The COVID-19 pandemic has disrupted the delivery of healthcare services, including sexual health services (SHS) in England. Many SHS remained open for urgent or complex cases, but at reduced capacity; meanwhile, the use of online and telephone services increased to meet the continued demand for STI services.1 We compared trends in testing and diagnoses for bacterial STIs in England throughout different periods of COVID-19 restrictions during 2020 with the equivalent prepandemic data for 2019.
National data for England on tests and diagnoses for chlamydia, gonorrhoea and syphilis (primary, secondary and early latent stages) between 1 January 2019 and 31 December 2020 were extracted from the GUMCAD STI Surveillance2 and the CTAD chlamydia surveillance systems.3 To prevent double-counting, only one test or diagnosis for each STI was counted within a 42-day period. Online tests were defined as self-sampling kits supplied by online service providers. All data were analysed using STATA V.15.1 (Stata, College Station, Texas, USA).
Between January and April 2020, testing more than halved for chlamydia, gonorrhoea and syphilis, particularly between March and April (range: 52.1%–58.7% decrease; figure 1), coinciding with the first national lockdown. The number of STI tests recovered as restrictions were progressively eased but levelled as stricter social distancing measures were reintroduced in October 2020, and remained at 70%–80% of 2019 levels, with testing for chlamydia and gonorrhoea recovering slightly better than for syphilis. Online testing played an increasing role in 2020, with the proportion of STI tests accessed online in 2020 double that of 2019 (40.6% vs 18.0%). Diagnoses of chlamydia and gonorrhoea followed a similar trajectory to testing and returned to 60%–70% of 2019 levels by December 2020. However, infectious syphilis diagnoses continued to increase in 2020, despite testing levels being lower than 2019. Positivity remained higher for syphilis, while returning to previous or lower levels for chlamydia and gonorrhoea.
Figure 1.
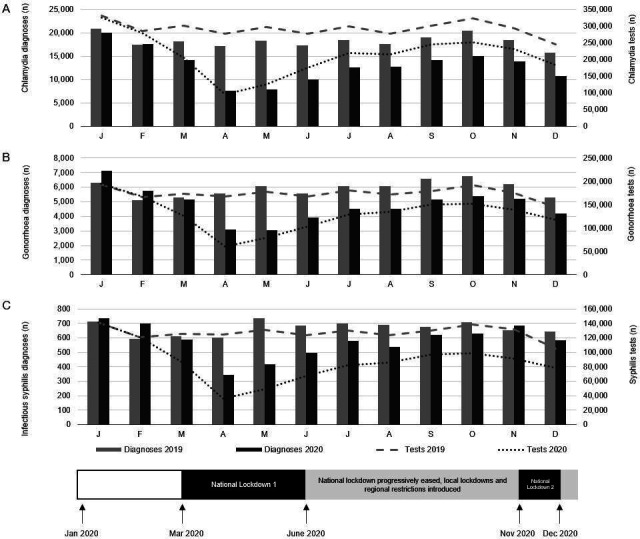
Number of chlamydia, gonorrhoea and syphilis diagnoses and tests at sexual health services, January 2019 to December 2020, England*. *National lockdown 1 in England was from 23 March to 11 May 2020. National lockdown 2 was from 5 November to 2 December 2020. Public health restrictions were not fully relaxed between national lockdown 1 and national lockdown 2. Regional restrictions remained in place during December 2020 and a third national lockdown started on 6 January 2021. (A) Chlamydia diagnoses and tests; (B) gonorrhoea diagnoses and tests; (C) infectious syphilis diagnoses and tests. Infectious syphilis includes primary, secondary and early latent stages. Different scales are used on the y-axes of the graphs above.
Social distancing measures and disruption to sexual healthcare associated with the COVID-19 pandemic appear to have had, at least initially, a marked impact on chlamydia, gonorrhoea and syphilis tests and diagnoses, as seen in other high-income countries.4–6 Diagnoses rates were highly related to testing rates in 2020.
The pattern of overall decline, followed by recovery, is similar to that seen in the USA, with chlamydia diagnoses most impacted and syphilis diagnoses least affected by COVID-19 restrictions.7 England, like the USA, was reporting the highest levels of syphilis and gonorrhoea diagnoses for decades immediately before the pandemic and our findings suggest that STI transmission continued throughout the period of national and regional restrictions. Of particular concern, the increased positivity for syphilis in 2020 indicates that the burden of infection could be increasing. Alternatively, this could be an artefact related to changes in testing practices, such that partners and symptomatic cases were more likely to be tested, during the COVID-19 pandemic. This aligns with previous analyses which described a higher proportion of people aged 25–34 years and of men who have sex with men accessing bacterial STI testing in the first half of 2020, compared with the same period in 2019.1
Although the relative contribution of reduced availability of tests or any reduction in prevalence on the observed reduction in diagnoses is unclear, there is the potential for a continued increase in diagnoses as we reduce social restrictions. Therefore, we emphasise the need for comprehensive and inclusive ways to ensure equitable access to STI testing, diagnosis and treatment as social and physical distancing measures are relaxed, and for surveillance data to continue to inform the emerging picture for, and response to, these infections.
Footnotes
Handling editor: Anna Maria Geretti
Contributors: HC, KS, NR, LT and TS planned the analysis. HC, NR, LT, TS and SS analysed the data. HC wrote first draft of manuscript. HC, NR, LT, TS, SS, HM, KF and KS reviewed and edited manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Public Health England . The impact of the COVID-19 pandemic on prevention, testing, diagnosis and care for sexually transmitted infections, HIV and viral hepatitis in England (appendix); 2020.
- 2. Public Health England . GUMCAD STI surveillance system: guidance, 2013. Available: https://www.gov.uk/guidance/gumcad-sti-surveillance-system [Accessed 9 Aug 2021].
- 3. Public Health England . CTAD Chlamydia surveillance system: guidance, 2012. Available: https://www.gov.uk/guidance/ctad-chlamydia-surveillance-system [Accessed 9 Aug 2021].
- 4. Kuitunen I, Ponkilainen V. COVID-19-related nationwide lockdown did not reduce the reported diagnoses of Chlamydia trachomatis and Neisseria gonorrhoeae in Finland. Sex Transm Infect 2021;97:550. 10.1136/sextrans-2020-054881 [DOI] [PubMed] [Google Scholar]
- 5. Heerfordt IM. STIs during the first and second wave of COVID-19 in Denmark. Sex Transm Infect 2022;98:150–1. 10.1136/sextrans-2021-055021 [DOI] [PubMed] [Google Scholar]
- 6. Apalla Z, Lallas A, Mastraftsi S, et al. Impact of COVID-19 pandemic on STIs in Greece. Sex Transm Infect 2022;98:70. 10.1136/sextrans-2021-054965 [DOI] [PubMed] [Google Scholar]
- 7. Crane MA, Popovic A, Stolbach AI, et al. Reporting of sexually transmitted infections during the COVID-19 pandemic. Sex Transm Infect 2021;97:101–2. 10.1136/sextrans-2020-054805 [DOI] [PubMed] [Google Scholar]


