Abstract
Background:
Diagnosis of duodenal perforation (DP) in children is often delayed. This worsens the clinical condition and complicates simple closure.
Objectives:
To explore the advantages of using T-tube in surgeries for DP in children.
Patients and Methods:
A retrospective study was conducted on all patients of DP managed in the Department of Paediatric surgery at a tertiary centre from January 2016 to December 2020. Clinical, operative and post-operative data were collected. Patients, with closure over a T-tube to ensure tension-free healing, were critically analysed.
Results:
A total of nine DP patients with ages ranging from 2 years to 9 years were managed. Five (55.6%) patients had blunt abdominal trauma; a 2-year-old male had perforation following accidental ingestion of lollypop-stick while a 3-year-old male had DP during endoscopic evaluation (iatrogenic) of bleeding duodenal ulcers; cause could not be found in other 2 (22.2%) patients. Of the five patients with blunt abdominal trauma, 4 (80%) had large perforation with oedematous bowel, necessitating repair over T-tube. Both patients with unknown causes had uneventful outcomes following primary repair with Graham's patch. Patients with lollypop-stick ingestion and iatrogenic perforation did well with repair over T-tube. The only trauma patient with primary repair leaked but subsequently had successful repair over a T-tube. One patient with complete transection of the third part of the duodenum and pancreatic injury who had repair over T-tube died due to secondary haemorrhage on the 10th post-operative day.
Conclusion:
Closure over a T-tube in DP, presenting late with oedematous bowel, ensures low pressure at the perforation site, forms a controlled fistula and promotes healing, thereby lessening post-operative complications.
Keywords: Duodenum, pediatric, perforation, T-tube
INTRODUCTION
Paediatric duodenal perforation (DP) is less commonly encountered when compared to DP occurring in adults and the elderly.[1] While most DP in adults is secondary to the perforation of a peptic ulcer, peptic ulcers are not common in children.[1,2,3] Several series reported trauma to be the most important aetiology of a Paediatric DP in ambulatory children.[4,5] Traumatic DP differs from other causes of DP in that it may affect any site of the bowel, may be multiple in number and of larger size with unhealthy margins and may have associated injuries,[6] which may complicate the natural course and prolong the hospital stay of the child. Due to these characteristics and delayed presentation, simple suture closure with Graham's patch cover usually[7] does not suffice and there are high chances of leaks.[8] Several techniques have been described in the literature to overcome the high chances of the leak in such individuals including tube duodenostomy[9] and pyloric exclusion with procedures like gastro-enterostomy.[10,11] Experience with these techniques is limited in children. T-tubes have been used for tension-free healing of the repair site after retrieval of the stones in the common bile duct (CBD). They ensure biliary drainage away from the liver at low pressures converting it to a controlled fistula initially. This promotes healing without risks of stricture in the CBD. The same principle can be applied to cases of DP which are large sized, located at atypical locations and have unhealthy surrounding margins.
This retrospective study summarises the findings of managing DP in children at a tertiary care centre with special emphasis on the subset of patients who had had repair over a T-Ttube.
PATIENTS AND METHODS
A retrospective study was conducted in the Department of Pediatric Surgery at a tertiary care centre on all patients of DP managed from January 2016 to December 2020. After clearance from the institutional ethics committee (letter no. 1530/IEC/IGIMS/2020) and consent from the parents of the children included in the study, the clinical records were reviewed to get a detailed history, mechanism of injury (if any), clinical symptoms and examination and investigation findings. Intra-operative findings, details of the surgical procedure, post-operative and follow-up details were also noted. Data thus collected were tabulated and analysed.
Protocol for managing a patient with suspected duodenal perforation
Patients with suspected DP were resuscitated as any other patient of acute abdomen and emergency blood samples were sent. Abdominal assessment of trauma patients, who were stable, was done by X-ray, sonogram and if needed computed tomography scan of the abdomen and pelvis. Patients evaluated in this way or unstable patients not fit for detailed radiological assessment were counselled on the need for emergency surgery with explanation given about the nature of the surgical pathology and surgery.
Exploratory laparotomy was performed through the right upper supraumbilical transverse incision. After adequate lavage, the site and size of the perforation were noted. Special attention was given to the margins of the perforated bowel and whether some other injuries were present or not. Individual patients were graded based on the Duodenum injury scale given by the American Association of the Surgery of Trauma (AAST).[12] Patients who presented early and had small perforation with relatively healthy and non-friable margins underwent primary closure of the perforation with Graham's patch as done commonly in adult patients with DP. Patients with perforation at atypical sites in the duodenum, multiple perforation, perforation with friable and oedematous margins, late presenters with sepsis and poor nutrition, large perforation involving more than half of the circumference and traumatic perforation underwent repair over a T-tube.
Repair of DP over T-tube is a simple technique, does not involve an anastomosis and is easy to perform. After mobilisation of the right colon and exposure of the lateral and anterior walls of the duodenum (Kocherisation) to provide good visualisation, the extent of the defect was ascertained. A 10Fr to 14Fr of T-tube was chosen as per the age of the child, calibre of his duodenum and size of the perforation. The T-Tube was inserted into the duodenum to decompress the lumen, thereby making the repair a low pressure, tension-free zone. Furthermore, the tube streamlines the flow of the bile away from the liver towards the bowel mimicking normal physiology. This simple technique is of prime importance in cases with edematous and friable bowel with relatively large perforation. If ever a small leak occurs from the margins of the T-tube, it gets drained and gradually the repair heals without any complication. A nasogastric tube takes care of the bile reaching the stomach until post-operative ileus subsides and normal bowel movement appears. Two wide calibre drains were inserted into the peritoneal cavity (one each in the right sub-hepatic and pelvic cavity), following which the abdomen was closed in layers.
In the post-operative period, all the patients were put on nil oral with intravenous fluid, antibiotics and analgesia. Drain output was noted daily with the aim of maintaining the input-output balance. Drains were removed when their output ceased. Patients were started on oral liquids once bowel movement started and were gradually transitioned from semi-solid to solid diet. Sicker patients received partial parenteral nutrition. T-Tube clamping was started when the patient tolerated oral liquids (normally after 1 week of surgery); patients were discharged with a clamped T-tube neatly dressed underneath the dressing and on full feeds. T-tube removal was done after 2 weeks of the discharge as an outdoor procedure. Patients were followed up at monthly intervals for 3 months and if needed thereafter.
RESULTS
A total of nine patients of DP were managed during the study period. The age of these patients ranged from 2 years to 9 years. All were males except one female who presented as a 2-year-old without a known cause for perforation in the first part of the duodenum. All the patients included in the study presented late to the hospital (>3 days) since the symptoms of the acute abdomen were noticed.
All the patients presented with variable symptoms such as abdominal pain, abdominal distension, fever, bilious vomiting and difficulty in breathing in different combinations. One (11.1%) patient with a bleeding ulcer who had an iatrogenic perforation also had a history of hematemesis, melaena and blood transfusion. Three (33.3%) patients did not have any features of pneumoperitoneum on plain abdominal X-ray.
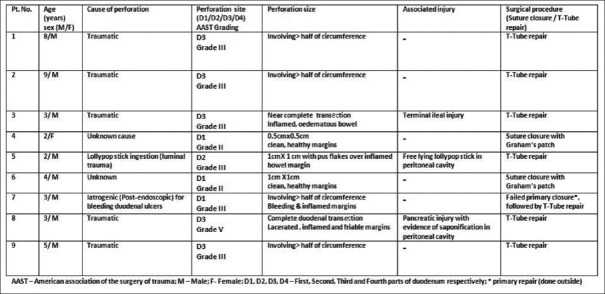
Blunt abdominal trauma was the most common cause and was found in 5 (55.6%) patients; 1 (11.1%) patient each had perforation during endoscopic evaluation for bleeding duodenal ulcer and perforation following ingested lollypop stick. The aetiologies of perforation in 2 (22.2%) children were unknown [Figure 1].
Figure 1.
Summary of the surgical methods used and their outcome in duodenal perforation patients
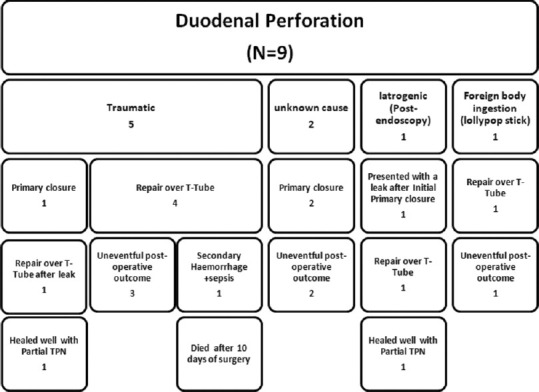
The cases with unknown causes or secondary to duodenal ulcers had relatively smaller perforations in the first part of the duodenum; those with traumatic causes were seen distal to the first part with large size and unhealthy margins. Two traumatic cases had associated injuries in the form of terminal ileal injury and pancreatic injury. Six (66.7%) patients had Grade III injury on the AAST duodenum injury scale. One (11.1%) patient had Grade V injury with complete duodenal transection and pancreatic injury with evidence of saponification in the peritoneal cavity. Patients with smaller perforation and Grade II injury (2, 22.2%) could be successfully managed with primary closure using Graham's patch [Figure 2].
Figure 2.
Characteristics of duodenal perforation and method of repair
Four (44.4%) patients who had a history of blunt abdominal trauma had large perforation (> half the circumference of the bowel) with oedematous and friable margins. These patients were not repaired primarily but underwent repair over T-tube. The only trauma patient who was repaired primarily leaked on the 4th post-operative day and had to be repaired over a T-tube with successful healing [Figure 1].
There were two patients with small DP without any significant bowel oedema and no obvious cause for perforation; both of them did well with simple closure of perforation using Graham's patch. Patient who presented with a leak following primary repair outside for iatrogenic perforation and also one who had perforation due to lollypop stick ingestion healed when repaired over a T-tube [Figure 3].
Figure 3.
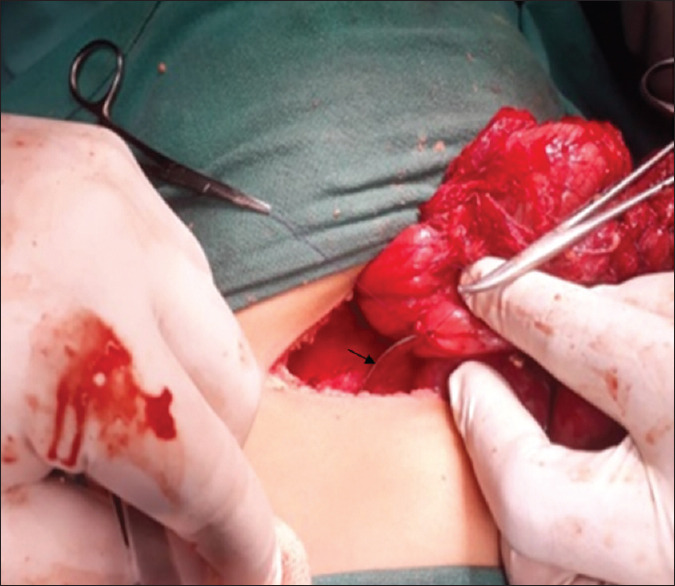
Repair of duodenal perforation over T-tube (black arrow shows the T-tube)
One patient with traumatic DP who had a complete transection of the duodenum also had an associated pancreatic injury [Figure 4]; he developed secondary haemorrhage on the 8th post-operative day and succumbed to it on the 10th post-operative day despite all efforts and multiple transfusions. None of the patients included in this study had a feeding jejunostomy done for enteral nutrition.
Figure 4.
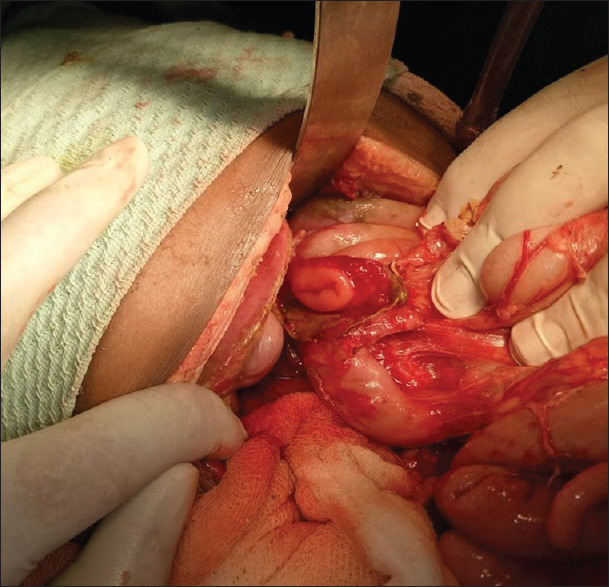
Complete transaction of the duodenum due to blunt abdominal trauma
Partial parenteral nutrition support was given in three patients (two with leak) and one with associated pancreatic injury.
Histopathologic examination of tissue from margins of perforation did not reveal any obvious pathology or atypical findings.
All the patients who survived and did well (8, 88.9%) were discharged when they tolerated a full oral diet. The subgroup of patients who had T-tube repair was sent home with a clamped T-tube neatly covered with a dressing. T-tubes were taken out after 2 weeks of discharge when the patient came for the follow-up to the hospital. None of them required imaging or a dye/contrast study to delineate the patency of the bowel or the position of the T-tube. All the patients (8, 88.9%) had uneventful follow-up.
DISCUSSION
Are DP in children and DP in adults similar in aetiology, clinical features and presentation? While duodenal ulcer perforation, iatrogenic (endoscopic/post-laparoscopic procedure) perforation and post-traumatic perforation are the main causes for DP in adults with the majority of cases still known to be due to perforation of duodenal ulcers,[13,14] the same is not true for paediatric DP. In children, duodenal ulcers are uncommon and so traumatic and iatrogenic causes outnumber other causes. Maudar et al., in an earlier series, reported only eleven cases of paediatric duodenal ulcers for 7 years at their centre, of which three had perforation.[15] This reflects the rarity of ulcers being the cause behind DP in children. Similar observations of other researchers suggest that DP in children differs from DP in adults when it comes to aetiology and epidemiology.[1,16]
Recent literature has emphasised on the role of other factors in Paediatric DP. Trauma,[4,5] child abuse,[17,18] steroid/post-medication therapy,[19] foreign-body ingestion[20,21,22,23] and stress-ulcer perforation and post-endoscopic (iatrogenic)[24,25] causes are some other important causes in children. Often, the cause is not known.
Blunt abdominal trauma is the second-most common cause of death in abused children.[26] Although the mobility of the small intestine is protective, the fixed retroperitoneal course of the duodenum makes it injury-prone between the posterior vertebral column and the impacting force from the anterior side; injury may occur instantaneously, or later secondary to tissue necrosis.[26]
In our study, we could only find nine patients with DP for 5 years. Most of them were due to trauma (blunt abdominal trauma) from outside. The other two important causes were trauma but from the luminal side (post-endoscopic and after lollypop stick ingestion). These observations point towards trauma being an important cause of DP in ambulatory children. Furthermore, with increase in the number of endoscopic procedures in children, iatrogenic DP has increased in frequency.[25,27,28]
Another observation is that the nature and site of perforation in trauma cases are variable and differ from the perforation seen secondary to perforation of duodenal ulcers which are usually small-sized and in the first part of the duodenum. Traumatic DP in children can come with any complexity in position, size and associated injuries.[29] In our study, all traumatic perforations were distal to the first part of the duodenum and were large with edematous and inflamed bowel margins. By contrast, perforation due to unknown cause and that due to bleeding duodenal ulcer after endoscopy was in the first part of duodenum with relatively small size.
Different methods have been described for managing DP.[4] Small-sized DP in the first part of the duodenum does well with simple closure with an omental patch.[7,30,31] On the other hand, large perforations or those that have leaked after primary repair often require diversion of gastric contents, which consists of pyloric exclusion and gastroenterostomy.[8,32] Tube duodenostomy also serves the same purpose of decreasing the pressure of intra-luminal contents at the site of the repair and is technically less demanding and less time-consuming in comparison to gastroenterostomy techniques.[33] Feeding jejunostomy can be secondarily added as an additional technique to ensure unimpeded enteral nutrition in sick children.[34]
The suboptimal outcomes of simple closure in large traumatic perforations (as seen in this study) suggest that a simple suture closure of such perforations is bound to leak and worsen the prognosis of the patient. Any procedure which would lessen the pressure at the repair site and drain bile would help in restoring normal physiology and promote healing at the injury site. This is the rationale behind the use of a T-tube at the site of perforation. Conventionally, closure over T-tube has helped in complication-free safe healing of CBD after stone retrieval in adult patients with choledocholithiasis.[35] The same principle can be used in lessening the tension at the site of DP in sick, septic children with oedematous, friable bowel.
Leak from the primary repair of giant duodenal ulcer is a well-known complication. Several factors responsible for the leak have been described like (a) widely gaped margins of the perforation which are inflamed and necrotic leading to repair under tension, (b) high intra-luminal pressure, (c) autodigestive effects of the bile mixed with the gastric and pancreatic juices, (d) tendency of mucosa to extrude from the anastomotic line and (e) precarious blood supply of the duodenum.[10,36] Considering the fact that most traumatic perforations are large-sized and away from the first part of the duodenum, these risk factors are increasingly associated with them. This makes simple repair vulnerable increasing the morbidity of the patient.[37,38]
In our study, all patients who had repair over T-tube either primarily or secondarily after the leak of a primary repair did well and had a good outcome. Unfortunately, one patient who died of secondary haemorrhage had associated pancreatic injury.
Several adult studies describe the role of tube duodenostomy in complicated and large DP with successful outcomes.[33,39]
Shilyansky et al.[39] and Lal et al.[33] compared the role of tube duodenostomies against primary closure in cases of giant duodenal ulcer perforation and recommended this procedure as a safe and reliable alternative
Kutlu et al. described the successful role of tube duodenostomy in managing three patients with giant duodenal ulcers.[40]
Isik et al. examined the role of tube duodenostomy in different sets of patients with additional insertion of T-tube into the CBD in complex patients of gastric resection with an insecure duodenal stump. None of the patients leaked where tube duodenostomy was used primarily and results were good in patients who were re-operated for leaks.[9] A subset of patients in this study also included those having DP following injury. Our study shows similar encouraging results with T-tube repairs in the pediatric age group.
In an earlier series on 321 duodenal wounds over 30 years on adult patients, Stone and Fabian reported 12% dehiscence rate with simple closure while the leak rate significantly came down with decompression procedures.[14] Futhermore, none of the three patients with associated pancreaticoduodenal injuries could be saved.[14] We had similar results in our small study on children which shows that decompressive procedures using a T-tube helps in complicated DP and that associated pancreatic injury worsens prognosis while making the initial management more complex.
Hua et al. reported female sex and simple closure of DP to be associated with poor outcomes in their large series on perforated peptic ulcer in children.[1]
Delay in diagnosis is often noted in DP patients. Rarity of this condition, vague symptoms and inability to get proper history in children delays operative treatment and therefore increase morbidity and mortality.[30,31] It has been observed that morbidity after duodenal injuries is approximately seen in 20% of cases while the operative delay of more than 24 h is reported to increase the complication rate from 29% to 43%.[41] All our patients presented late.
In summary, trauma is the most important cause for duodenal injury in ambulatory children and it often presents with various complexities of injury. Repair over a T-tube is a simple technique leading to low pressure at the repair site and uncomplicated, event-free post-operative outcome.
CONCLUSION
DP in children although rare, presents with two extremes. While simple suture closure suffices in small perforation with healthy margins, decompressive procedures like repair over a T-tube are indispensable in large perforations and complicated cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hua MC, Kong MS, Lai MW, Luo CC. Perforated peptic ulcer in children: A 20-year experience. J Pediatr Gastroenterol Nutr. 2007;45:71–4. doi: 10.1097/MPG.0b013e31804069cc. [DOI] [PubMed] [Google Scholar]
- 2.Ngom G, Diouf ML, Fall M, Konaté I, Sankalé AA, Diop M, et al. Perforation and haemorrhage duodenal bulbar ulcers in a child: A case report. Dakar Med. 2008;53:28–31. [PubMed] [Google Scholar]
- 3.Lee NM, Yun SW, Chae SA, Yoo BH, Cha SJ, Kwak BK. Perforated duodenal ulcer presenting with massive hematochezia in a 30-month-old child. World J Gastroenterol. 2009;15:4853–5. doi: 10.3748/wjg.15.4853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ladd AP, West KW, Rouse TM, Scherer LR, 3rd, Rescorla FJ, Engum SA, et al. Surgical management of duodenal injuries in children. Surgery. 2002;132:748–52. doi: 10.1067/msy.2002.127673. [DOI] [PubMed] [Google Scholar]
- 5.Childhood injuries in the United States. Division of Injury Control, Center for Environmental Health and Injury Control, Centers for Disease Control. Am J Dis Child. 1990;144:627–46. [PubMed] [Google Scholar]
- 6.Megremis S, Segkos N, Andrianaki A, Gavridakis G, Psillakis K, Triantafyllou L, et al. Sonographic diagnosis and monitoring of an obstructing duodenal hematoma after blunt trauma: Correlation with computed tomographic and surgical findings. J Ultrasound Med. 2004;23:1679–83. doi: 10.7863/jum.2004.23.12.1679. [DOI] [PubMed] [Google Scholar]
- 7.Graham RR. The treatment of perforated duodenal ulcer. Surg Gynecol Obstet. 1937;64:235–8. [Google Scholar]
- 8.Chaudhary A, Bose SM, Gupta NM, Wig JD, Khanna SK. Giant perforations of duodenal ulcer. Indian J Gastroenterol. 1991;10:14–5. [PubMed] [Google Scholar]
- 9.Isik B, Yilmaz S, Kirimlioglu V, Sogutlu G, Yilmaz M, Katz D. A life-saving but inadequately discussed procedure: Tube duodenostomy. Known and unknown aspects. World J Surg. 2007;31:1616–24. doi: 10.1007/s00268-007-9114-3. [DOI] [PubMed] [Google Scholar]
- 10.Gupta S, Kaushik R, Sharma R, Attri A. The management of large perforations of duodenal ulcers. BMC Surg. 2005;5:15. doi: 10.1186/1471-2482-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yadav SK, Gupta V, El Kohly A, Al Fadhli W. Perforated duodenal ulcer: A rare complication of deferasirox in children. Indian J Pharmacol. 2013;45:293–4. doi: 10.4103/0253-7613.111901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Gennarelli TA, et al. Organ injury scaling, II: Pancreas, duodenum, small bowel, colon, and rectum. J Trauma. 1990;30:1427–9. [PubMed] [Google Scholar]
- 13.Ansari D, Torén W, Lindberg S, Pyrhönen HS, Andersson R. Diagnosis and management of duodenal perforations: A narrative review. Scand J Gastroenterol. 2019;54:939–44. doi: 10.1080/00365521.2019.1647456. [DOI] [PubMed] [Google Scholar]
- 14.Stone HH, Fabian TC. Management of duodenal wounds. J Trauma. 1979;19:334–9. doi: 10.1097/00005373-197905000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Maudar KK, Dutta J, Mitra S. Duodenal ulcer disease in chidren. World J Surg. 1980;4:261–6. doi: 10.1007/BF02393598. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan PB. Peptic ulcer disease in children. Paediatr Child Health. 2010;20:462–4. [Google Scholar]
- 17.Bowkett B, Kolbe A. Traumatic duodenal perforations in children: Child abuse a frequent cause. Aust N Z J Surg. 1998;68:380–2. doi: 10.1111/j.1445-2197.1998.tb04779.x. [DOI] [PubMed] [Google Scholar]
- 18.Gaines BA, Shultz BS, Morrison K, Ford HR. Duodenal injuries in children: Beware of child abuse. J Pediatr Surg. 2004;39:600–2. doi: 10.1016/j.jpedsurg.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Yan X, Kuang H, Zhu Z, Wang H, Yang J, Duan X, et al. Gastroduodenal perforation in the pediatric population: A retrospective analysis of 20 cases. Pediatr Surg Int. 2019;35:473–7. doi: 10.1007/s00383-018-4420-4. [DOI] [PubMed] [Google Scholar]
- 20.Pinero Madrona A, Fernández Hernández JA, Carrasco Prats M, Riquelme Riquelme J, Parrila Paricio P. Intestinal perforation by foreign bodies. Eur J Surg. 2000;166:307–9. doi: 10.1080/110241500750009140. [DOI] [PubMed] [Google Scholar]
- 21.Kim MJ, Seo JM, Lee Y, Lee YM, Choe YH. An unusual cause of duodenal perforation due to a lollipop stick. Korean J Pediatr. 2013;56:182–5. doi: 10.3345/kjp.2013.56.4.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehran A, Podkameni D, Rosenthal R, Szomstein S. Gastric perforation secondary to ingestion of a sharp foreign body. JSLS. 2005;9:91–3. [PMC free article] [PubMed] [Google Scholar]
- 23.Stricker T, Kellenberger CJ, Neuhaus TJ, Schwoebel M, Braegger CP. Ingested pins causing perforation. Arch Dis Child. 2001;84:165–6. doi: 10.1136/adc.84.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diniz-Santos DR, de Andrade Cairo RC, Braga H, Araújo-Neto C, Paes IB, Silva LR. Duodenal hematoma following endoscopic duodenal biopsy: A case report and review of the existing literature. Can J Gastroenterol. 2006;20:39–42. doi: 10.1155/2006/391702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trainavicius K, Dagilyte RV. Intramural duodenal hematoma after upper gastrointestinal endoscopic biopsy in children: Two case reports and literature review. Ann Clin Case Rep. 2017;2:1265. [Google Scholar]
- 26.Champion MP, Richards CA, Boddy SA, Ward HC. Duodenal perforation: A diagnostic pitfall in non-accidental injury. Arch Dis Child. 2002;87:432–3. doi: 10.1136/adc.87.5.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grasshof C, Wolf A, Neuwirth F, Posovszky C. Intramural duodenal haematoma after endoscopic biopsy: Case report and review of the literature. Case Rep Gastroenterol. 2012;6:5–14. doi: 10.1159/000336022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ozcelik T, Hindilerden F, Hasbal B, Akyildiz M, Dayangac M, Killi R, et al. Intramural duodenal haematoma after upper gastrointestinal endoscopic biopsy in a bone marrow transplant recipient. Biol Blood Marrow Transplant. 2013;19:302. [Google Scholar]
- 29.Goh B, Soundappan SS. Traumatic duodenal injuries in children: A single-centre study. ANZ J Surg. 2021;91:95–9. doi: 10.1111/ans.16502. [DOI] [PubMed] [Google Scholar]
- 30.Desai KM, Dorward IG, Minkes RK, Dillon PA. Blunt duodenal injuries in children. J Trauma. 2003;54:640–5. doi: 10.1097/01.TA.0000056184.80706.9B. [DOI] [PubMed] [Google Scholar]
- 31.Clendenon JN, Meyers RL, Nance ML, Scaife ER. Management of duodenal injuries in children. J Pediatr Surg. 2004;39:964–8. doi: 10.1016/j.jpedsurg.2004.02.032. [DOI] [PubMed] [Google Scholar]
- 32.Karanjia ND, Shanahan DJ, Knight MJ. Omental patching of a large perforated duodenal ulcer: A new method. Br J Surg. 1993;80:65. doi: 10.1002/bjs.1800800123. [DOI] [PubMed] [Google Scholar]
- 33.Lal P, Vindal A, Hadke NS. Controlled tube duodenostomy in the management of giant duodenal ulcer perforation: A new technique for a surgically challenging condition. Am J Surg. 2009;198:319–23. doi: 10.1016/j.amjsurg.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 34.Chien JH, Ho TY, Shih-Peng L, Lee CL, Ou SF. Acquired duodenal obstruction in children. Pediatr Neonatol. 2008;49:193–6. doi: 10.1016/S1875-9572(09)60008-5. [DOI] [PubMed] [Google Scholar]
- 35.Al-Qudah G, Tuma F. StatPearls. Treasure Island (FL): StatPearls Publishing; 2021. [Last updated on 2020 Sep 08]. Tube. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532867/ [Google Scholar]
- 36.Mukhopadhyay M, Banerjee C, Sarkar S, Roy D, Rahman QM. Comparative study between omentopexy and omental plugging in treatment of giant peptic perforation. Indian J Surg. 2011;73:341–5. doi: 10.1007/s12262-011-0320-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jani K, Saxena AK, Vaghasia R. Omental plugging for large-sized duodenal peptic perforations: A prospective randomized study of 100 patients. South Med J. 2006;99:467–71. doi: 10.1097/01.smj.0000203814.87306.cd. [DOI] [PubMed] [Google Scholar]
- 38.Walley BD, Goco I. Duodenal patch grafting. Am J Surg. 1980;140:706–8. doi: 10.1016/0002-9610(80)90064-1. [DOI] [PubMed] [Google Scholar]
- 39.Shilyansky J, Pearl RH, Kreller M, Sena LM, Babyn PS. Diagnosis and management of duodenal injuries in children. J Pediatr Surg. 1997;32:880–6. doi: 10.1016/s0022-3468(97)90642-4. [DOI] [PubMed] [Google Scholar]
- 40.Kutlu OC, Garcia S, Dissanaike S. The successful use of simple tube duodenostomy in large duodenal perforations from varied etiologies. Int J Surg Case Rep. 2013;4:279–82. doi: 10.1016/j.ijscr.2012.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allen GS, Moore FA, Cox CS, Jr, Mehall JR, Duke JH. Delayed diagnosis of blunt duodenal injury: An avoidable complication. J Am Coll Surg. 1998;187:393–9. doi: 10.1016/s1072-7515(98)00205-1. [DOI] [PubMed] [Google Scholar]