Abstract
Background
Constipation seriously affects people’s life quality, and dietary adjustment has been one of the effective methods. Overall dietary quality has been reported to be associated with some diseases, while its association with constipation has not been reported. This study aims to explore the association between overall dietary quality and constipation.
Methods
A cross-sectional study was designed and data were extracted from National Health and Nutrition Examination Survey (NHANES). Overall dietary quality was assessed by healthy eating index-2015 (HEI-2015), and constipation was defined by either stool consistency or stool frequency. The association between overall dietary quality or components of HEI-2015 and constipation was assessed using logistic regression, with results expressed as odds ratio (OR) and 95% confidence intervals (95%CI). Subgroup analysis was conducted according to age and gender.
Results
A total of 13,945 participants were eligible, with 1,407 in constipation group and 12,538 in non-constipation group. Results showed that higher adherence to HEI-2015 was associated with reduced odds of constipation (OR: 0.98, 95%CI: 0.98–0.99) after adjusting potential confounders. Further, we found higher intake of total fruits, whole fruits, total vegetables, greens and beans, whole grains, total protein foods, seafood and plant proteins, and higher fatty acids ratio decreased the odds of constipation, while higher intake of sodium increased the odds (all P < 0.05). We also found negative association between HEI-2015 and constipation in participants with male sex, female sex, age ≥ 65 years, and age < 65 years (all P < 0.05).
Conclusion
We found higher adherence to HEI-2015 decreased the odds of constipation, suggesting that increasing HEI-2015 adherence may be one of effective methods to alleviate constipation.
Supplementary information
The online version contains supplementary material available at 10.1186/s12889-022-14360-w.
Keywords: Healthy eating index, Overall dietary quality, Constipation, Stool consistency, Stool frequency
Background
Constipation is characterized by bowel movements less than three times a week and hard, dry, or lumpy stools [1]. The prevalence of constipation ranges from 7 to 10% in adults, and the prevalence varies by age [2, 3]. Furthermore, the incidence of constipation is different between man and women, with 6% higher in women than that of men [4]. Constipation is associated with poor quality of life, resulting in anxiety, depression, and cognitive impairment [5, 6]. Besides, constipation elevates healthcare burden. The cost of constipation treatment is estimated over $230 million each year in America [7]. Generally, constipation is treated with dietary adjustment prior to medical intervention to minimize side effects of some drugs [8].
Healthy eating index (HEI) is a measure used to evaluate the overall dietary quality, and HEI is density-based rather than absolute amounts since the 2015 version [9]. HEI-2015 is scored based on the Dietary Guidelines for Americans (DGA) and consist of 13 food groups or nutrients with their correspondent to recommended intake levels [9]. The nine adequacy components of HEI include total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, and fatty acids. The four moderation components include refined grains, sodium, added sugars, and saturated fats. The maximum score of each component is 5 or 10, and the total score is 100, with a higher score indicating better compliance. Studies have reported the relationships between single nutrients or foods and constipation, such as lipid-rich foods, total fats, starch, sugary products, sodium, and water intake [10, 11]. In real life, people do not consume individual nutrients or certain foods, but rather mixed foods containing various nutrients [12].
Under this background, overall dietary quality has gained attention in studies of the relationship between diet and diseases [13, 14]. Association between overall dietary quality assessed by HEI and some diseases, such as diabetes, hypertension, and sleep disorder has been elucidated [15–17]. However, studies on the association between HEI-2015 and constipation have not been reported. In view of this, our study aims to assess associations of HEI-2015 with constipation.
Methods
Study design and data source
This was a cross-sectional study designed to conduct a secondary data analysis based on the National Health and Nutrition Examination Survey (NHANES) database (https://www.cdc.gov/nchs/nhanes/about_nhanes.htm) and the National Center for Health Statistics (NCHS) collected the data. NHANES is a research project aimed to evaluate the health and nutritional status of adults and children in the America. Each year, the survey visits 15 of counties across the country and examines a nationally representative sample of about 5,000 persons. The unique of this database is the combination of interviews and physical examinations. The interview contains demographic, dietary, socioeconomic, and health-related questions. The examination includes medical, dental, physiological, and laboratory measurements. Written informed consent was provided by all participants at the time of the survey. All NHANES data are de-identified and all NHANES studies have been approved by the National Center for Health Statistics Research Ethics Review Board (ERB) (https://www.cdc.gov/nchs/nhanes/irba98.htm). The requirement of ethical approval was waived by the Institutional Review Board of Subei People’s Hospital of Jiangsu Province, because the data was accessed from NHANES (a publicly available database). All procedures were carried out in accordance with relevant guidelines and regulations (https://www.cdc.gov/nchs/data_access/restrictions.htm).
Study population
The data of participants were extracted from 2005 to 2010 NHANES due to these three 2-year cycles (2005–2006, 2007–2008, 2009–2010) recorded data on constipation. Participants who aged equal to or over 20 years old, completed at least one valid 24-hour dietary recall, and with complete bowel health questionnaire were included. Participants who had extreme total energy intakes of < 500 or > 5000 kcal/day for women, and < 500 or > 8000 kcal/day for men [18], with self-reported history of inflammatory bowel disease (ulcerative colitis or crohn’s disease), celiac disease, and/or colon cancer, and pregnant women were excluded.
The 24-hour dietary recall interview were conducted by trained dietary interviewers fluent in Spanish and English. Dietary data were collected on both weekdays and weekends, and participants were requested to recall all the food and beverages consumed in the past 24 h (midnight to midnight). To obtain a more complete picture of daily dietary intake, two 24-hour dietary recalls were requested. The first dietary recall was performed by in-person interview in the Mobile Examination Center (MEC). The second dietary recall was performed by telephone scheduled 3 to 10 days later. Participants were provided with a standard set of measuring guides to help participants estimate portion sizes during both interviews, as well as a food model booklet to help report food amounts during the telephone interview [19–21].
The dietary data were collected with a computer-assisted food coding and utilized the U.S Department of Agriculture (USDA) Automated Multiple-Pass Method to account for day-to-day variations. The nutritional values of all food and beverages were provided by the USDA’s Food and Nutrient Database for Dietary Studies (FNDDS), which was regularly updated each cycle and supplied the nutrient profiles for every food and beverage reported in NHANES [19, 20, 22]. In this study, we used the reported value for the participants completed one 24-hour dietary recalls, and we used the average value for those completed two recalls [19].
Dietary quality assessment
The dietary quality was assessed by HEI-2015, which contained nine adequacy components and four moderation components [9]. For adequacy components, they were encouraged to consume and higher scores reflected higher intakes. For moderation components, they were limited to consume and higher scores reflected lower intakes. The adequacy components were total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, and fatty acids [ratio of poly- and monounsaturated fatty acids (PUFAs and MUFAs) to saturated fatty acids (SFAs)]. The moderation components were refined grains, sodium, added sugars, and saturated fats. Supplementary Table 1 shows the components, recommended intake levels, and calculation method of HEI-2015. The total score of HEI-2015 was 100, with higher score indicating better overall dietary quality.
Constipation definition
Constipation was defined by either stool consistency or stool frequency based on the NHANES database [23, 24]. Stool consistency and stool frequency were recorded for 30 days before data collection.
Stool consistency was estimated using the Bristol stool form scale, which included various colorful cards and detailed descriptions of seven stool types (Type 1: separate hard lumps, like nuts; Type 2: sausage-like, but lumpy; Type 3: like a sausage but with cracks in the surface; Type 4: like a sausage or snake, smooth and soft; Type 5: soft blobs with clear-cut edges; Type 6: fluffy pieces with ragged edges, a mushy stool; and Type 7: watery, no solid pieces) [25]. Participants were asked “Please look at this card and tell me the number that corresponds with your usual or most common stool type?” Constipation was defined as Type 1 or Type 2. Types 3–7 were defined as non-constipation [25].
Stool frequency was assessed with the following question: “How many times per week do you usually have a bowel movement?” Those who answered less than 3 times per week was defined as constipation, and 3 times or over per week was defined as non-constipation.
Data collection
The data were extracted based on demographic characteristics [gender, age, race, education level, marital status, family income, comorbidity (hypertension and depression), and body mass index (BMI)]; lifestyle characteristics (drinking, smoking, vigorous physical activity, and moderate physical activity); dietary intake (total energy intake); laboratory parameters (cotinine); and dietary supplements, calcium supplement, and use of laxatives.
The demographic characteristics (assessed via interview) included gender (male or female), age (divided into < 65 years and ≥ 65 years), race (Mexican American, Other Hispanic, Non-hispanic White, Non-Hispanic Black, Other Race-Including Multi-Racial), education level (less than or equal to 12th grade, General Educational Development, and college or above), marital status (married, widowed, divorced/separated, and never married), family income (< 20,000$ and ≥ 20,000$), and comorbidity (hypertension and depression), and BMI. BMI was not self-reported, and it was calculated as body weight (kg)/height (m)2. Weight and height were measured at the MEC. Weight was taken on a Toledo digital scale. When participants were properly positioned and the digital readout was stable, the recorder called the weight and entered it into the weight box of the automated system. Weight was measured in pounds and converted to kilograms in the automated system. Standing height was an evaluation of maximum vertical size, and measured with a fixed stadiometer with a vertical backboard and a moveable headboard. Participants were request to remove any ornaments and braids from the top of the head for accurate stature measurement.
The lifestyle characteristics contained drinking, smoking, vigorous physical activity, and moderate physical activity (assessed via interview). The participants had at least 12 alcohol drinks per year was defined as drinking. Those who smoked at least 100 cigarettes in the entire life was defined as smoking. The moderate physical activity was defined by doing moderate activities, such as brisk walking, bicycling for pleasure, golf, and dancing, that cause only light sweating or a slight to moderate increase in breathing or heart rate for at least 10 min over the past 30 days. The vigorous activities were defined by doing any vigorous activities, such as running, lap swimming, aerobics classes, or fast bicycling, that caused heavy sweating or large increases in breathing or heart rate for at least 10 min over the past 30 days.
Dietary supplements, calcium supplement, and use of laxatives were self-reported. When asked “Have you used or taken any vitamins, minerals or other dietary supplements in the past 30 days?”, someone answered “Yes” was considered to take dietary supplements. The intake of calcium supplement was obtained using 24-hour dietary recall.
Statistical analysis
The data in this study were weighted using appropriate sample weights provided by NHANES to account for complex sampling design of NHANES. The continuous data were represented as mean (standard error) (S.E), and differences between groups were compared using t test. The categorical data were shown as number (n) and percentage (%), and differences between groups were examined using chi-squared test. The missing data were processed using multiple imputation through R 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria).
Logistic regression analysis was used to explore the association between HEI-2015 and constipation, and results were expressed as odds ratio (OR) with 95% confidence intervals (95%CI). Model 1 was unadjusted model. Model 2 adjusted age and gender to decrease the selective bias. Based on Model 2, Model 3 further adjusted race, education level, marital status, family income, BMI, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, total energy intake, dietary supplements and calcium supplement which had statistical significance in general characteristics between the two groups.
The multiplicative interaction between age (or gender) and HEI-2015 on the odds of constipation was assessed using the logistic regression analysis. The sensitivity analysis was performed to avoid the bias caused by multiple imputation and different definitions of constipation. The subgroup analysis was performed based on age and gender. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) and two-sided P < 0.05 was considered statistically significant.
Results
Participants selection and general characteristics of the selected participants
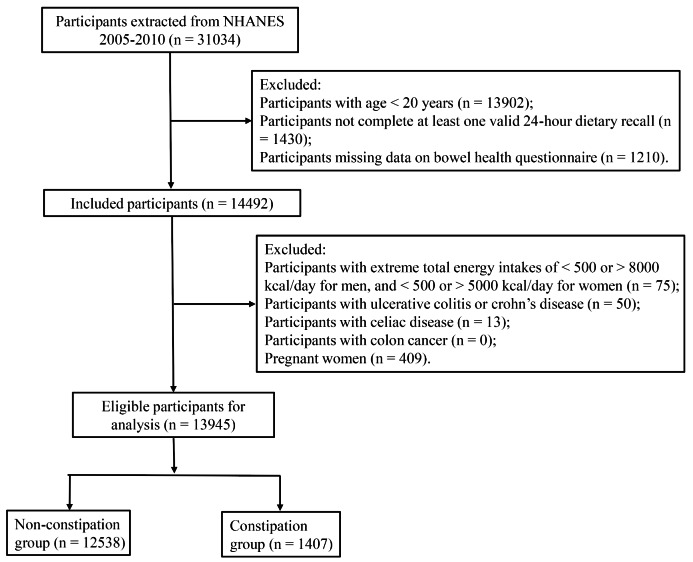
We extracted 31,034 participants from the NHANES database. After excluding participants with age < 20 years (n = 13,902), not complete at least one valid 24-hour dietary recall (n = 1,430), and missing data on bowel health questionnaire (n = 1,210), 14,492 participants were included. Further, we excluded participants with extreme total energy intakes (n = 75), with ulcerative colitis or crohn’s disease (n = 50), with celiac disease (n = 13), with colon cancer (n = 0), and pregnant women (n = 409), 13,945 participants were eligible for analysis (1,407 participants in the constipation group and 12,538 participants in the non-constipation group) (Fig. 1).
Fig. 1.
The flowchart of selecting participants
Of the eligible participants, there were 49.59% of male (n = 7,075) and 82.68% of participants aged less than 65 years (n = 10,488). Gender, BMI, race, education level, marital status, family income, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, total energy intake, dietary supplements, calcium supplement, and HEI score were significantly different between constipation group and non-constipation group (all P < 0.05) (Table 1). Further, we compared the components of HEI-2015 between the two groups, and found the statistical difference in whole fruits, total vegetables, greens and beans, whole grains, total protein foods, seafood and plant proteins, sodium, and added sugars (Supplementary Table 2).
Table 1.
General Characteristics of the participants from the National Health and Nutrition Examination Survey 2005–2010
| Characteristic |
Total
(n = 13,945) |
Non-constipation (n = 12,538) |
Constipation
(n = 1407) |
P |
|---|---|---|---|---|
| Gender, n (%) | < 0.001 | |||
| Female | 6870 (50.41) | 5898 (47.96) | 972 (73.85) | |
| Male | 7075 (49.59) | 6640 (52.04) | 435 (26.15) | |
| Age, n (%) | 0.202 | |||
| < 65 years | 10,488 (82.68) | 9395 (82.54) | 1093 (84.05) | |
| ≥ 65 years | 3457 (17.32) | 3143 (17.46) | 314 (15.95) | |
| BMI, kg/m2, Mean (S.E) | 28.71 (0.10) | 28.80 (0.11) | 27.84 (0.25) | < 0.001 |
| Race, n (%) | < 0.001 | |||
| Mexican American | 2506 (8.04) | 2280 (8.07) | 226 (7.80) | |
| Non-Hispanic Black | 2779 (10.84) | 2411 (10.28) | 368 (16.21) | |
| Non-Hispanic White | 6938 (71.45) | 6314 (72.02) | 624 (65.96) | |
| Other Hispanic | 1171 (4.33) | 1030 (4.24) | 141 (5.20) | |
| Other Race | 551 (5.33) | 503 (5.39) | 48 (4.83) | |
| Education level, n (%) | < 0.001 | |||
| ≤ 12th | 3906 (18.15) | 3447 (17.71) | 459 (22.32) | |
| GED | 3361 (24.53) | 2971 (24.02) | 390 (29.49) | |
| College or above | 6678 (57.32) | 6120 (58.27) | 558 (48.19) | |
| Marital status, n (%) | < 0.001 | |||
| Married | 7433 (57.15) | 6774 (57.83) | 659 (50.60) | |
| Widowed | 1193 (5.89) | 1055 (5.69) | 138 (7.75) | |
| Divorced/separated | 1982 (12.68) | 1763 (12.47) | 219 (14.71) | |
| Never married | 3330 (24.28) | 2939 (24.00) | 391 (26.94) | |
| Family Income, n (%) | < 0.001 | |||
| < 20,000$ | 3476 (17.43) | 3022 (16.73) | 454 (24.18) | |
| ≥ 20,000$ | 10,469 (82.57) | 9516 (83.27) | 953 (75.82) | |
| Drinking, n (%) | < 0.001 | |||
| No | 3915 (24.02) | 3380 (22.93) | 535 (34.46) | |
| Yes | 10,030 (75.98) | 9158 (77.07) | 872 (65.54) | |
| Smoking, n (%) | < 0.001 | |||
| No | 7265 (52.55) | 6456 (52.03) | 809 (57.56) | |
| Yes | 6680 (47.45) | 6082 (47.97) | 598 (42.44) | |
| Vigorous physical activity, n (%) | 0.007 | |||
| No | 10,763 (71.62) | 9627 (71.08) | 1136 (76.78) | |
| Yes | 3182 (28.38) | 2911 (28.92) | 271 (23.22) | |
| Moderate physical activity, n (%) | < 0.001 | |||
| No | 8010 (50.27) | 7133 (49.79) | 877 (54.87) | |
| Yes | 5935 (49.73) | 5405 (50.21) | 530 (45.13) | |
| Hypertension, n (%) | 0.015 | |||
| No | 9012 (69.14) | 8047 (68.84) | 965 (71.96) | |
| Yes | 4933 (30.86) | 4491 (31.16) | 442 (28.04) | |
| Depression, n (%) | < 0.001 | |||
| No | 12,751 (92.99) | 11,558 (93.71) | 1193 (86.02) | |
| Yes | 1194 (7.01) | 980 (6.29) | 214 (13.98) | |
| Cotinine, ng/mL, Mean (S.E) | 62.56 (2.58) | 62.35 (2.55) | 64.66 (5.72) | 0.657 |
| Total energy intake, kcal, Mean (S.E) | 2129.06 (13.61) | 2153.76 (14.76) | 1891.98 (20.16) | < 0.001 |
| Dietary supplements, n (%) | < 0.001 | |||
| No | 7248 (48.33) | 6444 (47.76) | 804 (53.86) | |
| Yes | 6697 (51.67) | 6094 (52.24) | 603 (46.14) | |
| Calcium supplement (mg), Mean (S.E) | 957.87 (9.03) | 970.38 (9.34) | 837.81 (15.51) | < 0.001 |
| Use of laxatives, n (%) | 0.117 | |||
| No | 13,891 (99.66) | 12,493 (99.70) | 1398 (99.34) | |
| Yes | 54 (0.34) | 45 (0.30) | 9 (0.66) | |
| HEI score, Mean (S.E) | 52.94 (0.29) | 53.19 (0.29) | 50.54 (0.43) | < 0.001 |
Abbreviation: BMI, body mass index; S.E, standard error; GED, General Educational Development; HEI, healthy eating index
Note: The continuous data were shown as mean (S.E), and differences between groups were compared using t test. The categorical data were shown as number and percentage [n (%)], and differences between groups were compared using chi-squared test
Association between HEI-2015 score and constipation
To explore the association between HEI-2015 score and constipation, logistic regression analysis was used. In the unadjusted model, HEI-2015 was negatively associated with constipation (OR: 0.98, 95%CI: 0.98–0.99). Similar result was observed after adjusting age and gender (OR: 0.98, 95%CI: 0.98–0.99). Further adjusting race, education level, marital status, family income, BMI, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, total energy intake, dietary supplements, and calcium supplement, higher HEI-2015 score was associated with the lower odds of constipation. The score was increased by 1 point, and the odds was reduced by 2% (OR: 0.98, 95%CI: 0.98–0.99) (Table 2). To avoid bias caused by multiple imputation, we performed the sensitivity analysis focused on the association of HEI-2015 with constipation before imputation. The results were consistent with those after imputation (Supplementary Table 3).
Table 2.
Association between overall dietary quality and constipation
| Variables | Model 1 | Mode 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | OR (95%CI) | P | |
| HEI score | 0.98 (0.98–0.99) | < 0.001 | 0.98 (0.98–0.99) | < 0.001 | 0.98 (0.98–0.99) | < 0.001 |
Abbreviation: OR, odds ratio; CI, confidence interval; HEI, healthy eating index
Model 1, unadjusted model;
Model 2, adjusted for age and gender;
Model 3, adjusted for age, gender, race, education level, marital status, family income, BMI, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, total energy intake, dietary supplements, and calcium supplement
Further, we explored the association between components of HEI-2015 and constipation. Results showed that higher intake of total fruits (OR: 0.96, 95%CI: 0.93–0.99), whole fruits (OR: 0.96, 95%CI: 0.92–0.99), total vegetables (OR: 0.89, 95%CI: 0.85–0.93), greens and beans (OR: 0.96, 95%CI: 0.92–0.99), whole grains (OR: 0.96, 95%CI: 0.93–0.99), total protein foods (OR: 0.90, 95%CI: 0.85–0.97), seafood and plant proteins (OR: 0.96, 95%CI: 0.93–0.99), higher fatty acids ratio (OR: 0.97, 95%CI: 0.95–0.99) decreased the odds of constipation, while higher intake of sodium (OR: 1.02, 95%CI: 1.01–1.04) increased the odds in fully adjusted model (Table 3).
Table 3.
Association between components of HEI-2015 and constipation
| Variables | Model 1 | Mode 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | OR (95%CI) | P | |
| Total fruits | 0.97 (0.94-1.00) | 0.063 | 0.95 (0.92–0.98) | 0.003 | 0.96 (0.93–0.99) | 0.042 |
| Whole fruits | 0.96 (0.93–0.99) | 0.012 | 0.94 (0.91–0.97) | < 0.001 | 0.96 (0.92–0.99) | 0.022 |
| Total vegetables | 0.89 (0.86–0.93) | < 0.001 | 0.86 (0.83–0.90) | < 0.001 | 0.89 (0.85–0.93) | < 0.001 |
| Greens and beans | 0.95 (0.91–0.98) | 0.006 | 0.93 (0.90–0.97) | < 0.001 | 0.96 (0.92–0.99) | 0.028 |
| Whole grains | 0.96 (0.93–0.98) | 0.002 | 0.95 (0.92–0.97) | < 0.001 | 0.96 (0.93–0.99) | 0.005 |
| Dairy | 1.00 (0.97–1.02) | 0.690 | 0.98 (0.96–0.99) | 0.045 | 1.03 (0.99–1.06) | 0.108 |
| Total protein foods | 0.85 (0.80–0.91) | < 0.001 | 0.89 (0.83–0.95) | < 0.001 | 0.90 (0.85–0.97) | 0.003 |
| Seafood and plant proteins | 0.94 (0.91–0.96) | < 0.001 | 0.94 (0.91–0.96) | < 0.001 | 0.96 (0.93–0.99) | 0.018 |
| Fatty acids ratio | 0.98 (0.96-1.00) | 0.060 | 0.98 (0.96-1.00) | 0.070 | 0.97 (0.95–0.99) | 0.003 |
| Refined grains | 0.98 (0.96-1.00) | 0.070 | 0.98 (0.96-1.00) | 0.107 | 0.99 (0.96–1.01) | 0.190 |
| Sodium | 1.03 (1.01–1.05) | 0.004 | 1.03 (1.01–1.05) | 0.001 | 1.02 (1.01–1.04) | 0.017 |
| Added sugars | 0.92 (0.91–0.94) | < 0.001 | 0.92 (0.91–0.94) | < 0.001 | 0.98 (0.94–1.02) | 0.247 |
| Saturated fats | 1.01 (0.99–1.03) | 0.447 | 1.01 (0.98–1.03) | 0.540 | 0.97 (0.92–1.02) | 0.211 |
Abbreviation: OR, odds ratio; CI, confidence interval; HEI, healthy eating index
Model 1, unadjusted model;
Model 2, adjusted for age and gender;
Model 3, adjusted for age, gender, race, education level, marital status, family income, BMI, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, total energy intake, dietary supplements, and calcium supplement
In addition, we explored the association between HEI-2015 and constipation according to different definitions of constipation. Based on the stool consistency definition, one score increased in HEI-2015 decreased 1% odds of constipation (OR: 0.99, 95%CI: 0.98–0.99) in fully adjusted model. Based on the stool frequency definition, the similar outcome was found in fully adjusted model, with one score increase of HEI-2015 decreasing 3% odds of constipation (OR: 0.97, 95%CI: 0.97–0.98). The results were shown in Supplementary Table 4.
Association between HEI-2015 score and constipation in different gender and ages
The association between HEI-2015 score and constipation was explored based on gender and ages. After adjusting age, race, education level, marital status, family income, BMI, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, energy intake, dietary supplements, and calcium supplement, we found every 1-point increase in HEI-2015 score was associated with 2% decreased odds of constipation in male (OR: 0.98, 95%CI: 0.97–0.99). The similar result was observed in female, with OR of 0.98 (95%CI: 0.98–0.99). For participants with age ≥ 65 years, HEI-2015 score was significantly associated with the reduced odds of constipation (OR: 0.98, 95% CI: 0.98–0.99). A similar result was observed for participants with age < 65 years, and OR was 0.98 (95% CI: 0.98–0.99). There was no multiplicative interaction between age or gender and HEI-2015 on the odds of constipation (Table 4).
Table 4.
Association between overall dietary quality and constipation in participants with different gender and age
| Variables | Model | ||
|---|---|---|---|
| OR (95%CI) | P | ||
| Gender a | |||
| Male | HEI score | 0.98 (0.97–0.99) | 0.007 |
| Female | HEI score | 0.98 (0.98–0.99) | < 0.001 |
| Gender * HEI score | 0.930 | ||
| Age b | |||
| ≥ 65 years | HEI score | 0.98 (0.98–0.99) | < 0.001 |
| < 65 years | HEI score | 0.98 (0.98–0.99) | < 0.001 |
| Age * HEI score | 0.829 | ||
Abbreviation: OR, odds ratio; CI, confidence interval; HEI, healthy eating index
Model a, adjusted for age, race, education level, marital status, family income, BMI, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, energy intake, dietary supplements, and calcium supplement
Model b, adjusted for gender, race, education level, marital status, family income, BMI, drinking, smoking, vigorous physical activity, moderate physical activity, hypertension, depression, total energy intake, dietary supplements, and calcium supplement
Discussion
In this study, we explored whether overall dietary quality was associated with constipation in adults from NHANES database with a large and nationally representative sample. After adjusting a wide range of potential confounders, we found the negative association between HEI-2015 score and constipation, and this association was not affected by different definitions of constipation. We also found the components of HEI-2015 that is total fruits, whole fruits, total vegetables, greens and beans, whole grains, total protein foods, seafood and plant proteins, fatty acids ratio decreased the odds of constipation, and that is sodium increased the odds. Either in male or female, HEI-2015 score was negatively associated with constipation. Similarly, we found higher adherence to HEI-2015 was associated with lower odds of constipation in participants with age ≥ 65 years and < 65 years.
Constipation has been reported to impair the quality of life, and the estimated prevalence of constipation is approximately 10% worldwide [2, 26]. Dietary adjustment is considered as an effective strategy to alleviate or treat this symptom [8]. It is impossible to distinguish the effect of specific dietary ingredients due to the interaction of nutrients in foods. Understanding overall dietary quality and its association with constipation overcomes the challenge of assessing the individual food or nutrient and considering their interaction effects. Since 1995, HEI has been a dietary index which is developed to assess the dietary quality according to DGA [27]. By the evidence-based recommendations of USDA and Health and Human Services (HHS), HEI is updated every five years [28, 29]. The latest version is HEI-2015, pointing out two essential features in nutrition guidelines, namely, adequacy and moderation for dietary intakes, and the first part is encouraged to intake and the second part is limited to intake [9]. HEI-2015 highlighted the higher intake of fruits, vegetables, whole grains, beans, dairy, seafood and plant proteins, that is consistent with Mediterranean diet [9, 30]. Evidence has shown the significant association between higher Mediterranean diet adherence and decreased constipation syndrome scores [31, 32]. HEI-2015 limits the intake of refined grains, sodium, added sugars, and saturated fats, while Western dietary pattern is characterized by the high intake of these food items [33, 34], and has been reported to less improve constipation [35]. Accordingly, our study found that higher adherence to HEI-2015 was associated with the reduced odds of constipation. The different definitions of constipation may cause some biases, leading to the inconsistent results [25]. In our study, whether the constipation defined by stool consistency or stool frequency, we found the similar association, indicating the robustness of our results.
To further clarify our findings, we explored the association between components of HEI-2015 and constipation. The results showed the negative association between total fruits, whole fruits, total vegetables, greens and beans, whole grains, total protein foods, seafood and plant proteins, fatty acids ratio and constipation, and positive association between sodium and constipation. Yang et al. have supported that higher consumption of fruits and vegetables decreased the prevalence of constipation [3]. This may be explained by that fruits and vegetables were rich in soluble fibers, which had a high affinity for water to soft the stools, thereby helping defecate [36]. Studies have revealed that the consumption of beans could improve the constipation [37, 38]. One potential explaining for this was that oligosaccharides in beans could stimulate the development of bifidobacterium to play a laxative role [39]. Rollet et al. found higher intake of whole grains was associated with a lower constipation score [10]. Whole grains were a rich source of dietary fiber (10–12 g/100 g), which increased fecal bulk and promoted faster time of intestinal/colonic transit [10]. Evidence also indicated the negative association between higher fatty acids ratio (PUFA/SFA) and constipation [10], due to SFA could change gut microbiota composition, potentially resulting in intestinal dysbiosis, while PUFA, such as omega-3 or long-chain PUFAs, could regulate inflammation and immune system, promoting a healthy symbiosis of intestinal bacteria [10, 40]. Also, the negative relationship between plant proteins and constipation was reported by You et al. [41] In addition, sodium was found to be positively associated with the odds of constipation [10]. This may be explained by that higher intake of salt reduced the amount of water in the stool, making it difficult to move along the digestive tract and causing difficulties in defecation [42].
Constipation has been reported to be associated with gender and age [43, 44]. Constipation was common in the elderly, inadequate intake of fiber or fluid and decrease of physical activity may increase the prevalence of constipation in elderly people, with the prevalence ranging from 9 to 60% [44, 45]. In our study, we found the negative association between HEI-2015 and constipation in participants aged < 65 years or ≥ 65 years. These findings suggested that people with age of either < 65 years or ≥ 65 years should increase the adherence of HEI-2015 to prevent constipation. Female gender was also an independent risk factor for constipation, and the prevalence of constipation in females was approximately twice as likely as males [43, 46]. Our study found that higher adherence to HEI-2015 was associated with lower odds of constipation in male and female, indicating the importance of increasing HEI-2015 adherence for both male and female to decrease the odds of constipation.
Our study includes a relatively larger sample size to explore the association between overall dietary quality and constipation. To avoid bias caused by multiple imputation and different definitions of constipation, we performed sensitivity analysis, which increases the robustness of results. Further, we perform subgroup analysis to determine the association in different populations. There are some limitations in our study. First, although we have adjusted the potential confounders affecting the constipation, there are still some confounders that may not be considered due to the limited data in the database. Second, this is a cross-sectional study, which cannot address causality. In the future, a prospective study should be designed to further investigate the association between the overall dietary quality and constipation.
Conclusion
In conclusion, we found that higher adherence to HEI-2015 was associated with the lower odds of constipation. The similar results were found in participants with age of < 65 years or ≥ 65 years and with gender of male or female. Our findings suggested that increasing HEI-2015 adherence to alleviate symptoms of constipation may be one of effective methods. Prior to medical intervention, clinicians should promote and emphasize a balanced diet as first line treatment.
Electronic supplementary material
The online version contains supplementary material available at https://doi. org/10.1186/s12889-022-14360-w.
Acknowledgements
Not applicable.
Abbreviations
- HEI
Healthy eating index
- DGA
Dietary Guidelines for Americans
- NHANES
National Health and Nutrition Examination Survey
- ERB
Ethics Review Board
- BMI
body mass index
Authors’ contributions
QL and JY designed the study. QL wrote the manuscript. YK collected, analyzed and interpreted the data. JY critically reviewed, edited and approved the manuscript. All authors have read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.
Declarations
Ethics approval and consent to participate
The requirement of ethical approval for this study was waived by the Institutional Review Board of Subei People’s Hospital of Jiangsu Province, because the data was accessed from NHANES (a publicly available database). Written informed consent was provided by all participants at the time of the survey. All procedures were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schiller LR. Chronic constipation: new insights, better outcomes? Lancet Gastroenterol Hepatol. 2019;4(11):873–82. doi: 10.1016/S2468-1253(19)30199-2. [DOI] [PubMed] [Google Scholar]
- 2.Sperber AD, Bangdiwala SI, Drossman DA, Ghoshal UC, Simren M, Tack J, et al. Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology. 2021;160(1):99–114. doi: 10.1053/j.gastro.2020.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Yang XJ, Zhang M, Zhu HM, Tang Z, Zhao DD, Li BY, et al. Epidemiological study: Correlation between diet habits and constipation among elderly in Beijing region. World J Gastroenterol. 2016;22(39):8806–11. doi: 10.3748/wjg.v22.i39.8806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng C, Chan AO, Hui WM, Lam SK. Coping strategies, illness perception, anxiety and depression of patients with idiopathic constipation: a population-based study. Aliment Pharmacol Ther. 2003;18(3):319–26. doi: 10.1046/j.1365-2036.2003.01663.x. [DOI] [PubMed] [Google Scholar]
- 5.Leta V, Urso D, Batzu L, Weintraub D, Titova N, Aarsland D, et al. Constipation is Associated with Development of Cognitive Impairment in de novo Parkinson’s Disease: A Longitudinal Analysis of Two International Cohorts. J Parkinsons Dis. 2021;11(3):1209–19. doi: 10.3233/JPD-212570. [DOI] [PubMed] [Google Scholar]
- 6.Kawamura Y, Yamamoto S, Funaki Y, Ohashi W, Yamamoto K, Ozeki T, et al. Internet survey on the actual situation of constipation in the Japanese population under 70 years old: focus on functional constipation and constipation-predominant irritable bowel syndrome. J Gastroenterol. 2020;55(1):27–38. doi: 10.1007/s00535-019-01611-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bharucha AE, Wald A. Chronic Constipation. Mayo Clin Proc. 2019;94(11):2340-57. [DOI] [PMC free article] [PubMed]
- 8.Bharucha AE, Lacy BE. Mechanisms, Evaluation, and Management of Chronic Constipation. Gastroenterology. 2020;158(5):1232–49. doi: 10.1053/j.gastro.2019.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krebs-Smith SM, Pannucci TE, Subar AF, Kirkpatrick SI, Lerman JL, Tooze JA, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118(9):1591–602. doi: 10.1016/j.jand.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rollet M, Bohn T, Vahid F, On Behalf Of The Oriscav Working G Association between Dietary Factors and Constipation in Adults Living in Luxembourg and Taking Part in the ORISCAV-LUX 2 Survey. Nutrients. 2021;14(1):122. doi: 10.3390/nu14010122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guelinckx I, Tavoularis G, König J, Morin C, Gharbi H, Gandy J. Contribution of Water from Food and Fluids to Total Water Intake: Analysis of a French and UK Population Surveys. Nutrients. 2016;8(10):630. doi: 10.3390/nu8100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li L, Huang AP, Wang LQ, Yu XL. Empirically derived dietary patterns and constipation among a middle-aged population from China, 2016–2018. Nutr J. 2019;18(1):88. doi: 10.1186/s12937-019-0512-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Airaksinen V, Ruohomäki A, Hantunen S, Keski-Nisula L, Luojus MK, Pekkanen J, et al. Longitudinal Analyses of Diet Quality and Maternal Depressive Symptoms During Pregnancy: the Kuopio Birth Cohort Study. J Acad Nutr Diet. 2022 doi: 10.1016/j.jand.2022.05.018. [DOI] [PubMed] [Google Scholar]
- 14.Julián-Serrano S, Reedy J, Robien K, Stolzenberg-Solomon R. Adherence to five diet quality indices and pancreatic cancer risk in a large US prospective cohort. Am J Epidemiol. 2022;191(9):1584–600. doi: 10.1093/aje/kwac082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanjeevi N, Freeland-Graves JH. Low diet quality is associated with adverse levels of metabolic health markers and clustering of risk factors in adults with type 2 diabetes. J Hum Nutr Diet. 2022 doi: 10.1111/jhn.13020. [DOI] [PubMed] [Google Scholar]
- 16.Pasdar Y, Hamzeh B, Moradi S, Mohammadi E, Cheshmeh S, Darbandi M, et al. Healthy eating index 2015 and major dietary patterns in relation to incident hypertension; a prospective cohort study. BMC Public Health. 2022;22(1):734. doi: 10.1186/s12889-022-13166-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deng MG, Nie JQ, Li YY, Yu X, Zhang ZJ, Higher HEI-2015 Scores Are Associated with Lower Risk of Sleep Disorder: Results from a Nationally Representative Survey of United States Adults. Nutrients. 2022;14(4):873. doi: 10.3390/nu14040873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu L, Qiao S, Zhuang L, Xu S, Chen L, Lai Q, et al. Choline Intake Correlates with Cognitive Performance among Elder Adults in the United States. Behav Neurol. 2021;2021:2962245. doi: 10.1155/2021/2962245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gress TW, Mansoor K, Rayyan YM, Khthir RA, Tayyem RF, Tzamaloukas AH, et al. Relationship between dietary sodium and sugar intake: A cross-sectional study of the National Health and Nutrition Examination Survey 2001–2016. J Clin Hypertens. 2020;22(9):1694–702. doi: 10.1111/jch.13985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jensen-Otsu E, Austin GL. Antidepressant Use is Associated with Increased Energy Intake and Similar Levels of Physical Activity. Nutrients. 2015;7(11):9662–71. doi: 10.3390/nu7115489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NHANES. https://www.cdc.gov/nchs/nhanes/measuring_guides_dri/measuringguides.htm. Accessed 26 Aug 2022.
- 22.USDA. USDA Agricultural Research Service. https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/DR2TOT_C.htm. Accessed 26 Aug 2022.
- 23.Markland AD, Palsson O, Goode PS, Burgio KL, Busby-Whitehead J, Whitehead WE. Association of low dietary intake of fiber and liquids with constipation: evidence from the National Health and Nutrition Examination Survey. Am J Gastroenterol. 2013;108(5):796–803. doi: 10.1038/ajg.2013.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson PB. Associations between physical activity and constipation in adult Americans: Results from the National Health and Nutrition Examination Survey. Neurogastroenterol Motil. 2020;32(5):e13789. doi: 10.1111/nmo.13789. [DOI] [PubMed] [Google Scholar]
- 25.Li Y, Tong WD, Qian Y. Effect of Physical Activity on the Association Between Dietary Fiber and Constipation: Evidence From the National Health and Nutrition Examination Survey 2005–2010. J Neurogastroenterol Motil. 2021;27(1):97–107. doi: 10.5056/jnm20051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tomita T, Kazumori K, Baba K, Zhao X, Chen Y, Miwa H. Impact of chronic constipation on health-related quality of life and work productivity in Japan. J Gastroenterol Hepatol. 2021;36(6):1529–37. doi: 10.1111/jgh.15295. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95(10):1103–8. doi: 10.1016/S0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- 28.Panizza CE, Shvetsov YB, Harmon BE, Wilkens LR, Le Marchand L, Haiman C, et al. Testing the Predictive Validity of the Healthy Eating Index-2015 in the Multiethnic Cohort: Is the Score Associated with a Reduced Risk of All-Cause and Cause-Specific Mortality? Nutrients. 2018;10(4):452. doi: 10.3390/nu10040452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pasdar Y, Moradi S, Moradinazar M, Hamzeh B, Najafi F. Better muscle strength with healthy eating. Eat Weight Disord. 2021;26(1):367–74. doi: 10.1007/s40519-020-00863-1. [DOI] [PubMed] [Google Scholar]
- 30.Mentella MC, Scaldaferri F, Ricci C, Gasbarrini A, Miggiano GAD. Cancer and Mediterranean Diet: A Review Nutrients. 2019;11(9):2059. doi: 10.3390/nu11092059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rusch C, Beke M, Tucciarone L, Nieves C, Jr, Ukhanova M, Tagliamonte MS, et al. Mediterranean Diet Adherence in People With Parkinson’s Disease Reduces Constipation Symptoms and Changes Fecal Microbiota After a 5-Week Single-Arm Pilot Study. Front Neurol. 2021;12:794640. doi: 10.3389/fneur.2021.794640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Montagnese C, Porciello G, Vitale S, Palumbo E, Crispo A, Grimaldi M, et al. Quality of Life in Women Diagnosed with Breast Cancer after a 12-Month Treatment of Lifestyle Modifications. Nutrients. 2020;13(1):136. doi: 10.3390/nu13010136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dianatinasab M, Wesselius A, Salehi-Abargouei A, Yu EYW, Brinkman M, Fararouei M, et al. Adherence to a Western dietary pattern and risk of bladder cancer: A pooled analysis of 13 cohort studies of the Bladder Cancer Epidemiology and Nutritional Determinants international study. Int J Cancer. 2020;147(12):3394–403. doi: 10.1002/ijc.33173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Strate LL, Keeley BR, Cao Y, Wu K, Giovannucci EL, Chan AT. Western Dietary Pattern Increases, and Prudent Dietary Pattern Decreases, Risk of Incident Diverticulitis in a Prospective Cohort Study. Gastroenterology. 2017;152(5):1023–30. doi: 10.1053/j.gastro.2016.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gigic B, Boeing H, Toth R, Böhm J, Habermann N, Scherer D, et al. Associations Between Dietary Patterns and Longitudinal Quality of Life Changes in Colorectal Cancer Patients: The ColoCare Study. Nutr Cancer. 2018;70(1):51–60. doi: 10.1080/01635581.2018.1397707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gill SK, Rossi M, Bajka B, Whelan K. Dietary fibre in gastrointestinal health and disease. Nat Rev Gastroenterol Hepatol. 2021;18(2):101–16. doi: 10.1038/s41575-020-00375-4. [DOI] [PubMed] [Google Scholar]
- 37.Winham DM, Hutchins AM, Thompson SV, Dougherty MK. Arizona Registered Dietitians Show Gaps in Knowledge of Bean Health Benefits. Nutrients. 2018;10(1):52. doi: 10.3390/nu10010052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Doma KM, Farrell EL, Leith-Bailey ER, Soucier VD, Duncan AM. Older Adults’ Awareness and Knowledge of Beans in Relation to Their Nutrient Content and Role in Chronic Disease Risk. Nutrients. 2019;11(11):2680. doi: 10.3390/nu11112680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ruiz-López MA, Barrientos-Ramírez L, García-López PM, Valdés-Miramontes EH, Zamora-Natera JF, Rodríguez-Macias R, et al. Nutritional and Bioactive Compounds in Mexican Lupin Beans Species: A Mini-Review. Nutrients. 2019;11(8):1785. doi: 10.3390/nu11081785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reichardt F, Chassaing B, Nezami BG, Li G, Tabatabavakili S, Mwangi S, et al. Western diet induces colonic nitrergic myenteric neuropathy and dysmotility in mice via saturated fatty acid- and lipopolysaccharide-induced TLR4 signalling. J Physiol. 2017;595(5):1831–46. doi: 10.1113/JP273269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.You JS, Park JY, Chang KJ. A case-control study on the dietary taurine intake, nutrient status and life stress of functional constipation patients in Korean male college students. J Biomed Sci. 2010;17(Suppl 1(Suppl 1):41. doi: 10.1186/1423-0127-17-S1-S41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Agócs R, Sugár D, Szabó AJ. Is too much salt harmful? Yes. Pediatr Nephrol. 2020;35(9):1777–85. doi: 10.1007/s00467-019-04387-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Werth BL, Christopher SA. Potential risk factors for constipation in the community. World J Gastroenterol. 2021;27(21):2795–817. doi: 10.3748/wjg.v27.i21.2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dore MP, Pes GM, Bibbò S, Tedde P, Bassotti G. Constipation in the elderly from Northern Sardinia is positively associated with depression, malnutrition and female gender. Scand J Gastroenterol. 2018;53(7):797–802. doi: 10.1080/00365521.2018.1473485. [DOI] [PubMed] [Google Scholar]
- 45.Włodarczyk J, Waśniewska A, Fichna J, Dziki A, Dziki Ł, Włodarczyk M. Current Overview on Clinical Management of Chronic Constipation. J Clin Med. 2021;10(8):1738. doi: 10.3390/jcm10081738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tamura A, Tomita T, Oshima T, Toyoshima F, Yamasaki T, Okugawa T, et al. Prevalence and Self-recognition of Chronic Constipation: Results of an Internet Survey. J Neurogastroenterol Motil. 2016;22(4):677–85. doi: 10.5056/jnm15187. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the NHANES database, https://wwwn.cdc.gov/nchs/nhanes/.