1. Introduction
Cervical cancer is the fourth most common cancer among women worldwide, with an estimated 570,000 new cases and over 310,000 deaths from cervical cancer each year [1,2]. Over 87% of all new cases and deaths occur in low- and lower-middle-income countries, largely because routine cervical cancer screening and treatment is not widely available [3]. Incidence of cervical cancer is highest in southern and eastern Africa [4]. The World Health Organization (WHO) recommends human papillomavirus (HPV) vaccination for girls 9–14 years old for the primary prevention of cervical cancer.
Following WHO recommendations, Gavi, the Vaccine Alliance (Gavi) has offered support to eligible countries for the introduction of HPV vaccine since 2012, initially through pilot introduction programs targeting 1–2 districts (<15,000 girls), followed by support for national HPV vaccine introduction. Countries could apply lessons learned from pilot programs to national scale-up. Subsequent to WHO’s 2017 HPV vaccine policy encouraging countries to vaccinate multiple-age cohorts in the first year of introduction, Gavi extended support for eligible countries to vaccinate multiple-age cohorts in the first year, followed by single-age cohorts each year thereafter [5]. Many eligible countries applied for Gavi support to vaccinate girls across multiple ages to reduce HPV prevalence and address high cervical cancer burden. In 2018, as more countries began introducing this vaccine, Gavi and global partners were informed by HPV vaccine manufacturers of vaccine supply constraints, stemming from the lack of manufacturing capacity [6–8]. With the increasing demand due to increasing country vaccine introductions, vaccine supply was insufficient for multiple-age cohort vaccination. Therefore, Gavi-eligible countries needed to make programmatic decisions on which age cohorts to vaccinate based on available vaccine stock.
This commentary discusses one country’s experience with HPV vaccination and programmatic decisions made as a result of vaccine supply constraints. It draws on information gathered during an evaluation of HPV introduction in Tanzania; the full description of nationwide HPV vaccine introduction in Tanzania is included in this same issue.
2. Tanzania’s national HPV vaccine introduction
In Tanzania, cervical cancer is the leading cause of female cancer, with almost 10,000 new cervical cancer cases and 7000 estimated deaths annually [1,9]. In a study of HIV-positive and HIV-negative women in Tanzania, the most prevalent types of HPV were HPV52 and HPV16 with HPV51, 35, 18, and 66 also common [10].
Beginning in 2014, Tanzania conducted a 2-year HPV vaccine pilot program with Gavi support in the Kilimanjaro region, targeting 9-year-old girls or older enrolled in Class 4 in school and 9-year-old girls out-of-school with two doses of the quadrivalent HPV vaccine administered with a six month interval between doses [11–13]. The Kilimanjaro region implemented a school-based campaign delivery strategy the first year of the pilot, followed by a routine delivery strategy the second year, using both fixed health facility and outreach sites (community, community mobile (>10 km from the health facility), and school sites) [14]. Following the Kilimanjaro pilot program, Kilimanjaro region continued to vaccinate 9-year-old girls using the routine delivery strategy, sponsored by the government of Tanzania.
After a successful pilot program, Tanzania applied to Gavi for national HPV vaccine introduction in 2017 targeting multiple age cohorts (all girls aged 9–14 years old). At the time of their application, there were two available HPV vaccine options with Gavi support: the bivalent and quadrivalent HPV vaccines. Tanzania selected the quadrivalent vaccine because it was successfully used during the pilot program in Kilimanjaro region, previously licensed by the Tanzania Food and Drug Authority, and was recommended by the Tanzania Immunization Technical Advisory Group (TAITAG) for national introduction [10,15]. However, due to global vaccine supply constraints, there was only sufficient stock for Tanzania to receive quadrivalent HPV vaccine supply for a single-age cohort. Tanzania chose to target 14-year-old girls for vaccination to promote equity and not miss any eligible girls, as girls become ineligible at age 15, however, the Kilimanjaro region would continue vaccination of 9-year-old girls. Tanzania sought to ensure the largest number of girls would be protected, expressing confidence in being able to reach this older age cohort because of high primary and secondary school enrollment throughout the country. When vaccine supply increases, Tanzania expects to vaccinate all 9–14-year-old girls, and then continue routine vaccination of 9-year-old girls, aligning the target age group nationally with Kilimanjaro region. At the time of this programmatic decision-making, Tanzania expected adequate supply for multiple-age cohort vaccination to become available 1–2 years after national introduction.
Tanzania used lessons learned from the pilot program to determine the best delivery strategy to reach this novel age group of adolescent girls; the pilot program utilized both campaign delivery and routine delivery strategies. Based on Kilimanjaro region’s experience and to ensure program sustainability, HPV vaccine was integrated into the routine immunization delivery system nationally. HPV vaccine is offered at health facilities and through community outreach, mobile outreach (>10 km from the health facility), and outreach to primary and secondary schools. It was thought that integration into the routine delivery system would capitalize on the existing immunization program resources.
Tanzania introduced HPV vaccine nationwide in April 2018, targeting 14-year-old girls throughout the country and continuing vaccination of 9-year-old girls in Kilimanjaro region, with two doses of the quadrivalent HPV vaccine administered with a minimum six-month interval between doses. Nationwide administrative coverage of the first dose of HPV vaccine was 78% and administrative coverage of the second dose of HPV vaccine was 49% at the end of 2019.
3. Challenges of program implementation with vaccine supply constraints in Tanzania
In Tanzania, the decision to introduce HPV vaccine nationally was driven by the high cervical cancer burden in the country, strong political commitment, a successful pilot program, and widespread community acceptance of the vaccine. Global factors (i.e., vaccine supply constraints) drove programmatic decisions regarding the implementation of HPV vaccine. Key lessons learned are shown in Fig. 1.
Fig. 1.
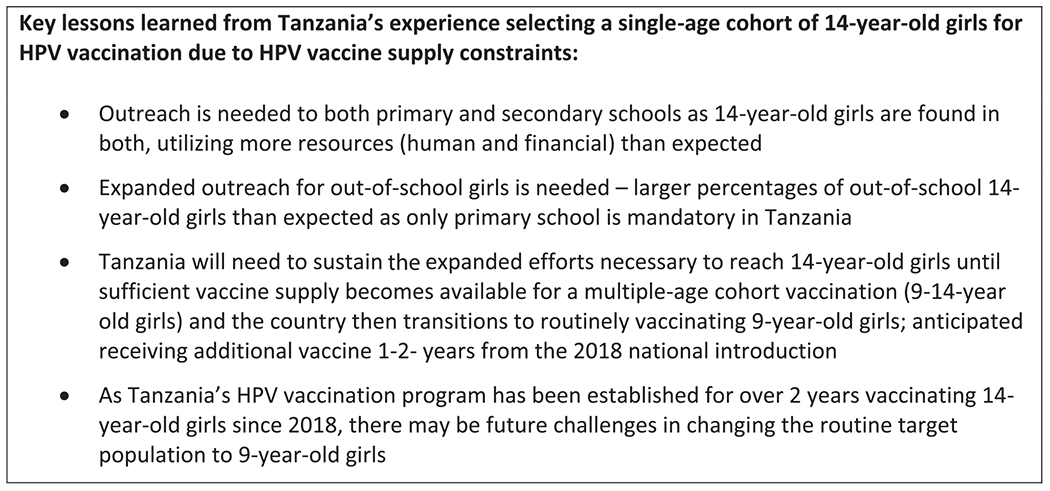
Key lessons learned from Tanzania’s experience selecting a single-age cohort of 14-year-old girls for HPV vaccination due to HPV vaccine supply constraints.
A large part of Tanzania’s routine delivery strategy for HPV vaccine includes outreach to schools. To reach 14-year-old girls, school outreach efforts needed to extend to both primary and secondary schools. While outreach to secondary schools would have been needed for a multiple-age cohort introduction (inclusive of 14-year-old girls), Tanzania had not anticipated needing to sustain this additional outreach effort beyond two years. Schools are critical to reaching girls in the target age group, and including both primary and secondary schools has almost doubled the school outreach efforts, further stretching the health system [12,15–18].
Additionally, only primary school is mandatory in Tanzania; those girls not continuing on to secondary school cannot be reached through school outreach [19–21]. Tracking out-of-school girls in this older target age group to initiate the 2-dose series or provide the second dose for those who received a first dose in school has been challenging. Many 14-year-old girls that continue secondary schooling move to a different council or region, making tracking very difficult. Supplementary out-of-school outreach efforts have been needed to reach this older target age population, as compared to 9-year-old girls who have higher school enrollment within the primary school system. Lower than expected HPV vaccination coverage, particularly for the second dose, may be due to the extensive efforts needed to reach girls in both primary and secondary schools and high percentages of 14-year-old girls being out of school. Tanzania will need to sustain expanded efforts (i.e., secondary school outreach, intensified outreach to out-of-school girls) until sufficient vaccine supply becomes available and the country transitions to routinely vaccinating 9-year-old girls.
Finally, the target age group for HPV vaccination is not uniform throughout the country with Kilimanjaro region vaccinating 9-year-old girls while the rest of the country vaccinates 14-year-old girls. As the majority of Tanzania’s regions continue vaccinating 14-year-old girls through 2020 (over two years since the national introduction), there may be future challenges in changing the routine target population including communicating the updated target age group and potential confusion among health workers, school personnel, and the community. Changes in the target age group may also lead to challenges with vaccine demand due to the sensitive nature of HPV vaccine in some settings, despite the current high acceptance. Ensuring the updated target age group of 9-year-old girls is instituted uniformly throughout the country will require added social mobilization efforts, that could be quite resource-intensive. Ongoing evaluation of Tanzania’s national introduction, coverage, and sustainability is critical to assess the impact of the HPV vaccine introduction decisions.
4. Way forward for other countries introducing HPV vaccine
Many Gavi-eligible countries have faced the dilemma of needing to choose a single-age cohort after planning for a multiple-age cohort vaccine introduction. The Strategic Advisory Group of Experts on Immunization (SAGE) has recommended to temporarily pause multiple-age cohort vaccination, given current vaccine supply limitations [22]. Therefore, currently, Gavi-eligible countries are only applying for support to vaccinate a single-age cohort. The supply constraint is projected to continue until at least 2024 with many Gavi-eligible countries planning introductions in the interim (16 additional Gavi-eligible countries are projected to introduce HPV vaccine nationally by 2022) [7,8]. As countries continue introducing HPV vaccine, ongoing vaccine supply limitations will have implications for national HPV vaccination programs.
Country-level decision-makers and global partners should think critically about the implications of their decisions on national HPV vaccination programs. Countries need to consider the impact of their target age group selection on the delivery strategy and consequences for the program. Given their country situation, decision-makers will need to balance equity concerns with the feasibility of reaching the selected target population and achieving high vaccination coverage. Global partners must support countries in this decision-making and inform countries about supply availability and timelines in advance. Countries should be well informed of the vaccine supply situation to be able to plan for the length of time they may be vaccinating the selected single-age cohort, particularly if planning for different routine target age groups in the future.
In 2018, WHO issued a call to action toward global cervical cancer elimination with a global target of 90% of girls vaccinated with HPV vaccine by 15 years of age [23]. As the global community responds to this call to action, the vaccine supply needs to be increased concurrently to reach eligible girls through planned HPV vaccine national introductions, particularly among countries with the highest burden of cervical cancer–also most impacted by vaccine supply constraints. While additional vaccine manufacturers and single-dose vaccination strategies might relieve the supply constraints in the future, country programs and the global community must work together now to align efforts and utilize the currently available resources optimally.
Acknowledgements
Ngwegwe Christopher Bulula, Julie Garon, Joseline Ishengoma, Christian Maembe, Yusuf Makame, Green Sadru.
Funding
This work was supported by the Gavi, the Vaccine Alliance [“Evaluation of Human Papillomavirus (HPV) Vaccine National Introduction in Low- and Lower-Middle Income Countries”- Contract No. ME 9422 12 20].
Footnotes
This article was published as part of a supplement supported by Centers for Disease Control and Prevention Global Immunization Division. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or World Health Organization. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors.
CRediT authorship contribution statement
Anyie J. Li: Conceptualization, Writing - original draft. Furaha Kyesi: Conceptualization, Writing - review & editing. William Mwengee: Conceptualization, Writing - review & editing. Alex Mphuru: Conceptualization, Writing - review & editing. Mary Rose Giattas: Writing - review & editing. Berrington Shayo: Writing - review & editing. Raphael Nshunju: Writing - review & editing. Dafrossa Lyimo: Supervision. Anagha Loharikar: Conceptualization, Writing - review & editing, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Disclaimer
The authors alone are responsible for the views expressed in this article, which do not necessarily represent the views, decisions, or policies of the institutions with which the authors are affiliated.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.01.036.
References
- [1].Bruni L, Albero G, Serrano B, Mena M, Gomez D, Munoz J, et al. Human Papillomavirus and Related Diseases in Tanzania. Summary Report. <http://www.hpvcentre.net/statistics/reports/TZA.pdf?t=1544735268334>; (2018) [accessed 10 Dec 2018]. [Google Scholar]
- [2].International Agency for Research on Cancer. Cervix uteri. <https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf>; (2018) [accessed 20 Nov 2019].
- [3].International Agency for Research on Cancer. Cancer Fact Sheets: Cervical Cancer. <http://gco.iarc.fr/today/data/pdf/fact-sheets/cancers/cancer-fact-sheets-16.pdf>; (2012) [accessed 20 Nov 2019].
- [4].International Agency for Research on Cancer. Cervix uteri cancer fact sheet. <https://gco.iarc.fr/today/data/factsheets/cancers/23-Cervix-uteri-fact-sheet.pdf>; (2018) [accessed 20 Sept 2018].
- [5].Human papillomavirus vaccines: WHO position paper, May 2017. Releve epidemiologique hebdomadaire. 2017;92:241–68. [PubMed] [Google Scholar]
- [6].Gavi, The Vaccine Alliance. HPV Supply and Procurement Roadmap. <https://www.gavi.org/sites/default/files/document/hpv-supply-and-procurement–roadmappdf.pdf>; (2017) [accessed 6 Apr 2020].
- [7].UNICEF. Human Papillomavirus Vaccine: Supply and Demand Update. <https://www.unicef.org/supply/files/HPV_3_Status_Update.pdf>; (2019) [accessed 6 Apr 2020].
- [8].World Health Organization. Global Market Study: HPV. <https://www.who.int/immunization/programmes_systems/procurement/mi4a/platform/module2/WHO_HPV_market_study_public_summary.pdf>; (2018) [accessed 6 Apr 2020].
- [9].International Agency for Research on Cancer. Tanzania, United Republic of Fact Sheet. <https://gco.iarc.fr/today/data/factsheets/populations/834-tanzania-united-republic-of-fact-sheets.pdf>; (2018) [accessed 1 Apr 2020].
- [10].Dartell M, Rasch V, Kahesa C, Mwaiselage J, Ngoma T, Junge J, et al. Human papillomavirus prevalence and type distribution in 3603 HIV-positive and HIV-negative women in the general population of Tanzania: the PROTECT study. Sex Transm Dis 2012;39:201–8. [DOI] [PubMed] [Google Scholar]
- [11].World Health Organization. Stakeholders’ Meeting on the introduction of Human Papilloma Virus (HPV) Vaccine kicks off in the United Republic of Tanzania. <https://www.afro.who.int/news/stakeholders-meeting-introduction-human-papiilloma-virus-hpv-vaccine-kicks-united-republic>; [accessed 13 Apr 2020].
- [12].Gallagher KE, Erio T, Baisley K, Lees S, Watson-Jones D. The impact of a human papillomavirus (HPV) vaccination campaign on routine primary health service provision and health workers in Tanzania: a controlled before and after study. BMC Health Serv Res 2018;18:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Human Papillomavirus vaccination demonstration programme. Post-introduction evaluation report. Kilimanjaro region, Tanzania: Tanzania Ministry of Health and Social Welfare; 2014. [Google Scholar]
- [14].United Republic of Tanzania. Application for Gavi new vaccine support. <https://www.gavi.org/sites/default/files/document/proposal-for-hpv-support-2017-tanzaniapdf.pdf>; (2017) [accessed 13 Dec 2018].
- [15].Watson-Jones D, Baisley K, Ponsiano R, Lemme F, Remes P, Ross D, et al. Human papillomavirus vaccination in Tanzanian schoolgirls: cluster-randomized trial comparing 2 vaccine-delivery strategies. J Infect Dis 2012;206:678–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Gallagher KE, Howard N, Kabakama S, Mounier-Jack S, Griffiths UK, Feletto M, et al. Lessons learnt from human papillomavirus (HPV) vaccination in 45 low- and middle-income countries. PLoS ONE 2017;12:e0177773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hanson CM, Eckert L, Bloem P, Cernuschi T. Gavi HPV Programs: Application to Implementation. Vaccines (Basel) 2015;3:408–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ladner J, Besson MH, Hampshire R, Tapert L, Chirenje M, Saba J. Assessment of eight HPV vaccination programs implemented in lowest income countries. BMC Public Health 2012;12:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].UNICEF. Tanzania Education Factsheet. <https://www.unicef.org/tanzania/media/681/file/UNICEF-Tanzania-2017-Education-fact-sheet.pdf>; (2017) [accessed 13 Apr 2020].
- [20].FHI360. Tanzania National Education Profile. <https://www.epdc.org/sites/default/files/documents/EPDC_NEP_2018_Tanzania.pdf>; (2018) [accessed 13 Apr 2020].
- [21].Human Rights Watch. I had a dream to finish school: Barriers to secondary education in Tanzania <https://www.hrw.org/report/2017/02/14/i-had-dream-finish-school/barriers-secondary-education-tanzania>; (2017) [accessed 13 Apr 2020].
- [22].Meeting of the Strategic Advisory Group of Experts on Immunization, October 2019: conclusions and recommendations. Releve epidemiologique hebdomadaire. 2019;94:541–60. [PubMed] [Google Scholar]
- [23].World Health Organization. A Global Strategy for elimination of cervical cancer. <https://www.who.int/activities/a-global-strategy-for-elimination-of-cervical-cancer>; (2019) [accessed 6 Apr 2020].


