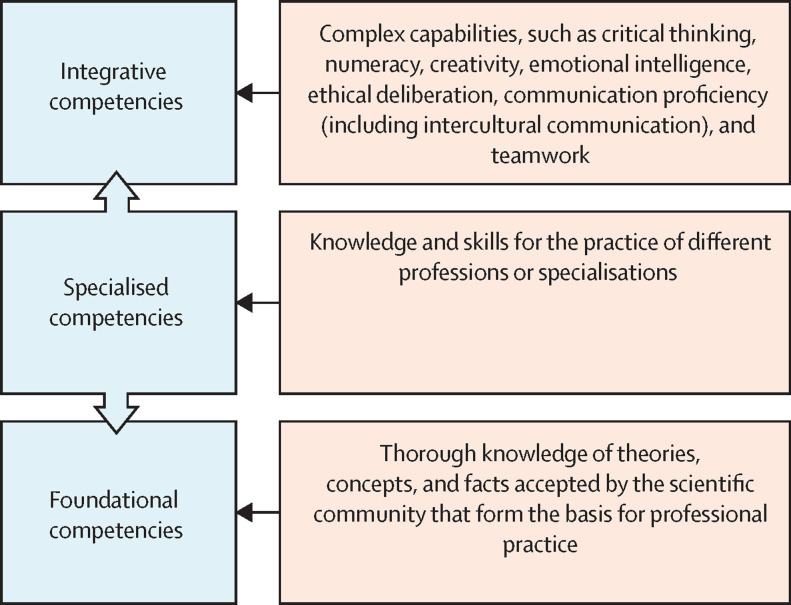
A new set of competencies
The unprecedented changes in the health-care systems that graduates of educational institutions will operate in require a renewed perspective on the competencies these graduates should develop as important outcomes of the teaching and learning process. These competencies can be categorised into three groups: foundational competencies, specialised competencies, and integrative competencies (figure 2 ). Foundational competencies involve establishing a comprehensive knowledge of theories, concepts, and facts that are widely accepted by the scientific community and that form the basis for professional practice. Specialised competencies refer to the knowledge and skills required for the practice of different professions or specialisations. Integrative competencies refer to complex capabilities, such as critical thinking, numeracy, creativity, innovation, communication proficiency (including intercultural communication), teamwork, emotional intelligence, ethical deliberation, and social responsibility. For health-care systems in which innovation will disrupt the ways of practice learned during initial teaching, developing metacompetence (the competence to develop new competencies) is essential.162
Figure 2.
Framework of health-care professional competencies
The disruption of education and health care caused by COVID-19 happened alongside the emergence of many new competencies that should be part of the armamentarium of health professionals. These competencies include capabilities in multiple emerging fields,163 such as information technology, telemedicine, situational leadership, collaboration across traditional boundaries (boundaries between each profession within and outside health care), creation of academic–community partnerships, and advocacy based on an understanding of the social determinants of health. Health professionals do not have to become experts in each of these areas, but they should develop the competencies required to increase the scope of interprofessional practice. Traditionally, most inter-professional education programmes focused on collaboration between the different clinical professions engaged in direct patient care.
One way to increase the scope of interprofessional practice includes population health professionals who work in community settings and public health organisations. The COVID-19 pandemic has highlighted the need for collaboration between clinical and population health professionals. The scope of collaboration should also include non-health professionals who work in the health-care system, such as computer scientists, engineers, and data scientists, and other jobs in areas such as artificial intelligence. As health-care systems become increasingly complex, they become substantial employers of professionals who can provide necessary legal, financial, and managerial expertise. New technologies, particularly in information technology, have increased the number of people with expertise in areas other than health care working in health care due to the complexity of health-care systems (particularly in the USA), and who should therefore learn to work alongside medical staff.
Environmental sustainability is another area of expertise that health-care organisations should use to adequately meet their social responsibility. In this context, traditional hierarchies in which clinical professionals are at the apex of health-care organisations should be replaced by a network of diverse expertise that is essential for these organisations to succeed.
Educational institutions should broaden traditional approaches to interprofessional education to include students in professions other than health care. Furthermore, students in health professions should develop an understanding of emerging health-care-related professions and different professional perspectives on health-care topics.
In 2019, the UK National Health Service (NHS)164 did an independent review on how technology and technology-related developments will affect health professionals and their training in the next 20 years. As technology augments the work of health professionals, future health care will require extensive retraining of the clinical workforce and purposeful integration of data scientists, engineers, computer scientists, and others in cross-disciplinary training activities. In the next 20 years, 90% of NHS jobs will probably require some digital proficiency.164 The independent review recommends creating a culture of learning and innovation within the NHS and introducing industry exchange networks to enhance collaborative partnerships and the development of technical specialists to work in health-care settings.
Competencies will continue to develop as technological innovation disrupts existing jobs and creates new jobs. The first part of the education for life model will need to constantly update practitioner skills regarding these emerging requirements that are essential for successful clinical and public health practice in the future. The reliable and valid assessments of these competencies should also continue to be developed and assessed.
Other than technological competencies, it will also be necessary to develop new ways of defining, developing, and assessing integrative competencies associated with the third part of education for life (figure 1). The COVID-19 pandemic has shown the need to improve adaptive strategies, including self-care to prevent occupational burnout, the ability to cope with uncertainty, and the capacity to anticipate, prepare for, and respond to adversity. These individual competencies should be developed through institutional solutions, such as wellness initiatives and increased workplace amenities (eg, child care), to reduce the organisational stressors leading to personnel burnout and turnover. If these competencies are not developed, health-care systems are likely to have to overcome a paradoxical issue; at a time when the pandemic has increased public recognition and appreciation of health professionals (leading to large numbers of applications to health-professional education in many countries, such as the UK and the USA), occupational distress is causing current professionals to leave the health-care workforce. These professionals leaving could exacerbate existing shortages and other labour market imbalances, such as the maldistribution of the existing workforce, in health care.
Integrative competencies that are associated with transformative learning, which refers to the development of leadership capabilities that allow health professionals to make change happen both within the workplace and in other areas, should be developed. Part of these leadership capabilities is dispelling unscientific misinformation, which has increased during the COVID-19 pandemic. Health professionals are having to curate the substantial amount of information that is widely available.165 In addition to traditional ways of communication with patients and populations, health professionals need to be increasingly engaged and proficient on social media platforms.
The COVID-19 pandemic has also revealed and increased inequalities in health and access to health care, so health professionals should know how to influence social determinants of health. Health professionals should understand both the technical content and social context of their practice.
Health equity and social justice
The focus on competencies recommended by the 2010 Lancet Commission, and many other papers, is a fundamental change in the way educational institutions conceptualise and assess the quality of their programmes, from inputs (eg, the number of credits for a specific course) or intermediate results (eg, examination grades) to outcomes (eg, a comprehensive set of competencies). Accountability for improved quality of training via improved outcomes is integral to the value that educational institutions provide to the societies of which they are part. For this value to be realised, these institutions should increase access to high-quality training. If access is not increased, education can reproduce social inequality instead of encouraging upward social mobility.
Technological innovation can improve health equity and social justice. For example, at the Khan Academy, high-quality courses can be done online from anywhere in the world by anyone with an internet connection. The Khan Academy aims to remove inequalities in access to education worldwide for both students and teachers. The ability of information technology to improve global health equity is seen in open access medical education platforms, such as DigitalMEdIC from Stanford University (Stanford, CA, USA), Free Open Access Medical Education,97 NextGenU, and ScholarRx Consortium, which collate and curate free or low-cost online educational resources and provide them to all interested health professionals.
Previous attempts to improve equity in health-professional education have used online platforms to access students in low-income and middle-income countries. The People's Open Access Education Initiative in 2008 and OxPal MedLink166 in 2011 are examples of this process. The Global Medical Education Collaborative,167 established during the COVID-19 pandemic, is an innovation that is being used in 12 countries and 20 medical schools in Asia and Africa, in which staff from Oxford University (Oxford, UK) and Harvard Medical School (Boston, MA, USA) use collaborative case-based learning as the primary teaching method.
Increasing access to high-quality education should always be an aim of professional education, but requires further emphasis now the COVID-19 pandemic has revealed and increased pre-existing inequities. Social justice is part of both the institutional and instructional aspects of educational strategy; it should be a main component of the commitment to equitable access while representing an integrative competency that contributes to a successful professional career.
Increasing collaboration in health care and education
In addition to the positive effects of information technology on the teaching aspect of health-professional education, it can enable institutional innovations. For example, the 2010 Lancet Commission recommended global collaborative consortia be created, although few emerged in the 10 years after publication. Information technology can now use the integration of these consortia with other institutional solutions to encourage global equity. The COVID-19 pandemic showed the increasing interdependence of health risks. If the realisation of this interdependence is used in a positive way, it can increase the speed of the search for global solutions to health-care disparities and shortages of health-care workers, including the development of a competent health-care workforce via shared, globally available educational resources. The opportunity to educate individuals from all traditional geographical and professional groups allows for a more equitable diversity of students, teachers, and perspectives.
The Lancet Commission introduced the concept of transprofessional education to refer to training that includes the full spectrum of professional and non-professional health-care workers (eg, technicians and community health-care workers). Our literature review done before COVID-19 revealed few examples of programmes focused on this broad scope of collaborative education. This omission is paradoxical alongside the increased recognition of the importance of health-care workers, especially community health-care workers, and the multiple examples of national programmes that recognise their contributions in countries such as Bangladesh, Pakistan, Rwanda, and Ethiopia that rely on well trained and supervised community health-care workers who are provided with career opportunities in low-income countries to practise with support from experienced professionals. Properly connected community health-care workers are both efficient and important in encouraging health equity. The new generation of reforms as a result of the COVID-19 pandemic should include transprofessional education to help overcome the individualism affecting the health-care workforce and encourage inclusive teamwork. This would improve professional identities by encouraging development from uniprofessional to interprofessional identities. In this Health Policy, we make three recommendations for the future of health-professional education (panel 3 ).
Panel 3. Recommendations.
Use education for life as a principle for health-professional education:
-
•
Learning throughout life to maintain professional excellence in the constantly developing environment of scientific discovery, technological improvement, and environmental and social change
-
•
Learning to promote and restore health and to improve the lives and wellbeing of individuals, families, and communities
-
•
Individuals learning to successfully live their own lives, to balance work and other activities, and to preserve a sense of purpose, service, and mental vitality
Use competency-based education in new areas including:
-
•
Information technology and big data interpretation
-
•
Artificial intelligence and machine learning in health-care decision making
-
•
Telemedicine uses and limitations
-
•
Social determinants of health and health equity
-
•
Climate change and health; One Health; and planetary health
-
•
Communication using social media to increase evidence-based understanding and to counter health misinformation
-
•
Ethical dilemmas about new technology, such as genetic engineering
-
•
Teamwork and leadership for excellence in clinical care and progress in population health; aiming to improve health, improve the experience of care for a patient, and increase efficiency
-
•
Interprofessional collaboration, including population health; practitioners and non-health professionals working collaboratively in health-care organisations, aiming to improve institutional and system-wide processes
Use learning technology to make health professional education effective, efficient, and inclusive; to encourage transprofessional collaboration at clinical, institutional, and systems levels; and to make the education of health-care professionals resilient to future pandemics, any similar disruption, and the changing needs of society:
-
•
Innovate on blended educational models
-
•
Increase institution-to-institution global education networks and consortia
-
•
Develop enhanced robotics and simulation training
-
•
Implement experiential learning in multiple professions and areas of expertise
-
•
Prepare staff for success in a technology-dependent learning environment
-
•
Rigorously assess educational interventions to improve learning and teaching
The growth of information technology applications to increase competency-based and transprofessional education, the development of collaborative networks with global connectivity, and a new professionalism based on social responsibility are all ways to establish an improved normal way of training after the COVID-19 pandemic using the education for life model. The education of health professionals should improve to become a humane and effective way of creating students who are prepared, for their entire career and at every age, to meet the changing health-care needs of individuals and populations. Health professionals should also be able to work in teams, take advantage of developing technologies, and remediate the social factors that affect access to health care for many individuals.
The origin of the COVID-19 pandemic as a zoonotic disease and its substantial global effects show the need to overcome the separation between human, animal, and planetary health. There is a consensus that the world will face another pandemic in the future. Our ability to overcome another pandemic is dependent on how quickly society can implement successful strategies for education and health. If we can establish adaptive and resilient health-care systems that are operated with excellent health-professional education, we will be able to protect and promote all aspects of wellbeing during and between future pandemics.
Declaration of interests
Acknowledgments
Acknowledgments
The authors acknowledge China Medical Board for funding related to the acquisition of relevant data for this Health Policy. The authors also acknowledge the contributions of the 20 members of the 2010 Lancet Commission, especially those who reviewed early drafts of this Health Policy (Zulfiqar Bhutta, Jordan Cohen, Nigel Crisp, Timothy Evans, Patricia J Garcia, David Naylor, Srinath Reddy, David M Serwadda, and Huda Zurayk); Henri Ford, Dean of the University of Miami Miller School of Medicine; Kurrdeige Alexander and Sabrina R Payoute for literature review and data collection for this Health Policy; Eric L Keuffel and Alexander S Preker for the estimates on number of health professional graduates, cost of education, and size of the health-care workforce; Xiaoqing Zhang for her review of the COVID-19 academic medicine literature; and Barbara J Stoll for her guidance on report content and her critical review of the manuscript.
Contributors
JF and HVF conceptualised this Health Policy. LCC and AM designed this Health Policy. LC, EOHG, and RK acquired, analysed, and interpreted data. AM acquired data. JF, LCC, LC, EOHG, and HVF wrote and drafted the manuscript. All authors revised the manuscript and approved the final draft.
We declare no competing interests.
Supplementary Material
References
- 1.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 2.Flexner A. Carnegie Foundation for the Advancement of Teaching; New York City, NY: 1910. Medical education in the United States and Canada. From the Carnegie Foundation for the Advancement of Teaching, bulletin number four, 1910. [PMC free article] [PubMed] [Google Scholar]
- 3.World Federation for Medical Education World Directory of Medical Schools. 2017. https://wfme.org/world-directory/
- 4.Association of Schools of Public Health in Africa ASPHA members. https://asphaafrica.net/membership/members/
- 5.Council on Education for Public Health List of accredited schools and programs. https://ceph.org/about/org-info/who-we-accredit/accredited/
- 6.Asia-Pacific Academic Consortium for Public Health Member institutions. https://www.apacph.org/wp/members-list/
- 7.The Association of School of Public Health in the European Region ASPHER Directory. https://www.aspher.org/users.html?etykieta=3&kraj=0
- 8.WHO National health workforce accounts data portal. https://apps.who.int/nhwaportal/
- 9.Organisation for Economic Co-operation and Development OECD health statistics 2021. 2021. https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_REAC
- 10.The World Bank Population, total. 2021. https://data.worldbank.org/indicator/SP.POP.TOTL
- 11.WHO State of the world's nursing 2020: investing in education, jobs and leadership. 2020. https://www.who.int/publications/i/item/9789240003279
- 12.Haakenstad A, Irvine CMS, Knight M, et al. Measuring the availability of human resources for health and its relationship to universal health coverage for 204 countries and territories from 1990 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;399:2129–2154. doi: 10.1016/S0140-6736(22)00532-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shaffer FA. Sustain and retain: an urgent action agenda for a sustainable global nursing workforce beyond the pandemic. 2022. https://www.myamericannurse.com/sustain-and-retain-workforce/
- 14.Ten Cate O, Graafmans L, Posthumus I, Welink L, van Dijk M. The EPA-based Utrecht undergraduate clinical curriculum: development and implementation. Med Teach. 2018;40:506–513. doi: 10.1080/0142159X.2018.1435856. [DOI] [PubMed] [Google Scholar]
- 15.Berberat PO, Harendza S, Kadmon M. Entrustable professional activities—visualization of competencies in postgraduate training. Position paper of the Committee on Postgraduate Medical Training of the German Society for Medical Education (GMA) GMS Z Med Ausbild. 2013;30 doi: 10.3205/zma000890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Westein MPD, de Vries H, Floor A, Koster AS, Buurma H. Development of a postgraduate community pharmacist specialization program using CANMEDS competencies, and entrustable professional activities. Am J Pharm Educ. 2019;83 doi: 10.5688/ajpe6863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lomis K, Amiel JM, Ryan MS, et al. Implementing an entrustable professional activities framework in undergraduate medical education: early lessons from the AAMC core entrustable professional activities for entering residency pilot. Acad Med. 2017;92:765–770. doi: 10.1097/ACM.0000000000001543. [DOI] [PubMed] [Google Scholar]
- 18.Edgar L, Roberts S, Holmboe E. Milestones 2.0: a step forward. J Grad Med Educ. 2018;10:367–369. doi: 10.4300/JGME-D-18-00372.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matlow A, Chan MK, Bohnen JD, et al. Collaborating internationally on physician leadership education: first steps. Leadersh Health Serv (Bradf Engl) 2016;29:220–230. doi: 10.1108/LHS-12-2015-0049. [DOI] [PubMed] [Google Scholar]
- 20.Arora G, Condurache T, Batra M, et al. Miles away milestones: a framework for assessment of pediatric residents during global health rotations. Acad Pediatr. 2017;17:577–579. doi: 10.1016/j.acap.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 21.Kelly T, Lazenby M. Developing and validating learning domains, competencies, and evaluation items for global health clinical immersion practicums for graduate-level nursing programs. J Adv Nurs. 2019;75:234–252. doi: 10.1111/jan.13851. [DOI] [PubMed] [Google Scholar]
- 22.Lutfiyya MN, Brandt B, Delaney C, Pechacek J, Cerra F. Setting a research agenda for interprofessional education and collaborative practice in the context of United States health system reform. J Interprof Care. 2016;30:7–14. doi: 10.3109/13561820.2015.1040875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ely LI, Toassi RFC. Integration among curricula in health professionals’ education: the power of interprofessional education in undergraduate courses. Interface Comunicacao Saude Educ. 2018;22:1563–1575. [Google Scholar]
- 24.Caverzagie KJ, Lane SW, Sharma N, et al. Proposed performance-based metrics for the future funding of graduate medical education: starting the conversation. Acad Med. 2018;93:1002–1013. doi: 10.1097/ACM.0000000000002096. [DOI] [PubMed] [Google Scholar]
- 25.Kutt A, Mayan M, Bienko I, Davies J, Bhatt H, Vohra S. An undergraduate course combining interprofessional education and complementary health approaches learning objectives: successful integrative learning that improves interest and reduces redundancy. Explore (NY) 2019;15:273–282. doi: 10.1016/j.explore.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 26.Pepin J, Goudreau J, Lavoie P, et al. A nursing education research framework for transformative learning and interdependence of academia and practice. Nurse Educ Today. 2017;52:50–52. doi: 10.1016/j.nedt.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 27.Fonn S. Linking public health training and health systems development in sub-Saharan Africa: opportunities for improvement and collaboration. J Public Health Policy. 2011;32(suppl 1):S44–S51. doi: 10.1057/jphp.2011.37. [DOI] [PubMed] [Google Scholar]
- 28.Phlypo I, De Tobel J, Marks L, De Visschere L, Koole S. Integrating community service learning in undergraduate dental education: a controlled trial in a residential facility for people with intellectual disabilities. Spec Care Dentist. 2018;38:201–207. doi: 10.1111/scd.12298. [DOI] [PubMed] [Google Scholar]
- 29.Manabe YC, Campbell JD, Ovuga E, Maling S, Bollinger RC, Sewankambo N. Optimisation of the Medical Education Partnership Initiative to address African health-care challenges. Lancet Glob Health. 2014;2:e392. doi: 10.1016/S2214-109X(14)70235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naegle MA, Hanley K, Gourevitch MN, Tuchman E, More FG, Bereket S. Project SARET: an interprofessional education (IPE) lens examines substance use disorders research education for health professional students. J Interprof Educ Pract. 2017;9:99–103. doi: 10.1016/j.xjep.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rawal LB, Mahmud K, Islam SMS, Mahumud RA, Nuruzaman M, Ahmed SM. Training mid-level health cadres to improve health service delivery in rural Bangladesh. Prim Health Care Res Dev. 2016;17:503–513. doi: 10.1017/S1463423616000104. [DOI] [PubMed] [Google Scholar]
- 32.Caverzagie KJ, Nousiainen MT, Ferguson PC, et al. Overarching challenges to the implementation of competency-based medical education. Med Teach. 2017;39:588–593. doi: 10.1080/0142159X.2017.1315075. [DOI] [PubMed] [Google Scholar]
- 33.Tomiak A, Braund H, Egan R, et al. Exploring how the new entrustable professional activity assessment tools affect the quality of feedback given to medical oncology residents. J Cancer Educ. 2020;35:165–177. doi: 10.1007/s13187-018-1456-z. [DOI] [PubMed] [Google Scholar]
- 34.Patrício MF, Julião M, Fareleira F, Carneiro AV. Is the OSCE a feasible tool to assess competencies in undergraduate medical education? Med Teach. 2013;35:503–514. doi: 10.3109/0142159X.2013.774330. [DOI] [PubMed] [Google Scholar]
- 35.Peluso MJ, van Schalkwyk S, Kellett A, et al. Reframing undergraduate medical education in global health: rationale and key principles from the Bellagio Global Health Education Initiative. Med Teach. 2017;39:639–645. doi: 10.1080/0142159X.2017.1301654. [DOI] [PubMed] [Google Scholar]
- 36.Hauer KE, Hirsh D, Ma I, et al. The role of role: learning in longitudinal integrated and traditional block clerkships. Med Educ. 2012;46:698–710. doi: 10.1111/j.1365-2923.2012.04285.x. [DOI] [PubMed] [Google Scholar]
- 37.Rekman J, Gofton W, Dudek N, Gofton T, Hamstra SJ. Entrustability scales: outlining their usefulness for competency-based clinical assessment. Acad Med. 2016;91:186–190. doi: 10.1097/ACM.0000000000001045. [DOI] [PubMed] [Google Scholar]
- 38.Albarqouni L, Elessi K. Awareness, attitudes and knowledge about evidence based medicine among doctors in Gaza: a crosssectional survey. East Mediterr Health J. 2017;23:626–631. [PubMed] [Google Scholar]
- 39.Michaud PA. Reforms of the pre-graduate curriculum for medical students: the Bologna process and beyond. Swiss Med Wkly. 2012;142 doi: 10.4414/smw.2012.13738. [DOI] [PubMed] [Google Scholar]
- 40.Evans DP, Anderson M, Shahpar C, Del Rio C, Curran JW. Innovation in graduate education for health professionals in humanitarian emergencies. Prehosp Disaster Med. 2016;31:532–538. doi: 10.1017/S1049023X16000650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pinto HA, Andreazza R, Ribeiro RJ, Loula MR, Dos Reis AAC. The more doctors program and the changing role of the state in the regulation and organization of medical education. Interface (Botucatu) 2019;23 [Google Scholar]
- 42.Mazotti L, Adams J, Peyser B, Chretien K, Duffy B, Hirsh DA. Diffusion of innovation and longitudinal integrated clerkships: results of the clerkship directors in internal medicine annual survey. Med Teach. 2019;41:347–353. doi: 10.1080/0142159X.2018.1472369. [DOI] [PubMed] [Google Scholar]
- 43.Blum N, Berlin A, Isaacs A, Burch WJ, Willott C. Medical students as global citizens: a qualitative study of medical students’ views on global health teaching within the undergraduate medical curriculum. BMC Med Educ. 2019;19:175. doi: 10.1186/s12909-019-1631-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Amuguni H, Bikaako W, Naigaga I, Bazeyo W. Building a framework for the design and implementation of One Health curricula in East and Central Africa: OHCEAs One Health Training Modules Development Process. One Health. 2019;7:7. doi: 10.1016/j.onehlt.2018.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Busari J, Chan MK, Dath D, Matlow A, Meschino DC. Sanokondu. Leadersh Health Serv (Bradf Engl) 2018;31:254–264. doi: 10.1108/LHS-01-2018-0001. [DOI] [PubMed] [Google Scholar]
- 46.Josiah Macy Jr. Foundation Macy Faculty Scholars Program. https://macyfoundation.org/macy-scholars
- 47.Berman P, Frenk J. The new Harvard Doctor of Public Health: lessons from the design and implementation of an innovative program in advanced professional leadership. Public Health Rep. 2018;133:759–766. doi: 10.1177/0033354918804523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Withers M, Lin HH, Schmidt T, Delos Trinos JPCR, Kumar S. Establishing competencies for a global health workforce: recommendations from the Association of Pacific Rim Universities. Ann Glob Health. 2019;85:47. doi: 10.5334/aogh.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shilkofski N, Crichlow A, Rice J, et al. A standardized needs assessment tool to inform the curriculum development process for pediatric resuscitation simulation-based education in resources-limited settings. Front Pediatr. 2018;6:37. doi: 10.3389/fped.2018.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kelly CM, Vins H, Spicer JO, et al. The rapid scale up of medical education in Ethiopia: medical student experiences and the role of e-learning at Addis Ababa University. PLoS One. 2019;14 doi: 10.1371/journal.pone.0221989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Seymour B, Muhumuza I, Mumena C, Isyagi M, Barrow J, Meeks V. Including oral health training in a health system strengthening program in Rwanda. Glob Health Action. 2013;6:1–6. doi: 10.3402/gha.v6i0.20109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaaya EE, Macfarlane SB, Mkony CA, et al. Educating enough competent health professionals: advancing educational innovation at Muhimbili University of Health and Allied Sciences, Tanzania. PLoS Med. 2012;9 doi: 10.1371/journal.pmed.1001284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Interprofessional Education Collaborative Core competencies for interprofessional collaborative practice: 2016 update. 2016. https://ipec.memberclicks.net/assets/2016-Update.pdf
- 54.Brashers V, Owen J, Haizlip J. Interprofessional education and practice guide number 2: developing and implementing a center for interprofessional education. J Interprof Care. 2015;29:95–99. doi: 10.3109/13561820.2014.962130. [DOI] [PubMed] [Google Scholar]
- 55.Brashers V, Erickson JM, Blackhall L, Owen JA, Thomas SM, Conaway MR. Measuring the impact of clinically relevant interprofessional education on undergraduate medical and nursing student competencies: a longitudinal mixed methods approach. J Interprof Care. 2016;30:448–457. doi: 10.3109/13561820.2016.1162139. [DOI] [PubMed] [Google Scholar]
- 56.Botma Y, Snyman S. Africa Interprofessional Education Network (AfrIPEN) J Interprof Care. 2019;33:274–276. doi: 10.1080/13561820.2019.1605236. [DOI] [PubMed] [Google Scholar]
- 57.Chuenkongkaew W. In: Sustainability and interprofessional collaboration: ensuring leadership resilience in collaborative health care. Forman D, Jones M, Thistlethwaite J, editors. Springer International Publishing; Cham: 2020. Starting, growing and sustaining leadership in interprofessional collaboration in Thailand; pp. 83–102. [Google Scholar]
- 58.Arndell C, Proffitt B, Disco M, Clithero A. Street outreach and shelter care elective for senior health professional students: an interprofessional educational model for addressing the needs of vulnerable populations. Educ Health (Abingdon) 2014;27:99–102. doi: 10.4103/1357-6283.134361. [DOI] [PubMed] [Google Scholar]
- 59.Jakobsen F, Hansen J. Spreading the concept: an attempt to translate an interprofessional clinical placement across a Danish hospital. J Interprof Care. 2014;28:407–412. doi: 10.3109/13561820.2014.900479. [DOI] [PubMed] [Google Scholar]
- 60.Pilon BA, Ketel C, Davidson HA, et al. Evidence-guided integration of interprofessional collaborative practice into nurse managed health centers. J Prof Nurs. 2015;31:340–350. doi: 10.1016/j.profnurs.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 61.Brewer ML, Flavell H, Trede F, Smith M. Creating change agents for interprofessional education and practice: a leadership programme for academic staff and health practitioners. Int J Leadersh Educ. 2018;21:580–592. [Google Scholar]
- 62.Hall LW, Zierler BK. Interprofessional education and practice guide number 1: developing faculty to effectively facilitate interprofessional education. J Interprof Care. 2015;29:3–7. doi: 10.3109/13561820.2014.937483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khalili H, Orchard C, Laschinger HKS, Farah R. An interprofessional socialization framework for developing an interprofessional identity among health professions students. J Interprof Care. 2013;27:448–453. doi: 10.3109/13561820.2013.804042. [DOI] [PubMed] [Google Scholar]
- 64.Joynes VCT. Defining and understanding the relationship between professional identity and interprofessional responsibility: implications for educating health and social care students. Adv Health Sci Educ Theory Pract. 2018;23:133–149. doi: 10.1007/s10459-017-9778-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kahaleh AA, Danielson J, Franson KL, Nuffer WA, Umland EM. An interprofessional education panel on development, implementation, and assessment strategies. Am J Pharm Educ. 2015;79:78. doi: 10.5688/ajpe79678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Anderson ES, Ford J, Kinnair DJ. Interprofessional education and practice guide number 6: developing practice-based interprofessional learning using a short placement model. J Interprof Care. 2016;30:433–440. doi: 10.3109/13561820.2016.1160040. [DOI] [PubMed] [Google Scholar]
- 67.Langlois S. Mapping current health professional curricula: identifying common topics for an integrated interprofessional education curriculum. J Interprof Educ Pract. 2016;5:7–9. [Google Scholar]
- 68.Tong SF, Mohamad N, Tan CE, Efendie B, Chelliah KK, Gilbert JHV. In: Leading research and evaluation in interprofessional education and collaborative practice. Forman D, Jones M, Thristlethwaite J, editors. Palgrave Macmillan; London: 2016. Transition from uniprofessional towards interprofessional education: the Malaysian experience of a pragmatic model; pp. 169–192. [Google Scholar]
- 69.Ghebrehiwet T, Ammon M, Burbiel I, Botbol M. In: Person centered psychiatry. Mezzich J, Botbol M, Christodoulou G, Cloninger C, Salloum I, editors. Springer; Cham: 2016. Interdisciplinary team approach to clinical care; pp. 211–222. [Google Scholar]
- 70.Busari JO, Moll FM, Duits AJ. Understanding the impact of interprofessional collaboration on the quality of care: a case report from a small-scale resource limited health care environment. J Multidiscip Healthc. 2017;10:227–234. doi: 10.2147/JMDH.S140042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hämel K, Vössing C. The collaboration of general practitioners and nurses in primary care: a comparative analysis of concepts and practices in Slovenia and Spain. Prim Health Care Res Dev. 2017;18:492–506. doi: 10.1017/S1463423617000354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Findyartini A, Kambey DR, Yusra RY, et al. Interprofessional collaborative practice in primary healthcare settings in Indonesia: a mixed-methods study. J Interprof Educ Pract. 2019;17:17. [Google Scholar]
- 73.Fritze O, Lammerding-Koeppel M, Boeker M, et al. Boosting competence-orientation in undergraduate medical education— a web-based tool linking curricular mapping and visual analytics. Med Teach. 2019;41:422–432. doi: 10.1080/0142159X.2018.1487047. [DOI] [PubMed] [Google Scholar]
- 74.Komenda M, Karolyi M, Pokorná A, Vaitsis C. Medical and healthcare curriculum exploratory analysis. Stud Health Technol Inform. 2017;235:231–235. [PubMed] [Google Scholar]
- 75.Prober CG, Khan S. Medical education reimagined: a call to action. Acad Med. 2013;88:1407–1410. doi: 10.1097/ACM.0b013e3182a368bd. [DOI] [PubMed] [Google Scholar]
- 76.Hrastinski S. Asynchronous and synchronous e-learning. EDUCASE Review. 2008. https://er.educause.edu/articles/2008/11/asynchronous-and-synchronous-elearning
- 77.Robert Wood Johnson Foundation Project ECHO. https://www.rwjf.org/en/how-we-work/grants-explorer/featured-programs/project-echo.html
- 78.American Academy of Pediatrics Project ECHO. https://www.aap.org/en/practice-management/project-echo/
- 79.Phillips Phillips ICU telemedicine program. https://www.usa.philips.com/healthcare/resources/landing/teleicu
- 80.DeFilippis EM, Jaigirdar T, Gaglani SM, et al. Open osmosis: library of open educational resources (OER) for medical education. Innovations in Global Health Professions Education. 2015;3 [Google Scholar]
- 81.Berman NB, Durning SJ, Fischer MR, Huwendiek S, Triola MM. The role for virtual patients in the future of medical education. Acad Med. 2016;91:1217–1222. doi: 10.1097/ACM.0000000000001146. [DOI] [PubMed] [Google Scholar]
- 82.Surgical Science Sweden AB LAP Mentor VR. https://www.3dsystems.com/healthcare/lap-mentor-vr
- 83.Cook NF, McAloon T, O'Neill P, Beggs R. Impact of a web based interactive simulation game (PULSE) on nursing students’ experience and performance in life support training—a pilot study. Nurse Educ Today. 2012;32:714–720. doi: 10.1016/j.nedt.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 84.Zhonggen Y. A meta-analysis of use of serious games in education over a decade. Int J Comput Games Technol. 2019;2019:1–8. [Google Scholar]
- 85.Carlson K, Gagnon D. Augmented reality integrated simulation education in health care. Clin Simul Nurs. 2016;12:123–127. [Google Scholar]
- 86.Martini ND, Webster CS. Evaluation of interprofessional learning among medical and pharmacy students using a virtual patient simulation. IEEE 6th International Conference on Serious Games and Applications for Health (SeGAH); May 16–18, 2018.
- 87.Nicol P. University of Technology; Sydney: 2013. Interprofessional education for health professions in Western Australia: perspectives and activity. [Google Scholar]
- 88.Englander R, Cameron T, Ballard AJ, Dodge J, Bull J, Aschenbrener CA. Toward a common taxonomy of competency domains for the health professions and competencies for physicians. Acad Med. 2013;88:1088–1094. doi: 10.1097/ACM.0b013e31829a3b2b. [DOI] [PubMed] [Google Scholar]
- 89.Frank JR, Mungroo R, Ahmad Y, Wang M, De Rossi S, Horsley T. Toward a definition of competency-based education in medicine: a systematic review of published definitions. Med Teach. 2010;32:631–637. doi: 10.3109/0142159X.2010.500898. [DOI] [PubMed] [Google Scholar]
- 90.Zieck MRM, Um IS, Chaar BB. The future of weight management in pharmacy education—perspectives of new generation pharmacists. Curr Pharm Teach Learn. 2018;10:596–601. doi: 10.1016/j.cptl.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 91.WHO Framework for action on interprofessional education and collaborative practice. 2010. https://www.who.int/publications/i/item/framework-for-action-on-interprofessional-education-collaborative-practice [PubMed]
- 92.Centre for Advancement of Interprofessional Education About CAIPE. https://www.caipe.org/about
- 93.Speyer R, Denman D, Wilkes-Gillan S, et al. Effects of telehealth by allied health professionals and nurses in rural and remote areas: a systematic review and meta-analysis. J Rehabil Med. 2018;50:225–235. doi: 10.2340/16501977-2297. [DOI] [PubMed] [Google Scholar]
- 94.Hasham S, Sayani S. Implementation lessons on the use of innovation in information technology in the developing world. World Hosp Health Serv. 2013;49:10–13. [PubMed] [Google Scholar]
- 95.Taveira-Gomes T, Saffarzadeh A, Severo M, Guimarães MJ, Ferreira MA. A novel collaborative e-learning platform for medical students—alert student. BMC Med Educ. 2014;14:143. doi: 10.1186/1472-6920-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gao XY, Yu RB, Shen HB, Chen Q. An outline of a proposed five-plus three-year combined undergraduate-master's degree for clinical medicine majors at Nanjing Medical University. Chin Educ Soc. 2014;47:6–23. [Google Scholar]
- 97.Cevik AA, Aksel G, Akoglu H, Eroglu SE, Dogan NO, Altunci YA. Social media, FOAMed in medical education and knowledge sharing: local experiences with international perspective. Turk J Emerg Med. 2016;16:112–117. doi: 10.1016/j.tjem.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Battat R, Jhonson M, Wiseblatt L, et al. The Haiti Medical Education Project: development and analysis of a competency based continuing medical education course in Haiti through distance learning. BMC Med Educ. 2016;16:275. doi: 10.1186/s12909-016-0795-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Aboshady OA, Radwan AE, Eltaweel AR, et al. Perception and use of massive open online courses among medical students in a developing country: multicentre cross-sectional study. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-006804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wikipedia List of countries by number of internet users. 2020. https://en.wikipedia.org/wiki/List_of_countries_by_number_of_Internet_users
- 101.Koenig R. With money from Facebook, ten colleges turn their campuses into ‘metaversities’. 2022. https://www.edsurge.com/news/2022-06-01-withmoney-from-facebook-10-colleges-turn-their-campuses-into-metaversities
- 102.Gordon M, Patricio M, Horne L, et al. Developments in medical education in response to the COVID-19 pandemic: a rapid BEME systematic review: BEME guide number 63. Med Teach. 2020;42:1202–1215. doi: 10.1080/0142159X.2020.1807484. [DOI] [PubMed] [Google Scholar]
- 103.Daniel M, Gordon M, Patricio M, et al. An update on developments in medical education in response to the COVID-19 pandemic: a BEME scoping review: BEME guide number 64. Med Teach. 2021;43:253–271. doi: 10.1080/0142159X.2020.1864310. [DOI] [PubMed] [Google Scholar]
- 104.International Council of Nurses Nursing education and the emerging nursing workforce in COVID-19 pandemic. 2021. https://www.icn.ch/sites/default/files/inline-files/ICN%20Policy%20Brief_Nursing%20Education.pdf
- 105.Carroll Turpin MA, Steele K, Matuk-Villazon O, Rowland K, Dayton CB, Horn KV. Rapid transition to a virtual multiple mini-interview admissions process: a new medical school's experience during the COVID-19 pandemic. Acad Med. 2021;96:1152–1155. doi: 10.1097/ACM.0000000000004179. [DOI] [PubMed] [Google Scholar]
- 106.Kulasegaram K, Baxan V, Giannone E, Latter D, Hanson MD. Adapting the admissions interview during COVID-19: a comparison of in-person and video-based interview validity evidence. Acad Med. 2022;97:200–206. doi: 10.1097/ACM.0000000000004331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Samarasekera DD, Goh DLM, Yeo SP, et al. Response and lessons learnt managing the COVID-19 crisis by School of Medicine, National University of Singapore. MedEdPublish. 2020;9 doi: 10.15694/mep.2020.000092.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Day RW, Taylor BM, Bednarski BK, et al. Virtual interviews for surgical training program applicants during COVID-19: lessons learned and recommendations. Ann Surg. 2020;272:e144–e147. doi: 10.1097/SLA.0000000000004064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Molina G, Mehtsun WT, Qadan M, Hause KC, Raut CP, Fairweather M. Virtual interviews for the complex general surgical oncology fellowship: the Dana-Farber/partners experience. Ann Surg Oncol. 2020;27:3103–3106. doi: 10.1245/s10434-020-08778-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Vining CC, Eng OS, Hogg ME, et al. Virtual surgical fellowship recruitment during COVID-19 and its implications for resident/fellow recruitment in the future. Ann Surg Oncol. 2020;27(suppl 3):911–915. doi: 10.1245/s10434-020-08623-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Marbin J, Hutchinson YV, Schaeffer S. Avoiding the virtual pitfall: identifying and mitigating biases in graduate medical education videoconference interviews. Acad Med. 2021;96:1120–1124. doi: 10.1097/ACM.0000000000003914. [DOI] [PubMed] [Google Scholar]
- 112.Perez M, Williams C, Vapiwala N. “Holistic admissions” during a pandemic: the effects of COVID-19 on socioeconomically disadvantaged medical school applicants. Acad Med. 2021;96:e3–e4. doi: 10.1097/ACM.0000000000003613. [DOI] [PubMed] [Google Scholar]
- 113.Burk-Rafel J, Standiford TC. A novel ticket system for capping residency interview numbers: reimagining interviews in the COVID-19 era. Acad Med. 2021;96:50–55. doi: 10.1097/ACM.0000000000003745. [DOI] [PubMed] [Google Scholar]
- 114.Chick RC, Clifton GT, Peace KM, et al. Using technology to maintain the education of residents during the COVID-19 pandemic. J Surg Educ. 2020;77:729–732. doi: 10.1016/j.jsurg.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kanneganti A, Sia CH, Ashokka B, Ooi SBS. Continuing medical education during a pandemic: an academic institution's experience. Postgrad Med J. 2020;96:384–386. doi: 10.1136/postgradmedj-2020-137840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Buonsenso D, Moro F, Inchingolo R, et al. Effectiveness of a ‘fast lung ultrasound teaching program’ for gynecologists/obstetricians dealing with pregnant women with suspicion of COVID-19 infection. Ultrasound Obstet Gynecol. 2020;56:110–111. doi: 10.1002/uog.22066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gardiner C, Veall J, Lockhart S. The use of UV fluorescent powder for COVID-19 airway management simulation training. Anaesthesia. 2020;75:964–965. doi: 10.1111/anae.15089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hanel E, Bilic M, Hassall K, et al. Virtual application of in situ simulation during a pandemic. CJEM. 2020;24:1–6. doi: 10.1017/cem.2020.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Christensen L, Rasmussen CS, Benfield T, Franc JM. A randomized trial of instructor-led training versus video lesson in training health care providers in proper donning and doffing of personal protective equipment. Disaster Med Public Health Prep. 2020;14:514–520. doi: 10.1017/dmp.2020.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lang A, Burger B, Doraiswamy V, et al. POPCoRN one-pagers: educational materials for pediatric providers caring for adults. Acad Pediatr. 2020;20:757–758. doi: 10.1016/j.acap.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hannon P, Lappe K, Griffin C, Roussel D, Colbert-Getz J. An objective structured clinical examination: from examination room to Zoom breakout room. Med Educ. 2020;54:861. doi: 10.1111/medu.14241. [DOI] [PubMed] [Google Scholar]
- 122.Prigoff J, Hunter M, Nowygrod R. Medical student assessment in the time of COVID-19. J Surg Educ. 2021;78:370–374. doi: 10.1016/j.jsurg.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Gulati RR, Reid H, Gill M. Instagram for peer teaching: opportunity and challenge. Educ Prim Care. 2020;31:382–384. doi: 10.1080/14739879.2020.1811163. [DOI] [PubMed] [Google Scholar]
- 124.Malhotra R, Gautam D, George J, Goyal D, Ansari MT. Conducting orthopaedic practical examination during the COVID-19 pandemic. J Clin Orthop Trauma. 2020;11(suppl 4):S448–S455. doi: 10.1016/j.jcot.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jain S, Carlos WG., 3rd Learning in the time of COVID-19: key lessons from the pandemic for medical trainees. Acad Med. 2021;96:1660–1662. doi: 10.1097/ACM.0000000000003909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tsang VWL, Yu A, Haines MJ, et al. Transforming disruption into innovation: a partnership between the COVID-19 medical student response team and the University of British Columbia. Acad Med. 2021;96:1650–1654. doi: 10.1097/ACM.0000000000004156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cantave M, Perlson J, Lewis C, Byers B. COVID-19 reveals why we need physician advocates now. Acad Med. 2020;95 doi: 10.1097/ACM.0000000000003479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Clark VR. Erasing the false equivalency: pandemics, public health, and physician education. Acad Med. 2020;95:e11. doi: 10.1097/ACM.0000000000003607. [DOI] [PubMed] [Google Scholar]
- 129.Godley BF, Lawley TJ, Rubenstein A, Pizzo PA. How academic medical centers can navigate the pandemic and its aftermath: solutions for 3 major issues. Acad Med. 2021;96:1529–1533. doi: 10.1097/ACM.0000000000004155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jumreornvong O, Yang E, Race J, Appel J. Telemedicine and medical education in the age of COVID-19. Acad Med. 2020;95:1838–1843. doi: 10.1097/ACM.0000000000003711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rose CC, Haas MRC, Yilmaz Y, et al. ALiEM connect: large-scale, interactive, virtual residency programming in response to COVID-19. Acad Med. 2021;96:1419–1424. doi: 10.1097/ACM.0000000000004122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Rydel TA, Bajra R, Schillinger E. Hands off yet all in: a virtual clerkship pilot in the ambulatory setting during the COVID-19 pandemic. Acad Med. 2021;96:1702–1705. doi: 10.1097/ACM.0000000000004127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Xu L, Ambinder D, Kang J, et al. Virtual grand rounds as a novel means for applicants and programs to connect in the era of COVID-19. Am J Surg. 2021;221:956–961. doi: 10.1016/j.amjsurg.2020.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Lara S, Foster CW, Hawks M, Montgomery M. Remote assessment of clinical skills during COVID-19: a virtual, high-stakes, summative pediatric objective structured clinical examination. Acad Pediatr. 2020;20:760–761. doi: 10.1016/j.acap.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lawrence K, Hanley K, Adams J, Sartori DJ, Greene R, Zabar S. Building telemedicine capacity for trainees during the novel coronavirus outbreak: a case study and lessons learned. J Gen Intern Med. 2020;35:2675–2679. doi: 10.1007/s11606-020-05979-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Gaber DA, Shehata MH, Amin HAA. Online team-based learning sessions as interactive methodologies during the pandemic. Med Educ. 2020;54:666–667. doi: 10.1111/medu.14198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Agarwal S, Sabadia S, Abou-Fayssal N, Kurzweil A, Balcer LJ, Galetta SL. Training in neurology: flexibility and adaptability of a neurology training program at the epicenter of COVID-19. Neurology. 2020;94:e2608–e2614. doi: 10.1212/WNL.0000000000009675. [DOI] [PubMed] [Google Scholar]
- 138.Durrani M. Debate style lecturing to engage and enrich resident education virtually. Med Educ. 2020;54:955–956. doi: 10.1111/medu.14217. [DOI] [PubMed] [Google Scholar]
- 139.Fernandez-Altuna M, Gutierrez Rayon D, Ramirez Resendiz M, Cruz Mendez P, Tovar Lopez KA. Experience of the biggest med school in Mexico during the COVID-19 pandemic. MedEdPublish. 2020;9 doi: 10.15694/mep.2020.000101.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Hofmann H, Harding C, Youm J, Wiechmann W. Virtual bedside teaching rounds with patients with COVID-19. Med Educ. 2020;54:959–960. doi: 10.1111/medu.14223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Peterson WJ, Munzer BW, Tucker RV, et al. Rapid dissemination of a COVID-19 airway management simulation using a train-the-trainers curriculum. Acad Med. 2021;96:1414–1418. doi: 10.1097/ACM.0000000000004120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Choi GYS, Wan WTP, Chan AKM, Tong SK, Poon ST, Joynt GM. Preparedness for COVID-19: in situ simulation to enhance infection control systems in the intensive care unit. Br J Anaesth. 2020;125:e236–e239. doi: 10.1016/j.bja.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Colman N, Doughty C, Arnold J, et al. Simulation-based clinical systems testing for healthcare spaces: from intake through implementation. Adv Simul (Lond) 2019;4:19. doi: 10.1186/s41077-019-0108-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Dubé M, Kaba A, Cronin T, Barnes S, Fuselli T, Grant V. COVID-19 pandemic preparation: using simulation for systems-based learning to prepare the largest healthcare workforce and system in Canada. Adv Simul (Lond) 2020;5:22. doi: 10.1186/s41077-020-00138-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ray JM, Wong AH, Yang TJ, et al. Virtual telesimulation for medical students during the COVID-19 pandemic. Acad Med. 2021;96:1431–1435. doi: 10.1097/ACM.0000000000004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Giving. A teaching hospital for the 21st century. 2022. https://giving.massgeneral.org/stories/a-teaching-hospital-for-the-21st-century
- 147.Co M, Chu KM. Distant surgical teaching during COVID-19— a pilot study on final year medical students. Surg Pract. 2020;24:105–109. doi: 10.1111/1744-1633.12436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Kuo M, Poirier MV, Pettitt-Schieber B, et al. Efficacy of vascular virtual medical student education during the coronavirus disease 2019 pandemic. J Vasc Surg. 2021;73:348–349. doi: 10.1016/j.jvs.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gallardo FC, Martin C, Targa Garcia AA, Bustamante JL, Nuñez M, Feldman SE. Home program for acquisition and maintenance of microsurgical skills during the coronavirus disease 2019 outbreak. World Neurosurg. 2020;143:557–563.e1. doi: 10.1016/j.wneu.2020.07.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Nix K, Liu EL, Oh L, et al. A distance-learning approach to point-of-care ultrasound training (ADAPT): a multi-institutional educational response during the COVID-19 pandemic. Acad Med. 2021;96:1711–1716. doi: 10.1097/ACM.0000000000004399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kimmons R, Graham CR, West RE. The PICRAT model for technology integration in teacher preparation. Contemp Issues Technol Teach Educ. 2020;20:176–198. [Google Scholar]
- 152.Khamees D, Peterson W, Patricio M, et al. Remote learning developments in postgraduate medical education in response to the COVID-19 pandemic—a BEME systematic review: BEME guide number 71. Med Teach. 2022;44:466–485. doi: 10.1080/0142159X.2022.2040732. [DOI] [PubMed] [Google Scholar]
- 153.Blankenburg R, Gonzalez Del Rey J, Aylor M, et al. The impact of the COVID-19 pandemic on pediatric graduate medical education: lessons learned and pathways forward. Acad Med. 2022;97:S35–S39. doi: 10.1097/ACM.0000000000004532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ramotshwana B, Gupta A, Seth S, Shah H. New physicians, new challenges: the impact of accelerated graduation and deployment due to COVID-19. Acad Med. 2021;96:e15. doi: 10.1097/ACM.0000000000003996. [DOI] [PubMed] [Google Scholar]
- 156.Flotte TR, Larkin AC, Fischer MA, et al. Accelerated graduation and the deployment of new physicians during the COVID-19 pandemic. Acad Med. 2020;95:1492–1494. doi: 10.1097/ACM.0000000000003540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Vande Vusse LK, Ryder HF, Best JA. Maximizing career advancement during the COVID-19 pandemic: recommendations for postgraduate training programs. Acad Med. 2021;96:967–973. doi: 10.1097/ACM.0000000000003938. [DOI] [PubMed] [Google Scholar]
- 158.Rotenstein LS, Berwick DM, Cassel CK. Addressing well-being throughout the health care workforce: the next imperative. JAMA. 2022;328:521–522. doi: 10.1001/jama.2022.12437. [DOI] [PubMed] [Google Scholar]
- 159.Aiken LH, Simonetti M, Sloane DM, et al. Hospital nurse staffing and patient outcomes in Chile: a multilevel cross-sectional study. Lancet Glob Health. 2021;9:e1145–e1153. doi: 10.1016/S2214-109X(21)00209-6. [DOI] [PubMed] [Google Scholar]
- 160.Allen M, Mabry E, Mattrey M, Bourhis J, Titsworth S, Burrell N. Evaluating the effectiveness of distance learning: a comparison using meta-analysis. J Commun. 2004;54:402–420. [Google Scholar]
- 161.Alrassi J, Katsufrakis PJ, Chandran L. Technology can augment, but not replace, critical human skills needed for patient care. Acad Med. 2021;96:37–43. doi: 10.1097/ACM.0000000000003733. [DOI] [PubMed] [Google Scholar]
- 162.Cheetham G, Chivers G. Edward Elgar; Cheltenham, UK: 2005. Professions, competence and informal learning. [Google Scholar]
- 163.Dzau VJ, Laitner MH, Balatbat CA. Has traditional medicine had its day? The need to redefine academic medicine. Lancet. 2022 doi: 10.1016/S0140-6736(22)01603-8. published online Sept 20. [DOI] [PubMed] [Google Scholar]
- 164.Topol E. Health Education England; England: 2019. The Topol review. Preparing the healthcare workforce to deliver the digital future. [Google Scholar]
- 165.Crisp N, Poulter D, Gnanapragasam S, et al. Health workers as agents of change and curators of knowledge. Lancet. 2022;400:417–418. doi: 10.1016/S0140-6736(22)01300-9. [DOI] [PubMed] [Google Scholar]
- 166.Penfold RS, Ali MA, Ali AM, et al. Evaluation of the first year of the Oxpal Medlink: a web-based partnership designed to address specific challenges facing medical education in the occupied Palestinian territories. JRSM Open. 2014;5 doi: 10.1177/2042533313517692. 2042533313517692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Posever N, Sehdev M, Sylla M, Mashar R, Mashar M, Abioye A. Addressing equity in global medical education during the COVID-19 pandemic: the Global Medical Education Collaborative. Acad Med. 2021;96:1574–1579. doi: 10.1097/ACM.0000000000004230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.