INTRODUCTION
Acute chest pain is the second most common cause of admission to the emergency department after trauma. Causes of chest pain vary and can be cardiac or noncardiac.1 Angina triggered by cardiac ischemia can indicate an acute coronary syndrome.2 Upon suspicion of acute coronary syndrome, risk stratification for cardiac ischemia dictates management.1 In this case, an episode of angina in a patient is presented in the setting of intravenous phosphate supplementation in acute severe complicated pancreatitis. This was a case of acute chest pain associated with sodium phosphate intravenous infusion in complicated acute pancreatitis associated with severe hypophosphatemia.
CASE REPORT
A 46-year-old male patient with no past cardiac history presented for severe abdominal pain. He had a past medical history of cholecystitis treated with laparoscopic cholecystectomy 12 days prior to presentation. One day prior to his presentation, he underwent an endoscopic retrograde cholangiopancreatography (ERCP). He developed epigastric pain one hour after ERCP. The pain was radiating to the back, progressively worsening, and associated with subjective shortness of breath, decreased oral intake, and nausea.
On physical examination, the patient was in distress. His abdomen was diffusely tender to palpation, with guarding but no rebound pain. Chest exam showed tachypnea with no abnormal breath sounds on auscultation. Otherwise, vital signs were normal. His lipase level was > 7500 U/L, and his abdominal computed tomography (CT) scan showed fat stranding around the pancreas suggesting pancreatitis (Figure 1). Blood urea nitrogen and hematocrit levels were normal with values of 18 mg/dl and 43.9%, respectively. Accordingly, the patient was diagnosed with ERCP-induced pancreatitis.
Figure 1.
Abdominal CT scan shows peripancreatic fat stranding suggestive of pancreatitis.
The patient received medical management for pain, was given intravenous fluids, and kept from food or drink intake for bowel rest until he could tolerate oral intake. He began to develop severe hypocalcemia, mild hypomagnesemia, and severe hypophosphatemia with levels reaching 5.6 mg/dl, 1.5 mg/dl, and 0.9 mg/dl, respectively. Thus, oral and intravenous supplementation were initiated. An abdominal CT scan performed on day two showed acute pancreatitis with development of peripancreatic collection measuring approximately 8 cm anteroposterior, 11.7 cm transverse, and 4.5 cm craniocaudal interposed between the pancreas and stomach (Figure 2).
Figure 2.
Abdominal CT scan shows pancreatitis and newly forming peripancreatic fluid.
When 40 mmol of intravenous sodium phosphate was initiated at a rate of 250 ml/hour, the patient experienced pressure-like substernal chest pain and worsened tachycardia reaching 127 bpm, which did not resolve until intravenous infusion was stopped. An electrocardiogram showed sinus tachycardia and nonspecific ST and T wave changes (Figure 3). Troponin I levels were elevated, reaching 0.71 ng/ml. Chest x-ray showed moderate left and mild right pleural effusion. Calcium level was 6.9 mg/dl.
Figure 3.
Electrocardiogram shows sinus tachycardia and ST and T wave changes.
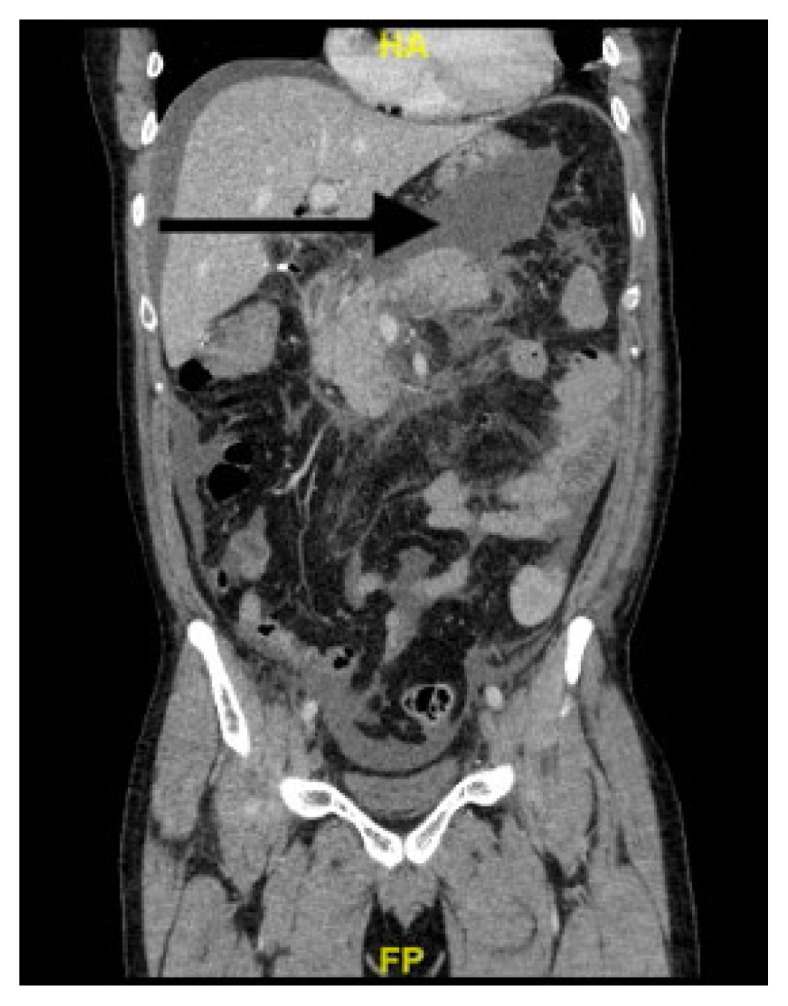
The patient’s angina in the presence of elevated cardiac enzymes prompted treatment with aspirin, 324 mg, and intravenous heparin drip. Troponin trended down afterwards, reaching 0.09 ng/mL. A repeat abdominal CT scan (Figure 4) showed increased peripancreatic and mesenteric inflammatory changes concerning for worsening pancreatitis, no evidence of pancreatic necrosis, and a peripancreatic fluid collection superior to the pancreas extending from the head/proximal body into the left upper quadrant measuring 16.7 x 6.9 x 11.3 cm.
Figure 4.
Abdominal CT scan shows pancreatitis and expanding peripancreatic fluid collection.
The hospital course continued without cardiac disease manifestation and electrolytes were replenished. Intravenous potassium phosphate was infused at a slower rate of 187.5 ml/hour to supplement phosphate without causing side effects, which may have been attributed to the phosphate infusion. Chest pain resolved soon after the initiation of treatment and was discharged home safely. The patient remained asymptomatic afterwards, but required further follow-up on complications secondary to his pancreatitis.
Echocardiogram performed one month later showed no myocardial wall abnormality, ejection fraction of 60–65%, and no pericardial effusion.
DISCUSSION
Acute pancreatitis is a very common gastrointestinal disease and can present with varying severity spanning from a mild disease requiring conservative management to severe disease associated with a worse prognosis.3 Management of acute pancreatitis includes early aggressive fluid resuscitation and pain management.4
The pathophysiology of acute pancreatitis includes activation of trypsinogen into trypsin within the acinar cells upon increased ductal pressures and adenosine triphosphate depletion resulting in increased intra-acinar calcium concentration which activates zymogens.5,6 This leads to the destruction of pancreatic parenchyma and the release of Damage Associated Molecular Patterns (DAMPs) that activate neutrophils and trigger the inflammatory cascade responsible for the systemic manifestation of acute pancreatitis. As a result, increased capillary permeability and damage of the endothelium results along with microvascular thrombosis that leads to multiorgan dysfunction syndrome (MODS).
Electrolyte abnormalities associated with pancreatitis include hypocalcemia and hypomagnesemia. The pathophysiology is not clear but suggested to be secondary to pancreatic enzymes digesting peripancreatic fat, and thus releasing fatty acids that bind free calcium.7,8 However, severe hypophosphatemia (< 1 mg/dl) in acute pancreatitis rarely was mentioned in the literature, and when it was, it often was attributed to alcohol in alcohol-induced pancreatitis.9 Intravenous supplementation of phosphate in critically ill patients has been documented to be safe and efficacious.10 In general, causes of hypophosphatemia were inadequate phosphate intake, extracellular to intracellular space phosphate shift, and increased phosphate excretion.11 Severe hypophosphatemia rarely was mentioned in acute pancreatitis, and its management is not explained in this context.
Side effects of intravenous phosphate supplementation are limited to confusion, weakness, lightheadedness, nausea, chest pain, irregular cardiac rhythm, numbness or tingling in extremities, weakness, decreased heart rate, weak pulse, or decreased respiratory rate.12 It can result in hypocalcemia as the infused phosphate binds the free calcium.10 This can precipitate vasospasms or arrhythmias leading to decreased blood supply to the cardiac muscle and precipitate anginal symptoms.13
We speculate that the angina that our patient experienced might have been precipitated by decreased cardiac blood and oxygen supply secondary to phosphate supplementation directly or due to iatrogenic transient hypocalcemia and resulting in hypotension or transient arrhythmia. Guidelines for the assessment of acute chest pain recently were published to guide management of similar episodes.1 Another study suggested several biomarkers to differentiate between type I myocardial infarction, type II myocardial infarction, and myocardial injury.14 This can lead to more accurate diagnoses and understanding of the underlying pathophysiology of cardiac chest pain in the future. Further studies also are needed to assess the mechanism and guide treatment of severe hypophosphatemia in patients with acute severe pancreatitis.
Limitations of our case report included the absence of a troponin level prior to the chest pain incident, which did not provide an accurate temporal relationship between enzyme elevation and the chest pain.
REFERENCES
- 1.Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/ SAEM/SCCT/ SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: Executive Summary: A Report of the American College of Cardiology/ American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):2218–2261. doi: 10.1016/j.jacc.2021.07.052. [DOI] [PubMed] [Google Scholar]
- 2.Balla C, Pavasini R, Ferrari R. Treatment of angina: Where are we? Cardiology. 2018;140(1):52–67. doi: 10.1159/000487936. [DOI] [PubMed] [Google Scholar]
- 3.Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis--2012: Revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–111. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- 4.Crockett SD, Wani S, Gardner TB, FalckYtter Y, Barkun AN American Gastroenterological Association Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology. 2018;154(4):1096–1101. doi: 10.1053/j.gastro.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 5.Tyberg A, Karia K, Gabr M, et al. Management of pancreatic fluid collections: A comprehensive review of the literature. World J Gastroenterol. 2016;22(7):2256–2270. doi: 10.3748/wjg.v22.i7.2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Constantinoiu S, Cochior D. Severe acute pancreatitis - Determinant factors and current therapeutic conduct. Chirurgia (Bucur) 2018;113(3):385–390. doi: 10.21614/chirurgia.113.3.385. [DOI] [PubMed] [Google Scholar]
- 7.Condon JR, Ives D, Knight MJ, Day J. The aetiology of hypocalcaemia in acute pancreatitis. Br J Surg. 1975;62(2):115–118. doi: 10.1002/bjs.1800620209. [DOI] [PubMed] [Google Scholar]
- 8.McMahon MJ, Woodhead JS, Hayward RD. The nature of hypocalcaemia in acute pancreatitis. Br J Surg. 1978;65(3):216–218. doi: 10.1002/bjs.1800650323. [DOI] [PubMed] [Google Scholar]
- 9.Farooq A, Richman CM, Swain SM, Shahid RA, Vigna SR, Liddle RA. The role of phosphate in alcohol-induced experimental pancreatitis. Gastroenterology. 2021;161(3):982–995e2. doi: 10.1053/j.gastro.2021.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perreault MM, Ostrop NJ, Tierney MG. Efficacy and safety of intravenous phosphate replacement in critically ill patients. Ann Pharmacother. 2016;31(6):683–688. doi: 10.1177/106002809703100603. [DOI] [PubMed] [Google Scholar]
- 11.Reilly RF. Disorders of Phosphorus Balance: Hyperphosphatemia and Hypophosphatemia. In: Lerma EV, Rosner MH, Perazella MA, editors. CURRENT Diagnosis & Treatment: Nephrology & Hypertension. 2e. McGraw Hill; 2017. [Accessed September 16, 2021]. https://accessmedicine.mhmedical.com/Content.aspx?bookid=2287§ionid=177426857 . [Google Scholar]
- 12.Drugs.com. Potassium phosphate. [Accessed August 29, 2021]. https://www.drugs.com/mtm/potassium-phosphate.html .
- 13.Singh A, Museedi AS, Grossman SA. StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Acute coronary syndrome July 19, 2021. [PubMed] [Google Scholar]
- 14.Neumann JT, Weimann J, Sörensen NA, et al. A biomarker model to distinguish types of myocardial infarction and injury. J Am Coll Cardiol. 2021;78(8):781–790. doi: 10.1016/j.jacc.2021.06.027. [DOI] [PubMed] [Google Scholar]





