Abstract
Introduction
A healthy diet is recommended to support diabetes management, including HbA1c, blood pressure, and cholesterol (ABC) control, but food insecurity is a barrier to consuming a healthy diet. We determined the prevalence of food insecurity and diet quality among US adults with diabetes and the associations with ABC management.
Research design and methods
Cross-sectional analyses were conducted among 2075 adults ≥20 years with diagnosed diabetes who participated in the 2013–2018 National Health and Nutrition Examination Surveys. Food insecurity was assessed using a standard questionnaire and diet quality was assessed using quartiles of the 2015 Healthy Eating Index. Adjusted ORs (aOR, 95% CI) were calculated from logistic regression models to determine the association between household food insecurity/diet quality and the ABCs while controlling for sociodemographic characteristics, healthcare utilization, smoking, medication for diabetes, blood pressure, or cholesterol, and body mass index.
Results
Overall, 17.6% of adults had food insecurity/low diet quality; 14.2% had food insecurity/high diet quality; 33.1% had food security/low diet quality; and 35.2% had food security/high diet quality. Compared with adults with food security/high diet quality, those with food insecurity/low diet quality were significantly more likely to have HbA1c ≥7.0% (aOR=1.85, 95% CI 1.23 to 2.80) and HbA1c ≥8.0% (aOR=1.79, 95% CI 1.04 to 3.08); food insecurity/high diet quality was significantly associated with elevated HbA1c; and food security/low diet quality with elevated A1c.
Conclusions
Food insecurity, regardless of diet quality, was significantly associated with elevated A1c. For people with food insecurity, providing resources to reduce food insecurity could strengthen the overall approach to optimal diabetes management.
Keywords: diet, epidemiology, disease management, poverty
WHAT IS ALREADY KNOWN ON THIS TOPIC
While a healthy diet is important for persons with diabetes to manage their disease, food insecurity may negatively impact healthy eating. Few national studies have assessed the combination of food insecurity and diet quality on the management of diabetes.
WHAT THIS STUDY ADDS
Among a national sample of US adults with diabetes, food insecurity, regardless of diet quality, was significantly associated with elevated A1c.
Low diet quality, even in the presence of food security, was significantly associated with elevated A1c.
There were no statistically significant associations between food insecurity and low diet quality with high blood pressure or elevated low-density lipoprotein cholesterol.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Identifying persons with food insecurity in healthcare settings and referring them to interventions and resources to reduce food insecurity could strengthen the overall approach to optimal diabetes management.
Introduction
The American Diabetes Association (ADA) recommends that individuals with diabetes eat a healthy diet that includes a variety of nutrient-dense foods such as fruits, vegetables, and whole grains in appropriate portion sizes and is limited in added sugars and fats.1 Consuming a healthy diet may help people with diabetes maintain or achieve a desired body weight; achieve individualized HbA1c, blood pressure (BP), and cholesterol (ABCs) targets; and delay or prevent comorbidities and diabetes-related complications.2 However, there are barriers to consuming a healthy diet, including adequate disposable income to purchase food, access to healthy food, education on preparing and cooking healthy meals, and healthy eating support from friends and family.3–5
Food security, a state of having reliable access to sufficient quantity of affordable and nutritious food, is one factor that may affect healthy eating among people with diabetes.6 A report based on the 1999–2002 National Health and Nutrition Examination Surveys (NHANES) demonstrated that diabetes prevalence was higher among people with severe food insecurity than people without food insecurity; the association remained after adjusting for body mass index (BMI).7 Another NHANES study showed that while diet quality trends among adults with diabetes improved overall between 1999 and 2014, there were substantial disparities in consuming a high-quality diet; adults with low education, low income, and food insecurity were less likely to consume a healthy diet and showed no improvement in diet quality over time.8 Further, results from the 1999–2008 NHANES data showed that food insecurity among adults with diabetes was significantly associated with HbA1c ≥9.0% and low-density lipoprotein cholesterol (LDL-C) ≥100 mg/dL after controlling for several sociodemographic and diabetes-related factors.9 A prospective cohort study of adult patients with diabetes in a primary care network also found that food insecurity was associated with higher HbA1c levels.10 A 2011–2016 NHANES study among adults with diabetes (diagnosed and undiagnosed) found an interaction between diet quality and food insecurity on the association with HbA1c at 8.0% to <9.0%.11
Given the gaps in the literature, the objective of this study was to determine the prevalence of combined food insecurity and healthy diet quality status among US adults with diabetes, overall and stratified by sociodemographic characteristics and health behaviors. In addition, we examined how food insecurity/diet quality status was associated with ABC management while accounting for factors related to achieving these ABC targets.
Research design and methods
Study population
The NHANES is a stratified multistage probability cluster survey conducted in the non-institutionalized civilian US population.12 Participants were interviewed in their homes to obtain demographic and health information and then visited a mobile examination center (MEC) for physical examinations and laboratory measures.13 14
Data were analyzed from three cycles of NHANES (2013–2014, 2015–2016, 2017–2018). Unweighted response rates ranged from 51.9% to 71.0% for the interviewed sample and from 48.8% to 68.5% for the examination sample. Study participants selected for inclusion in these analyses which combined the data from the three NHANES cycles included 2075 adults aged ≥20 years with diagnosed diabetes and at least one reliable 24-hour dietary recall.
Measures
Diagnosed diabetes was considered present if study participants answered ‘yes’ when asked if a physician or other healthcare professional ever told them that they had diabetes or sugar diabetes. Adults with HbA1c indicative of diabetes without a physician diagnosis of diabetes were not included in these analyses since this study focuses on diabetes management of the ABCs. Participants self-reported sociodemographic characteristics (current age, race and ethnicity, household income, and household size, to determine poverty income ratio (PIR), with PIR <1.0 indicating below the household poverty threshold), highest education level, receipt of Supplemental Nutrition Assistance Program (SNAP) benefits, health insurance status and type of health insurance, healthcare utilization (seen a physician or diabetes specialist in the past year, HbA1c checked in the past year), smoking status (current, former, or never), and diabetes, BP, and cholesterol medication use. Height and weight were measured by a trained interviewer to determine the BMI (kg/m2), defined as: normal <25.0 kg/m2, overweight 25.0–29.9 kg/m2; obesity ≥30 kg/m2.
Main independent measures: food insecurity and diet quality
To assess the food insecurity status for adults in their household, participants responded to either the first 10 items (if no children in the household) or full 18 items (if children in the household) of the US Department of Agriculture’s household food security questionnaire, which assessed running out of food and not being able to afford more, cutting meal size, skipping meals, eating less or not at all, or going hungry due to lack of money for food in the past 12 months.15 16 Participants were categorized as having full food security, marginal food security, or low/very low food security based on the frequency of responses to the questionnaire items and the standard scoring methods.17
Diet quality was determined by the Healthy Eating Index 2015 (HEI-2015),18 which measures how well an individual’s diet aligns with federal dietary guidelines and is generally considered a good marker of overall diet quality. The HEI-2015 includes 13 food group components that reflect the key recommendations in the 2015–2020 Dietary Guidelines for Americans—nine ‘adequacy’ components represent food groups whose consumption is encouraged (total fruits, whole fruits, total vegetables, greens and beans, whole grains, total protein foods, seafood and plant proteins dairy, fatty acids) and four ‘moderation’ components to represent food groups for which there are recommended limits to consumption (refined grains, sodium, added sugars, saturated fats). The composite HEI-2015 scores range from 0 to 100, with higher scores denoting better alignment with dietary recommendations (ie, diet quality).18 In NHANES, HEI-2015 scores were determined using participant data from at least one reliable 24-hour dietary recall and the simple HEI scoring algorithm-per person method.19 20 Participants’ diet quality was classified into four categories based on HEI-2015 score quartiles, with the first quartile indicating low diet quality, second quartile indicating low-moderate diet quality, third quartile indicating moderate-high diet quality, and the fourth quartile indicating high diet quality.
A combined food insecurity/diet quality variable was defined as (1) food secure (full food security) and moderate-high diet quality (third and fourth HEI-2015 quartiles, referred hereafter as ‘high diet quality’), (2) food secure and low-moderate diet quality (first and second HEI-2015 quartiles, referred hereafter as ‘low diet quality’), (3) food insecure (low/very low or marginal food security) and high diet quality, and (4) food insecure and low diet quality. In a sensitivity analysis, we assessed a combined food insecurity/diet quality variable that defined high diet quality as only the fourth quartile of the HEI-2015 and low diet quality as the first to third quartiles of the HEI-2015; categorization of food insecurity remained the same.
Main dependent (outcome) variables: ABCs
A phlebotomist obtained a blood sample from all participants during the MEC visit using a standardized protocol.14 BP was measured using a standardized mercury sphygmomanometer after the participant rested quietly for 5 min.13 Up to four readings were taken, and the readings were averaged, excluding the first measure. HbA1c was directly measured.14 LDL-C levels were calculated for people who had fasted ≥8 to <24 hours using the Friedewald formula, which is not valid when triglycerides are ≥400 mg/dL.21 Outcomes for the ABC measures were based on clinically elevated values. The cut-points for elevated HbA1c (≥7.0%, ≥8.0%, ≥9.0%), hypertension (BP ≥130/80 mm Hg, BP ≥140/90 mm Hg), and cholesterol (LDL-C ≥100 mg/dL, LDL-C ≥130 mg/dL) were based on current guidelines from the ADA Standards of Care.22
Statistical analysis
We used descriptive statistics to describe the characteristics of the study population overall and by food insecurity and diet quality categories. Bivariate associations between food insecurity and diet quality categories and demographic characteristics and health behaviors were tested using a χ2 test for significance. Logistic regression was used to calculate ORs (95% CI) for the association between (1) food insecurity, (2) diet quality, and (3) food insecurity/diet quality (four-level combined variable) and elevated ABC levels. Models were (1) unadjusted, (2) adjusted for age, sex, race, and ethnicity, (3) additionally adjusted for PIR, education, health insurance, (4) additionally adjusted for healthcare utilization (seeing a physician or specialist in the past year, having HbA1c checked), (5) additionally adjusted for smoking status, diabetes, BP, and cholesterol medications, and BMI, and (6) additionally adjusted for food insecurity or diet quality when these variables were not the main covariates. P values <0.05 were considered statistically significant. All statistical analyses used sampling weights to account for the NHANES’ complex survey design using SUDAAN (SUDAAN User’s Manual, Release 11, 2012; Research Triangle Institute). A 6-year dietary weight was used for all analyses except for analyses among the fasting sample (LDL-C and triglycerides) where a 6-year fasting weight was used.
Results
Participant characteristics
Among US adults with diagnosed diabetes, the mean age was 60.4 years, 53.0% were men, 15.3% were living below the poverty threshold, and 19.3% had low/very low food security (food insecure) (online supplemental appendix table 1). Mean HEI score was 53.6, with 66.7% having an HEI score <60. The mean HEI-2015 scores were 36.5 (range, 10.0–43.2) for the first quartile, 48.3 (range, 43.2–52.7) for the second quartile, 57.9 (range, 52.7–62.9) for the third quartile, and 71.8 (range, 62.8–99.5) for the fourth quartile. Nearly half (49.8%) had HbA1c ≥7.0%, 28.5% had BP ≥140/90 mm Hg, and 18.0% had LDL-C ≥130 mg/dL. Several sociodemographic characteristics and metabolic control varied by food insecurity and diet quality.
bmjdrc-2022-003033supp001.pdf (86.6KB, pdf)
Participant characteristics by food insecurity and diet quality
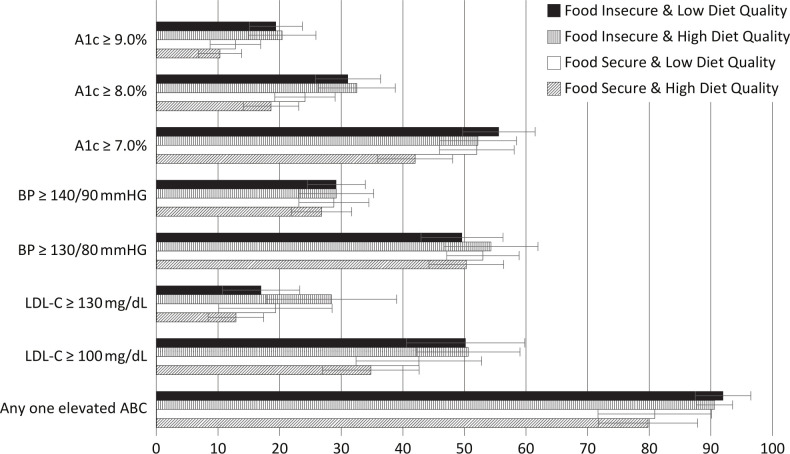
When food insecurity and diet quality were combined into a four-level variable, 17.6% of persons with diabetes had food insecurity (low/very low or marginal)/low diet quality (first/second HEI-2015 quartile); 14.2% had food insecurity/high diet quality (third/fourth HEI-2015 quartile); 33.1% had food security/low diet quality; and 35.2% had food security/high diet quality (table 1). Among adults with diabetes, the distribution of age, sex, race and ethnicity, PIR, education, receiving SNAP benefits, and health insurance status all varied by food insecurity/diet quality category (p<0.01 for all). In addition, the per cent with uncontrolled HbA1c, elevated LDL-C, and having any one elevated ABC measure varied by food insecurity/diet quality category (p<0.03 for all) (figure 1).
Table 1.
Characteristics of US adults with diagnosed diabetes by food insecurity and diet quality
| Food insecurity and diet quality (HEI-2015)* | P value, χ2 | ||||
| Food secure and high diet quality | Food secure and low diet quality | Food insecure and high diet quality | Food insecure and low diet quality | ||
| Unweighted n | 681 | 551 | 400 | 443 | |
| % (SE) | |||||
| Total | 35.2 (1.5) | 33.1 (1.5) | 14.2 (1.1) | 17.6 (1.3) | |
| Age (years) | |||||
| Mean | 62.5 (0.7) | 60.3 (0.7) | 59.9 (0.94) | 56.3 (0.8) | |
| 20–44 | 6.9 (1.4) | 13.0 (1.3) | 15.6 (2.5) | 19.9 (1.9) | 0.001 |
| 45–64 | 45.1 (2.7) | 48.2 (2.5) | 43.3 (3.6) | 50.5 (3.7) | |
| ≥65 | 48.0 (2.8) | 38.8 (2.6) | 41.1 (4.0) | 29.7 (3.5) | |
| Sex | |||||
| Men | 58.1 (2.8) | 57.5 (3.3) | 36.8 (3.3) | 49.3 (2.6) | <0.001 |
| Women | 41.9 (2.8) | 42.5 (3.3) | 63.2 (3.3) | 50.7 (2.6) | |
| Race and ethnicity | |||||
| Non-Hispanic White | 67.4 (3.0) | 74.1 (2.5) | 45.8 (4.7) | 59.0 (3.8) | <0.001 |
| Non-Hispanic Black | 12.7 (1.9) | 11.0 (1.3) | 19.2 (2.9) | 16.7 (2.4) | |
| Hispanic/Latino | 11.3 (1.8) | 12.5 (2.2) | 29.7 (4.0) | 21.6 (2.7) | |
| Non-Hispanic Asian | 8.6 (1.5) | 2.4 (0.6) | 5.3 (1.6) | 2.7 (0.8) | |
| Poverty income ratio | |||||
| <1.00 | 6.9 (1.3) | 8.0 (1.2) | 26.5 (2.8) | 35.6 (3.6) | <0.001 |
| 1.00–2.00 | 13.8 (1.9) | 16.8 (1.9) | 35.0 (3.2) | 29.5 (3.5) | |
| >2.00 | 72.5 (2.9) | 69.8 (2.3) | 31.0 (3.4) | 29.6 (3.7) | |
| Missing | 6.8 (1.4) | 5.5 (0.7) | 7.5 (1.5) | 5.3 (1.7) | |
| Education | |||||
| Less than high school | 12.4 (1.7) | 16.1 (1.7) | 31.3 (2.9) | 27.3 (3.1) | <0.001 |
| High school graduate | 23.0 (2.2) | 23.6 (2.6) | 32.5 (3.0) | 30.4 (3.2) | |
| Some college | 33.4 (2.9) | 37.2 (3.1) | 26.2 (2.7) | 35.7 (3.2) | |
| College graduate or above | 31.2 (3.3) | 23.1 (2.3) | 10.1 (1.6) | 6.6 (1.9) | |
| SNAP benefit | |||||
| Yes | 9.3 (1.6) | 13.2 (1.7) | 34.1 (3.3) | 43.9 (3.5) | <0.001 |
| No | 90.7 (1.6) | 86.8 (1.7) | 65.9 (3.3) | 56.1 (3.5) | |
| Health insurance | |||||
| Uninsured | 4.8 (0.8) | 7.7 (1.5) | 12.5 (1.9) | 12.9 (2.2) | 0.002 |
| Insured | 95.2 (0.8) | 92.3 (1.5) | 87.5 (1.9) | 87.1 (2.2) | |
| Health insurance type | |||||
| Private | 65.3 (3.6) | 68.3 (3.1) | 53.6 (4.0) | 42.7 (3.3) | <0.001 |
| Medicare | 48.2 (2.7) | 42.8 (2.7) | 48.6 (4.4) | 46.8 (3.4) | 0.599 |
| Medicaid | 7.7 (1.7) | 9.1 (1.3) | 22.7 (2.8) | 27.0 (2.8) | <0.001 |
| Military/other government | 16.4 (2.1) | 13.5 (2.4) | 12.4 (2.4) | 17.3 (2.5) | 0.409 |
| Seen physician in the past year | |||||
| Yes | 98.1 (0.8) | 97.6 (0.9) | 94.0 (1.5) | 95.2 (1.1) | 0.124 |
| No | 1.9 (0.8) | 2.4 (0.9) | 6.0 (1.5) | 4.8 (1.1) | |
| Seen diabetes specialist in the past year | |||||
| Yes | 33.3 (2.9) | 24.3 (2.4) | 34.8 (2.7) | 26.6 (2.9) | 0.021 |
| No | 35.6 (3.2) | 35.5 (2.4) | 28.3 (2.5) | 36.2 (3.3) | |
| Never | 31.1 (2.4) | 40.2 (2.6) | 36.9 (2.4) | 37.2 (3.6) | |
| HbA1c checked in the past year | |||||
| Yes | 89.7 (1.2) | 81.2 (2.5) | 78.2 (2.5) | 74.9 (2.9) | 0.001 |
| No | 7.4 (1.0) | 13.1 (2.1) | 18.0 (2.1) | 19.7 (2.8) | |
| Do not know | 2.9 (0.7) | 5.7 (1.5) | 3.8 (1.1) | 5.4 (1.3) | |
| Smoking status | |||||
| Current | 5.9 (1.4) | 15.1 (2.2) | 13.6 (2.2) | 25.6 (3.1) | <0.001 |
| Former | 43.8 (3.3) | 35.2 (2.8) | 33.7 (2.7) | 32.8 (2.9) | |
| Never | 50.3 (3.0) | 49.7 (3.3) | 52.7 (3.2) | 41.6 (3.1) | |
| Diabetes medication | |||||
| Insulin only | 11.7 (1.8) | 9.0 (1.7) | 9.3 (1.7) | 18.7 (2.7) | 0.003 |
| Oral medication only | 61.4 (2.7) | 58.1 (3.3) | 54.1 (2.6) | 42.8 (3.0) | |
| Both insulin and oral | 11.2 (1.8) | 15.5 (2.3) | 18.8 (2.6) | 18.4 (1.9) | |
| None | 15.8 (2.1) | 17.4 (2.7) | 17.9 (2.1) | 20.2 (2.3) | |
| Taking antihypertensive medication | 65.7 (2.7) | 63.5 (3.0) | 57.4 (3.3) | 60.8 (2.7) | 0.094 |
| Taking antilipidemic medication | 61.3 (2.9) | 64.9 (2.2) | 50.1 (3.4) | 56.3 (2.7) | 0.007 |
| BMI (kg/m2) | |||||
| Mean | 32.0 (0.4) | 34.0 (0.5) | 33.1 (0.6) | 34.8 (0.6) | |
| <25.0 | 11.7 (1.7) | 8.5 (1.4) | 10.4 (1.7) | 8.0 (1.5) | 0.027 |
| 25.0–29.9 | 30.1 (2.8) | 23.2 (2.1) | 32.1 (2.6) | 21.1 (2.7) | |
| ≥30 | 58.2 (3.3) | 68.3 (1.7) | 57.5 (3.0) | 70.9 (3.1) | |
Boldface p values indicate statistical significance of p<0.05.
*Food insecurity is defined as marginal or low/very low food security; food secure is defined as full food security; low diet quality is defined as HEI-2015 score in the 1st or 2nd quartile; high diet quality is defined as HEI-2015 score in the 3rd or 4th quartile.
BMI, body mass index; HEI-2015, Healthy Eating Index 2015; SNAP, Supplemental Nutrition Assistance Program.
Figure 1.
Prevalence of suboptimal diabetes ABC management by food insecurity and diet quality. Error bars represent 95% CIs. ABC, HbA1c, blood pressure, and cholesterol; BP, blood pressure; LDL-C, low-density lipoprotein cholesterol.
Adjusted associations between food insecurity and ABCs
Adults with diabetes who were food insecure were significantly more likely to have elevated HbA1c compared with those with full food security after adjusting for sociodemographic characteristics, healthcare utilization, smoking status, diabetes, BP, and cholesterol medication use, BMI, and diet quality (adjusted OR (aOR)=1.62, 95% CI 1.07 to 2.47 for HbA1c ≥7.0%; aOR=1.71, 95% CI 1.14 to 2.56 for HbA1c ≥8.0%; aOR=1.59, 95% CI 1.04 to 2.43 for HbA1c ≥9.0%) (online supplemental appendix table 2). There were no significant associations between food insecurity and elevated BP and LDL-C except for the unadjusted association between food insecurity and LDL-C ≥100 mg/dL (OR=1.50, 95% CI 1.05 to 2.15).
bmjdrc-2022-003033supp002.pdf (142.1KB, pdf)
Adjusted associations between diet quality and ABCs
Adults with diabetes who had low diet quality (lowest, first quartile) were significantly more likely to have elevated HbA1c (aOR=1.61, 95% CI 1.06 to 2.46 for ≥7.0%; aOR=1.60, 95% CI 1.01 to 2.53 for ≥8.0%) compared with those with high diet quality (highest, fourth quartile) after full adjustment (online supplemental appendix table 2). There were no significant associations between food insecurity and elevated BP and LDL-C.
Adjusted joint associations between food insecurity, diet quality, and ABCs
Adults with diabetes who had food insecurity (low/very low or marginal food security)/low diet quality (first/second HEI-2015 quartile) were significantly more likely to have HbA1c ≥7.0% (aOR=1.85, 95% CI 1.23 to 2.80) and HbA1c ≥8.0% (aOR=1.79, 95% CI 1.04 to 3.08) compared with those who had food security (full food security)/high diet quality (third/fourth HEI-2015 quartile) in fully adjusted models (table 2). A similar association for HbA1c ≥7.0% and HbA1c ≥8.0% was shown for those who had food insecurity/high diet quality versus food security/high diet quality. Adults who had food security/low diet quality were significantly more likely to have HbA1c ≥7.0% (aOR=1.55, 95% CI 1.07 to 2.24). In unadjusted analysis, adults with diabetes who had food insecurity/low diet quality were significantly more likely to have A1c ≥9.0% compared with those who had food security/high diet quality (OR=2.10, 95% CI 1.24 to 3.55), but this association became non-significant after adjusting for age, sex, and race/ethnicity; a similar finding was shown for those with food insecurity/high diet quality, but the association became non-significant after adjusting for all sociodemographic characteristics. There were no significant interactions between food insecurity and diet quality for any of the other ABC outcomes.
Table 2.
OR (95% CI) for suboptimal diabetes ABC management by food security and diet quality
| Food security and diet quality (HEI-2015)* | |||||
| Prevalence, % (SE) | Food secure and high diet quality | Food secure and low diet quality | Food insecure and high diet quality | Food insecure and low diet quality |
|
| HbA1c ≥7.0% | 49.8 (1.8) | ||||
| Unadjusted | 1.00 | 1.49 (1.08 to 2.07) | 1.51 (1.06 to 2.14) | 1.73 (1.26 to 2.36) | |
| Model 1 | 1.00 | 1.50 (1.08 to 2.09) | 1.59 (1.08 to 2.34) | 1.76 (1.25 to 2.47) | |
| Model 2 | 1.00 | 1.52 (1.09 to 2.12) | 1.64 (1.11 to 2.42) | 1.89 (1.34 to 2.66) | |
| Model 3 | 1.00 | 1.55 (1.10 to 2.18) | 1.64 (1.11 to 2.44) | 1.92 (1.36 to 2.71) | |
| Model 4 | 1.00 | 1.55 (1.07 to 2.24) | 1.69 (1.14 to 2.51) | 1.85 (1.23 to 2.80) | |
| HbA1c ≥8.0% | 26.1 (1.3) | ||||
| Unadjusted | 1.00 | 1.39 (0.93 to 2.07) | 2.10 (1.37 to 2.32) | 1.97 (1.30 to 2.99) | |
| Model 1 | 1.00 | 1.29 (0.86 to 1.94) | 1.80 (1.15 to 2.82) | 1.67 (1.07 to 2.59) | |
| Model 2 | 1.00 | 1.28 (0.85 to 1.93) | 1.74 (1.08 to 2.79) | 1.61 (0.99 to 2.61) | |
| Model 3 | 1.00 | 1.30 (0.87 to 1.95) | 1.71 (1.06 to 2.75) | 1.62 (1.00 to 2.65) | |
| Model 4 | 1.00 | 1.37 (0.91 to 2.07) | 1.83 (1.12 to 2.98) | 1.79 (1.04 to 3.08) | |
| HbA1c ≥9.0% | 14.4 (1.0) | ||||
| Unadjusted | 1.00 | 1.27 (0.75 to 2.16) | 2.22 (1.40 to 3.52) | 2.10 (1.24 to 3.55) | |
| Model 1 | 1.00 | 1.11 (0.65 to 1.88) | 1.70 (1.07 to 2.71) | 1.58 (0.90 to 2.77) | |
| Model 2 | 1.00 | 1.10 (0.66 to 1.84) | 1.56 (0.94 to 2.60) | 1.43 (0.79 to 2.59) | |
| Model 3 | 1.00 | 1.11 (0.67 to 1.84) | 1.48 (0.88 to 2.47) | 1.42 (0.77 to 2.65) | |
| Model 4 | 1.00 | 1.18 (0.70 to 1.98) | 1.54 (0.92 to 2.60) | 1.47 (0.80 to 2.70) | |
| Blood pressure ≥140/90 mm Hg | 28.5 (1.5) | ||||
| Unadjusted | 1.00 | 1.10 (0.78 to 1.56) | 1.12 (0.78 to 1.62) | 1.13 (0.80 to 1.59) | |
| Model 1 | 1.00 | 1.18 (0.82 to 1.71) | 1.18 (0.80 to 1.74) | 1.22 (0.84 to 1.79) | |
| Model 2 | 1.00 | 1.16 (0.80 to 1.67) | 1.11 (0.75 to 1.65) | 1.16 (0.77 to 1.74) | |
| Model 3 | 1.00 | 1.15 (0.80 to 1.65) | 1.12 (0.75 to 1.67) | 1.16 (0.78 to 1.74) | |
| Model 4 | 1.00 | 1.21 (0.83 to 1.77) | 1.14 (0.76 to 1.70) | 1.14 (0.74 to 1.75) | |
| Blood pressure ≥130/80 mm Hg | 52.0 (1.5) | ||||
| Unadjusted | 1.00 | 1.11 (0.81 to 1.53) | 1.17 (0.76 to 1.83) | 0.97 (0.70 to 1.35) | |
| Model 1 | 1.00 | 1.15 (0.82 to 1.62) | 1.32 (0.86 to 2.04) | 1.01 (0.71 to 1.45) | |
| Model 2 | 1.00 | 1.14 (0.80 to 1.61) | 1.17 (0.73 to 1.88) | 0.90 (0.62 to 1.31) | |
| Model 3 | 1.00 | 1.15 (0.81 to 1.63) | 1.15 (0.72 to 1.83) | 0.92 (0.64 to 1.32) | |
| Model 4 | 1.00 | 1.17 (0.78 to 1.75) | 1.15 (0.74 to 1.79) | 0.87 (0.58 to 1.31) | |
| LDL-C ≥100 mg/dL | 41.8 (2.4) | ||||
| Unadjusted | 1.00 | 1.39 (0.82 to 2.36) | 1.93 (1.20 to 3.09) | 1.89 (1.15 to 3.11) | |
| Model 1 | 1.00 | 1.12 (0.64 to 1.97) | 1.36 (0.79 to 2.35) | 1.40 (0.78 to 2.51) | |
| Model 2 | 1.00 | 1.13 (0.64 to 1.99) | 1.19 (0.69 to 2.05) | 1.25 (0.68 to 2.29) | |
| Model 3 | 1.00 | 1.04 (0.59 to 1.82) | 1.11 (0.65 to 1.88) | 1.25 (0.66 to 2.34) | |
| Model 4 | 1.00 | 1.00 (0.62 to 1.62) | 0.93 (0.53 to 1.65) | 1.08 (0.52 to 2.23) | |
| LDL-C ≥130 mg/dL | 18.0 (1.7) | ||||
| Unadjusted | 1.00 | 1.63 (0.77 to 3.41) | 2.69 (1.31 to 5.52) | 1.39 (0.71 to 2.74) | |
| Model 1 | 1.00 | 1.24 (0.60 to 2.54) | 1.82 (0.84 to 3.94) | 1.01 (0.50 to 2.05) | |
| Model 2 | 1.00 | 1.27 (0.66 to 2.45) | 1.70 (0.72 to 4.02) | 0.97 (0.42 to 2.25) | |
| Model 3 | 1.00 | 1.22 (0.65 to 2.30) | 1.65 (0.73 to 3.72) | 0.99 (0.44 to 2.22) | |
| Model 4 | 1.00 | 1.37 (0.76 to 2.48) | 1.24 (0.61 to 2.55) | 0.77 (0.31 to 1.90) | |
| At least one elevated ABC (HbA1c ≥7.0%, BP ≥130/80 mm Hg, LDL ≥100 mg/dL) |
84.3 (2.1) | ||||
| Unadjusted | 1.00 | 1.07 (0.48 to 2.39) | 2.44 (1.37 to 4.35) | 2.90 (1.24 to 6.82) | |
| Model 1 | 1.00 | 0.90 (0.39 to 2.09) | 1.87 (1.04 to 3.36) | 2.00 (0.82 to 4.89) | |
| Model 2 | 1.00 | 0.88 (0.38 to 2.03) | 1.70 (0.96 to 3.01) | 1.87 (0.81 to 4.32) | |
| Model 3 | 1.00 | 0.88 (0.37 to 2.05) | 1.67 (0.93 to 3.00) | 1.86 (0.80 to 4.34) | |
| Model 4 | 1.00 | 0.80 (0.34 to 1.90) | 1.59 (0.73 to 3.43) | 1.98 (0.72 to 5.49) | |
| At least one elevated ABC (HbA1c ≥8.0%, BP ≥140/90 mm Hg, LDL ≥130 mg/dL) |
55.0 (2.6) | ||||
| Unadjusted | 1.00 | 1.01 (0.57 to 1.80) | 2.38 (1.52 to 3.73) | 1.19 (0.78 to 1.83) | |
| Model 1 | 1.00 | 0.96 (0.52 to 1.76) | 1.89 (1.18 to 3.02) | 1.08 (0.67 to 1.76) | |
| Model 2 | 1.00 | 0.95 (0.52 to 1.72) | 1.75 (1.04 to 2.93) | 1.03 (0.61 to 1.76) | |
| Model 3 | 1.00 | 0.96 (0.53 to 1.72) | 1.72 (1.04 to 2.86) | 1.05 (0.60 to 1.86) | |
| Model 4 | 1.00 | 0.99 (0.55 to 1.79) | 1.58 (0.87 to 2.86) | 1.05 (0.57 to 1.96) | |
Model 1: adjusted for age, sex, race/ethnicity.
Model 2: Model 1 and additionally adjusted for PIR, education, health insurance.
Model 3: Model 2 and additionally adjusted for healthcare utilization (seeing physicians in the past year, having HbA1c checked).
Model 4: Model 3 and additionally adjusted for smoking status, diabetes medication, blood pressure medication, cholesterol medication, BMI.
Boldface indicates statistical significance of p<0.05.
*Food insecurity is defined as marginal or low/very low food security; food secure is defined as full food security; low diet quality is defined as HEI-2015 score in the 1st or 2nd quartile; high diet quality is defined as HEI-2015 in the 3rd or 4th quartile.
ABC, HbA1c, blood pressure, and cholesterol; BMI, body mass index; BP, blood pressure; HEI-2015, Healthy Eating Index 2015; LDL, low-density lipoprotein; PIR, poverty income ratio.
When high diet quality was defined as only the fourth quartile of the HEI-2015 (vs low/moderate diet quality, first to third HEI-2015 quartiles), the results remained largely unchanged for those with food insecurity and low/moderate diet quality (online supplemental appendix table 3). In fully adjusted models, adults who had food insecurity and low/moderate diet quality (first to third HEI-2015 quartiles) were significantly more likely to have elevated HbA1c compared with those who had food security/high diet quality (fourth HEI-2015 quartile).
bmjdrc-2022-003033supp003.pdf (44KB, pdf)
Discussion
In this national study of US adults with diabetes, the combination of food insecurity and low diet quality was significantly associated with poorer glycemic management compared with those who were food secure and had high diet quality, independent of sociodemographic characteristics, healthcare utilization, diabetes medications, and BMI; findings were similar for those with food insecurity and high diet quality. In addition, low diet quality, even in the presence of food security, was significantly associated with A1c ≥7.0%. We did not find any statistically significant associations between food insecurity and low diet quality and high BP or LDL-C.
Lower socioeconomic status, which, by definition, is strongly associated with food insecurity, has been previously associated with poorer ABC control.23 24 Indeed, in the current study among adults with food insecurity, living below the poverty threshold or having Medicaid was five times more prevalent compared with those adults with full food security; having less than a high school education was nearly 2.5 times more prevalent among those with food insecurity compared with those adults with full food security. Diet quality was also worse for those with less income, but the difference was not as large in magnitude as it was for food insecurity. Previous studies have found that diet quality is related to the affordability of healthy foods,25–27 but access to healthy food and the ability to afford these foods does not directly equate to a high-quality diet; diet quality is a modifiable behavior, more so than food insecurity. However, it is well established that behavior change is difficult and challenging to maintain.28
Previous studies in various populations have shown that food insecurity is associated with poorer glycemic control. Among low-income urban residents with type 2 diabetes, food insecurity was associated with poorer glucose control; however, among those who were food insecure, the receipt of SNAP benefits was associated with a significantly reduced odds of having poor glucose control.29 Thus, economic food assistance appears helpful for those with diabetes; these data suggest that food insecure adults were eating healthier with SNAP than those without assistance. SNAP assistance has also been shown to reduce psychological distress related to food insecurity.30 In a different study of low-income patients with diabetes, those who were food insecure had higher mean HbA1c levels compared with those who were food secure.31 A previous study using NHANES 2011–2016 data among adults with diagnosed and undiagnosed diabetes found an interaction between food insecurity and diet quality with elevated HbA1c (8.0% to <9.0%) but the relationship between food insecurity and diet quality was not fully elucidated.11 In another earlier study using NHANES data from 1999 to 2008, food insecurity was associated with HbA1c >9.0% and poor LDL control after adjustment for sociodemographic characteristics and diabetes-related factors; however, dietary intake was not included in that study.9 The results were similar to those from our study, where we found that food insecurity was associated with all categories of poorer glucose control after adjusting for sociodemographic characteristics, diabetes-related factors, including prescription medications, and diet quality. Further, we also found that food insecurity, regardless of whether diet quality was high or low, was associated with elevated HbA1c before and after adjustment for other covariates. Given that diet quality did not account for the association between food insecurity and poor glucose control, future research could investigate the intricacies of food insecurity and the pathways by which it is associated with metabolic outcomes. Potential pathways highlighted in a recent scientific review of social determinants of health as they relate to diabetes included nutritional, compensatory, and psychological pathways, each of which warrants further investigation including the intersectionality of these pathways.32
While food insecurity was significantly associated with the highest level of uncontrolled HbA1c (≥9.0%) after full adjustment including diet quality, when food insecurity and diet quality were combined into the four-category variable, only the unadjusted associations for food insecurity/low diet quality and food insecurity/high diet quality were significant. There may be other unmeasured factors contributing to the lack of significant associations for the highest level of uncontrolled HbA1c. In addition, 14% of our sample had HbA1c ≥9.0%, thus our sample size was limited to detect an association for this outcome.
Our study suggests that food insecurity may have a direct impact on metabolic outcomes such as HbA1c. Previous research has shown that stress from food insecurity may result in consuming high-carbohydrate, high-sugar, or high-fat foods which may offer temporary feelings of comfort.33 Securing these palatable foods may be easier in areas with high food insecurity due to a higher prevalence of food swamps, areas with a high density of establishments selling high-calorie fast food and junk food relative to healthier food items.5 However, food assistance programs such as food pantries, Women, Infants, and Children program, and SNAP benefits are resources available to those with food insecurity and may support a higher quality diet.34–36
Consuming a high-quality diet, as recommended by the ADA,2 is strongly associated with a variety of factors including community-level resources (eg, access to healthy foods), support for a healthy diet from friends and family, and individual-level sociodemographic characteristics (eg, income barriers), behaviors, and habits. At the community level, lower availability of healthy food has been associated with lower quality dietary intake and poorer glycemic control in some studies10 37–39; other studies have been inconclusive.40 41 Considering the many contextual factors that influence diet quality is important when developing interventions and programs to support people with diabetes and improve metabolic outcomes.42
We found no significant association between food insecurity/diet quality and BP or LDL-C. Many of the adults in our study had controlled BP and LDL-C, with 63% on antihypertensive medication and 60% on antilipidemic medication. Therefore, there may have been less of an association for food insecurity and diet quality on these outcomes. In addition, the associations between food insecurity/diet quality may be mediated through obesity, a condition that effected nearly two-thirds of the population of adults with diabetes. This may also partially explain the lack of an association for BP and LDL-C. While LDL-C is considered the hallmark measure for cholesterol management among people with diabetes, triglycerides and high-density lipoprotein cholesterol (HDL-C) are also important markers for hyperlipidemia. Of note, in analyses that were not included in the paper, we found that compared with adults with food security/high diet quality, those with food insecurity/low diet quality were statistically significantly more likely to have high triglycerides and low HDL-C; the significant association with high triglycerides was also found for those with food insecurity/high diet quality. When any of these lipid measures are suboptimal, current diabetes management guidelines recommend optimizing glycemic control.43
Limitations
NHANES is a cross-sectional survey, thus causal associations between our exposures of interest, food insecurity and diet quality, and outcomes of ABC management cannot be determined. Trends in associations of food insecurity/diet quality and ABC management outcomes were not assessed. However, declines in A1c control after 2010 may be associated with the notable prevalence of food insecurity and suboptimal dietary intake among adults with diabetes during 2013–2018. Dietary intake was self-reported, which is subject to measurement error similar to other self-reported data44; however, these data still provide valuable information on food intake and eating patterns.45 Although we adjusted for many sociodemographic factors, residual confounding may have occurred and the true association between food insecurity/low diet quality and poor ABC management may be associated with other unmeasured variables. Additionally, we do not distinguish between type 1 and type 2 diabetes mellitus in this analysis; however, given that the NHANES is nationally representative, we can assume that 90%–95% of diagnosed diabetes in this study is type 2 diabetes.46 In supplemental analysis, we found no interaction between continuous insulin use, an indicator of type 1 diabetes mellitus, and food insecurity/diet quality. However, this study used a nationally representative sample allowing generalization to the US adult non-institutionalized population with diabetes. Multiple clinical outcomes were assessed using standardized measures to characterize diabetes control.
Conclusions
In this nationally representative study among US adults with diabetes, food insecurity plus low diet quality was associated with higher HbA1c levels even after accounting for sociodemographic characteristics and health behaviors, with food insecurity having a greater impact on metabolic outcomes than low diet quality. Healthcare providers treating adults with diabetes may consider including an assessment of food insecurity as a part of their overall approach to diabetes-related healthcare, particularly for their patients with suboptimal HbA1c and those living in low-income or under-resourced communities. Future research on food insecurity among adults with diabetes might focus on how food insecurity affects metabolic outcomes and address the multiple pathways that may contribute to these outcomes. Healthcare delivery systems could link patients to social or food services as part of clinical care, in addition to point-of-care interventions that promote healthier lifestyles.
Acknowledgments
The authors would like to acknowledge Pamela L Thornton for her review and comments on this paper.
Footnotes
Presented at: Parts of this study were presented in abstract form at the 82nd Scientific Sessions of the American Diabetes Association, New Orleans, Louisiana, 3–7 June 2022.
Contributors: SSC: Conceptualization and design; Acquired, analyzed, and interpreted the data; Drafted the manuscript; Provided critical revision for important intellectual content. KMB and KRS: Interpreted the data; Provided critical revision for important intellectual content. JML: Conceptualization and design; Provided critical revision for important intellectual content. SSC is the guarantor of this work and takes responsibility for the integrity of the data and the accuracy of the analysis.
Funding: This study was supported by a contract with the National Institute of Diabetes and Digestive and Kidney Diseases (contract number: 75N94022F00050).
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institutes of Health.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Data for the NHANES are publicly available at https://wwwn.cdc.gov/nchs/nhanes/.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the National Center for Health Statistics (NCHS) Research Ethics Review Board (protocol numbers: 2018-01 and 2011-17). Participants gave informed consent to participate in the study before taking part.
References
- 1.American Diabetes Association . 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2021. Diabetes Care 2021;44:S53–72. 10.2337/dc21-S005 [DOI] [PubMed] [Google Scholar]
- 2.Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care 2019;42:731–54. 10.2337/dci19-0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lehr AL, Driver SL, Stone NJ. The ABCDs of lifestyle counseling. JAMA Cardiol 2016;1:505–6. 10.1001/jamacardio.2016.1419 [DOI] [PubMed] [Google Scholar]
- 4.Seguin R, Connor L, Nelson M, et al. Understanding barriers and facilitators to healthy eating and active living in rural communities. J Nutr Metab 2014;2014:1–8. 10.1155/2014/146502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooksey-Stowers K, Schwartz MB, Brownell KD. Food swamps predict obesity rates better than food Deserts in the United States. Int J Environ Res Public Health 2017;14. 10.3390/ijerph14111366. [Epub ahead of print: 14 11 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gucciardi E, Vahabi M, Norris N, et al. The intersection between food insecurity and diabetes: a review. Curr Nutr Rep 2014;3:324–32. 10.1007/s13668-014-0104-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seligman HK, Bindman AB, Vittinghoff E, et al. Food insecurity is associated with diabetes mellitus: results from the National health examination and nutrition examination survey (NHANES) 1999-2002. J Gen Intern Med 2007;22:1018–23. 10.1007/s11606-007-0192-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orr CJ, Keyserling TC, Ammerman AS, et al. Diet quality trends among adults with diabetes by socioeconomic status in the U.S.: 1999-2014. BMC Endocr Disord 2019;19:54. 10.1186/s12902-019-0382-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berkowitz SA, Baggett TP, Wexler DJ, et al. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care 2013;36:3093–9. 10.2337/dc13-0570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berkowitz SA, Karter AJ, Corbie-Smith G, et al. Food Insecurity, Food "Deserts," and Glycemic Control in Patients With Diabetes: A Longitudinal Analysis. Diabetes Care 2018;41:1188–95. 10.2337/dc17-1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaheen M, Kibe LW, Schrode KM. Dietary quality, food security and glycemic control among adults with diabetes. Clin Nutr ESPEN 2021;46:336–42. 10.1016/j.clnesp.2021.09.735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) . National health and nutrition examination survey; 2013-2018. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2018. [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) . National health and nutrition examination survey examination protocol: 2017-2018. Hyattsville, MD: Department of Health and Human Services, Centers for Disease Control and Prevention; 2018. [Google Scholar]
- 14.Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) . National health and nutrition examination survey laboratory protocol: glucose, cholesterol and triglycerides. 2017-2018 2018.
- 15.National Center for Health Statistics . National health and nutrition examination survey, data documentation, food security: 2017-2018, 2021. Available: https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/FSQ_J.htm
- 16.Bickel G, Nord M, Price C. Guide to measuring household food security USDA Food and Nutrition Service; 2000. [Google Scholar]
- 17.National Center for Health Statistics . National health and nutrition examination survey: food security questionnaire, 2021. Available: https://wwwn.cdc.gov/Nchs/Nhanes/2017-2018/FSQ_J.htm
- 18.Division of Cancer Control & Population Sciences . Developing the healthy eating index, 2015, 2021. Available: https://epi.grants.cancer.gov/hei/developing.html#2015c
- 19.Division of Cancer Control & Population Sciences . Healthy eating index SAS code, 2022. Available: https://epi.grants.cancer.gov/hei/sas-code.html
- 20.National Center for Health Statistics . NHANES 2013-2018 dietary data: Analytic documentation. 2013-2018, 2021. Available: https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Dietary&CycleBeginYear=2017
- 21.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499–502. 10.1093/clinchem/18.6.499 [DOI] [PubMed] [Google Scholar]
- 22.ADA’s standards of medical care in diabetes. Clin Diabetes 2021;39:128. 10.2337/cd21-pe01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stark Casagrande S, Fradkin JE, Saydah SH, et al. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care 2013;36:2271–9. 10.2337/dc12-2258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA 2021;326:704. 10.1001/jama.2021.9883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Darmon N, Drewnowski A. Does social class predict diet quality? Am J Clin Nutr 2008;87:1107–17. 10.1093/ajcn/87.5.1107 [DOI] [PubMed] [Google Scholar]
- 26.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev 2015;73:643–60. 10.1093/nutrit/nuv027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pechey R, Monsivais P. Socioeconomic inequalities in the healthiness of food choices: exploring the contributions of food expenditures. Prev Med 2016;88:203–9. 10.1016/j.ypmed.2016.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kelly MP, Barker M. Why is changing health-related behaviour so difficult? Public Health 2016;136:109–16. 10.1016/j.puhe.2016.03.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mayer VL, McDonough K, Seligman H, et al. Food insecurity, coping strategies and glucose control in low-income patients with diabetes. Public Health Nutr 2016;19:1103–11. 10.1017/S1368980015002323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oddo VM, Mabli J. Association of participation in the supplemental nutrition assistance program and psychological distress. Am J Public Health 2015;105:e30–5. 10.2105/AJPH.2014.302480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lyles CR, Wolf MS, Schillinger D, et al. Food insecurity in relation to changes in hemoglobin A1c, self-efficacy, and fruit/vegetable intake during a diabetes educational intervention. Diabetes Care 2013;36:1448–53. 10.2337/dc12-1961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care 2020. 10.2337/dci20-0053. [Epub ahead of print: 02 Nov 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ulrich-Lai YM, Fulton S, Wilson M, et al. Stress exposure, food intake and emotional state. Stress 2015;18:381–99. 10.3109/10253890.2015.1062981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Aiyer JN, Raber M, Bello RS, et al. A pilot food prescription program promotes produce intake and decreases food insecurity. Transl Behav Med 2019;9:922–30. 10.1093/tbm/ibz112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Caspi CE, Davey C, Barsness CB, et al. Applying the healthy eating Index-2015 in a sample of Choice-Based Minnesota food Pantries to test associations between food Pantry inventory, client food selection, and client diet. J Acad Nutr Diet 2021;121:2242–50. 10.1016/j.jand.2021.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ratcliffe C, McKernan S-M, Zhang S. How much does the supplemental nutrition assistance program reduce food insecurity? Am J Agric Econ 2011;93:1082–98. 10.1093/ajae/aar026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Franco M, Diez-Roux AV, Nettleton JA, et al. Availability of healthy foods and dietary patterns: the multi-ethnic study of atherosclerosis. Am J Clin Nutr 2009;89:897–904. 10.3945/ajcn.2008.26434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kanchi R, Lopez P, Rummo PE, et al. Longitudinal analysis of neighborhood food environment and diabetes risk in the Veterans administration diabetes risk cohort. JAMA Netw Open 2021;4:e2130789. 10.1001/jamanetworkopen.2021.30789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tabaei BP, Rundle AG, Wu WY, et al. Associations of residential socioeconomic, food, and built environments with glycemic control in persons with diabetes in New York City from 2007-2013. Am J Epidemiol 2018;187:736–45. 10.1093/aje/kwx300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hager ER, Cockerham A, O'Reilly N, et al. Food swamps and food deserts in Baltimore City, MD, USA: associations with dietary behaviours among urban adolescent girls. Public Health Nutr 2017;20:2598–607. 10.1017/S1368980016002123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Travert A-S, Sidney Annerstedt K, Daivadanam M. Built environment and health behaviors: Deconstructing the black box of interactions-a review of reviews. Int J Environ Res Public Health 2019;16. 10.3390/ijerph16081454. [Epub ahead of print: 24 04 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stokols D, Allen J, Bellingham RL. The social ecology of health promotion: implications for research and practice. Am J Health Promot 1996;10:247–51. 10.4278/0890-1171-10.4.247 [DOI] [PubMed] [Google Scholar]
- 43.American Diabetes Association Professional Practice Committee . 10. cardiovascular disease and risk management: standards of medical care in Diabetes-2022. Diabetes Care 2022;45:S144–74. 10.2337/dc22-S010 [DOI] [PubMed] [Google Scholar]
- 44.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US department of agriculture automated Multiple-Pass method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32. 10.1093/ajcn/88.2.324 [DOI] [PubMed] [Google Scholar]
- 45.Subar AF, Freedman LS, Tooze JA, et al. Addressing current criticism regarding the value of self-report dietary data. J Nutr 2015;145:2639–45. 10.3945/jn.115.219634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention . Diabetes basics: quick facts 2021, 2022. Available: https://www.cdc.gov/diabetes/basics/type2.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2022-003033supp001.pdf (86.6KB, pdf)
bmjdrc-2022-003033supp002.pdf (142.1KB, pdf)
bmjdrc-2022-003033supp003.pdf (44KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Data for the NHANES are publicly available at https://wwwn.cdc.gov/nchs/nhanes/.