Abstract
Background:
Considering the need for developing and examining evidenced-based programs using a brief group format for management of social anxiety disorder (SAD) at the community level, we studied the efficacy of two brief versions of cognitive-behavioral therapy (CBT) programs, brief cognitive-behavioral group therapy (bCBGT), and verbal exposure augmented cognitive behavioral therapy (VE-CBT), on social anxiety among university students.
Methods:
A single-center, randomized, parallel-group design was adopted. We delivered six weekly two-hour group sessions, bCBGT and VE-CBT, to 41 university students diagnosed with SAD. An independent rater assessed participants using the Liebowitz Social Anxiety Scale (LSAS) and Clinical Global Impression scale-Severity (CGI-S) at baseline, postintervention, and two-month follow-up. A patient-rated measure, Social Phobia Inventory (SPIN), was assessed at the same time-points.
Results:
There was a significant improvement in severity of social anxiety from baseline to posttreatment and baseline to two-month follow-up in both groups. However, the treatment effects in bCBGT were statistically superior to VE-CBT at postintervention (SPIN, P = 0.038; LSAS, P = 0.028; CGI-S, P = 0.036) and follow-up (SPIN, P = 0.006; LSAS, P = 0.01; CGI-S, P = 0.04).
Conclusions:
Brief CBT treatments, both bCBGT and VE-CBT, are efficacious for SAD among university students. They have the potential to address barriers associated with SAD management. However, we recommend a longer follow-up and replications in diverse settings.
Clinical trial registration number: CTRI/2019/11/021954
Keywords: Social anxiety disorder, cognitive-behavioral group therapy, brief CBT, randomized controlled trial, university students
Key Messages:
This is the first trial studying the effects of two brief versions of CBT programs in managing SAD among university students. Both bCBGT and VE-CBT are efficient in treating SAD among university students.
Studies have evinced social anxiety disorder (SAD) to be highly prevalent in university students globally, including India,1–3 with the lifetime prevalence ranging from 10% to 33%.
SAD is characterized by fear of negative evaluation at, avoidance of, and distress in social situations. It is associated with a significant and direct negative relationship with academic achievement and an indirect effect on academic achievement through social ties. 4 Students with SAD are at increased risk of depression, 5 suicide, 6 problematic internet use, 7 and detrimental well-being. 8 Students with social anxiety symptoms drink more than others, to be accepted by peers, and are more likely than drinkers without SAD to experience negative consequences. 9
Despite the impairment associated with SAD, a national survey found that approximately three-fourths of SAD patients did not utilize mental health services; such utilization rates were lower than patients diagnosed with other anxiety or mood disorders. 10 Such statistics are unfortunate, especially because effective, evidence-based treatments for SAD are available.11–13 Among these studies, cognitive behavioral therapy (CBT) is the treatment of choice for SAD, with most protocols recommending ≥ 12 sessions.
Studies in the recent past14,15 have endorsed shame, stigma, treatment cost, ability to make time for treatment, and lack of knowledge regarding where to seek treatment as treatment barriers in SAD. Considering these issues of treatment cost, ability to make time for treatment, and the paucity of resources to manage such problems, the length of the current evidence-based practice recommendation of ≥ 12 sessions may not be pragmatic enough to meet these demands.
There is an increasing requirement to find treatments that are accessible and address these barriers. One such approach may be evolving effective brief evidence-based programs, notably for outreach initiatives like treating at the community level, for instance, in a college where SAD is in the early part of a student’s career.
Brief interventions that can be delivered at educational campuses may serve many purposes. They would enhance mental health literacy and attenuate the problems associated with stigma that may be experienced when visiting a mental health facility. 16 Additionally, group-based brief intervention administered on campus would address problems associated with treatment timings and increase cost-effectiveness, leading to better treatment dissemination.17,18 Considering the above needs and paucity of trials that examined brief cognitive-behavioral intervention for SAD, we examined the efficacy of two brief versions of group CBT programs as part of community outreach for SAD among university students.
Material and Method
Participants
A single-center, rater-blind, randomized, parallel-group design was adopted. Participants were 41 undergraduate university students from Raipur, Chhattisgarh, India. We obtained written informed consent from the participants. The inclusion criteria were being adults and meeting the criteria for a diagnosis of SAD as per the Diagnostic and Statistical Manual of Mental Disorders, fifth Edition (DSM-5; Table 1). 19 The exclusion criteria were current severe major depressive episode or substance use and having received treatment of SAD (pharmacotherapy or psychotherapy) in the preceding six months. An independent scholar used the lottery method to randomize the participants to receive either the brief cognitive behavioral group therapy (bCBGT) or verbal exposure augmented CBT (VE-CBT). Twenty participants completed six weeks of bCBGT, out of which 19 were available at the two-month follow-up. In the VE-CBT group, 20 participants were available at the postintervention and follow-up.>
Table 1.
Demographic and Clinical Characteristics of the Samples at the Baseline
| Variables | bCBGT (n = 21) | VE-CBT (n = 20) | t Value/X2 | P |
| Age, mean (SD) | 20.23(0.88) | 20.25 (1.01) | –.04 | .968 |
| Age of onset, mean (SD) | 16.57(1.89) | 16.45 (1.49) | .22 | .826 |
| Duration of SAD, mean (SD) | 3.66 (2.12) | 3.8 (1.69) | –.22 | .83 |
| Severity, mean (SD) | 4.42 (0.68) | 4.35 (0.67) | .37 | .711 |
| Sex female, n (%) |
13 (61.9) | 12 (60) | .02 | .901 |
| Current comorbid disorder Other anxiety disorder, n (%) Major depressive episode, n (%) Dysthymia, n (%) Avoidant personality disorder, n (%) |
4 (19) 5 (23.8) 3 (14.28) 5 (23.8) |
3 (15) 4 (20) 2 (10) 6 (30) |
Procedure
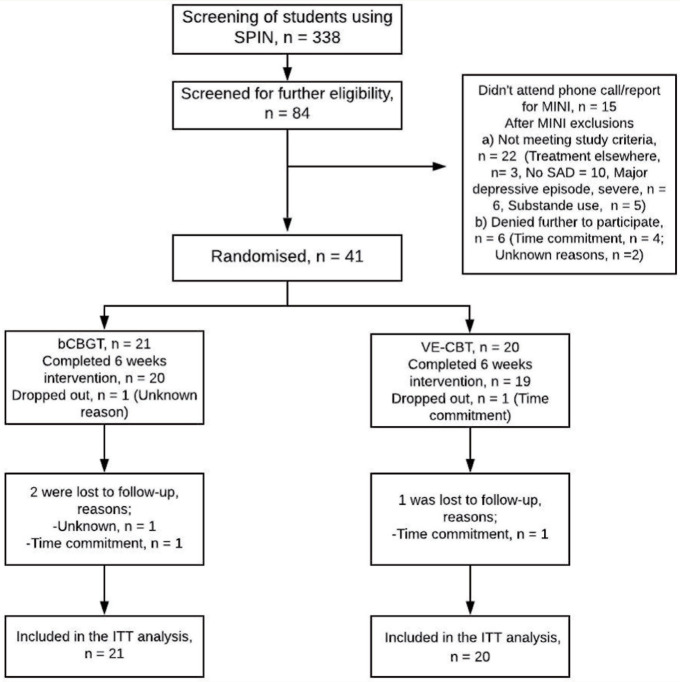
Of 338 university students assessed, 84 scored ≥ 19 on the Social Phobia Inventory (SPIN), considered validated clinical cut-off scores. 20 Twenty individuals did not respond to phone calls for interviews using Mini International Neuropsychiatry Interview (MINI). 21 The first author used the clinical expertise to diagnose dysthymia as a comorbid condition following DSM-5 criteria. A total of 22 participants did not fulfill study criteria and hence were not recruited. Here, we used the Beck Depression Inventory-II, a 21-item self-rated measure, 22 to rate the severity of depression, following which, of 22 participants, 6 were ruled out for their severe level. Later, six participants meeting the study criteria declined to participate further because of time commitment and unknown reasons. The process of data collection continued from January 2020 to March 2020. We randomized the remaining 41 participants to bCBGT or VE-CBT in groups consisting of 10 to 11 participants (Figure 1). Subsequently, to assess for the presence of avoidant personality disorder, we used international personality disorder examination, 23 a 99-item semi-structured clinical interview for personality disorders, on the final 41 participants only.
Figure 1. Participants Flowchart Throughout the Trial .
After the Institute Ethics Committee’s approval, we registered at the Indian Council for Medical Research (ICMR; CTRI/2019/11/021954) trial registry. An independent rater assessed the clinician outcome measures at the baseline, posttreatment, and two-month follow-up.
Interventions
bCBGT
A registered clinical psychologist (PS) with seven years of experience in CBT administered six weekly bCBGT sessions, each of two hours, in the two groups. The bCBGT intervention was adapted from Heimberg and Becker’s 24 group protocol and is typically administered over 12 weeks. We used the abbreviated format, based on our previous study in a similar sample of undergraduates with SAD. 25 Bjornsson et al. 26 and Herbert’s et al. 27 have reported evaluating abbreviated versions of Heimberg and Becker’s treatment.
In the first session, we communicated the rationale of treatment to conceptualize the maintaining factors of SAD, including discussion on the role of avoidance and safety behaviors in exacerbating the held feared consequences and anxiety symptoms. Using metaphor-based conceptualization, 28 we encouraged participants to reflect that systematic exposures to feared social situations without safety behaviors can help overcome SAD. Then we introduced the cognitive restructuring (CR) method followed by assignment of homework sessions.
In the second session, we reviewed the given homework assignments and introduced in-vivo exposures during sessions. For all the assigned exposures, we asked participants to keep a record consisting of:
Feared consequences before carrying out the exposure tasks.
Description of the exposure task.
Finally, what one learned, during and after the exposure, concerning the preheld feared consequences.
We did not focus much on identifying other SAD distortions; instead, for the daily exposure tasks, we emphasized making observable behavioral goals and testing the direct feared consequences. In this line, we, further, assigned tailor-made homework tasks consisting of exposure and other CR.
In the remaining sessions, we conducted graded exposure, cognitive processing of experiences learned from it, and practicing CR and assigned tailor-made home-tasks for both exposure and CR.
VE-CBT
VE-CBT is a variant of CBT based on the protocol by Kumar,29,30 which he also termed as cognitive-drill therapy. PS administered VE-CBT for six weekly two-hour sessions in two groups. Studies have shown its efficacy in anxiety disorders, including SAD. 31 In the first session, we shared the conceptualization of the treatment. Then the participants were required to repeat their feared consequences verbally, persistently till habituation took place. The statement that is repeated consists of anticipated apprehensions into words that are occurring or have already occurred; for instance, “others are laughing at me,” “I have lost respect,” “I am proven as village-idiot,” until there is a significant drop in the anxiety response. Such steps were carried out for all sessions.
On every homework assignment, we encouraged the participants to practice such verbal exposure and told them that if needed, they can write such statements on a sheet of paper or listen to their own recorded account in audio. We suggested them to maintain a diary to document their daily practices. At the beginning of the second to the sixth sessions, we reviewed the home tasks given. Further, we assigned in vivo exposures.
Difference Between the Two Treatment Conditions: Only in the VE-CBT group there was verbal exposure during sessions and in homework. No specific CR techniques were assigned in the VE-CBT group.
Outcome Measures
The SPIN 20 is a patient-reported measure consisting of 17 items. It rates social anxiety on a 5-point scale and the score ranges from 0 to 68. Its psychometric properties are well-reported. 32
The Liebowitz Social Anxiety Scale (LSAS) 33 is a clinician-rated measure assessing fear and avoidance in 24 social situations using a 4-point Likert scale. It is widely used for its excellent psychometric properties. 34 SPIN and LSAS were the primary outcome measures.
The CGI 35 is a commonly used measure to assess the overall severity and improvement in SAD. 36 Here, a blind rater scored it using its 7-point scale. On the Clinical Global Impression-Improvement scale (CGI-I), rating of only one or two suggests clinically significant improvement; hence, such patients are considered responders. Those with a rating of ≥ 3 are considered as nonresponders.
Treatment Adherence Measure
Revised Cognitive Therapy Scale (CTS-R) 37 was used to rate therapist competence and protocol adherence. It consists of 12 items ordered on a scale ranging from 0 to 6. A mean score of 3 and ≥ 4 indicates satisfactory and good-to-excellent competency, respectively.
Data Analysis
Intent-to-treat analysis was implemented. Last observation carried forward was used to replace the missing data. 38 Baseline data were analyzed using chi-square tests and independent-sample t-tests. We used linear mixed model analyses of variance (ANOVAs) to analyze the interaction between the intervention and time and differences in the magnitude of symptom change across the two groups. For within-group analyses, we calculated paired-sample t-tests for each treatment group. For between-group analyses, independent-sample t-tests were calculated. Statistical significance was considered at P < .05. Cohen’s d formula 39 was used to calculate the effect size for pre to postintervention and preintervention to follow-up for both treatments. SPSS version 20.0 was used for the analyses.
Result
Baseline Profile
Table 1 shows the background variables and clinical conditions of the participants. The two treatment groups were similar at the baseline in the distribution of age, sex, onset, duration, and SAD severity. Also, no significant differences were noticed between the two treatment groups in their LSAS and SPIN baseline scores (Table 2).
Table 2.
Means, Standard Deviations, and t-test Results for the SPIN, LSAS, and CGI-S of Both the Treatment Groups
| bCBGT | VE-CBT | Between Group t Value (P Value) df = 39 | Within Group t Value (P value) | ||||||
| df = 20 | df = 19 | ||||||||
| Pre M (SD) | Post M (SD) | FU M (SD) | Pre M (SD) | Post M (SD) | FU M (SD) | a) Pre b) Post c) FU |
CBT a) Pre-post b) Pre-FU c) Post-FU |
VER a) Pre-post b) Pre-FU c) Post-FU |
|
| SPIN | 38.52 (6.58) |
25.952 (7.02) |
24.71 (6.86) |
39.2 (8.27) |
31.6 (9.71) |
32.3 (9.57) |
a) t = –0.29 (0.773) b) t = –2.14 (0.038) c) t = –2.93 (0.006) |
a) t = 7.5 (<0.0005) b) t = 9.22 (<0.0005) c) t = 3.1 (0.006) |
a) t = 4.09 (0.001) b) t = 3.66 (0.002) c) t = –1.22 (0.238) |
| LSAS | 74.86 (11.37) |
49.19 (15.88) |
48 (13.98) |
75.05 (11.72) |
60.45 (15.75) |
61.5 (17.61) |
a) t = –0.053 (0.958) b) t = –2.28 (0.028) c) t = –2.73 (0.01) |
a) t = 7.5 (<0.0005) b) t = 8.67 (<0.0005) c) t = 2.64 (0.016) |
a) t = 3.66 (0.002) b) t = 2.98 (0.008) c) t = –0.77(0.452) |
| CGI-S | 4.43 (0.68) |
3.05 (0.8) |
3 (0.95) |
4.35 (0.67) |
3.6 (0.82) |
3.55 (0.68) |
a) t = 0.37 (0.711) b) t = –2.18 (0.036) c) t = –2.12 (0.041) |
a) t = 5.9 (<0.0005) b) t = 5.84 (<0.0005) c) t = 2.6 (0.017) |
a) t = 4.26 (<0.0005) b) t = 4.29 (<0.0005) c) t = –0.25 (0.804) |
bCBGT: brief cognitive behavioral group therapy, VE-CBT: verbal exposure augmented cognitive behavioral therapy, M: mean, SD: standard deviation, FU: follow-up, SPIN: Social Phobia Inventory, LSAS: Liebowitz Social Anxiety Scale, CGI-S: Clinical Global Impression scale-Severity.
Treatment Adherence
An independent observer, a therapist with over 15 years of psychotherapy training, was present for all the treatment sessions. She was introduced as a co-therapist to the participants but did not participate in the therapeutic sessions. All sessions were rated by the independent observer on the adherence measure CTS-R. The mean (SD) score was 4.41 (0.1) for CBT and 4.29 (0.08) for VE, indicating good-to-excellent therapist competence and adherence. There was no significant difference in therapy adherence in the treatment groups: t (10) = 2.2, P = 0.052.
Treatment Outcome
We used linear mixed model ANOVAs to analyze the interaction between the intervention and time and differences in the magnitude of symptom change across the two groups from pre to posttreatment and follow-up. Mauchly’s test of sphericity indicated that the assumption of sphericity was violated for the two-way interaction; hence, we used the Greenhouse–Geisser correction.
There was a statistically significant interaction between intervention and time on the self-report outcome measure SPIN, F (1.29, 50.41) = 5.8, P = 0.013, and similarly on the clinician-rated measure LSAS, F (1.28, 49.92) = 4.88, P = 0.024. There was a statistically significant interaction between the intervention and time on CGI-S, F (1.7, 66.52) = 3.48, P = o.043.
Within-group analyses using paired sample t tests indicated that both intervention groups improved significantly across time periods from pre-to-post and pre-to-follow-up in all measures (Table 2). In the bCBGT group, the results were: on SPIN (t (20) = 7.49, P < 0.0005 and t (20) = 9.22, P < 0.0005), LSAS (t (20) = 7.5, P < 0.0005 and t (20) = 8.67, P < 0.0005), and CGI-S (t (20) = 5.9, P < 0.0005 and t (20) = 5.84, P < 0.0005). In the VE-CBT group, similar significant improvements were noticed from pre-to-post and preintervention-to-follow-up periods in SPIN (t (19) = 4.09, P = 0.001 and t (19) = 3.66, P = 0.002), LSAS (t (19) = 3.66, P = 0.002 and t (19) = 2.98, P = 0.008), and CGI-S (t (19) = 4.26, P < 0.0005 and t (19) = 4.29, P < 0.0005).
Cohen’s d formula 39 was used to calculate the within-effect size for baseline-to-postintervention and baseline-to-follow-up for both treatments using the threefold classification of effect sizes. In both the treatment groups (Table 3), a large effect size was observed in pre-post-treatment on SPIN and LSAS. In pre-follow-up, a large effect size was observed in both groups on LSAS, while a large effect size was observed on SPIN in the bCBGT group only.
Table 3.
Effect Sizes (Cohen’s d) at Different Periods of Both Treatment Groups
| Assessment | bCBGT | VE-CBT |
| SPIN Posttreatment Two-month follow-up |
1.84 | 0.84 |
| 2.05 | 0.77 | |
| LSAS Posttreatment Two-month follow-up |
1.85 | 1.05 |
| 2.1 | 0.9 |
bCBGT: Brief cognitive behavioral group therapy, VE-CBT: Verbal exposure augmented cognitive behavioral therapy, SPIN: Social Phobia Inventory, LSAS: Liebowitz Social Anxiety Scale.
Between-group analyses, using independent sample t tests, evinced statistically significant treatment difference between the two intervention groups on all outcome measures, SPIN, LSAS, and CGI-S, at postintervention; t (39) = –0.2.143, P = 0.038; t (39) = –2.28, P = 0.028; t (39) = –2.18, P = 0.036. Similarly, at the follow-up, on the same measures, a significant treatment difference was observed; t (39) = –2.93, P = 0.006; t (39) = –2.73, P = 0.01; and t (39) = 2.19, P = 0.04.
Responders and Nonresponders
In the bCBGT and VE-CBT groups, 20 participants completed all six sessions of treatment. At posttreatment time point and follow-up, 60% (n = 12) participants in the bCBGT met clinical responders criteria, while in VE-CBT, 50% at the post and 40% at the follow-up were responders.
Discussion
This study demonstrates evidence of both brief CBTs, bCBGT and VE-CBT, being efficacious treatments for SAD among undergraduate university students. Participants in both treatment groups improved significantly on all measures of social anxiety at postintervention and follow-up. However, at postintervention and follow-up, bCBGT treatment effects were significantly greater than those seen in VE-CBT. Following completion of treatment, at posttreatment assessment, large effect size was observed on the outcome measures in both treatment groups.
These findings of bCBGT efficacy are consistent with other studies,25,27 with a few notable differences. In Samantaray et al.’s 25 study on medical college undergraduate students, only the bCBGT group demonstrated significant improvement at the postintervention and follow-up. That study also showed a significant treatment difference compared to the placebo condition at the posttreatment and follow-up. In comparison, this study found both treatment groups to have significant treatment differences in the post and follow-up periods from their respective pretreatment stage. This study found bCBGT to be an effective treatment without social skill training, unlike in the Herbert et al. study.
In Bjornsson’s study, 26 an abbreviated CBGT was not superior to the other treatment. One reason for such a difference might be that we used an active control condition, a variant of CBT that has additional verbal exposures. In contrast, they used only a group placebo therapy to control nonspecific factors related to group treatment.
There has been no trial on such VE-CBT in SAD to the best of our knowledge, barring a case study. 31 However, as we had previously stated, VE-CBT is a form of CBT augmented by verbal exposures. The results of this feasibility trial of VE-CBT are thus encouraging with reference in particular to its application in such a population.
A comparison of our findings with studies using ≥ 12 sessions for SAD management in community40,41 or clinic settings42,43 revealed similar treatment results in both postintervention and follow-up stages. However, these studies’ follow-up duration varied from six to 12 months, compared to two months in this study. Nevertheless, considering the similar treatment significance found in these and this study, we can affirm that brief CBT formats consisting of fewer sessions addressed in university population can be effective treatments for SAD at the community level. These can be a pragmatic solution to the barriers associated with SAD management such as treatment cost, timings for treatment, 15 and the paucity of trained professionals 44 and may further increase treatment dissemination.
However, there are certain limitations in this study, which might be addressed in further research. The purpose of the present was to study the efficacy of two brief CBT protocols at the community level and not per se superiority of one intervention over another. However, considering that VE-CBT is a relatively new form of treatment, either noninferiority or an equivalence trial design would be a better form to test its efficacy. A direct comparison of the present six-week protocol to another group exposed to standard 12-week CBGT protocol in the same study is essential to establish the efficacy of brief versions of CBT. Replication with a larger sample size and a longer follow-up, like 6–12 months, is recommended to assess the maintenance of treatment gains of bCBGT. Measures of quality of life, well-being, and other cognitive assessments related to treatment effects can inform the effectiveness of such brief versions in a multidimensional way, which is essential for choosing treatment. The current protocol needs to be tested in a clinical setting to study the protocol’s applicability to a broader SAD population.
Conclusions
Brief CBT protocols, both bCBGT and VE-CBT, are efficacious treatments for managing SAD among university students. These have the potential to address the barriers associated with SAD management. However, we recommend a longer follow-up and replications in diverse settings to study its efficacy in a broader SAD population.
Acknowledgments
The authors thank immensely Dr Paulomi Sudhir, NIMHANS, for her review of the manuscript. The authors thank Dr Rakesh Kumar Jain, for his academic and clinical inputs for understanding the concepts behind verbal exposure. The authors enormously thank Dr Priyambada Shrivastava, HOD of Department of Psychology, and other faculties of Pt. Ravishankar Shukla University, for their assistance and cooperation on the project. The authors thank students of Pt. Ravishankar Shukla University, Raipur, India, for their cooperation on this project.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Jaiswal A, Manchanda S, Gautam V, et al. Burden of internet addiction, social anxiety and social phobia among university students. J Fam Med Prim Care, 2020. July; 9(7): 3607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reta Y, Ayalew M, Yeneabat T, et al. Social anxiety disorder among undergraduate students of Hawassa University, College of Medicine and Health Sciences. Neuropsychiatr Dis Treat, 2020; 16: 571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Russell G and Shaw S. A study to investigate the prevalence of social anxiety in a sample of higher education students in the United Kingdom. J Ment Health, 2009. January 1; 18(3): 198–206. [Google Scholar]
- 4.Brook CA and Willoughby T. The social ties that bind: Social anxiety and academic achievement across the university years. J Youth Adolesc, 2015. May 1; 44(5): 1139–1152. [DOI] [PubMed] [Google Scholar]
- 5.Kraft JD, Grant DM, White EJ, et al. Cognitive mechanisms influence the relationship between social anxiety and depression among college students. J Am Coll Health, 2019. September 11 1–7. [DOI] [PubMed] [Google Scholar]
- 6.Davidson CL, Wingate LR, Grant DM, et al. Interpersonal suicide risk and ideation: The influence of depression and social anxiety. J Soc Clin Psychol, 2011. October; 30(8): 842–855. [Google Scholar]
- 7.Weinstein A, Dorani D, Elhadif R, et al. Internet addiction is associated with social anxiety in young adults. Ann Clin Psychiatry, 2015. Feburary 1; 27(1): 4–9. [PubMed] [Google Scholar]
- 8.Russell G and Topham P. The impact of social anxiety on student learning and well-being in higher education. J Ment Health, 2012. August 1; 21(4): 375–385. [DOI] [PubMed] [Google Scholar]
- 9.Villarosa MC, Madson MB, Zeigler-Hill V, et al. Social anxiety symptoms and drinking behaviors among college students: The mediating effects of drinking motives. Psychol Addict Behav, 2014. September; 28(3): 710. [DOI] [PubMed] [Google Scholar]
- 10.Wang PS, Lane M, Olfson M, et al. Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Arch Gen Psychiatry, 2005. June 1; 62(6): 629–640. [DOI] [PubMed] [Google Scholar]
- 11.Curtiss J, Andrews L, Davis M, et al. A meta-analysis of pharmacotherapy for social anxiety disorder: An examination of efficacy, moderators, and mediators. Expert Opin Pharmacother, 2017. February 11; 18(3): 243–251. [DOI] [PubMed] [Google Scholar]
- 12.Mayo-Wilson E, Dias S, Mavranezouli I, et al. Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. Lancet Psychiatry, 2014. October 1; 1(5): 368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wersebe H, Sijbrandij M, and Cuijpers P. Psychological group-treatments of social anxiety disorder: A meta-analysis. PloS one, 2013. November 15; 8(11): e79034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goetter EM, Frumkin MR, Palitz SA, et al. Barriers to mental health treatment among individuals with social anxiety disorder and generalized anxiety disorder. Psychol Serv, 2020. Feburary; 17(1): 5. [DOI] [PubMed] [Google Scholar]
- 15.Olfson M, Guardino M, Struening E, et al. Barriers to the treatment of social anxiety. Am J Psychiatry, 2000. April 1; 157(4): 521–527. [DOI] [PubMed] [Google Scholar]
- 16.Wang J and Lai D. The relationship between mental health literacy, personal contacts and personal stigma against depression. J Affect Disord, 2008. September 1; 110 (1–2): 191–196. [DOI] [PubMed] [Google Scholar]
- 17.Jorm AF. Mental health literacy: Empowering the community to take action for better mental health. Am Psychol, 2012. April; 67(3): 231. [DOI] [PubMed] [Google Scholar]
- 18.CBT BP. Brief cognitive-behavioral therapy: Definition and scientific foundations. Handbook of Brief Cognitive Behaviour Therapy, 2002: 1. [Google Scholar]
- 19.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®), 5th ed. American Psychiatric Pub, 2013. May 22. CBS. [Google Scholar]
- 20.Connor KM, Davidson JR, Churchill LE, et al. Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. Br J Psychiatry, 2000. April; 176(4): 379–386. [DOI] [PubMed] [Google Scholar]
- 21.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry, 1998; 59 (Suppl 20): 22–33. [PubMed] [Google Scholar]
- 22.Beck AT, Steer RA, and Brown GK. Manual for the beck depression inventory-II. Psychol Corporation, 1996; 1: 82. [Google Scholar]
- 23.Loranger AW, Sartorius N, Andreoli A, et al. The international personality disorder examination: The World Health Organization/alcohol, drug abuse, and mental health administration international pilot study of personality disorders. Arch Gen Psychiatry, 1994. March 1; 51(3): 215–224. [DOI] [PubMed] [Google Scholar]
- 24.Heimberg RG and Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. Guilford Press, 2002. July 3. [Google Scholar]
- 25.Samantaray NN, Nath B, Behera N, et al. Brief cognitive behavior group therapy for social anxiety among medical students: A randomized placebo-controlled trial. Asian J Psychiatry, 2020. December 15; 55: 102526. [DOI] [PubMed] [Google Scholar]
- 26.Bjornsson AS, Bidwell LC, Brosse AL, et al. Cognitive–behavioral group therapy versus group psychotherapy for social anxiety disorder among college students: A randomized controlled trial. Depress Anxiety, 2011. November; 28(11): 1034–1042. [DOI] [PubMed] [Google Scholar]
- 27.Herbert JD, Rheingold AA, and Goldstein SG. Brief cognitive behavioral group therapy for social anxiety disorder. Cogn Behav Pract, 2002. December 1; 9(1): 1–8. [Google Scholar]
- 28.Samantaray NN, Kar N, and Singh P. Four-session cognitive behavioral therapy for the management of obsessive–compulsive disorder using a metaphor for conceptualization: A case report. Indian J Psychiatry, 2019; 61(4): 424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kumar R. Verbal exposure for irrational fears: New directions in research and applications. Clin Exp Psychol, 2017; 3: 157. [Google Scholar]
- 30.Kumar R. Experiences in verbal exposure for stimulus bound anxiety. Indian J Clin Psychol, 2017; 44(1): 14–20. [Google Scholar]
- 31.Arya B, Verma S, and Kumar R. Cognitive drill therapy: A case study of social anxiety disorder. Indian J Clin Psychol, 2019; 46(1): 81–84. [Google Scholar]
- 32.Antony MM, Coons MJ, McCabe RE, et al. Psychometric properties of the social phobia inventory: Further evaluation. Behav Res Ther, 2006. August 1; 44(8): 1177–1185. [DOI] [PubMed] [Google Scholar]
- 33.Liebowitz MR. Social Phobia. Mod Probl Pharmacopsychiatry, 1987; 22 141–173. [DOI] [PubMed] [Google Scholar]
- 34.Fresco DM, Coles ME, and Heimberg RG. The liebowitz social anxiety scale: A comparison of the psychometric properties of self-report and clinician-administered formats. Psychol Med, 2001. August 1; 31(6): 1025–1035. [DOI] [PubMed] [Google Scholar]
- 35.Guy W. ECDEU assessment manual for psychopharmacology. US Department of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs, 1976. [Google Scholar]
- 36.Zaider TI, Heimberg RG, Fresco DM, et al. Evaluation of the clinical global impression scale among individuals with social anxiety disorder. Psychol Med, 2003. May 1; 33(4): 611. [DOI] [PubMed] [Google Scholar]
- 37.Blackburn IM, James IA, Milne DL, et al. The revised cognitive therapy scale (CTS-R): Psychometric properties. Behav Cogn Psychother, 2001. October 1; 29(4): 431. [Google Scholar]
- 38.Enders CK. Applied missing data analysis. Guilford press, 2010. April 23. [Google Scholar]
- 39.Cohen J. Methods in psychology: a power primer. Psychol Bull, 1992; 112(1): 155–159. [DOI] [PubMed] [Google Scholar]
- 40.McCarthy O, Hevey D, Brogan A, et al. Effectiveness of a cognitive behavioural group therapy (CBGT) for social anxiety disorder: Immediate and long-term benefits. Cogn Behav Therapist, 2013; 6. doi: 10.1017/S1754470X13000111 [DOI] [PubMed] [Google Scholar]
- 41.McEvoy PM, Nathan P, Rapee RM, et al. Cognitive behavioural group therapy for social phobia: Evidence of transportability to community clinics. Behav Res Ther, 2012. April 1; 50(4): 258–265. [DOI] [PubMed] [Google Scholar]
- 42.Aderka IM, Hermesh H, Marom S, et al. Cognitive behavior therapy for social phobia in large groups. Int J Cogn Ther, 2011. March; 4(1): 92–103. [Google Scholar]
- 43.Hedman E, Andersson G, Ljótsson B, et al. Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: A randomized controlled non-inferiority trial. PloS one, 2011. March 25; 6(3): e18001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goodman L. Mental health on university campuses and the needs of students they seek to serve. Build Healthy Acad Communities J, 2017. November 27; 1(2): 31–44. [Google Scholar]