Nutcracker phenomenon (NCP) occurs when the left renal vein (LRV) is excessively compressed between the abdominal aorta (AA) and the superior mesenteric artery (SMA) [1]. It is called nutcracker syndrome (NCS) when NCP is accompanied by otherwise-unexplainable symptoms or signs, such as hematuria, proteinuria, or left flank pain. NCS is rare, but its exact prevalence remains unknown [2]. NCS is registered as a rare condition on medical websites, such as the Genetic and Rare Diseases Information Center at the National Institutes of Health (NIH-GARD) and Orphanet [2]. This letter alerts readers that this syndrome may be much more common than previously thought. Kim [3] reported, “we may assume that NCS may not be a rare entity, and the prevalence may be higher than previously thought.”
We investigated the prevalence of NCP and NCS in a kidney-specialty referral clinic in 1223 consecutive patients who underwent Doppler ultrasound (US) examinations. A peak flow velocity > 100 cm/s at the aortomesenteric LRV was a Doppler criterion of NCP. Approximately 30% and 15% of the patients were diagnosed with NCP and NCS, respectively, and the results were presented at the 2020 Annual Congress of the Korean Society of Ultrasound in Medicine [4]. Although the results were from a single kidney-specialty referral clinic, they suggest that NCP and NCS may not be rare conditions.
In the same kidney-specialty referral clinic, we further investigated the NCP and NCS and enrolled 1475 patients. The demographic, clinical, and Doppler US characteristics of the patients are summarized in Table 1. There were 715 patients with NCP and 760 with NCS. Both NCP and NCS were more common in women than in females. Common symptoms or signs were gross or microscopic hematuria, proteinuria, or left flank pain. Other symptoms or signs possibly related to NCS included pain or discomfort in other areas of the abdomen or pelvis, bladder symptoms like frequent urination or nocturia, foamy urine, and fluctuating glomerular filtration rates. In 1475 patients with NCP or NCS, Doppler US findings other than high peak flow velocity of the aortomesenteric LRV showed scanty color flow signals at the proximal LRV, indicating sluggish flow, and prominent flow signals in the pelvic cavity, indicating pelvic congestion.
Table 1. Demographic and Characteristics of NCP and NCS.
| Total | NCP | NCS | |||
|---|---|---|---|---|---|
| Age, median (IQR) | 56 (40–66) | 59 (4–67) | 53 (37–64) | ||
| Sex | |||||
| Female | 948 | 397 | 551 | ||
| Male | 527 | 318 | 209 | ||
| Total | 1475 | 715 | 760 | ||
| Symptoms | |||||
| Gross hematuria | 66 | 18 | 48 | ||
| Microscopic hematuria | 545 | 143 | 402 | ||
| Proteinuria | 728 | 217 | 511 | ||
| Left flank pain | 68 | 5 | 63 | ||
| Bladder symptoms | 113 | 47 | 66 | ||
| Fluctuating GFR | 100 | 61 | 39 | ||
| Doppler US findings | |||||
| Type | |||||
| 1 | 384 | 141 | 243 | ||
| 2 | 746 | 377 | 369 | ||
| 3 | 345 | 197 | 148 | ||
| Sluggish LRV flow | 633 | 299 | 334 | ||
| Pelvic congestion | 565 | 252 | 313 | ||
Data are number of patients except for age, which is year. GFR = glomerular filtration rate, IQR = interquartile range, LRV = left renal vein, NCP = nutcracker phenomenon, NCS = nutcracker syndrome, US = ultrasound
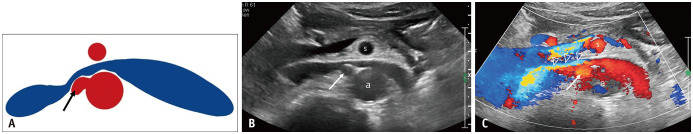
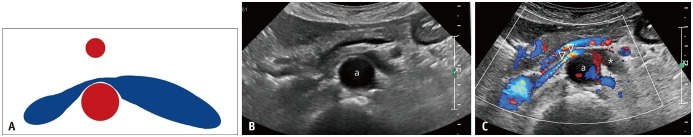
Doppler US images were saved in cine mode in all patients, and cine clips were reviewed to categorize the LRV compression patterns. There were three patterns of LRV compression in the aortomesenteric area: classical compression in the narrow space between the AA and SMA (type 1) (Fig. 1), compression of the LRV posteriorly by the origin of the right renal artery (type 2) (Fig. 2), and narrowed and stretched LRV anterior to the AA (type 3) (Fig. 3). Some patients showed mixed patterns and were categorized according to their dominant pattern. Type 2 compression was more common than type 1 or type 3 compressions.
Fig. 1. Type 1 NCP.
A. Schematic diagram showing the compression of the LRV in the narrow space between the AA and SMA. B, C. Type 1 compression of the LRV in a 33-year-old female with proteinuria. Greyscale (B) and color Doppler US (C) images show a tightly compressed LRV (arrow) between the AA (a) and SMA (s) and a dilated proximal LRV (asterisk). Note the bright-colored jetting of blood flow (arrowheads) from the aortomesenteric LRV. Supplementary video 1 is a video-clip of color Doppler US (C). AA = abdominal aorta, IVC = inferior vena cava, LRV = left renal vein, NCP = nutcracker phenomenon, SMA = superior mesenteric artery, US = ultrasound
Fig. 2. Type 2 nutcracker phenomenon.
A. Schematic diagram showing the compression of the LRV posteriorly by the origin of the right renal artery (arrow). B, C. Type 2 compression of the LRV in a 68-year-old male with proteinuria. Greyscale (B) and color Doppler US (C) images of the LRV show that the space between the AA (a) and SMA (s) is not narrow, but the LRV is compressed posteriorly by the origin of the right renal artery (arrows). Note the bright-colored jetting of the blood flow (arrowheads) from the site where the right renal artery compresses the LRV. Supplementary video 2 is a video-clip of color Doppler US (C). AA = abdominal aorta, LRV = left renal vein, SMA = superior mesenteric artery, US = ultrasound
Fig. 3. Type 3 nutcracker phenomenon.
A. Schematic diagram of the LRV narrowed and stretched anterior to the AA. B, C. Type 3 compression of the LRV in a 74-year-old male with microscopic hematuria and proteinuria. Greyscale (B) and color Doppler US (C) images of the LRV show that the LRV is narrowed and stretched over the AA (a). Note the bright-colored jetting of the blood flow (arrowheads) from the site where the LRV is narrowed by stretching over the AA. In addition, scanty flow signals in the dilated proximal LRV indicate slow flow (asterisk). Supplementary video 3 is a video-clip of color Doppler US (C). AA = abdominal aorta, LRV = left renal vein, US = ultrasound
Although the data from a single kidney-specialty referral clinic may have overestimated the prevalence, we feel confident that NCP and NCS may not be rare conditions. NCS has various symptoms and signs, and there are at least three patterns of LRV compression in these conditions.
Footnotes
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Seung Hyup Kim, Eungtaek Kang, Suhnggwon Kim.
- Data curation: Taewho Yoon.
- Formal analysis: Taewho Yoon.
- Investigation: Taewho Yoon.
- Methodology: Seung Hyup Kim.
- Project administration: Seung Hyup Kim.
- Resources: Seung Hyup Kim.
- Supervision: Seung Hyup Kim.
- Visualization: Seung Hyup Kim, Taewho Yoon.
- Writing—original draft: Taewho Yoon.
- Writing—review & editing: Seung Hyup Kim, Eungtaek Kang, Suhnggwon Kim.
Funding Statement: None
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Supplement
The Supplement is available with this article at https://doi.org/10.3348/kjr.2022.0617.
The cine clip of the color Doppler US shows bright-colored flow jetting from the aortomesenteric LRV.
The cine clip of the color Doppler US shows bright-colored jetting of the blood flow from the site where the right renal artery compresses the LRV.
The cine clip of the color Doppler US shows bright-colored jetting of the blood flow from the site where the LRV is narrowed and stretched over the AA and slow flow in the dilated proximal LRV.
References
- 1.Kurklinsky AK, Rooke TW. Nutcracker phenomenon and nutcracker syndrome. Mayo Clin Proc. 2010;85:552–559. doi: 10.4065/mcp.2009.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Orphanet. Renal nutcracker syndrome. orpha.net Web site. [Accessed September 30, 2022]. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=GB&Expert=71273 .
- 3.Kim SH. Doppler US and CT diagnosis of nutcracker syndrome. Korean J Radiol. 2019;20:1627–1637. doi: 10.3348/kjr.2019.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim SH, Yoon T, Kang E. Nutcracker phenomenon and nutcracker syndrome, one-year experience at a nephrology-uroradiology clinic. ksum.or.kr Web site. [Accessed September 30, 2022]. https://2020.ksum.or.kr/file/KSUM_2020_Program_Abstract_Book.pdf .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The cine clip of the color Doppler US shows bright-colored flow jetting from the aortomesenteric LRV.
The cine clip of the color Doppler US shows bright-colored jetting of the blood flow from the site where the right renal artery compresses the LRV.
The cine clip of the color Doppler US shows bright-colored jetting of the blood flow from the site where the LRV is narrowed and stretched over the AA and slow flow in the dilated proximal LRV.
Data Availability Statement
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.