Abstract
Background
This meta-analysis and systematic review aimed to evaluate the global prevalence and risk factors of mental problems (i.e., depression, anxiety, stress, sleep disorder, posttraumatic stress disorder (PTSD), burnout, psychological distress, and suicidal ideation) among medical students during the COVID-19 pandemic.
Method
We searched PubMed, Embase, Web of Science, psycARTICLES, PsycINFO, CNKI, and Wan Fang for studies on the prevalence of mental problems among medical students from January 1, 2020, to April 1, 2022. The pooled prevalence was calculated by random-effect models. We performed a narrative review to identify the risk factors.
Results
The meta-analysis included 201 studies (N = 198,000). The prevalence of depression (41 %, 95 % CI, 37–45 %,), anxiety (38 %,95 % CI, 34 %–42 %), stress (34 %, 95 % CI, 27 %–42 %), sleep disorder (52 %, 95 % CI, 44 %–60 %), psychological distress (58 %, 95 % CI, 51 %–65 %), PTSD (34 %, 95 % CI, 22 %–46 %), suicidal ideation (15 %, 95 % CI, 11 %–18 %) and burnout (38 %, 95 % CI, 25 %–50 %) was high. The major risk factors were being female, being junior or preclinical students, exposure to COVID-19, academic stress, psychiatric or physical disorders history, economic trouble, fear of education impairment, online learning trouble, fear of infection, loneliness, low physical activity, low social support, problematic internet or smartphone use, and young age.
Limitations
Most studies were cross-sectional. Few studies provided a reasonable response rate, suggesting potential selection bias.
Conclusions
The study demonstrated a high prevalence and risk factors for mental problems during COVID-19, calling for mental health services. Our findings are valuable for college and health authorities to identify high-risk students and provide targeted intervention.
Keywords: Medical students, COVID-19, Mental health, Meta-analysis
1. Introduction
The outbreak of the coronavirus disease 2019 (COVID-19) has caused profound and long-lasting psychological harm (Kunzler et al., 2021; Prati and Mancini, 2021; Wu et al., 2021b). Medical students were found to be extremely vulnerable to the mental problems during the pandemic, which might result from the high risk of infection, significant lifestyle change, strict confinement, and disturbance in education program (Eleftheriou et al., 2021). Studies demonstrated a high prevalence of depression, anxiety, and sleep disorder among medical students worldwide during the pandemic (Cao et al., 2020; Chandratre, 2020; Eleftheriou et al., 2021; Kuman Tunçel et al., 2021; Leroy et al., 2021; Yuan et al., 2021). In addition, the common mental problems might lead to their attrition from the medicine learning (Deng et al., 2021a; Khalafallah et al., 2021; Peng et al., 2022; Wang et al., 2020; Yang et al., 2022b), suggesting the urgent need to screen mental problems and explore their risk factors among medical students.
To date, most of the studies among medical students were limited by small sample size and reported varied prevalence and possible associated factors. So far, only a few reviews on the mental health of medical students during this pandemic were available (Chandratre, 2020; Lasheras et al., 2020; Mittal et al., 2021; Vythilingam and Atiomo, 2021). Nevertheless, those reviews focused on certain mental problems (depression or anxiety) and most of the included studies were from the very early phase of the pandemic. More importantly, the risk factors of those symptoms were rarely reviewed. A more comprehensive review which assesses a broader range of mental problems and their risk factors in medical students shall provide more valuable insights for university, hospital, and health policymakers to identify at-risk students and to provide timely mental intervention.
Hence, we conducted the present systemic review and meta-analysis of the prevalence and risk factors of mental problems among medical students. Our study aims to evaluate the global prevalence and risk factors of several mental problems (i.e., depression symptoms, anxiety symptoms, burnout, sleep disorder, high perceived stress, PTSD, psychological distress, burnout, and suicidal ideation) among medical students during the COVID-19 pandemic.
2. Method
The systematic review and meta-analysis was performed according to Preferred Reporting Items For Systematic Reviews and Meta-analyses (PRISMA) guidelines (Moher et al., 2009), and the checklist could be found in Table S1. The study was registered in PROSPERO (CRD42022306025).
2.1. Search strategy
Two independent researchers, Qiuxia Wu and Pu Peng, searched the following database: PubMed, Embase, Web of Science, psycARTICLES, PsycINFO, CNKI, and Wan Fang. All the publications from 01 January 2020 to 01 April 2022 will be researched without country and language restrictions. We did the first search in Feb 2022, and updated them on 01 April 2022. Reference lists of all selected articles will independently be screened to identify additional studies left out in the initial search. Detailed search strategies were provided in Supplementary materials Table S2.
2.2. Selection criteria
All abstracts and full-text were independently reviewed by two researchers: Pu Peng and Qiuxia Wu. Any disagreement will be dissolved by discussion until reaching consensus or by consulting Tieqiao Liu.
To be included in the meta-analysis, the studies should (i) assess a group of medical students (ii) provide the prevalence of mental problems or the prevalence could be calculated according to the article; (iii) determine the prevalence of that mental problem using validated instruments and questionnaires, and (iv) be carried out at least 1 week after the onset of COVID-19 in the specific country where the study was conducted. Studies that included medical students as a subgroup will also be included when detailed information on the prevalence of mental problems of medical students was provided. The exclusion criteria were: (i) failed to provide any aggregate prevalence of mental problems in the medical students group; (ii) had included nursing, dentistry, or pharmacy students as part of the medical student group and did not provide enough data to calculate the prevalence of mental problems in medical students (iii) were not accessible for full review; (iv) all interventional studies, editorials, case reports, case series, meeting abstracts and commentaries; (v) were carried out before the breakout of COVID-19 or failed to provide the study setting, and (vi) the number of participants was <50.
For the narrative review of associated factors of mental problems, studies should meet the additional criteria that they performed appropriate statistical methods (i.e., multiple or single-factor regression model, chi-square test, Student's t-test, Pearson's/Spearman's correlation test, and Wilcoxon Rank-Sum test) to evaluate the possible associated factors. When the studies provided both multiple and single-factor regression, we only included the results of multiple regression.
2.3. Data extraction
Two authors (Pu Peng and Qiuxia Wu) did the literature search and quality assessment independently and completed a data extraction form: author, study design, geographic location; study time, sample characteristics (age, gender, size), study period (during the lockdown or out of the lockdown), measurement tools (the questionnaires and cutoff points, for example), reported prevalence estimates (the number of cases and the total participants), risk factors of that mental problems, and quality assessment. For studies assessing the prevalence of mental problems at multiple time points, only the latest data was extracted. When multiple studies were found reporting on the same population cohort, only the study reporting the most informative and complete data was chosen. We contacted the corresponding authors to gain the information when necessary.
2.4. Quality assessment
A modified version of the Newcastle-Ottawa Quality Assessment Scale (NOS) was used to evaluate the quality of literature (Rotenstein et al., 2016). Five dimensions include sample size, representativeness, response rate, valid assessment of mental problems, and strong statistic methods. Details of the scoring system could be found in Table S3. A score lower than three represented a high risk of bias.
2.5. Data synthesis and statistical analyses
We performed the statistical analyses on R foundation (Version 4.0.2). The main outcome was the pooled prevalence and 95 % confidence intervals (CI) of mental problems (depressive symptoms, anxiety symptoms, high stress, sleep disorder, burnout, psychological distress, suicidal ideation, and PTSD). Random effect models were performed due to the high heterogeneity between studies. The publication bias was evaluated by funnel plot and egger's test, with a p > 0.05 showing low public bias. We assessed the heterogeneity by I2 statistic, and an I2 > 75 % indicated a high heterogeneity. Subgroup analysis and meta-regression were performed to identify the source of heterogeneity including study time, COVID-19 period, study location, measurement tools, and study quality. Subgroup analysis was conducted when k ≥ 10 with a cell size of k > 3 for each categorical comparison.
3. Result
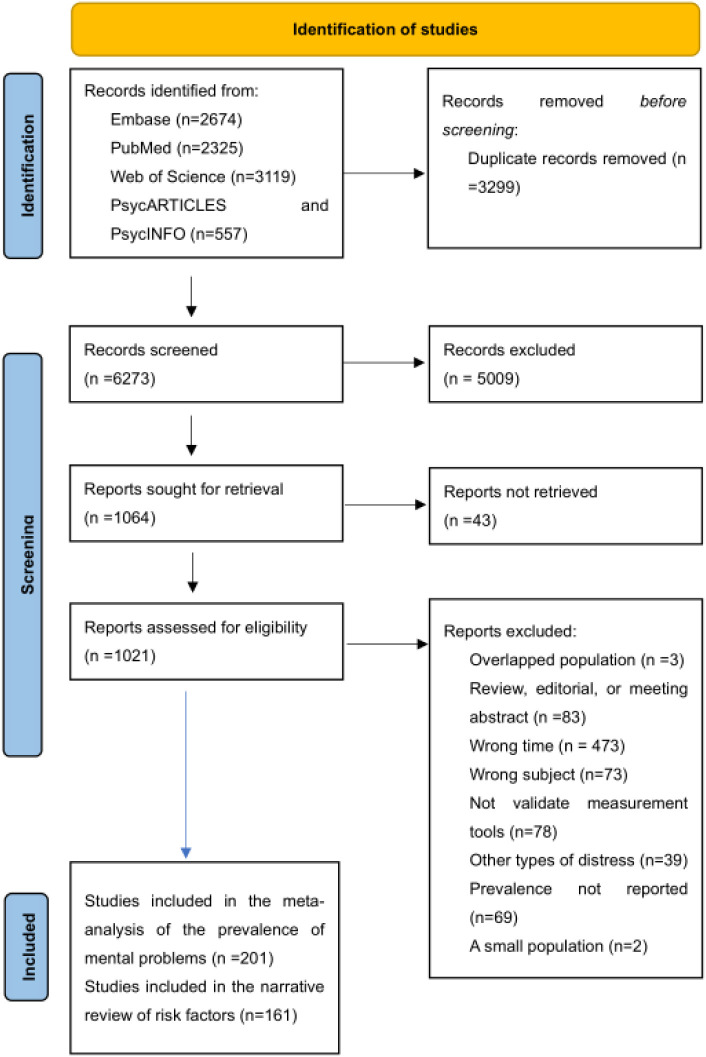
As illustrated in the flow diagram (Fig. 1 ), 6273 records were screened after removing duplicates. 1021 studies were read in full text to include studies that met the inclusion criteria. 201 studies were included in the meta-analysis. The study reference, geographic location, study time, sample characteristics (age, gender, size), study period (during the lockdown or out of the lockdown), measurement tools, and prevalence of mental problems were provided in Table S2.
Fig. 1.
PRISMA workflow of identification of studies.
3.1. Study characters
A total of 201 studies regarding 198,000 medical students were included in this study. Of them, the prevalence of a wide range of mental problems was assessed including depression (in 116 studies), anxiety (in 125 studies), high perceived stress (in 43 studies), sleep problems (in 34 studies), psychological distress (in 25 studies), PTSD (in 13 studies), suicidal ideation (in 13 studies) and burnout (in 13 studies).
Most of the studies were from Asia (72, 35.8 %) and East Asia (72, 35.8 %), followed by Europe (24, 11.9 %), South America (11, 5.4 %), North America (10, 5 %), and Africa (9, 4.4 %). Only one study was carried out in Australia and two studies recruited participants from diverse geographical regions. Nearly half of the studies were carried out during the nationwide COVID-19 lockdown, while 85 (42.3 %) studies were in the post-lockdown period. 24 studies were carried out before lockdown or did not report enough information to identify. 162 studies were carried out during 2020, and 24 studies were carried out in 2021. 15 studies did not report the exact time point. The majority of the studies (193 in 201) were cross-sectional, and 8 studies were longitudinal or repeat cross-sectional.
3.2. Pooled prevalence of mental health problems
The pooled prevalence of depression (41 %, 95 % CI, 37–45 %), anxiety (38 %,95 % CI, 34 %–42 %), stress (34 %, 95 % CI, 27 %–42 %), sleep disorder (52 %, 95 % CI, 44 %–60 %), psychological distress (58 %, 95 % CI, 51 %–65 %), PTSD (34 %, 95 % CI, 22 %–46 %), suicidal ideation (15 %, 95 % CI, 11 %–18 %) and burnout (38 %, 95 % CI, 25 %–50 %) are summarized in Table 1 . 81 studies investigated the moderate or severe depression, yielding a pooled prevalence of 27 % (95 % CI, 22 %–31 %). The pooled prevalence of moderate or severe anxiety was 24 % (95 % CI, 20 %–29 %). There was high heterogeneity between studies, with I2 ranging from 98.5 %–100 %. The forest plot of each mental health problem was found in Figs. S1–8.
Table 1.
Pooled prevalence, heterogeneity, and publication bias.
| Distress | Studies | Cases | N | Prevalence | 95 % CI | I2 | p-Value1 |
|---|---|---|---|---|---|---|---|
| Depression | |||||||
| Overall depression | 116 | 43,557 | 126,044 | 41 % | 37 %–45 % | 99.9 % | 0.052 |
| Mild and above | 89 | 33,264 | 93,310 | 43 % | 39 %–48 % | 99.8 % | |
| Moderate and severe | 81 | 19,735 | 82,418 | 27 % | 22 %–31 % | 99.9 % | |
| Anxiety | |||||||
| Overall anxiety | 125 | 46,755 | 155,291 | 38 % | 34 %–42 % | 100 % | <0.001 |
| Mild and above | 103 | 38,819 | 122,966 | 39 % | 34 %–43 % | 100 % | |
| Moderate and severe | 89 | 18,488 | 107,648 | 24 % | 20 %–29 % | 100 % | |
| Stress | 43 | 9102 | 34,231 | 34 % | 27 %–42 % | 99.9 % | 0.932 |
| Sleep disorder | 34 | 10,945 | 20,661 | 52 % | 44 %–60 % | 99.7 % | 0.002 |
| PTSD | 13 | 3231 | 17,622 | 34 % | 22 %–46 % | 99.5 % | 0.001 |
| Distress | 25 | 8146 | 15,195 | 58 % | 51 %–65 % | 99.2 % | 0.178 |
| Suicidal ideation | 13 | 3857 | 26,708 | 15 % | 11 %–18 % | 98.7 % | 0.219 |
| Burnout | 13 | 8089 | 17,577 | 38 % | 25 %–50 % | 99.8 % | 0.928 |
p-Value for egger's test, with a p > 0.05 suggested no publication bias.
3.3. Publication bias
Egger's test indicated that there was no publication bias in the prevalence of depression, stress, psychological distress, suicidal ideation, and burnout (All p > 0.05). However, egger's test suggested a significant publication bias in anxiety, sleep disorder, and PTSD. The funnel plot of each mental health problem was provided in Fig. S9.
3.4. Meta-regression
Meta-regression suggested a rising prevalence of depression and anxiety symptoms over time. For every 1-month increase, a 1.14 % increase in the prevalence of depression (k = 108; rate = 0.0142, 95 % CI: 0.0032, 0.0206; p = 0.0071) and a 1.17 % increase in anxiety (k = 117; rate = 0.0117, 95 % CI: 0.0020, 0.0214; p = 0.018). The regression model bubble plot was available in Fig. S9. No association of study time with other mental health problems was found.
3.5. Subgroup analysis
We performed a subgroup analysis of the prevalence of mental symptoms based on lockdown period, study quality, study location, and measurement tools (Table 2 ). Subgroup difference between groups was only conducted in subgroups with a cell size of k > 3, and the full results could be found in Table S5. We found no association between the lockdown period and the prevalence of all mental health problems. Studies with a high risk of bias demonstrated a significantly higher prevalence of anxiety symptoms (44 % vs 34 %, p = 0.033) than studies with a low risk of bias, while such association did not exist in other mental health problems. The subgroup analysis revealed that study location was the major resource of heterogeneity of depression (p < 0.001), anxiety (p < 0.001), and distress (p = 0.041), with studies from East Asia demonstrating a lower prevalence. Moreover, a similar trend was observed in sleep disorder (p = 0.204) and stress (p = 0.102). Measurement tools were the main moderators of the prevalence of depression (p = 0.016), anxiety (p < 0.001), sleep disorder (p < 0.001), and PTSD (p = 0.009). However, we found no such relationship in the prevalence of stress (p = 0.913), and psychological distress (p = 0.488). The forest plot of each subgroup for mental health symptoms was available in Figs. S10–18.
Table 2.
Subgroup analysis of mental health problems.
| Symptom | Subgroup | k | Prevalence | LLCI | ULCI | I2 | p1 |
|---|---|---|---|---|---|---|---|
| Depression | Lockdown | 0.917 | |||||
| After lockdown | 47 | 0.41 | 0.35 | 0.47 | 1 | ||
| Lockdown | 59 | 0.41 | 0.35 | 0.47 | 1 | ||
| Area | <0.001 | ||||||
| Africa | 6 | 0.66 | 0.51 | 0.81 | 0.99 | ||
| Asia | 36 | 0.49 | 0.41 | 0.57 | 1 | ||
| East Asia | 47 | 0.29 | 0.24 | 0.33 | 1 | ||
| Europe | 12 | 0.43 | 0.31 | 0.54 | 1 | ||
| North America | 6 | 0.41 | 0.28 | 0.54 | 0.99 | ||
| South America | 7 | 0.54 | 0.4 | 0.68 | 0.99 | ||
| Quality | 0.511 | ||||||
| High risk of bias | 34 | 0.39 | 0.32 | 0.46 | 1 | ||
| Low risk of bias | 82 | 0.42 | 0.37 | 0.47 | 1 | ||
| Scale | 0.016 | ||||||
| BDI or BDI-2 | 10 | 0.38 | 0.31 | 0.46 | 0.99 | ||
| DASS-21 | 25 | 0.40 | 0.30 | 0.50 | 1 | ||
| HADS | 4 | 0.41 | 0.21 | 0.62 | 1 | ||
| PHQ2 | 4 | 0.27 | 0.17 | 0.37 | 0.93 | ||
| PHQ9 or PHQ8 | 55 | 0.46 | 0.40 | 0.52 | 1 | ||
| SDS | 13 | 0.32 | 0.22 | 0.41 | 0.99 | ||
| Anxiety | Lockdown | 0.376 | |||||
| After lockdown | 44 | 0.39 | 0.33 | 0.46 | 1 | ||
| Lockdown | 71 | 0.36 | 0.30 | 0.41 | 1 | ||
| Area | <0.001 | ||||||
| Africa | 5 | 0.58 | 0.51 | 0.65 | 0.98 | ||
| Asia | 40 | 0.46 | 0.38 | 0.54 | 1 | ||
| East Asia | 53 | 0.23 | 0.19 | 0.27 | 0.99 | ||
| Europe | 11 | 0.42 | 0.30 | 0.55 | 0.99 | ||
| North America | 7 | 0.61 | 0.48 | 0.74 | 1 | ||
| South America | 8 | 0.54 | 0.45 | 0.63 | 0.94 | ||
| Quality | 0.033 | ||||||
| High risk of bias | 42 | 0.44 | 0.36 | 0.52 | 1 | ||
| Low risk of bias | 83 | 0.34 | 0.30 | 0.39 | 1 | ||
| Scale | <0.001 | ||||||
| BAI | 4 | 0.40 | 0.27 | 0.53 | 0.98 | ||
| DASS-21 | 26 | 0.39 | 0.30 | 0.48 | 1 | ||
| GAD2 | 4 | 0.34 | 0.21 | 0.47 | 0.96 | ||
| GAD7 | 64 | 0.42 | 0.36 | 0.48 | 1 | ||
| HADS | 5 | 0.50 | 0.34 | 0.65 | 0.99 | ||
| SAS | 16 | 0.16 | 0.10 | 0.22 | 0.99 | ||
| STAI | 5 | 0.40 | 0.19 | 0.60 | 0.98 | ||
| Stress | Lockdown | 0.265 | |||||
| After lockdown | 14 | 0.32 | 0.19 | 0.45 | 0.99 | ||
| Lockdown | 25 | 0.37 | 0.27 | 0.48 | 1 | ||
| Area | 0.102 | ||||||
| Asia | 19 | 0.35 | 0.23 | 0.47 | 1 | ||
| East Asia | 15 | 0.23 | 0.16 | 0.31 | 1 | ||
| Europe | 4 | 0.49 | 0.18 | 0.80 | 0.99 | ||
| Quality | 0.216 | ||||||
| High risk of bias | 14 | 0.42 | 0.26 | 0.59 | 1 | ||
| Low risk of bias | 29 | 0.31 | 0.23 | 0.38 | 1 | ||
| Scales | 0.792 | ||||||
| DASS-21 | 24 | 0.32 | 0.21 | 0.43 | 1 | ||
| PSS-10 | 13 | 0.38 | 0.23 | 0.52 | 0.99 | ||
| PSS-14 | 6 | 0.37 | 0.28 | 0.45 | 0.98 | ||
| Sleep disorder | Lockdown | 0.602 | |||||
| After lockdown | 18 | 0.55 | 0.45 | 0.65 | 1 | ||
| Lockdown | 14 | 0.51 | 0.39 | 0.63 | 1 | ||
| Area | 0.204 | ||||||
| Asia | 14 | 0.53 | 0.44 | 0.61 | 0.98 | ||
| East Asia | 12 | 0.41 | 0.26 | 0.56 | 1 | ||
| Quality | 0.345 | ||||||
| High risk of bias | 12 | 0.58 | 0.41 | 0.75 | 1 | ||
| Low risk of bias | 22 | 0.49 | 0.42 | 0.56 | 0.99 | ||
| Scale | 0.029 | ||||||
| ISI | 5 | 0.38 | 0.24 | 0.52 | 0.99 | ||
| PSQI | 21 | 0.57 | 0.47 | 0.67 | 1 | ||
| Distress | Lockdown | 0.625 | |||||
| After lockdown | 12 | 0.58 | 0.48 | 0.69 | 0.99 | ||
| Lockdown | 9 | 0.54 | 0.42 | 0.68 | 0.99 | ||
| Area | 0.041 | ||||||
| Asia | 11 | 0.64 | 0.53 | 0.74 | 0.99 | ||
| East Asia | 4 | 0.38 | 0.16 | 0.60 | 0.98 | ||
| Quality | 0.849 | ||||||
| High risk of bias | 6 | 0.60 | 0.43 | 0.76 | 0.98 | ||
| Low risk of bias | 19 | 0.58 | 0.50 | 0.66 | 0.99 | ||
| Scale | 0.417 | ||||||
| GHQ12 | 7 | 0.62 | 0.53 | 0.72 | 0.97 | ||
| K10 | 9 | 0.64 | 0.51 | 0.77 | 0.99 | ||
| K6 | 5 | 0.51 | 0.32 | 0.70 | 0.99 | ||
| SQR20 | 4 | 0.48 | 0.28 | 0.68 | 0.98 | ||
| PTSD | Lockdown | 0.887 | |||||
| After lockdown | 4 | 0.32 | 0.04 | 0.61 | 1 | ||
| Lockdown | 6 | 0.35 | 0.16 | 0.54 | 1 | ||
| Quality | 0.880 | ||||||
| High risk of bias | 3 | 0.33 | 0.06 | 0.60 | 1 | ||
| Low risk of bias | 10 | 0.35 | 0.21 | 0.49 | 1 | ||
| Scale | 0.009 | ||||||
| IES-R | 9 | 0.42 | 0.28 | 0.56 | 0.99 | ||
| PCL-5 | 4 | 0.18 | 0.05 | 0.30 | 0.99 | ||
| Quality | 0.736 | ||||||
| High risk of bias | 4 | 0.40 | 0.24 | 0.56 | 0.95 | ||
| Low risk of bias | 9 | 0.36 | 0.20 | 0.53 | 1 | ||
| Area | 0.055 | ||||||
| Asia | 6 | 0.29 | 0.09 | 0.50 | 0.99 | ||
| Europe | 6 | 0.51 | 0.42 | 0.60 | 0.99 | ||
| Suicidal ideation | Lockdown | 0.772 | |||||
| After lockdown | 8 | 0.15 | 0.11 | 0.20 | 0.96 | ||
| Lockdown | 4 | 0.14 | 0.06 | 0.21 | 0.99 | ||
| Area | 0.418 | ||||||
| East Asia | 4 | 0.12 | 0.06 | 0.19 | 0.99 | ||
| Europe | 4 | 0.16 | 0.11 | 0.20 | 0.94 |
Abbreviation: BAI Beck Anxiety Inventory, BDI Beck Depression Inventory, BDI(–II) Beck Depression Inventory(–II), DASS-21 Depression Anxiety Stress Scale-21, GAD-2(–7) Generalized Anxiety Disorder Scale-2(/–7), HADS Hospital Anxiety and Depression Scale, IES-R Impact of Event Scale-Revised, ISI Insomnia Severity Index, K-6(/–10) Kessler Psychological Distress Scale-6(/–10), NA not available, PCL-5 Post-traumatic Stress Disorder Checklist-5, PHQ-2(/–8/–9) Patient Health Questionnaire-2(/–8/–9/), PSQI Pittsburgh Sleep Quality Index, PSS–10(–14) Perceived Stress Scale–10(–14), SAS Self-Rating Anxiety Scale, SDS Self-Rating Depression Scale, SRQ-20 20-item Self-Report Questionnaire, STAI-Y State Trait Anxiety Inventory-Y, GHQ12 General health questionnaire-12.
p<0.05 indicated significant difference between the subrgoups.
3.6. Factors associated with mental health symptoms
161 studies were included in the narrative review of factors associated with mental health symptoms. We categorized these factors in terms of “Sociodemographic factor” (such as gender, age, and “household income”) “Education factor” (such as education level, preclinical or clinical, academic performance, disruption of education, and online education), “COVID-19 factor” (such as fear of COVID-19 infection, relatives infected COVID-19, and lived in a high-epidemic COVID-19 area), “Physiological factor” (such as a history of mental disorder), “Lifestyle factor” (such as physical activity, internet addiction, and diet.), “Physiological and health factor” (such as a history of disease or current health status), “Relational factor” (such as family relationship, friendship, and loneliness) and “Predictors of response to trauma” based on the Furber's theory with some modification (Furber et al., 2017).
Table 3 summarized the most frequently reported associated factors. The major risk factors for mental symptoms were being female (in 62 studies), being preclinical students (in 31 studies), being in a high-epidemic COVID-19 area or having relatives infected with COVID-19 (in 26 studies), having low academic performance or heavy academic burden (in 19 studies), with psychiatric disorders history (in 18 studies), economic instability (in 14 studies), fear of education or career impairment (in 12 studies), difficulties with online learning (in 14 studies), fear of COVID-19 infection (in 12 studies), with physical illness or bad somatic health (in 11 studies), living alone or loneliness (in 12 studies), low physical activity (in 10 studies), low social support (in 10 studies), smartphone addiction or extreme screen time (in 10 studies), and young age (in 11 studies). However, there were inconsistent results across the literature. Nine studies demonstrated that male was more prone to mental problems than female. Six studies reported a positive association between age and the incidence of mental problems. Moreover, for the study period, seven studies showed that clinical students had a higher mental health burden than preclinical students.
Table 3.
Most frequently reported risk factors for mental health symptomsa.
Factors which were reported as statistically significant associated factors in at least k = 3 studies were defined as frequently reported associated factors.
Junior students refer to 1st year or 2nd year medical students.
Senior students refer to 4th year or 5th year medical students.
Compared with undergraduate students.
4. Discussion
The present meta-analysis is composed of 201 studies. It assesses the global prevalence and risk factors of various mental symptoms among medical students during the COVID-19 pandemic, including depression, anxiety, high perceived stress, sleep disorder, psychological distress, PTSD, burnout, and suicidal ideation. This is the largest meta-analysis on that topic. Our study demonstrates a heavy mental burden among medical students worldwide during this period and highlights risk factors for mental symptoms at a variety of levels. Our findings are valuable for university and health policy makers to early detect and provide targeted interventions for mental problems in medical students.
Our study demonstrated the profound and long-lasting psychological impact of COVID-19 on medical students. There was an extreme high prevalence of depression (41 %, 95 % CI, 37–45 %,), anxiety (38 %, 95 % CI, 34 %–42 %), stress (34 %, 95 % CI, 27 %–42 %), sleep disorder (52 %, 95 % CI, 44 %–60 %), psychological distress (58 %, 95 % CI, 51 %–65 %), PTSD (34 %, 95 % CI, 22 %–46 %), suicidal ideation (15 %, 95 % CI, 11 %–18 %) and burnout (38 %, 95 % CI, 25 %–50 %) among medical students during the pandemic period. The prevalence of depression, anxiety, suicidal ideation, and psychological distress was higher than that before the COVID-19 pandemic (Hope and Henderson, 2014; Quek et al., 2019; Rotenstein et al., 2016). However, the prevalence of sleep disorder or burnout was similar to that before the COVID-19 pandemic (Frajerman et al., 2019; Rao et al., 2020). Moreover, when compared with studies on the general public during the COVID-19 pandemic, our study demonstrated a much higher prevalence of depression, anxiety, distress, sleep disorder, and PTSD (de Sousa et al., 2021; Jahrami et al., 2022; Yunitri et al., 2022).
Based on the subgroup analysis and meta-regression, our study indicated a slight increase in the prevalence of all symptoms except stress and PTSD during the post-lockdown period. However, the changes were not significant. Besides, we found a positive association between the time of data collection and the prevalence of depression and anxiety. Those findings suggest that COVID-19 might be continuing to affect psychological health even long after the initial or peak point. This hypothesis was supported by numerous longitudinal studies which found increasing mental distress among the general population over time (Ausín et al., 2022; Kok et al., 2022; MacDonald et al., 2022). Taken together, our study suggested the mental problems might persist in the late stage of this pandemic. Therefore, it is critical that medical schools and hospitals screen medical students for common mental problems when medical students returned back.
In line with similar meta-analyses in other populations, our study found that studies in East Asia reported the lowest prevalence of mental symptoms (Deng et al., 2021b; Zhu et al., 2021), which might result from effective epidemic disease control. Various studies showed that the severity of the epidemic was positively associated with unhealthy mental status (Essangri et al., 2021; Lee et al., 2021; Lu et al., 2022). Most studies in East Asia were carried out in China, which was the very first country hit by COVID-19 but managed to control it in three months.
Our study has identified several high-risk groups that deserved more attention. Despite several inconsistent results, most studies found female medical students were at a higher risk for mental problems, which was in line with previous studies in different populations (Balakrishnan et al., 2022; Kunzler et al., 2021; Sheldon et al., 2021). There might be several explanations. First, epidemiological studies demonstrated that females could be more suspectable to mental distress even before the pandemic (Lim et al., 2018). The gender difference in mental distress might be maintained during the pandemic. Second, studies suggested that females might have severer health anxiety, which might lead to worse mental health during the pandemic (Bleichhardt and Hiller, 2007; Solomou and Constantinidou, 2020). Another important risk factor for mental problems was being preclinical or junior students. Interestingly, studies on non-medical students reported similar results, finding junior students were more prone to mental distress (Wathelet et al., 2020). Junior or preclinical students were at the early stage of their medical education. They might have difficulties in adjusting to the stressful medicine learning and the new online learning mode during the pandemic (Çimen et al., 2021). Several studies also suggest junior students might experience more academic stress than senior students during the pandemic (Hakami et al., 2021), which might result in mental problems. Our study also demonstrated low social support and bad family relationship were positively associated with mental distress, which might be explained by the lockdown policy. During the home quarantine, medical students had to live with their family members for a long time. Hence, low social support and bad family relationship might lead to conflicts, which caused mental problems (Wu et al., 2021a). Other important risk factors included economic trouble, pre-existing mental or physical illness, and COVID-19 infection or exposure, which was consistent with studies in other populations (Yuan et al., 2022). Further qualitative interviews in those high-risk students are needed to determine how these factors impacted the mental health of the medical students.
Moreover, our study indicated many modifiable risk factors for mental symptoms, hence targeted intervention could be applied. For example, fear of COVID-19 infection (Bilgi et al., 2021; Gruba et al., 2021; Kuman Tunçel et al., 2021; Safa et al., 2021; Saraswathi et al., 2020; Simic et al., 2021; Teixeira et al., 2021; Wang et al., 2021, Wang et al., 2020; Wu et al., 2020) and little health literacy (Gao et al., 2021; Jindal et al., 2020; Muhammad Alfareed Zafar et al., 2020; Xie et al., 2021; Ye et al., 2020; Zhong et al., 2021) was found negatively associated with mental health. Therefore, more education on the knowledge of the prevention and control of COVID-19 might help reduce the mental burden. Dissatisfaction with online learning and fear of education impairment due to COVID-19 was other risk factor for mental symptoms (Abdulghani et al., 2020; AlJhani et al., 2021; Chang et al., 2021; Forycka et al., 2022; Nikas et al., 2022; Nishimura et al., 2021; Pelissier et al., 2021; Potapova et al., 2021; Teixeira et al., 2021; Wang et al., 2021; Zhao et al., 2021). Difficulties in following online learning, communicating with teachers, and developing practical skills are major concerns of medical students (Forycka et al., 2022; Pelissier et al., 2021; Jin et al., 2021). Those findings highlighted the need for medical colleges to gather students' opinions on the present online learning mode and made timely adjustments. Besides, growing studies showed unhealthy lifestyles (i.e., low physical activities (Cardoso et al., 2022; Mendes et al., 2021; Menon et al., 2021; Saguem et al., 2021; Souza et al., 2021; Toubasi et al., 2021; Xiao et al., 2021; Zhang et al., 2021c)), increasing substance use (Capdevila-Gaudens et al., 2021; Cardoso et al., 2022; Gao et al., 2021; Pelissier et al., 2021; Safarini et al., 2021; Saguem et al., 2021), irregular diet and sleep (Gao et al., 2021; Mishra et al., 2021; Shafique et al., 2021; Teixeira et al., 2021; Xiao et al., 2020, Xiao et al., 2021; Zhang et al., 2021c), and problematic smartphone and internet use (Biswas et al., 2021; Dhamija et al., 2021; Goweda et al., 2020; Milasauskiene et al., 2021; Mishra et al., 2021; Tahir et al., 2021; Telgote et al., 2021; Xie et al., 2021; Zhang et al., 2021a) was an emerging risk factor for mental problems, which were less frequently discussed among medical students before the pandemic. The rapid lifestyle change might result from the stay-at-home policy during this period (Colley et al., 2020; Li et al., 2021; Tison et al., 2020). Further studies are in need to determine whether lifestyle modification, such as exercise at home, will help protect students from mental symptoms.
5. Strength and limitation
The present study has several substantial strengths. First, to our knowledge, this study is the first meta-analysis and systemic review that assessed the prevalence and risk factors for mental problems in medical students in the context of the COVID-19 pandemic. By including a broader range of mental problems (depression, anxiety, stress, sleep problem, PTSD, burnout, psychological distress, burnout, and suicidal ideation), our study provided a more comprehensive description of mental problems in this population. Second, we applied the validated risk categorization scheme, which provided a detailed taxonomy of risk factors for mental problems. In addition to risk factors that were consistently reported in previous findings in the general population, our study also identified a unique set of risk factors, which was closely related to the medicine learning process such as being preclinical students, low academic performance, fear of education impairment, online learning trouble, and decreased willingness in medicine learning. In addition, most of the risk factors we identified were reversible, which could be promising targets for the prevention and intervention of psychological distress in medical students. Taken together, our findings could help hospitals, universities, and health policymakers to identify groups of medical students at risk of poor mental health and to make timely modifications.
Our results should be interpreted with the following limitation. First, there is a high heterogeneity between studies, which might come from the varied study design and measurement tools. The subgroup analysis and meta-regression didn't account for the total heterogeneity. Second, as most of the studies included were cross-sectional, we could not establish a causal relationship between mental symptoms and risk factors. Moreover, the inconsistency of those risk factors across literature might affect the accuracy of our results. Besides, the lack of longitudinal studies limited us to track the trajectory of these symptoms. Third, only one study adapted diagnosed interviews to identify major depression disorder (Rolland et al., 2022b). Most studies used a self-rating scale which might reduce the accuracy of the study. Fourth, there might be a large selection bias as only a few studies gave a reasonable response rate. Also, most of the studies were web-based and applied convenience sampling, which limited the representativeness of the participants. Fifth, although our meta-analysis included all available research up to date and provided the most comprehensive analysis of the prevalence and risk factors for mental problems during the COVID-19 period, most of those studies were carried out during the first year of COVID-19 and were limited to the first wave. More studies regarding the mental problems during the recurrent waves or remission period of the COVID-19 pandemic are in need. Taken together, more longitudinal, multicenter studies with large sample sizes and validated measurement tools are in need to track the dynamics of those mental symptoms.
6. Conclusion and relevance
Our study demonstrated an extremely high prevalence of mental symptoms during the COVID-19 pandemic and identified multiple risk factors. These findings call for timely mental screening and intervention for medical students. The revealed risk factors are valuable for schools, health systems, and policymakers to identify high-risk subgroups of medical students and provide targeted intervention, as most of the risk factors we found in this study are reversible.
CRediT authorship contribution statement
QX Wu, P Peng, TQ Liu contributed to study design, article search, review and quality assessment. Q Yang, MY Li, and X Wang reviewed the study protocol and contributed to the data collection. P Peng, HY He, YZ Hao, and QX Wu contributed to the drafting of the manuscript. SB Chen, YF Wang, and YH Liu designed the statistical analysis strategy and performed statistical analyses. All authors contributed to the critical revision of the paper and have agreed to be accountable for all aspects of the work.
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgments
Acknowledgments
None.
Financial disclosure
This study was supported by the Provincial Natural Science Foundation of Hunan (Grant No. 2020JJ4795 to TQ Liu). The funders had no influence on study design, analysis or decision to publish.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.10.040.
Appendix A. Supplementary data
Supplementary material
References
- Abdulghani H.M., Sattar K., Ahmad T., Akram A. Association of COVID-19 pandemic with undergraduate medical students’ perceived stress and coping. Psychol. Res. Behav. Manag. 2020;13:871–881. doi: 10.2147/prbm.S276938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AbuDujain N.M., Almuhaideb Q.A., Alrumaihi N.A., Alrabiah M.A., Alanazy M.H., Abdulghani H. The impact of the COVID-19 pandemic on medical interns’ education, training, and mental health: a cross-sectional study. Cureus. 2021;13 doi: 10.7759/cureus.19250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adhikari A., Sujakhu E., Sandervee G.C., Zoowa S.B. Depression among medical students of a medical college in Nepal during covid-19 pandemic: a descriptive cross-sectional study. J. Nepal Med. Assoc. 2021;59:645–648. doi: 10.31729/jnma.5441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aftab M., Abadi A.M., Nahar S., Ahmed R.A., Mahmood S.E., Madaan M., Ahmad A. COVID-19 pandemic affects the medical students’ learning process and assaults their psychological wellbeing. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18115792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Hasani I.D., Salih H.S., Abdul Wahid A.T., Jabarah M. The impact of social support on students’ behavior in the context of iraqi medical education. Open Access Macedonian J. Med. Sci. 2021;9:1553–1559. doi: 10.3889/oamjms.2021.7688. [DOI] [Google Scholar]
- Ali A., Mahnoor S., Ahmed S., Naseem S., Shah S.W., Shehryar S. COVID-19 online teaching and its impact on psychological health in higher education: a cross sectional study on medical students of 1st 2nd and 3rd year MBBS. J. Res. Med. Dental Sci. 2020;8:275–279. [Google Scholar]
- AlJhani S., Alateeq D., Alwabili A., Alamro A. Mental health and online learning among medical students during the COVID-19 pandemic: a saudi national study. J. Mental Health Train. Educ. Pract. 2021 doi: 10.1108/jmhtep-04-2021-0037. [DOI] [Google Scholar]
- Alkhamees A.A., Alaqil N.S., Alsoghayer A.S., Alharbi B.A. Prevalence and determinants of burnout syndrome and depression among medical students at qassim university, Saudi Arabia. Saudi Med. J. 2020;41:1375–1380. doi: 10.15537/smj.2020.12.25427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkwai H.M. Graduating from medical school amid a pandemic: a study of graduates’ mental health and concerns. Educ. Res. Int. 2021;2021 doi: 10.1155/2021/8854587. [DOI] [Google Scholar]
- Allah A.A., Algethami N.E., Algethami R.A., RH A.LAyyubi, Altalhi W.A., Atalla A.A.A. Impact of COVID-19 on psychological and academic performance of medical students in Saudi Arabia. J. Fam. Med. Prim. Care. 2021;10:3857–3862. doi: 10.4103/jfmpc.jfmpc_1004_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alotiby A., Almaghrabi M., Alosaimy R., Alharthi A., Khawandanah B., Alansari R., Basahal A., Zamil G. Learning environment quality for medical students at umm Al-Qura University: a comprehensive study on stressors, sources, and solutions after introduction of a new bachelor of medicine and bachelor of surgery (MBBS) curriculum. Adv. Med. Educ. Pract. 2021;12:1487–1497. doi: 10.2147/amep.S343792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alrashed F.A., Sattar K., Ahmad T., Akram A., Karim S.I., Alsubiheen A.M. Prevalence of insomnia and related psychological factors with coping strategies among medical students in clinical years during the COVID-19 pandemic. Saudi J. Biol. Sci. 2021;28:6508–6514. doi: 10.1016/j.sjbs.2021.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshammari K.F., Alassaf O.M., Alomaim H.Y., Alnais I.A., Alswayda S.H. Prevalence of low back pain and its relation to stress and study hours among medical students in University of Hail in Saudi Arabia. Med. Sci. 2021;25:432–439. [Google Scholar]
- Atta I.S., Almilaibary A. The prevalence of stress among medical students studying an integrative curriculum during the COVID-19 pandemic. Adv. Med. Educ. Pract. 2022;13:35–45. doi: 10.2147/amep.S345330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ausín B., González-Sanguino C., Castellanos M.A., Sáiz J., Zamorano S., Vaquero C., Muñoz M. The psychological impact of the COVID-19 pandemic in Spain: a longitudinal study. Psicothema. 2022;34:66–73. doi: 10.7334/psicothema2021.290. [DOI] [PubMed] [Google Scholar]
- Balakrishnan V., Ng K.S., Kaur W., Govaichelvan K., Lee Z.L. COVID-19 depression and its risk factors in Asia Pacific - a systematic review and meta-analysis. J. Affect. Disord. 2022;298:47–56. doi: 10.1016/j.jad.2021.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilgi K., Aytaş G., Karatoprak U., Kazancıoǧlu R., Özçelik S. The effects of coronavirus disease 2019 outbreak on medical students. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.637946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas M., Hasan M.T., Samir N., Alin S.I., Homaira N., Hassan M.Z., Khatun M.R., Anjum A., Hossain S., Koly K.N., Safa F., Alam S.F., Rafi M.A., Osman Biswas M.A.A., Yasmin F., Podder V., Trisa T.I., Azad D.T., Nodi R.N., Ashraf F., Akther S.M.Q., Ahmed H.U. The prevalence and associated factors of depressive symptoms among medical students in Bangladesh during the COVID-19 pandemic: a cross-sectional pilot study. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.811345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleichhardt G., Hiller W. Hypochondriasis and health anxiety in the German population. Br. J. Health Psychol. 2007;12:511–523. doi: 10.1348/135910706X146034. [DOI] [PubMed] [Google Scholar]
- Bolatov A.K., Seisembekov T.Z., Askarova A.Z., Baikanova R.K., Smailova D.S., Fabbro E. Online-learning due to COVID-19 improved mental health among medical students. Med. Sci. Educ. 2020;31:1–10. doi: 10.1007/s40670-020-01165-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Büssing A., Lindeberg A., Stock-Schröer B., Martin D., Scheffer C., Bachmann H.S. Motivations and experiences of volunteering medical students in the COVID-19 pandemic-results of a survey in Germany. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.768341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capdevila-Gaudens P., Miguel García-Abajo J., Flores-Funes D., García-Barbero M., García-Estañ J. Depression, anxiety, burnout and empathy among spanish medical students. PLoS One. 2021;16 doi: 10.1371/journal.pone.0260359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardoso A.C.C., Quintanilha L.F., Barbosa L.A.de O., Avena K.de M. Prevalence of common mental disorders among medical students during the Covid-19 pandemic. Revista Brasileira de Educação Médica. 2022;46:e006. doi: 10.1590/1981-5271v46.1-20210242.ing. [DOI] [Google Scholar]
- Chan C.K., Yin Lam T., Seevalingam K.K., Rajandram R., Kuppusamy S. The impact of recurrent waves of COVID-19 on the mental health of medical students: a cross-sectional study. Asia Pac. J. Public Health. 2022 doi: 10.1177/10105395221077061. 10105395221077060. [DOI] [PubMed] [Google Scholar]
- Chandratre S. Medical students and COVID-19: challenges and supportive strategies. J. Med. Educ. Curric. Dev. 2020;7 doi: 10.1177/2382120520935059. 2382120520935059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang W.W., Shi L.X., Zhang L., Jin Y.L., Yu J.G. The mental health status and associated factors among medical students engaged in online learning at home during the pandemic: a cross-sectional study from China. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.755503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chootong R., Sono S., Choomalee K., Wiwattanaworaset P., Phusawat N., Wanghirankul N., Laojaroensuk P., Thongkhundum P., Saetang R., Euanontat S., Anantathaweekul S. The association between physical activity and prevalence of anxiety and depression in medical students during COVID-19 pandemic: a cross-sectional study. Ann. Med. Surg. (Lond.) 2022;75 doi: 10.1016/j.amsu.2022.103408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çimen İ.D., Alvur T.M., Coşkun B., Şükür N. Mental health of Turkish medical students during the COVID-19 pandemic. Int. J. Soc. Psychiatry. 2021 doi: 10.1177/00207640211066734. 207640211066734. [DOI] [PubMed] [Google Scholar]
- Cockburn J.G., Tan C.Y., Poh D., Tan D.J., Foong C.C., Hong W.H. Mental health and self-determination profiles of the diverse population of medical students in Malaysia during the COVID-19 pandemic. BMC Psychol. 2022;10:49. doi: 10.1186/s40359-022-00759-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colley R.C., Bushnik T., Langlois K. Exercise and screen time during the COVID-19 pandemic. Health Rep. 2020;31:3–11. doi: 10.25318/82-003-x202000600001-eng. [DOI] [PubMed] [Google Scholar]
- Crisol-Deza D., Poma-Ramírez D., Pacherres-López A., Noriega-Baella C., Villanueva-Zúñiga L., Salvador-Carrillo J., Huarcaya-Victoria J. Factors associated with suicidal ideation among medical students during the initial phase of the COVID-19 pandemic in Peru: a multicenter study. Death Stud. 2022;1–9 doi: 10.1080/07481187.2022.2042752. [DOI] [PubMed] [Google Scholar]
- Cuschieri S., Calleja Agius J. Spotlight on the shift to remote anatomical teaching during COVID-19 pandemic: perspectives and experiences from the University of Malta. Anat. Sci. Educ. 2020;13:671–679. doi: 10.1002/ase.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahanayake D., Rajapakse H., Wickramasinghe A., Chandradasa M., Rohanachandra Y., Perera S., Nillo A.M., Molodynski A. Psychological wellbeing and mental health amongst medical undergraduates: a descriptive study assessing more than 1,000 medical students in Sri Lanka. Int. J. Soc. Psychiatry. 2021 doi: 10.1177/00207640211027211. 207640211027211. [DOI] [PubMed] [Google Scholar]
- de Sousa G.M., de Meiroz Grilo M.L.P., Coelho M.L.G., de Lima-Araújo G.L., Schuch F.B., Galvão-Coelho N.L., Tavares V.D.de O. Mental health in COVID-19 pandemic: a meta-review of prevalence meta-analyses. Front. Psychol. 2021;12:703838. doi: 10.3389/fpsyg.2021.703838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng J., Que J., Wu S., Zhang Y., Liu J., Chen S., Wu Y., Gong Y., Sun S., Yuan K., Bao Y., Ran M., Shi J., Wing Y.K., Shi L., Lu L. Effects of COVID-19 on career and specialty choices among chinese medical students. Med. Educ. Online. 2021;26:1913785. doi: 10.1080/10872981.2021.1913785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Jiawen, Zhou F., Hou W., Silver Z., Wong C.Y., Chang O., Drakos A., Zuo Q.K., Huang E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 2021;301 doi: 10.1016/j.psychres.2021.113863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhamija S., Shailaja B., Chaudhari B., Chaudhury S., Saldanha D. Prevalence of smartphone addiction and its relation with sleep disturbance and low self- esteem among medical college students. Ind. Psychiatry J. 2021;30:S189–s194. doi: 10.4103/0972-6748.328813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domínguez-González A.D., Guzmán-Valdivia G., Ángeles-Téllez F.S., Manjarrez-Ángeles M.A., Secín-Diep R. Depression and suicidal ideation in Mexican medical students during COVID-19 outbreak. A longitudinal study. Heliyon. 2022;8 doi: 10.1016/j.heliyon.2022.e08851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan H., Gong M., Zhang Q., Huang X., Wan B. Research on sleep status, body mass index, anxiety and depression of college students during the post-pandemic era in Wuhan, China. J. Affect. Disord. 2022;301:189–192. doi: 10.1016/j.jad.2022.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwivedi D., Kaur N., Shukla S., Gandhi A., Tripathi S. Perception of stress among medical undergraduate during coronavirus disease-19 pandemic on exposure to online teaching. Natl. J. Physiol. Pharm. Pharmacol. 2020;10:657–662. doi: 10.5455/njppp.2020.10.05107202009052020. [DOI] [Google Scholar]
- Ecker A., Berenson A.B., Gonzalez S.J., Zoorob R., Hirth J.M. Depression among medical students in the United States during the COVID-19 pandemic: the role of communication between universities and their students. Disast. Med. Public Health Prep. 2022;1–21 doi: 10.1017/dmp.2022.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eid M.M., Alsufiany M.B., Alshehri F.H., Wazna N.I., Alzahrani H., Ahmed R.M., Faizo N.L., El-Gendy A.M., Abdelbasset W.K., Eladl H.M. Psychological impact of COVID-19 pandemic on university students: a cross-sectional study. Med. Sci. 2021;25:964–972. [Google Scholar]
- Eleftheriou A., Rokou A., Arvaniti A., Nena E., Steiropoulos P. Sleep quality and mental health of medical students in Greece during the COVID-19 pandemic. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.775374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhadi M., Buzreg A., Bouhuwaish A., Khaled A., Alhadi A., Msherghi A., Alsoufi A., Alameen H., Biala M., Elgherwi A., Elkhafeefi F., Elmabrouk A., Abdulmalik A., Alhaddad S., Elgzairi M., Khaled A. Psychological impact of the civil war and COVID-19 on Libyan medical students: a cross-sectional study. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.570435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esmat S., Attia A., Elhabashi E. Prevalence and predictors for depression among medical students during coronavirus disease-19 pandemic: a cross-sectional study. Open Access Macedonian J. Med. Sci. 2021;9:1454–1460. doi: 10.3889/oamjms.2021.7390. [DOI] [Google Scholar]
- Essadek A., Gressier F., Robin M., Shadili G., Bastien L., Peronnet J.C., Falissard B., Rabeyron T. Mental health of medical students during the COVID19: impact of studies years. J. Affect Disord. Rep. 2022;100318 doi: 10.1016/j.jadr.2022.100318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essangri H., Sabir M., Benkabbou A., Majbar M.A., Amrani L., Ghannam A., Lekehal B., Mohsine R., Souadka A. Predictive factors for impaired mental health among medical students during the early stage of the COVID-19 pandemic in Morocco. Am. J. Trop. Med. Hyg. 2021;104:95–102. doi: 10.4269/AJTMH.20-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forycka J., Pawłowicz-Szlarska E., Burczyńska A., Cegielska N., Harendarz K., Nowicki M. Polish medical students facing the pandemic-assessment of resilience, well-being and burnout in the COVID-19 era. PLoS One. 2022;17 doi: 10.1371/journal.pone.0261652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frajerman A., Morvan Y., Krebs M.-O., Gorwood P., Chaumette B. Burnout in medical students before residency: a systematic review and meta-analysis. Eur. Psychiatry. 2019;55:36–42. doi: 10.1016/j.eurpsy.2018.08.006. [DOI] [PubMed] [Google Scholar]
- Furber G., Leach M., Guy S., Segal L. Developing a broad categorisation scheme to describe risk factors for mental illness, for use in prevention policy and planning. Aust. N. Z. J. Psychiatry. 2017;51:230–240. doi: 10.1177/0004867416642844. [DOI] [PubMed] [Google Scholar]
- Gao F., Jiao S.X., Bi Y.Q., Huang Z.Y., Wang P., Zhang B.Y., Fang J., Han R.L., Fan L., Wang M.J., Lv X.L., Li J., Hu Y.X., Zhang M.D., Qiao Q., Zhao X., Li D., Xiao Z.B., Chang F.H., Bai T.Y. The impact of the SARS-COV-2 pandemic on the mental health and employment decisions of medical students in North China. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.641138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goweda R.A., Hassan-Hussein A., Alqahtani M.A., Janaini M.M., Alzahrani A.H., Sindy B.M., Alharbi M.M., Kalantan S.A. Prevalence of sleep disorders among medical students of umm Al-Qura University, Makkah, Kingdom of Saudi Arabia. J. Public Health Res. 2020;9:45–49. doi: 10.4081/jphr.2020.1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruba G., Kasiak P.S., Gębarowska J., Adamczyk N., Sikora Z., Jodczyk A.M., Mamcarz A., Śliż D. Pals study of sleep deprivation and mental health consequences of the covid-19 pandemic among university students: a cross-sectional survey. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18189581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo A.A., Crum M.A., Fowler L.A. Assessing the psychological impacts of covid-19 in undergraduate medical students. Int. J. Environ. Res. Public Health. 2021;18:1–14. doi: 10.3390/ijerph18062952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta P., BK A., Ramakrishna K. Prevalence of depression and anxiety among medical students and house staff during the covid-19 health-care crisis. Academic Psychiatry. 2021 doi: 10.1007/s40596-021-01454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guse J., Heinen I., Mohr S., Bergelt C. Understanding mental burden and factors associated with study worries among undergraduate medical students during the COVID-19 pandemic. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.734264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakami Z., Vishwanathaiah S., Abuzinadah S.H., Alhaddad A.J., Bokhari A.M., Marghalani H.Y.A., Shahin S.Y. Effects of COVID-19 lockdown on the mental health of dental students: a longitudinal study. J. Dent. Educ. 2021;85:1854–1862. doi: 10.1002/jdd.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halperin S.J., Henderson M.N., Prenner S., Grauer J.N. Prevalence of anxiety and depression among medical students during the Covid-19 pandemic: a cross-sectional study. J. Med. Educ. Curric. Dev. 2021;8 doi: 10.1177/2382120521991150. 2382120521991150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassnain S., Ahmad A., Qayyum M.S., Farrukh M.G., Nawaz U.A., Ahmad H. Effects of covid-19 lockdown on mental health of medical students in Lahore, Pakistan. Bangladesh J. Med. Sci. 2021;20:125–130. doi: 10.3329/BJMS.V20I5.55406. [DOI] [Google Scholar]
- Hope V., Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med. Educ. 2014;48:963–979. doi: 10.1111/medu.12512. [DOI] [PubMed] [Google Scholar]
- Huarcaya-Victoria J., Elera-Fitzcarrald C., Crisol-Deza D., Villanueva-Zúñiga L., Pacherres A., Torres A., Huertas G., Calderón D., Noriega-Baella C., Astonitas E., Salvador-Carrillo J. Factors associated with mental health in peruvian medical students during the COVID-19 pandemic: a multicentre quantitative study. Rev. Colomb. Psiquiatr (Engl. Ed.) 2021 doi: 10.1016/j.rcp.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail N., Tajjudin A.I., Jaafar H., Nik Jaafar N.R., Baharudin A., Ibrahim N. The relationship between internet addiction, internet gaming and anxiety among medical students in a malaysian public university during covid-19 pandemic. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph182211870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahrami H.A., Alhaj O.A., Humood A.M., Alenezi A.F., Fekih-Romdhane F., AlRasheed M.M., Saif Z.Q., Bragazzi N.L., Pandi-Perumal S.R., BaHammam A.S., Vitiello M.V. Sleep disturbances during the COVID-19 pandemic: a systematic review, meta-analysis, and meta-regression. Sleep Med. Rev. 2022;62 doi: 10.1016/j.smrv.2022.101591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jindal V., Mittal S., Kaur T., Bansal A.S., Kaur P., Kaur G., Sati H.C., Garg A. Knowledge, anxiety and the use of hydroxychloroquine prophylaxis among health care students and professionals regarding COVID-19 pandemic. Adv. Respir. Med. 2020;88:520–530. doi: 10.5603/ARM.a2020.0163. [DOI] [PubMed] [Google Scholar]
- Khalafallah A.M., Jimenez A.E., Lam S., Gami A., Dornbos D.L., Sivakumar W., Johnson J.N., Mukherjee D. Burnout among medical students interested in neurosurgery during the COVID-19 era. Clin. Neurol. Neurosurg. 2021;210 doi: 10.1016/j.clineuro.2021.106958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurram R., Razzak D.A., Ahmad W., Qamar A., Mumtaz T., Sameed Q.U.A. Mental distress after 1st wave of COVID-19 among medical students. J. Pharm. Res. Int. 2020;32:7–12. doi: 10.9734/JPRI/2020/v32i4431075. [DOI] [Google Scholar]
- Kok A.A.L., Pan K.-Y., Ottenheim N.R., Jörg F., Eikelenboom M., Horsfall M., Luteijn R., van Oppen P., Rhebergen D., Schoevers R.A., Giltay E.J., Penninx B.W.J.H. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in dutch case-control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J. Affect. Disord. 2022;S0165–0327(22) doi: 10.1016/j.jad.2022.02.056. 00205–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolcu G., Başer Kolcu M. Psychological effects of COVID-19 in medical students. Psychiatr. Danub. 2021;33:387–391. [PubMed] [Google Scholar]
- Kostina L., Ibragimov I., Kubekova A., Sergeeva M. Depression and attitudes to depression among students of a russian medical university during the pandemic coronavirus. Archiv. Euromedica. 2021;11:16–19. doi: 10.35630/2199-885x/2021/11/6.3. [DOI] [Google Scholar]
- Kuman Tunçel Ö., Taşbakan S.E., Gökengin D., Erdem H.A., Yamazhan T., Sipahi O.R., Pullukçu H., Önen Sertöz Ö., Işıkgöz Taşbakan M. The deep impact of the COVID-19 pandemic on medical students: an online cross-sectional study evaluating Turkish students' anxiety. Int. J. Clin. Pract. 2021;75 doi: 10.1111/ijcp.14139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Kumar A., Shrama D., Sharma S., Bansal R., Shukla A., Ahmad S. The psychological impact of the covid-19 lockdown on medical students of a college in North India. Indian J. Public Health Res. Dev. 2020;11:82–87. doi: 10.37506/ijphrd.v11i10.11118. [DOI] [Google Scholar]
- Kumar R., Kumar H., Kumari R., Dars J., Qureshi S., Hamza M.A., Khoso A.B., Mubeen S.M. The impact of covid-19 on medical students: a cross sectional survey. Pakistan Journal of Medical and Health Sciences. 2021;15:2905–2908. doi: 10.53350/pjmhs2115112905. [DOI] [Google Scholar]
- Kunzler A.M., Röthke N., Günthner L., Stoffers-Winterling J., Tüscher O., Coenen M., Rehfuess E., Schwarzer G., Binder H., Schmucker C., Meerpohl J.J., Lieb K. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health. 2021;17:34. doi: 10.1186/s12992-021-00670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasheras I., Gracia-García P., Lipnicki D.M., Bueno-Notivol J., López-Antón R., de la Cámara C., Lobo A., Santabárbara J. Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health. 2020;17:E6603. doi: 10.3390/ijerph17186603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.M., Juarez M., Rae G., Jones L., Rodriguez R.M., Davis J.A., Boysen-Osborn M., Kashima K.J., Krane N.K., Kman N., Langsfeld J.M., Harries A.J. Anxiety, PTSD, and stressors in medical students during the initial peak of the COVID-19 pandemic. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leroy A., Wathelet M., Fovet T., Habran E., Granon B., Martignène N., Amad A., Notredame C.E., Vaiva G., D’Hondt F. Mental health among medical, healthcare, and other university students during the first COVID-19 lockdown in France. J. Affect. Disord. Rep. 2021;6 doi: 10.1016/j.jadr.2021.100260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y.-Y., Sun Y., Meng S.-Q., Bao Y.-P., Cheng J.-L., Chang X.-W., Ran M.-S., Sun Y.-K., Kosten T., Strang J., Lu L., Shi J. Internet addiction increases in the general population during COVID-19: evidence from China. Am. J. Addict. 2021;30:389–397. doi: 10.1111/ajad.13156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim G.Y., Tam W.W., Lu Y., Ho C.S., Zhang M.W., Ho R.C. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 2018;8:1–10. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lingyu Z., Jiaying W., Chuying D., Meimei Z., Changjin L., Qi W. Mental health and personality implications among medical students during the outbreak of the COVID-19 pandemic. Social Behavior & Personality: an international journal. 2021;49:1–11. doi: 10.2224/sbp.10544. [DOI] [Google Scholar]
- Liu B., Qiao K., Lu Y. The relationship between perceived stress, state-trait anxiety, and sleep quality among university graduates in China during the COVID-19 pandemic. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.664780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L., Wang X., Wang X., Guo X., Pan B. Association of Covid-19 pandemic-related stress and depressive symptoms among international medical students. BMC Psychiatry. 2022;22 doi: 10.1186/s12888-021-03671-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald J.J., Baxter-King R., Vavreck L., Naeim A., Wenger N., Sepucha K., Stanton A.L. Depressive symptoms and anxiety during the COVID-19 pandemic: large, longitudinal, cross-sectional survey. JMIR Ment Health. 2022;9 doi: 10.2196/33585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes T.B., de Souza K.C., Franca C.N., Rossi F.E., Guimaraes Santos R.P., Duailibi K., Tuleta I., Stubbs B., Neves L.M., Armond J.de E. Physical activity and symptoms of anxiety and depression among medical students during a pandemic. Revista Brasileira De Medicina Do Esporte. 2021;27:582–587. doi: 10.1590/1517-8692202127062021_0059. [DOI] [Google Scholar]
- Meng N., Liu Z., Wang Y., Feng Y., Liu Q., Huang J., Li X. Beyond sociodemographic and COVID-19-related factors: the association between the need for psychological and information support from school and anxiety and depression. Med. Sci. Monit. 2021;27 doi: 10.12659/MSM.929280. e929280-1-e929280-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon B., Sannapareddy S., Menon M. Assessment of severity of stress among medical and dental students during the COVID-19 pandemic. Ann. Indian Acad. Neurol. 2021;24:703–707. doi: 10.4103/aian.AIAN_19_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milasauskiene E., Burkauskas J., Podlipskyte A., Király O., Demetrovics Z., Ambrasas L., Steibliene V. Compulsive internet use scale: psychometric properties and associations with sleeping patterns, mental health, and well-being in lithuanian medical students during the coronavirus disease 2019 pandemic. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.685137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra J., Panigrahi A., Samanta P., Dash K., Mahapatra P., Behera M.R. Sleep quality and associated factors among undergraduate medical students during Covid-19 confinement. Clin. Epidemiol. Glob. Health. 2022;15 doi: 10.1016/j.cegh.2022.101004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra J., Samanta P., Panigrahi A., Dash K., Behera M.R., Das R. Mental health status, coping strategies during covid-19 pandemic among undergraduate students of healthcare profession. Int. J. Ment. Heal. Addict. 2021 doi: 10.1007/s11469-021-00611-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal R., Su L., Jain R. COVID-19 mental health consequences on medical students worldwide. J. Commun. Hosp. Intern. Med. Perspect. 2021;11:296–298. doi: 10.1080/20009666.2021.1918475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moayed M.S., Vahedian-Azimi A., Mirmomeni G., Rahimi-Bashar F., Goharimoghadam K., Pourhoseingholi M.A., Abbasi-Farajzadeh M., Khatibzadeh A., Sathyapalan T., Guest P.C., Sahebkar A. Coronavirus (COVID-19)-associated psychological distress among medical students in Iran. Adv. Exp. Med. Biol. 2021;1321:245–251. doi: 10.1007/978-3-030-59261-5_21. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhammad Alfareed Zafar S., Junaid Tahir M., Malik M., Irfan Malik M., Kamal Akhtar F., Ghazala R. Awareness, anxiety, and depression in healthcare professionals, medical students, and general population of Pakistan during COVID-19 pandemic: a cross sectional online survey. Med J Islam Repub Iran. 2020;34:131. doi: 10.34171/mjiri.34.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakhostin-Ansari A., Sherafati A., Aghajani F., Khonji M., Aghajani R., Shahmansouri N. Depression and anxiety among iranian medical students during COVID-19 pandemic. Iran. J. Psychiatry. 2020;15:228–235. doi: 10.18502/ijps.v15i3.3815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natalia D., Syakurah R.A. Mental health state in medical students during COVID-19 pandemic. J. Educ. Health Promot. 2021;10:208. doi: 10.4103/jehp.jehp_1296_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni J., Wang F., Liu Y., Wu M., Jiang Y., Zhou Y., Zhou Y., Sha D. Psychological impact of the COVID-19 pandemic on chinese health care workers: cross-sectional survey study. JMIR Mental Health. 2021;8 doi: 10.2196/23125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nihmath Nisha S., Francis Y.M., Balaji K., Raghunath G., Kumaresan M. A survey on anxiety and depression level among south indian medical students during the COVID 19 pandemic. Int. J. Res. Pharm. Sci. 2020;11:779–786. doi: 10.26452/ijrps.v11iSPL1.3082. [DOI] [Google Scholar]
- Nikas I.P., Lamnisos D., Meletiou-Mavrotheris M., Themistocleous S.C., Pieridi C., Mytilinaios D.G., Michaelides C., Johnson E.O. Shift to emergency remote preclinical medical education amidst the Covid-19 pandemic: a single-institution study. Anat. Sci. Educ. 2022;15:27–41. doi: 10.1002/ase.2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimura Y., Ochi K., Tokumasu K., Obika M., Hagiya H., Kataoka H., Otsuka F. Impact of the COVID-19 pandemic on the psychological distress of medical students in Japan: cross-sectional survey study. J. Med. Internet Res. 2021;23 doi: 10.2196/25232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedraz-Petrozzi B., Krüger-Malpartida H., Arevalo-Flores M., Salmavides-Cuba F., Anculle-Arauco V., Dancuart-Mendoza M. Emotional impact on health personnel, medical students, and general population samples during the COVID-19 pandemic in Lima, Peru. Rev. Colomb. Psiquiatria. 2021;50:189–198. doi: 10.1016/j.rcp.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelaccia T., Sibilia J., Fels É., Gauer L., Musanda A., Severac F., Abbiati M. And if we had to do it all over again, would we send medical students to the emergency departments during a pandemic? Lessons learned from the COVID-19 outbreak. Intern. Emerg. Med. 2021;16:1967–1974. doi: 10.1007/s11739-020-02629-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelissier C., Viale M., Berthelot P., Poizat B., Massoubre C., Tiffet T., Fontana L. Factors associated with psychological distress in french medical students during the covid-19 health crisis: a cross-sectional study. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph182412951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng P., Yang W.F., Liu Y., Chen S., Wang Y., Yang Q., Wang X., Li M., Wang Y., Hao Y., He L., Wang Q., Zhang J., Ma Y., He H., Zhou Y., Long J., Qi C., Tang Y.Y., Liao Y., Tang J., Wu Q., Liu T. High prevalence and risk factors of dropout intention among chinese medical postgraduates. Med. Educ. Online. 2022;27:2058866. doi: 10.1080/10872981.2022.2058866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Periasamy P., Suganthi V., Sukala P.M., Janani S., Krishnakumar V., Kannan V.R., Gunasekaran S. Burnout amongmedical students and correlation with academic performance, sleep quality during covid19 pandemic online class in erode district. Pharmacologyonline. 2021;2:962–971. [Google Scholar]
- Perissotto T., Silva T.C.R.P.D., Miskulin F.P.C., Pereira M.B., Neves B.A., Almeida B.C., Casagrande A.V., Ribeiz S.R.I., Nunes P.V. Mental health in medical students during COVID-19 quarantine: a comprehensive analysis across year-classes. Clinics (Sao Paulo, Brazil) 2021;76 doi: 10.6061/clinics/2021/e3007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potapova E.A., Zemlyanoy D.A., Kondratyev G.V. Features of life and well-being in medical students during distance learning in the course of the COVID-19 epidemic. Psikhologicheskaya Nauka I Obrazovanie. 2021;26:70–81. doi: 10.17759/pse.2021260304. [DOI] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51:201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puranachaikere T., Hataiyusuk S., Anupansupsai R., In-Iw S., Saisavoey N., Techapanuwat T., Arunrodpanya F., Charonpongsuntorn C., Wiwattanaworaset P., Siripongpan A., Pruttithavorn W., Wonglertwisawakorn C., Pojanapotha P., Rueangrong B., Pattrakornkul N., Piyawattanametha N., Piyawattanametha S., Ratanapichayachai D. Stress and associated factors with received and needed support in medical students during COVID-19 pandemic: a multicenter study. Korean J. Med. Educ. 2021;33:203–213. doi: 10.3946/kjme.2021.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quek T.T.-C., Tam W.W.-S., Tran B.X., Zhang M., Zhang Z., Ho C.S.-H., Ho R.C.-M. The global prevalence of anxiety among medical students: a meta-analysis. Int. J. Environ. Res. Public Health. 2019;16:E2735. doi: 10.3390/ijerph16152735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao W.-W., Li W., Qi H., Hong L., Chen C., Li C.-Y., Ng C.H., Ungvari G.S., Xiang Y.-T. Sleep quality in medical students: a comprehensive meta-analysis of observational studies. Sleep Breath. 2020;24:1151–1165. doi: 10.1007/s11325-020-02020-5. [DOI] [PubMed] [Google Scholar]
- Risal A., Shikhrakar S., Mishra S., Kunwar D., Karki E., Shrestha B., Khadka S., Holen A. Anxiety and depression during COVID-19 pandemic among medical students in Nepal. Kathmandu Univ. Med. J. 2020;18:333–339. [PubMed] [Google Scholar]
- Roka K., Khadka S., Dahal S., Yadav M., Thapa P., Rubina K.C. Excessive daytime sleepiness among first to fourth year undergraduate students of a medical (allege in Nepal: a descriptive cross-sectional study. J. Nepal Med. Assoc. 2020;58:640–644. doi: 10.31729/jnma.5297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland F., Frajerman A., Falissard B., Bertschy G., Diquet B., Marra D. Impact of the first wave of the COVID-19 pandemic on french health students. Encéphale. 2022 doi: 10.1016/j.encep.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland F., Hadouiri N., Haas-Jordache A., Gouy E., Mathieu L., Goulard A., Morvan Y., Frajerman A. Mental health and working conditions among french medical students: a nationwide study. J. Affect. Disord. 2022;306:124–130. doi: 10.1016/j.jad.2022.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romic I., Silovski H., Mance M., Pavlek G., Petrovic I., Figl J., Grbavac D., Moric T., Romic R., Bakula B., Vulic A. Psychological effects of “Double crisis” (COVID-19 pandemic and Earthquakes) on croatian medical students. Psychiatr. Danub. 2021;33:120–125. [PubMed] [Google Scholar]
- Rotenstein L.S., Ramos M.A., Torre M., Segal J.B., Peluso M.J., Guille C., Sen S., Mata D.A. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214–2236. doi: 10.1001/jama.2016.17324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saali A., Stanislawski E.R., Kumar V., Chan C., Hurtado A., Pietrzak R.H., Charney D.S., Ripp J., Katz C.L. The psychiatric burden on medical students in New York city entering clinical clerkships during the covid-19 pandemic. Psychiatry Q. 2021 doi: 10.1007/s11126-021-09955-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed N., Javed N. Lessons from the covid-19 pandemic: perspectives of medical students. Pakistan J. Med. Sci. 2021;37:1402–1407. doi: 10.12669/pjms.37.5.4177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safa F., Anjum A., Hossain S., Trisa T.I., Alam S.F., Rafi M.A., Podder V., Koly K.N., Azad D.T., Ahmad W.U., Nodi R.N., Ashraf F., Akhter S.M.Q., Ahmed H.U., Hasan M.T. Immediate psychological responses during the initial period of the COVID-19 pandemic among bangladeshi medical students. Child Youth Serv. Rev. 2021;122 doi: 10.1016/j.childyouth.2020.105912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safarini O.A., Taya H., Abu Elhija Y., Qadous M., Farhoud A., Thabaleh A., Khayyat A., Nazzal Z., Abuhassan A.M., Ghanim N., Mahamid F., Al Ali R., Damiri B. Assessment of the relationship of depression with tobacco and caffeine use among university students: a cross-sectional study. Cureus. 2021;13 doi: 10.7759/cureus.19098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saguem B.N., Nakhli J., Romdhane I., Nasr S.B. Predictors of sleep quality in medical students during COVID-19 confinement. Encéphale. 2021 doi: 10.1016/j.encep.2021.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandoval K.D., Morote-Jayacc P.V., Moreno-Molina M., Taype-Rondan A. Depression, stress and anxiety in students of human medicine in Ayacucho (Peru) in the context of the COVID-19 pandemic. Rev. Colomb. Psiquiatr. 2021 doi: 10.1016/j.rcp.2021.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraswathi I., Saikarthik J., Senthil Kumar K., Madhan Srinivasan K., Ardhanaari M., Gunapriya R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: a prospective longitudinal study. PeerJ. 2020;8 doi: 10.7717/peerj.10164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saravia-Bartra M.M., Cazorla-Saravia P., Cedillo-Ramirez L. Anxiety level of first-year medicine students at a private university in Peru in times of covid-19. Rev Facult. Med. Hum. 2020;20:568–573. doi: 10.25176/RFMH.V20I4.3198. [DOI] [Google Scholar]
- Seetan K., Al-Zubi M., Rubbai Y., Athamneh M., Khamees A., Radaideh T. Impact of COVID-19 on medical students' mental wellbeing in Jordan. PLoS One. 2021;16 doi: 10.1371/journal.pone.0253295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafique Z., Syed F., Naz S., Urooj S., Khan S., Javed S. Assessment of factors affecting the sleep hygiene of medical students in Bahawalpur, Pakistan: a cross-sectional study. Sleep Sci. 2021;14:273–279. doi: 10.5935/1984-0063.20200063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldon E., Simmonds-Buckley M., Bone C., Mascarenhas T., Chan N., Wincott M., Gleeson H., Sow K., Hind D., Barkham M. Prevalence and risk factors for mental health problems in university undergraduate students: a systematic review with meta-analysis. J. Affect. Disord. 2021;287:282–292. doi: 10.1016/j.jad.2021.03.054. [DOI] [PubMed] [Google Scholar]
- Shrestha D., Adhikari S.P., Rawal N., Budhathoki P., Pokharel S., Adhikari Y., Rokaya P., Raut U. Sleep quality among undergraduate students of a medical college in Nepal during COVID-19 pandemic: an online survey. F1000Research. 2021;10:505. doi: 10.12688/f1000research.53904.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simic S., Obrdalj E.C., Bevanda M., Bevanda D., Rizikalo A., Marijanovic I. Impact of COVID-19 pandemic on mental health of medical students at the university of Mostar. Psychiatr. Danub. 2021;33:114–119. doi: 10.24869/psyd.2021.114. [DOI] [PubMed] [Google Scholar]
- Solomou I., Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: age and sex matter. Int. J. Environ. Res. Public Health. 2020;17:4924. doi: 10.3390/ijerph17144924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltan M.R., Soliman S.S., Dawoud M.E. A study of anxiety, depression and stress symptoms among Fayoum medical students during COVID-19 lockdown, Egypt. Egyptian Journal of Neurology, Psychiatry and Neurosurgery. 2021;57 doi: 10.1186/s41983-021-00377-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song H.-T., Ge C.-H., Chang L.-X., Zhao T.-T., Wu W., Ge D.-X., Zhai C.-P., Zhang X.-L. Investigation on the psychological status of college students during the coronavirus disease-2019 epidemic. J. Gen. Psychol. 2021 doi: 10.1080/00221309.2021.1893637. [DOI] [PubMed] [Google Scholar]
- Souza K.C.D., Mendes T.B., Gomes T.H.S., Silva A.A.D., Nali L.H.D.S., Bachi A.L.L., Rossi F.E., Gil S., França C.N., Neves L.M. Medical students show lower physical activity levels and higher anxiety than physical education students: a cross-sectional study during the COVID-19 pandemic. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.804967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahir M.J., Malik N.I., Ullah I., Khan H.R., Perveen S., Ramalho R., Siddiqi A.R., Waheed S., Shalaby M.M.M., De Berardis D., Jain S., Vetrivendan G.L., Chatterjee H., Gopar Franco W.X., Shafiq M.A., Fatima N.T., Abeysekera M., Sayyeda Q., Shamat S.F., Aiman W., Akhtar Q., Devi A., Aftab A., Shoib S., Lin C.Y., Pakpour A.H. Internet addiction and sleep quality among medical students during the COVID-19 pandemic: a multinational cross-sectional survey. PLoS One. 2021;16 doi: 10.1371/journal.pone.0259594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira L.de A.C., Costa R.A., Mattos R.M.P.R.de, Pimentel D. Saúde mental dos estudantes de Medicina do Brasil durante a pandemia da coronavirus disease 2019. Jornal Brasileiro de Psiquiatria. 2021;70:21–29. doi: 10.1590/0047-2085000000315. [DOI] [Google Scholar]
- Telgote S.A., Ghogare A.S., Khadse V., Karwande S.G. Smartphone addiction and its impact on insomnia among the undergraduate medical students of a teaching Hospital of Maharashtra, India-a cross-sectional study. J. Clin. Diagn. Res. 2021;15:VC01–VC05. doi: 10.7860/JCDR/2021/52819.15753. [DOI] [Google Scholar]
- Tison G.H., Avram R., Kuhar P., Abreau S., Marcus G.M., Pletcher M.J., Olgin J.E. Worldwide effect of COVID-19 on physical activity: a descriptive study. Ann. Intern. Med. 2020;173:767–770. doi: 10.7326/M20-2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toubasi A.A., Khraisat B.R., AbuAnzeh R.B., Kalbouneh H.M. A cross sectional study: the association between sleeping quality and stress among second and third medical students at the University of Jordan. Int. J. Psychiatry Med. 2021;912174211011287 doi: 10.1177/00912174211011287. [DOI] [PubMed] [Google Scholar]
- Vala N.H., Vachhani M.V., Sorani A.M. Study of anxiety, stress, and depression level among medical students during covid-19 pandemic phase in Jamnagar city. Natl. J. Physiol. Pharm. Pharmacol. 2020;10:1043–1045. doi: 10.5455/njppp.2020.10.07205202031072020. [DOI] [Google Scholar]
- Vythilingam D.I., Atiomo W.U. medRxiv; 2021. A Systematic Scoping Review on the Impact of the COVID-19 Quarantine on the Psychological Wellbeing of Medical Students. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Liu W., Zhang Y., Xie S., Yang B. Perceived stress among chinese medical students engaging in online learning in light of COVID-19. Psychol. Res. Behav. Manag. 2021;14:549–562. doi: 10.2147/prbm.S308497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Li Y., Jiang J., Feng Y., Lu D., Zhang W., Song H. COVID-19 outbreak-related psychological distress among healthcare trainees: a cross-sectional study in China. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-041671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wathelet M., Duhem S., Vaiva G., Baubet T., Habran E., Veerapa E., Debien C., Molenda S., Horn M., Grandgenèvre P., Notredame C.-E., D’Hondt F. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.25591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Li Z., Li Z., Xiang W., Yuan Y., Liu Y., Xiong Z. The mental state and risk factors of chinese medical staff and medical students in early stages of the COVID-19 epidemic. Compr. Psychiatry. 2020;102 doi: 10.1016/j.comppsych.2020.152202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Zhang K., Parks-Stamm E.J., Hu Z., Ji Y., Cui X. Increases in anxiety and depression during COVID-19: a large longitudinal study from China. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.706601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu T., Jia X., Shi H., Niu J., Yin X., Xie J., Wang X. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J. Affect. Disord. 2021;281:91–98. doi: 10.1016/j.jad.2020.11.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Shu W., Li M., Li Z., Tao F., Wu X., Yu Y., Meng H., Vermund S.H., Hu Y. Social distancing among medical students during the 2019 coronavirus disease pandemic in China: disease awareness, anxiety disorder, depression, and behavioral activities. Int. J. Environ. Res. Public Health. 2020;17:1–13. doi: 10.3390/ijerph17145047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao P., Chen L., Dong X., Zhao Z., Yu J., Wang D., Li W. Anxiety, depression, and satisfaction with life among college students in China: nine months after initiation of the outbreak of COVID-19. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.777190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Li X., Luo H., He L., Bai Y., Zheng F., Zhang L., Ma J., Niu Z., Qin Y., Wang L., Ma W., Yu H., Zhang R., Guo Y. Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in China: a survey of medical students. Front. Public Health. 2020;8 doi: 10.3389/fpubh.2020.588578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie X., Zhu K., Xue Q., Zhou Y., Liu Q., Wu H., Wan Z., Zhang J., Meng H., Zhu B., Song R. Problematic internet use was associated with psychological problems among university students during COVID-19 outbreak in China. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.675380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong P., Ming W.K., Zhang C., Bai J., Luo C., Cao W., Zhang F., Tao Q. Factors influencing mental health among chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front. Public Health. 2021;9 doi: 10.3389/fpubh.2021.603331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang K.H., Wang L., Liu H., Li L.X., Jiang X.L. Impact of coronavirus disease 2019 on the mental health of university students in Sichuan Province, China: an online cross-sectional study. Int. J. Ment. Health Nurs. 2021;30:875–884. doi: 10.1111/inm.12828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Q., Liu Y., Yang W.F., Peng P., Chen S., Wang Y., Wang X., Li M., Wang Y., Hao Y., He L., Wang Q., Zhang J., Ma Y., He H., Zhou Y., Long J., Qi C., Tang Y.Y., Liao Y., Tang J., Wu Q., Liu T. Mental health conditions and academic burnout among medical and non-medical undergraduates during the mitigation of COVID-19 pandemic in China. Environ. Sci. Pollut. Res. Int. 2022 doi: 10.1007/s11356-022-19932-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang X., Gao L., Zhang S., Zhang L., Zhang L., Zhou S., Qi M., Chen J. The professional identity and career attitude of chinese medical students during the COVID-19 pandemic: a cross-sectional survey in China. Front. Psychiatry. 2022;13 doi: 10.3389/fpsyt.2022.774467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye W., Ye X., Liu Y., Liu Q., Vafaei S., Gao Y., Yu H., Zhong Y., Zhan C. Effect of the novel coronavirus pneumonia pandemic on medical students' psychological stress and its influencing factors. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.548506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K., Zheng Y.-B., Wang Y.-J., Sun Y.-K., Gong Y.-M., Huang Y.-T., Chen X., Liu X.-X., Zhong Y., Su S.-Z., Gao N., Lu Y.-L., Wang Z., Liu W.-J., Que J.-Y., Yang Y.-B., Zhang A.-Y., Jing M.-N., Yuan C.-W., Zeng N., Vitiello M.V., Patel V., Fazel S., Minas H., Thornicroft G., Fan T.-T., Lin X., Yan W., Shi L., Shi J., Kosten T., Bao Y.-P., Lu L. A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol. Psychiatry. 2022 doi: 10.1038/s41380-022-01638-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan L.L., Lu L., Wang X.H., Guo X.X., Ren H., Gao Y.Q., Pan B.C. Prevalence and predictors of anxiety and depressive symptoms among international medical students in China during COVID-19 pandemic. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.761964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yunitri N., Chu H., Kang X.L., Jen H.-J., Pien L.-C., Tsai H.-T., Kamil A.R., Chou K.-R. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: a meta-analysis. Int. J. Nurs. Stud. 2022;126 doi: 10.1016/j.ijnurstu.2021.104136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhan J., Sun S., Xie L., Wen Y., Fu J. Medical students’ mental health, professional pride, and intention to work in the front-line during coronavirus disease 2019 pandemic. Zhong nan da xue xue bao. Yi xue ban = journal of Central South University. Med. Sci. 2020;45:649–656. doi: 10.11817/j.issn.1672-7347.2020.200440. [DOI] [PubMed] [Google Scholar]
- Zhang C., Zeng P., Tan J., Sun S., Zhao M., Cui J., Zhang G., Jia J., Liu D. Relationship of problematic smartphone use, sleep quality, and daytime fatigue among quarantined medical students during the COVID-19 pandemic. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.755059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang K., Lin Z., Peng Y., Li L. A longitudinal study on psychological burden of medical students during COVID-19 outbreak and remission period in China. Eur. J. Psychiatry. 2021;35:234–241. doi: 10.1016/j.ejpsy.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M., Zhou Z., Tao X., Huang L., Zhu E., Yu L., Liu H. Prevalence of subhealth status and its effects on mental health and smartphone addiction: a cross-sectional study among chinese medical students. Rev. Assoc. Med. Bras. 2022;1992(68):222–226. doi: 10.1590/1806-9282.20210977. [DOI] [PubMed] [Google Scholar]
- Zhang X., Shi X., Wang Y., Jing H., Zhai Q., Li K., Zhao D., Zhong S., Song Y., Zhang F., Bao Y. Risk factors of psychological responses of chinese university students during the COVID-19 outbreak: cross-sectional web-based survey study. J. Med. Internet Res. 2021;23 doi: 10.2196/29312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao F.F., Yang L., Ma J.P., Qin Z.J. Path analysis of the association between self-compassion and depressive symptoms among nursing and medical students: a cross-sectional survey. BMC Nurs. 2022;21:67. doi: 10.1186/s12912-022-00835-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L., Sznajder K., Cheng D., Wang S., Cui C., Yang X. Coping styles for mediating the effect of resilience on depression among medical students in web-based classes during the covid-19 pandemic: cross-sectional questionnaire study. J. Med. Internet Res. 2021;23 doi: 10.2196/25259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X., Guo Y., Yang H., Luo L., Ya B., Xu H., Xue Z., Li Q., Shi J., Bi J., Ma W., Wang P. A cross-sectional study on mental health problems of medical and nonmedical students in Shandong during the COVID-19 epidemic recovery period. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.680202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Y., Schroeder E., Gao Y., Guo X., Gu Y. Social support, health literacy and depressive symptoms among medical students: an analysis of mediating effects. Int. J. Environ. Res. Public Health. 2021;18:1–12. doi: 10.3390/ijerph18020633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Racine N., Xie E.B., Park J., Watt J., Eirich R., Dobson K., Madigan S. Post-secondary student mental health during COVID-19: a meta-analysis. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.777251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zis P., Artemiadis A., Bargiotas P., Nteveros A., Hadjigeorgiou G.M. Medical studies during the COVID-19 pandemic: the impact of digital learning on medical students’ burnout and mental health. Int. J. Environ. Res. Public Health. 2021;18:1–9. doi: 10.3390/ijerph18010349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren H.J., Tian W.P., Wang Y.L., Wang H., Wei C.H., Zhao W.X. A survey on the depression status of clinical medicine postgraduates in a university in Inner Mongolia (In Chinese) J. Baotou Med. Coll. 2021;37:112–114. doi: 10.16833/j.cnki.jbmc.2021.06.036. [DOI] [Google Scholar]
- Feng G., Wu X.H., Chen M., Wang K., Yan Q.Q. A study on the association between depression and anxiety states of medical students based on generalized summation model (In Chinese) China Pharm. Herald. 2021;18:59–62. [Google Scholar]
- Liu W., Li F.Q., Zhou T., Li Q., Liu L.Q., Wu C., Liu Y.L. A survey of medical students' daily behavior during holidays (In Chinese) Chin. Geriatr. Orthop. Rehabil. Electron. J. 2020;6:217–222. [Google Scholar]
- Liu P.J., Wang S., Ding Y., Qin N., Li R.Z., Xu X.Y. A survey of medical students' perceptions and levels of psychological behavior and anxiety regarding the COVID-19 pandemic. J. Qingdao Univ. (Med. Ed.) 2021;57:286–289. [Google Scholar]
- Xia X.F., Pan W.X., Li X.L., Luo Q., Deng C.Q., Xiang H.R. The Moderating Role of Psychological Defense Mechanisms Between Solitary Behavior and Depression in Medical Students (In Chinese) Vol. 38. 2022. pp. 684–689. [DOI] [Google Scholar]
- Zhang T.J., Meng Y.B., Deng D.Y., Huang H.T., Tang L., You S.N., Jiang Y., Duan Y. Survey on the mental health of medical students in the face of public health emergencies (In Chinese) J. Xiangnan Coll. (Med. Ed.) 2020;22:51–55. doi: 10.16500/j.cnki.1673-498x.2020.04.015. [DOI] [Google Scholar]
- Zhang X.L., Jia W., Duan L.M. A survey and analysis of 1486 medical students' psychological status during the COVID-19 pandemic (In Chinese) J. Inner Mongolia Med. Univ. 2020;42:128–130. doi: 10.16343/j.cnki.issn.2095-512x.20200305.001. [DOI] [Google Scholar]
- Zhang S.Y., Gao L., Yang X.J., Zhang L.G., Qi M., Chen J.X. Association of COVID-19 exposure with depression and anxiety and social support among medical students (In Chinese) School Health China. 2020;41:657–660. doi: 10.16835/j.cnki.1000-9817.2020.05.006. [DOI] [Google Scholar]
- Zhang Y.L., Wang C., Zou G.S., Lv J.C. The relationship between sense of meaning in life and suicidal ideation among medical students (In Chinese) J. Shandong Univ. (Med. Ed.) 2021;59 93-99+107. [Google Scholar]
- Xu J.C., Chen L., Fan R. The mediating role of psychological resilience in the relationship between stress and anxiety symptoms among medical students in the post-epidemic period. J. Environ. Occup. Med. 2021;38:853–859. doi: 10.13213/j.cnki.jeom.2021.20612. (In Chinese) [DOI] [Google Scholar]
- Wang C., Zhang Y.L., Zou G.S., Lv J.C. Survey of 686 medical students with or without suicidal ideation and analysis of influencing factors (In Chinese) J. Shandong Univ. (Med. Ed.) 2022;60:78–85. [Google Scholar]
- Tian C., Su J., Wang A.H. Current state of knowledge and beliefs about novel coronavirus pneumonia among general medical students in Chongqing based on job competency (In Chinese) Guangxi Med. 2021;43:1491–1496. [Google Scholar]
- Miu X.S., Y S. Investigation and analysis of sleep disorders during the COVID-19 pandemic among medical students. Journal of Kunming Medical University. 2021;42:166–169. (In Chinese) [Google Scholar]
- Jiang P., Yu W.Z., Guan L.Y., Zhuang N.N., Cao J.Q., Hou W.L., Hou Y.Y., Zhu Z.H., Yin X.L., Jia Q.F., Hui L. A survey on the psychological condition of Chinese medical students during winter vacation (In Chinese) Modern Chin. Doctors. 2020;58:141–146. [Google Scholar]
- Xing B.Y., Ge W.J., Lu Y.G., Shu W., Miu Q.F. Medical students' perception, psychological and behavioral survey on the COVID-19 pandemic (In Chinese) Health Res. 2020;40:369–372. [Google Scholar]
- Zheng Y.W., Xu J.B., Yang T.T., Gao W.N., Wang Y.J., Jiang Q. The relationship between perceived stress status, coping style and perceived social support among medical students during the COVID-19 pandemic: an example from Fujian Province (In Chinese) Strait Science. 2021:71–73. +77. [Google Scholar]
- Zheng Q.Y., Wei M., Jiang Q., Ye X., Lin X.H. Effects of the COVID-19 pandemic on medical Students' psychological status and attitudes toward medical practice. J. Fujian Med. Univ. (Soc. Sci. Ed.) 2021;22 29-33+39. [Google Scholar]
- Jin Y.L., Chang W.W., Chang X., Zhu L.J., Fang Z.M., Chen Y., Yao Y.S. Analysis of mental health and factors affecting college students during online study of the COVID-19 pandemic (In Chinese) School Health China. 2021;42:574–578. doi: 10.16835/j.cnki.1000-9817.2021.04.022. [DOI] [Google Scholar]
- Chen G., Xu J.D., Lu J. Anxiety and its associated factors when medical students' return to school during the COVID-19 pandemic (In Chinese) School Health China. 2020;41:1851–1855. doi: 10.16835/j.cnki.1000-9817.2020.12.022. [DOI] [Google Scholar]
- Lei Q.L., Liao M.L., Jia J., Wang L.L., Jiang Q. A study on the relationship between physical exercise, emotion regulation and suicidal ideation among medical students (In Chinese) Fujian Sports Technol. 2021;40:14–19. [Google Scholar]
- Ma S.Y., Chen Y., Wang F.F., Wang H.H., Jin Y.L., Yao Y.S. Medical students' anxiety and its influencing factors during the COVID-19 pandemic (In Chinese) School Health China. 2021;42:1351–1355. doi: 10.16835/j.cnki.1000-9817.2021.09.018. [DOI] [Google Scholar]
- Gao L., Yang X.J., Zhang S.Y., Zhang L.G., Chen K., Qi M., Chen J.X. Depressive and anxiety symptoms and associated factors among medical students during the COVID-19 pandemic (In Chinese) Chin. J. Mental Health. 2020;34:878–882. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material