Abstract
Context
Patients and community members are engaged in nearly every aspect of health systems. However, the engagement literature remains siloed and fragmented, which makes it difficult to connect engagement efforts with broader goals of health, equity and sustainability. Integrated and inclusive models of engagement are needed to support further transformative efforts.
Methods
This article describes the Ecology of Engagement, an integrated model of engagement. The model posits that: (1) Health ecosystems include all members of society engaged in health; (2) Engagement is the ‘together’ piece of health and healthcare (e.g., caring for each other, preventing, researching, teaching and building policies together); (3) Health ecosystems and engagement are interdependent from each other, both influencing health, equity, resilience and sustainability.
Conclusion
The Ecology of Engagement offers a common sketch to foster dialogue on engagement across health ecosystems. The model can drive cooperative efforts with patients and communities on health, equity, resilience and sustainability.
Patients and Public Contribution
Three of the authors have lived experiences as patients. One has a socially disclosed identity as a patient partner leader with extensive experience in engagement (individual care, education, research, management and policy). Two authors have significant experience as patients and informal caregivers, which were mobilized in descriptive illustrations. A fourth author has experience as an engaged citizen in health policy debates. All authors have professional lived experience in health (manager, researcher, health professional, consultant and educator). Six patient and caregiver partners with lived experience of engagement (other than the authors) contributed important revisions and intellectual content.
Keywords: community engagement, ecological models, health coproduction, patient and public involve, patient engagement, theory
1. THE NEED FOR AN ECOLOGICAL PERSPECTIVE ON HEALTH COPRODUCTION
Patients and community members are engaged in nearly every aspect of health ecosystems (e.g., self‐care, clinical care, research, education, public health and policy). Dozens of models and conceptual frameworks have been published to support engagement with patients and community members. 1 , 2 , 3 , 4
Patient and community engagement tend to assume an intrinsic distinction between care providers (e.g., health professionals) and care receivers (e.g., patients), with patients and citizens being framed as ‘end‐users’, ‘beneficiaries’ and ‘consumers’. 5 Accordingly, engagement is viewed as ‘inviting people from outside’ into professional health systems. 6 This assumes that professionals are leading the engagement ‘intervention’ (whom to engage and how) to achieve health systems' goals (e.g., vaccination rates, medication adherence, research uptake and social acceptability of policies). 7
Increased recognition that health is coproduced with patients and communities calls for more reciprocal and integrated models of engagement, acknowledging that leadership and roles can evolve over time. Coproduction refers to the idea that care is produced jointly by ‘providers’ and ‘users’, thus blurring the distinction between who gives and receives care. 8 Coproduction of individual care recognizes the role of informal care provided by patients, family members and citizens, emphasizing the fact that professional delivery of healthcare services only represents a fraction of the total care received. 9 From a public health perspective, collective coproduction of health recognizes the influence that communities and civic institutions have on environmental and social determinants of health (e.g., mutual support, education, income distribution, employment, climate change). 10
While the idea of health coproduction has been around for years, 8 its application in practice remains problematic and inequitable. Engagement practices are still largely characterized by fragmented, short‐term initiatives, leaving important segments of health systems uninviting and not interacting with community members. Also, many communities remain excluded from influential decision‐making roles, thus perpetuating knowledge and power imbalance that impedes global capacities for system transformation and health coproduction. 11
The International Summit on Patient and Public Partnership—which convened over 100 patient, community and health system leaders—highlighted the need to ‘assemble the puzzle’ and develop a common vision for systemic transformation anchored in a partnership model of health. Participants stressed the need to ‘look at the whole elephant, in interaction with its environment’. International leaders recognized the challenge of building an integrated vision of engagement in health coproduction, emphasizing the need to ‘broaden the tent’ to new ideas and perspectives. 12 , 13 Inclusive engagement models are therefore needed to push towards health coproduction for all. 14
Other disciplines have faced similar challenges in building integrated views of complex systems. In response, ecological models have been fruitfully developed and used in biology, public health, psychology and sociology to understand dynamic and interdependent relationships across systems' levels. 15 This paper capitalizes on the strengths of ecological models to propose an integrated perspective on engagement in health coproduction.
1.1. Objective
The Ecology of Engagement is a conceptual model focused on understanding, supporting and evaluating engagement relationships across health ecosystems. The goal of this article is to describe the Ecology of Engagement and illustrate its potential implications for practice and research. The article is divided into four sections:
-
1.
After a brief description of our theory‐building approach, we sketch an overview of the Ecology of Engagement and offer definitions of key concepts;
-
2.
We then describe the core components of the model: health ecosystems, engagement and the interactions between both;
-
3.
Following the idea that ‘there is nothing more practical than a good theory’, 16 we illustrate the pragmatic application of the model using international empirical examples;
-
4.
We finally reflect on the strengths and limitations of the model, while outlining a research agenda for the future.
1.2. Theory‐building approach
To build the Ecology of Engagement Model, we followed Lynham's interpretive approach to theory‐building in applied research. Theory‐building is understood as ‘the purposeful process or recurring cycle by which coherent descriptions, explanations and representations of observed or experienced phenomena are generated, verified and refined’. 17 Interpretive theory‐building inquiry focuses on the practical construction of meanings to understand and interpret complex phenomena. Our theory‐building goal was to provide engagement practitioners and scientists with a common language to conceptualize engagement across health systems. As such, we did not seek to inductively build new theories (as in grounded theory approaches) nor did we try to build predictive models based on analytical approaches (as in meta‐analysis). Instead, we examined the fit between existing theories and actual engagement experiences through practice‐to‐theory dialogue based on two sources of expertize: the practical knowledge of patients, professionals and citizens who experienced engagement, and the theoretical expertize of engagement scientists. Our writing team met over a 2‐year period to conceptualize and refine the model and was composed of patients, informal caregivers, citizens, health professionals and researchers with decades of collective engagement experience in different health domains (individual care, education, research, management and policy), disciplines (health services research, medicine, community psychology, management, sociology, anthropology, public health and philosophy) and from different countries (Canada, France, the United Kingdom and the United States). The practical applicability and theoretical coherence of the model were discussed with international experts in engagement science, as well as six patients and caregivers with several years of engagement experience. Our collective approach as a diverse writing team was anchored in dialogical traditions of science highlighting the importance of carefully listening, understanding and learning from multiple paradigms and perspectives while thriving on differences and intellectual tensions. 18 , 19 The resulting model should be considered exploratory and descriptive, seeking to pragmatically support further collaboration among practitioners and scientists. 20
1.3. The Ecology of Engagement model overview
The Ecology of Engagement focuses on understanding, supporting and evaluating engagement relationships in health ecosystems. Table 1 offers definitions of key concepts. The core assumptions underpinning the model are:
-
1.
Health ecosystems include all members of society engaged in health. Health ecosystems are broader than professional health systems and incorporate patients, informal caregivers communities and their environment as integral contributors to individual and population health.
-
2.
Engagement is the ‘together’ piece of health and healthcare. Engagement is dynamic relationships oriented towards joint health‐related activities being carried out together (e.g., caring for each other, doing research together, teaching together, promoting health together and building policies together). Engagement relationships can be categorized according to power and knowledge (activism, information, consultation, participation and partnership), at what levels of health ecosystems they operate (micro‐, meso‐ and macrolevels), among whom (bonding, bridging and linking) and based on its ecosystemic distribution (density, intensity and diversity).
-
3.
Health ecosystems and engagement are interdependent. Engagement transforms health ecosystems and is influenced by its ecological context (e.g., social structures, culture, institutions and individuals). Engagement relationships have systemic influences on the equilibrium between health, equity, resilience and sustainability.
Table 1.
Definitions
| Concept | Definition |
|---|---|
| Health Ecosystems (‘outer core’ of the model) | |
| Ecology of Engagement | An ecological model focused on understanding, supporting and evaluating engagement relationships at different levels of health ecosystems. |
| Ecological model | A conceptual framework designed to draw attention to the interdependence between individual and collective determinants of knowledge, attitudes and behaviours. Ecological models assume interaction and multidirectional influence between individuals, collective and environmental factors. Ecosystems are living, open and evolutive systems. |
| Health Ecosystem | Include all members of society engaged in health‐related activities. Health‐related activities include caring for self or others, health promotion, research, education, governance and policy. Health ecosystems are broader than professional health systems and incorporate patients, informal caregivers, communities and their environment as integral contributors to individual and population health. |
| Community system | Community members (patients, family members, informal caregivers and citizens) and community groups (patient associations, networks, civic institutions and social movements) who engage in health‐related activities. |
| Professional system | Professional members (e.g., clinicians, managers, researchers, policymakers) and institutions (healthcare institutions, public health agencies, government) who engage in health‐related activities. |
| Microlevel | Individual‐level relationships (e.g., individual patient and professionals' decision‐making). |
| Mesolevel | Groups and institutions in which individuals interact together (e.g., patient association, clinic, research team, training institutions). |
| Macrolevel | Forces within the larger social system in which groups and institutions are embedded (e.g., culture, policies, values, legislation, environment). |
| Engagement relationships (‘inner dynamic’ of the model) | |
| Engagement | Dynamic relationships among individuals or groups oriented toward joint health‐related activities. Engagement is the ‘together’ piece of health and healthcare (e.g., caring together, doing research together, teaching together, promoting health together and developing policies together). |
| Typology of engagement | Characterization of engagement relationships according to power and knowledge flow (activism, information, consultation, participation and partnership), at what levels of health ecosystems they operate (micro‐, meso‐ and macrolevels), and among which individuals and groups (e.g., bonding, bridging and linking). |
| Information | Engagement relationship where knowledge is communicated from engagement leaders to engaged individuals or groups. |
| Consultation | Engagement relationship where knowledge is collected from engaged individuals/groups toward engagement leaders. |
| Participation | Engagement relationship where knowledge is exchanged between engagement leaders and engaged people. |
| Partnership | Engagement relationship where engaged parties colead (governance), cobuild (process) and are coaccountable (results) for a common initiative being carried together. |
| Activism | Engagement relationship where engagement leaders challenge existing power relationships and social structures to change the status quo (including social norms, embedded practices, policies or the dominance of certain social groups). |
| Bonding | Engagement relationships within community or professional systems. Bonding relationships are ‘inward looking’, reinforcing connections among homogenous groups of people with a shared identity (e.g., self‐support group, professional team) |
| Bridging | Engagement relationships across community or professional systems. Bridging relationships are ‘outward looking’, reinforcing connections across a heterogeneous group of people with different identities (e.g., quality improvement committees with patients and health professional members). |
| Linking | Engagement relationships across ecosystem levels. Linking relationships are ‘upward looking’, reinforcing connections with people across power and authority gradients (e.g., tenants' participation in a social housing management committee, project coleadership between a patient and health authority manager, community development project with citizens and municipal government leaders). |
| Density | Total number of engagement relationships among individuals and groups. Density quantifies how many engagement relationships are developed and maintained among community members and professionals, each offering opportunities for mutual influence across the whole ecosystem. |
| Intensity | Strength of bonding, bridging and linking engagement relationships within the health ecosystem as a whole, allowing sustained connections within and across community and professional systems. |
| Diversity | Variety of individuals and groups forging engagement relationships within the health ecosystem as a whole. Diversity points to the inclusiveness of engagement relationships, and the potential exclusion of certain individuals and groups with whom knowledge, power and health production capacity may be unequally distributed. |
| Ecological effects of engagement (‘inputs and outputs’ of the model) | |
| Health coproduction | Change in the health of individuals and groups resulting from the joint actions of community members and professionals. |
| Resilience | Ability of health ecosystems to adapt, evolve and survive as a result of changes and crises. |
| Resource use | Use of human, financial or environmental resources by the health ecosystem. |
| Equity | Inclusive distribution of knowledge, power and health production capacity among individuals and groups within health ecosystems. |
2. HEALTH ECOSYSTEMS INCLUDE ALL MEMBERS OF SOCIETY ENGAGED IN HEALTH
Ecological perspectives bring to the foreground a number of key assumptions in the understanding of health systems and their relationships to engagement.
First, ‘health systems’ are viewed as ‘ecosystems’ that are not restricted to professional services and institutions (e.g., health professionals, hospitals and clinics, research institutions and health ministries). Health ecosystems incorporate patients, informal caregivers, citizens, communities and their environment as integral components of health production. 8
Ecological systems are ‘living systems’. Mechanical systems (e.g., cars, the solar system) operate under constant, predictable rules. Conversely, living systems (e.g., the human body, a forest) are characterized by complexity and emergent properties arising across levels. 21 Individuals are embedded within communities, institutions and societies with emergent properties across levels 22 (e.g., collective ability to shape policy decisions). Engagement among individuals is qualitatively different from collective engagement across communities, institutions and groups, which have emergent properties beyond those of its participating members.
Ecological perspectives emphasize the interdependence and multidirectional influence between individual and collective factors. 15 Central to ecological perspectives are the assumption of mutual interaction and reciprocal causation among levels. The microlevel refers to individuals (e.g., individual patient and professional decision‐making). The mesolevel refers to groups and institutions (e.g., patient association, clinical team, community support group and research institution). The macrolevel refers to larger forces within the social systems in which groups and institutions are embedded (e.g., environment, culture, policies and legislation). From an engagement perspective, engagement at the microlevel (e.g., care) can generate knowledge and opportunities for engagement at the meso‐ (e.g., institution) and macrolevels (e.g., policy). Conversely, engaging patients and professionals at the meso‐and macrolevel (e.g., change in legislation) can transform the opportunities for engagement at the individual level.
Ecological systems are ‘open systems’, drawing energy from the outside environment. Health systems cannot be isolated from broader economic, societal and environmental systems. Living systems like the human body or the health system need to constantly extract energy from their environment to survive. 23
Ecological systems are evolutive: individual trees are born, grow and die, just like individuals evolve in their health status, knowledge, care capacity and relationships. Instability is an intrinsic feature of ecological models, which can be influenced by internal changes (e.g., pandemics) or external changes (e.g., climate change). 24 Health ecosystems are transformed by historical changes in culture, technologies, economic growth, social inequalities, population change and crisis. Resilience refers to the ability of individuals and systems to adapt, evolve and survive as a result of change and crisis.
In sum, the Ecology of Engagement proposes an ecological perspective on health systems, which are reconceptualized as ‘health ecosystems’ that include all members of society potentially engaged in health coproduction. Health ecosystems are open, living and evolutive systems characterized by interdependent relationships across individuals and groups.
3. ENGAGEMENT IS THE ‘TOGETHER’ PIECE OF HEALTH AND HEALTHCARE
3.1. Defining engagement
Dozens of definitions of engagement have been proposed in the literature. 25 Grounded in an ecological perspective, our definition of engagement is relationship‐focused and systemic. We define engagement as dynamic relationships oriented towards joint health‐related actions. We assume that engagement represents a specific type of relationship between individuals and groups, focused on actions being carried together. This broad definition of engagement does not mean that ‘everything in health is engagement’ but that ‘engagement can be related to any component of health ecosystems’. Engagement is the ‘together’ piece of health and healthcare: caring together, doing research together, teaching together, designing innovations together, promoting health together, defining community priorities together, educating children together and building policies together.
To unpack this umbrella definition, we propose a typology of engagement relationships according to power and knowledge flow (activism, information, consultation, participation, partnership), at what levels of health ecosystems they operate (micro‐, meso‐ and macrolevels), among which individuals and groups (e.g., bonding, bridging, linking), and their ecological distribution (density, intensity and diversity).
3.2. ‘The Loop’: Distinguishing engagement based on knowledge and power
Following other authors, 2 we assume that theoretically relevant differences exist between engagement relationship categories. 1 , 2 , 3 A common assumption of existing typologies is that engagement is either led by professionals (e.g., Rowe and Frewer ‘typology of public engagement mechanisms’ ranging from ‘information’ to ‘participation’ 2 ) or led by citizens themselves (e.g., Sherry Arstein's ‘ladder of citizen participation’ ranging from ‘manipulation’ to ‘citizen control’ 1 ).
The Ecology of Engagement adopts a reciprocal perspective on engagement: the ‘Engagement Loop’ (Figure 1). A loop is a symmetrical figure representing a process the end of which is connected to the beginning. The Engagement Loop is:
-
1.
Reciprocal, recognizing that engagement relationships can be led by professionals, community members or both. Unlike a scale or ladder, the loop does not have a top or a bottom (specifying ‘higher’ or ‘lower’ levels of engagement), but two poles of attraction at each end (community vs. professionally‐led engagement) that can be more or less powerful or balanced at different points in time;
-
2.
Dynamic, highlighting the shifting nature of engagement relationships over time. For example, a patient can take leadership of self‐care activities at home, be led by professionals during hospitalizations and engage in partnership decision‐making during outpatient follow‐up appointments. This shift in engagement leadership can also be observed at the collective level, where professionally led initiatives can transition to community‐led programmes over time, and vice‐versa. 26
Figure 1.
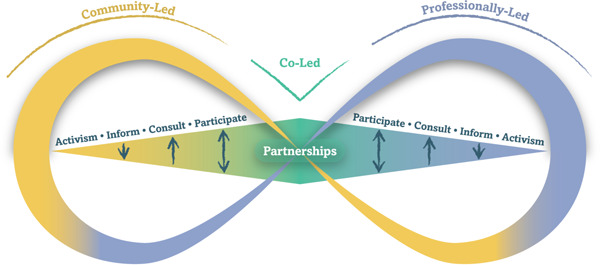
The loop (engaging how and under whose leadership). Engagement are dynamic relationships oriented toward joint health‐related actions. Engagement can be led by the community (yellow), by professionals (blue), or co‐led (green). Engagement is distinguished by knowledge flow (information to, consultation from, participation between) and power (activism to transform power dynamics from the outside, partnering by sharing power from the inside). Engagement relationships evolve over time (‘bouncing along the loop’).
The Engagement Loop distinguishes between five types of engagement relationships according to power (who frames engagement goals and approach) and knowledge (in which direction knowledge is produced and exchanged between individuals and groups). 1 , 2 , 3
Information, consultation and participation approaches are distinguished by the direction of knowledge flow. Knowledge is either communicated to (information), collected from (consultation) or exchanged between individuals and groups (participation). 2 Information, consultation and participation assume unilateral leadership of the engagement process by professionals or community members. Reciprocity of the typology allows consideration of situations where community members are acting as engagement leaders (e.g., community‐led information campaign targeting professionals) or the other way around (e.g., professionally‐led education programme).
Partnership and activism approaches are distinguished by power relationships. Partnership is characterized by power sharing and coleadership. Relationship‐building and power‐sharing are assumed as preconditions of engagement. 27 Conversely, activism targets the transformation of power relationships and social structures as a potential result of engagement. 28 , 29 Partnership approaches seek to achieve ‘transformation from the inside’ (through collaborative leadership, sharing of expertize and resources and partnership synergy), 27 while activism focuses on changing power relationships and institutional structures ‘from the outside’ (through critical questioning of discourses and redistribution of resources and power). 30 , 31
Differences in engagement approaches are reflected in the choice of appropriate evaluation criteria to assess the process and outcomes of engagement. Table 2 illustrates examples of engagement at different health ecosystem levels, along with their potential evaluation criteria.
Table 2.
Examples of engagement relationships and evaluation criteria
| Engagement category | Definition | Engagement methods | Microlevel engagement examples | Meso/macrolevel engagement examples | Evaluation criteria |
|---|---|---|---|---|---|
| Information | Knowledge is communicated from engagement leaders to engaged individuals/groups |
|
Professional‐led: Professional informs the patient on individual long‐term risks of cardiovascular disease. | Professional‐led: Professional education programme to raise public awareness of mental health issues. |
Process: Information content, quality, understanding and reach. Outcomes: Change in awareness, knowledge, attitude and behaviours of people engaged. |
| Community‐led: Patient takes the initiative of informing professional on side effects of medication. | Community‐led: Patient‐led education programme where patients train health professionals on relationship skills. | ||||
| Consultation | Knowledge is collected from engaged individuals/groups towards engagement leaders |
|
Professional‐led: Professional consults patient on his preferences for home or institution‐based palliative care, but the orientation of care is ultimately based on a clinical algorithm. | Professional‐led: Research team set up a patient‐advisory committee for input into research questions or guideline recommendation. |
Process: Representativeness, reliability, generalizability. Outcomes: Change in knowledge, attitudes and behaviours of engagement leaders, influence on policies. |
| Community‐led: Patient consults professional for advice on the use of over‐the‐counter vitamin supplements and makes the final decision by him/herself. | Community‐led: Community group consults scientific advisors to validate the content of public campaign documents | ||||
| Participation | Knowledge is exchanged between engagement leaders and engaged people. |
|
Professional‐led: Parents contribute to implementing a professionally led home‐care plan for a sick child by exchanging information with the clinic. | Professional‐led: Professionally led practice guideline group invite patients to the guideline development panel. |
Process: Information exchange, inclusivity, independence, fairness. Outcome: Mutual learning and influence between engaged parties, informed collective proposal, influence on policies. |
| Community‐led: Parents initiate deliberation with clinical ethicists on care options for their child while keeping leadership on the decision. | Community‐led: Parent association host deliberative panel between clinicians, researchers, youths and parents to improve mental health services. | ||||
| Partnership | Engaged parties colead (governance), cobuild (process) and are coaccountable (results) for a common initiative being carried together. | Co‐led: Shared decision‐making between patient and professional in establishing clinical agenda, generating and implementing care options, coassessing progress and being coresponsible for health results. | Co‐led: Community members and professionals colead a project where patients, clinicians and citizens care together for people with social and medical issues. |
Process: Partners' relationships; sharing of power, resources and information; trust. Outcome: Partnership synergy, sustained collaborative efforts, collective production of care, knowledge, services and policies. |
|
| Activism | Engagement leaders challenge existing power relationships and social structures to change the status quo (including social norms, embedded practices, policies or the dominance of certain social groups). |
|
Professional‐led: Medical activism to challenge health insurer coverage restriction for a single patient. | Professional‐led: Health professionals initiate media campaigns to change tobacco policies. |
Process: Coalition‐building, prepare/communicate convincing data and rationales, lobby policymakers. Outcome: Change in power distribution, group dominance, institutional structure, social norms, practices and policies. |
| Community‐led: Patient advocates for his/her right to access a specific treatment from his/her insurer. | Community‐led: Women groups challenge medical dominance over childbirth and advocate for legal recognition of midwives. |
Engagement approaches labelled as ‘codesign’, ‘shared decision‐making’, ‘coconstruction’ or ‘coproduction’ are best classified in the partnership category when leadership is shared between parties. However, they are best classified in the information, consultation or participation category when leadership is held by a single party (e.g., ‘codesign’ of health technology led by engineers where patients are consulted at the initial or pilot testing stage, ‘coproduction’ of research led by scientists where citizens are engaged in crowdsourcing of data collection, ‘shared decision‐making’ on antidepressant medication choice where agenda‐setting is led by clinicians only and patient is consulted on the choice of drug).
bEngagement approaches labelled as ‘committee participation’ are best classified in the consultation category when the committee is structured around a collection of opinions, feedback, advice and recommendations with little or no information exchange (membership in a citizen advisory council). The defining characteristic of participation methods is two‐way interaction and influence between engagement leaders and participants.
3.3. Engagement with whom: Bonding, bridging and linking
Drawing from social capital theory, we further distinguish engagement relationships according to who is engaged with whom (Figure 2) 32 , 33 :
-
1.
Bonding refers to engagement relationships within community or professional systems. Bonding relationships are ‘inward looking’, reinforcing connections among homogenous groups of people with a shared identity (e.g., a patient association, peer support group, research network or professional team).
-
2.
Bridging refers to engagement relationships across community or professional systems. Bridging relationships are ‘outward looking’, reinforcing connections across a heterogeneous group of people with different identities (e.g., care team with peer‐support workers and health professionals working together; governance committees with patients and managers; research teams with academic researchers and citizens).
-
3.
Linking is ‘upward looking’, reinforcing connections with people across power, authority gradients and levels (e.g., tenants' participation in a social housing management committee, project coleadership between a patient and health authority manager, community development project with citizens and municipal government leaders).
Figure 2.
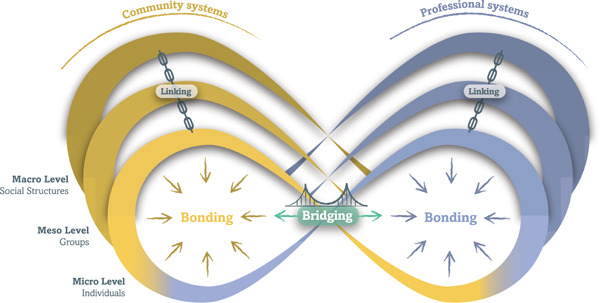
Engagement relationships can be distinguished according to who is engaged and at what level. Bonding are ‘inward looking’ engagement relationships among community members (yellow) or professionals (blue). Bridging are ‘looking across’ engagement relationships between community and professional groups (green). Linking are ‘upward looking’ engagement relationships across power authority and levels (black).
Bonding and bridging relationships are distinguished by an open and fluid distinction between community and professional identities based on socially constructed identities, rather than static and predetermined characteristics. 34 , 35 For example, the same individual may identify and be socially labelled as ‘patient’, ‘physician’, ‘researcher’ or ‘citizen’ depending on their own self‐identification and roles. Distinguishing between community and professional identities remains conceptually and pragmatically useful to understand engagement relationships within health ecosystems. Holding a socially recognized identity of ‘physician’ opens certain bonding and linking relationship opportunities (e.g., professional colleague or manager) that are different if the same individual self identifies as a ‘patient partner’.
3.4. Ecosystemic distribution of engagement relationships
Engagement relationships can be studied ‘from the inside out’, by characterizing the relationships of a focal individual or collective (e.g., bonding and bridging relationships established by a single patient partner) or studied from the ‘outside‐in’, by characterizing the distribution of engagement relationships within a health ecosystem. 36 The ecosystemic distribution of engagement relationships can be characterized based on its density, intensity and diversity:
-
1.
Density refers to the total number of engagement relationships among individuals and groups within an ecosystem. It quantifies how many engagement relationships are developed and maintained, thus offering opportunities for influence across the whole ecosystem.
-
2.
Intensity refers to the strength of engagement relationships within the health ecosystem. Stronger engagement relationships (e.g., team membership) tend to allow for more constant and sustained connections within and across community and professional systems, while weaker ties (e.g., informal contacts among individuals) can play a role in bridging more isolated community and professional groups. 37
-
3.
Diversity refers to the variety of individuals and groups forging engagement relationships within the health ecosystem as a whole. Diversity points to the inclusiveness of engagement relationships and the potential exclusion of certain individuals and groups with whom knowledge, power and health production capacity may be unequally distributed.
4. HEALTH ECOSYSTEMS AND ENGAGEMENT ARE INTERDEPENDENT
The Ecology of Engagement assumes a bidirectional influence between engagement and health ecosystems: engagement transforms ecosystems and is shaped by its ecological context. Engagement relationships have systemic effects on the equilibrium between health, resilience, equity and sustainability (Figure 3). This section illustrates the interdependence between engagement and health ecosystems.
Figure 3.
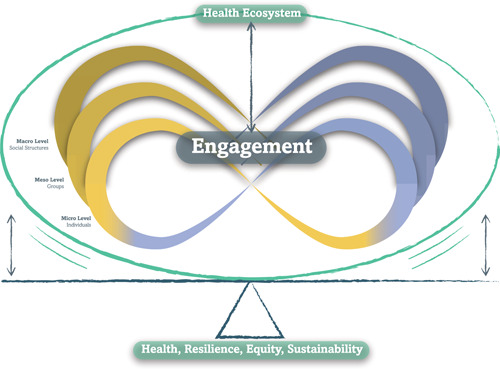
Health Ecosystems and Engagement are interdependent. Engagement transforms Health Ecosystems and is influenced by it. Engagement relationships have systemic effects on the equilibrium between health, resilience, equity and sustainability.
4.1. Engagement transforms health ecosystems
A growing empirical literature has documented how the engagement of patients, professionals and communities can transform its ecological context by shaping policies, social determinants of health, research, health institutions, education programmes and direct care. 38 , 39 , 40 , 41 , 42 , 43 , 44 Similarly, several ecological factors (e.g., culture, institutions, policies) influence the process and outcomes of engagement. 45 , 46 , 47 , 48 These influences can operate ‘upstream’ (micro‐ to macrolevels), ‘downstream’ (macro‐ to microlevels) or ‘laterally’ (across a single level).
The example of patient engagement in medical education helps illustrate this transformative impact of engagement on health ecosystems. A number of medical schools are engaging with patients as teachers. 49 , 50 The decade‐long experience of patient engagement in medical education at Université de Montreal (Canada) illustrates how long‐term engagement in education can have ecological effects on research, policy and individual care. Initiated in 2010 under the coleadership of the faculty of medicine dean and a patient leader, the ‘Montreal Model’ has grown into one of the largest patient partnership training programmes internationally (over 250 paid patient educators training 1500 health professionals from 14 health disciplines every year). 50 Over time, patient engagement in professional education influenced the (lateral) engagement of patients in health governance institutions, which created momentum for (upstream) policy reforms on engagement in quality improvement, research and accreditation. 51 Patient engagement in education also had (downstream) influence on individual care through its kindling effects on peer support in clinical care and national training programmes for informal caregivers. 52 Overall, this experience illustrates the potential long‐term relationships between engagement in education, policy, research, care and health and its ecological impacts across health ecosystems.
4.2. Engaging communities and professionals in health coproduction
Health ecosystems can move back and forth between community‐led, professionally led or co‐led health production systems as a result of historical, technological, political and cultural forces. For example, low‐income countries tend to rely heavily on community health production systems (e.g., informal care by family and community members). Community structures tend to be marginalized with technological progress and the professionalization of care. 48 , 52 Conversely, extreme professionalization of care tends to be limited by its high resource use and inability to reach certain underserved communities, which creates counter‐balancing forces towards coproduction models built on the synergy between community and professional resources.
Bridging engagement relationships between professionals and community members can also support health coproduction dynamics. 26 For example, peer‐support workers foster health coproduction through their ability to build trustful relationships across professionals and community systems. This bridge can operate from the clinic to the community (e.g., peer‐mentors connecting chronic disease patients living in poverty with community organizations offering housing and food support), 52 or from the community to the clinic (e.g., peer‐support workers helping to reconnect people experiencing homelessness with professional healthcare services or harm‐reduction strategies aligned with people's own goal and values). 49 Community members can also foster bonding (e.g., introduction to mutual support group) and linking relationships (e.g., advocating for service delivery adaptation).
4.3. Engagement influences resilience, equity and sustainability
Engagement relationships have potential effects on health ecosystems' resource use (entropy), adaptation to change and crisis (resilience) and disparities (equity).
An ecological perspective suggests that the diversity and intensity of engagement relationships influence health ecosystems' sustainability (use of human, financial and environmental resources). 50 Several initiatives mobilizing patients, citizens and communities as care partners have shown comparable or improved outcomes compared to professionally led models of care, 51 , 53 with lower use of resource‐intensive services (e.g., emergency room visits and hospitalizations) and overall costs of care. 54 , 55 , 56
The environmental impacts of different health production systems further illustrate the relationships between engagement and sustainability. Climate change has significant impacts on global health and the healthcare sector is a direct contributor to climate change. 57 , 58 Professional health production systems tend to produce higher (environmental) effects than community‐based or health coproduction systems. Large urban hospitals tend to have a high carbon footprint because of direct energy use, disposable technologies and transportation. 58 Conversely, community‐based care focused on people empowerment and self‐management has greater potential for low carbon footprint healthcare. 57 Engagement relationships can also influence the entropic effects of health on the environment, through professional and citizen mobilization efforts. 59 , 60
Equity is also influenced by engagement. Despite its massive investment in healthcare (17.9% of gross domestic product), the United States ranks last among developed countries for many health indicators notably because of persistent inequalities according to socioeconomic status, race and gender 14 , 61 Although the density and intensity of patient and family engagement programmes is relatively well developed in the United States (e.g., shared decision‐making, public performance reports of health coverage plans, self‐management programmes), the engagement of a diversity of groups remains problematic, particularly with disadvantaged and marginalized communities. 14 Local engagement strategies initiated by or developed with marginalized groups have shown promising results in reducing health inequities, especially when they can address structural and power issues. 53 , 62 The effects of engagement on equity can either increase or decrease health inequalities, depending on the diversity (and power) of engagement relationships.
Finally, engagement relationships can affect resilience, defined as the ability to adapt, evolve and survive as a result of changes and crises. 32 High degrees of interactions among individuals and groups act as stabilizing forces to counter the effects of ecological instabilities. 24 Ecological systems with more dense, diverse and intense relationships (e.g., forests) are more likely to adapt to environmental changes than homogenous ecosystems characterized by low diversity and interactions (e.g., agricultural monoculture). Within the health context, empirical studies have highlighted the contribution of engagement relationships to resilience, as exemplified by the Ebola and COVID‐19 pandemics. 32
The 2014–2015 Ebola outbreak in West Africa had mortality rates of approximately 70% and occurred in the context of fragile and under‐resourced professional healthcare systems. Community engagement thus became a pillar of intervention to reduce the progression of the disease, including the design and planning of public health response with communities; building public trust, communication strategies; and community engagement in case detection, follow‐up and quarantine. These measures directly contributed to controlling the outbreak and supporting the resilience of the health ecosystem in a concerted effort with its limited professional structure. 63 , 64 , 65 The response to COVID‐19 offers a contrasting perspective on resilience in professionally led health ecosystems. Equipped with well‐resourced healthcare systems, countries in North America and Europe have heavily relied on professional strategies and centralized decision‐making. Governance of national COVID‐19 strategies has been dominated by professional experts, with little direct input from patients and civil society. 66 , 67 Community groups have most often been mobilized as delivery mechanisms, with little decision‐making power over the design and planning of local pandemic response. 68 While the importance of community engagement has been recognized in later phases of the pandemic, 68 , 69 , 70 over‐reliance on professional care during the first wave of COVID resulted in rapid overloads of professional health systems. 71 , 72 , 73
In summary, the Ecology of Engagement points towards systemic impacts of engagement, through its transforming influence on individuals, institutions and policies, as well as its ecological effects on health, resilience, equity and sustainability.
5. STRENGTHS, LIMITATIONS AND AREAS FOR FUTURE DEVELOPMENT
The main contribution of the Ecology of Engagement is to offer an integrated perspective on engagement and health. It proposes a conceptually coherent model helping to bridge engagement practice and science. Because social interactions are embedded in nearly all health activities, the Ecology of Engagement offers a useful theoretical architecture to connect engagement relationships across domains (e.g., care, research, education, health promotion and policymaking) and levels (micro‐, meso‐ and macrolevels). 32 , 36 , 74 The proposed typology of engagement offers a reciprocal perspective on engagement leadership by community members and professionals. The use of a descriptive typology also helps disentangle engagement approaches labelled with generic terms hiding important differences in theory and practice. 75 Finally, the model proposes core assumptions about the potential systemic effects of engagement on health coproduction, resilience, equity and entropy. The model is applicable to concrete examples and can drive further action and research.
We present the Ecology of Engagement model with humility, acknowledging that the model is building on the work of many others. The integrative nature of the Ecology of Engagement seeks to connect engagement theories that are often disconnected from each other while offering a common language to support further dialogue. This does not imply that the model offers a comprehensive theory of engagement in health. It is merely offered as a pragmatic sketch to build upon.
Drawing from multiple scientific and epistemic traditions can create paradoxes that are difficult to reconcile (e.g., postpositivist views of entropy coexisting alongside constructivist views of social identities), and is influenced by the perspectives of experts involved in theory‐building. 76 Such internal tensions are intrinsic to transdisciplinary undertaking and should inform further research and practice dialogue.
The idea that patients, professionals and communities can be engaged at the micro‐, meso‐ and macrolevels has been proposed elsewhere 34 and our main contribution is to add a common theoretical architecture to connect engagement among domains and levels. The model bridges the engagement literature with broader research traditions on ecological approaches to health and social capital. 15 , 32 , 36 , 74 Proposed categories of the engagement typology (e.g., information, consultation, participation, partnership and activism) are not new 1 , 2 and the main innovation is to present them in a reciprocal perspective to describe engagement relationships led by professionals, communities or both. The evolutive nature of engagement presented in this paper resonates with other scholars looking at engagement as a ‘journey’ that transforms its actors and context over time. 77
Theoretical models perform a central role in mediating between science and practice. 78 Because of its broad perspective, translation of the Ecology of Engagement into a specific engagement domain and projects will require adaptation. For example, an ecological perspective of engagement in research requires clarification of relevant institutions (e.g., research centres), policies (e.g., research policies), social norms (e.g., what is recognized as valid knowledge) and individual factors (e.g., researchers' attitude toward engagement) that can affect engagement.
Future research: As simplified versions of complex realities, ‘all models are wrong but some are useful’. 79 Readers should keep in mind that the Ecology of Engagement presents a set of organized hypotheses to be tested by empirical research (e.g., the density, diversity and intensity of engagement relationships influences health coproduction, resilience, equity and entropy). ‘A theory is a tender growth, naturally imperfect when first proposed’ and requires further testing, refinement and critical questioning. 16 Ecological perspectives, because of their multilayered and dynamic nature, should raise caution about simple statements of cause and effects (e.g., ‘more engagement leads to better health at a reduced cost’). Further research, critical testing and refinement of the model are required:
-
1.
First, there is a need to synthesize what is known about ecological factors influencing engagement. A number of reviews have highlighted social, organizational and individual‐level factors that influence the engagement process and outcomes. 47 , 48 Conversely, abundant literature has documented the impacts of engagement on individuals, institutions and policies. 18 , 38 , 39 , 40 , 41 , 42 , 43 , 44 However, this literature remains highly fragmented and siloed (e.g., engagement in care, education, research, quality improvement, service delivery, health promotion and policy). The literature is in need of an ‘ecological synthesis’ to reconnect the pieces together and build a more comprehensive view of the ecosystemic relationships between engagement and health. Such an integrated approach to research is pragmatically important to build coherent engagement policies across sectors, as opposed to fragmented and short‐lived engagement support strategies.
-
2.
The Ecology of Engagement Model reframes engagement as dynamic relationships embedded in evolutive ecological systems, rather than framing engagement as a static ‘intervention’ or ‘method’ designed by professionals. An instrumental approach to engagement is prominent in the evidence‐based medicine literature, which has sought to test the effectiveness of engagement in achieving predefined outcomes. 19 Adoption of an ecological perspective pushes researchers to approach engagement differently, calling for explicit consideration of the mutual influences between engagement and its ecological context. It also points towards the unexpected effects of engagement beyond its predefined objectives, as professionals and community actors are transformed by their engagement relationships. It also underlines the potential for engagement to reshape the ecological context in which it is embedded by transforming organizations, communities, culture and social norms. This constant interplay between engagement and its ecological contexts requires innovative, flexible and dynamic approaches to research and evaluation. 80 , 81
-
3.
Finally, the primary literature is in need of theoretically sound research on the long‐term influence of engagement over time (e.g., how mesolevel engagement of patients in research can have ‘upstream’ influence on macrolevel policies or ‘downstream’ influence on individual care and population health). An ecological perspective calls for long‐term follow‐up of the rippling effects of engagement, an important gap in the existing scientific literature that is still dominated by short‐term descriptive studies of engagement initiatives. 20
6. CONCLUSION
In conclusion, the Ecology of Engagement opens new avenues for engagement practice and science by proposing an integrated, interdependent and reciprocal model of engagement in health ecosystems. Grounded in a coproduction of health perspective, the model adopts a reciprocal typology of engagement relationships among individuals and groups, acknowledging dynamic changes in the leadership between community members and professionals. The model can serve as a common sketch to foster dialogue between system leaders, engagement practitioners and scientists to drive cooperative efforts on health system improvement, sustainability, resilience and equity. Future research should strengthen ecological perspectives on engagement, drawing from decades of experience in other research disciplines.
AUTHOR CONTRIBUTIONS
Antoine Boivin was involved in the conceptualization of the Ecology of Engagement Model and typology, drafting the manuscript and visual representation. Vincent Dumez, Geneviève Castonguay and Alexandre Berkesse contributed important intellectual input to the model conceptualization, description, visual representation and illustrative examples. All reviewed and approved the final version of the manuscript.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
Antoine Boivin holds the Canada Research Chair in Partnership with Patients and Communities. Genevieve Castonguay is supported by the Quebec SUPPORT Unit for Learning Health Systems (Unité Soutien SSA‐Québec). Angela Coulter (Oxford University) contributed substantive comments on the integrated model, its relationship with engagement theories and its empirical health system implications. Kristin Carman (Patient‐Centred Outcome Institutes) commented on the potential applications of an integrated ecological model and its contribution to existing conceptual frameworks for engagement in research, care and policy. Members of the Canada Research Chair in Partnership with Patients and Communities (Ghislaine Rouly, Emilie Lessard, Gwenvaël Ballu, Christine St‐Onge) commented on early versions of the model. Members of the Center of Excellence for Partnership with Patients and the Public (including four senior patient partners engaged in health policy, research, education and care) contributed to clarifications of the model, linkages with lived experience of engagement and offered potential applications of the model for engagement practice. Conceptual clarifications were brought by Mathieu Bouchard (social capital theory, epistemic foundations) and Audrey L'Espérance (activism theory, discursive turn in social sciences). François‐Pierre Gauvin and Paule Lebel contributed to early iterations of the typology of engagement (‘Engagement Loop’). Pascale Lehoux (University of Montreal School of Public Health) helped illustrate the illustrative examples of the relationships between engagement and environmental health. Graphic design was realized by Jonathan Rehel. Antoine Boivin holds the Canada Research Chair in Partnership with Patients and Communities (Government of Canada Research Chairs programme). Genevieve Castonguay is supported by the Quebec SUPPORT Unit for Learning Health Systems (Unité Soutien SSA‐Québec). Vincent Dumez is supported by the Université de Montréal Faculty of Medicine. Alexandre Berkesse is supported by the French School of Public Health (EHESP) and Center of Excellence for Partnership with Patients and the Public. Funding organizations had no role in the model development, preparation and approval of the manuscript.
Boivin A, Dumez V, Castonguay G, Berkesse A. The Ecology of Engagement: fostering cooperative efforts in health with patients and communities. Health Expect. 2022;25:2314‐2327. 10.1111/hex.13571
DATA AVAILABILITY STATEMENT
The data availability statement does not apply.
REFERENCES
- 1. Arnstein S. A ladder of citizen participation in the USA. J Am Inst Plann. 1969;35(4):216‐224. [Google Scholar]
- 2. Rowe G, Frewer L. A typology of public engagement mechanisms. Sci Technology Hum Values. 2005;30(2):251‐290. 10.1177/0162243904271724 [DOI] [Google Scholar]
- 3. Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Affair. 2013;32(2):223‐231. 10.1377/hlthaff.2012.1133 [DOI] [PubMed] [Google Scholar]
- 4. Pomey MP, Flora L, Karazivan P, et al. The Montreal model: the challenges of a partnership relationship between patients and healthcare professionals. Sante Publique. 2015;27:S41‐S50. [PubMed] [Google Scholar]
- 5. Hall MA, Schneider CE. Patients as consumers: courts, contracts, and the new medical marketplace. Mich Law Rev. 2008;106(4):643‐689. [PubMed] [Google Scholar]
- 6. Williams O, Robert G, Martin GP, Hanna E, O'Hara J. Is co‐production just really good PPI? Making sense of patient and public involvement and co‐production networks. In: Bevir M, Waring J, eds. Decentring Health and Care Networks. Organizational Behaviour in Healthcare. Palgrave Macmillan; 2020:213‐237. 10.1007/978-3-030-40889-3_10 [DOI] [Google Scholar]
- 7. Rifkin SB. Paradigms lost: toward a new understanding of community participation in health programmes. Acta Trop. 1996;61(2):79‐92. 10.1016/0001-706x(95)00105-n [DOI] [PubMed] [Google Scholar]
- 8. Filipe A, Renedo A, Marston C. The co‐production of what? Knowledge, values, and social relations in health care. PLoS Biol. 2017;15(5):e2001403. 10.1371/journal.pbio.2001403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Coulter A. Engaging Patients in Healthcare. Open University Press; 2011. [Google Scholar]
- 10. Barr V, Robinson S, Marin‐Link B, et al. The expanded chronic care model. Hosp Q. 2003;7(1):73‐82. [DOI] [PubMed] [Google Scholar]
- 11. Popay J, Whitehead M, Ponsford R, Egan M, Mead R. Power, control, communities and health inequalities I: theories, concepts and analytical frameworks. Health Promot Int. 2020;36(5):1253‐1263. 10.1093/heapro/daaa133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Boivin A, Rouly G, Dumez V, Pomey MP, Karazivan P, Wong C. International Summit on Patient and Public Partnership (Synthesis). May 3, 2019. Accessed June 1, 2022. www.ceppp.ca/isppp
- 13. Richards T. Transforming healthcare—one flower at a time. BMJ . 2019. Accessed July 17, 2022. https://blogs.bmj.com/bmj/2019/05/10/tessa-richards-transforming-healthcare-one-flower-at-a-time/
- 14. Maurer M, Dardess P, Rouse TB. Patient and family engagement in the United States: a social movement from patient to advocate to partner. In: Pomey MP, Denis JL, Dumez V, eds. Patient Engagement. Organizational Behaviour in Healthcare. Palgrave Macmillan; 2019:91‐128. 10.1007/978-3-030-14101-1_5 [DOI] [Google Scholar]
- 15. McLaren L, Hawe P. Ecological perspectives in health research. J Epidemiol Community Health. 2005;59(1):6‐14. 10.1136/jech.2003.018044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Eysenck HJ. “There is Nothing More Practical Than A Good Theory” (Kurt Lewin)—true or false? Adv Psychol. 1987;40:49‐64. 10.1016/s0166-4115(08)60064-3 [DOI] [Google Scholar]
- 17. Lynham SA. The general method of theory‐building research in applied disciplines. Adv Dev Hum Resour. 2002;4(3):221‐241. 10.1177/1523422302043002 [DOI] [Google Scholar]
- 18. Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1):1‐22. 10.1186/s13012-018-0784-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database Syst Rev. 2006;3(3):CD004563. 10.1002/14651858.cd004563.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brett J, Staniszewska S, Mockford C, Seers K, Herron‐Marx S, Bayliss H. The PIRICOM Study: a systematic review of the conceptualisation, measurement, impact and outcomes of patients and public involvement in health and social care research. 2010. Accessed July 17, 2022. https://www.ukcrc.org/wp-content/uploads/2014/03/Piricom%2BReview%2BFinal%2B2010.pdf
- 21. Cohen IR, Harel D. Explaining a complex living system: dynamics, multi‐scaling and emergence. J Roy Soc Interface. 2007;4(13):175‐182. 10.1098/rsif.2006.0173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mella P, Gazzola P. The holonic view of organizations and firms. Syst Res Behav Sci. 2017;34(3):354‐374. 10.1002/sres.2457 [DOI] [Google Scholar]
- 23. Aktouf O. La stratégie de l'autruche: post‐mondialisation, management et rationalité économique. 2002. Accessed July 17, 2022. https://ecosociete.org/livres/la-strategie-de-l-autruche
- 24. DeAngelis D, Waterhouse J. Equilibrium and nonequilibrium concepts in ecological models. Ecol Monograph. 1987;57(1):1‐21. [Google Scholar]
- 25. Barello S, Graffigna G, Vegni E, Bosio AC. The challenges of conceptualizing patient engagement in health care: a lexicographic literature review. 2014.
- 26. Salsberg J, Macridis S, Bengoechea EG, Macaulay AC, Moore S. The shifting dynamics of social roles and project ownership over the lifecycle of a community‐based participatory research project. Fam Pract. 2017;34(3):305‐312. 10.1093/fampra/cmx006 [DOI] [PubMed] [Google Scholar]
- 27. Lasker RD, Weiss ES, Miller R. Partnership synergy: a practical framework for studying and strengthening the collaborative advantage. Milbank Q. 2001;79(2):179‐205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zoller HM. Health activism: communication theory and action for social change. Commun Theory. 2005;15:341‐364. [Google Scholar]
- 29. Lee MA, Smith TJ, Henry RG. Power politics: advocacy to activism in social justice counseling. J Soc Action Couns Psychol. 2018;5(3):70‐94. 10.33043/jsacp.5.3.70-94 [DOI] [Google Scholar]
- 30. Wong‐Rieger D. Moving from patient advocacy to partnership: A long and bumpy road. Patient. 2017;10(3):271‐276. 10.1007/s40271-017-0216-1 [DOI] [PubMed] [Google Scholar]
- 31. Shields CM. Transformative leadership: working for equity in diverse contexts. Educ Admin Quart. 2010;46(4):558‐589. 10.1177/0013161x10375609 [DOI] [Google Scholar]
- 32. Poortinga W. Community resilience and health: the role of bonding, bridging, and linking aspects of social capital. Health Place. 2012;18(2):286‐295. 10.1016/j.healthplace.2011.09.017 [DOI] [PubMed] [Google Scholar]
- 33. Perras CP, Normandin JM. Mesurer Le Capital Social: Guide Destiné Aux Organisations. 2019. pp. 1‐34.
- 34. Codsi MP, Boivin A, Karazivan P, Rouly G, Leclair M. Changing relationships: how does patient involvement transform professional identity? An ethnographic study. BMJ Open. 2021;11:e045520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Linstead A, Brewis J. Beyond boundaries: towards fluidity in theorizing and practice. Gend Work Organ. 2021;11(4):355‐362. [Google Scholar]
- 36. Adler P, Kwon SW. Social capital: prospects for a new concept. Acad Manage Rev. 2002;27(1):17‐40. [Google Scholar]
- 37. Grannovetter M. The strength of weak ties. Am J Sociol. 1973;78(6):1360‐1380. [Google Scholar]
- 38. Milton B, Attree P, French B, Povall S, Whitehead M, Popay J. The impact of community engagement on health and social outcomes: a systematic review. Community Dev J. 2011;47(3):316‐334. 10.1093/cdj/bsr043 [DOI] [PubMed] [Google Scholar]
- 39. Djellouli N, Jones L, Barratt H, Ramsay AIG, Towndrow S, Oliver S. Involving the public in decision‐making about large‐scale changes to health services: a scoping review. Health Policy. 2019;123(7):635‐645. 10.1016/j.healthpol.2019.05.006 [DOI] [PubMed] [Google Scholar]
- 40. Morris G, Simon G, Debra T, Michael R, Ernie M, Angela M. Patient/service user involvement in medical education: a best evidence medical education (BEME) systematic review: BEME Guide No. 58. Med Teach . 2019:1‐13. 10.1080/0142159x.2019.1652731 [DOI] [PubMed]
- 41. Haldane V, Chuah FLH, Srivastava A, et al. Community participation in health services development, implementation, and evaluation: a systematic review of empowerment, health, community, and process outcomes. PLoS One. 2019;14(5):e0216112‐e0216125. 10.1371/journal.pone.0216112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sharma AE, Rivadeneira NA, Barr‐Walker J, Stern RJ, Johnson AK, Sarkar U. Patient engagement in health care safety: an overview of mixed‐quality evidence. Health Aff. 2018;37(11):1813‐1820. 10.1377/hlthaff.2018.0716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res. 2014;14(1):1‐9. 10.1186/1472-6963-14-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Boaz A, Hanney S, Jones T, Soper B. Does the engagement of clinicians and organisations in research improve healthcare performance: a three‐stage review. BMJ Open. 2015;5(12):e009415. 10.1136/bmjopen-2015-009415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Weger ED, Vooren NV, Luijkx KG, Baan CA, Drewes HW. Achieving successful community engagement: a rapid realist review. BMC Health Serv Res. 2018;18(1):285. 10.1186/s12913-018-3090-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jagosh J, Bush PL, Salsberg J, et al. A realist evaluation of community‐based participatory research: partnership synergy, trust building and related ripple effects. BMC Public Health. 2015;15(1):1‐11. 10.1186/s12889-015-1949-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Boivin A, Dumez V, Fancott C, L'Espérance A. Growing a healthy ecosystem for patient and citizen partnerships. Healthc Q Tor Ont. 2018;21(SP):73‐82. 10.12927/hcq.2018.25634 [DOI] [PubMed] [Google Scholar]
- 48. Baker R, Judd M, Fancott C, Maika C. Creating “Engagement‐Capable Environments” in healthcare. In: Patient Engagement—Catalyzing Improvement and Innovation in Healthcare. n.d.;11‐34. Accessed July 17, 2022. https://www.longwoods.com/content/24908/books%2B/creating-engagement-capable-environments-in-healthcare
- 49. Barker SL, Maguire N. Experts by experience: peer support and its use with the homeless. Community Ment Health J. 2017;53(5):598‐612. 10.1007/s10597-017-0102-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Planck M. Initiation à La Physique. Flamarion; 2013. [Google Scholar]
- 51. Wells KB, Jones L, Chung B, et al. Community‐partnered cluster‐randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. J Gen Intern Med. 2013;28(10):1268‐1278. 10.1007/s11606-013-2484-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Boivin A, Rouly G. Community initiative co‐led with patients could improve care for people with complex health and social needs. BMJ . 2020. Accessed July 17, 2022. https://blogs.bmj.com/bmj/2020/02/28/community-initiative-co-led-with-patients-could-improve-care-for-people-with-complex-health-and-social-needs/
- 53. O'Mara‐Eves A, Brunton G, McDaid D, et al. Community engagement to reduce inequalities in health: a systematic review, meta‐analysis and economic analysis. Public Health Res. 2013;1(4):1‐526. 10.3310/phr01040 [DOI] [PubMed] [Google Scholar]
- 54. Abel J, Kingston H, Scally A, et al. Reducing emergency hospital admissions: a population health complex intervention of an enhanced model of primary care and compassionate communities. Br J Gen Pract. 2018;68(676):e803‐e810. 10.3399/bjgp18x699437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Laurance J, Henderson S, Howitt PJ, et al. Patient engagement: four case studies that highlight the potential for improved health outcomes and reduced costs. Health Aff. 2017;33(9):1627‐1634. 10.1377/hlthaff.2014.0375 [DOI] [PubMed] [Google Scholar]
- 56. Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change, too. Health Aff. 2017;34(3):431‐437. 10.1377/hlthaff.2014.0452 [DOI] [PubMed] [Google Scholar]
- 57. Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2020;397(10269):129‐170. 10.1016/s0140-6736(20)32290-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Pencheon D, Wight J. Making healthcare and health systems net zero. BMJ. 2020;368:m970. 10.1136/bmj.m970 [DOI] [PubMed] [Google Scholar]
- 59. Wise J. Climate crisis: over 200 health journals urge world leaders to tackle “catastrophic harm.”. BMJ. 2021;374:n2177. 10.1136/bmj.n2177 [DOI] [PubMed] [Google Scholar]
- 60. Nissen S, Wong JHK, Carlton S. Children and young people's climate crisis activism—a perspective on long‐term effects. Child Geogr. 2020;19(3):1‐7. 10.1080/14733285.2020.1812535 [DOI] [Google Scholar]
- 61. Schneider EC, Sarnak DO, Squires D, Shah A, Doty MM. Mirror, Mirror 2017: International Comparison Reflects Flaws and Opportunities for Better U.S. Health Care. 2017. 10.15868/socialsector.27698 [DOI]
- 62. Farrer L, Marinetti C, Cavaco YK. Advocacy for health equity: a synthesis review. Milbank Q. 2015;93(2):392‐437. 10.1111/1468-0009.12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Anoko JN, Barry BR, Boiro H, et al. Community engagement for successful COVID‐19 pandemic response: 10 lessons from Ebola outbreak responses in Africa. BMJ Glob Heal. 2020;4(suppl 7):e003121. 10.1136/bmjgh-2020-003121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Barker KM, Ling EJ, Fallah M, et al. Community engagement for health system resilience: evidence from Liberia's Ebola epidemic. Health Policy Plan. 2020;35(4):416‐423. 10.1093/heapol/czz174 [DOI] [PubMed] [Google Scholar]
- 65. Gillespie AM, Obregon R, Asawi RE, et al. Social mobilization and community engagement central to the Ebola response in West Africa: lessons for future public health emergencies. Global Health Sci Pract. 2016;4(4):626‐646. 10.9745/ghsp-d-16-00226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Rajan D, Koch K, Rohrer K, et al. Governance of the Covid‐19 response: a call for more inclusive and transparent decision‐making. BMJ Glob Health. 2020;5(5):e002655. 10.1136/bmjgh-2020-002655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Immonen K. The views of patients and the public should be included in policy responses to covid‐19. BMJ . 2020. Accessed July 17, 2022. https://blogs.bmj.com/bmj/2020/03/30/the-views-of-patients-and-the-public-should-be-included-in-policy-responses-to-covid-19/
- 68. Gilmore B, Ndejjo R, Tchetchia A, et al. Community engagement for COVID‐19 prevention and control: a rapid evidence synthesis. BMJ Glob Health. 2020;5(10):e003188. 10.1136/bmjgh-2020-003188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. WHO . Risk communication and community engagement for COVID‐19 contact tracing. n.d. Accessed July 17, 2022. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/risk-communication-and-community-engagement/
- 70. Mouter N, Hernandez JI, Itten AV. Public participation in crisis policymaking. how 30,000 Dutch citizens advised their government on relaxing COVID‐19 lockdown measures. PLoS One. 2021;16(5):e0250614. 10.1371/journal.pone.0250614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Janke AT, Mei H, Rothenberg C, Becher RD, Lin Z, Venkatesh AK. Analysis of hospital resource availability and COVID‐19 mortality across the United States. J Hosp Med. 2021;16:E1‐E4. 10.12788/jhm.3539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Berger E, Winkelmann J, Eckhardt H, et al. A country level analysis comparing hospital capacity and utilisation during the first COVID‐19 wave across Europe. Health Policy . 2021. 10.21203/rs.3.rs-251815/v1 [DOI] [PMC free article] [PubMed]
- 73. Finnigan R. Self‐reported impacts of the COVID‐19 pandemic for people experiencing homelessness in Sacramento, California. J Soc Distress Homeless. 2021;31:1‐9. 10.1080/10530789.2021.1879618 [DOI] [Google Scholar]
- 74. Szreter S, Woolcock M. Health by association? Social capital, social theory, and the political economy of public health. Int J Epidemiol. 2004;33(4):650‐667. 10.1093/ije/dyh013 [DOI] [PubMed] [Google Scholar]
- 75. Sanders EBN, Stappers PJ. Co‐creation and the new landscapes of design. Codesign. 2008;4(1):5‐18. 10.1080/15710880701875068 [DOI] [Google Scholar]
- 76. Proctor J. The social construction of nature: relativist accusations, pragmatist and critical realist responses. Ann Assoc Am Geogr. 1998;88(3):352‐376. [Google Scholar]
- 77. Switzer S, Flicker S, McClelland A, et al. Journeying together: a visual exploration of “engagement” as a journey in HIV programming and service delivery. Health Place. 2020;61:102247. 10.1016/j.healthplace.2019.102247 [DOI] [PubMed] [Google Scholar]
- 78. Jariego IM. Ecological settings and theory of community action. Glob J Community Psychol Pract . 2016;7(2). 10.7728/0702201605 [DOI] [Google Scholar]
- 79. Box GEP. Robustness in the strategy of scientific model building. Robustness in Statistics. Academic Press; 1979:201‐236. 10.1016/b978-0-12-438150-6.50018-2 [DOI] [Google Scholar]
- 80. Rifkin SB. Examining the links between community participation and health outcomes: a review of the literature. Health Policy Plan. 2014;29(suppl_2):ii98‐ii106. 10.1093/heapol/czu076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. South J, Phillips G. Evaluating community engagement as part of the public health system. J Epidemiol Community Health. 2014;68(7):692‐696. 10.1136/jech-2013-203742 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data availability statement does not apply.


