Abstract
Background
There has been considerable expansion in online postal self-sampling (OPSS) STI services in many parts of the UK, driven by increasing demand on sexual health services and developments in diagnostics and digital health provision. This shift in service delivery has occurred against a backdrop of reduced funding and service fragmentation and the impact is unknown. We explored characteristics of people accessing and using OPSS services for STIs in the UK, the acceptability of these services and their impact on sexual health inequalities.
Methods
A scoping review was conducted of studies published in English-language based on pre-agreed inclusion/exclusion criteria, between 01 January 2010 and 07 July 2021. Nine databases were searched, and 23 studies that met the eligibility criteria were included. Studies were appraised using the Mixed Methods Appraisal Tool.
Results
Study designs were heterogeneous, including quantitative, qualitative and mixed-methods analyses. The majority were either evaluating a single-site/self-sampling provider, exploratory or observational and of variable quality. Few studies collected comprehensive user demographic data. Individuals accessing OPSS tended to be asymptomatic, of white ethnicity, women, over 20 years and from less deprived areas. OPSS tended to increase overall STI testing demand and access, although return rates for blood samples were low, as was test positivity. There were varied results on whether services reduced time to treatment. OPSS services were acceptable to the majority of users. Qualitative studies showed the importance of trust, confidentiality, discretion, reliability, convenience and improved patient choice.
Conclusion
OPSS services appear highly acceptable to users. However, uptake appears to be socially patterned and some groups who bear a disproportionate burden of poor sexual health in the UK are under-represented among users. Current provision of online self-sampling could widen health inequalities, particularly where other options for testing are limited. Work is needed to fully evaluate the impact and cost-effectiveness of OPSS services.
Keywords: SEXUAL HEALTH, HIV, Telemedicine
Key messages.
An increasing proportion of STI testing in the UK is occurring via online postal self-sampling (OPSS) services.
Service users tend to be asymptomatic, white, women, over 20s and from less deprived areas.
OPSS services are acceptable to users and can improve choice.
There is a need for a wide-ranging evaluation of OPSS services to determine their impact on sexual health inequalities, access, clinical outcomes and service delivery.
Introduction
‘Home testing’ whereby an individual tests for STIs and/or blood-borne viruses (BBVs) remote from traditional healthcare settings, encompasses user self-sampling (the laboratory processes and tests the samples) or self-testing (the user tests their own samples).1 The most widely used option in the UK is online postal self-sampling (OPSS) in which users order specimen collection kits via the internet. Kits are delivered by post or may be collected from a sexual health clinic. Users obtain their own samples (typically urine or vulvo-vaginal swab, blood, and anorectal and pharyngeal swabs where appropriate), and repackage before posting back to a laboratory for testing. Test results are made available by text message or online. OPSS is increasingly provided in high-income countries.2–4 England’s earliest online chlamydia testing services began in 2006,5 but the other devolved nations of the UK introduced OPSS rather later.6–8 The BASHH recommends online testing and care provision as an adjunct to in-person services to increase choice for service users.9
The UK had seen a sustained rise in diagnoses of several STIs, and increase in demand for sexual health service (SHS) consultations, until the start of the COVID-19 pandemic.10 Between 2015 and 2019 in England, there was a 23% increase in the number of SHS consultations (3 143 144–3 852 121). Total sexual health screens for chlamydia, gonorrhoea, syphilis and HIV increased by 31% (1 657 425 to 2 175 525) in this period. Internet-based services have assumed an increasing proportion of consultations and screening activity. In 2018–2019, while overall consultations and tests in England rose by 7% and 10%, respectively, consultations and STI screens provided by internet-based services surged by 94% and 69%.10 This trend of an increasing proportion of testing and consultations being accessed and provided online has accelerated as a result of the COVID-19 pandemic.11 Young people, people from ethnic minority groups, men who have sex with men (MSM), people who are gender diverse, and those living in more deprived areas have borne a disproportionate burden of STIs and poorer sexual health for many years.12–17 The reasons for this disparity are not sufficiently understood.18
Some evidence suggests that OPSS might improve access to STI services for those who feel uncomfortable or struggle to attend face-to-face services,19 and might cost less than in-person care.20 21 However, relatively little is known about the characteristics of people who use OPSS and the existing literature is heterogeneous and has not previously been comprehensively reviewed. With a drive towards further online sexual health provision in the UK,22 the pre-existing unequal burden of sexual ill health in the population and well-described inequalities in access to sexual healthcare, it is important to understand the impact of this shift in service delivery. We aimed to evaluate the current evidence on access to and usage of OPSS services. We have restricted our scope to the UK because online care has been relatively mainstreamed in at least one country (England) for many years and sexual healthcare is provided free at the point of access without the need for specialist referral. Our specific objectives were to: (1) describe characteristics of people accessing and using STI self-sampling services in the UK; (2) assess whether OPSS increases demand for testing; (3) assess the impact of OPSS on clinical outcomes; (4) assess levels of acceptability of OPSS services in the UK.
Methods
We conducted a systematic scoping review in order to map and synthesise the current research evidence, in an area where the existing literature is heterogeneous and has not previously been comprehensively reviewed.23 We followed the Joanna Briggs Institute Framework of Evidence Synthesis (https://jbi.global/scoping-review-network/resources) and Preferred Reporting Items for Systematic Review and Meta-Analyses extension for scoping reviews guidelines.24 A review protocol has not been registered. The Population/Intervention/Comparators/Outcome framework was used to identify the research question and objectives:
Population
People residing in the UK who are engaging in sexual activity and accessing online SHS.
Intervention
Self-sampling STI testing kits which are posted to individuals’ homes by online SHS.
Comparators
The alternatives to this intervention are for individuals to visit sexual health clinics, general practice, or community outreach services to be tested by healthcare professionals, self-sample in a clinical setting, or collect kits to bring home. This review will compare OPSS with these comparators where included studies have done so.
Outcome
Accessibility and usage of OPSS services, with a focus on inequalities in access and acceptability of services, and the impact of these on sexual health inequalities.
Study selection criteria
Studies were included if they described the use of home self-sampling kits provided by online SHS in the UK, published between 1 January 2010 and 30 June 2021 in the English language. All non-theoretical study types with full-text online access were included. Studies were excluded if they described services outside of the UK, published prior to 2010 or not in English, and not focusing on home self-sampling kits provided by online SHS (for example, STI education, contraception or self-testing kits). We also excluded ‘siloed’ (HIV only) HIV self-sampling services because the national HIV self-sampling service targets specific key populations such as MSM and black African groups22 rather than the general population, and one of our key objectives was to evaluate access to, including potential inequalities with, the use of OPSS services. Protocols of studies and research displayed via conference or other forms of presentation were excluded if there was no full-text access.
Study selection
De-duplication and title screening was conducted by the first author; 20% of the abstract screening and 100% of the full-text screening were verified by a second reviewer (KCL and JG, respectively) independently to reduce selection bias.25 The inter-reliability rate of the two reviewers was over 90% at the abstract screening stage and was 100% for full-text screening.
Search method
A systematic search and data extraction was conducted on 22 June 2020 to fulfil requirements of KS’ Masters dissertation and was rerun on 7 July 2021 by JG in nine databases: Medline, EMBASE, PsycInfo, the Health Management Information Consortium, Web of Science, CINAHL Plus, Scopus, Open Grey and Ethos. The use of two grey literature databases (Open Grey and Ethos) aimed to reduce potential publication bias and provide a more comprehensive view of the evidence.26 The search consisted of a selection of medical subject headings terms, where appropriate, and free-text. Limits were used in applicable databases which limited by date and language. The search comprised of four concepts: types of STI, type of online or self-sampling service, accessibility or inequalities, and UK filters. For example, terms such as ‘STI’, ‘Chlamydia’, ‘Self-Sampl*’, ‘eHealth’, ‘Access*’, ‘Inequalit*’, ‘United Kingdom’ and ‘England’ were used. To ensure the search strategy was fully comprehensive, additional terms for ‘eHealth’ were included,27 and adapted and simplified versions of two verified filters for the UK were used in database searches, where appropriate.28 29
The search only included studies published between 2010 and 2021; this was due to the very low numbers of users of OPSS services prior to 20105 (see online supplemental file 1 for details of the full search strategy).
sextrans-2021-055376supp001.pdf (456.3KB, pdf)
Data extraction
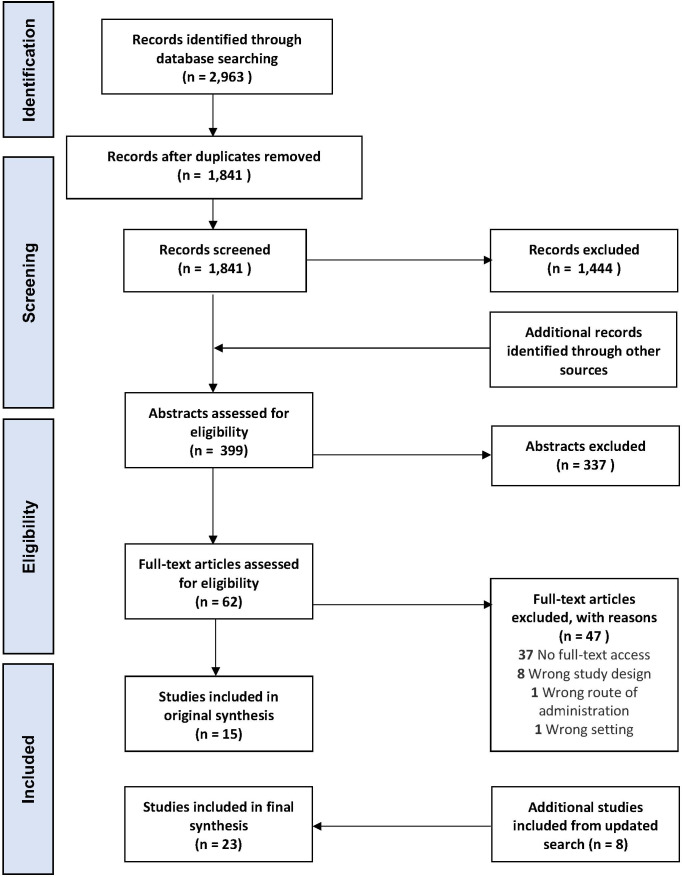
The phases of data identification, de-duplication, screening and eligibility checks are shown in figure 1. For included studies, a data extraction form (online supplemental file 2) was used to extract the demographics of the study participants (online supplemental file 3), the study design and key findings from each study (online supplemental file 4).
Figure 1.
Flow of Information, based on the Preferred Reporting Items for Systematic Review and Meta-Analyses flow diagram.32
Empirical appraisal and analysis of included articles
Study designs were heterogeneous, including quantitative, qualitative and mixed-methods analysis, and were therefore appraised using the Mixed Methods Appraisal Tool (MMAT).30 Quantitative data were analysed using descriptive statistics, and qualitative data were analysed using inductive thematic analysis.31
Results
Overview of included studies
This search strategy identified 23 relevant articles that described 10 different OPSS services, all located in England (see table 1 and online supplemental files 3 and 4). The overall quality was variable, with the majority either evaluating a single-site/testing provider, and exploratory or observational (see online supplemental file 5 for the full MMAT results; for a summary of each individual service or intervention, see online supplemental file 6). We found only one randomised controlled trial, which was single blind and where the intervention was a Short Message Service (SMS) containing a link to an OPSS website and the control was a link to a webpage that contained information for clinics where the recruits aged 16–30 years old could access testing. Six studies explored solely chlamydia testing, 1 assessed a chlamydia and gonorrhoea testing service and 17 assessed services which tested for chlamydia, gonorrhoea, HIV and syphilis. Five articles compared demographic characteristics and outcomes of users of OPSS with clinic-based services.20 32–36
Table 1.
Overview of included studies
| Service | Author (year) | Study type | Study aims | Demographic characteristics captured | ||||
| Gender | Age | Ethnicity | Sexual orientation | IMD | ||||
| eSexual Health Clinic (eSHC) | Aicken et al 201851 | Qualitative interviews | To understand use and experience of the eSHC to inform future evaluation and refinement | Binary | 18–35 | ✓ | ✓ | – |
| Estcourt et al 201749 | Quasi-experimental | To assess the safety and feasibility of eSHC | Binary | 18+ | ✓ | ✓ | – | |
| Gibbs et al 201838 | Mixed-methods evaluation of quasi-experimental study | To evaluate the eSHC results service | – | – | – | – | – | |
| Freetest.me | Dolan and Rudisill 201439 | Quasi-experimental | To explore the effect on chlamydia test return rates of non-cash financial incentives, and the influence of socioeconomic status | Binary | 16–24 | ✓ | – | Mean score |
| Letstalkaboutit | Gasmelsid et al 202134 | Observational | To determine whether online screening is accessible by those patients most at need by comparing the demographics and number of asymptomatic chlamydial infections detected online and in clinic | Binary | <25, 25+ | ✓ | ✓ | –** |
| National Chlamydia Screening Programme (NCSP) | Woodhall et al 20125 | Observational | To describe and evaluate access to the NCSP’s online chlamydia testing service | Binary | 15–24 | ✓ | – | ✓ |
| North East Essex Primary Care Trust (PCT) | Bracebridge et al 201240 | Observational | To quantify uptake and test-positivity rates, identify factors associated with screening and compare costs of the intervention with the NCSP | Binary | 17–25 | ✓ | – | ✓# |
| Saving Lives | Page et al 201947 | Observational | To ascertain how DBS HIV kits compared with MT kits in this postal testing service | Female, male, trans | Median 26 | ✓ | ✓ | – |
| Sexual Health London (SHL) | Day et al 202050 | Observational | To report the rate of recent sexual assault disclosure among users of SHL, and identify the outcomes of their call-back discussions | Female, male, trans or non-binary | 18–55 | ✓ | ✓ | – |
| Day et al 202143 | Observational | To assess the sexual health needs, sexual practices, STI/HIV positivity and satisfaction rates of trans and non-binary users of Sexual Health London | Female, male, trans, non-binary/gender fluid | 15–82 | ✓ | – | – | |
| Day et al 202048 | Observational | To report the safeguarding concerns and outcomes of those aged 16–17 years old accessing SHL | Female, male, trans or non-binary | 16–17 | ✓ | ✓ | – | |
| Day et al 202161 | Observational | To identify the characteristics and transfer to care rates of those who have a reactive HIV test result via SHL | Binary | 21–50 | ✓ | ✓ | – | |
| SH:24 | Barnard et al 201832 | Observational | To compare the characteristics of e-STI service users with clinic users, and OPSS kit returners with non-returners | Binary | 16+ | ✓ | ✓ | ✓ |
| Barnard 2020 (Chapter 6)52 | Qualitative interviews | To describe the experiences, barriers and facilitators of SH:24 in Lambeth and Southwark | Female, male, trans | 16–30 | ✓ | ✓ | – | |
| Syred et al 201937 | Observational | To describe user choice of OPSS orders and diagnoses in a ‘choose to test’ intervention | Binary | 16–24 | ✓ | ✓ | ✓ | |
| Turner et al 201820 | Observational | To investigate the effect of decision-making on resource allocation in a clinic after the introduction of an e-STI service in Lambeth and Southwark | Binary | 16+ | ✓ | ✓ | – | |
| Turner et al 201933 | Observational and model generation | To establish cost-effectiveness of an OPSS service, and explore cost per diagnosis in different scenarios | – | – | – | – | – | |
| Wilson et al 201744 | Experimental | To assess the effectiveness of an OPSS service compared with face-to-face services | Female, male, trans | 16–30 | ✓ | ✓ | – | |
| Wilson et al 201945 | Secondary data analysis of experimental study | To examine the effect of an e-STI service on testing uptake on people who had never previously tested (never-testers) | Female, male, trans | 16–30 | ✓ | ✓ | – | |
| TakeATestUK.com | Page et al 202141 | Observational | To ascertain how DBS HIV and syphilis kits compared with MT kits in this postal testing service | Female, male, trans | Mean 27 | ✓ | ✓ | – |
| Umbrella | Banerjee et al 201835 | Observational | To evaluate the rates of uptake and return of OPSS kits and compare patient demographics and clinical outcomes in home and clinic testers | Female, male, trans | 16+ | ✓ | ✓ | – |
| Banerjee et al 202036 | Observational | To evaluate the uptake, return rate and new diagnosis rates of home-based testing in comparison with clinic-based testing for HIV, syphilis and hepatitis B | Female, male, trans | 16+ | ✓ | ✓ | – | |
| Manavi and Hodson 201746 | Observational | To establish which factors influence return of OPSS kits | Female, male, trans | – | – | – | IMD rank | |
** Unstated, but reported as no difference between groups # Bracebridge et al. 2012 have labelled IMD quintile 1 as least deprived and IMD quintile 5 as most deprived in their paper. This may be an error and makes this data difficult to interpret. The corresponding author has been contacted for clarification.
DBS, dried blood sample; IMD, Index of Multiple Deprivation; MT, mini-test; OPSS, online postal self-sampling.
As standardised definitions were not used across the included studies for terms such as ‘access’, ‘usage’ or ‘demand’, we have not attempted to define related terms in this scoping review.
Characteristics of those accessing OPSS services
Comprehensive demographic data were not consistently collected across studies, in terms of both type of data collected and what was collected (see table 1). Only two studies collected demographic data on all of gender, age, ethnicity, sexual orientation and the Index of Multiple Deprivation (IMD)32 37; two collected none of these items.20 38 In addition to age and gender, 6 studies collected IMD data, 17 collected sexual orientation and 21 collected ethnicity, the majority of which were described in different ways using a variety of groupings. Gender types captured also varied between studies, with 2 that did not collect these data, and 10 only reporting binary types.
Those who accessed services tended to be majority women (56.7%–69.4% women, five studies reported statistical significance),5 20 32 34–36 39–41 were residents in less deprived areas compared with accessing testing in other settings (p<0.001),5 32 39 40 white or white British (53.3%–92% users, four studies reported statistical significance),5 32 34–36 39 41 and 20 years old or over (95.4% when compared with any age group,20 32 32.0%–42.9% when c.f. people aged 20–2540 42), with two studies reporting statistical significance.20 32
In those studies that collected more comprehensive gender data, people who identified as gender diverse made up a small proportion of the overall population accessing the service (0.0%–0.4%).35 36 41 43–46
There were limited and conflicting data on access according to sexual orientation; one study reported more MSM requesting access than heterosexual men,32 and one study found that a higher proportion of people identifying as non-heterosexual accessed online self-sampling compared with clinic-based testing (OR 0.44, 95% CI 0.27 to 0.72).34 This is in contrast to findings from the Umbrella service, Birmingham.36
Those accessing online services sometimes displayed higher risk behaviours,5 39 but often had a greater proportion of negative test results compared with clinic-based populations.32 33 35 36 Individuals were more likely to order OPSS kits if they had used STI testing services before.39 Of those who were never-testers, a significant proportion was recruited face-to-face in communities.45
Usage of OPSS services
The proportion of users returning self-sampling test kits varied by study (range 48.3%–78.4%).32 35 36 43 Women were more likely than men to access and return STI self-sampling kits in the majority of studies.20 32 35 36 39 40 46 One service evaluation found no difference between kit return rates between those identifying as gender diverse and those identifying as cisgender (OR 1.00, 95% CI 0.81 to 1.24), although successful return (OR 1.6, 95% CI 1.06 to 2.36) and successful testing (OR 1.2, 95% CI 0.87 to 1.66) of blood samples were higher in those identifying as trans or non-binary/gender fluid.43 Characteristics of those who returned test kits varied between studies for age32 36 39 and by level of deprivation.39 46 However, across several studies, people of white ethnicity were more likely to return the kit compared with other ethnicities.32 35 36
A study that evaluated those accessing an OPSS spontaneously, compared with those who attended clinic and were triaged to testing online, found that the return rate was slightly lower in the triage and signpost group compared with the spontaneous online group (67.0% vs 70.5% by 6 weeks, respectively).20
There are limited data on return rate of blood sampling kits, with one study finding only 54.4% (9033 of 16 611) of people returned a blood sample with a sufficient quantity of blood for testing.36 Studies that examined different types of blood sampling kits found no difference between return rates for dried blood samples (DBS) versus mini-tests (MTs) (66.5% vs 68.7%),47 but did find that the samples were significantly more likely to be successfully processed with DBS (94.6%–98.8%) compared with MT (55.7%–54.5%, p<0.001).41 47
Impact of OPSS services on demand
In many areas, the introduction of OPSS services was not associated with a change in numbers of people attending clinics, but increased the overall demand for STI testing services.20 33 44
Impact on clinical outcomes
Test positivity
Overall, test positivity for chlamydia and gonorrhoea was lower in OPSS services (4.4%–8.1%) than clinic-based services (10.3%–14.4%).32 35 Two studies found a low HIV prevalence in their OPSS testing population; 0.1% (144 of 148 257)48 and 0.8% (75 of 16 611)36 of users in the evaluation period had a reactive HIV result. Of these, 65.3%36 and 91.6%48 had confirmatory testing, and 1.3% (1 of 75)36 and 23.6% (34 of 144) had a new diagnosis of HIV confirmed. When comparing DBS and MT for HIV self-sampling, MT was found to have a higher proportion of reactive tests (6.2% vs 0.5%),41 lower proportion of confirmed reactive tests (n=1 of 30 (3.3%) vs 1 of 11 (9.1%))41 and higher false positive tests (5.2%–5.4% vs 0.0%–0.4%).41 47 However, these were service evaluations and the blood sampling kit options were offered sequentially rather than in parallel, so the populations being compared are not directly comparable. In addition, the tests were not compared with the results of a gold standard test (HIV Ab/Ag test), and the authors were unable to provide sensitivity and specificity data.47 These results should therefore be interpreted with caution.
Time to treatment
There were varied results regarding time to treatment; one paper reported that online patients took longer to receive treatment than clinic users,35 and one study found that there was no statistically significant difference.44 When an entire care pathway was trialled online and asymptomatic chlamydia-positive individuals could access an automated online clinical consultation which allowed people to collect their treatment at a community pharmacy, median time to treatment was 1 day (IQR 0–1).49 A study comparing outcomes of asymptomatic service users testing positive for chlamydia via clinic-based services and online found that those diagnosed online were less likely to wait more than a week for treatment compared with those diagnosed in clinic (OR 9.94, 95% CI 2.87 to 34.42).34
Reporting sexual assault and safeguarding outcomes
When evaluating outcomes of those people who reported online a recent sexual assault over a 6-month period in 2020, one service found that 0.5% (n=242 of 45 841) of users indicated they had been a victim of a recent sexual assault, which led to telephone intervention by a clinical healthcare professional. Of these, nearly 80% of people were contacted. However, 41.7% (n=101 of 242) of users stated that they had not intended to report recent sexual assault. Fifteen people had already reported the sexual assault and had been seen by the police or by a Sexual Assault Referral Centre (SARC). One person required a SARC referral, and eight people were referred to a clinic-based service.50 The same service also evaluated their safeguarding outcomes in those aged 16–17 years old, finding that a high proportion of this population (42.5%) met the service criteria for a follow-up telephone call from a health advisor. The most frequent reason that a call was triggered was related to drug and alcohol use (27%). The outcome of 8.5% of calls was a discussion with the child protection team, with 7.0% requiring a referral or discussion with social services.48 There was no evidence as to whether safeguarding opportunities were missed, or an in-depth understanding of the acceptability of providing this information in an online setting.
Acceptability of OPSS services
Qualitative research showed the importance of trust, confidentiality, discretion, reliability, convenience and improved patient choice in ensuring the successful use of OPSS,51 52 and between 71.1% and 98.0% of individuals surveyed expressed that they were pleased with and found these services acceptable.38 44 45
Economics
Although this review did not specifically set out to evaluate the economic outcomes of OPSS services, only one study included any costing data.33 This study, evaluating the impact of online testing across specialist SHS in two London boroughs found that, although there was an increase in the total annual cost of STI testing following the introduction of online testing, the average cost per test and diagnosis decreased.33
Discussion
Although evaluations of OPSS of variable quality were found, we did not identify any large-scale, multicentre robust studies. Available evidence suggests that OPSS services appear to be more likely to be used by, and acceptable to, asymptomatic individuals who are predominately women, over 20 years of age, residents in less deprived areas and of white ethnicities, when compared with clinic-based populations. There is preliminary evidence that people from groups experiencing a disproportionate burden of STIs use OPSS less than other groups. The heterogeneity of the included studies prevented full evaluation of clinical outcomes.
Online services tend to be targeted at asymptomatic individuals who do not have other sexual health needs. The ability for asymptomatic people to manage their care needs remotely is an important and useful contribution to detect symptomless STIs, in order to enable treatment of the index patient and partner notification, and reduce morbidity and onward transmission. However, asymptomatic users reported higher risk behaviours in some studies,5 39 and there were no data on the impact of using OPSS on future sexual behaviour. In addition, there was insufficient evidence to be able to establish the impact of OPSS on treatment and partner notification outcomes.
Women were more likely than men to access and return STI self-sampling kits in the majority of studies.20 32 35 39 40 46 For services that provided accessibility information by sexual orientation, MSM seemed to be successfully using OPSS services.32 46 This finding is consistent with those from an OPSS in Canada.53 Certain minority ethnic groups such as black Caribbean, black African and mixed ethnicities, who are also key populations who are at higher risk of poor sexual health, were under-represented in OPSS users,11 perhaps due to a preference for face-to-face care.52
Some services appear to appropriately reach younger people, but other services were more popular with those aged over 20 years.35 This could be because younger people are more likely to live at home and have concerns about parents finding a test kit delivered through the post.54 Using chlamydia as an exemplar, chlamydia has formed 49% of new STI diagnoses in 2019, yet there has been a 13% reduction in tests completed by young people since 2015.11 Chlamydia is the most commonly reported STI in the UK, and disproportionately affects young people from deprived areas,42 so it is crucial to ensure services are targeting these groups within their region. Despite this, recent research shows that both men (adjusted OR (aOR): 1.36 (95% CI: 1.35 to 1.39), p<0.001) and women (aOR: 1.32 (95% CI: 1.31 to 1.33), p<0.001) living in the least deprived quintile were more likely to use OPSS services for chlamydia screening than those from the most deprived quintile.55
Understanding inequalities in access and usage of OPSS services requires services to collect comprehensive sociodemographic data. Of the 15 included studies, only 2 collected gender, age, ethnicity, sexual orientation and IMD data.32 37 Most studies included categories such as ‘other’ ethnicity or sexual orientation and though a few included trans participants, only one described people of non-binary, gender fluid or other genders.43 This data gap results in not only a skewed understanding of the impact of STIs on minorities, but also ‘facilitates the erasure of communities’.18 Further, the inter-relations between demographic groups have not been sufficiently examined in these studies despite reference in the literature20 42 56 (eg, 4, 11, 65).
Return rates of blood samples that were sufficient for testing were relatively low, and in keeping with findings from the national HIV self-sampling service.57 Overall test positivity was lower in OPSS services compared with clinic-based services.32 36 This is in keeping with, but more marked than, findings from both selective and unselective national datasets.10 57 As highlighted within one study, the low positive predictive value (PPV) for home-based BBV testing is concerning36 and requires further evaluation from both a cost-effectiveness and well-being perspective.
To our knowledge, this is the first review to explore the accessibility of OPSS services in the UK. The inclusion of qualitative as well as quantitative studies ensured that both acceptability and core themes regarding people’s access to and use of services could be explored. The included studies were heterogeneous in design using a variety of methodologies which added value to the review. By excluding hypothetical studies, acceptability and barriers to service use are indicative of the real-life experience of online service users.
Fourteen of 23 studies took place in London and no studies were conducted in Wales, Scotland or Northern Ireland, so findings may not be generalisable to all of the UK. This review did not set out to evaluate partner notification or economic outcomes of OPSS services, but the authors observed that there was a dearth of information on these within the studies that were included in this review. This study only focused on the UK setting as it was focusing on access, and the infrastructure of SHS provision in the UK is different to other settings. However, the findings relating to acceptability and convenience are similar to those reported in systematic review and synthesis of qualitative research on OPSS services.54
OPSS services appear acceptable to current users and improve choice, but evaluation is limited. The existing evidence suggests that successful services achieve reliability, privacy, convenience, trust and are integrated with clinic-based services to provide ease of transition between modalities of care. Online services are successful in relieving pressure from clinics,58 but clinic-based services remain essential for symptomatic individuals, people who have digital constraints and those who prefer face-to-face care and or require additional safeguarding, among others.18 Further research is required to understand impact on clinical outcomes, including safeguarding opportunities.
With the extensive expansion in provision of OPSS services in recent years, a large-scale, multicentre evaluation is needed to determine their cost-effectiveness and impact on access, clinical outcomes and service delivery. In addition to more targeted evaluations, it would be beneficial to conduct a holistic evaluation across all service modalities (including face-to-face services). Clinical outcomes are key to understanding the cost-effectiveness of these services and there is limited research into this important factor. Further research is required to understand why people aged under 20 years have lower uptake, and whether this is related to, for example, an individual’s experience of autonomy, competence and relatedness59 and how awareness and access can be improved for these individuals.60
Footnotes
Handling editor: Alec Miners
Twitter: @KarenCLloyd, @jogibbs76
Correction notice: This article has been corrected since it was first published online. 'Clinic' was changed to 'clinical' in the title.
Contributors: KS conducted the original scoping review to fulfil requirements of KS’ Masters dissertation, supervised by JG and KCL. JG, KCL, KS, CSE and FB conceived of the original idea. KS, JG and KCL contributed to the design of the study. KS led, and KCL and JG contributed to the establishment of the search strategy and method of analysis. The original article reviewing and data analysis were led by KS, with contribution from KCL and JG. The updated article review and data analysis were led by JG, with contribution from KCL and KS. All authors (KS, KCL, CSE, FB and JG) have made contributions to the drafting and revising of the article, and have approved the final version.
Funding: Not applicable.
Competing interests: FB, CSE and JG report receiving NIHR funding to research digital sexual health (NIHR129157 (FB, JG) and NIHR200856 (CSE, JG)). CSE and JG are associate editors for STI journal, and have coauthored three papers included within this review.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not applicable.
References
- 1. Harding-Esch EM, Hollis E, Mohammed H, et al. Self-Sampling and self-testing for STIs and HIV: the case for consistent nomenclature. Sex Transm Infect 2017;93:445–8. 10.1136/sextrans-2016-052841 [DOI] [PubMed] [Google Scholar]
- 2. Gilbert M, Thomson K, Salway T, et al. Differences in experiences of barriers to STI testing between clients of the Internet-based diagnostic testing service GetCheckedOnline.com and an STI clinic in Vancouver, Canada. Sex Transm Infect 2019;95:151–6. 10.1136/sextrans-2017-053325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Greenland KE, Op de Coul ELM, van Bergen JEAM, et al. Acceptability of the Internet-based Chlamydia screening implementation in the Netherlands and insights into nonresponse. Sex Transm Dis 2011;38:467–74. 10.1097/OLQ.0b013e318204546e [DOI] [PubMed] [Google Scholar]
- 4. Chai SJ, Aumakhan B, Barnes M, et al. Internet-Based screening for sexually transmitted infections to reach nonclinic populations in the community: risk factors for infection in men. Sex Transm Dis 2010;37:756–63. 10.1097/OLQ.0b013e3181e3d771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Woodhall SC, Sile B, Talebi A, et al. Internet testing for Chlamydia trachomatis in England, 2006 to 2010. BMC Public Health 2012;12:1–8. 10.1186/1471-2458-12-1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. FriskyWales . FriskyWales webpage, 2020. Available: https://www.friskywales.org/chlamydia-and-gonorrhoea-home-testing-pilot.html [Accessed 29 Sep 2020].
- 7. Estcourt CS. Reference type: personal communication, 2020. [Google Scholar]
- 8. SH:24. About SH:24 [Internet], 2020. Available: https://sh24.org.uk/about-sh24 [Accessed 30 Sep 2020].
- 9. British Association for Sexual Health and HIV. Standards for the Management of STIs [Internet], 2019. Available: https://www.bashh.org/about-bashh/publications/standards-for-the-management-of-stis/ [Accessed 30 Sep 2020].
- 10. Public Health England . Sexually transmitted infections and screening for Chlamydia in England, 2019, 2020. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/914184/STI_NCSP_report_2019.pdf [Accessed 29 Sep 2020].
- 11. Public Health England . Sexually transmitted infections and screening for Chlamydia in England, 2020, 2021. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1015176/STI_NCSP_report_2020.pdf [Accessed 10 Oct 2021].
- 12. Mercer CH, Tanton C, Prah P, et al. Changes in sexual attitudes and lifestyles in Britain through the life course and over time: findings from the National surveys of sexual attitudes and lifestyles (Natsal). The Lancet 2013;382:1781–94. 10.1016/S0140-6736(13)62035-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ford K, Sohn W, Lepkowski J. Characteristics of adolescents' sexual partners and their association with use of condoms and other contraceptive methods. Fam Plann Perspect 2001;33:100. 10.2307/2673765 [DOI] [PubMed] [Google Scholar]
- 14. Wayal S, Hughes G, Sonnenberg P, et al. Ethnic variations in sexual behaviours and sexual health markers: findings from the third British national survey of sexual attitudes and lifestyles (Natsal-3). Lancet Public Health 2017;2:e458–72. 10.1016/S2468-2667(17)30159-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Daskalopoulou M, Rodger AJ, Phillips AN, et al. Condomless sex in HIV-diagnosed men who have sex with men in the UK: prevalence, correlates, and implications for HIV transmission. Sex Transm Infect 2017;93:590–8. 10.1136/sextrans-2016-053029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Curtis TJ, Rodger AJ, Burns F, et al. Patterns of sexualised recreational drug use and its association with risk behaviours and sexual health outcomes in men who have sex with men in London, UK: a comparison of cross-sectional studies conducted in 2013 and 2016. Sex Transm Infect 2020;96:197–203. 10.1136/sextrans-2019-054139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sewell J, Cambiano V, Miltz A, et al. Changes in recreational drug use, drug use associated with chemsex, and HIV-related behaviours, among HIV-negative men who have sex with men in London and Brighton, 2013-2016. Sex Transm Infect 2018;94:494–501. 10.1136/sextrans-2017-053439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Terrence Higgins Trust,, British Association for Sexual Health and HIV . The state of the nation sexually transmitted infections in England, 2020. Available: https://www.tht.org.uk/sites/default/files/2020-02/StateofThenationReport.pdf [Accessed 30 Sep 2020].
- 19. Robertson R, Wenzel L, Thompson J. Understanding NHS financial pressures - How are they affecting patient care? 2017. Available: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/UnderstandingNHSfinancial pressures-fullreport.pdf [Accessed 28 Jul 2020].
- 20. Turner KM, Zienkiewicz AK, Syred J, et al. Web-Based activity within a sexual health economy: observational study. J Med Internet Res 2018;20:e74. 10.2196/jmir.8101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kersaudy-Rahib D, Lydié N, Leroy C, et al. Chlamyweb Study II: a randomised controlled trial (RCT) of an online offer of home-based Chlamydia trachomatis sampling in France. Sex Transm Infect 2017;93:188–95. 10.1136/sextrans-2015-052510 [DOI] [PubMed] [Google Scholar]
- 22. British Association for Sexual Health and HIV . Principles for Recovery for out-patient Genitourinary Medicine, Contraception and Sexual Health Services and outpatient HIV Services Summary of Document & Purpose, 2020. Available: https://members.bashh.org/Documents/COVID-19/PrinciplesforRecoveryofSexualHealthDraft08.06.2020-forwebsiteupload.pdf
- 23. Khalil H, Peters M, Godfrey CM, et al. An evidence-based approach to scoping reviews. Worldviews Evid Based Nurs 2016;13:118–23. 10.1111/wvn.12144 [DOI] [PubMed] [Google Scholar]
- 24. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 25. Lefebvre C, Glanville J, Briscoe S, et al. Chapter 4: searching for and selecting studies. Cochrane Handbook for systematic reviews of interventions (version 6.0), 2019. [Google Scholar]
- 26. Paez A. Gray literature: an important resource in systematic reviews. J Evid Based Med 2017;10:233–40. 10.1111/jebm.12266 [DOI] [PubMed] [Google Scholar]
- 27. Pagliari C, Sloan D, Gregor P, et al. What is eHealth (4): a scoping exercise to map the field. J Med Internet Res 2005;7:e9. 10.2196/jmir.7.1.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ayiku L, Levay P, Hudson T, et al. The Medline UK filter: development and validation of a geographic search filter to retrieve research about the UK from OVID Medline. Health Info Libr J 2017;34:200–16. 10.1111/hir.12187 [DOI] [PubMed] [Google Scholar]
- 29. Ayiku L, Levay P, Hudson T, et al. The Embase UK filter: validation of a geographic search filter to retrieve research about the UK from OVID Embase. Health Info Libr J 2019;36:121–33. 10.1111/hir.12252 [DOI] [PubMed] [Google Scholar]
- 30.et alNha HONG Q, Pluye P, bregues S F. Mixed methods appraisal tool (MMAT) version 2018 user guide, 2018. Available: http://mixedmethodsappraisaltoolpublic.pbworks.com/ [Accessed 28 Sep 2020].
- 31. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 32. Barnard S, Free C, Bakolis I, et al. Comparing the characteristics of users of an online service for STI self-sampling with clinic service users: a cross-sectional analysis. Sex Transm Infect 2018;94:377–83. 10.1136/sextrans-2017-053302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Turner KME, Looker KJ, Syred J, et al. Online testing for sexually transmitted infections: a whole systems approach to predicting value. PLoS One 2019;14:e0212420. 10.1371/journal.pone.0212420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gasmelsid N, Moran BC, Nadarzynski T, et al. Does online sexually transmitted infection screening compromise care? A service evaluation comparing the management of chlamydial infection diagnosed online and in clinic. Int J STD AIDS 2021;32:528–32. 10.1177/0956462420980929 [DOI] [PubMed] [Google Scholar]
- 35. Banerjee P, Thorley N, Radcliffe K. A service evaluation comparing home-based testing to clinic-based testing for Chlamydia and gonorrhoea in Birmingham and Solihull. Int J STD AIDS 2018;29:974–9. 10.1177/0956462418767180 [DOI] [PubMed] [Google Scholar]
- 36. Banerjee P, Madhwapathi V, Thorley N, et al. A service evaluation comparing home-based testing to clinic-based testing for HIV, syphilis and hepatitis B in Birmingham and Solihull. Int J STD AIDS 2020;31:613–8. 10.1177/0956462419900461 [DOI] [PubMed] [Google Scholar]
- 37. Syred J, Holdsworth G, Howroyd C, et al. Choose to test: self-selected testing for sexually transmitted infections within an online service. Sex Transm Infect 2019;95:171–4. 10.1136/sextrans-2018-053796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gibbs J, Aicken CRH, Sutcliffe LJ, et al. Mixed-Methods evaluation of a novel online STI results service. Sex Transm Infect 2018;94:622–4. 10.1136/sextrans-2017-053318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dolan P, Rudisill C. The effect of financial incentives on Chlamydia testing rates: evidence from a randomized experiment. Soc Sci Med 2014;105:140–8. 10.1016/j.socscimed.2013.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bracebridge S, Bachmann MO, Ramkhelawon K, et al. Evaluation of a systematic postal screening and treatment service for genital Chlamydia trachomatis, with remote clinic access via the Internet: a cross-sectional study, East of England. Sex Transm Infect 2012;88:375–81. 10.1136/sextrans-2011-050267 [DOI] [PubMed] [Google Scholar]
- 41. Page M, Atabani S, Arumainayagam J, et al. Are all blood-based postal sampling kits the same? A comparative service evaluation of the performance of dried blood spot and mini tube sample collection systems for postal HIV and syphilis testing. Sex Transm Infect 2021;97:209–14. 10.1136/sextrans-2020-054692 [DOI] [PubMed] [Google Scholar]
- 42. Woodhall SC, Soldan K, Sonnenberg P, et al. Is Chlamydia screening and testing in Britain reaching young adults at risk of infection? findings from the third national survey of sexual attitudes and lifestyles (Natsal-3). Sex Transm Infect 2016;92:218–27. 10.1136/sextrans-2015-052013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Day S, Smith J, Perera S, et al. Beyond the binary: sexual health outcomes of transgender and non-binary service users of an online sexual health service. Int J STD AIDS 2021;32:896–902. 10.1177/0956462420982830 [DOI] [PubMed] [Google Scholar]
- 44. Wilson E, Free C, Morris TP, et al. Internet-accessed sexually transmitted infection (e-STI) testing and results service: a randomised, single-blind, controlled trial. PLoS Med 2017;14:e1002479. 10.1371/journal.pmed.1002479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wilson E, Leyrat C, Baraitser P, et al. Does internet-accessed STI (e-STI) testing increase testing uptake for Chlamydia and other STIs among a young population who have never tested? secondary analyses of data from a randomised controlled trial. Sex Transm Infect 2019;95:569–74. 10.1136/sextrans-2019-053992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Manavi K, Hodson J. Observational study of factors associated with return of home sampling kits for sexually transmitted infections requested online in the UK. BMJ Open 2017;7:e017978. 10.1136/bmjopen-2017-017978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Page M, Atabani SF, Wood M, et al. Dried blood spot and mini-tube blood sample collection kits for postal HIV testing services: a comparative review of successes in a real-world setting. Sex Transm Infect 2019;95:43–5. 10.1136/sextrans-2018-053567 [DOI] [PubMed] [Google Scholar]
- 48. Day S, Kinsella R, Jones S, et al. Safeguarding outcomes of 16 and 17-year-old service users of sexual health London (SHL.uk), a pan-London online sexual health service. Int J STD AIDS 2020;31:1373–9. 10.1177/0956462420933462 [DOI] [PubMed] [Google Scholar]
- 49. Estcourt CS, Gibbs J, Sutcliffe LJ, et al. The eSexual health clinic system for management, prevention, and control of sexually transmitted infections: exploratory studies in people testing for Chlamydia trachomatis. Lancet Public Health 2017;2:e182–90. 10.1016/S2468-2667(17)30034-8 [DOI] [PubMed] [Google Scholar]
- 50. Day S, Singh GJ, Jones S, et al. Sexual assault reporting amongst users of online sexual health services. Int J STD AIDS 2021;32:280–5. 10.1177/0956462420963940 [DOI] [PubMed] [Google Scholar]
- 51. Aicken CRH, Sutcliffe LJ, Gibbs J, et al. Using the eSexual health clinic to access Chlamydia treatment and care via the Internet: a qualitative interview study. Sex Transm Infect 2018;94:241–7. 10.1136/sextrans-2017-053227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Barnard SL. Access to online services for sexually transmitted infection self-sampling at home [Internet]. [London]: King’s College London, 2020. Available: https://kclpure.kcl.ac.uk/portal/en/theses/access-to-online-services-for-sexually-transmitted-infection-selfsampling-at-home(7e625417-c622-4cdf-a8f6-e82e44e5bcb0).html [Accessed 20 Aug 2020].
- 53. Gilbert M, Salway T, Haag D, et al. Use of GetCheckedOnline, a comprehensive web-based testing service for sexually transmitted and blood-borne infections. J Med Internet Res 2017;19:e81. 10.2196/jmir.7097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Spence T, Kander I, Walsh J, et al. Perceptions and experiences of Internet-based testing for sexually transmitted infections: systematic review and synthesis of qualitative research. J Med Internet Res 2020;22:e17667. 10.2196/17667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sonubi T, Allen H, Kuyumdzhieva G, et al. The relationship between socioeconomic deprivation and chlamydia screening in England - an analysis of national surveillance data, 2015-2019. In: Poster presented at: BASHH Annual Conference 2020, Virtual, 2020. [Google Scholar]
- 56. Furegato M, Chen Y, Mohammed H, et al. Examining the role of socioeconomic deprivation in ethnic differences in sexually transmitted infection diagnosis rates in England: evidence from surveillance data. Epidemiol Infect 2016;144:3253–62. 10.1017/S0950268816001679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Public Health England . National HIV self-sampling service: November 2018 to October 2019, 2020. Available: www.test.hiv [Accessed 5 Dec 2021].
- 58. Department of Health and Social Care . Government Response to the Health and Social Care Committee report on Sexual Health - CP186, 2019. Available: www.gov.uk/official-documents [Accessed 29 Sep 2020].
- 59. Morrison LG. Theory-based strategies for enhancing the impact and usage of digital health behaviour change interventions: a review. Digit Health 2015;1:205520761559533. 10.1177/2055207615595335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Munro CH, Patel R, Brito-Mutunayagam S. FSRH/BASHH Standards for Online and Remote Providers of Sexual and Reproductive Health Services - January 2019, 2020. Available: https://www.fsrh.org/standards-and-guidance/documents/fsrhbashh-standards-for-online-and-remote-providers-of-sexual/
- 61. Day S, Khan K, Kelly AM, et al. Characteristics of newly diagnosed HIV-positive service users using a pan-London e-sexually transmitted infection screening service. Int J STD AIDS 2021;32:1036–42. 10.1177/09564624211014729 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
sextrans-2021-055376supp001.pdf (456.3KB, pdf)