Abstract
Introduction
Habituation and loss of efficacy from spinal cord stimulation are commonly reported. This retrospective analysis investigated rescue of analgesia from spinal cord stimulation failure after implementing a strategy called a stimulation holiday, during which spinal cord stimulation is interrupted for a defined period and subsequently restarted.
Methods
A 6-year review (June 1, 2016–May 13, 2022) from a tertiary care center was conducted on patients who underwent 10 kHz frequency dorsal column spinal cord stimulation for ≥3 months, experienced loss of efficacy (≤30% pain relief or patient self-report of lack of meaningful pain relief), subsequently underwent a stimulation holiday, and then restarted spinal cord stimulation. The primary outcome was comparison of pain relief and responder rate (≥50% relief in pain intensity) before and after stimulation holiday.
Results
Of 212 patients, 40 (18.9%) experienced loss of efficacy at a mean follow-up period of 452.7±326.4 days after stimulator implantation and underwent stimulation holiday. Pain relief was significantly higher 1 month after stimulation holiday (39.4%±28.6%) compared with before stimulation holiday (8.7%±13.0%; mean difference 30.6%, 95% CI 21.9% to 39.3%, paired t-test p<0.001). A significantly higher responder rate (≥50% relief in pain intensity) was identified after stimulation holiday (57.5%) compared with before stimulation holiday (0%; Fisher’s exact test p<0.001). Associations of superior pain relief and responder rate remained significant at 3 and 6 months after stimulation holiday.
Discussion
Patients who experience loss of efficacy from spinal cord stimulation habituation could attempt a stimulation holiday rather than abandon therapy. Rescue of analgesia may be achieved after implementing a stimulation holiday and restarting spinal cord stimulation.
Keywords: Spinal Cord Stimulation, CHRONIC PAIN, Neuromodulation
WHAT IS ALREADY KNOWN ON THIS TOPIC
There are limited strategies to salvage analgesia after a patient experiences long-term habituation and loss of efficacy from dorsal column spinal cord stimulation.
This analysis investigated a treatment strategy called stimulation holiday, during which spinal cord stimulation is interrupted for a defined period and subsequently restarted.
WHAT THIS STUDY ADDS
In patients who experienced failure from long-term spinal cord stimulation, pain relief can be salvaged after implementing a stimulation holiday and then restarting spinal cord stimulation therapy.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Before completely abandoning spinal cord stimulation therapy in patients who experience therapy habituation and loss of efficacy, pain specialists should offer a stimulation holiday as a strategy to salvage analgesia.
Introduction
Spinal cord stimulation (SCS) has been used to treat chronic pain for over 50 years. SCS is currently approved by the Food and Drug Administration for treatment of chronic pain in persistent spinal pain syndrome type 2,1 non-surgical refractory low back pain,2 complex regional pain syndrome,3 and painful diabetic neuropathy.4 5 Several landmark trials have highlighted superior analgesia of SCS therapy versus conventional medical therapy alone for chronic pain conditions, with responder rates ranging between 50% and 80%1 3 5–7 over the course of 6–12 months after SCS implantation. However, these landmark trials failed to capture the long-term outcomes over several years. Observational studies that followed participants for greater than 2 years after SCS implantation have suggested diminishing responder rate with SCS therapy over time.8 9
Habituation, a process of diminishing response to a repeated stimulus or therapy, may be a reason for loss of efficacy from long-term SCS therapy.10 A retrospective analysis of SCS explantations revealed that over half of the explants were due to loss of efficacy from SCS during a 6-year period.11 Similarly, in another retrospective analysis, 81% of participants underwent SCS explantation due to loss of efficacy over a 9-year period.12 Although the mechanism for long-term habituation is unknown, potential multifactorial etiologies may play a role, including neural plasticity, disease progression, development of fibrosis on the implanted leads, and diminished placebo effect. Common strategies to rescue analgesia from SCS therapy habituation include reprogramming of the SCS waveform, revision of existing hardware, and trial of another neuromodulation intervention.
A strategy that we introduce in this study is called ‘stimulation holiday’, during which SCS therapy is discontinued for a defined period followed by reinitiation of therapy in an attempt to salvage analgesia. This term stems from the more familiar term ‘drug holiday’, which is a treatment strategy of deliberate interruption of pharmacotherapy used in situations of drug tolerance.13 14 A drug holiday provides a pause in physiological and psychological effects induced by the chronic intake of a drug. With reinitiation of therapy, the body is able to resensitize its drug receptors and achieve a greater response similar to what was achieved during the first intake of the drug. As an illustrative example, patients with Parkinson’s disease who underwent a 7-day interruption of levodopa therapy experienced improved mobility and balance up to 36 months after reinitiation.13 In patients with opioid tolerance and dependence, implementation of an opioid holiday may re-establish the patient’s sensitivity to opioids and improve pain relief.14
Akin to how a drug holiday may be associated with an increased therapeutic response after drug reinitiation, we hypothesize that implementation of a stimulation holiday followed by reinitiation of SCS therapy may be associated with rescue of analgesia. Several studies have reported poor rescue of relief after implementing a stimulation holiday, although the efficacy of stimulation holiday was not the primary or secondary outcome in these prior studies.15–19 Thus, the primary aim of this retrospective observational study was to compare pain relief and responder rate from SCS therapy before and after implementation of a stimulation holiday.
Methods
Study design and population
We conducted a 6-year retrospective review (June 1, 2016–May 13, 2022) of all patients from a single tertiary care center (Mayo Clinic, Rochester, Minnesota, USA) who underwent a dorsal column SCS implant that can deliver 10 kHz frequency stimulation. The authors only included devices delivering 10 kHz SCS as data on stimulation parameters were maintained on a separate vendor-specific database that was able to be queried to determine which patients underwent a stimulation holiday. The authors queried the existing electronic database to identify patients who had an SCS implant for at least 3 months that provided a successful response post implant (>30% pain relief or patient self-report of meaningful pain relief), experienced loss of efficacy (≤30% pain relief or patient self-report of lack of clinically meaningful pain relief), and subsequently underwent a stimulation holiday as part of their treatment plan to salvage efficacy. Exclusion criteria were any patient complications or hardware issues that may explain loss of efficacy (eg, lead migration, lead fracture, etc) instead of therapy habituation. The requirement for written informed consent was waived. Patients were excluded if they had declined research authorization for review of medical records and if stimulation holiday was not part of their treatment plan to salvage efficacy from SCS therapy.
Data extraction
Data were abstracted retrospectively for the following variables immediately prior to initiation of stimulation holiday: demographics (age, sex), body mass index, current tobacco use, current opioid use, daily oral morphine equivalents (OMEs), current neuropathic medication use, preimplant pain score on an 11-point Numeric Rating Scale (NRS), preholiday NRS pain score, time from implant to stimulation holiday, duration of stimulation holiday, and primary pain diagnosis. We also abstracted the type of waveform that was delivered during reinitiation of stimulation after stimulation holiday. All data were extracted via manual chart review performed in parallel by the authors (RSD and YFH). Specific waveform settings from reprogramming sessions before and after stimulation holiday were obtained from the vendor (Nevro, Redwood City, California, USA).
To inform variables of opioid use and daily OME, data on type of opioid and dosing immediately prior to stimulation holiday were extracted for oral opioids (hydrocodone, meperidine, morphine, opium/belladonna, oxycodone immediate release, oxycodone sustained release, tapentadol, and tramadol) and transdermal opioids (buprenorphine patch, and fentanyl patch). We converted these cumulative doses to their respective OME values using an institutional opioid calculator based on the Centers for Disease Control and Prevention conversion tables.20 To inform the variable of neuropathic medication use, data were extracted on use of tricyclic antidepressants, serotonin norepinephrine reuptake inhibitors, or anticonvulsants.
Pertinent to the outcomes of interest, data on the following before and after stimulation holiday were manually extracted from chart review: patient-reported percentage pain relief, number of patients who reported ≥50% relief in pain intensity, and number of patients who reported ≥30% relief in pain intensity. Data extraction was conducted for the following time points after stimulation holiday (ranges are provided in parentheses for maximum capture of patient follow-up data): 1 month (±2 weeks), 3 months (±1 month), and 6 months (±1 month).
Outcomes of interest
One primary outcome was comparison of mean pain relief (continuous outcome variable) before and after stimulation holiday (1 month, 3 months, and 6 months post holiday). Another primary outcome was comparison of responder rate (≥50% relief in pain intensity) before and after stimulation holiday (1 month, 3 months, and 6 months post holiday). As part of a sensitivity analysis determined a priori, we also compared responder rate at a lower threshold (≥30% relief in pain intensity) before and after stimulation holiday. This sensitivity analysis was justified as prior research has suggested that a 30% reduction in pain intensity is considered clinically significant.21 22
Statistical analysis
Baseline variables and outcomes were summarized by mean and SD for continuous variables and frequency (%) for categorical variables. Baseline variables were compared between responder status (≥50% relief in pain intensity after stimulation holiday) and non-responder status (<50% relief in pain intensity after stimulation holiday) using independent t-test for continuous outcomes and Fisher’s exact test for categorical outcomes. For the primary outcome comparison of mean pain relief before and after stimulation holiday, pairwise comparisons were conducted between preholiday relief and postholiday relief at each time point (‘pre-holiday vs one month post-holiday’, ‘pre-holiday vs three month post-holiday’, and ‘pre-holiday vs six month post-holiday’) using paired t-tests. Similarly, pairwise comparisons were also conducted for responder rate (>50% relief and >30% relief) before and after stimulation holiday using Fisher’s exact test.
A p value under 0.05 was considered statistically significant. As there were no pre-existing data regarding stimulation holidays for patients who lost efficacy from SCS, a power analysis for sample size estimation was deferred. However, a 6-year review was deemed adequate to provide a sizeable and clinically relevant sample. All statistical calculations were performed using SPSS V.21.0.
Results
Baseline characteristics
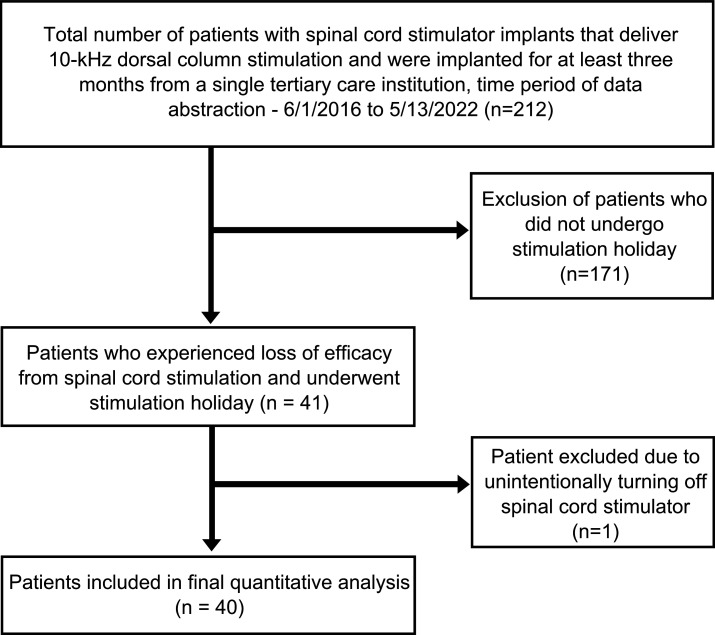
Of 212 patients, 40 (18.9%) experienced loss of efficacy and underwent stimulation holiday at a mean follow-up period of 452.7±326.4 days after SCS implantation (figure 1). Of note, all patients who experienced loss of efficacy underwent several reprogramming sessions to adjust waveform parameters (eg, amplitude, bipole, etc) prior to stimulation holiday, which failed to salvage any relief. The mean age was 67.9±12.9 years, with 45% of the cohort consisting of female patients (table 1). Immediately before the stimulation holiday, 25.0% of patients reported current tobacco use and 42.5% reported opioid use with a mean daily OME of 13.2±22.3 mg. The mean preholiday NRS pain score was 7.3±1.7. The mean time from SCS implant to stimulation holiday was 452.7±326.4 days (range: 44–1317 days) and the mean duration of the stimulation holiday was 17.3±20.6 days (range: 3–111 days). All patients underwent one stimulation holiday and no repeat stimulation holidays were pursued. The primary indication for SCS implant was failed back surgery syndrome in 65.0% of patients, followed by non-surgical refractory back pain in 22.5% of patients, painful diabetic neuropathy and radiculopathy each in 5.0% of patients, and idiopathic peripheral neuropathy in 2.5% of patients. Overall, 34 patients (85.0%) received 10 kHz SCS and 6 patients (15.0%) received tonic/10 kHz combination SCS after the stimulation holiday, which was the same waveform type they received before the stimulation holiday. Of the 34 patients who received 10 kHz SCS, 13 (38.2%) received high-duty cycled 10 kHz SCS. When baseline variables were stratified based on responder status to the stimulation holiday, there were no differences between the two groups (table 1).
Figure 1.
CONSORT flow diagram. A CONSORT diagram is displayed showing the study selection process consisting of patients with a spinal cord stimulator implant for at least 3 months who subsequently experienced loss of efficacy and underwent a stimulation holiday. CONSORT, Consolidated Standards of Reporting Trials.
Table 1.
Characteristics by responder status
| Variable | Overall cohort* | Responder*† | Non-responder*† | P value‡ |
| Sample size, n | 40 | 23 | 17 | – |
| Mean age (SD) in years | 67.9 (12.9) | 67.8 (12.2) | 68.0 (14.3) | 0.97 |
| Sex, n (%) | ||||
| Female | 18 (45.0) | 10 (43.5) | 8 (47.0) | 1.00 |
| Male | 22 (55.0) | 13 (56.5) | 9 (53.0) | |
| Body mass index (SD) in kg/m2 | 31.3 (5.7) | 31.7 (4.2) | 31.0 (7.4) | 0.67 |
| Current tobacco use, n (%) | 10 (25.0) | 5 (21.7) | 5 (29.4) | 0.72 |
| Opioid use, n (%) | 17 (42.5) | 8 (34.8) | 9 (53.0) | 0.34 |
| Daily OME (SD) in mg | 13.2 (22.3) | 8.8 (18.1) | 15.0 (25.6) | 0.38 |
| Neuropathic medication use, n (%) | 20 (50.0) | 14 (60.9) | 6 (35.3) | 0.20 |
| Preimplant NRS pain score (SD) | 8.3 (1.4) | 8.2 (1.5) | 8.4 (1.0) | 0.75 |
| Preholiday NRS pain score (SD) | 7.3 (1.7) | 7.0 (1.7) | 7.7 (1.5) | 0.18 |
| Time from implant to holiday (SD) in days | 452.7 (326.4) | 451.1 (277.7) | 453.4 (355.9) | 0.98 |
| Length of holiday (SD) in days | 17.3 (20.6) | 13.0 (8.4) | 20.5 (27.3) | 0.23 |
| Type of waveform after holiday, n (%) | ||||
| 10 kHz | 34 (85.0) | 22 (95.6) | 12 (70.6) | 0.07 |
| Tonic/10 kHz combination | 6 (15.0) | 1 (4.3) | 5 (29.4) | |
| Pain diagnosis, n (%) | ||||
| FBSS | 26 (65.0) | 12 (52.2) | 14 (82.4) | 0.09 |
| NSRBP | 9 (22.5) | 7 (30.4) | 2 (11.8) | 0.26 |
| PDN | 2 (5.0) | 2 (8.7) | 0 (0) | 0.50 |
| Radiculopathy | 2 (5.0) | 1 (4.3) | 1 (5.9) | 1.00 |
| Peripheral neuropathy | 1 (2.5) | 1 (4.3) | 0 (0) | 1.00 |
Baseline characteristics are reported at the time of stimulation holiday initiation.
Comparisons were made using independent t-test for continuous outcomes and Fisher’s exact test for categorical outcomes.
*Mean±SD presented for continuous outcomes and frequency with percentage presented for categorical outcomes.
†Responder status denotes ≥50% relief in pain intensity after stimulation holiday, whereas non-responder status denotes <50% relief in pain intensity after stimulation holiday.
‡Independent sample t-tests used to compare means and Fisher’s exact test used to compare proportions between responders and non-responders.
FBSS, failed back surgery syndrome; NRS, Numeric Rating Scale; NSRBP, non-surgical refractory back pain; OME, oral morphine equivalent; PDN, painful diabetic neuropathy.
Outcomes of interest
Of the 40 patients who experienced loss of efficacy, 35 reported preholiday percentage pain relief, 40 reported 1-month postholiday percentage pain relief, 34 reported 3-month postholiday percentage pain relief, and 25 reported 6-month postholiday percentage pain relief. No patients underwent device explantation during the 6-month period. Mean percentage pain relief in table 2 comprised all patients who reported percentage pain relief at each respective time point. However, the results in the following section reports different mean percentage pain relief values that were calculated in the context of statistical comparisons. When using a paired t-test to perform pairwise statistical comparisons (‘pre-holiday vs one month post-holiday’, ‘pre-holiday vs three month post-holiday’, and ‘pre-holiday vs six month post-holiday’), only patients who reported pain relief at both time points that are being compared are included in the paired statistical test and mean pain relief calculations stated in the following section.
Table 2.
Comparison of pain relief and responder status before and after stimulation holiday
| Preholiday | 1-month postholiday | 3-month postholiday | 6-month postholiday | |||
| Continuous outcome analysis | Mean difference (95% CI)* | P value* | ||||
| Sample size, n | 35 | 40 | 34 | 25 | ||
| Mean percentage pain relief (SD)† | 8.7 (13.0) | 41.2 (27.5) | 40.8 (27.3) | 34.0 (27.8) | 30.6 (21.9 to 39.3) | <0.001 |
| Categorical outcome analysis | OR (95% CI)* | P value* | ||||
| Sample size, n | 35 | 40 | 34 | 25 | ||
| ≥50% relief in pain intensity, n (%) | 0 (0) | 23 (57.5) | 21 (61.8) | 11 (44.0) | ‡ | <0.001 |
| ≥30% relief in pain intensity, n (%) | 6 (17.1) | 30 (75.0) | 23 (67.6) | 13 (52.0) | 14.5 (4.7 to 45.0) | <0.001 |
*Pairwise comparison between preholiday and 1-month postholiday pain relief and responder status is reported here. Pairwise comparisons between preholiday vs 3-month postholiday metrics and preholiday vs 6-month postholiday metrics are reported in the text. For the continuous outcome analysis, mean percentage pain relief was compared before and after stimulation holiday using paired t-test. For the categorical outcome analysis, responder status frequency based on various pain relief thresholds (≥50% and ≥30%) was compared before and after stimulation holiday using Fisher’s exact test.
†Mean percentage pain relief is presented for all patients at each study time point (preholiday, 1-month postholiday, 3-month postholiday, and 6-month postholiday). When conducting pairwise statistical comparisons between preholiday mean relief and postholiday mean relief, patients who did not report relief at both time points were omitted from analysis. Thus, the mean values in this table include all patients who reported percentage pain relief for that time point. This differs from the mean values reported in the text, which includes only patients who reported percentage pain relief at both time points that were included in the paired statistical comparison.
‡OR is infinite. This is because there were zero patients who experienced ≥50% relief before stimulation holiday.
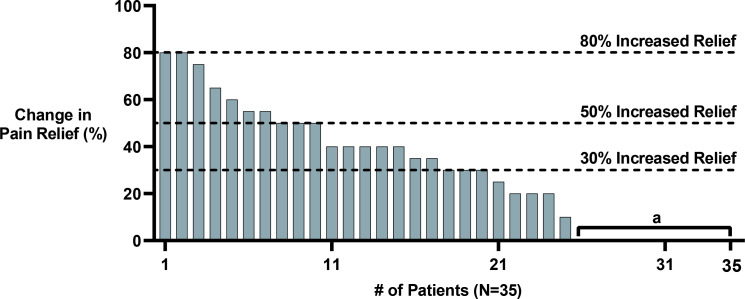
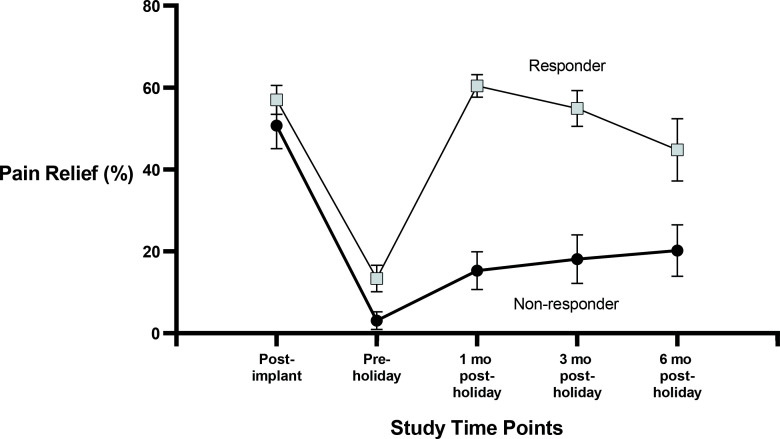
Compared with the mean percentage pain relief before stimulation holiday, the mean percentage pain relief after stimulation holiday was significantly higher at 1-month postholiday (8.7%±13.0% vs 39.4%±28.6%; n=35, mean difference (MD) 30.6%, 95% CI 21.9% to 39.3%, paired t-test p<0.001; table 2), at 3-month postholiday (7.2%±12.4% vs 38.6%±27.6%; n=31, MD 31.4%, 95% CI 21.6% to 41.1%, paired t-test p<0.001), and at 6-month postholiday (7.8%±13.1% vs 34.1%±27.3%; n=23, MD 26.3%, 95% CI 14.9% to 37.7%, paired t-test p<0.001). Change in percentage pain relief for each patient before stimulation holiday and 1 month after stimulation holiday is displayed in figure 2. The mean percentage pain relief values stratified by responder status at all study time points are displayed in figure 3.
Figure 2.
Waterfall plot displaying change in per cent pain relief. Change in percent pain relief from preholiday to 1 month after stimulation holiday is displayed in this waterfall plot. Although there were a total of 40 patients in this study, only 35 reported percent pain relief before stimulation holiday; thus, change in pain relief is only displayed for these 35 patients. aTen patients did not experience any improvement in relief after stimulation holiday.
Figure 3.
Per cent pain relief at all study time points stratified by responder status. Mean percent pain relief is reported at all study time points for responders and non-responders separately. Error bars are SE bars. mo, month.
Compared with the responder rate (≥50% relief in pain intensity) before stimulation holiday, responder rate after stimulation holiday was significantly higher at 1-month postholiday (0% vs 57.5%; Fisher’s exact test p<0.001; table 2), at 3-month postholiday (0% vs 61.8%; Fisher’s exact test p<0.001), and at 6-month postholiday (0% vs 44.0%; Fisher’s exact test p<0.01). Ten patients experienced 0% pain relief before and after stimulation holiday.
Sensitivity analysis
Compared with responder rate before stimulation holiday using a lower responder threshold of ≥30% relief in pain intensity, there was a higher proportion of responders after stimulation holiday at 1-month postholiday (17.1% vs 75.0%; OR 14.5, 95% CI 4.7 to 45.0, Fisher’s exact test p<0.001; table 2), at 3-month postholiday (17.1% vs 67.6%; OR 10.1, 95% CI 3.2 to 31.4, Fisher’s exact test p<0.001), and at 6-month postholiday (17.1% vs 52.0%; OR 5.2, 95% CI 1.6 to 17.0, Fisher’s exact test p<0.01).
Discussion
This study highlights that among patients who experience loss of efficacy and habituation from SCS therapy, implementation of a stimulation holiday is a strategy associated with salvage of pain relief. This is demonstrated by approximately 40% pain relief from baseline, a mean of 30.6% improvement in pain relief compared with preholiday relief, and a responder rate of 57.5% after stimulation holiday. Further, sensitivity analysis revealed that 75.0% of the overall cohort met the lower responder status threshold of ≥30% pain relief, a threshold that is considered clinically meaningful pain relief in prior work.21 22 Associations of superior pain relief and responder rate persisted at 3 months and 6 months after stimulation holiday. These findings are important because long-term habituation, tolerance to stimulation, and loss of efficacy are commonly reported in the neuromodulation literature and thus strategies to salvage analgesia in these scenarios are a priority in chronic pain conditions.10 23 Although habituation to neuromodulation therapy remains poorly understood, the human body is known to undergo physiological adaptations to a new maladaptive ‘set point’ in disease states.23 In these situations, a common strategy is to reprogram the SCS device to deliver a different waveform setting. Since different waveform paradigms likely evoke unique cellular mechanisms of analgesia, it is plausible that patients who develop tolerance to one waveform may experience analgesia with a different waveform. This is consistent with studies reporting rescue of analgesia in patients who switched to a new waveform after failing tonic stimulation.24 25
When waveform adjustments fail to deliver analgesia, patients and their implanting physicians may be inclined to abandon SCS therapy altogether and pursue alternative modalities of chronic pain treatment. However, our data highlight that current loss of efficacy does not always imply complete failure of SCS therapy in the future and that implementing a stimulation holiday is a viable strategy associated with rescue of analgesia. One potential explanation for this is that patients who undergo long-term SCS therapy may have forgotten about their original baseline pain prior to SCS implantation. Subsequently, cessation of stimulation may lead to recurrence of their higher baseline pain intensity, enabling patients to acknowledge that SCS therapy was actually providing analgesia. Another plausible explanation relates to the same mechanism of rescue analgesia underlying ‘drug holiday’ or ‘strategic treatment interruption’ of analgesic medications. Interruption of centrally acting pain medications may regenerate intrinsic responsivity and biochemical receptors within the analgesic pathways that were lost during the development of tolerance. This strategy may address analgesic failure from long-term analgesic usage, particularly opioid medications, and may be related to the mechanism of rescue analgesia following interruption of SCS therapy.26
The optimal length of stimulation holiday is unclear and warrants further investigation. In our cohort, the mean duration that stimulation was interrupted was slightly over 2 weeks (17.3±20.6 days), although there was a wide range from as little as 3 days to as long as 111 days. In pharmacology, the duration of a drug holiday is independent for each individual drug and is dependent on the kinetics of tolerance development. For instance, in animal models with full tolerance to morphine, a drug holiday of 6 days would be necessary to regenerate 50% of intrinsic response to morphine that was lost due to tolerance.27 In contrast, only about 3 hours of holding nicotine would be required for almost complete recovery and resensitization of nicotine receptors.28 It is likely that distinct waveform settings may also have distinct washout periods for resensitization, warranting future research on optimal holiday length associated with rescue of analgesia from SCS therapy habituation.
We observed that 10 patients experienced no improvement after stimulation holiday (eg, 0% pain relief). One potential explanation is that interruption of stimulation was too short to allow for meaningful resensitization of analgesic pathways. Another explanation is that the patient’s underlying painful condition may have worsened or may be compounded by a separate painful condition that is no longer amenable to analgesia from SCS therapy. It is important that the pain specialist evaluates for any hardware-related complications, such as lead migration and internal pulse generator failure, which may require revision surgery. Although extension of a stimulation holiday for a longer duration and completion of waveform reprogramming sessions both remain as reasonable options, the pain specialist should be prepared for the scenario where complete loss of efficacy occurs. In these challenging situations, the pain specialist may consider offering alternative treatments such as interventional pain injections, other neuromodulation modalities, and optimization of pharmacological regimen.
This study has several notable limitations. First, our study was limited to only SCS devices that deliver 10 kHz waveform as data from other devices were unable to be extracted from our institutional database. Thus, our findings are less generalizable and future studies are warranted to confirm if stimulation holiday is associated with salvage of efficacy with other SCS paradigms. Second, our study design was retrospective, contained a small sample size, and did not incorporate an a priori power analysis. Given that only 34 of 40 patients and 25 of 40 patients reported a mean percentage pain relief at the 3-month and 6-month follow-up, respectively, this introduces a source of attrition bias and selection bias. Given the paucity of literature defining the minimum length required to establish a stimulation holiday, we did not define this in our study. Finally, we did not abstract data on other important outcomes such as physical function, emotional function, patient satisfaction, and adverse events. Future prospective, powered, and randomized controlled trials are warranted to determine the efficacy of stimulation holiday in patients who experience SCS therapy habituation. Studies should also investigate the optimal duration of stimulation holiday, as well as stimulation holidays in other neuromodulation modalities such as peripheral nerve stimulation.
In conclusion, patients who experience loss of efficacy from SCS therapy habituation could attempt a stimulation holiday, which may be associated with salvage of analgesia from dorsal column SCS therapy.
Footnotes
Contributors: Both authors helped with study conception and design; performed research background and analysis, generation of figures, and analysis and interpretation of data; drafted the manuscript; and gave final approval of the manuscript. RSD accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: RSD’S has an investigator-initiated grant with Nevro. YFH has no conflict of interest related to this work.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the Mayo Clinic Institutional Review Board (identification number 22-005853).
References
- 1. Kumar K, Taylor RS, Jacques L, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicentre randomised controlled trial in patients with failed back surgery syndrome. Pain 2007;132:179–88. 10.1016/j.pain.2007.07.028 [DOI] [PubMed] [Google Scholar]
- 2. Kapural L, Yu C, Doust MW, et al. Novel 10-khz high-frequency therapy (hf10 therapy) is superior to traditional low-frequency spinal cord stimulation for the treatment of chronic back and leg pain: the senza-rct randomized controlled trial. Anesthesiology 2015;123:851–60. 10.1097/ALN.0000000000000774 [DOI] [PubMed] [Google Scholar]
- 3. Kemler MA, De Vet HCW, Barendse GAM, et al. The effect of spinal cord stimulation in patients with chronic reflex sympathetic dystrophy: two years' follow-up of the randomized controlled trial. Ann Neurol 2004;55:13–18. 10.1002/ana.10996 [DOI] [PubMed] [Google Scholar]
- 4. D'Souza RS, Langford B, Dombovy-Johnson M, et al. Neuromodulation interventions for the treatment of painful diabetic neuropathy: a systematic review. Curr Pain Headache Rep 2022;26:365–77. 10.1007/s11916-022-01035-9 [DOI] [PubMed] [Google Scholar]
- 5. Petersen EA, Stauss TG, Scowcroft JA, et al. Effect of high-frequency (10-khz) spinal cord stimulation in patients with painful diabetic neuropathy: a randomized clinical trial. JAMA Neurol 2021;78:687–98. 10.1001/jamaneurol.2021.0538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kemler MA, Barendse GA, van Kleef M, et al. Spinal cord stimulation in patients with chronic reflex sympathetic dystrophy. N Engl J Med 2000;343:618–24. 10.1056/NEJM200008313430904 [DOI] [PubMed] [Google Scholar]
- 7. North RB, Kidd DH, Farrokhi F, et al. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery 2005;56:discussion 106-7:98–107. 10.1227/01.NEU.0000144839.65524.E0 [DOI] [PubMed] [Google Scholar]
- 8. Hagedorn JM, Romero J, Thuc Ha C, et al. Paresthesia-based versus high-frequency spinal cord stimulation: a retrospective, real-world, single-center comparison. Neuromodulation 2021. 10.1111/ner.13497. [Epub ahead of print: 17 Jul 2021]. [DOI] [PubMed] [Google Scholar]
- 9. Hagedorn JM, Lam CM, D'Souza RS, et al. Explantation of 10 kHz spinal cord stimulation devices: a retrospective review of 744 patients followed for at least 12 Months. Neuromodulation 2021;24:499–506. 10.1111/ner.13359 [DOI] [PubMed] [Google Scholar]
- 10. Levy RM, Mekhail N, Kramer J, et al. Therapy habituation at 12 months: spinal cord stimulation versus dorsal root ganglion stimulation for complex regional pain syndrome type I and II. J Pain 2020;21:399–408. 10.1016/j.jpain.2019.08.005 [DOI] [PubMed] [Google Scholar]
- 11. Van Buyten J-P, Wille F, Smet I, et al. Therapy-related explants after spinal cord stimulation: results of an international retrospective chart review study. Neuromodulation 2017;20:642–9. 10.1111/ner.12642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Patel SK, Gozal YM, Saleh MS, et al. Spinal cord stimulation failure: evaluation of factors underlying hardware explantation. J Neurosurg Spine 2019:1–6. 10.3171/2019.6.SPINE181099 [DOI] [PubMed] [Google Scholar]
- 13. Corona T, Rivera C, Otero E, et al. A longitudinal study of the effects of an L-dopa drug holiday on the course of Parkinson's disease. Clin Neuropharmacol 1995;18:325–32. 10.1097/00002826-199508000-00004 [DOI] [PubMed] [Google Scholar]
- 14. Breitfeld C, Eikermann M, Kienbaum P, et al. Opioid "holiday" following antagonist supported detoxification during general anesthesia improves opioid agonist response in a cancer patient with opioid addiction. Anesthesiology 2003;98:571–3. 10.1097/00000542-200302000-00039 [DOI] [PubMed] [Google Scholar]
- 15. Al-Kaisy A, Royds J, Al-Kaisy O, et al. Cascade programming for 10 kHz spinal cord stimulation: a single center case series of 114 patients with neuropathic back and leg pain. Neuromodulation 2021;24:488–98. 10.1111/ner.13219 [DOI] [PubMed] [Google Scholar]
- 16. Staudt MD, Patel S, Hellman A, et al. Efficacy of simultaneous usage of spinal cord stimulation and intrathecal therapy for nonmalignant chronic neuropathic pain. World Neurosurg 2020;143:e442–9. 10.1016/j.wneu.2020.07.187 [DOI] [PubMed] [Google Scholar]
- 17. Ghosh P, Gungor S. Utilization of concurrent dorsal root ganglion stimulation and dorsal column spinal cord stimulation in complex regional pain syndrome. Neuromodulation 2021;24:769–73. 10.1111/ner.13144 [DOI] [PubMed] [Google Scholar]
- 18. Kumar K, Hunter G, Demeria D. Spinal cord stimulation in treatment of chronic benign pain: challenges in treatment planning and present status, a 22-year experience. Neurosurgery 2006;58:discussion 481-96:481–96. 10.1227/01.NEU.0000192162.99567.96 [DOI] [PubMed] [Google Scholar]
- 19. Hunter CW, Carlson J, Yang A, et al. Burst(able): A retrospective, multicenter study examining the impact of spinal cord stimulation with burst on pain and opioid consumption in the setting of salvage treatment and "Upgrade". Pain Physician 2020;23:E643–58. [PubMed] [Google Scholar]
- 20. Center for Disease Control (CDC) . Calculating total daily dose of opioids for safer dosage, 2020. Available: https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf.March
- 21. Farrar JT, Young JP, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149–58. 10.1016/S0304-3959(01)00349-9 [DOI] [PubMed] [Google Scholar]
- 22. Younger J, McCue R, Mackey S. Pain outcomes: a brief review of instruments and techniques. Curr Pain Headache Rep 2009;13:39–43. 10.1007/s11916-009-0009-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fishman MA, Antony A, Esposito M, et al. The evolution of neuromodulation in the treatment of chronic pain: Forward-looking perspectives. Pain Med 2019;20:S58–68. 10.1093/pm/pnz074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. De Ridder D, Lenders MWPM, De Vos CC, et al. A 2-center comparative study on tonic versus burst spinal cord stimulation: amount of responders and amount of pain suppression. Clin J Pain 2015;31:433–7. 10.1097/AJP.0000000000000129 [DOI] [PubMed] [Google Scholar]
- 25. Pope JE, Falowski S, Deer TR. Advanced waveforms and frequency with spinal cord stimulation: burst and high-frequency energy delivery. Expert Rev Med Devices 2015;12:431–7. 10.1586/17434440.2015.1026805 [DOI] [PubMed] [Google Scholar]
- 26. Blondell RD, Ashrafioun L. Treating opioid dependency and coexistent chronic nonmalignant pain. Am Fam Physician 2008;78:1132–3. [PubMed] [Google Scholar]
- 27. Ouellet DM, Pollack GM. Pharmacodynamics and tolerance development during multiple intravenous bolus morphine administration in rats. J Pharmacol Exp Ther 1997;281:713–20. [PubMed] [Google Scholar]
- 28. Porchet HC, Benowitz NL, Sheiner LB. Pharmacodynamic model of tolerance: application to nicotine. J Pharmacol Exp Ther 1988;244:231–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.