Abstract
Introduction
Coronavirus Disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has spread globally, becoming a long-lasting pandemic. Dengue is the most common arboviral disease in tropical and subtropical regions worldwide. COVID-19 and dengue coinfections have been reported, associated with worse outcomes with significant morbidity and mortality. Therefore, this study aims to determine the epidemiological situation of COVID-19 and dengue coinfection in Latin America.
Methods
A systematic literature review was performed using PubMed, Scopus, Embase, Web of Science, LILACS, and BVS databases from January 1, 2020, to September 4, 2021. The key search terms used were "dengue" and "COVID-19".
Results
Nineteen published articles were included. The studies were case reports with a detailed description of the coinfection's clinical, laboratory, diagnostic, and treatment features.
Conclusion
Coinfection with SARS-CoV-2 and dengue virus is associated with worse outcomes with significant morbidity and mortality. The similar clinical and laboratory features of each infection are a challenge in accurately diagnosing and treating cases. Establishing an early diagnosis could be the answer to reducing the estimated significant burden of these conditions.
Keywords: Clinical features, coinfection, COVID-19, dengue, Latin America
1. Introduction
Coronavirus Disease 2019 (COVID-19) is a highly transmissible and pathogenic viral infection [1] caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [2], has become a long-lasting pandemic [3,4]. SARS-CoV-2 belongs to the Coronaviridae (CoV) subfamily of the RNA virus family Coronavirinae [5], this was first identified in Wuhan, Hubei province, China, in December 2019 [6].
SARS-CoV-2 is spread by both direct means (droplet and person-to-person transmission) and indirect contact (contaminated objects and airborne transmission) [7]. A person infected with SARS-CoV-2 develops COVID-19, which presents as a respiratory syndrome [8], characterized mainly by fever, dry cough, fatigue, myalgia, shortness of breath, and diarrhoea [9].
Globally, as of June 29, 2022, the World Health Organization (WHO) has reported more than 543 million confirmed cases of COVID-19, including more than 6 million deaths [10]. During this COVID-19 pandemic, the incidence of dengue has increased dramatically worldwide [11]. Annually, an estimated 400 million dengue infections with 22,000 deaths are reported worldwide [12].
Dengue is the world's most common arboviral infection [13], a non-segmented single-stranded RNA virus belonging to the family Flaviviridae and genus Flavivirus [14]. The virus is transmitted to humans through the bites of infected female mosquitoes, primarily the Aedes aegypti mosquito, but also A. albopictus and A. vittatus [11]. Dengue infection presents many signs and symptoms, including fever, headache, arthromyalgia, retro-orbital pain, and rash [8].
As the world struggles with the impact of the COVID-19 pandemic [15], dengue-endemic regions face the possibility of a double pandemic that could completely overpower health care administrations [16]. Simultaneous outbreaks of dengue and COVID-19, as well as probable cases of overlapping infections, have already begun in Latin America and certain Asian countries [17].
Dengue and COVID-19 share clinical and laboratory characteristics [18,19]. Therefore, specific tests using real-time reverse transcription-polymerase chain reaction (RT-PCR) or enzyme-linked immunosorbent assay (ELISA) are needed to confirm the diagnosis of these diseases [8,20].
Therefore, this study aims to determine the epidemiological situation of COVID-19 and dengue coinfection in Latin America.
2. Materials and methods
2.1. Protocol and registration
This protocol follows the recommendations established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [21], and it has been reported in the International Prospective Register of Systematic Reviews (PROSPERO) database (CRD42022328445). Since the case reports lack a denominator for any variable that may be included in the meta-analysis, only a descriptive analysis was carried out.
2.2. Eligibility criteria
To evaluate cases of COVID-19 and dengue coinfection in Latin America published, peer-reviewed articles with study designs of case reports, case series, and observational studies were included. No language limit was set for the articles, and publications from January 1, 2020, to September 4, 2021, were included. Systematic review articles, narrative reviews, randomized clinical trials, conference proceedings, editorials, and letters to the editor were excluded.
2.3. Information sources and search strategy
A systematic search was carried out in PubMed, Scopus, Embase, Web of Science, LILACS, and BVS. The search terms used were: "Dengue", "COVID-19″, and "Latin America". The searches were completed on September 4, 2021, and four investigators independently evaluated the search results (Table 1).
Table 1.
Bibliographic search strategy.
| Base | Search strategy |
|---|---|
| PUBMED |
#1 (Dengue[mh] OR Dengue[tiab] OR “Breakbone Fever”[tiab] OR “Break-Bone Fever”[tiab] OR “Break Bone Fever”[tiab] OR Dengue[ot] OR “Breakbone Fever”[ot] OR “Break-Bone Fever”[ot] OR “Break Bone Fever”[ot]) #2 COVID-19[mh] OR COVID-19[tiab] OR “COVID 19”[tiab] OR COVID19[tiab] OR Covid[tiab] OR Covid[ot] OR “2019-nCoV Infection∗”[tiab] OR “2019 nCoV Infection∗”[tiab] OR “2019-nCoV Disease∗”[tiab] OR “2019 nCoV Disease∗”[tiab] OR “Coronavirus Disease-19”[tiab] OR “Coronavirus Disease 19”[tiab] OR “2019 Novel Coronavirus Disease∗”[tiab] OR “2019 Novel Coronavirus Infection∗”[tiab] OR “Coronavirus Disease 2019”[tiab] OR “SARS Coronavirus 2 Infection∗”[tiab] OR “SARS-CoV-2 Infection∗”[tiab] OR “SARS CoV 2 Infection∗”[tiab] OR “COVID-19 Pandemic∗”[tiab] OR “COVID 19 Pandemic∗”[tiab] OR COVID-19[ot] OR “COVID 19”[ot] OR COVID19[ot] OR “2019-nCoV Infection∗”[ot] OR “2019 nCoV Infection∗”[ot] OR “2019-nCoV Disease∗”[ot] OR “2019 nCoV Disease∗”[ot] OR “Coronavirus Disease-19”[ot] OR “Coronavirus Disease 19”[ot] OR “2019 Novel Coronavirus Disease∗”[ot] OR “2019 Novel Coronavirus Infection∗”[ot] OR “Coronavirus Disease 2019”[ot] OR “SARS Coronavirus 2 Infection∗”[ot] OR “SARS-CoV-2 Infection∗”[ot] OR “SARS CoV 2 Infection∗”[ot] OR “COVID-19 Pandemic∗”[ot] OR “COVID 19 Pandemic∗”[ot] OR SARS-CoV-2[mh] OR SARS-CoV-2[tiab] OR “SARS CoV 2”[tiab] OR “Coronavirus Disease 2019 Virus”[tiab] OR “2019 Novel Coronavirus∗”[tiab] OR “Wuhan Seafood Market Pneumonia Virus”[tiab] OR 2019-nCoV[tiab] OR “COVID-19 Virus∗”[tiab] OR “COVID 19 Virus∗”[tiab] OR “Wuhan Coronavirus”[tiab] OR “SARS Coronavirus 2”[tiab] OR “Severe Acute Respiratory Syndrome Coronavirus 2”[tiab] OR SARS-CoV-2[ot] OR “SARS CoV 2”[ot] OR “Coronavirus Disease 2019 Virus”[ot] OR “2019 Novel Coronavirus∗”[ot] OR “Wuhan Seafood Market Pneumonia Virus”[ot] OR 2019-nCoV[ot] OR “COVID-19 Virus∗”[ot] OR “COVID 19 Virus∗”[ot] OR “Wuhan Coronavirus”[ot] OR “SARS Coronavirus 2”[ot] OR “Severe Acute Respiratory Syndrome Coronavirus 2”[ot]) #3 (Americas[mh] OR America∗[tiab] OR America∗[ot] OR Latin America[mh] OR "Latin America"[tiab] OR "Latin America"[ot] OR "Hispano America"[tiab] OR Latin∗[tiab] OR Latin∗[ot] OR Hispan∗[tiab] OR Hispan∗[ot] OR Central America[mh] OR "Central America"[tiab] OR "Central America"[ot] OR Caribbean Region[mh] OR Caribbean[tiab] OR Caribbean[ot] OR South America[mh] OR "South America"[tiab] OR "South America"[ot] OR Mexico[mh] OR Mexico[tiab] OR Mexico[ot] OR Belize[mh] OR Belize[tiab] OR Belize[ot] OR Belice[tiab] OR Belice[ot] OR "British Honduras"[tiab] OR Costa Rica[mh] OR "Costa Rica"[tiab] OR "Costa Rica"[ot] OR El Salvador[mh] OR "El Salvador"[tiab] OR "El Salvador"[ot] OR Guatemala[mh] OR Guatemala[tiab] OR Guatemala[ot] OR Honduras[mh] OR Honduras[tiab] OR Honduras[ot] OR Nicaragua[mh] OR Nicaragua[tiab] OR Nicaragua[ot] OR Panama[mh] OR Panama[tiab] OR Panama[ot] OR West Indies[mh] OR "West Indies"[tiab] OR "West Indies"[ot] OR "Caribbean Islands"[tiab] OR "Caribbean Islands"[ot] OR Montserrat[tiab] OR Montserrat[ot] OR "Turks and Caicos Islands"[tiab] OR "Turks and Caicos Islands"[ot] OR "Cayman Islands"[tiab] OR "Cayman Islands"[ot] OR Antilles[tiab] OR Antilles[ot] OR "Leeward Islands"[tiab] OR "Leeward Islands"[ot] OR "Windward Islands"[tiab] OR "Windward Islands"[ot] OR Caribbean Region[mh] OR Caribbean[tiab] OR Caribbean[ot] OR Caribbean Netherlands[mh] OR Anguilla[tiab] OR Anguilla[ot] OR Anguila[tiab] OR Anguila[tiab] OR Antigua and Barbuda[mh] OR Antigua[tiab] OR Antigua[ot] OR Barbuda[tiab] OR Barbuda[ot] OR Aruba[mh] OR Aruba[tiab] OR Aruba[ot] OR Bahamas[mh] OR Bahamas[tiab] OR Bahamas[ot] OR Barbados[mh] OR Barbados[tiab] OR Barbados[ot] OR Bonaire[tiab] OR Bonaire[ot] OR "Sint Eustatius"[tiab] OR Saba[tiab] OR Saba[ot] OR Cuba[mh] OR Cuba[tiab] OR Cuba[ot] OR Curacao[mh] OR Curacao[tiab] OR Curacao[ot] OR Curazao[tiab] OR Dominica[mh] OR Dominica[tiab] OR Dominica[ot] OR Grenada[tiab] OR Grenada[ot] OR Granada[tiab] OR Granada[ot] OR Guadeloupe[mh] OR Guadeloupe[tiab] OR Guadeloupe[ot] OR Guadalupe[tiab] OR Guadalupe[ot] OR Haiti[mh] OR Haiti[tiab] OR Haiti[ot] OR "Virgin Islands"[tiab] OR "Virgin Islands"[ot] OR Virgenes[tiab] OR British Virgin Islands[mh] OR United States Virgin Islands[mh] OR Jamaica[mh] OR Jamaica[tiab] OR Jamaica[ot] OR Martinique[mh] OR Martinique[tiab] OR Martinique[ot] OR Martinica[tiab] OR Martinica[ot] OR Puerto Rico[mh] OR "Puerto Rico"[tiab] OR "Puerto Rico"[ot] OR Dominican Republic[mh] OR "Dominican Republic"[tiab] OR "Dominican Republic"[ot] OR "Republica Dominicana"[tiab] OR "Republica Dominicana"[ot] OR "San Bartolome"[tiab] OR Saint Kitts and Nevis[mh] OR "St. Kitts and Nevis"[tiab] OR Kitts[tiab] OR Kitts[ot] OR Nevis[tiab] OR Nevis[ot] OR Saint Vincent and the Grenadines[mh] OR "St. Vincent and the Grenadines"[tiab] OR "St. Vincent and the Grenadines"[ot] OR Grenadines[tiab] OR Grenadines[ot] OR Saint Lucia[mh] OR "Saint Lucia"[tiab] OR "Saint Lucia"[ot] OR "St. Lucia"[tiab] OR "St. Lucia"[ot] OR "Santa Lucia"[tiab] OR "Santa Lucia"[ot] OR Sint Maarten[mh] OR "Sint Maarten"[tiab] OR "Sint Maarten"[ot] OR "Saint Martin"[tiab] OR "Saint Martin"[ot] OR "San Martin"[tiab] OR "San Martin"[ot] OR Trinidad and Tobago[mh] OR Trinidad[tiab] OR Trinidad[ot] OR Tobago[tiab] OR Tobago[ot] OR Argentina[mh] OR Argentina[tiab] OR Argentina[ot] OR Bolivia[mh] OR Bolivia[tiab] OR Bolivia[ot] OR Brazil[mh] OR Brazil[tiab] OR Brazil[ot] OR Brasil[tiab] OR Brasil[ot] OR Chile[mh] OR Chile[tiab] OR Chile[ot] OR Colombia[mh] OR Colombia[tiab] OR Colombia[ot] OR Ecuador[mh] OR Ecuador[tiab] OR Ecuador[ot] OR Malvinas[tiab] OR Malvinas[ot] OR Guyana[mh] OR Guyana[tiab] OR Guyana[ot] OR Guiana[tiab] OR Guiana[ot] OR French Guiana[mh] OR Paraguay[mh] OR Paraguay[tiab] OR Paraguay[ot] OR Peru[mh] OR Peru[tiab] OR Peru[ot] OR Suriname[mh] OR Surinam∗[tiab] OR Surinam∗[ot] OR Uruguay[mh] OR Uruguay[tiab] OR Uruguay[ot] OR Venezuela[mh] OR Venezuela[tiab] OR Venezuela[ot]) #4 = #1 AND #2 AND #3 |
| SCOPUS |
#1 TITLE-ABS-KEY(Dengue OR “Breakbone Fever” OR “Break-Bone Fever” OR “Break Bone Fever”) #2 TITLE-ABS-KEY(COVID-19 OR “COVID 19” OR COVID19 OR Covid OR “2019-nCoV Infection∗” OR “2019 nCoV Infection∗” OR “2019-nCoV Disease∗” OR “2019 nCoV Disease∗” OR “Coronavirus Disease-19” OR “Coronavirus Disease 19” OR “2019 Novel Coronavirus Disease∗” OR “2019 Novel Coronavirus Infection∗” OR “Coronavirus Disease 2019” OR “SARS Coronavirus 2 Infection∗” OR “SARS-CoV-2 Infection∗” OR “SARS CoV 2 Infection∗” OR “COVID-19 Pandemic∗” OR “COVID 19 Pandemic∗” OR SARS-CoV-2 OR “SARS CoV 2” OR “Coronavirus Disease 2019 Virus” OR “2019 Novel Coronavirus∗” OR “Wuhan Seafood Market Pneumonia Virus” OR 2019-nCoV OR “COVID-19 Virus∗” OR “COVID 19 Virus∗” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Severe Acute Respiratory Syndrome Coronavirus 2”) #3 TITLE-ABS-KEY(America∗ OR "Latin America" OR "Hispano America" OR Latin∗ OR Hispan∗ OR "Central America" OR Caribb∗ OR "South America" OR Mexico OR Belize OR Belice OR "British Honduras" OR "Costa Rica" OR "El Salvador" OR Guatemala OR Honduras OR Nicaragua OR Panama OR "West Indies" OR "Caribbean Islands" OR Montserrat OR "Turks and Caicos Islands" OR "Cayman Islands" OR Antilles OR "Leeward Islands" OR "Windward Islands" OR “Caribbean Region” OR Anguilla OR Anguila OR “Antigua and Barbuda” OR Antigua OR Barbuda OR Aruba OR Bahamas OR Barbados OR Bonaire OR "Sint Eustatius" OR Saba OR Cuba OR Curacao OR Curazao OR Dominica OR Grenada OR Granada OR Guadeloupe OR Guadalupe OR Haiti OR "Virgin Islands" OR Virgenes OR Jamaica OR Martinique OR Martinica OR "Puerto Rico" OR "Dominican Republic" OR "Republica Dominicana" OR "San Bartolome" OR "Saint Kitts and Nevis" OR “St. Kitts and Nevis” OR Kitts OR Nevis OR "Saint Vincent and the Grenadines" OR "St. Vincent and the Grenadines" OR Grenadines OR "Saint Lucia" OR "St. Lucia" OR "Santa Lucia" OR "Sint Maarten" OR "Saint Martin" OR "San Martin" OR “Trinidad and Tobago” OR Trinidad OR Tobago OR Argentina OR Bolivia OR Brazil OR Brasil OR Chile OR Colombia OR Ecuador OR Malvinas OR Guyana OR Paraguay OR Peru OR Surinam∗ OR Uruguay OR Venezuela) #4 = #1 AND #2 AND 3 |
| WEB OF SCIENCE |
#1 TS=(Dengue OR “Breakbone Fever” OR “Break-Bone Fever” OR “Break Bone Fever”) OR TI=(Dengue OR “Breakbone Fever” OR “Break-Bone Fever” OR “Break Bone Fever”) OR AB=(Dengue OR “Breakbone Fever” OR “Break-Bone Fever” OR “Break Bone Fever”) OR AK=(Dengue OR “Breakbone Fever” OR “Break-Bone Fever” OR “Break Bone Fever”) #2 TS=(COVID-19 OR “COVID 19” OR COVID19 OR Covid OR “2019-nCoV Infection∗” OR “2019 nCoV Infection∗” OR “2019-nCoV Disease∗” OR “2019 nCoV Disease∗” OR “Coronavirus Disease-19” OR “Coronavirus Disease 19” OR “2019 Novel Coronavirus Disease∗” OR “2019 Novel Coronavirus Infection∗” OR “Coronavirus Disease 2019” OR “SARS Coronavirus 2 Infection∗” OR “SARS-CoV-2 Infection∗” OR “SARS CoV 2 Infection∗” OR “COVID-19 Pandemic∗” OR “COVID 19 Pandemic∗” OR SARS-CoV-2 OR “SARS CoV 2” OR “Coronavirus Disease 2019 Virus” OR “2019 Novel Coronavirus∗” OR “Wuhan Seafood Market Pneumonia Virus” OR 2019-nCoV OR “COVID-19 Virus∗” OR “COVID 19 Virus∗” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Severe Acute Respiratory Syndrome Coronavirus 2”) OR TI=(COVID-19 OR “COVID 19” OR COVID19 OR Covid OR “2019-nCoV Infection∗” OR “2019 nCoV Infection∗” OR “2019-nCoV Disease∗” OR “2019 nCoV Disease∗” OR “Coronavirus Disease-19” OR “Coronavirus Disease 19” OR “2019 Novel Coronavirus Disease∗” OR “2019 Novel Coronavirus Infection∗” OR “Coronavirus Disease 2019” OR “SARS Coronavirus 2 Infection∗” OR “SARS-CoV-2 Infection∗” OR “SARS CoV 2 Infection∗” OR “COVID-19 Pandemic∗” OR “COVID 19 Pandemic∗” OR SARS-CoV-2 OR “SARS CoV 2” OR “Coronavirus Disease 2019 Virus” OR “2019 Novel Coronavirus∗” OR “Wuhan Seafood Market Pneumonia Virus” OR 2019-nCoV OR “COVID-19 Virus∗” OR “COVID 19 Virus∗” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Severe Acute Respiratory Syndrome Coronavirus 2”) OR AB=(COVID-19 OR “COVID 19” OR COVID19 OR Covid OR “2019-nCoV Infection∗” OR “2019 nCoV Infection∗” OR “2019-nCoV Disease∗” OR “2019 nCoV Disease∗” OR “Coronavirus Disease-19” OR “Coronavirus Disease 19” OR “2019 Novel Coronavirus Disease∗” OR “2019 Novel Coronavirus Infection∗” OR “Coronavirus Disease 2019” OR “SARS Coronavirus 2 Infection∗” OR “SARS-CoV-2 Infection∗” OR “SARS CoV 2 Infection∗” OR “COVID-19 Pandemic∗” OR “COVID 19 Pandemic∗” OR SARS-CoV-2 OR “SARS CoV 2” OR “Coronavirus Disease 2019 Virus” OR “2019 Novel Coronavirus∗” OR “Wuhan Seafood Market Pneumonia Virus” OR 2019-nCoV OR “COVID-19 Virus∗” OR “COVID 19 Virus∗” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Severe Acute Respiratory Syndrome Coronavirus 2”) OR AK=(COVID-19 OR “COVID 19” OR COVID19 OR Covid OR “2019-nCoV Infection∗” OR “2019 nCoV Infection∗” OR “2019-nCoV Disease∗” OR “2019 nCoV Disease∗” OR “Coronavirus Disease-19” OR “Coronavirus Disease 19” OR “2019 Novel Coronavirus Disease∗” OR “2019 Novel Coronavirus Infection∗” OR “Coronavirus Disease 2019” OR “SARS Coronavirus 2 Infection∗” OR “SARS-CoV-2 Infection∗” OR “SARS CoV 2 Infection∗” OR “COVID-19 Pandemic∗” OR “COVID 19 Pandemic∗” OR SARS-CoV-2 OR “SARS CoV 2” OR “Coronavirus Disease 2019 Virus” OR “2019 Novel Coronavirus∗” OR “Wuhan Seafood Market Pneumonia Virus” OR 2019-nCoV OR “COVID-19 Virus∗” OR “COVID 19 Virus∗” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Severe Acute Respiratory Syndrome Coronavirus 2”) #3 TS=(America∗ OR "Latin America" OR "Hispano America" OR Latin∗ OR Hispan∗ OR "Central America" OR Caribb∗ OR "South America" OR Mexico OR Belize OR Belice OR "British Honduras" OR "Costa Rica" OR "El Salvador" OR Guatemala OR Honduras OR Nicaragua OR Panama OR "West Indies" OR "Caribbean Islands" OR Montserrat OR "Turks and Caicos Islands" OR "Cayman Islands" OR Antilles OR "Leeward Islands" OR "Windward Islands" OR “Caribbean Region” OR Anguilla OR Anguila OR “Antigua and Barbuda” OR Antigua OR Barbuda OR Aruba OR Bahamas OR Barbados OR Bonaire OR "Sint Eustatius" OR Saba OR Cuba OR Curacao OR Curazao OR Dominica OR Grenada OR Granada OR Guadeloupe OR Guadalupe OR Haiti OR "Virgin Islands" OR Virgenes OR Jamaica OR Martinique OR Martinica OR "Puerto Rico" OR "Dominican Republic" OR "Republica Dominicana" OR "San Bartolome" OR "Saint Kitts and Nevis" OR “St. Kitts and Nevis” OR Kitts OR Nevis OR "Saint Vincent and the Grenadines" OR "St. Vincent and the Grenadines" OR Grenadines OR "Saint Lucia" OR "St. Lucia" OR "Santa Lucia" OR "Sint Maarten" OR "Saint Martin" OR "San Martin" OR “Trinidad and Tobago” OR Trinidad OR Tobago OR Argentina OR Bolivia OR Brazil OR Brasil OR Chile OR Colombia OR Ecuador OR Malvinas OR Guyana OR Paraguay OR Peru OR Surinam∗ OR Uruguay OR Venezuela) OR TI=(America∗ OR "Latin America" OR "Hispano America" OR Latin∗ OR Hispan∗ OR "Central America" OR Caribb∗ OR "South America" OR Mexico OR Belize OR Belice OR "British Honduras" OR "Costa Rica" OR "El Salvador" OR Guatemala OR Honduras OR Nicaragua OR Panama OR "West Indies" OR "Caribbean Islands" OR Montserrat OR "Turks and Caicos Islands" OR "Cayman Islands" OR Antilles OR "Leeward Islands" OR "Windward Islands" OR “Caribbean Region” OR Anguilla OR Anguila OR “Antigua and Barbuda” OR Antigua OR Barbuda OR Aruba OR Bahamas OR Barbados OR Bonaire OR "Sint Eustatius" OR Saba OR Cuba OR Curacao OR Curazao OR Dominica OR Grenada OR Granada OR Guadeloupe OR Guadalupe OR Haiti OR "Virgin Islands" OR Virgenes OR Jamaica OR Martinique OR Martinica OR "Puerto Rico" OR "Dominican Republic" OR "Republica Dominicana" OR "San Bartolome" OR "Saint Kitts and Nevis" OR “St. Kitts and Nevis” OR Kitts OR Nevis OR "Saint Vincent and the Grenadines" OR "St. Vincent and the Grenadines" OR Grenadines OR "Saint Lucia" OR "St. Lucia" OR "Santa Lucia" OR "Sint Maarten" OR "Saint Martin" OR "San Martin" OR “Trinidad and Tobago” OR Trinidad OR Tobago OR Argentina OR Bolivia OR Brazil OR Brasil OR Chile OR Colombia OR Ecuador OR Malvinas OR Guyana OR Paraguay OR Peru OR Surinam∗ OR Uruguay OR Venezuela) OR AB=(America∗ OR "Latin America" OR "Hispano America" OR Latin∗ OR Hispan∗ OR "Central America" OR Caribb∗ OR "South America" OR Mexico OR Belize OR Belice OR "British Honduras" OR "Costa Rica" OR "El Salvador" OR Guatemala OR Honduras OR Nicaragua OR Panama OR "West Indies" OR "Caribbean Islands" OR Montserrat OR "Turks and Caicos Islands" OR "Cayman Islands" OR Antilles OR "Leeward Islands" OR "Windward Islands" OR “Caribbean Region” OR Anguilla OR Anguila OR “Antigua and Barbuda” OR Antigua OR Barbuda OR Aruba OR Bahamas OR Barbados OR Bonaire OR "Sint Eustatius" OR Saba OR Cuba OR Curacao OR Curazao OR Dominica OR Grenada OR Granada OR Guadeloupe OR Guadalupe OR Haiti OR "Virgin Islands" OR Virgenes OR Jamaica OR Martinique OR Martinica OR "Puerto Rico" OR "Dominican Republic" OR "Republica Dominicana" OR "San Bartolome" OR "Saint Kitts and Nevis" OR “St. Kitts and Nevis” OR Kitts OR Nevis OR "Saint Vincent and the Grenadines" OR "St. Vincent and the Grenadines" OR Grenadines OR "Saint Lucia" OR "St. Lucia" OR "Santa Lucia" OR "Sint Maarten" OR "Saint Martin" OR "San Martin" OR “Trinidad and Tobago” OR Trinidad OR Tobago OR Argentina OR Bolivia OR Brazil OR Brasil OR Chile OR Colombia OR Ecuador OR Malvinas OR Guyana OR Paraguay OR Peru OR Surinam∗ OR Uruguay OR Venezuela) OR AK=(America∗ OR "Latin America" OR "Hispano America" OR Latin∗ OR Hispan∗ OR "Central America" OR Caribb∗ OR "South America" OR Mexico OR Belize OR Belice OR "British Honduras" OR "Costa Rica" OR "El Salvador" OR Guatemala OR Honduras OR Nicaragua OR Panama OR "West Indies" OR "Caribbean Islands" OR Montserrat OR "Turks and Caicos Islands" OR "Cayman Islands" OR Antilles OR "Leeward Islands" OR "Windward Islands" OR “Caribbean Region” OR Anguilla OR Anguila OR “Antigua and Barbuda” OR Antigua OR Barbuda OR Aruba OR Bahamas OR Barbados OR Bonaire OR "Sint Eustatius" OR Saba OR Cuba OR Curacao OR Curazao OR Dominica OR Grenada OR Granada OR Guadeloupe OR Guadalupe OR Haiti OR "Virgin Islands" OR Virgenes OR Jamaica OR Martinique OR Martinica OR "Puerto Rico" OR "Dominican Republic" OR "Republica Dominicana" OR "San Bartolome" OR "Saint Kitts and Nevis" OR “St. Kitts and Nevis” OR Kitts OR Nevis OR "Saint Vincent and the Grenadines" OR "St. Vincent and the Grenadines" OR Grenadines OR "Saint Lucia" OR "St. Lucia" OR "Santa Lucia" OR "Sint Maarten" OR "Saint Martin" OR "San Martin" OR “Trinidad and Tobago” OR Trinidad OR Tobago OR Argentina OR Bolivia OR Brazil OR Brasil OR Chile OR Colombia OR Ecuador OR Malvinas OR Guyana OR Paraguay OR Peru OR Surinam∗ OR Uruguay OR Venezuela) #4 = #1 AND #2 AND #3 |
| EMBASE |
#1 'dengue'/exp OR 'aden fever':ti,ab,kw OR 'bouquet fever':ti,ab,kw OR 'break-bone fever':ti,ab,kw OR 'breakbone fever':ti,ab,kw OR 'classical dengue':ti,ab,kw OR 'classical dengue fever':ti,ab,kw OR 'dandy fever':ti,ab,kw OR 'dengue':ti,ab,kw OR 'dengue fever':ti,ab,kw OR 'dengue virus infection':ti,ab,kw OR 'solar fever':ti,ab,kw OR 'sun fever':ti,ab,kw OR 'dengue virus'/exp OR 'denv':ti,ab,kw OR 'dengue virus':ti,ab,kw OR 'dengue viruses':ti,ab,kw OR 'breakbone fever virus':ti,ab,kw OR 'dandy fever virus':ti,ab,kw OR 'dengue fever virus':ti,ab,kw OR 'dengue flavivirus':ti,ab,kw OR 'denque haemorrhagic virus':ti,ab,kw OR 'denque hemorrhagic virus':ti,ab,kw #2 'coronavirus disease 2019'/exp OR '2019 novel coronavirus disease':ti,ab,kw OR '2019 novel coronavirus epidemic':ti,ab,kw OR '2019 novel coronavirus infection':ti,ab,kw OR '2019-ncov disease':ti,ab,kw OR '2019-ncov infection':ti,ab,kw OR 'covid':ti,ab,kw OR 'covid 19':ti,ab,kw OR 'covid 19 induced pneumonia':ti,ab,kw OR 'covid 2019':ti,ab,kw OR 'covid-10':ti,ab,kw OR 'covid-19':ti,ab,kw OR 'covid-19 induced pneumonia':ti,ab,kw OR 'covid-19 pneumonia':ti,ab,kw OR 'covid19':ti,ab,kw OR 'sars coronavirus 2 infection':ti,ab,kw OR 'sars coronavirus 2 pneumonia':ti,ab,kw OR 'sars-cov-2 disease':ti,ab,kw OR 'sars-cov-2 infection':ti,ab,kw OR 'sars-cov-2 pneumonia':ti,ab,kw OR 'sars-cov2 disease':ti,ab,kw OR 'sars-cov2 infection':ti,ab,kw OR 'sarscov2 disease':ti,ab,kw OR 'sarscov2 infection':ti,ab,kw OR 'wuhan coronavirus disease':ti,ab,kw OR 'wuhan coronavirus infection':ti,ab,kw OR 'coronavirus disease 2':ti,ab,kw OR 'coronavirus disease 2010':ti,ab,kw OR 'coronavirus disease 2019':ti,ab,kw OR 'coronavirus disease 2019 pneumonia':ti,ab,kw OR 'coronavirus disease-19':ti,ab,kw OR 'coronavirus infection 2019':ti,ab,kw OR 'ncov 2019 disease':ti,ab,kw OR 'ncov 2019 infection':ti,ab,kw OR 'new coronavirus pneumonia':ti,ab,kw OR 'novel coronavirus 2019 disease':ti,ab,kw OR 'novel coronavirus 2019 infection':ti,ab,kw OR 'novel coronavirus disease 2019':ti,ab,kw OR 'novel coronavirus infected pneumonia':ti,ab,kw OR 'novel coronavirus infection 2019':ti,ab,kw OR 'novel coronavirus pneumonia':ti,ab,kw OR 'paucisymptomatic coronavirus disease 2019':ti,ab,kw OR 'severe acute respiratory syndrome 2':ti,ab,kw OR 'severe acute respiratory syndrome 2 pneumonia':ti,ab,kw OR 'severe acute respiratory syndrome cov-2 infection':ti,ab,kw OR 'severe acute respiratory syndrome coronavirus 2 infection':ti,ab,kw OR 'severe acute respiratory syndrome coronavirus 2019 infection':ti,ab,kw OR 'severe acute respiratory syndrome coronavirus 2'/exp OR '2019 ncov':ti,ab,kw OR '2019 new coronavirus':ti,ab,kw OR '2019 novel coronavirus':ti,ab,kw OR '2019 severe acute respiratory syndrome coronavirus 2':ti,ab,kw OR '2019-ncov':ti,ab,kw OR 'covid 19 virus':ti,ab,kw OR 'hcov-19':ti,ab,kw OR 'human coronavirus 2019':ti,ab,kw OR 'sars coronavirus 2':ti,ab,kw OR 'sars-cov-2':ti,ab,kw OR 'sars-related coronavirus 2':ti,ab,kw OR 'sars2 (virus)':ti,ab,kw OR 'sever acute respiratory syndrome coronavirus 2':ti,ab,kw OR 'severe acute respiratory coronavirus 2':ti,ab,kw OR 'severe acute respiratory syndorme coronavirus 2':ti,ab,kw OR 'severe acute respiratory syndrome coronavirus 2':ti,ab,kw OR 'severe acute respiratory syndrome coronoavirus 2':ti,ab,kw OR 'severe acute respiratory syndrome coronvirus 2':ti,ab,kw OR 'severe acute respiratory syndrome related coronavirus 2':ti,ab,kw OR 'severe acute respiratory syndrome virus 2':ti,ab,kw OR 'severe acute respiratoy syndrome coronavirus 2':ti,ab,kw OR 'wuhan coronavirus':ti,ab,kw OR 'wuhan seafood market pneumonia virus':ti,ab,kw OR 'ncov-2019':ti,ab,kw OR 'novel 2019 coronavirus':ti,ab,kw OR 'novel coronavirus 2019':ti,ab,kw OR 'novel coronavirus-19':ti,ab,kw OR 'severe acute respiratory syndrome 2 virus':ti,ab,kw OR 'severe acute respiratory syndrome cov-2 virus':ti,ab,kw OR 'severe acute respiratory syndrome corona virus 2':ti,ab,kw OR 'severe acute respiratory syndrome coronavirus 2019':ti,ab,kw #3 'western hemisphere'/exp OR 'western hemisphere' OR 'america' OR 'americas' OR 'north america'/exp OR 'north america' OR 'america, north' OR 'north american'/exp OR 'north american' OR 'north americans' OR 'caribbean islands'/exp OR 'caribbean islands' OR 'indies, west' OR 'west indies' OR 'caribbean'/exp OR 'caribbean' OR 'caribbean region' OR 'south america'/exp OR 'south america' OR 'america, south' OR 'south american'/exp OR 'south american' OR 'south americans' OR 'central america'/exp OR 'central america' OR 'america, central' OR 'central american'/exp OR 'central american' OR 'central americans' OR 'south and central america'/exp OR 'latin america' OR 'south and central america' OR 'america, south and central' OR 'hispanic'/exp OR 'hispanic' OR 'hispanic americans' OR 'latino' OR latin∗ OR hispan∗ OR caribb∗ OR 'mexico'/exp OR 'mexico' OR 'united mexican states' OR 'united states of mexico' OR 'mexican'/exp OR 'mexican' OR 'mexicans' OR 'belize'/exp OR 'belize' OR 'british honduras' OR 'belizean'/exp OR 'belizean' OR 'belizeans' OR 'costa rica'/exp OR 'costa rica' OR 'costa rican'/exp OR 'costa rican' OR 'costa ricans' OR 'el salvador'/exp OR 'el salvador' OR 'salvador' OR 'salvadoran'/exp OR 'el salvadoran' OR 'el salvadorans' OR 'el salvadorean' OR 'el salvadoreans' OR 'el salvadorian' OR 'el salvadorians' OR 'salvadoran' OR 'salvadorans' OR 'salvadorean' OR 'salvadoreans' OR 'salvadorian' OR 'salvadorians' OR 'guatemala'/exp OR 'guatemala' OR 'guatemalan'/exp OR 'guatemalan' OR 'guatemalans' OR 'honduras'/exp OR 'honduras' OR 'honduran'/exp OR 'honduran' OR 'hondurans' OR 'nicaragua'/exp OR 'nicaragua' OR 'nicaraguan'/exp OR 'nicaraguan' OR 'nicaraguans' OR 'panama'/exp OR 'panama' OR 'panama canal zone' OR 'panamanian'/exp OR 'panamanian' OR 'panamanians' OR 'montserrat'/exp OR 'montserrat' OR 'turks and caicos islands'/exp OR 'turks and caicos islands' OR 'cayman islands'/exp OR 'cayman islands' OR 'antillean'/exp OR 'antillean' OR 'antilleans' OR 'dutch antillean' OR 'dutch antilleans' OR 'netherlands antillean' OR 'netherlands antilleans' OR 'antigua and barbuda'/exp OR 'antigua' OR 'antigua and barbuda' OR 'barbuda and antigua' OR 'aruba'/exp OR 'aruba' OR 'bahamas'/exp OR 'bahama islands' OR 'bahamas' OR 'bahama' OR 'barbados'/exp OR 'barbados' OR 'bonaire'/exp OR 'bonaire' OR 'sint eustatius'/exp OR 'sint eustatius' OR 'st. eustatius' OR 'statia' OR 'saba'/exp OR 'saba' OR 'cuba'/exp OR 'cuba' OR 'cuban'/exp OR 'cuban' OR 'cubans' OR 'curacao'/exp OR 'curacao' OR 'dominica'/exp OR 'dominica' OR 'dominican (dominica)'/exp OR 'dominican (dominica)' OR 'dominicans (dominica)' OR 'grenada'/exp OR 'guadeloupe'/exp OR 'guadeloupe' OR 'haiti'/exp OR 'haiti' OR 'haitian'/exp OR 'haitian' OR 'haitians' OR 'virgin islands (u.s.)'/exp OR 'u.s. virgin islands' OR 'united states virgin islands' OR 'virgin islands (u.s.)' OR 'virgin islands of the united states' OR 'virgin islands (british)'/exp OR 'british virgin islands' OR 'virgin islands (british)' OR 'jamaica'/exp OR 'jamaica' OR 'jamaican'/exp OR 'jamaican' OR 'jamaicans' OR 'martinique'/exp OR 'martinique' OR 'puerto rico'/exp OR 'puerto rico' OR 'porto rico' OR 'puerto rican'/exp OR 'puerto rican' OR 'puerto ricans' OR 'dominican republic'/exp OR 'dominican republic' OR 'dominican (dominican republic)'/exp OR 'dominican (dominican republic)' OR 'dominicans (dominican republic)' OR 'saint kitts and nevis'/exp OR 'saint kitts and nevis' OR 'st. kitts and nevis' OR 'saint vincent and the grenadines'/exp OR 'saint vincent and the grenadines' OR 'st. vincent and the grenadines' OR 'saint lucia'/exp OR 'saint lucia' OR 'st. lucia' OR 'trinidad and tobago'/exp OR 'trinidad and tobago' OR 'trinidadian'/exp OR 'tobagonian' OR 'tobagonians' OR 'trinidadian' OR 'trinidadians' OR 'argentina'/exp OR 'argentina' OR 'argentinian'/exp OR 'argentinian' OR 'argentinians' OR 'bolivia'/exp OR 'bolivia' OR 'bolivian'/exp OR 'bolivian' OR 'bolivians' OR 'brazil'/exp OR 'brazil' OR 'federative republic of brazil' OR 'united states of brazil' OR 'brazilian'/exp OR 'brazilian' OR 'brazilians' OR 'chile'/exp OR 'chile' OR 'chili' OR 'chilean'/exp OR 'chilean' OR 'chileans' OR 'colombia'/exp OR 'colombia' OR 'columbia' OR 'colombian'/exp OR 'colombian' OR 'colombians' OR 'ecuador'/exp OR 'ecuador' OR 'ecuadorean'/exp OR 'ecuadorean' OR 'ecuadoreans' OR 'falkland islands (malvinas)'/exp OR 'falkland island' OR 'falkland islands' OR 'falkland islands (malvinas)' OR 'falklands' OR 'malvinas' OR 'malvinas islands' OR 'guyana'/exp OR 'guyana' OR 'guiana, british' OR 'french guiana'/exp OR 'french guiana' OR 'french guaiana' OR 'french guyana' OR 'guiana, french' OR 'guyana, french' OR 'paraguay'/exp OR 'paraguay' OR 'paraguayan'/exp OR 'paraguayan' OR 'paraguayans' OR 'peru'/exp OR 'peru' OR 'peruvian'/exp OR 'peruvian' OR 'peruvians' OR 'suriname'/exp OR 'suriname' OR 'surinam' OR 'surinamese'/exp OR 'surinamer' OR 'surinamere' OR 'surinamese' OR 'uruguay'/exp OR 'uruguay' OR 'uruguayan'/exp OR 'uruguayan' OR 'uruguayans' OR 'venezuela'/exp OR 'venezuela' OR 'venezuelan'/exp OR 'venezuelan' OR 'venezuelans' #4 = #1 AND #2 AND #3 |
| BVS |
#1 (Dengue) OR (“Breakbone Fever”) OR (“Break-Bone Fever”) OR (“Break Bone Fever”) #2 (COVID-19) OR (“COVID 19”) OR (COVID19) OR (Covid) OR (“2019-nCoV Infection∗”) OR (“2019 nCoV Infection∗”) OR (“2019-nCoV Disease∗”) OR (“2019 nCoV Disease∗”) OR (“Coronavirus Disease-19”) OR (“Coronavirus Disease 19”) OR (“2019 Novel Coronavirus Disease∗”) OR (“2019 Novel Coronavirus Infection∗”) OR (“Coronavirus Disease 2019”) OR (“SARS Coronavirus 2 Infection∗”) OR (“SARS-CoV-2 Infection∗”) OR (“SARS CoV 2 Infection∗”) OR (“COVID-19 Pandemic∗”) OR (“COVID 19 Pandemic∗”) OR (SARS-CoV-2) OR (“SARS CoV 2”) OR (“Coronavirus Disease 2019 Virus”) OR (“2019 Novel Coronavirus∗”) OR (“Wuhan Seafood Market Pneumonia Virus”) OR (2019-nCoV) OR (“COVID-19 Virus∗”) OR (“COVID 19 Virus∗”) OR (“Wuhan Coronavirus”) OR (“SARS Coronavirus 2”) OR (“Severe Acute Respiratory Syndrome Coronavirus 2”) #3 (America∗) OR ("Latin America") OR ("Hispano America") OR (Latin∗) OR (Hispan∗) OR ("Central America") OR (Caribb∗) OR ("South America") OR (Mexico) OR (Belize) OR (Belice) OR ("British Honduras") OR ("Costa Rica") OR ("El Salvador") OR (Guatemala) OR (Honduras) OR (Nicaragua) OR (Panama) OR ("West Indies") OR ("Caribbean Islands") OR (Montserrat) OR ("Turks and Caicos Islands") OR ("Cayman Islands") OR (Antilles) OR ("Leeward Islands") OR ("Windward Islands") OR (“Caribbean Region”) OR (Anguilla) OR (Anguila) OR (“Antigua and Barbuda”) OR (Antigua) OR (Barbuda) OR (Aruba) OR (Bahamas) OR (Barbados) OR (Bonaire) OR ("Sint Eustatius") OR (Saba) OR (Cuba) OR (Curacao) OR (Curazao) OR (Dominica) OR (Grenada) OR (Granada) OR (Guadeloupe) OR (Guadalupe) OR (Haiti) OR ("Virgin Islands") OR (Virgenes) OR (Jamaica) OR (Martinique) OR (Martinica) OR ("Puerto Rico") OR ("Dominican Republic") OR ("Republica Dominicana") OR ("San Bartolome") OR ("Saint Kitts and Nevis") OR (“St. Kitts and Nevis”) OR (Kitts OR Nevis) OR ("Saint Vincent and the Grenadines") OR ("St. Vincent and the Grenadines") OR (Grenadines) OR ("Saint Lucia") OR ("St. Lucia") OR ("Santa Lucia") OR ("Sint Maarten") OR ("Saint Martin") OR ("San Martin") OR (“Trinidad and Tobago”) OR (Trinidad) OR (Tobago) OR (Argentina) OR (Bolivia) OR (Brazi)l OR (Brasil) OR (Chile) OR (Colombia) OR (Ecuador) OR (Malvinas) OR (Guyana) OR (Paraguay) OR (Peru) OR (Surinam∗) OR (Uruguay) OR (Venezuela) #4 = #1 AND #2 AND #3 |
2.4. Study selection
Two researchers (DALF, JBM) created a database based on the electronic searches, managed it with the appropriate management software (EndNote), and removed duplicates. Then, through Rayyan QCRI (https://rayyan.qcri.org/) [22], two researchers (MOD, JNNL) carried out the screening process, analyzing the titles and abstracts provided by the search independently, choosing those that appeared to meet the inclusion criteria and, if necessary, evaluating the full text. In case of disagreement, the investigators will discuss until a consensus is reached; in case of dispute, a third investigator will be invited to the discussion to help resolve it.
The peer-review authors (SAU, RAYC, AJRM) reviewed the full-text reports and analyzed the inclusion criteria to reach a decision.
2.5. Outcomes
The primary outcome was to determine the epidemiological situation of COVID-19 and dengue coinfection.
2.6. Data collection process and data items
Four investigators independently extracted data from the selected studies in a Microsoft Excel spreadsheet. The following data were extracted from the selected studies: title, authors, year of publication, study design, country, inclusion and exclusion criteria, number of cases/participants, age, sex, comorbidities, symptoms and physical examination findings, method of diagnosis of COVID-19, method of diagnosis of dengue infection, initial diagnosis, delay in diagnosis of coinfection, laboratory findings, findings on imaging studies and other relevant results, need for hospitalization, need for ICU, treatment, clinical outcome (e.g., death), and follow-up. A fifth investigator checked the list of articles and data extractions to ensure that there were no duplicate articles or duplicate information and resolved discrepancies about study inclusion.
3. Results
3.1. Study selection
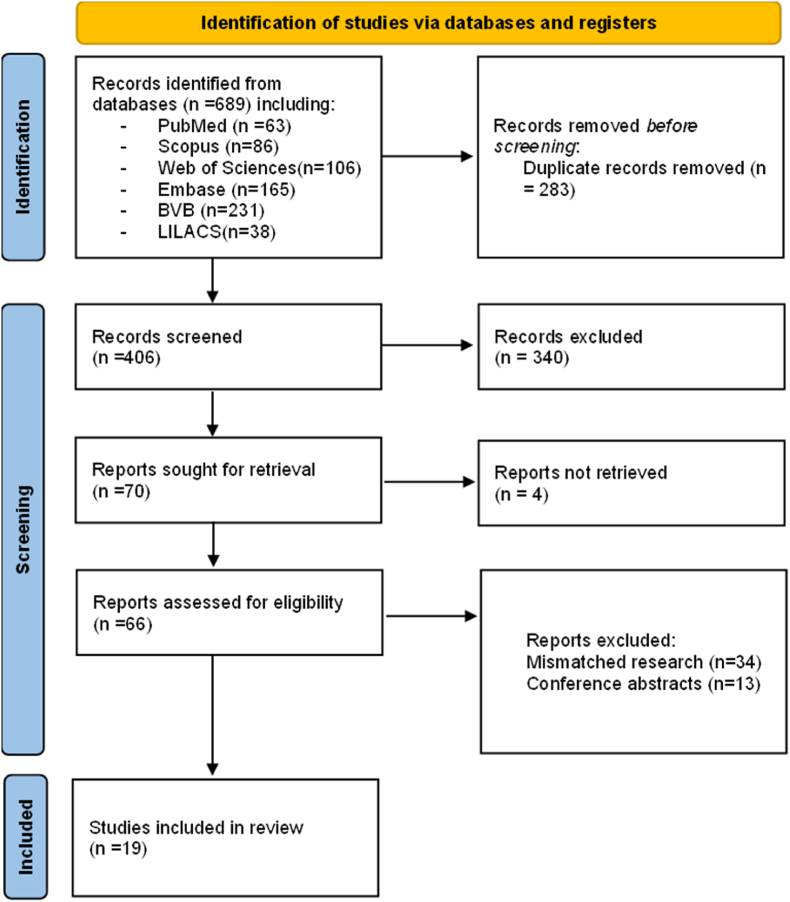
A total of 689 articles were retrieved using the search strategy. The selection strategy is shown in the prism flow chart (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (Fig. 1) [21]. After the removal of duplicates, 406 articles were screened by the reviewers. After filtering the titles and reading the abstracts, 66 articles were selected for full-text reading, and 19 were considered eligible for inclusion in this systematic review [[23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41]].
Fig. 1.
PRISMA flow chart of the studies selection process.
3.2. Study characteristics
The main characteristics of the articles included in this review are summarized in Table 2 and Table 3. Our review included 19 studies that were published between January 1, 2020, and August 30, 2021 [[23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41]]. The studies (n = 19) reported case reports with a detailed description of the clinical and health outcome (Table 2, Table 3). These studies also described the laboratory findings and treatment of COVID-19 and dengue co-infection (Table 4 and Table 5). A total of 152 cases of coinfections were reported in six countries: Brazil (n = 78) [23,26,27,31,34,35,39,40], Mexico (n = 1) [24], Colombia (n = 5) [25,30,32], Argentina (n = 16) [28,33,37,41], Peru (n = 51) [29,38] and Ecuador (n = 1) [36] (Table 2, Table 3). Brazil reported the highest number of coinfection cases, followed by Peru (Fig. 2). Most of the coinfection was in adults. In terms of diagnosis, PCR (n = 12) [23,24,27,30,32,34,37,41],IgM(n = 97) [25,26,28,31,33,35,36,[38], [39], [40]],IgG(n = 43) [25,26,31,32,34,38], seroconversion (n = 2) [30,37]and NS1 (n = 48) [28,29,31,[33], [34], [35],37,38] were used for dengue diagnosis, while PCR (n = 105) [[23], [24], [25], [26], [27], [28],[30], [31], [32],[34], [35], [36], [37], [38], [39],41], IgM (n = 92) [23,27,29,36,38,39] and IgG (n = 66) [23,27,29,36,38,40] were used for COVID-19 (Table 2, Table 3).
Table 2.
Main individual characteristics of the studies included.
| Authors | Year | Design | Country | Participants (N) | Age (Years) | Sex | Diagnosis method |
Serotype of dengue | Hospitalization (days) | Outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 | Dengue | ||||||||||
| Braatz M et al. [23] | 2021 | Case series | Brazil | 1 | 16 | F | IgM, IgG, and PCR SARS-CoV-2 positive | PCR positive | NR | 21 | Discharged after 21 days of hospitalization |
| Reyes J et al. [24] | 2021 | Case report | Mexico | 1 | 42 | F | PCR SARS-CoV-2 positive | PCR positive | DENV- 1 | 18 | Discharged on day 24 after the onset of symptoms |
| Agudelo R et al. [25] | 2021 | Case report | Colombia | 2 | 24 | F | PCR SARS-CoV-2 positive | IgM and IgG positive | DENV- 1 | 6 | She was discharged after six days of hospitalization |
| 59 | M | PCR SARS-CoV-2 positive | IgM/IgG positive | NR | 63 | Died | |||||
| Bicudo N et al. [26] | 2020 | Case report | Brazil | 1 | 56 | F | PCR SARS-CoV-2 positive | IgM/IgG positive | DENV- 1 | 6 | Discharged after 6 days. |
| Lopes R [27]. | 2020 | Case report | Brazil | 1 | 39 | M | IgM, IgG and PCR SARS-CoV-2 positive | PCR positive | DENV- 1 | NR | Clinical improvement |
| Salvo C et al. [28] | 2020 | Case report | Argentina | 1 | 43 | M | PCR SARS-CoV-2 positive | IgM and NS1 positive. | NR | NR | Discharged. |
| Nakandakari et al. [29] | 2021 | Case report | Peru | 1 | 13 | F | IgM and IgG positive | NS1 positive. | NR | 5 | Discharged after five days |
| Rosso et al. [30] | 2021 | Cross-sectional | Colombia | 2 | NR | NR | PCR SARS-CoV-2 positive | PCR positive | DENV 1 - 4 | NR | NR |
| NR | NR | PCR SARS-CoV-2 positive | Seroconversion | NR | NR | NR | |||||
| Estofolete et al. [31] | 2020 | Case report | Brazil | 1 | 60 | F | PCR SARS-CoV-2 positive | NS1, IgM and IgG positive | NR | NR | Died after five days |
| Villamil-Gomez WE et al. [32] | 2021 | Case report | Colombia | 1 | 52 | M | PCR SARS-CoV-2 positive | IgG, IgM and PCR positive | DENV- 2 | 7 | Discharged, after 7 days |
| Radisic M et al. [33] | 2020 | Case report | Argentina | 1 | 25 | M | PCR SARS-CoV-2 positive | IgM and NS1 positive | NR | NR | He turned afebrile and was discharged one week after diagnosis. |
| Rosso M et al. [41] | 2021 | Case report | Argentina | 1 | 57 | F | PCR SARS-CoV-2 positive | PCR positive | NR | NR | Gradually improved over five days. |
| Quental K et al. [34] | 2021 | Case report | Brazil | 2 | 53 | F | PCR SARS-CoV-2 positive | NS1, IgG, IgM and PCR positive. | DENV- 1 | NR | NR |
| 57 | M | PCR SARS-CoV-2 positive | NS1, IgG, IgM and PCR positive. | DENV- 1 | NR | NR | |||||
| Schulte H et al. [35] | 2021 | Retrospective cohort | Brazil | 13 | NR | M | PCR SARS-CoV-2 positive | NS1 positive | NR | NR | NR |
| NR | F | PCR SARS-CoV-2 positive | NS1 positive | NR | NR | Discharged after seven days. | |||||
| NR | F | PCR SARS-CoV-2 positive | IgM positive | NR | NR | Discharged after four days. | |||||
| NR | M | PCR SARS-CoV-2 positive | NS1 positive | NR | NR | NR | |||||
| NR | F | PCR SARS-CoV-2 positive | IgM positive | NR | NR | NR | |||||
| NR | M | PCR SARS-CoV-2 positive | NS1 positive | NR | NR | NR | |||||
| NR | M | PCR SARS-CoV-2 positive | IgM positive | NR | NR | NR | |||||
| NR | F | PCR SARS-CoV-2 positive | IgM positive | NR | NR | NR | |||||
| NR | M | PCR SARS-CoV-2 positive | IgM positive | NR | NR | NR | |||||
| NR | F | PCR SARS-CoV-2 positive | IgM positive | NR | NR | NR | |||||
| NR | F | PCR SARS-CoV-2 positive | NS1 positive | NR | NR | NR | |||||
| NR | M | PCR SARS-CoV-2 positive | IgM positive | NR | NR | NR | |||||
| NR | F | PCR SARS-CoV-2 positive | NS1 positive | NR | NR | Discharged after five days. | |||||
| Valdés J et al. [36] | 2020 | Case report | Ecuador | 1 | 50 | M | IgG, IgM and PCR SARS-CoV-2 positive. | IgM positive | NR | NR | Discharged for 26 days |
PCR: Polymerase Chain Reaction.
NR: No report.
M/F: Male/Female.
DENV 1-4: dengue virus serotype 1 and 4.
NS1: nonstructural protein 1.
Table 3.
Main results of COVID-19 and dengue coinfection studies included.
| Authors | Year | Design | Country | Cases (N) | Age (Years) Median (IQR) |
Sex N (%) |
Diagnosis method |
Serotype of dengue N (%) |
Hospitalization (days) Median (IQR) |
Outcome N (%) |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| COVID-19 N (%) |
Dengue N (%) |
||||||||||
| Carosella L et al. [37] | 2021 | Retrospective analysis | Argentina | 13 | 37 (29-50) | Male: 7 (54.0) Female: 6 (46.0) |
Real time-PCR SARS-CoV-2 +: 13 (100.0) | NS1 DENV +: 8 (61.5) RT - PCR +: 4 (30.8) Seroconvertion: 1 (7.7) |
NR | 12.0 (10.0 - 14.0) | Death: 0 (0.0) Discharged: 13 (100.0) |
| Mejía J et al. [38] | 2021 | Retrospective analysis | Peru | 50 | 55.5 (40.5 - 65) | Male: 39 (78.0) Female: 11 (22) |
SARS-CoV-2 IgG/IgM +: 39 (78.0) Real time-PCR SARS-CoV-2+: 4 (8.0) SARS-CoV-2 IgM +: 4 (8.0) SARS-CoV-2 IgG +: 3 (6.0) |
NS1 DENV + †: 30 (60.0) DENV IgM + ‡: 19 (38.0) DENV IgM/IgG + b: 1 (2.0) |
NR | NR | Dead: 14 (28.0) Discharged: 36 (72.0) |
| Soares I et al. [39] | 2021 | Retrospective cohort | Brazil | 43 | NR | NR | RT-PCR SARS-CoV-2 +: 43 (100.0) SARS-CoV-2 IgM + : 43(100.0) |
DENV IgM+: 43 (100.0) | NR | NR | NR |
| StringariI L et al. [40] | 2021 | Retrospective cohort | Brazil | 2 | 55.5 ± 6.36 | Females: 2 (100.0) | SARS-CoV-2 IgG +: 2 (100.0) | DENV IgM and IgG: 2 (100.0) | NR | NR | NR |
| Rosso et al. [30] | 2021 | Cross-sectional | Colombia | 2 | NR | NR | RT-PCR SARS-CoV-2+: 2 (100.0) | RT-PCR +: 1 (50.0) Seroconvertion +: 1 (50.0) | DENV 1-4: 1 (50.0) | NR | NR |
| Schulte H et al. [35] | 2021 | Retrospective cohort | Brazil | 13 | 27 - 79 | Male: 6 (46.2) Female: 7 (53.8) |
RT-PCR SARS-CoV-2 +: 13 (100.0) | NS1 DENV +: 6 (46.2) DENV IgM +: 7 (53.8)" |
NR | 12.0 (10.0 - 14.0) | Clinical improvement: 13 (100.0) Death: 0 (0.0) |
†Patients with less than five days of symptoms.
‡Patients with symptoms more significant than five days.
+Positive. DENV 1-4: dengue virus serotype 1 and 4; NS1: nonstructural protein 1; Real time-PCR: real-time polymerase chain reaction; RT-PCR: reverse transcription-polymerase chain reaction; Seroconvertion: persistence of positive anti-DENV antibodies 24 days after onset of symptoms.
Table 4.
Detailed individual characteristics of the studies included considering treatment, clinical and laboratory findings.
| Authors | Case | Comorbidities | Symptoms and findings in physical examination | Laboratory findings | Treatment |
|---|---|---|---|---|---|
| Braatz M et al. [23] | 1 | No comorbidities | Paresthesia, progressive difficulty in walking, acute paraparesis, hypoaesthesia | Protein (28.5 mg/dL), glucose (61 mg/dL) | Acyclovir for 14 days, intravenous human immunoglobulin for five days and methylprednisolone for five days |
| Reyes J et al. [24] | 1 | No comorbidities | Day 7: lymphocytes (32.2%), monocyte count (0.2x109/uL), monocyte ratio (8.2%), granulocyte count (1.4x109/uL), granulocyte ratio (59.6%), red blood cells (4.83x 106/uL), Hemoglobin (16 g/dl), Hematocrit (42.6%), MCV (88.3 fl), MCH (33p), MCHC (37.4g/dl), RDW-CV (12.4%), RDW-SD (40.2 fL), mean platelet volume (12.2 fl), platelet criterion (0.173%) and platelet distribution width (16%). | ||
| Day 9: lymphocytes (36.5%), monocyte count (0.1x109), monocyte ratio (7%), granulocyte count (cell x109), granulocyte ratio (56.5%), red blood cells (5.17x 106/uL), Hemoglobin (16.9 g/dl), Hematocrit (45.2%), MCV (87.5 fl), MCH (32.7 p), MCHC (37.4g/Dl), RDW-CV (12.3%), RDW-SD (39.3 fL), mean platelet volume (11.6 fl), platelet criterion (0.138%) and platelet distribution width (16.5%). | |||||
| Fever, headache, diarrhoea, chest pain, chills, odynophagia, myalgia, arthralgia, malaise, pruritus, low back pain, nausea, loss of appetite, sweating, 97% oxygen saturation; pulse, 88 beats per minute; respiratory rate, 20 breaths per minute; blood pressure, 130/90 mmHg; vomiting, nausea, hyperemia in the face, petechial rash and erythema | Day 11: lymphocytes (48.1%), monocyte count (0.2x109), monocyte ratio (7.6%), granulocyte count (1.4 x109), granulocyte ratio (44.3%), red blood cells (5.09 x 106/uL), hemoglobin (16.8 g/dl), hematocrit (44.7%), MCV (87.7 fl), MCH (32.9 p), MCHC (37.6 g/dl), RDW-CV (12.2%), RDW-SD (39.3 fL), mean platelet volume (12.3 fl), platelet criterion (0.147%) and platelet distribution width (16.2%). | Azithromycin, ibuprofen for four days and ivermectin. | |||
| Day 14: lymphocytes (42.4%), monocyte count (0.3x109), monocyte ratio (7.6%), granulocyte count (1.9 x109), granulocyte ratio (50%), red blood cells (4.97 x 106/uL), hemoglobin (16.3 g/dl), hematocrit (43.4%), MCV (87.3 fl), MCH (32.9 p), MCHC (37.6 g/dl), RDW-CV (12%), RDW-SD (38.4 fL), mean platelet volume (10.6 fl), platelet criterion (0.23%), platelet distribution width (16.5%), albumin (4.1 g/dL), globin (3.8 g/dL), albumin/globulin ratio (1.08), total bilirubin (0.5 mg/dL), direct bilirubin (0.1 mg/dL), indirect bilirubin (0.4 mg/dL), aspartate aminotransferase (48 U/L), alanine aminotransferase (75 U/L) and alkaline phosphatase (32 U/L). | |||||
| Agudelo R et al. [25] | 1 | No comorbidities | Fever, odynophagia, adynamia, myalgia, arthralgia, vomiting and diarrhoea | Thrombocytopenia, leukopenia | NR |
| 2 | Hypertension, obesity, and poorly controlled diabetes mellitus | Fever and dyspnoea | Thrombocytopenia, leukocytosis, lymphopenia and elevated transaminases | NR | |
| Bicudo N et al. [26] | 1 | NR | Sore throat, anosmia, ageusia, frontal headache, fever, dry cough, mild dyspnea without need for supplementary oxygen, SpO2 94% on room air for five days, diffuse erythematopapular rash with itching, localized in the limbs and trunk regions | Leukopenia, lymphopenia, thrombocytopenia, and elevated D-dimer | Chloroquine, azithromycin, anticoagulation |
| Lopes R [27]. | 1 | No comorbidities | Fever, myalgia, diarrhoea, ageusia, mild dyspnea | NR | Painkillers, antipyretics |
| Salvo C et al. [28] | 1 | HIV infection | Fever, generalized body pain, dry cough | Leucopenia, HIV viral load (6400 copies per mm3), CD4 count 341 cells per mm3 | NR |
| Nakandakari et al. [29] | 1 | No comorbidites | Recurrent fever, general malaise, abundant gingival bleeding, low intermenstrual bleeding, respiratory rate 20 breaths/minute, mean arterial pressure 73.3, saturation 98% with HFNC at 2 L/min, generalized skin rash, features of old bleeding from the oral cavity, decreased vesicular murmur in the lower 2/3 of both hemithorax, pain at superficial and deep palpation in epigastrium, lower extremities skin rash type "white islands in a sea of red." | leukopenia (5.1 [103/uL]), neutropenia (25.4%), lymphocytosis(50.4%), severe thrombocytopenia (17 [103/uL]), hemoconcentration 41.9%, elevated C-reactive protein (12.5), elevated Aspartate aminotransferase (728 U/L), elevated Glutamate Aminotransferase (215 U/L) | 0.9% sodium chloride three cc/kg/hour, Ceftriaxone intravenous 1 g/12 h, Dexamethasone intravenous 4 mg at 8 am and 4 pm, Oxygen therapy high-flow nasal cannula (HFNC) at 2 L/min, Fluid therapy was increased at 5 cc/kg/hour, ceftriaxone was increased to 80 mg/kg/day, HFNC was progressively withdrawn |
| Rosso et al. [30] | 1 | NR | NR | NR | NR |
| 2 | NR | NR | NR | NR | |
| Estofolete et al. [31] | 1 | Hypertension and obesity | Fever, myalgia, headache, retroorbital pain, dry cough, sudden paresis of the right-upper member, respiratory failure, saturation 89%, respiratory rate 30 bpm, blood pressure 120/70 mmHg, heart rate 89 bpm | Hematocrit 42.7%, Leukocytosis 25.120 (cells/mm3), increased Neutrophils 82%, Lymphopenia 4%, Thrombocytopenia 48( × 103), increased C-reative protein 9.51 (mg/dl), increased AST/ALT 74/83 (U/L), increased GGT 862 (U/L), increased AP 177 (U/L), increased direct bilirrubin 0.62 (mg/dl), increased TTPa 30.5 (s), increased D Dimer 5.85 (μg/ml), increased CPK 416 (U/L), increased pO2 170.2 mmHg, increased lactate 2.7 (mmol/L), decreased HCO3 18 mmHg, decreased PH 7.22, decreased excess base -9.4 (mmol/L) | Orotracheal intubation, invasive mechanical ventilation, vasoactive drugs, hemodialysis, a high fraction of inspired oxygen (60-100%), high positive end-expiratory pressure (16 cmH2O), ceftriaxone, azithromycin, oseltamivir phosphate, heparin |
| Villamil-Gomez WE et al. [32] | 1 | Obesity | Flu-like symptoms, worsening fever, chills, pruritus, temperature 41°C, blood pressure 110/70 mmHg, heart rate 100 bpm, respiratory frequency 40 bpm, oxygen saturation 90-92%, BMI 31.7 kg/m2, bibasilar crackles extending to both mid pulmonary fields, arthralgia, myalgia, dorso-lumbar pain, asthenia, adynamia, dyspnea, dry cough, roseoliform maculopapular rash, scarlatiniform-like rash, "white islands in a red sea". Oral mucosa, hand and feet are not involved | leukocytosis 4.000 cel/mL, increased C-reactive protein 7 mg/L, thrombocytopenia 120.000 cel/mL, increased LDH 700 UI/L, increased ferritin 650 mcg/mL, increased D-dimer 5.175 ng/mL, increased troponin 0.8 ng/mL, increased AST 55 IU/L, increased ALT 40 IU/L | Ceftriaxone, enoxaparin 1.5 mg/kg, methylprednisolone, ipratropium bromide, isotonic crystalloid 10 mL/kg, and supplementary oxygen by nasal cannula and Continuous Positive Airway Pressure |
| Radisic M et al. [33] | 1 | No comorbidities | Asthenia, headache, joint, muscle pain, fever, sore throat, heart rate: 112 per minute, respiratory rate 20 bpm, oxygen saturation: 98%, temperature: 38 °C | Lymphocytes, thrombocytopenia, elevated transaminases, alkaline phosphatase and urea | NR |
| Rosso M et al. [41] | 1 | Tobacco use and chronic obstructive pulmonary disease | Diarrhoea, abdominal pain, headache, retro-orbital pain, aching joints, dyspnea, subfever, pruritic rash, unspecific thoracic pain; physical examination revealed: a non-blanching, generalized rash with scattered petechiae predominantly on the extremities, upper trunk and abdomen | Biomarkers: normal, acute phase reactants: normal, thrombocytopenia | Treated symptomatically |
| Quental K et al. [34] | 1 | No comorbidities | High fever, chills, severe headaches, muscle pain, arthralgia, malaise and persistent vomiting during treatment | Hemoconcentration (hematocrit 46.3%), thrombocytopenia (platelet count 147,000/mm3), high C reactive protein (18.2 mg/L), elevated serum aspartate aminotransferase and alanine aminotransferase (92 U/L and 67 U/L, respectively) | Oral analgesics, antipyretics, intravenous hydration after malaise and persistent vomiting |
| 2 | Sedentary lifestyle, obesity, hepatic steatosis and insulin resistance | Low fever, asthenia, headache, muscle pain, itchy rash on the trunk and upper members | Thrombocytopenia (135,000/mm3), high CRP levels (35 mg/L), and elevated AST/GOT (75 U/L) and ALT/GPT (75 U/L) | NR | |
| Schulte H et al. [35] | 1 | Diabetes and hypertension | Fever, myalgia, ecchymosis dyspnea (SpO2 = 95%) | Platelet (84,000/μL), Lymphocyte (2982/μL) | Analgesics |
| 2 | No comorbidities | Fever, dry cough, dyspnea, myalgia | Platelet (93,000/μL), Lymphocyte (730/μL) | Analgesics, hydration with 0.9% saline, amoxicillin-clavulanate, prophylaxis of thrombosis with compression stockings | |
| 3 | Diabetes | Dyspnea (SpO2 = 91%) | Platelet (169,000/μL), Lymphocyte (2627/μL) | Analgesics, enoxaparin 40 mg/day | |
| 4 | Hypopituitarism and adrenal insufficiency | Myalgia, ecchymosis, dyspnea | Platelet (110,000/μL), Lymphocyte (3254/μL) | Analgesics, prednisone dosage increased from 5 to 15 mg for five days | |
| 5 | Pregnancy | Retro-orbital pain, arthralgia, myalgia | Platelet (94,000/μL), Lymphocyte (1500/μL) | Hydroxychloroquine 400 mg twice a day for 1 day, chloroquine 450 mg for 1 day, enoxaparin 40 mg/day for 2 weeks, azithromycin 500 mg/day for five days, ceftriaxone 2g/day for five days | |
| 6 | No comorbidities | Fever | NR | Self-medication with ivermectin 6 mg/kg | |
| 7 | NR | Dry cough, sore throat | Platelet (191,000/μL), Lymphocyte (2200/μL) | Analgesics, hydration with 0.9% saline. | |
| 8 | No comorbidities | Myalgia, nasal congestion, dyspnea, fatigue, diarrhoea | Platelet (238,000/μL), Lymphocyte (1490/μL) | Azithromycin 500 mg for two days, self-medication with ivermectin 6 mg/kg | |
| 9 | No comorbidities | Retro-orbital pain, myalgia, fever, anosmia, diarrhoea | Platelet (180,000/μL), Lymphocyte (1561/μL) | Analgesics | |
| 10 | Pregnancy, gestational diabetes, chronic gastritis and depression | Fever, dry cough, myalgia, sore throat, nasal congestion, diarrhoea, anosmia, ageusia, pruritus | Platelet (196,000/μL), Lymphocyte (1500/μL) | Analgesics, prednisone 20 mg for five days, hydration with 0.9% saline | |
| 11 | Pituitary tumour and hypopituitarism | Fever, myalgia and fatigue dyspnea (SpO2 = 93%) | Platelet (50,000/μL), Lymphocyte (3100/μL) | Azithromycin 500 mg for five days, prednisone dosage increased from 5 to 20 mg for seven days | |
| 12 | No comorbidities | Myalgia | Platelet (169,000/μL), Lymphocyte (2327/μL) | None | |
| 13 | No comorbidities | Fever, myalgia dyspnea (SpO2 = 92%), urethral bleeding | Platelet (87,000/μL), Lymphocyte (1450/μL) | Corticoids, azithromycin 500 mg, oxygen in the first two days | |
| Valdés J et al. [36] | 1 | Gout and smoker | Fever, Polyarticular pain, Frontooccipitoparietal headache, myalgias, arthralgias, tiredness, decay, fatigue, semi-pasty diarrhoea, evening and night sweating, dry mucous membranes, low-grade jaundice, anal erythema, osteoarticular alteration, dry, non-productive cough, dorsal pain, subcrepitant rales in lung bases, pale fasciae, decreased vesicular murmur in lung bases, respiratory rate: 28 breaths/min, tachycardia: 102 beats/min, temperature 39 oC and oxygen saturation: 80%, moderate epistaxis, intense melenas, liquid diarrhoea, cough | Leukocytosis, mild anaemia (11.8 g/L), elevated serum ferritin, transaminases, lactate dehydrogenase, elevated serum ferritin, transaminases, lactate dehydrogenase and leukocytosis with neutrophilia (89.3%) and lymphopenia (6.5%) | Paracetamol, fluids, physical antipyretic measures, amoxicillin plus clavulanic acid |
NR: No report.
Table 5.
Detailed group characteristics of the studies included considering treatment, clinical and laboratory findings
| Authors | Comorbidities N (%) |
Symptoms and findings in physical examination N (%) |
Laboratory findings Mean (SD) |
Treatment N (%) |
|---|---|---|---|---|
| Carosella L et al. [37] | - Obesity: 3 (23.0) - Chronic obstructive pulmonary disease: 2 (15.3) - Hypertension: 2 (15.3) - Smoking: 2 (15.3) - Diabetes: 1 (7.7) - Cirrhosis: 1 (7.7) |
- Fever: 13 (100.0) - Headache: 8 (61.5) - Myalgia: 7 (53.8) - Cough: 3 (23.1) - Rash: 3 (23.1) - Chills: 3 (23.1) - Dyspnea: 2 (15.3) - Diarrhea: 2 (15.3) - Odynophagia: 2 (15.3) - Nasal congestion: 2 (15.3) - Anosmia: 1 (7.7) - Dysgeusia: 1 (7.7) - Arthralgia: 1 (7.7) - Nausea or vomiting: 1 (7.7) |
- Hematocrit (%): 44 (41.0) - Hemoglobin (g/dL): 14.1 (14.0) - Leukocytes (1 × 103 cells/μL): 4.3 (8.9) - Leukopenia(<4 × 103 cells/μL) †: 4 (31.0) - Lymphocyte count (1 × 103 cells/μL): 0.81 (2.6) - Lymphopenia (<1.5 × 103 cells/μL) †: 12 (92.0) - Platelets (1 × 103/μL): 172 (156.0) - Platelets (1 × <150 × 103/μL)a: 6 (46.0) - Platelets (1 × <100 × 103/μL)a: 3 (23.0) - Abnormal AST level†: 6 (46.0) - Abnormal ALT level†: 6 (46.0) |
- Lopinavir/ritonavir: 3 (23.1) - Hydroxychloroquine: 1 (7.7) - Antimicrobial drug therapy: 6 (46.1) |
| Mejía J et al. [38] | -High blood pressure: 16 (32.0) -Type 2 diabetes mellitus: 13 (26.0) -Chronic kidney failure: 7 (14.0) -Obesity: 6 (12.0) -Cancer: 4 (8.0) -Asthma: 4 (8.0) -Pulmonary fibrosis: 2 (2.0) |
Haematological manifestations - Bleeding or hemorrhage: 11 (22.0) Temperature-related manifestations - Fever: 26 (52.0) - Chills: 2 (4.0) - Hypothermia: 1 (2.0) Osteoarticular manifestations - Arthralgia: 8 (16.0) - General malaise: 7 (14.0) - Myalgia: 5 (10.0) - General weakness: 2 (4.0) - Low back pain: 2 (4.0) Gastrointestinal manifestations - Abdominal pain: 6 (12.0) - Nausea or vomiting: 4 (8.0) - Hepatomegaly: 1 (2.0) - Splenomegaly: 1 (2.0) Cutaneous and subcutaneous manifestations - Ecchymosis: 5 (10.0) - Edema: 5 (10.0) - Erythematous lesions: 4 (8.0) - Petechiae: 3 (6.0) - Rash: 3 (6.0) - Bruises: 2 (4.0) - Adenopathies: 1 (2.0) - Pale: 1 (2.0) - Pruritus: 1 (2.0) Neuro-ophthalmological alterations - Headache: 2 (4.0) - Retroocular pain: 2 (4.0) - Disorientation: 1 (2.0) - Organic failure: 3 (6.0) |
- Thrombocytopenia †: 30 (60.0) - Hematocrit concentrationa: 24 (48.0) |
NR |
| Soares I et al. [39] | NR | - Fever (78.6) - Cough (76.8) - Dyspnea (50.0) - Anosmia (41.1) - Sore throat (36.6) |
- Leucocytes (%): 6.74 (2.88) - Neutrophils (1 × 103/μL): 4.5 (2.9) - Lymphocytes (1x10³/μL): 1.5 (6.6) - Monocytes (1x10³/μL): 0.42 (2.00) - Hemoglobin (g/100 mL): 14.36 (1.53) - Platelets (1x10³/μL): 224.76 (73.61)- AST (UI/L): 43.81 (25.57)- ALT (UI/L): 54.62 (54.26) - Urea (mg/100 mL): 37.63 (22.74) - Creatinine (mg/100 mL): 1.84 (5.65)- CK (UI/L): 139.55 (119.56)- LDH (U/L): 545.02 (308.59) - Glucose (mg/100 mL): 172.5 (124.44) |
NR |
| StringariI L et al. [40] | NR | NR | NR | NR |
| Rosso et al. [30] | NR | NR | NR | NR |
| Schulte H et al. [35] | - Diabetes: 2 (15.4) - Hypopituitarism: 2 (15.4) - Pregnancy: 2 (15.4)- Gestational diabetes: 1 (7.7) - Hypertension: 1 (7.7) - Adrenal insufficiency: 1 (7.7) - Pituitary tumor: 1 (7.7) - Chronic gastritis: 1 (7.7) - Depression: 1 (7.7) - Without comorbidities: 6 (46.2) - NR: 1 (7.7) |
- Fever: 7 (53.9) - Myalgia: 10 (76.9) - Dry cough: 3 (23.1) - Ecchymosis: 2 (15.4) - Dyspnea: 7 (53.9) - Retro-orbital pain: 2(15.4) - Arthralgia: 1 (7.7) - Sore throat: 2 (15.4) - Nasal congestion: 2 (15.4) - Diarrhea: 2 (15.4) - Fatigue: 1 (7.7) - Ageusia: 1 (7.7) - Pruritus: 1 (7.7) - Urethral bleeding: 1 (7.7) |
- Platelets (1 × 103/μL): 138.4 (58.7) - Lymphocytes (1 × 103 cells/μL): 2.1 (0.8) |
- Analgesics: 7 (53.8) - Azithromycin: 4 (30.8) - Prednisone: 4(30.8)- Enoxaparin: 2 (15.4) - Hydration with 0.9% saline: 3(23.1) - Amoxicillin clavulanate: 1 (7.7) - Prophylaxis of thrombosis with compression stockings: 1 (7.7) - Hydroxychloroquine: 1 (7.7) - Chloroquine: 1 (7.7) - Ceftriaxone: 1 (7.7) - Self-medication with ivermectin: 2 (15.4) - Oxygen in the first 2 days: 1(7.7) - No treatment: 1 (7.7) |
NR: No report.
†Frequency (percentage).
Fig. 2.
Cases of co-infection between COVID-19 and dengue in Latin America. Only coinfection cases from Latin American countries reported in selected studies were included. Updated September 4, 2021.
3.3. Demographical characteristics and comorbidities
Most coinfections were reported in adults aged 24 to 79 [[23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41]]; the youngest patient was a 13-year-old boy [29]. Approximately twice as many men as women were reported to be coinfected (Male: Female: 2: 1) [[23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41]]. The most frequent comorbidities in coinfected patients were hypertension, obesity, and diabetes [25,31,32,34,35,37,38] (Table 4, Table 5).
3.4. Clinical manifestations and laboratory findings
The medical records of 152 cases were extracted [[23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41]]. Fever and dyspnea were the most frequent findings [[24], [25], [26], [27], [28], [29],[31], [32], [33], [34], [35], [36], [37], [38], [39],41]. Other clinical manifestations were odynophagia, adynamia, myalgia, arthralgia, vomiting, and diarrhoea (Table 4, Table 5).
The most frequently reported laboratory findings were thrombocytopenia, leukopenia, high C-reactive protein, and leukocytosis [[23], [24], [25], [26],28,29,[31], [32], [33], [34], [35], [36], [37], [38], [39],41]. Other less frequently reported laboratory findings were elevated D-dimer, lymphopenia, reduced haemoglobin, elevated serum aspartate aminotransferase and alanine aminotransferase, monocytosis, and high erythrocyte sedimentation rate (Table 4, Table 5).
3.5. Imaging, complications, and outcomes
Chest x-ray and CT images are reported with the following characteristics: Diffuse focal opacities in both lung fields, consistent with the ground glass pattern [26,29,32,36,37,39]; Two studies report signs of pulmonary venous hypertension, confirmed acute pulmonary thromboembolism of multiple bilateral lobular and bilateral segmental branches [25,31].
It was reported in the selected studies that the patients after clinical improvement [27,28,33,35,36,41] were discharged 1 to 24 days after the start of the symptoms with 18 days of hospitalization [24], 1 case at six days of hospitalization [26], 1 case at seven days of hospitalization [32], 1 case at five days of diagnosis and 5 of hospitalization [29], 1 case at 21 days of hospitalization and discharged afterwards [23], 2 cases 6 days after hospitalization [25]. Finally, patients who died at five days [31] are reported, 14 of 28 patients who died [38] and one case died at 63 days post-hospitalization (Table 4, Table 5).
4. Discussion
As is well known, dengue is the most important arboviral disease in terms of morbidity and mortality worldwide, especially in highly endemic areas of Latin America and South-East Asia. However, its diagnosis may be challenging as it may overlap clinically with many other febrile syndrome causes since 2020, including COVID-19.
In the present systematic review, our main objective was to determine the epidemiological situation of cases of COVID-19 and dengue coinfection in Latin America. Knowledge of the clinical and laboratory characteristics of SARS-CoV-2 and dengue virus coinfection is essential for correct diagnosis and patient management [42].
SARS-CoV-2 and dengue virus (DENV) have different entry points, but both diseases cause a systemic infection and share several clinical signs, including fever, headache, myalgia, and gastrointestinal problems [43]. While severe COVID-19 is characterized by the development of micro and macrothrombi, dengue is typically associated with a predisposition to bleed [44]. In addition to the initial clinical presentation similarities, there are also commonalities between the two conditions, including endothelial dysfunction, cytokine storms, risk factors for the development of severe illness, and multi-organ failure. Both infections are characterized by a proinflammatory immune response and a delayed and impaired type I IFN response [45]. COVID-19 and Dengue share common pathogenic routes that have been explored in recent publications [46].
Latin America has been severely affected since the beginning of the pandemic. Endemic infectious diseases such as dengue, coupled with economic and public health disparities, increased the challenge of overcoming a simultaneous pandemic [47]. This review found that tropical countries reported COVID-19 and dengue coinfection with different clinical conditions. In Ecuador [48], Peru [49], Colombia [50], and Brazil [19], among others in the region, circulation of both diseases has been reported with a potential underreporting of dengue due to the prioritization of COVID-19 control with greater emphasis on the first waves.
In this sense, the strict COVID-19 protection measures were associated with a decreased risk of dengue incidence, so coinfection reporting could be lower, especially in countries where dengue is endemic [51]. In our review, myalgia and fever were the most common symptoms, while thrombocytopenia was the most reported laboratory finding. However, it is challenging to distinguish febrile dengue fever from COVID-19 as they share clinical and laboratory findings [52]. So, then, in endemic zones, as well as in patients returning from dengue-endemic areas, this arboviral disease should be not only a differential diagnosis with COVID-19 but also coinfection is a possibility that should be carefully assessed, especially in patients with risk factors, that may contribute in the evolution to severe disease, associated with both viral infections, that may progress and require management at the intensive care unit, and even lead to death.
In addition, we found heterogeneous diagnostic methods for dengue, which could intervene in an accurate diagnosis of coinfection from the onset of symptoms. Diagnostic suspicion of coinfection is sometimes made several days after the first day of admission [53]. Identification of travel to endemic areas, contact with infected family members, and clinical progression provides medical personnel with increased suspicion. However, the lack of molecular diagnosis and dengue overlap make accurate coinfection diagnosis difficult [54]. Ideally, both infections should be laboratory diagnosed by RT-PCR, or at least with antigen detection tests, as antibody-based tests may yield false-positive results due to cross-reactivity.
Mortality from dengue is known to be lower than from COVID-19. However, this review found that hospitalization was necessary for most patients. At the same time, a case report in Colombia [25] and a retrospective study in Peru [38] reported the death of one and fourteen patients, respectively, and other deaths are now sporadically associated with this coinfection. That could be attributed to the high prevalence of pulmonary, cardiovascular, and chronic renal diseases, which have been extensively discussed in previous literature, especially in COVID-19 [55].
5. Conclusions
Coinfection with SARS-CoV-2 and dengue virus is associated with worse outcomes with significant morbidity and mortality, although further studies should assess this in more detail [8,42]. The similar clinical and laboratory features of each infection are a challenge in accurately diagnosing and treating cases. Establishing an early diagnosis could be the answer to reducing the estimated significant burden of these conditions.
6. Recommendations
Diagnosing co-infection between dengue and COVID-19 can be difficult because the symptoms of dengue are nonspecific and may coincide with those of covid-19 or other diseases. Public education campaigns are very important because patients who know the main symptoms of the disease will be able to go to health centers for early diagnosis. Eradication of Aedes aegypti, effective solid waste disposal, and the development of water storage technologies are the best ways to stop the spread of the dengue virus [56].
In addition, it is recommended to develop care procedures for the clinical management of patients in endemic areas, including dengue and COVID-19 testing for all patients with reported fever. Finally, increase funding to combat endemic infectious diseases. It is important to have a fixed budget for dengue treatment and to ensure that district authorities use these funds effectively [57].
Funding
This research received no external funding.
Institutional review board statement
Not applicable.
Informed consent statement
Not applicable.
Data availability statement
This section provides details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study.
CRediT authorship contribution statement
Darwin A. León-Figueroa: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing. Sebastian Abanto-Urbano: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing. Mely Olarte-Durand: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing. Janeth N. Nuñez-Lupaca: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing. Joshuan J. Barboza: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing. D. Katterine Bonilla-Aldana: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing. Robinson A. Yrene-Cubas: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing. Alfonso J. Rodriguez-Morales: Conceptualization, Methodology, Software, Data curation, Writing – original draft, preparation, Visualization, Investigation, Supervision, Validation, Writing – review & editing.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgements
Many thanks to Carlos S. Mamani-García and Dayanne S. Salas-Idme, for their support in the initial versions of the research work.
Contributor Information
Darwin A. León-Figueroa, Email: dalefi19@gmail.com.
Sebastian Abanto-Urbano, Email: sebastianabanto22@gmail.com.
Mely Olarte-Durand, Email: melyolarte@upeu.edu.pe.
Janeth N. Nuñez-Lupaca, Email: jnunezl@unjbg.edu.pe.
Joshuan J. Barboza, Email: jbarbozameca@relaped.com.
D. Katterine Bonilla-Aldana, Email: dbonilla@continental.edu.pe.
Robinson A. Yrene-Cubas, Email: robinalcubas21@gmail.com.
Alfonso J. Rodriguez-Morales, Email: ajrodriguezmmd@gmail.com.
References
- 1.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91. doi: 10.1016/J.JARE.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsang H.F., Wing L., Chan C., Chi W., Cho S., Chi A., et al. An update on COVID-19 pandemic: the epidemiology, pathogenesis, prevention and treatment strategies. Expert Rev Anti Infect Ther. 2021;19:877–888. doi: 10.1080/14787210.2021.1863146. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez-Morales A.J., León-Figueroa D.A., Romaní L., McHugh T.D., Leblebicioglu H. Vaccination of children against COVID-19: the experience in Latin America. Ann Clin Microbiol Antimicrob. 2022;21:1–5. doi: 10.1186/S12941-022-00505-7/FIGURES/1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J., Huang D.Q., Zou B., Yang H., Hui W.Z., Rui F., et al. Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors and outcomes. J Med Virol. 2021;93:1449–1458. doi: 10.1002/JMV.26424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Platto S., Wang Y., Zhou J., Carafoli E. History of the COVID-19 pandemic: origin, explosion, worldwide spreading. Biochem Biophys Res Commun. 2021;538:14–23. doi: 10.1016/J.BBRC.2020.10.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morens D.M., Breman J.G., Calisher C.H., Doherty P.C., Hahn B.H., Keusch G.T., et al. The origin of COVID-19 and why it matters. Am J Trop Med Hyg. 2020;103:955. doi: 10.4269/AJTMH.20-0849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lotfi M., Hamblin M.R., Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254–266. doi: 10.1016/J.CCA.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsheten T., Clements A.C.A., Gray D.J., Adhikary R.K., Wangdi K. Clinical features and outcomes of COVID-19 and dengue co-infection: a systematic review. BMC Infect Dis. 2021;21 doi: 10.1186/S12879-021-06409-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hemmer C.J., Geerdes-Fenge H.F., Reisinger E.C. [COVID-19: epidemiology and clinical facts] Radiologe. 2020;60:893–898. doi: 10.1007/S00117-020-00741-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO Coronavirus (COVID-19) dashboard | WHO Coronavirus (COVID-19) dashboard with vaccination data n.d. https://covid19.who.int/?mapFilter=cases (accessed May 24, 2022).
- 11.Dengue and severe dengue n.d. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue(accessed May 24, 2022).
- 12.Roy S.K., Bhattacharjee S. Dengue virus: epidemiology, biology, and disease aetiology. Can J Microbiol. 2021;67:687–702. doi: 10.1139/CJM-2020-0572. [DOI] [PubMed] [Google Scholar]
- 13.Raafat N., Blacksell S.D., Maude R.J. A review of dengue diagnostics and implications for surveillance and control. Trans R Soc Trop Med Hyg. 2019;113:653. doi: 10.1093/TRSTMH/TRZ068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jayarajah U., Lahiru M., de Zoysa I., Seneviratne S.L. Dengue infections and the surgical patient. Am J Trop Med Hyg. 2021;104:52. doi: 10.4269/AJTMH.20-0983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harapan H., Ryan M., Yohan B., Abidin R.S., Nainu F., Rakib A., et al. Covid-19 and dengue: double punches for dengue-endemic countries in Asia. Rev Med Virol. 2021;31 doi: 10.1002/RMV.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ridwan R. COVID-19 and dengue: a deadly duo. Trop Doct. 2020;50:270–272. doi: 10.1177/0049475520936874. [DOI] [PubMed] [Google Scholar]
- 17.Panda P.K., Sharawat I.K. COVID-19 and/with dengue infection: a curse in an overburdened healthcare system. Trop Doct. 2021;51:106–108. doi: 10.1177/0049475520975945. [DOI] [PubMed] [Google Scholar]
- 18.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lorenz C., Azevedo T.S., Chiaravalloti-Neto F. COVID-19 and dengue fever: a dangerous combination for the health system in Brazil. Travel Med Infect Dis. 2020;35 doi: 10.1016/J.TMAID.2020.101659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-Qushayri A.E., Kamel A.M.A., Reda A., Ghozy S. Does dengue and COVID-19 co-infection have worse outcomes? A systematic review of current evidence. Rev Med Virol. 2022 doi: 10.1002/RMV.2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/BMJ.N71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ouzzani M., Hammady H., Fedorowicz Z., Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5 doi: 10.1186/S13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krueger M.B., Montenegro R.C., de Araújo Coimbra P.P., de Queiroz Lemos L., Fiorenza R.M., da Silva Fernandes C.J., et al. A wide spectrum of neurological manifestations in pediatrics patients with the COVID-19 infection: a case series. J Neurovirol. 2021;27:782–786. doi: 10.1007/S13365-021-01004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reyes-Ruiz J.M., Campuzano-Vences R., Osuna-Ramos J.F., de Jesus-González L.A., Pérez-Méndez M.J., González-González C., et al. Case report: extrapulmonary manifestations of COVID-19 and dengue coinfection. Am J Trop Med Hyg. 2021;105:363–397. doi: 10.4269/AJTMH.21-0177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agudelo Rojas O.L., Tello-Cajiao M.E., Rosso F. Challenges of dengue and coronavirus disease 2019 coinfection: two case reports. J Med Case Rep. 2021:15. doi: 10.1186/S13256-021-02973-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bicudo N., Bicudo E., Costa J.D., Castro J.A.L.P., Barra G.B. Co-infection of SARS-CoV-2 and dengue virus: a clinical challenge. Braz J Infect Dis. 2020;24:452–454. doi: 10.1016/J.BJID.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pontes R.L., de Brito B.B., da Silva F.A.F., Figueredo M.S., Correia T.M.L., Teixeira A.F., et al. Coinfection by SARS-CoV-2 and dengue virus in a dual viral circulation setting. Travel Med Infect Dis. 2020;37 doi: 10.1016/J.TMAID.2020.101862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salvo C.P., di Lella N., López F.S., Hugo J., Zito J.G., Vilela A. [Dengue and SARS-CoV-2 coinfection in an HIV positive patient] Medicina (B Aires) 2020;80(Suppl. 6):94–96. [PubMed] [Google Scholar]
- 29.Nakandakari Gomez M.D., Marín-Macedo H., Seminario-Vilca R. Dengue with signs of alarm and Leptospirosis in a pediatric patient with COVID-19. Revista de La Facultad de Medicina Humana. 2021;21:24. doi: 10.25176/RFMH.v21i2.3459. [DOI] [Google Scholar]
- 30.Rosso F., Parra-Lara L.G., Agudelo-Rojas O.L., Martinez-Ruiz D.M. Differentiating dengue from COVID-19: comparison of cases in Colombia. Am J Trop Med Hyg. 2021;105:745–750. doi: 10.4269/AJTMH.20-0912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Estofolete C.F., Machado L.F., Zini N., Luckemeyer G.D., Moraes M.M., dos Santos T.M.I.L., et al. Presentation of fatal stroke due to SARS-CoV-2 and dengue virus coinfection. J Med Virol. 2021;93:1770–1775. doi: 10.1002/JMV.26476. [DOI] [PubMed] [Google Scholar]
- 32.Villamil-Gómez W.E., Rojas-Torres I., Perea-Vásquez L.E., Collazos-Torres L.A., Murillo-Moreno M.A., Morales-Rudas J.D., et al. SARS-CoV-2 and Dengue virus co-infection: a case from North Caribbean Colombia. Travel Med Infect Dis. 2021;43 doi: 10.1016/J.TMAID.2021.102096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Radisic M.V., Piro M.A., Mori I., Rotryng F., Santamarina J.F. SARS-CoV-2 and dengue virus Co-infection. A case report. Infez Med. 2020;28:416–419. [PubMed] [Google Scholar]
- 34.Quental K.N., Leite A.L., Feitosa A do N.A., Oliveira ZNPde, Tavares Lv de S., Tavares WG. de S., et al. SARS-CoV-2 co-infection with dengue virus in Brazil: a potential case of viral transmission by a health care provider to household members. Travel Med Infect Dis. 2021;40 doi: 10.1016/J.TMAID.2021.101975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schulte H.L., Brito-Sousa J.D., Lacerda M.V.G., Naves L.A., de Gois, et al. Fernandes M.S., et al. SARS-CoV-2/DENV co-infection: a series of cases from the Federal District, Midwestern Brazil. BMC Infect Dis. 2021;21 doi: 10.1186/S12879-021-06456-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valdés González J.L., Valdés González E.M., Solis Cartas U., Sigcho Romero S.F. Dengue, COVID-19 and gout, an uncommon association. Revista Cubana de Reumatología. 2020:22. [Google Scholar]
- 37.Carosella L.M., Pryluka D., Maranzana A., Barcan L., Cuini R., Freuler C., et al. Characteristics of patients Co-infected with severe acute respiratory syndrome coronavirus 2 and dengue virus, buenos Aires, Argentina, march-June 2020. Emerg Infect Dis. 2021;27 doi: 10.3201/EID2702.203439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mejía-Parra J.L., Aguilar-Martinez S., Fernández-Mogollón J.L., Luna C., Bonilla-Aldana D.K., Rodriguez-Morales A.J., et al. Characteristics of patients coinfected with severe acute respiratory syndrome coronavirus 2 and dengue virus, lambayeque, Peru, may-August 2020: a retrospective analysis. Travel Med Infect Dis. 2021;43 doi: 10.1016/J.TMAID.2021.102132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Teotônio I.M.S.N., de Carvalho J.L., Castro L.C., Nitz N., Hagström L., Rios G.G., et al. Clinical and biochemical parameters of COVID-19 patients with prior or active dengue fever. Acta Trop. 2021;214 doi: 10.1016/J.ACTATROPICA.2020.105782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stringari L.L., de Souza M.N., de Medeiros Junior N.F., Goulart J.P., Giuberti C., Dietze R., et al. Covert cases of severe acute respiratory syndrome coronavirus 2: an obscure but present danger in regions endemic for dengue and chikungunya viruses. PLoS One. 2021;16 doi: 10.1371/JOURNAL.PONE.0244937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosso M.v., Clemant T., Quiroga C.A.F., García S., Mulinaris E.O. SARS-CoV-2 and dengue virus coinfection involving the skin of an Argentinian female. Int J Womens Dermatol. 2021;7:824–825. doi: 10.1016/J.IJWD.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.El-Qushayri A.E., Kamel A.M.A., Reda A., Ghozy S. Does dengue and COVID-19 co-infection have worse outcomes? A systematic review of current evidence. Rev Med Virol. 2022 doi: 10.1002/RMV.2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khatri G., Hasan M.M., Shaikh S., Mir S.L., Sahito A.M., Priya, et al. The simultaneous crises of dengue and COVID-19 in Pakistan: a double hazard for the country’s debilitated healthcare system. Trop Med Health. 2022;50:1–5. doi: 10.1186/S41182-022-00410-X/METRICS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.El-Qushayri A.E., Kamel A.M.A., Reda A., Ghozy S. Does dengue and COVID-19 co-infection have worse outcomes? A systematic review of current evidence. Rev Med Virol. 2022;32 doi: 10.1002/RMV.2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Malavige G.N., Jeewandara C., Ogg G.S. Dengue and COVID-19: two sides of the same coin. J Biomed Sci. 2022;29 doi: 10.1186/S12929-022-00833-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harapan H., Ryan M., Yohan B., Abidin R.S., Nainu F., Rakib A., et al. Covid-19 and dengue: double punches for dengue-endemic countries in Asia. Rev Med Virol. 2021;31:e2161. doi: 10.1002/RMV.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nacher M., Douine M., Gaillet M., Flamand C., Rousset D., Rousseau C., et al. Simultaneous dengue and COVID-19 epidemics: difficult days ahead? PLoS Negl Trop Dis. 2020;14:1–8. doi: 10.1371/JOURNAL.PNTD.0008426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Navarro J.C., Arrivillaga-Henríquez J., Salazar-Loor J., Rodriguez-Morales A.J. COVID-19 and dengue, co-epidemics in Ecuador and other countries in Latin America: pushing strained health care systems over the edge. Travel Med Infect Dis. 2020;37 doi: 10.1016/J.TMAID.2020.101656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Plasencia-Dueñas R., Failoc-Rojas V.E., Rodriguez-Morales A.J. Impact of the COVID-19 pandemic on the incidence of dengue fever in Peru. J Med Virol. 2022;94:393–398. doi: 10.1002/JMV.27298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cardona-Ospina J.A., Arteaga-Livias K., Villamil-Gómez W.E., Pérez-Díaz C.E., Katterine Bonilla-Aldana D., Mondragon-Cardona Á., et al. Dengue and COVID-19, overlapping epidemics? An analysis from Colombia. J Med Virol. 2021;93:522–527. doi: 10.1002/JMV.26194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen Y., Li N., Lourenço J., Wang L., Cazelles B., Dong L., et al. Measuring the effects of COVID-19-related disruption on dengue transmission in southeast Asia and Latin America: a statistical modelling study. Lancet Infect Dis. 2022;22:657–667. doi: 10.1016/S1473-3099(22)00025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.da Rosa Mesquita R., Francelino Silva Junior L.C., Santos Santana F.M., Farias de Oliveira T., Campos Alcântara R., Monteiro Arnozo G., et al. Clinical manifestations of COVID-19 in the general population: systematic review. Wien Klin Wochenschr. 2021;133:377–382. doi: 10.1007/S00508-020-01760-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Feldman C., Anderson R. vol. 13. Nathan); 2021. (The role of co-infections and secondary infections in patients with COVID-19. Pneumonia). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramos-Castañeda J., Barreto dos Santos F., Martínez-Vega R., Galvão de Araujo J.M., Joint G., Sarti E. Dengue in Latin America: systematic review of molecular epidemiological trends. PLoS Negl Trop Dis. 2017;11 doi: 10.1371/JOURNAL.PNTD.0005224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Macias A.E., Werneck G.L., Castro R., Mascareñas C., Coudeville L., Morley D., et al. Mortality among hospitalized dengue patients with comorbidities in Mexico, Brazil, and Colombia. Am J Trop Med Hyg. 2021;105:102–109. doi: 10.4269/AJTMH.20-1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hasan M.M., Hernández-Yépez P.J., de los Angeles Rivera-Cabrera M., Sarkar A., dos Santos Costa A.C., Essar M.Y. Concurrent epidemics of dengue and COVID-19 in Peru: which way forward? The Lancet Regional Health - Americas. 2022;12 doi: 10.1016/j.lana.2022.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Plasencia-Dueñas R., Failoc-Rojas V.E., Rodriguez-Morales A.J. Impact of the COVID-19 pandemic on the incidence of dengue fever in Peru. J Med Virol. 2022;94:393–398. doi: 10.1002/JMV.27298. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This section provides details regarding where data supporting reported results can be found, including links to publicly archived datasets analyzed or generated during the study.