Abstract
Objective:
Childhood attention-deficit/hyperactivity disorder (ADHD) is associated with substantial burden to caregiver quality of life (QoL). However, a paucity of work has focused on quantifying QoL among caregivers of adolescents with a history of ADHD. The purpose of the current study was (1) to quantify maternal quality of life (QoL) in a sample of mothers of adolescents with (N = 110) and without childhood ADHD (N = 90); and (2) to examine predictors (i.e., parent and child characteristics and behavior) associated with reductions in maternal QoL.
Method:
Participants included mothers of adolescents with and without childhood ADHD (Mean Age = 16.09, 91.5% male). The Quality Adjusted Life-Year (QALY) approach was used to calculate maternal health-related QoL. QALYs are valued monetarily to conduct cost-benefit and cost-effectiveness analyses.
Results:
Mothers of adolescents with childhood ADHD experienced significantly worse QoL relative to mothers in the comparison group. Maternal depression, as well as adolescent age, ADHD status, and discipline problems significantly predicted reductions in maternal QALY scores, with ADHD being the strongest predictor. This is equal to a reduction in 1.96 QALYs when summed over the course of a child’s lifetime and is associated with a loss of $98,000 to $196,000.
Conclusions:
The results of the investigation help to further elucidate the health impacts incurred by families of adolescents with ADHD and have important public health implications. Further, parental QoL should be considered when conceptualizing the financial and negative health impact of ADHD.
Keywords: Attention-Deficit/Hyperactivity Disorder, caregiver, quality of life, adolescence
Raising a child with attention-deficit/hyperactivity disorder (ADHD) is associated with substantial burden to caregiver quality of life (QoL; Bussing et al., 2003; Hakkaart-van Roijen et al., 2007; Johnston & Chronis-Tuscano, 2015; Pelham et al., 2007). Mothers continue to fill the role of primary caregiver for a majority of youth (U.S. Bureau of the Census, 2017) and therefore often bear the responsibility of initiating and maintaining treatment for their child, advocating for their child at school, and managing challenging behaviors at home. As a result, mothers often incur financial costs, such as increased medical spending (Matza et al., 2005), as well as personal costs, such as marital difficulty, depression, work loss and financial strain related to their child’s ADHD and related academic, behavioral, and social difficulties (Johnston & Chronis-Tuscano, 2015; Wymbs et al., 2008; Zhao et al., 2019). The cumulative toll associated with raising a child with ADHD presents substantial long-term risk for families, as caregiver burden to QoL is associated with poor child treatment outcomes as well as long-term negative mental and physical health consequences for families (Brannan et al., 2003; Pellerin et al., 2010).
To date, research examining caregiver and maternal QoL has focused primarily on school-aged children with ADHD (Andrade et al., 2016; Avrech Bar et al., 2018; Cappe et al., 2017; Lange et al., 2005; Xiang et al., 2009; Zare et al., 2017), with no studies quantifying QoL in caregivers of adolescents specifically. Trends in research involving younger children have revealed significantly lower QoL in caregivers of children with compared to without ADHD. Given that ADHD and its functional sequelae persist into adolescence for the majority of youth (Kent et al., 2011; Sibley et al., 2012), many of the same burdens identified among caregivers of children with ADHD likely continue to be relevant for caregivers of adolescents with ADHD. In addition, caregivers appear to experience continued or worsening emotional distress as their children age into adolescence (Babinski et al., 2016, 2020; Wiener et al., 2016). This may be exacerbated by physiological and neurobiological changes associated with puberty, increases in responsibility, and decreased academic motivation associated with the adolescent developmental period (Smith et al., 2020; Smith & Langberg, 2018; Steinberg et al., 2014). Mothers, in particular, continue to be critical in promoting positive youth outcomes for adolescents with ADHD (Gordon & Hinshaw, 2017), yet poor QoL may impede mothers’ capacity to perform normative parenting duties into adolescence and adulthood, such as developmentally appropriate monitoring of offspring behavior and seeking or facilitating treatment for their adolescent with ADHD. Therefore, examining maternal QoL is important in understanding and improving long-term outcomes for youth with ADHD and their families.
Existing work examining the burden of ADHD to caregiver functioning has primarily focused on caregiver stress (Craig et al., 2016; Theule et al., 2013) and strain (Babinski et al., 2020), as well as parent psychological symptoms (e.g., depression, anxiety, and ADHD; Cheung et al., 2016, 2018), rather than QoL specifically. QoL is a broad, holistic, and multidimensional measure of health-related functioning (Meyer et al., 2016), such that measured yearly impact to lifetime QoL can be used to understand the summative effects of caring for a child with ADHD from early childhood through adolescence.
One method of quantifying QoL is to calculate the Quality Adjusted Life-Year (QALY), an internationally recognized concept and widely used health outcome and utility measurement implemented in health economics and policy research (Drummond et al., 2015; Lipscomb et al., 2009; Ryen & Svennson, 2015). QALYs are typically used to evaluate health states by regulatory agencies that impact public health decision making and resource allocation (Sassi, 2006). QALYs represent a health outcome measure incorporating both quantity (time) and quality of life (Lipscomb et al., 2009; Torrance, 1986; Whitehead & Ali, 2010) with consideration for disruption across various dimensions of health-related functioning (e.g., pain/discomfort, anxiety/depression, mobility, self-care, and ability to carry out usual daily activities; Herdman et al., 2011). QALYs can be derived from a number of multi-attribute, health-related functioning measures (Scufham et al., 2008), with one of the most commonly used measures being the EQ-5D-5L (Whitehead & Ali, 2010). QALYs have been utilized in previous work to estimate disease burden in mental health problems in adults such as depression (e.g., Jia & Lubetkin, 2017), chronic physical health conditions (e.g., Jia et al., 2018), and other public health concerns, such as child maltreatment (Corso et al., 2008; Letourneau et al., 2018). To our knowledge QALY estimates have yet to be applied to caregiver QoL for families of children and adolescents with ADHD, which is an important concept for estimating the public health impact associated with raising youth with ADHD.
Additionally, QALYs can be employed to assess change in QoL or estimate cost-of-illness (Drummond & Sculpher, 2005), which facilitates an estimate of disease burden that is comparable to other chronic health conditions. For example, QALYs are associated with a monetary value (e.g., $50,000 to $100,000 USD) to indicate a financial loss associated with each incremental reduction in QALYs (Ryen & Svensson, 2015). QALYs can then be summed to estimate a lifetime cost (Hirth et al., 2000). Measuring the impact of ADHD on caregiver functioning in this way provides a health status index and cost-utility estimate from a public health perspective, as well as provides a societal cost that can be compared to many other chronic health conditions. To date, we are unaware of any attempts to provide a health status index and cost-utility estimate for ADHD and externalizing behavior disorders.
Predictors of Maternal QoL
Due to the lack of research focused on understanding QoL in mothers of adolescents with ADHD histories, it is unclear which maternal and adolescent factors implicated in the caregiver distress literature affect maternal QoL. Prior work has identified several factors associated with immediate and lifetime caregiver burden that may also influence overall QoL. These potentially explanatory factors include maternal characteristics (e.g., educational attainment, age, divorce history, psychopathology; DuPaul & Langberg, 2015; Johnston & Chronis-Tuscano, 2015; Schermerhorn et al., 2012; Theule et al., 2013; Wymbs et al., 2008), as well as adolescent characteristics and behavior (e.g., ADHD status, co-morbid oppositional behavior, school behavior and academic difficulties; Babinski et al., 2020; Fridman et al., 2017).
Maternal Predictors.
Evidence suggests that mothers of children with ADHD may experience lower educational attainment compared to mothers of children without ADHD (DuPaul & Langberg, 2015). Academic underachievement may reduce employment prospects and increase financial burden, in turn negatively affecting maternal QoL outcomes. Overall, the literature examining maternal education and socioeconomic status in relation to caregiver burden in families with ADHD is mixed with some studies finding an association between financial strain and caregiver outcomes (Baker, 1994; Baldwin, 1995) and others finding these factors to be unrelated (Harrison & Sofronoff, 2002; Theule et al., 2011). Further, there is heterogeneity in the association between educational attainment and various health outcomes in the broader QoL literature (for review see Hamad et al., 2018). Given these mixed findings it is unclear whether raising an adolescent with ADHD is associated with lower maternal QoL beyond what may be expected for maternal education and SES.
Moreover, parents of youth with ADHD experience marital conflict and divorce at higher rates than parents of youth without ADHD (Johnston & Chronis-Tuscano, 2015; Schermerhorn et al., 2012; Wymbs et al., 2008). In a large sample drawn from the Australian Twin Registry, researchers found that the presence of childhood ADHD predicted marital problems even when controlling for genetic and shared environmental factors (Schermerhorn et al., 2012), suggesting a strong link between childhood ADHD and marital conflict. Strain associated with increased family conflict, financial burden due to single-parenthood, and related health impairment is likely to be associated with lower QoL. To date, no studies have directly compared the differential contributions of divorce and adolescent ADHD history on maternal QoL.
Approximately half of mothers of youth with ADHD have a depression history (Johnston & Chronis-Tuscano, 2015; Theule et al., 2013), with roughly 17% meeting criteria for a depressive disorder (Theule et al., 2013). Maternal depression is in turn associated with a host of negative outcomes that may compromise overall QoL, such as increased family conflict (Foster et al., 2008), higher rates of child behavior problems and psychopathology (Dette-Hagenmeyer & Reichle, 2014), caregiver strain (Johnston & Chronis-Tuscano, 2015; Theule et al., 2013), and negative health outcomes (Kiecolt-Glaser, 2018). A recent meta-analysis revealed that maternal depressive symptoms are moderately associated with child ADHD symptoms, as the strength of this relation varies across studies (Cheung et al., 2018). Further research is necessary to disentangle the relation between maternal depression and QoL for mothers of adolescents with ADHD histories.
Adolescent Predictors.
Several adolescent characteristics (i.e., childhood ADHD status, age) and behaviors (i.e., co-morbid oppositional and defiant behavior, school behavior problems, academic difficulties) have been identified as predictors of maternal QoL. There is a substantial body of evidence indicating that caregiver burden of youth with ADHD is maintained throughout the lifespan (Altszuler et al., 2016; Babinski et al., 2020; Hechtman et al., 2016; Kuriyan et al., 2013; Pelham et al., 2020; Sibley et al., 2012). Significant symptoms and functional impairment often persist into adulthood and are associated with increased caregiver strain (Babinski et al., 2020). For example, comorbid academic and conduct problems serve as a co-occurring stressor for parents during adolescence (Bussing et al., 2003; Johnston & Chronis-Tuscano, 2015; Kuriyan et al., 2013; Sibley et al., 2012; Wiener et al., 2016).
Current Study
To our knowledge, this is the first study to quantify lifetime QoL in mothers of adolescents with and without ADHD histories to better elucidate the burden associated with raising youth with ADHD. By utilizing QALY estimates, we were able to calculate an estimate of disease burden to understand how being a caregiver of an adolescent with an ADHD history compares to other chronic health conditions. Additionally, we sought to identify risk factors associated with lower QoL that can inform intervention targets for treatment focused on supporting maternal health functioning. Consistent with work examining QoL in mothers of school-aged children (e.g., Andrade et al., 2016; Avrech Bar et al., 2018; Cappe et al., 2017), it was hypothesized that mothers of adolescents in the ADHD group would demonstrate significantly lower QoL compared to the non-ADHD group. Additionally, it was expected that higher educational attainment would be related to higher QoL and that divorce or separation history, maternal depression, ADHD group status, behavior problems, and academic difficulties would be related to lower rates of maternal QoL.
Method
Participants
Data were gathered from mothers of adolescents with and without childhood ADHD participating in the Pittsburgh ADHD Longitudinal Study (PALS; Faden et al., 2004; Molina et al., 2007). The study was approved by the University of Pittsburgh Institutional Review Board. Informed consent was obtained for all PALS participants (i.e., parents and adolescents) during their enrollment. All participants were assured confidentiality of all disclosed material, except in cases of impending danger or harm to self or others (reinforced with a Department of Health and Human Services Certificate of Confidentiality). After the initial PALS consent was obtained, consent was repeated at each wave of data collection whenever there was a change to the assessment protocol or when new measures were added.
ADHD Group.
Adolescents in the ADHD group were recruited from a pool of 516 individuals who were diagnosed with ADHD in childhood and treated at the Summer Treatment Program (STP) at Western Psychiatric Institute and Clinic in Pittsburgh, PA between 1987 and 1996. The average age at the initial evaluation was 9.40 years old (SD = 2.27, range = 5.0–16.92) and 90% fell between ages 5 and 12. Of the 516 potential participants, 493 were re-contacted an average of 8.35 years (SD = 2.79) after their initial evaluation and 364 (71%) enrolled in the PALS. Participants were compared with nonparticipants on many demographic (i.e., age at first treatment, race, parental education level and marital status) and diagnostic (i.e., parent and teacher ratings of ADHD symptomology) variables. Of the 14 comparisons, the only significant (p < .05) difference was that conduct disorder (CD) symptoms, as indicated by composite parent and teacher ratings, were slightly higher for nonparticipants (M = 0.53 on a 4-point scale) compared to participants (M = 0.43).
Initial diagnostic information was collected according to the gold-standard assessment procedures current at the time (Pelham et al., 2005), such that information was collected from multiple sources. Parents and teachers completed the Disruptive Behavior Disorders Rating Scale (DBD; Pelham et al., 1992) to assess symptoms of ADHD, oppositional defiant disorder (ODD), and CD. Parents were also administered a semi-structured clinical interview by a Ph.D. level clinician to assess for DSM symptoms as well as situational and severity factors (instrument available at http://ccf.fiu.edu). Using DSM guidelines, diagnoses were made if either parents or teachers endorsed a sufficient number of symptoms. Two Ph.D. level clinicians reviewed ratings and interviews independently to confirm diagnoses. If disagreement occurred, a third clinician reviewed the file, and the majority decision was used. Children were excluded from participation in the STP if their estimated full-scale IQ fell below 80, and if they had a history of seizures or other instances of impending danger or harm to self or others.
ADHD group participants were admitted to the study on a rolling basis from 1999 to 2003 and the initial follow-up interview (i.e., Wave 1) was completed immediately upon enrollment. At the first Wave 1, participants ranged in age from 11 to 28, with 99% of participants falling between 11 and 25 years old. Follow-up interviews in adolescence and young adulthood were conducted by research staff. Questionnaires (paper and pencil or web-based) were completed by participants and their parents. In cases where distance prevented travel to the clinic, mail and telephone correspondence were used, with home visits, as necessary. At the time of enrollment in the PALS study, participants in the ADHD group also provided consent to utilize data collected from their participation in the STP.
Comparison Group.
A total of 240 demographically similar adolescents without ADHD were recruited on a rolling basis from 1999 to 2001 to participate in the annual PALS interviews. Comparison recruitment lagged behind the ADHD group recruitment in order to facilitate efforts to obtain a demographically similar sample (discussed below). Comparison participants were recruited from several sources in the greater Pittsburgh area, including medical records from pediatric practices in Allegheny County (41%), advertisements in local newspapers (28%), local universities and colleges (21%), and other methods (11%), such as word-of-mouth and local public schools. A telephone screening interview was administered to parents to gather basic demographic information, history of diagnosis and/or treatment for ADHD and other behavior problems, the presence of exclusionary criteria as listed for the ADHD group, and a checklist of ADHD symptoms. Participants who met Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R or DSM-IV) criteria for ADHD, either currently or historically, were excluded from the study. If a potential comparison participant passed the initial telephone screen, senior research staff met to determine study eligibility based on five demographic variables: 1) age, 2) race, 3) gender, 4) parental education level, and 5) marital status. A participant was considered appropriate for the study if their enrollment maintained the demographic similarity of the comparison group to that of the ADHD group. Resulting ADHD/non-ADHD groups were similar on all but marital status (fewer married in the ADHD group). Once recruited, all participants were interviewed annually until age 23 when subsequent assessments were spread out into less frequent age-specific interviews (Molina et al., 2017)
Current Study.
The current study used data from the childhood assessments conducted with the ADHD group and the annual Wave 3 follow-up interviews conducted with both the ADHD and comparison groups. Participants were the mothers of PALS participants who were 18 years old or younger (M = 16.09 years, SD = 1.50, range: 13 to 18 years) at the time of the Wave 3 interview, when a key measure for the current study (the Caregiver Strain Questionnaire, see below) was added. This sampling resulted in 200 participants (110 mothers of ADHD participants; 90 mothers of comparison participants), described in Table 1, whose Wave 3 interviews took place between 2001 and 2004.
Table 1.
Demographic Variables
| ADHD (n = 110) |
Comparison (n = 90) |
X2 or F | df | Effect Size | |
|---|---|---|---|---|---|
| Mother Characteristics | |||||
|
| |||||
| Age M (SD) | 45.20 (7.53) | 46.49 (5.34) | 1.86 | 1,197 | 0.01a |
| Race (%) | 3 | 0.08c | |||
| White | 87 | 86 | 0.40 | ||
| Black or African American | 11 | 10 | 0.14 | ||
| Two or more races | 1 | 2 | 0.52 | ||
| Other | 1 | 2 | 0.52 | ||
| Education Level (%) | 4.45* | 1,197 | 0.02a | ||
| High school diploma or GED | 9 | 12 | 0.21 | ||
| Technical or specialized training | 16 | 11 | 0.89 | ||
| Some college | 22 | 11 | 4.26* | ||
| Associate’s/2-year degree | 15 | 8 | 2.37 | ||
| College/University degree | 19 | 23 | 0.44 | ||
| Graduate degree | 18 | 34 | 7.39** | ||
| Marital Status (%) | 8.22* | 3 | 0.20c | ||
| Single, never married | 8 | 3 | 2.11 | ||
| Married or living with partner | 65 | 82 | 7.28** | ||
| Separated or divorced | 25 | 14 | 3.27 | ||
| Widowed | 2 | 0 | 1.67 | ||
|
| |||||
| Adolescent Characteristics | |||||
|
| |||||
| Age M (SD) | 16.14 (1.49) | 16.03 (1.52) | 0.23 | 1,199 | 0.00a |
| Gender (% Male) | 91 | 92 | 0.11 | 1 | 0.02b |
| Race (%) | 3 | 0.08c | |||
| White | 79 | 82 | 0.31 | ||
| Black or African American | 8 | 9 | 0.03 | ||
| Two or more races | 10 | 6 | 1.33 | ||
| Other | 3 | 3 | 0.06 | ||
| Baseline Full-Scale IQ M (SD) | 100.60 (18.02) | 109.20 (15.18) | 12.93*** | 1, 198 | 0.06a |
Note. Chi-square tests were conducted for categorical variables and ANOVAs were conducted for continuous variables
p < .001
p <.01
p < .05
= η2
= ϕ
= V.
Measures
Quality of Life.
In the current study, mother-reported data from the Caregiver Strain Questionnaire (CGSQ; Brannan et al., 1997) was used to estimate health-related QoL on domains consistent with the broader health economics literature. The CGSQ is a 21-item self-report questionnaire that assesses the impact of caring for a child with emotional and/or behavioral difficulties on three dimensions of strain: objective strain (e.g., disruption of activities), subjective externalized strain (e.g., becoming angry or embarrassed due to child’s problems), and subjective internalized strain (e.g., anxiety or depression due to child’s problems). The CGSQ has demonstrated strong psychometric properties and is correlated with measures of family functioning and parent psychopathology (Brannan et al., 1997),. The CGSQ demonstrated high internal consistency within the current sample (α = 0.97). The CGSQ was administered for the first time in Wave 3 of the PALS and mothers were asked to rate strain over their child’s lifetime using a 1 (not at all) to 5 (very much) scale. The current study only used data from the objective strain and subjective internalized strain subscales, as these subscales map on best to the EQ-5D-5L (Herdman et al., 2011), a well-established and most common measure of health-related QoL (Janssen et al., 2013; Craig & Rand, 2018). The objective strain subscale consists of 11 items that measure how much child emotional/behavioral problems disrupt family routines, activities, and relationships (α = 0.96). A sample item from the objective strain subscale is, “How much of a problem was you missing work or neglecting other duties because of your child’s emotional or behavioral problem?” The subjective internalized strain subscale consists of 6 items assessing mothers’ sadness and worry due to their child’s problems (α = 0.92). A sample item from the subjective internalized strain subscale includes, “How tired or strained did you feel as a result of your child’s emotional or behavioral problem?”
QALY is derived from measures of individual’s health according to five dimensions: mobility (walking about), self-care (washing or dressing), usual activities (e.g., work, study, housework, family, or leisure activities), pain/discomfort, and anxiety/depression. Each dimension is rated on a 1 (none) to 5 (extreme) scale and responses are combined to form a 5-digit health profile, with 11111 representing a perfect health-state. Means from the mother-reported CGSQ objective strain and subjective internalized strain scales were used to assign scores on the usual activities and anxiety/depression dimensions, respectively. All other dimensions were assigned a score of 1, indicating no problem in those domains, as having a child with ADHD would not be expected to directly impact those areas. These scores were used to develop health-states for the mothers of youth with and without an ADHD history (Figure 1). Using national norms, health-states were then converted to QALYs where 1.0 represents one year of perfect health (Van Hout et al., 2012). QALYs ranged from 0.52 to 1.0 (M = 0.82, SD = 0.15) in the current sample.
Figure 1.
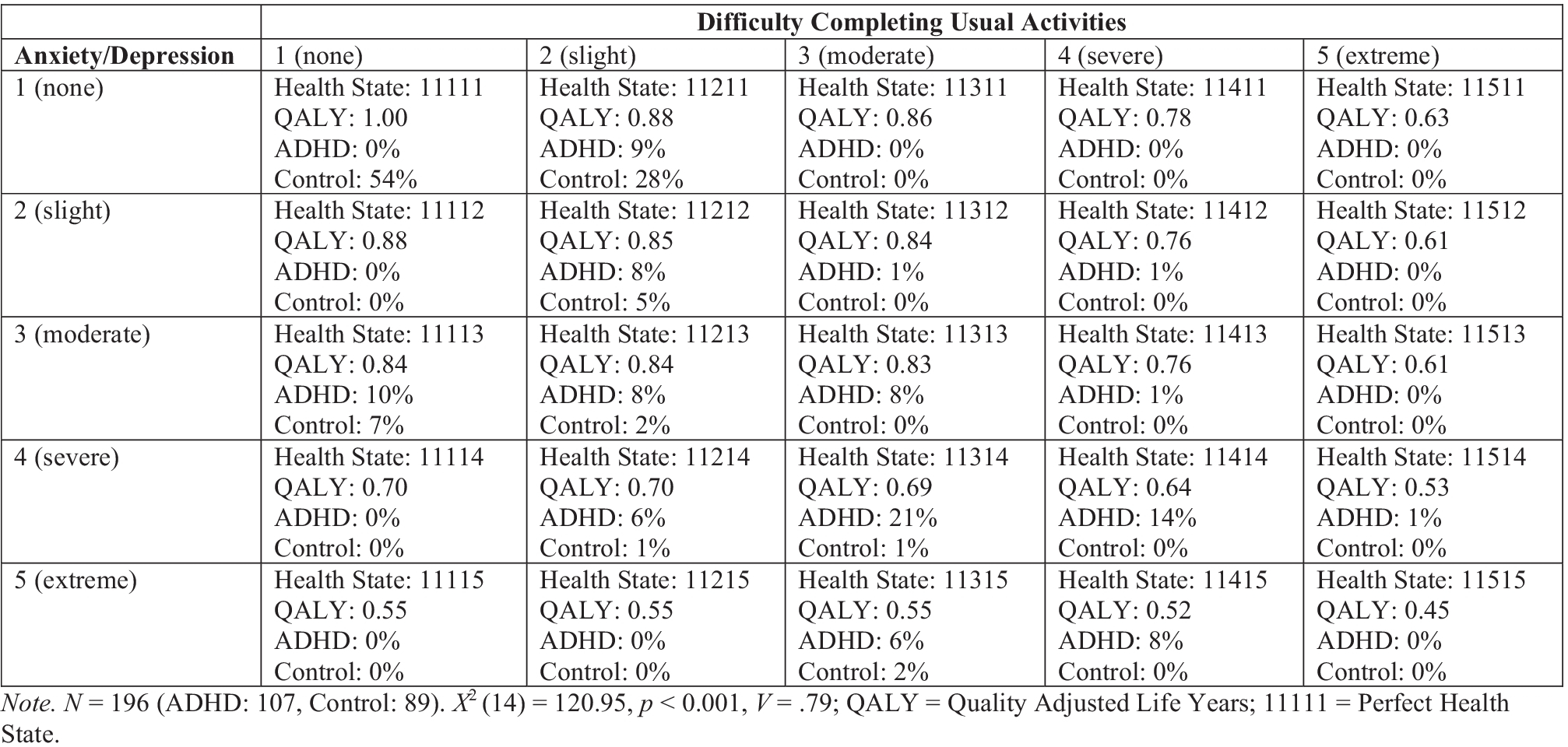
Maternal Health-States
Predictors of Health-Related QoL.
Demographic Information.
Participants and their offspring completed an annual demographic questionnaire developed for this study. Participants were asked about their age, educational attainment, and marital status. In the current study, the highest level of education achieved by participating mothers was assessed at Wave 3. For purposes of our analyses, higher scores are associated with higher levels of educational achievement. A divorce history variable was created from data provided on the yearly demographic questionnaire. Mothers who had ever reported being divorced were assigned a 1 and mothers who never reported being divorced were assigned a 0.
Maternal Depression.
At Wave 2, mothers self-reported depression symptoms on the Center for Epidemiological Studies Depression Scale (CES-D; Radloff, 1977). The CES-D consists of 20 items, scored from 0 (rarely or none of the time) to 3 (most or all of the time). Scores range from 0 to 60 with a recommended clinical cut-off of 16 (Radloff, 1977). The CES-D has demonstrated excellent validity and reliability in past studies and demonstrated high internal consistency in the current sample (α = 0.93).
Adolescent Cognitive Functioning.
An intelligence screener was administered at Wave 1. For those younger than age 17 at Wave 1, an estimate of Intelligence Quotient (IQ) was calculated from the vocabulary and block design subtests of the Wechsler Intelligence Scale for Children-III (WISC-III; Wechsler, 1991). For those age 17 and older, an estimate of IQ was calculated using the same subtests of the Wechsler Adult Intelligence Scale-Revised (WAIS-R; Wechsler, 1981).
Adolescent Academic Problems:
A summary variable reflecting total academic problems over the course of a child’s schooling was created using data from the Education History Questionnaire (EHQ). The EHQ is a 38-item measure that was developed for PALS based on measures used in the Pittsburgh Adolescent Alcohol Research Center and Center for Education and Drug Abuse Research studies in which parents and participants reported on schools attended, classroom placement, special education services, and school discipline problems. At the first follow-up visit (Wave 1), parents and participants provided retrospective reports for each year from kindergarten through the participant’s current grade at Wave 1. Academic problems included placement in remedial classes, academic probation, grade retention, and failing courses (failed courses were only assessed for grades 7–12). A summary variable was used to minimize multicollinearity (Kuriyan et al., 2013). Academic problems from kindergarten through grade 12 were totaled for each problem and then divided by the number of data points available for that problem. For example, if a participant reported being placed in remedial classes five times from kindergarten through grade 10, the proportion score was calculated as 5/11 = 0.45. Proportions for each problem were then summed to create a yearly index of academic problems.
Adolescent Discipline Problems:
A summary discipline problems variable was calculated using data from the EHQ, including expulsions, out-of-school suspensions, in-school suspensions, verbal and written warnings, and being sent to the principal’s office. A summary proportion variable was calculated in the same way as was done for academic problems. The proportion score was recoded into four categories due to a non-normal distribution of the proportional data that included extreme outliers (Kuriyan et al., 2013). Yearly rate of disciplinary actions was coded as 0 (up to one disciplinary action, lifetime) for 0 – 0.10 disciplinary actions per year, 1 (up to one disciplinary action per year) for 0.11 – 1.0 actions, 2 (more than one to five disciplinary actions per year) for 1.1 – 5.0 actions, and 3 (more than five disciplinary actions per year) for 5.1 or more actions. The distribution of this variable is as follows: category 0 (ADHD: 6%, Comparison: 34%), category 1 (ADHD: 16%, Comparison: 41%), category 2 (ADHD: 36%, Comparison: 20%), and category 3 (ADHD: 43%, Comparison: 4%).
Data Analytic Plan and Handling of Missing Data
Analyses were conducted in SPSS 19.0. Overall, 1% of values were missing. Data were determined to be missing completely at random (MCAR) using Little’s MCAR test (Little, 1988), χ2 (33) = 29.67, p = .63 and list-wise deletion was therefore used. To examine group differences in maternal QoL, a chi-square was conducted on EQ-5D-5L health states. An ANCOVA was conducted on maternal QALY estimates to examine the impact of childhood ADHD status on maternal QoL while controlling for maternal education attainment, maternal divorce history, and adolescent IQ. Next, predictors of maternal QALYs were evaluated using linear regression models. Predictors included maternal characteristics: age at Wave 3 visit, depression, divorce history, and education level; adolescent characteristics: full-scale IQ at baseline, age at Wave 3 visit; and adolescent behaviors: ADHD diagnosis, academic problems, and discipline problems. Multicollinearity of predictors and covariates was assessed; variance inflation factor scores were all less than 1.99 and tolerance statistics were above 0.5, minimizing concern for multicollinearity. Predictor analyses were conducted in three steps: maternal characteristics, adolescent characteristics, and adolescent behaviors.
Often in health economics research, improvements in QALYs are valued monetarily to conduct cost-benefit and cost-effectiveness analyses. A treatment or intervention would be considered cost-effective and acceptable from a societal perspective if it could produce an additional QALY for less than an assumed threshold value (Johannesson, 1995; Kaplan & Bush, 1982). Traditionally, a threshold value of $50,000 was assumed for each QALY; however, to account for inflation and rising costs of healthcare, a $100,000 threshold value is now commonly assumed (Neumann et al., 2014). Using this concept, the difference in QALYs between the ADHD and control group were summed over the life of the child, from age 5 (when ADHD is commonly first diagnosed; Applegate et al., 1997) through age 18. This approach has been utilized in other work estimating QALYs over time (e.g., Letourneau et al., 2018; Whang et al., 2022). This summation yielded the total number of maternal QALYs lost due to the presence of ADHD. To obtain a range of estimated economic value of these lost QALYs, both commonly used threshold values of $50,000 and $100,000 were applied to estimates obtained from the regression models controlling for other potential confounding characteristics.
Results
Preliminary Results
Prior to conducting the primary analyses, group differences on demographic and hypothesized predictor variables were examined. While the ADHD and comparison groups did not differ on racial/ethnic background or age, maternal education level was significantly different across the resulting ADHD (M = 3.70, SD = 1.61) and comparison groups (M = 4.22, SD = 1.80), where 3 = some college and 4 = Associate’s or 2-year degree, F (1, 197) = 4.55, p < .05, η2 = 0.02. Significantly more mothers in the ADHD group (45%) had a positive divorce history compared to mothers of comparisons (17%), χ2 (1) = 17.68, p < 0.001, ϕ = 0.30. The IQ score for the ADHD and comparison groups differed significantly, F (1, 198) = 12.93, p < 0.001. η2 = 0.06. As such, background characteristics including maternal education and divorce history, as well as adolescent IQ were included as covariates in the primary analyses.
Regarding predictor variables, significant differences between participant groups in adolescent discipline problems, adolescent academic problems, and maternal depression were identified. Participants in the ADHD (M = 2.17, SD = 0.89) and comparison (M = 0.94, SD = 0.85) groups differed significantly on adolescent discipline problems, χ2 (3) = 67.09, p < 0.001, V = 0.58. Participants in the ADHD group experienced significantly more academic problems (M = 0.45, SD = 0.56) relative to those in the comparison group (M = 0.04, SD = 0.15), F (1, 197) = 45.24, p < 0.001, η2 = 0.18. In terms of maternal depression, mothers of adolescents in the ADHD group (M = 12.40, SD = 9.97) and mothers of comparison participants (M = 8.28, SD = 8.94), F (1, 188) = 8.86, p = 0.003, differed significantly. η2 = 0.04.
Group Differences in Maternal QoL
As displayed in Figure 1, mothers of adolescents in the ADHD group experienced significantly worse QoL relative to mothers in the comparison group, X2 (14) = 120.95, p < 0.001. The majority of mothers of comparison participants (87%) reported having no or slight disruption in QoL due to interference in usual activities and/or anxiety/depression, and over half of these mothers were categorized as having perfect health (11111). In contrast, no mothers of ADHD group participants were categorized as has having perfect health-states. Most of these mothers (83%) reported having moderate to severe disruption in QoL due to interference in usual activities and/or anxiety/depression. When controlling for covariates, mothers in the ADHD group also had significantly lower QALYs (M = 0.73, SD = 0.12) than did mothers in the comparison group (M = 0.93, SD = 0.10), F (1, 189) = 152.85, p <0.001, ηp2 = 0.45. Higher levels of maternal education were also significantly associated with lower QALYs, but this effect was much smaller, F (1, 189) = 4.25, p = 0.04, ηp 2 = 0.02.
Predictors of Maternal QoL
Results of predictor analyses are presented in Table 2. Controlling for all variables in the model, childhood ADHD status had the largest effect on maternal QALY, with a positive ADHD history significantly predicting lower QoL. History of adolescent discipline problems, but not academic problems, also significantly predicted lower maternal QoL. Adolescent age had a small but significant association with QALY, such that older age was related to lower QoL. With all variables in the model, the only maternal characteristic that remained significantly related to QALY was maternal depression, such that mothers with higher depressive symptoms reported poorer QoL. However, maternal education level remained marginally significant (p = 0.05), with higher education levels predicting lower QoL.
Table 2.
Predictors of Maternal Quality of Life
| B | SE B | t | β | 95% CI | |
|---|---|---|---|---|---|
| Mother Characteristics | |||||
| Highest Education Level | −0.00 | 0.00 | −1.96† | −0.10 | (−0.20, 0.00) |
| Age | −0.00 | 0.00 | −1.04 | −0.06 | (−0.00, 0.00) |
| Depression | −0.00 | 0.00 | −4.51*** | −0.23 | (−0.01, −0.00) |
| Divorce Historya | −0.01 | 0.02 | −0.65 | −0.03 | (−0.04, 0.02) |
| Adolescent Characteristics | |||||
| Age | −0.01 | 0.01 | −2.21* | −0.11 | (−0.02, −0.00) |
| IQ | <0.00 | <0.00 | −0.15 | 0.00 | (−0.00, 0.00) |
| Adolescent Behavior | |||||
| Academic Problems | −0.03 | 0.02 | −1.39 | −0.08 | (−0.06, 0.01) |
| Discipline Problems | −0.03 | 0.01 | −3.27** | −0.21 | (−0.05, −0.01) |
| ADHDb | −0.14 | 0.02 | −6.86*** | −0.47 | (−0.18, −0.10) |
Note. B = linear regression coefficient. Overall model: F (9, 173) = 27.44, p < .001, Adjusted R2 = .57
Positive divorce history = 1, Negative divorce history = 0
ADHD = 1, Comparison = 0
p < .001
p <.01
p < .05,
p < .10.
Estimated Cost of Disease Burden
Regression results suggest the presence of ADHD reduces maternal QoL by 0.14 (95% CI [−0.178, −0.098]) QALYs. Assuming this reduction in QALY is constant over time, summing this value from the child’s age 5 (when children are typically diagnosed with ADHD) to 18 yields a total reduction in QALYs of 1.96 over this period. Utilizing QALY values of $50,000 and $100,000 (Ryen & Svensson, 2015), the estimated value of these lost QALYs ranges from $98,000 to $196,000.
Discussion
The purpose of the present study was twofold: 1) estimate and compare lifetime maternal QoL in a sample of mothers of adolescents with and without ADHD histories and 2) examine predictors of lifetime maternal QoL. This paper represents the first study to measure life-time maternal QoL via QALYs and examine how maternal health states are related to caregiver and adolescent functioning. Use of QALYs to quantify QoL is consistent with public health and economic research in estimating disease burden that can be compared across other chronic health conditions and has important implications for informing public health priorities and resource allocation (Sassi et al., 2006; Torrance, 1986; Whitehead & Ali, 2010). Furthermore, the present study has important implications for further explicating the financial and health impacts incurred by families raising youth with ADHD.
As expected, results indicated that mothers of adolescents in the ADHD group experienced significantly lower QoL, compared to mothers of comparison participants with results indicating a large effect of ADHD (ηp2 = 0.45). This is consistent with prior work which has reliably identified increased difficulty in psychological, social, and financial functioning among families of youth with ADHD (Bussing et al., 2003; Hakkaart-van Roijen et al., 2007; Johnston & Chronis-Tuscano, 2015; Zhao et al., 2019). Additionally, findings align with research indicating reduced QoL in caregivers of school-aged children with ADHD compared to control samples (e.g., Lange et al., 2005).
In particular, the current study revealed that mothers in the ADHD group were more likely to report having moderate to severe disruption in health-related functioning, compared to 87% of the comparison group who reported little to no disruption. These results suggest a significant reduction in maternal QoL with the presence of ADHD with an estimated cost of illness ranging from $98,000 to $196,000 from childhood through adolescence. Taken together with prior research, the results of the current study indicate significant health and financial burden for families of youth with ADHD compared to those without. For example, a $400,000-$600,000 lifetime income loss for individuals with ADHD was estimated for participants in this sample using adulthood data (Pelham et al., 2020). Additionally, the individual household financial impact of ADHD is five times higher for families raising youth with ADHD compared to youth without ADHD (Zhao et al., 2019). The current data show that the overall economic impact of ADHD is likely substantially larger when caregiver QoL is included.
Secondly, we included several maternal and adolescent risk factors to determine their unique value in predicting maternal QoL. After controlling for all other variables in the model, childhood ADHD was found to be the strongest predictor of maternal QoL, in that the presence of ADHD was related to decreased maternal QoL. The strength of this relation is notable and underscores the importance of considering maternal functioning when conceptualizing the functional sequelae associated with ADHD in adolescence. Long-term maternal functioning is essential to the successful implementation of treatment to manage adolescent ADHD symptoms. As such, examining maternal QoL as an outcome and/or predictor of treatment (e.g., behavioral management training, medication) could help disentangle this transactional relationship and identify components of treatment that may help to prevent further impact on maternal QoL.
Among the predictors tested, adolescent discipline problems were also associated with worse QoL, suggesting that youth with ADHD and externalizing comorbidities (e.g., oppositionality, defiance) may similarly, increase negative health outcomes for mothers over the lifetime. Adolescent age had a small but significant association with maternal QALYs, such that older age was related to lower QoL. Given that prior work on caregiver QoL has largely focused on school-aged children, results of the current study emphasize the need to examine the functioning of caregivers of youth with ADHD across the child’s lifespan and into adulthood. Children with ADHD are more likely to be financially dependent on their families during adulthood (Pelham et al., 2020). Yet, the associated impact on caregiver QoL is unknown currently. Adolescents whose problems have the potential to become more concerning and costly with age (e.g., not graduating, legal problems, substance abuse, etc.), may place an additional burden to maternal QoL that is not captured in studies focusing exclusively on childhood.
In terms of maternal predictors, depression significantly predicted lifetime maternal QoL in our model, such that increased depressive symptoms were associated with significantly lower QALYs. Consistent with prior work (Cheung et al., 2018; Chronis et al., 2003a), mothers in the ADHD group demonstrated significantly higher levels of depression symptoms compared to controls. These findings highlight the importance of screening for maternal depression when working with families of youth with ADHD, as maternal depression is associated with a host of adverse developmental outcomes in children, such as increased conduct problems, depression, and suicide attempts (Chronis et al., 2007; Chronis-Tuscano et al., 2010; Wang et al., 2021). Mothers who experience significant depression symptoms and thereby have a lower QoL may be less likely to complete treatment or find certain aspects of treatment acceptable (Owens et al., 2003; Pellerin et al., 2010). Evidence-based interventions for children with ADHD that target maternal depression (e.g., Integrated Parenting Intervention for ADHD (IPI-A); Chronis-Toscano et al., 2013) necessitate further attention to increase the long-term benefit for both caregiver and child outcomes.
Mothers of adolescents with ADHD were less likely to be married or living with a partner. However, maternal separation and divorce history was not found to significantly predict maternal lifetime QoL. This was surprising given the extensive literature supporting negative physical and psychological health outcomes associated with divorce status (Kiecolt-Glaser, 2018), as well as the relation between childhood ADHD symptoms and divorce (Wymbs et al., 2008). Future research may choose to focus on martial conflict and partner relationship quality rather than divorce or separation history to further elucidate this phenomenon (e.g., Wymbs et al., 2015).
Clinical Implications
The differences in QALYs suggest that parental QoL should be considered as a treatment outcome in ADHD research. Although behavioral parent training is associated with improvements in caregiver strain in the short-term (e.g., Ciesielski et al., 2020; Sibley et al., 2016), it is unclear how evidence-based treatment may or may not improve long-term QoL for parents of youth with ADHD. As such, assessing changes in caregiver QALYs in response to treatment may help identify treatment components that are likely to increase overall QoL and which may be most cost-effective. For example, if factors associated with lower QoL, such as caregiver health, depression, and other external stressors are targeted concurrently with traditional evidence-based treatment (e.g., behavioral parent training), this may increase accessibility and feasibility of treatment for families with multiple risk factors associated with lower QoL. This is particularly important for adolescents, as the most recent update on evidence-based treatment for children and adolescents with ADHD indicates that traditional behavioral parent training produces only minimal effects for adolescents and highlights the need for developmentally appropriate adaptations for adolescents and their families (Evans et al., 2018). Furthermore, research suggests that stimulant medication, another common and well-established treatment for managing ADHD, has a positive impact on the parent-child relationship, but does not have a significant effect on non-child-related caregiver variables, such as negative affect (Chronis et al., 2003b). To date no research has investigated the impact of treatment on parent QoL, an important line for future inquiry.
Given that the highest treatment attrition rates are among those parents who experience higher levels of self-reported stress and depression, as well as social (e.g., single parenthood, lower socio-economic status) and financial stressors (Schnieder et al., 2013), these factors should be integrated into treatment programs to maximize gains for high-risk families. Prior work suggests that parents with increased psychopathology, stress, and whom have children with severe mental health problems also tend to prefer minimal, outcome-oriented interventions (Waschbusch et al., 2011; Wymbs et al., 2016). As such, factors that may have a significant impact on maternal QoL should be addressed when examining treatment preferences and barriers to successful treatment uptake and completion.
Finally, results of the present study have important public health implications. Taken together with other work demonstrating the significant burden experienced by individual families impacted by ADHD (Altszuler et al., 2016; Pelham et al., 2020), as well as the economic burden on society (Chhibber et al., 2020; Zhao et al., 2019), the health-related impacts on maternal QoL identified in this study provides additional evidence that the dissemination of efficacious treatment for ADHD should be set as a public health priority for children and their families. One study examining multiple domains of caregiver QoL, found that caregivers of children with ADHD had similar QoL as adult patients with diabetes (Andrade et al.; 2016), suggesting that the impact of raising a child with ADHD places a significant burden on caregivers’ overall health-related functioning. Although more work is needed to increase our understanding of the cost-of-illness related to ADHD, emerging work in this area highlights the need to prioritize ADHD as a public health concern that requires a similar level of policy intervention, resources, and advocacy as other chronic health conditions. Including caregiver QoL and using QALY to evaluate outcomes in ADHD treatment studies would provide more accurate cost-effectiveness estimates of treatment options.
Limitations
The results of the present study should be taken in light of several limitations. First, the CGSQ was given at one time point (during Wave 3, when participants were adolescents). The analysis considered only the impact on QoL through child’s age 18 and assumed a constant impact over time. It is possible that QALYs would change with the child’s age. Therefore, the lifetime impact should be interpreted with caution. Future research should consider including measures of health functioning longitudinally to calculate a more accurate estimate of lifetime burden to QoL. Similarly, our QoL assessment included two health domains that are commonly impaired when raising a child or adolescent with ADHD. Therefore, the economic impact associated with raising a child with ADHD identified in this study, may be an underrepresentation.
Furthermore, given that prior work has established the ongoing impact of youth’s ADHD symptoms on long-term caregiver burden (Altszuler et al., 2016; Babinski et al., 2020; Pelham et al., 2020; Zhao et al., 2019), it is likely that this impact would continue into young adulthood. Additionally, follow up work may seek to further disentangle the transactional relationship between ADHD symptoms and related impairment in adulthood with maternal QoL and disease burden. Given the lack of father participation in the present study, we were only able to assess maternal QoL. A larger impact would be expected with reports from both parents. Finally, our sample of adolescents with ADHD histories was clinic-referred in childhood and therefore generalizability of results to non-clinical referred families should be interpreted with caution. Further limitations in the samples include predominantly white, male representation and age of the data. Future work should obtain a more diverse sample of families, as factors such as income, race, ethnicity may significantly impact results, especially due to systemic inequalities in health care that may be associated with reductions in QoL.
Despite these limitations, results suggest a significant impact of childhood ADHD on parental QoL and significant contribution to the lifetime economic burden of ADHD. Specifically, this paper represents the first known attempt to measure the impact of raising an adolescent with childhood ADHD on maternal QoL via QALY. Adolescence is an important developmental period that may exacerbate ADHD-related impairment in adolescent and parent functioning. Furthermore, there is a lack of well-established, evidence-based interventions for adolescents with ADHD. As such, it is necessary to identify potential targets for treatment adaptations. The present study advances the field’s understanding of the health impact of raising an adolescent with ADHD by evaluating maternal health states utilizing an internationally recognized and commonly used approach in health economics research, which has yet to be applied to youth mental health concerns. Results highlight ADHD as an important public health burden that should be addressed in the same light as other chronic health conditions and provide evidence to consider QoL in treatment adaptations for adolescents with ADHD.
Funding:
This work was supported by the National Institute on Drug Abuse (Grants # DA12414) to Dr. Pelham and the National Institute of Alcohol Abuse and Alcoholism (#AA11873) to Dr. Molina. Research was also supported in part by AA00202, AA08746, AA12342, and AA0626 to Dr. Molina, grants from the National Institute on Mental Health (MH12010, MH4815, MH47390, MH45576, MH50467, MH53554, MH069614) and Institute of Education Sciences (IESLO3000665A, IESR324B060045) to Dr. Pelham, and the National Institute on Drug Abuse (T32DA043449) to Dr. Piscitello.
Footnotes
- The authors have no relevant financial or non-financial interests to disclose.
- The authors have no conflicts of interest to declare that are relevant to the content of this article.
- All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
- The authors have no financial or proprietary interests in any material discussed in this article.
Compliance with Ethical Standards: The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. If doubt exists whether the research was conducted in accordance with the 1964 Helsinki Declaration or comparable standards, the authors must explain the reasons for their approach, and demonstrate that an independent ethics committee or institutional review board explicitly approved the doubtful aspects of the study. Informed consent to participate in the study was obtained from participants (or their parent/legal guardian in the case of children under 16).
References
- Andrade EM, Geha LM, Duran P, Suwwan R, Machado F & do Rosário MC (2016) Quality of life in caregivers of ADHD children and diabetes patients. Frontiers in Psychiatry, 7:127. doi: 10.3389/fpsyt.2016.00127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altszuler AR, Page TF, Gnagy EM, Coxe S, Arrieta A, Molina BS, & Pelham WE (2016). Financial dependence of young adults with childhood ADHD. Journal of Abnormal Child Psychology, 44(6), 1217–1229. doi: 10.1007/s10802-015-0093-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Applegate B, Lahey BB, Hart EL, Biederman J, Hynd GW, Barkley RA, ... & Shaffer D (1997). Validity of the age-of-onset criterion for ADHD: a report from the DSM-IV field trials. Journal of the American Academy of Child & Adolescent Psychiatry, 36(9), 1211–1221. doi: 10.1097/00004583-199709000-00013 [DOI] [PubMed] [Google Scholar]
- Avrech Bar M, Jlole Majadla S, & Bart O (2018). Managing everyday occupations as a predictor of health and life satisfaction among mothers of children with ADHD. Journal of Attention Disorders, 22(10), 1008–1016. doi: 10.1177/1087054715601211 [DOI] [PubMed] [Google Scholar]
- Babinski DE, Mazzant JR, Merrill BM, Waschbusch DA, Sibley MH, Gnagy EM, Molina BSG, & Pelham WE Jr. (2020). Lifetime caregiver strain among mothers of adolescents and young adults with attention-deficit/hyperactivity disorder. Journal of Family Psychology, 34(3), 342–352. doi: 10.1037/fam0000609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babinski DE, Pelham WE Jr, Molina BS, Gnagy EM, Waschbusch DA, Wymbs BT, ... & Kuriyan AB (2016). Maternal ADHD, parenting, and psychopathology among mothers of adolescents with ADHD. Journal of Attention Disorders, 20(5), 458–468. doi: 10.1177/1087054712461688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brannan AM, Heflinger CA, & Bickman L (1997). The Caregiver Strain Questionnaire: Measuring the impact on the family of living with a child with serious emotional disturbance. Journal of Emotional and Behavioral Disorders, 5(4), 212–222. doi: 10.1177/106342669700500404 [DOI] [Google Scholar]
- Brannan AM, Heflinger CA, & Foster EM (2003). The role of caregiver strain and other family variables in determining children’s use of mental health services. Journal of Emotional and Behavioral Disorders, 11(2), 77–91. doi: 10.1177/106342660301100202 [DOI] [Google Scholar]
- Bussing R, Gary FA, Mason DM, Leon CE, Sinha K, & Garvan CW (2003). Child temperament, ADHD, and caregiver strain: Exploring relationships in an epidemiological sample. Journal of the American Academy of Child & Adolescent Psychiatry, 42(2), 184–192. doi: 10.1097/00004583-200302000-00012 [DOI] [PubMed] [Google Scholar]
- Cappe E, Bolduc M, Rougé MC, Saiag MC, & Delorme R (2017). Quality of life, psychological characteristics, and adjustment in parents of children with attention-deficit/hyperactivity disorder. Quality of Life Research, 26(5), 1283–1294. doi: 10.1007/s11136-016-1446-8 [DOI] [PubMed] [Google Scholar]
- Cheung K, Aberdeen K, Ward MA, & Theule J (2018). Maternal depression in families of children with ADHD: A meta-analysis. Journal of Child and Family Studies, 27(4), 1015–1028. doi: 10.1007/s10826-018-1017-4 [DOI] [Google Scholar]
- Cheung K, & Theule J (2016). Parental psychopathology in families of children with ADHD: A meta-analysis. Journal of Child and Family Studies, 25(12), 3451–3461. doi: 10.1007/s10826-016-0499-1 [DOI] [Google Scholar]
- Chhibber A, Watanabe AH, Chaisai C, Veettil SK, & Chaiyakunapruk N (2021). Global Economic Burden of Attention-Deficit/Hyperactivity Disorder: A Systematic Review. PharmacoEconomics, 1–22. doi: 10.1007/s40273-020-00998-0 [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Kipp H, Baumann B, & Lee SS (2003a). Psychopathology and substance abuse in parents of young children with ADHD. Journal of the American Academy of Child & Adolescent Psychiatry. 42, 1424–1432. doi: 10.1097/00004583-200312000-00009 [DOI] [PubMed] [Google Scholar]
- Chronis AM, Pelham WE, Gnagy EM, Roberts JE, & Aronoff HR (2003b). The impact of late-afternoon stimulant dosing for children with ADHD on parent and parent-child domains. Journal of Clinical Child and Adolescent Psychology, 32(1), 118–126. doi: 10.1207/S15374424JCCP3201_11 [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Williams SH, Baumann BL, Kipp H, & Rathouz PJ (2007). Maternal depression and early positive parenting predict future conduct problems in young children with attention-deficit/hyperactivity disorder. Developmental Psychology. 43, 70–82. doi: 10.1037/0012-1649.43.1.70 [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Clarke TL, O’Brien KA, Raggi VL, Diaz Y, Mintz AD, ... & Lewinsohn P (2013). Development and preliminary evaluation of an integrated treatment targeting parenting and depressive symptoms in mothers of children with attention-deficit/hyperactivity disorder. Journal of Consulting and Clinical Psychology, 81(5), 918–925. doi: 10.1037/a0032112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BSG, Pelham WE, Applegate B, Dahlke A, Overmyer M, & Lahey BB (2010). Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 67, 1044–1051. doi: 10.1001/archgenpsychiatry.2010.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciesielski HA, Loren RE, & Tamm L (2020). Behavioral parent training for ADHD reduces situational severity of child noncompliance and related parental stress. Journal of attention disorders, 24(5), 758–767. doi: 10.1177/1087054719843181 [DOI] [PubMed] [Google Scholar]
- Corso PS, Edwards VJ, Fang X, & Mercy JA (2008). Health-related quality of life among adults who experienced maltreatment during childhood. American Journal of Public Health, 98(6), 1094–1100. doi: 10.2105/AJPH.2007.119826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig F, Operto FF, De Giacomo A, Margari L, Frolli A, Conson M, ... & Margari F (2016). Parenting stress among parents of children with neurodevelopmental disorders. Psychiatry Research, 242, 121–129. doi: 10.1016/j.psychres.2016.05.016 [DOI] [PubMed] [Google Scholar]
- Craig BM, & Rand K (2018). Choice defines QALYs: a US valuation of the EQ-5D-5L. Value in Health, 21, S12. doi: 10.1016/j.jval.2018.04.057 [DOI] [PubMed] [Google Scholar]
- Dette-Hagenmeyer DE, & Reichle B (2014). Parents’ depressive symptoms and children’s adjustment over time are mediated by parenting, but differentially for fathers and mothers. European Journal of Developmental Psychology, 11, 196–210. doi: 10.1080/17405629.2013.848789 [DOI] [Google Scholar]
- Drummond M, & Sculpher M (2005). Common methodological flaws in economic evaluations. Medical Care, II5–II14. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, & Langberg JM (2015). Educational impairments in children with ADHD. In Barkley RA (Ed.), Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (p. 169–190). The Guilford Press [Google Scholar]
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, & Torrance GW (2015). Methods for the economic evaluation of health care programmes. Oxford university press. [Google Scholar]
- Evans SW, Owens JS, Wymbs BT, & Ray AR (2018). Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. Journal of Clinical Child & Adolescent Psychology, 47(2), 157–198. doi: 10.1080/15374416.2017.1390757 [DOI] [PubMed] [Google Scholar]
- Faden VB, Day NL, Windle M, Windle R, Grube JW, Molina BSG, et al. (2004). Collecting longitudinal data through childhood, adolescence, and young adulthood: Methodological challenges. Alcoholism: Clinical and Experimental Research, 28, 330–340. doi: 10.1097/01.ALC.0000113411.33088.FE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster CE, Webster MC, Weissman MM, Pilowsky DJ, Wickramaratne PJ, Rush AJ, ... & King CA (2008). Course and severity of maternal depression: Associations with family functioning and child adjustment. Journal of Youth and Adolescence, 37(8), 906–916. doi: 10.1007/s10964-007-9216-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman M, Banaschewski T, Sikirica V, Quintero J, Erder MH, & Chen KS (2017). Factors associated with caregiver burden among pharmacotherapy-treated children/adolescents with ADHD in the caregiver perspective on pediatric ADHD survey in Europe. Neuropsychiatric Disease and Treatment, 13, 373. doi: 10.2147/NDT.S121391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamad R, Elser H, Tran DC, Rehkopf DH, & Goodman SN (2018). How and why studies disagree about the effects of education on health: A systematic review and meta-analysis of studies of compulsory schooling laws. Social Science & Medicine, 212, 168–178. doi: 10.1016/j.socscimed.2018.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakkaart-van Roijen L, Zwirs BWC, Bouwmans C, Tan SS, Schulpen TWJ, Vlasveld L, & Buitelaar JK (2007). Societal costs and quality of life of children suffering from attention deficient hyperactivity disorder (ADHD). European Child & Adolescent Psychiatry, 16(5), 316–326. doi: 10.1007/s00787-007-0603-6 [DOI] [PubMed] [Google Scholar]
- Harrison C, & Sofronoff K (2002). ADHD and parental psychological distress: Role of demographics, child behavioral characteristics, and parental cognitions. Journal of the American Academy of Child & Adolescent Psychiatry, 41(6), 703–711. doi: 10.1097/00004583-200206000-00010 [DOI] [PubMed] [Google Scholar]
- Hechtman L, Swanson JM, Sibley MH, Stehli A, Owens EB, Mitchell JT, ... & Stern K (2016). Functional adult outcomes 16 years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. Journal of the American Academy of Child & Adolescent Psychiatry, 55(11), 945–952. doi: 10.1016/j.jaac.2016.07.774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herdman M, Gudex C, Lloyd A, Janssen MF, Kind P, Parkin D, Bonsel G, & Badia X (2011). Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Quality of Life Research, 20, 1727–1736. doi: 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirth RA, Chernew ME, Miller E, Fendrick AM, & Weissert WG (2000). Willingness to pay for a quality-adjusted life year: in search of a standard. Medical Decision Making, 20(3), 332–342. doi: 10.1177/0272989X0002000310 [DOI] [PubMed] [Google Scholar]
- Gordon CT, & Hinshaw SP (2017). Parenting stress as a mediator between childhood ADHD and early adult female outcomes. Journal of Clinical Child & Adolescent Psychology, 46(4), 588–599. doi: 10.1080/15374416.2015.1041595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, ... & Busschbach J (2013). Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Quality of Life Research, 22(7), 1717–1727. doi: 10.1007/s11136-012-0322-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia H, & Lubetkin EI (2017). Incremental decreases in quality-adjusted life years (QALY) associated with higher levels of depressive symptoms for US Adults aged 65 years and older. Health and Quality of Life Outcomes, 15(1), 1–9. doi: 10.1186/s12955-016-0582-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia H, Lubetkin EI, Barile JP, Horner-Johnson W, DeMichele K, Stark DS, ... & Thompson WW (2018). Quality-adjusted life years (QALY) for 15 chronic conditions and combinations of conditions among US adults aged 65 and older. Medical Care, 56(8), 740–746. doi: 10.1097/MLR.0000000000000943 [DOI] [PubMed] [Google Scholar]
- Johannesson M (1995). The relationship between cost-effectiveness analysis and cost benefit analysis. Social Science & Medicine, 41, 483–489. doi: 10.1016/0277-9536(94)00353-U [DOI] [PubMed] [Google Scholar]
- Johnston C, & Chronis-Tuscano A (2015). Families and ADHD. In Barkley RA (Ed.), Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (p. 191–209). The Guilford Press. [Google Scholar]
- Kaplan RM & Bush JW (1982). Health-related quality of life measurement for evaluation research and policy analysis. Health Psychology, 1, 61–80. doi: 10.1037/0278-6133.1.1.61 [DOI] [Google Scholar]
- Kent KM, Pelham WE, Molina BS, Sibley MH, Waschbusch DA, Yu J, ... & Karch KM (2011). The academic experience of male high school students with ADHD. Journal of abnormal child psychology, 39(3), 451–462. doi: 10.1007/s10802-010-9472-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK (2018). Marriage, divorce, and the immune system. American Psychologist, 73(9), 1098. doi: 10.1037/amp0000388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriyan AB, Pelham WE, Molina BS, Waschbusch DA, Gnagy EM, Sibley MH, ... & Kent KM (2013). Young adult educational and vocational outcomes of children diagnosed with ADHD. Journal of Abnormal Child Psychology, 41(1), 27–41. doi: 10.1007/s10802-012-9658-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange G, Sheerin D, Carr A, Dooley B, Barton V, Marshall D, Mulligan A. Lawlor, Belton M, & Doyle M (2005). Family factors associated with attention deficit hyperactivity disorder and emotional disorders in children. Journal of Family Therapy, 27(1), 76–96. doi: 10.1111/j.1467-6427.2005.00300.x [DOI] [Google Scholar]
- Letourneau EJ, Brown DS, Fang X, Hassan A, & Mercy JA (2018). The economic burden of child sexual abuse in the United States. Child Abuse & Neglect, 79, 413–422. doi: 10.1016/j.chiabu.2018.02.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipscomb J, Drummond M, Fryback D, Gold M, & Revicki D (2009). Retaining, and enhancing, the QALY. Value in Health, 12, S18–S26. doi: 10.1111/j.1524-4733.2009.00518.x [DOI] [PubMed] [Google Scholar]
- Neumann PJ, Cohen JT, & Weinstein MC (2014). Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. New England Journal of Medicine, 371(9), 796–797. doi: 10.1056/NEJMp1405158 [DOI] [PubMed] [Google Scholar]
- Matza LS, Paramore C, & Prasad M (2005). A review of the economic burden of ADHD. Cost Effectiveness and Resource Allocation, 3(1), 1–9. doi: 10.1186/1478-7547-3-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer M, Oberhoffer R, Hock J, Giegerich T, & Müller J (2016). Health-related quality of life in children and adolescents: Current normative data, determinants, and reliability on proxy-report. Journal of Paediatrics & Child Health, 52, 628–31. doi: 10.1111/jpc.13166 [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, Gnagy EM, Thompson AL, & Marshal MP (2007). Attention-deficit/hyperactivity disorder risk for heavy drinking and alcohol use disorder is age specific. Alcoholism: Clinical and Experimental Research, 31(4), 643–654. doi: 10.1111/j.1530-0277.2007.00349.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BSG, Sibley MH, Pderson SL, & Pelham WE (2017). The Pittsburgh ADHD Longitudinal Study. In Hechtman L (Eds.), Attention-deficit hyperactivity disorder: Adult outcomes and predictors. Oxford University Press: New York, NY, pp 105–155. [Google Scholar]
- Owens EB, Hinshaw SP, Kraemer HC, Arnold LE, Abikoff HB, Cantwell DP, & Wigal T (2003). What treatment for whom for ADHD: Moderators of treatment in the MTA. Journal of Consulting and Clinical Psychology, 71, 540–552. doi: 10.1037/0022-006X.71.3.540 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr, Fabiano GA, & Massetti GM (2005). Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34(3), 449–476. doi: 10.1207/s15374424jccp3403_5 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Foster EM, & Robb JA (2007). The economic impact of attention-deficit/hyperactivity disorder in children and adolescents. Journal of Pediatric Psychology, 32(6), 711–727. doi: 10.1093/jpepsy/jsm022 [DOI] [PubMed] [Google Scholar]
- Pelham WE Jr, Evans SW, Gnagy EM, & Greenslade KE (1992). Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders: Prevalence, factor analyses, and conditional probabilities in a special education sample. School Psychology Review, 21(2), 285–299. doi: 10.1080/02796015.1992.12085615 [DOI] [Google Scholar]
- Pelham WE III, Page TF, Altszuler AR, Gnagy EM, Molina BSG, & Pelham WE Jr. (2020). The long-term financial outcome of children diagnosed with ADHD. Journal of Consulting and Clinical Psychology, 88(2), 160–171. doi: 10.1037/ccp0000461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellerin KA, Costa NM, Weems CF, & Dalton RF (2010). An examination of treatment completers and non-completers at a child and adolescent community mental health clinic. Community Mental Health Journal, 46, 273–281. doi: 10.1007/s10597-009-9285-5 [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Sassi Franco. “Calculating QALYs, comparing QALY and DALY calculations.” Health policy and planning 21.5 (2006): 402–408. doi: 10.1093/heapol/czl018 [DOI] [PubMed] [Google Scholar]
- Schermerhorn AC, D’Onofrio BM, Slutske WS, Emery RE, Turkheimer E, Harden KP, ... & Martin NG (2012). Offspring ADHD as a risk factor for parental marital problems: Controls for genetic and environmental confounds. Twin Research and Human Genetics, 15(6), 700–713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider BW, Gerdes AC, Haack LM, & Lawton KE (2013). Predicting treatment dropout in parent training interventions for families of school-aged children with ADHD. Child & Family Behavior Therapy, 35(2), 144–169. doi: 10.1017/thg.2012.55 [DOI] [Google Scholar]
- Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriguez L, ... & Ward A (2016). Parent–teen behavior therapy+ motivational interviewing for adolescents with ADHD. Journal of Consulting and Clinical Psychology, 84(8), 699. doi: 10.1037/ccp0000106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE Jr, Molina BS, Gnagy EM, Waschbusch DA, Garefino AC, ... & Karch KM (2012). Diagnosing ADHD in adolescence. Journal of Consulting and Clinical Psychology, 80(1), 139. doi: 10.1037/a0026577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ZR, & Langberg JM (2018). Review of the evidence for motivation deficits in youth with ADHD and their association with functional outcomes. Clinical Child and Family Psychology Review, 21(4), 500–526. doi: 10.1007/s10567-018-0268-3 [DOI] [PubMed] [Google Scholar]
- Smith ZR, Langberg JM, Cusick CN, Green CD, & Becker SP (2020). Academic motivation deficits in adolescents with ADHD and associations with academic functioning. Journal of abnormal child psychology, 48(2), 237–249. doi: 10.1007/s10802-019-00601-x [DOI] [PubMed] [Google Scholar]
- Steinberg L (2014). Age of opportunity: Lessons from the new science of adolescence. New York, NY: Houghton Mifflin Harcourt. [Google Scholar]
- Theule J, Wiener J, Rogers MA, & Marton I (2011). Predicting parenting stress in families of children with ADHD: Parent and contextual factors. Journal of Child and Family studies, 20(5), 640–647. doi: 10.1007/s10826-010-9439-7 [DOI] [Google Scholar]
- Theule J, Wiener J, Tannock R, & Jenkins JM (2013). Parenting stress in families of children with ADHD: A meta-analysis. Journal of Emotional and Behavioral Disorders, 21(1), 3–17. doi: 10.1177/1063426610387433 [DOI] [Google Scholar]
- Torrance GW (1986). Measurement of health state utilities for economic appraisal: a review. Journal of Health Economics, 5(1), 1–30. doi: 10.1016/0167-6296(86)90020-2 [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of the Census. (2017). Table C2: Household relationship and living arrangements of children under 18 years, by age and sex: 2017. America’s Family and Living Arrangements. Retrieved from: https://www.census.gov/data/tables/2017/demo/families/cps-2017.html [Google Scholar]
- Van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, ... & Pickard AS (2012). Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value in Health, 15(5), 708–715. doi: 10.1016/j.jval.2012.02.008 [DOI] [PubMed] [Google Scholar]
- Wiener J, Biondic D, Grimbos T, & Herbert M (2016). Parenting stress of parents of adolescents with attention-deficit hyperactivity disorder. Journal of Abnormal Child Psychology, 44(3), 561–574. doi: 10.1007/s10802-015-0050-7 [DOI] [PubMed] [Google Scholar]
- Wang CH, Felton JW, Baumann B, Pelham WE, & Chronis-Tuscano A (2021). Recurrence and Timing of Maternal Depression Predict Early Adolescent Functioning for Children with and Without ADHD. Journal of Attention Disorders, 25(5), 704–714. doi: 10.1177/1087054719832656 [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, Cunningham CE, Pelham WE Jr, Rimas HL, Greiner AR, Gnagy EM, ... & Hoffman MT (2011). A discrete choice conjoint experiment to evaluate parent preferences for treatment of young, medication naive children with ADHD. Journal of Clinical Child & Adolescent Psychology, 40(4), 546–561. doi: 10.1080/15374416.2011.581617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whang KA, Le TK, Khanna R, Williams KA, Roh YS, Sutaria N, ... & Kwatra SG (2021). Health-related quality of life and economic burden of prurigo nodularis. Journal of the American Academy of Dermatology. doi: 10.1016/j.jaad.2021.05.036 [DOI] [PubMed] [Google Scholar]
- Whitehead SJ, & Ali S (2010). Health outcomes in economic evaluation: the QALY and utilities. British Medical Bulletin, 96(1), 5–21. doi: 10.1093/bmb/ldq033 [DOI] [PubMed] [Google Scholar]
- Wymbs BT, Pelham WE Jr., Molina BSG, Gnagy EM, Wilson TK, & Greenhouse JB (2008). Rate and predictors of divorce among parents of youths with ADHD. Journal of Consulting and Clinical Psychology, 76(5), 735–744. doi: 10.1037/a0012719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wymbs BT, Wymbs FA, & Dawson AE (2015). Child ADHD and ODD behavior interacts with parent ADHD symptoms to worsen parenting and interparental communication. Journal of Abnormal Child Psychology, 43(1), 107–119. doi: 10.1007/s10802-014-9887-4 [DOI] [PubMed] [Google Scholar]
- Wymbs FA, Cunningham CE, Chen Y, Rimas HM, Deal K, Waschbusch DA, & Pelham WE Jr (2016). Examining parents’ preferences for group and individual parent training for children with ADHD symptoms. Journal of Clinical Child & Adolescent Psychology, 45(5), 614–631. doi: 10.1080/15374416.2015.1004678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang YT, Luk ES, & Lai KY (2009). Quality of life in parents of children with attention-deficit–hyperactivity disorder in Hong Kong. ?Journal of Psychiatry, 43(8), 731–738. doi: 10.1080/00048670903001968 [DOI] [PubMed] [Google Scholar]
- Zare R, Jafari P, & Ghanizadeh A (2017). Do Adult Attention Deficit Hyperactivity Disorder Quality-Of-Life (AAQoL) scale and the SF-36 scale measure the same construct of health-related quality of life? ADHD Attention Deficit and Hyperactivity Disorders, 9(1), 39–45. doi: 10.1007/s12402-016-0206-5 [DOI] [PubMed] [Google Scholar]
- Zhao X, Page TF, Altszuler AR, Pelham WE, Kipp H, Gnagy EM, ... & Macphee FL (2019). Family burden of raising a child with ADHD. Journal of Abnormal Child Psychology, 47(8), 1327–1338. doi: 10.1007/s10802-019-00518-5 [DOI] [PubMed] [Google Scholar]


