Abstract
Objectives:
Fentanyl has come to dominate the U.S. illicit opioid supply. We aimed to characterize and examine correlates of preferences for fentanyl vs. other opioids among individuals starting OUD treatment.
Methods:
We interviewed 250 adults initiating buprenorphine treatment with positive fentanyl toxicology at intake. We characterized opioid preferences and examined bivariate associations between opioid preference (preference for heroin, fentanyl, heroin-fentanyl mix, or other opioid) and sociodemographic characteristics, psychosocial factors, and substance use behaviors. We then used multinomial logistic regression to examine factors independently associated with fentanyl preferences.
Results:
Over half (52.0 %) of participants preferred fentanyl (21.2 % fentanyl alone, 30.8 % heroin-fentanyl mix). In bivariate comparisons, participants who preferred fentanyl were a higher acuity group with respect to risks and problems in general. In the multinomial logistic regression, people who preferred fentanyl, either alone or mixed with heroin, used non-prescribed buprenorphine less in the 30 days preceding treatment entry compared to people who preferred heroin or other opioids (RRRalone= 0.88 [0.78, 0.99]; P = 0.037 and RRRmixed= 0.91 [0.84, 0.99]; P = 0.046). People who preferred fentanyl alone were also younger (RRR= 0.93 [0.90, 0.97]; P < 0.001) and more likely to have severe mental illness (RRR= 2.5 [1.1, 5.6]; P = 0.027) than people who prefer heroin or other opioids.
Conclusions:
Many people with OUD report preferring fentanyl. People who express preference for fentanyl differ substantively from those with other opioid preferences, and may be at elevated risk for poor health outcomes. Understanding preferences surrounding fentanyl could inform treatment and harm reduction interventions.
Keywords: Fentanyl preference, Opioid use disorder, Buprenorphine treatment
1. Background
Drug overdose is the leading cause of injury-related death in the United States (Anon, 2020). More than 100,000 people in the U.S. died from drug overdose during the 12-month period ending in April 2021, a record high and nearly 30 % increase from the previous year (Centers for Disease Control and Prevention, 2021b). Opioids were involved in approximately 75 % of overdose deaths during this time period, and synthetic opioids, primarily illicitly manufactured fentanyl (IMF) and its analogues, were the most common opioids involved, accounting for an estimated 64,774 deaths (Anon, 2022).
While misused fentanyl may originate from pharmaceutical fentanyl, which is prescribed by doctors to treat severe pain, most cases of fentanyl-related overdose are linked to IMF, which is often synthesized in clandestine laboratories and distributed through illegal drug markets (Anon, 2021). IMF primarily enters the drug supply as an adulterant, making opioids cheaper and more powerful. It is often added to heroin, mixed with stimulants such as cocaine, or pressed into counterfeit medication tablets (Ciccarone, 2017; Rothberg and Stith, 2018). However, IMF is increasingly being used as a solo product, which may be a reflection of increased opioid tolerance requiring stronger drugs and/or more frequent use (Ciccarone et al., 2017; Daniulaityte et al., 2019; Foglia et al., 2021). Fentanyl’s high potency, which is approximately 50–100 times that of morphine (Centers for Disease Control and Prevention, 2021a), significantly increases the risk of overdose, especially when people unknowingly take fentanyl-adulterated drugs and when there is variable purity in the drug supply (Ciccarone, 2017; Rothberg and Stith, 2018).
Several studies have documented fentanyl market penetration and shifts in drug preferences. Ethnographers conducted an assessment among 38 people who inject drugs in Massachusetts and New Hampshire and presented a heroin typology to describe “types” of heroin available on the streets: heroin alone, fentanyl alone, and heroin-fentanyl mix. This study found that people are trying to discern these substances and their preferences for each form vary (Ciccarone et al., 2017). Other studies have documented how the physiological effects of using heroin compare to fentanyl (Mars et al., 2018a; Mayer et al., 2018; Zibbell et al., 2021) and how people who use drugs have endorsed a number of ways to distinguish heroin from IMF (Daniulaityte et al., 2019) and adopted drug sampling strategies to determine drug ingredients and strength, such as snorting, smoking, tasting the drug prior to injecting, or doing a “tester shot” with small doses (Mars et al., 2018b).
As fentanyl continues to drive the overdose epidemic, several recent studies have emerged examining the extent to which individuals who use drugs are exposed to fentanyl, characteristics associated with exposure, and intentional versus unintentional exposure. Estimates of fentanyl exposure have increased over time and varied across different geographic and sociodemographic populations. Several studies have detected high rates of fentanyl exposure using urine toxicology testing (Amlani et al., 2015; Carroll et al., 2017; Gryczynski et al., 2019; Hayashi et al., 2018; Kenney et al., 2018; Mackay et al., 2021), and studies that used surveys or mixed-methods found that awareness of exposure was common (Amlani et al., 2015; Carroll et al., 2017; Gryczynski et al., 2019; Kilwein et al., 2018; Macmadu et al., 2017; Palamar et al., 2019). These studies have also identified several characteristics associated with fentanyl exposure, including younger age (Hayashi et al., 2018), lower education (Kenney et al., 2018), use of drugs by injection (Hayashi et al., 2018; Kenney et al., 2018; Macmadu et al., 2017), use of other drugs (primarily heroin, but also cocaine, buprenorphine, and amphetamines) (Hayashi et al., 2018; Kenney et al., 2018; Macmadu et al., 2017), overdose experiences (Macmadu et al., 2017), prior addiction treatment, and poorer mental health (Gryczynski et al., 2019).
Recent studies in the U.S. have also examined the extent to which people who use drugs actively seek fentanyl and characteristics associated with people who prefer fentanyl (PPF). Studies have found high rates of fentanyl preference: 31 % (39/125) of people who inject drugs in Greensboro, North Carolina preferred fentanyl (Peiper et al., 2019); 45 % (51/114) of patients at a community opioid use disorder (OUD) treatment program in Baltimore, Maryland had a preference for fentanyl (Gryczynski et al., 2019); 40 % (24/60) of people who use drugs in Dayton, Ohio said they would prefer street fentanyl over heroin (Daniulaityte et al., 2019); and 18 % (169/954) of AIDS Linked to the Intravenous Experience (ALIVE) study participants in Baltimore, Maryland who recently used fentanyl reported being more likely to buy heroin they knew was laced with fentanyl than standard heroin (Buresh et al., 2019). While these studies did not examine correlates of fentanyl preference, another study among people in three large cities who illicitly used heroin or prescription opioids found 27 % (83/308) preferred fentanyl, and fentanyl preference was associated with non-Hispanic White identification, younger age, daily illicit drug use, and overdose ≥ 1 year ago (Morales et al., 2019). Another study from 2018 among rural people who inject drugs and who report having ever used fentanyl in West Virginia found a preference for drugs containing fentanyl was prevalent among 43 % (135/311) of the study sample and associated with being younger, female, and increased drug use (Mazhnaya et al., 2020). People who use fentanyl report a more intense “rush” and the ability to overcome opioid tolerance as key benefits of fentanyl (Ciccarone et al., 2017).
While these studies have laid important groundwork for fentanyl preferences research, there are still many gaps in the literature. For example, studies have not examined correlates of fentanyl preferences among treatment-seeking or in-treatment populations, who often differ from non-treatment seeking or out-of-treatment populations across several demographic and clinical factors (Ray et al., 2017; Schwartz et al., 2008). Understanding fentanyl preferences among these populations is important as there have been reports of chronic fentanyl exposure posing distinct challenges for medication treatment, such as by complicating buprenorphine induction (Shearer et al., 2022; Varshneya et al., 2022). Additionally, the extent to which people prefer to use fentanyl alone or mixed with heroin, and whether characteristics differ between these drug preferences, has not been previously studied and is important for developing interventions that address the risks unique to these subgroups. As the fentanyl crisis rapidly evolves and continuously changes the risk environment and awareness (Ciccarone, 2017; Jones et al., 2020), it is critical to expand research on fentanyl preferences to inform harm reduction and treatment practices. Implications of such research may include more targeted naloxone distribution and overdose prevention services, promotion of fentanyl testing kits, development of safe injection facilities, and perhaps modified dosing of medications for OUD.
The emerging research demonstrates how the influx of fentanyl in the drug supply have shifted individuals’ drug preferences. In addition to the elevated risk of mortality, preference for the highly potent opioid may place individuals at an increased risk of treatment discontinuation, OUD recurrence, and other harms. In the current study, we sought to characterize fentanyl preferences and examine their correlates among new admissions to a community OUD treatment program. We hypothesize that PPF will be a higher acuity group with respect to behavioral and psychosocial problems and report a higher propensity for risktaking compared to people with preference for non-fentanyl opioids. Findings from this study may be used to guide intervention design and services for this high-risk population.
2. Methods
2.1. Study site
This study was conducted at a non-profit community OUD treatment program in Baltimore, Maryland. The program offers a continuum of addiction treatment including withdrawal management/buprenorphine induction, high and low intensity residential treatment, highly intensive and standard outpatient and mental health/psychiatric treatment. The majority of patients have public insurance, present with severe OUD, and receive buprenorphine.
2.2. Recruitment
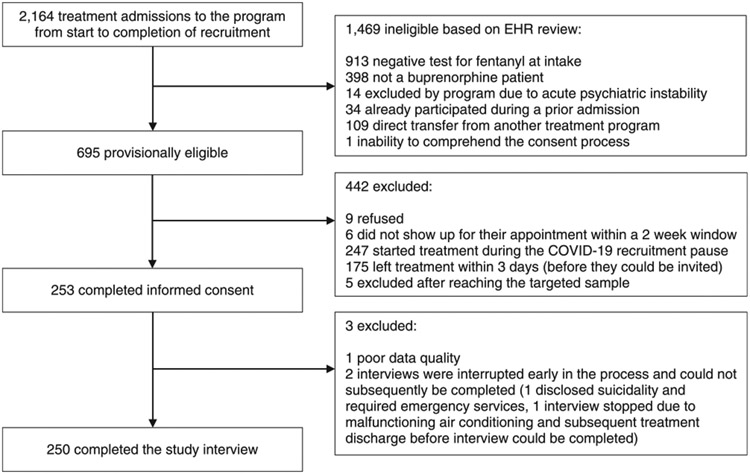
Inclusion criteria included: age 18 or older, admitted to OUD treatment with buprenorphine, positive onsite urine laboratory assay test for fentanyl at intake, and willingness to provide informed consent. Treatment with buprenorphine was an inclusion criterion because this is the standard of care at the recruitment site. Fentanyl exposure was an inclusion criterion to efficiently target the PPF subgroup of interest and allow their comparison with patients exposed to fentanyl unintentionally. Patients with a positive fentanyl test were invited to meet with research staff to learn about the study. For patients who were interested and eligible, research staff completed an informed consent process and structured assessment. Recruitment and participation occurred from December 2019 to July 2021. Recruitment was paused in March 2020 due to disruptions caused by the onset of the COVID-19 pandemic. Recruitment resumed in October 2020, but interviews were conducted virtually using televideo. The recruitment flow is shown in Fig. 1. REDCap was used for data collection. Participants received $30 for completing the one-time assessment. This study was approved by the Western Institutional Review Board.
Fig. 1.
Flow of participant recruitment.
2.3. Measures
Fentanyl preference ranking. The main variable of interest is whether the participant expressed a preference for fentanyl over other opioids. Procedures and phrasing for assessing participants’ preferences were informed by pilot work conducted by our team. Our intention was to gauge preferences prior to the participants’ current treatment episode. Participants were asked “When you were in active addiction and using opioids, what was your preferred opioid of choice?” Participants were asked to rank the following opioids in order from most preferred to least preferred: (1) heroin alone, (2) fentanyl alone, (3) heroin-fentanyl mix, and (4) other opioid. Preferences for fentanyl combined with nonopioids (e.g., stimulants) were not assessed. Participants were then asked a series of questions about the reasons for their preferences and could modify their rankings at the conclusion of that discussion. For the current analysis, the final ranking was used.
Other measures of fentanyl preferences and experiences. As an additional gauge of preference, participants were also asked the question used by Morales et al. (2019) to indicate their agreement with the statement “I prefer drugs with fentanyl in them” (strongly disagree, somewhat disagree, somewhat agree, strongly agree; Morales et al., 2019). We also asked participants if someone wanted to get drugs containing fentanyl on the street, how difficult they would be to get, and contrariwise, if someone wanted to get heroin without fentanyl on the street, how difficult it would be to get, on a Likert scale from 1 (very difficult) to 4 (very easy). Lastly, we asked individuals who believed they had enough experience with both heroin and fentanyl to compare the euphoric effect and withdrawal experiences of heroin to fentanyl.
Sociodemographic characteristics. Demographic information included age, gender, race, ethnicity, education level, employment, and health insurance status. Using questions from the Addiction Severity Index-Lite (ASI-Lite), we also collected information on relationship status, homelessness, family and other social conflicts, engagement in criminal activity for profit, and criminal justice involvement. We selected these measures from the Lite version of the ASI to minimize participant response burden and to avoid collecting extraneous information.
Mental Health and Psychosocial functioning. We used the Kessler K6 Psychological Distress Scale to assess general (i.e., non-specific) psychological distress in the prior 30 days (Kessler et al., 2002). The K6 has 6 questions about anxiety and depressive systems and is scored using a 5-level response scale, ranging from 0 (none of the time) to 4 (all of the time); this generates a scoring scale with a range of 0–24. K6 scores were dichotomized using the validated cut-point of ≥ 13 to define severe mental illness (Kessler et al., 2003). Impulsiveness was assessed using the Barratt Impulsiveness Scale, 11th edition (BIS-11) (Stanford et al., 2009), a measure of general impulsiveness widely used in research and clinical settings. The BIS-11 is composed of 30 items describing common impulsive or non-impulsive (for reverse scored items) behaviors and preferences. Items are scored on a 4-level scale, ranging from 1 (rarely/never) to 4 (almost always/always), resulting in a scoring scale with a range of 30–120. BIS-11 scores were dichotomized based on a literature review that suggests a total score ≥ 72 be used to classify an individual as highly impulsive (Stanford et al., 2009). We also assessed 3 domains of social functioning using the Texas Christian University Client Evaluation of Self and Treatment (CEST) scales: hostility, risk taking, and social support (Anon, 2010). These three social functioning domains have been shown to predict drug use among people with OUD (Aklin et al., 2009; Dobkin et al., 2002; Rao et al., 2004). The CEST scores for each domain range from 10 to 50 and are based on 7–9 items with 5-category responses (1 =strongly disagree to 5 =strongly agree).
Substance use characteristics and preferences. Using the ASI-Lite, we collected information on the frequency of use for alcohol, cocaine, amphetamines, illicit opioids (heroin, fentanyl) and non-prescribed methadone and buprenorphine in the 30 days prior to treatment entry. We also assessed polysubstance use, whether they ever injected any drugs, number of lifetime opioid overdoses, and use of naloxone using project-specific questionnaires.
2.4. Statistical analysis
Descriptive statistics of the study sample as a whole and stratified by the 4 opioid preference groups are presented. We first examined bivariate associations between opioid preference and candidate sociodemographic characteristics, psychosocial measures, and substance use behaviors using Person’s chi-square test, Fisher’s exact test, and one-way analysis of variance (ANOVA). We then fit a multinomial logistic regression model to discern which patient-level factors were independently associated with fentanyl preference. We combined the groups of people who prefer non-fentanyl opioids (i.e., people who prefer heroin alone or other opioids), and compare them to (1) people who prefer fentanyl alone and (2) people who prefer fentanyl mixed with heroin. All variables that were statistically significant in the bivariate associations were included in the regression model, except variables that conceptually overlap with preferences for fentanyl (i.e., the frequency of heroin or other illicit opioid use and opinions about the high and withdrawal from fentanyl). While not significant in bivariate analyses, gender was also included in regression models because of its significance in prior fentanyl preferences research (Mazhnaya et al., 2020). We tested for multicollinearity between variables included in the regression model by measuring the variance inflation factor. Relative risk ratios (RRRs) and 95 % confidence intervals (CIs) are reported, and statistical significance was determined as P ≤ 0.050. All statistical analyses were conducted using Stata/SE 17.0.
3. Results
3.1. Descriptive statistics of study sample
In total, 250 patients with OUD completed the one-time assessment. Among these, 103 (41 %) preferred heroin alone, 53 (21 %) preferred fentanyl alone, 77 (31 %) preferred a heroin-fentanyl mix, and 17 (7 %) preferred another opioid. Thus, there were 130 (52 %) PPF, either alone or in mixed with heroin, and 120 (48 %) people who prefer heroin or other opioids. We found a similar prevalence of 53 % (n = 132) for fentanyl preference using the Morales et al. (2019) question. There were no significant differences in opioid preferences between the 70 (28 %) individuals who participated in-person prior to the COVID-19 shutdown, and the 180 (72 %) who participated virtually. Table 1 presents sociodemographic characteristics overall and among each opioid preference category. Among the 250 participants, 185 (74 %) were male, 149 (60 %) were Black, and the mean (SD) age was 42.9 (11.6) years. Approximately one-third (n = 78, 31 %) did not have a high school diploma or GED and only 4 individuals (2 %) were employed at baseline. Among the total sample, 247 (99 %) said if someone wanted to get drugs containing fentanyl on the street it would be very easy or somewhat easy, and 220 (88 %) said if someone wanted to get heroin without fentanyl on the street it would be very difficult or somewhat difficult (Table 2).
Table 1.
Sociodemographic characteristics and correlates of opioid preferences.
| Sociodemographic Characteristics | Total (N = 250), n ( %) |
Heroin (n = 103), n ( %) |
Fentanyl (n = 53), n ( %) |
Heroin-Fentanyl Mix (n = 77), n ( %) |
Other Opioid (n = 17), n ( %) |
P-value |
|---|---|---|---|---|---|---|
| Age, mean (SD) | 42.9 (11.6) | 48.4 (11.4) | 38.2 (10.3) | 40.7 (10.1) | 34.6 (8.3) | < 0.001* |
| 18–24 | 6 (2.4) | 2 (1.9) | 3 (5.7) | 0 (0.0) | 1 (5.9) | |
| 25–34 | 69 (27.6) | 14 (13.6) | 22 (41.5) | 25 (32.5) | 8 (47.1) | |
| 35–44 | 59 (23.6) | 17 (16.5) | 12 (22.6) | 24 (31.2) | 6 (35.3) | |
| 45–54 | 63 (25.2) | 35 (34.0) | 12 (22.6) | 15 (19.5) | 1 (5.9) | |
| ≥ 55 | 53 (21.2) | 35 (34.0) | 4 (7.6) | 13 (16.9) | 1 (5.9) | |
| Male | 185 (74.0) | 82 (79.6) | 42 (79.3) | 49 (63.6) | 12 (70.6) | 0.080 |
| Race | ||||||
| White | 76 (30.5) | 23 (22.3) | 23 (43.4) | 25 (32.9) | 5 (29.4) | 0.030* |
| Black | 149 (59.8) | 73 (70.9) | 26 (49.1) | 42 (55.3) | 8 (47.1) | |
| Other or Multiple | 24 (9.6) | 7 (6.8) | 4 (7.6) | 9 (11.8) | 4 (23.5) | |
| Hispanic or Latino | 11 (4.4) | 2 (1.9) | 3 (5.7) | 4 (5.3) | 2 (11.8) | 0.178 |
| HS Diploma/ GED or higher | 172 (68.8) | 70 (68.0) | 36 (67.9) | 54 (70.1) | 12 (70.6) | 0.989 |
| Employed | 4 (1.6) | 3 (2.9) | 1 (1.9) | 0 (0.0) | 0 (0.0) | 0.513 |
| Marital Status | ||||||
| Married | 14 (5.6) | 5 (4.9) | 2 (3.8) | 7 (9.1) | 0 (0.0) | 0.209 |
| Never married | 171 (68.4) | 68 (66.0) | 38 (71.7) | 56 (72.7) | 9 (52.9) | |
| Separated, Divorced, or Widowed | 65 (26.0) | 30 (29.1) | 13 (24.5) | 14 (18.2) | 8 (47.1) | |
| Has Health Insurance | 237 (94.8) | 99 (96.1) | 52 (98.1) | 72 (93.5) | 14 (82.4) | 0.082 |
| Currently homeless | 107 (42.8) | 42 (40.8) | 30 (56.6) | 29 (37.7) | 6 (35.3) | 0.138 |
| Lives with someone who has an alcohol problem | 42 (16.8) | 18 (17.5) | 10 (18.9) | 13 (16.9) | 1 (5.9) | 0.709 |
| Lives with someone who has a drug problem | 92 (36.8) | 33 (32.0) | 16 (30.2) | 35 (45.5) | 8 (47.1) | 0.154 |
| Days in the past 30, had serious conflicts with family, mean (SD) | 2.4 (6.7) | 2.1 (6.7) | 4.2 (9.2) | 1.8 (5.0) | 1.8 (3.1) | 0.183 |
| Days in the past 30, had serious conflicts with other people (excluding family), mean (SD) | 1.9 (5.4) | 1.5 (4.8) | 1.4 (4.2) | 2.7 (7.0) | 1.8 (4.4) | 0.425 |
| Currently on probation or parole | 62 (24.8) | 20 (19.4) | 14 (26.4) | 20 (26.0) | 8 (47.1) | 0.100 |
| Months of lifetime spent incarcerated, mean (SD) | 67.0 (88.6) | 82.2 (106.8) | 54.1 (61.9) | 63.4 (82.9) | 31.8 (33.2) | 0.073 |
| Days in the past 30, engaged in illegal activities for profit, mean (SD) | 11.9 (13.5) | 8.8 (12.8) | 15.8 (13.9) | 13.8 (13.5) | 9.6 (12.0) | 0.008* |
| Severe mental illness | 114 (45.6) | 36 (35.0) | 31 (58.5) | 39 (50.7) | 8 (47.1) | 0.028* |
| Highly impulsive | 146 (58.4) | 51 (49.5) | 38 (71.7) | 48 (62.3) | 9 (52.9) | 0.048* |
| Hostility score, mean (SD) | 27.5 (8.0) | 25.8 (7.6) | 27.5 (7.9) | 29.1 (8.1) | 30.8 (9.2) | 0.014* |
| Risk-taking score, mean (SD) | 34.5 (7.3) | 32.4 (7.4) | 36.9 (6.6) | 35.3 (7.1) | 36.7 (6.9) | 0.001* |
| Social support score, mean (SD) | 38.0 (6.8) | 39.0 (6.6) | 37.0 (7.1) | 37.2 (7.0) | 39.0 (5.1) | 0.207 |
Notes: Values are expressed as column percentages. Person’s chi-square test of independence was used for categorical variables with cell sizes > 5, Fisher’s exact test was used for categorical variables with cell sizes < 5, and one-way analysis of variance (ANOVA) was used for continuous variables.
Statistically significant (P < 0.05) SD=Standard Deviation, HS=High School, GED=General Educational Development
Table 2.
Fentanyl experiences and opinions by opioid preference groups.
| Fentanyl opinions | Total (N = 250), n (%) |
Heroin (n = 103), n (%) |
Fentanyl (n = 53), n ( %) |
Heroin-Fentanyl Mix (n = 77), n ( %) |
Other Opioid (n = 17), n ( %) |
P-value |
|---|---|---|---|---|---|---|
| Difficulty of getting drugs containing fentanyl on the street if they wanted to | ||||||
| Very difficult or somewhat difficult | 3 (1.2) | 1 (1.0) | 1 (1.9) | 1 (1.3) | 0 (0.0) | 1.00 |
| Very easy or somewhat easy | 247 (98.8) | 102 (99.0) | 52 (98.1) | 76 (98.7) | 17 (100.0) | |
| Difficulty of getting heroin without fentanyl on the street if they wanted | ||||||
| Very difficult or somewhat difficult | 220 (88.0) | 92 (89.3) | 46 (86.8) | 67 (87.0) | 15 (88.2) | 0.962 |
| Very easy or somewhat easy | 30 (12.0) | 11 (10.7) | 7 (13.2) | 10 (13.0) | 2 (11.8) | |
| Feel the effects of fentanyl faster than heroin1 | 151 (70.9) | 55 (63.2) | 36 (80.0) | 53 (74.7) | 7 (70.0) | 0.197 |
| Feel the high of fentanyl is stronger than heroin1 | 198 (93.0) | 76 (87.4) | 45 (100.0) | 68 (95.8) | 9 (90.0) | 0.020* |
| Feel the high of fentanyl is better than heroin1 | 101 (47.4) | 13 (14.9) | 35 (77.8) | 48 (67.6) | 5 (50.0) | < 0.001* |
| Feel the effects of fentanyl last longer than heroin1 | 89 (41.8) | 24 (27.6) | 19 (42.2) | 40 (56.3) | 6 (60.0) | 0.002* |
| Feel the withdrawal from fentanyl starts sooner than heroin2 | 108 (58.1) | 45 (60.8) | 28 (65.1) | 30 (50.0) | 5 (55.6) | 0.431 |
| Feel the withdrawal from fentanyl is more severe than heroin2 | 144 (77.4) | 55 (74.3) | 34 (79.1) | 48 (80.0) | 7 (77.8) | 0.873 |
Notes: Values are expressed as column percentages. Person’s chi-square test of independence was used for categorical variables with cell sizes > 5, Fisher’s exact test was used for categorical variables with cell sizes ≤ 5, and one-way analysis of variance (ANOVA) was used for continuous variables.
Among the 213 individuals who believed they had enough experience with both heroin and fentanyl to compare their effects
Among the 186 individuals who believed they had enough experience with both heroin and fentanyl to compare their withdrawals
Statistically significant (P < 0.05)
3.2. Characteristics associated with opioid preference
People who preferred heroin were significantly older (mean age 48.4 years) than people who preferred fentanyl alone, the fentanyl-heroin mix, or other opioids (P < 0.001). Compared to people who preferred heroin or other opioids, both fentanyl preference groups (alone or mixed with heroin) were more likely to be White (P = 0.030), have a severe mental illness (P = 0.028), be highly impulsive (P = 0.048), and reported more days of engaging in illegal activities for profit (P = 0.008). People who preferred heroin scored lower than all other opioid preference groups for general risk-taking (P = 0.001) and hostility (P = 0.014) measures.
Table 3 compares substance use behaviors and experiences between opioid preference groups. Compared to people who preferred heroin or other opioids, both fentanyl preference groups (alone or mixed with heroin) reported more days of cocaine use (P = 0.004) and poly-substance use (P = 0.042) on average, but fewer days of non-prescribed buprenorphine use (P = 0.038).
Table 3.
Substance use behaviors by opioid preference groups.
| Substance use behaviors | Total (N = 250), n ( %) |
Heroin (n = 103), n( %) |
Fentanyl (n = 53), n ( %) |
Heroin- Fentanyl Mix (n = 77), n ( %) |
Other Opioid (n = 17), n ( %) |
P-value |
|---|---|---|---|---|---|---|
| Days of substance use in the past 30, mean (SD) | ||||||
| Alcohol | 5.8 (10.2) | 7.0 (11.1) | 4.4 (8.9) | 5.3 (9.9) | 5.8 (10.1) | 0.457 |
| Heroin or other illicit opioid | 23.5 (9.0) | 22.9 (9.9) | 24.9 (7.0) | 25.7 (7.2) | 13.2 (9.5) | < 0.001* |
| Non-Rx Methadone | 0.82 (3.4) | 0.67 (3.2) | 0.74 (2.2) | 0.94 (3.6) | 1.5 (6.3) | 0.790 |
| Non-Rx Buprenorphine | 1.5 (4.6) | 1.8 (5.6) | 0.77 (3.1) | 0.94 (2.6) | 4.1 (7.1) | 0.038* |
| Cocaine | 13.4 (12.8) | 12.0 (12.7) | 14.3 (12.1) | 16.5 (13.2) | 5.3 (8.5) | 0.004* |
| Amphetamines | 0.39 (2.5) | 0.21 (1.2) | 0.58 (3.0) | 0.44 (3.4) | 0.59 (2.4) | 0.814 |
| Polysubstance | 17.9 (11.7) | 16.9 (12.2) | 19.0 (11.0) | 19.9 (11.6) | 11.9 (9.6) | 0.042* |
| Ever injected any drugs | 98 (39.2) | 35 (34.0) | 27 (50.9) | 31 (40.3) | 5 (29.4) | 0.183 |
| Times treated for substance use disorder in their lifetime, mean (SD) | 5.8 (5.4) | 5.3 (4.6) | 7.4 (7.1) | 5.8 (5.2) | 4.5 (4.1) | 0.101 |
| Days in the past 30, experienced drug problems (e.g., craving, not being able to stop, withdrawal symptoms), mean (SD) | 23.0 (11.3) | 21.2 (12.4) | 25.7 (9.1) | 23.4 (11.3) | 23.5 (10.1) | 0.121 |
| Number of opioid overdoses in lifetime,1 mean (SD) | 4.5 (7.2) | 4.4 (7.9) | 5.6 (7.4) | 4.4 (6.9) | 2.5 (2.6) | 0.476 |
| Ever given naloxone to someone else to revive them from an opioid overdose | 134 (53.6) | 45 (43.7) | 34 (64.1) | 44 (57.1) | 11 (64.7) | 0.053 |
| Regularly carry naloxone during period of active addiction | 157 (62.8) | 61 (59.2) | 37 (69.8) | 50 (64.9) | 9 (52.9) | 0.469 |
Notes: Values are expressed as column percentages. Person’s chi-square test of independence was used for categorical variables with cell sizes > 5, Fisher’s exact test was used for categorical variables with cell sizes ≤ 5, and one-way analysis of variance (ANOVA) was used for continuous variables.
One outlier was excluded for reporting 420 opioid overdoses
Statistically significant (P < 0.05) SD=Standard Deviation, Rx=Prescribed
Among the 250 participants, 213 (85 %) believed they had enough experience with both heroin and fentanyl to compare their effects. People in both fentanyl preference groups (alone or mixed with heroin) were more likely than people who preferred heroin or other opioids to report that the high from fentanyl is stronger (P = 0.020) and better (P < 0.001) than the high from heroin (Table 2). Additionally, people who preferred heroin were less likely than people with other opioid preferences to report that the effects of fentanyl last longer than heroin (P = 0.002). There were no statistically significant differences in withdrawal experiences across opioid preference groups.
3.3. Characteristics independently associated with fentanyl preference
Results of the multinomial logistic regression model are presented in Table 4. Compared to people who prefer heroin or other opioids, people who prefer fentanyl alone were younger (RRR=0.93; 95 % CI: 0.90–0.97; P < 0.001), more likely to have severe mental illness (RRR=2.5; 95 % CI: 1.1–5.6; P = 0.027), and less likely to use non-prescribed buprenorphine (RRR=0.88; 95 % CI: 0.78–0.99; P = 0.037). Similarly, people who prefer fentanyl mixed with heroin were younger than people who prefer heroin or other opioids (RRR=0.96; 95 % CI: 0.93–0.99; P = 0.008) and less likely to use non-prescribed buprenorphine (RRR=0.91; 95 % CI: 0.84–0.99, P = 0.046).
Table 4.
Results of the multinomial logistic regression models predicting fentanyl preference status.
| Characteristic | People who prefer fentanyl alone (n = 53), relative to people who prefer other opioids (n = 120) |
People who prefer fentanyl mixed with heroin (n = 77), relative to people who prefer other opioids (n = 120) |
||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted RRR | Adjusted |
Unadjusted RRR | Adjusted |
|||||
| RRR | 95 % CI | P-value | RRR | 95 % CI | P-value | |||
| Age | 0.94 | 0.93 | 0.90–0.97 | < 0.001* | 0.96 | 0.96 | 0.93–0.99 | 0.008* |
| Gender | ||||||||
| Female | Referent | Referent | – | – | Referent | Referent | – | – |
| Male | 0.95 | 0.68 | 0.27–1.7 | 0.419 | 2.1 | 1.6 | 0.75–3.3 | 0.233 |
| Race | ||||||||
| White | Referent | Referent | – | – | Referent | Referent | – | – |
| Black | 0.39 | 0.63 | 0.28–1.4 | 0.269 | 0.58 | 0.72 | 0.34–1.5 | 0.383 |
| Other or Multiple | 0.44 | 0.28 | 0.07–1.1 | 0.072 | 0.92 | 0.76 | 0.25–2.3 | 0.638 |
| Days in the past 30, engaged in illegal activities for profit | 1.0 | 1.0 | 0.99–1.0 | 0.872 | 1.0 | 1.0 | 0.99–1.0 | 0.685 |
| Severe mental illness | 2.4 | 2.5 | 1.1–5.6 | 0.027* | 1.8 | 1.6 | 0.78–3.1 | 0.211 |
| Highly impulsive | 2.5 | 1.5 | 0.62–3.6 | 0.368 | 1.7 | 1.0 | 0.50–2.1 | 0.957 |
| Risk-taking score | 1.1 | 1.0 | 0.98–1.1 | 0.152 | 1.0 | 1.0 | 0.97–1.1 | 0.486 |
| Hostility score | 1.0 | 0.97 | 0.93–1.0 | 0.294 | 1.0 | 1.0 | 0.97–1.1 | 0.573 |
| Days in the past 30, cocaine use | 1.0 | 1.0 | 0.97–1.1 | 0.616 | 1.0 | 1.0 | 0.99–1.1 | 0.138 |
| Days in the past 30, non-Rx Buprenorphine | 0.92 | 0.88 | 0.78–0.99 | 0.037* | 0.94 | 0.91 | 0.84–0.99 | 0.046* |
| Days in the past 30, polysubstance use | 1.0 | 1.0 | 0.96–1.1 | 0.731 | 1.0 | 1.0 | 0.97–1.0 | 0.741 |
Note: For this analysis, people who prefer other opioids include those who prefer heroin alone or other opioids.
Statistically significant (P < 0.05) RRR=Relative Risk Ratio, CI=Confidence Interval, Rx=Prescribed
4. Discussion
4.1. Principal findings
The current study characterized fentanyl preferences and its correlates among individuals entering OUD treatment. To our knowledge, this is the first study to do so in a sample entering treatment during the current U.S. opioid overdose epidemic that is fueled by IMF. We found that over half of participants expressed a preference for fentanyl as their opioid of choice; 21 % preferred fentanyl alone and 30 % preferred fentanyl mixed with heroin. The prevalence found in this study may be higher than that reported by other studies because our sample was limited to people with confirmed fentanyl exposure rather than a broader population of people who use drugs (Buresh et al., 2019; Daniulaityte et al., 2019; Mazhnaya et al., 2020; Morales et al., 2019; Peiper et al., 2019). However, prior research by our team at the same study site demonstrated that a high proportion (39 %) of patients entering OUD treatment had recently been exposed to fentanyl (Gryczynski et al., 2019). Thus, this study’s findings have important implications for public health strategies to address OUD and overdose.
Results from this study demonstrate that PPF may represent a higher acuity subpopulation of people who use drugs with more severe disease characteristics than people who prefer heroin or other opioids. We found that PPF, either alone or mixed with heroin, were less likely to use non-prescribed buprenorphine. This novel finding supports recent reports documenting precipitated withdrawal in patients recently exposed to fentanyl who are initiating buprenorphine treatment (Antoine et al., 2021; Silverstein et al., 2019; Varshneya et al., 2022). While experiences of buprenorphine-precipitated withdrawal leading individuals to avoid buprenorphine treatment have been documented (Spadaro et al., 2022), the current study demonstrates that PPF may also avoid non-prescribed buprenorphine, potentially influencing individuals’ self-treatment attempts, treatment seeking behaviors, and harm reduction practices. This finding also has important implications for OUD treatment, indicating that patients’ opioid preferences may influence treatment decisions, such as OUD medication choices. More research is needed to elucidate the relationship between patient’s preference for fentanyl and their preference and response to OUD treatment.
Another novel finding was how PPF alone were more likely to have severe mental illness than people who prefer heroin or other opioids. This finding supports the well-established relationships between increased substance use problems and poor mental health (Conway et al., 2006), and suggests a potentially higher demand for integrated substance use and mental health treatment services among PPF. The lack of association between severe mental illness and preference for the fentanyl-heroin mix may reflect an increased severity of illness among people exclusively using fentanyl. This hypothesis is supported by the descriptive statistics demonstrating that compared to people who prefer the mix, PPF alone are more likely to be homeless and to have ever injected drugs, and experienced more lifetime opioid overdoses, lifetime OUD treatment attempts, impulsive behaviors, serious conflicts with family, and acute drug problems such as cravings, not being able to stop, and withdrawal symptoms. These findings suggest that PPF alone may be at even greater risk of poor health outcomes than people who prefer the fentanyl-heroin mix and have important implications for OUD treatment, such as potentially needing higher intensity OUD treatment services and/or modified dosing of medications for OUD.
We also found that preference for fentanyl, either alone or mixed with heroin, was independently associated with being younger, which is consistent with the two prior studies by Morales et al. (2019) and Mazhnaya et al. (2020) that examined correlates of fentanyl preference. This may be an indication of younger people adapting to the fentanyl-saturated drug market in the early stages of their drug use, as prior research demonstrates that opioid use initiation and preference reflect changes in supply (Cicero et al., 2018; Novak et al., 2016). Because of this saturation of fentanyl in the drug supply, and consequently the reduced supply of non-adulterated heroin and prescription opioids, younger cohorts may be less likely than older cohorts to have even tried heroin or other opioids. Furthermore, younger age groups are more likely than older age groups to have inaccurate perceptions about their risk of overdose and other adverse health outcomes, which may increase their willingness to use fentanyl intentionally. Overdose prevention and other harm reduction interventions should specifically target young persons who use drugs and consider their unique subgroup risks.
4.2. Limitations
The main study limitation is generalizability. This study sample was drawn from a single site and limited to people entering OUD treatment, who may be more risk averse and have different preferences for drugs than individuals not seeking or never in treatment. Nevertheless, this study fills an important gap in the literature on characteristics and correlates of fentanyl preferences among people initiating OUD treatment who use fentanyl either intentionally or unintentionally. This study was geared towards identifying potential relationships meriting future investigation, and we did not adjust for conducting multiple bivariate tests which could inflate Type 1 error. Another limitation is the cross-sectional nature of the study. Thus, we were unable to establish causality or temporality between fentanyl preferences and behaviors or examine how patient characteristics are associated with changes in drug preferences over time.
5. Conclusions
While some people who use drugs view fentanyl as an undesirable adulterant in the heroin supply, a large proportion of people state a preference for fentanyl. PPF may be characterized by unique sociodemographic traits and behavioral tendencies, particularly younger age, decreased use of non-treatment buprenorphine, and increased prevalence of severe mental illness. In general, people who prefer fentanyl appear to be a higher acuity population on several dimensions and interventions that mitigate risks among PPF are urgently needed. Understanding patients’ opioid preferences can inform harm reduction and OUD treatment services.
Funding
NIH/NIDA R21DA047580
Role of funding source
The funders had no role in the study design; collection, analysis, and interpretation of data; writing of this manuscript; and decision to submit the article for publication.
Abbreviations:
- PPF
People who prefer fentanyl
- OUD
Opioid use disorder
- IMF
Illicitly manufactured fentanyl
Footnotes
Conflicts of interest
The authors have no conflicts of interest to disclose.
AUTHOR DISCLOSURES The authors make the following disclosures that are unrelated to the present study: JG is part owner of COG Analytics LLC and has received research funding from Indivior (paid to his institution and including project-related salary support). JG and RPS were investigators on a NIDA-funded study receiving in-kind medication from Indivior and Alkermes. RPS has consulted for Verily Life Sciences.
References
- Aklin WM, Tull MT, Kahler CW, Lejuez CW, 2009. Risk-taking propensity changes throughout the course of residential substance abuse treatment. Personal. Individ. Differ 46 (4), 454–459. 10.1016/j.paid.2008.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, Buxton JA, 2015. Why the FUSS (Fentanyl Urine Screen Study)? a cross-sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm Reduct. J 12, 54. 10.1186/s12954-015-0088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AnonTCU Institute of Behavioral Research. 2010. TCU ADOL SOCFORM: Scales and Item Scoring Guide. ⟨http://ibr.tcu.edu/wp-content/uploads/2014/01/TCU-ADOL-SOC-sg.pdf⟩.
- AnonCenters for Disease Control and Prevention. 2020, October 1). Opioid Overdose ∣ Drug Overdose ∣ CDC Injury Center. ⟨https://www.cdc.gov/drugoverdose/index.html⟩.
- AnonDrug Enforcement Administration. 2021). 2020 National Drug Threat Assessment. ⟨https://www.dea.gov/sites/default/files/2021-02/DIR-008-21%202020%20National%20Drug%20Threat%20Assessment_WEB.pdf⟩.
- AnonCenters for Disease Control and Prevention. 2022, January 6). Vital Statistics Rapid Release—Provisional Drug Overdose Data. ⟨https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm⟩.
- Antoine D, Huhn AS, Strain EC, Turner G, Jardot J, Hammond AS, Dunn KE, 2021. Method for successfully inducting individuals who use illicit fentanyl onto buprenorphine/naloxone. Am. J. Addict 30 (1), 83–87. 10.1111/ajad.13069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buresh M, Genberg BL, Astemborski J, Kirk GD, Mehta SH, 2019. Recent fentanyl use among people who inject drugs: results from a rapid assessment in Baltimore, Maryland. Int. J. Drug Policy 74, 41–46. 10.1016/j.drugpo.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll JJ, Marshall BDL, Rich JD, Green TC, 2017. Exposure to fentanyl-contaminated heroin and overdose risk among illicit opioid users in Rhode Island: A mixed methods study. Int. J. Drug Policy 46, 136–145. 10.1016/j.drugpo.2017.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2021a, October 2). Fentanyl. Opioids ⟨https://www.cdc.gov/opioids/basics/fentanyl.html⟩.
- Centers for Disease Control and Prevention. (2021b, November 17). Drug Overdose Deaths in the U.S. Top 100,000 Annually. ⟨https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm⟩.
- Ciccarone D, 2017. Fentanyl in the US heroin supply: a rapidly changing risk environment. Int. J. Drug Policy 46, 107–111. 10.1016/j.drugpo.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciccarone D, Ondocsin J, Mars S, 2017. Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin. Int. J. Drug Policy 46, 146–155. 10.1016/j.drugpo.2017.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicero TJ, Kasper ZA, Ellis MS, 2018. Increased use of heroin as an initiating opioid of abuse: further considerations and policy implications. Addict. Behav 87, 267–271. 10.1016/j.addbeh.2018.05.030. [DOI] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF, 2006. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on alcohol and related conditions. J. Clin. Psychiatry 67 (2), 247–257. 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Daniulaityte R, Carlson RR, Juhascik MP, Strayer KE, Sizemore IE, 2019. Street fentanyl use: experiences, preferences, and concordance between self-reports and urine toxicology. Int. J. Drug Policy 71, 3–9. 10.1016/j.drugpo.2019.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobkin PL, De CM, Paraherakis A, Gill K, 2002. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction 97 (3), 347–356. 10.1046/j.1360-0443.2002.00083.x. [DOI] [PubMed] [Google Scholar]
- Foglia R, Cooperman N, Mattern D, Borys S, Kline A, 2021. Predictors of intentional fentanyl use: market availability vs consumer demand. Int. J. Drug Policy 95, 103403. 10.1016/j.drugpo.2021.103403. [DOI] [PubMed] [Google Scholar]
- Gryczynski J, Nichols H, Schwartz RP, Mitchell SG, Hill P, Wireman K, 2019. Fentanyl exposure and preferences among individuals starting treatment for opioid use disorder. Drug Alcohol Depend. 204, 107515 10.1016/j.drugalcdep.2019.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi K, Milloy M-J, Lysyshyn M, DeBeck K, Nosova E, Wood E, Kerr T, 2018. Substance use patterns associated with recent exposure to fentanyl among people who inject drugs in Vancouver, Canada: a cross-sectional urine toxicology screening study. Drug Alcohol Depend. 183, 1–6. 10.1016/j.drugalcdep.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Bekheet F, Park JN, Alexander GC, 2020. The evolving overdose epidemic: synthetic opioids and rising stimulant-related harms. Epidemiol. Rev 42 (1), 154–166. 10.1093/epirev/mxaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Anderson BJ, Conti MT, Bailey GL, Stein MD, 2018. Expected and actual fentanyl exposure among persons seeking opioid withdrawal management. J. Subst. Abus. Treat 86, 65–69. 10.1016/j.jsat.2018.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, Zaslavsky AM, 2002. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med 32 (6), 959–976. 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand S-LT, Manderscheid RW, Walters EE, Zaslavsky AM, 2003. Screening for serious mental illness in the general population. Arch. Gen. Psychiatry 60 (2), 184–189. 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Kilwein TM, Hunt P, Looby A, 2018. A descriptive examination of nonmedical fentanyl use in the united states: characteristics of use, motives, and consequences. J. Drug Issues 48 (3), 409–420. 10.1177/0022042618765726. [DOI] [Google Scholar]
- Mackay L, Kerr T, Fairbairn N, Grant C, Milloy M-J, Hayashi K, 2021. The relationship between opioid agonist therapy satisfaction and fentanyl exposure in a Canadian setting. Addict. Sci. Clin. Pract 16 (1), 26. 10.1186/s13722-021-00234-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmadu A, Carroll JJ, Hadland SE, Green TC, Marshall BDL, 2017. Prevalence and correlates of fentanyl-contaminated heroin exposure among young adults who use prescription opioids non-medically. Addict. Behav 68, 35–38. 10.1016/j.addbeh.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Ondocsin J, Ciccarone D, 2018a. Sold as heroin: perceptions and use of an evolving drug in Baltimore, MD. J. Psychoact. Drugs 50 (2), 167–176. 10.1080/02791072.2017.1394508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars SG, Ondocsin J, Ciccarone D, 2018b. Toots, tastes and tester shots: User accounts of drug sampling methods for gauging heroin potency. Harm Reduct. J 15, 26. 10.1186/s12954-018-0232-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer S, Boyd J, Collins A, Kennedy MC, Fairbairn N, McNeil R, 2018. Characterizing fentanyl-related overdoses and implications for overdose response: findings from a rapid ethnographic study in Vancouver, Canada. Drug Alcohol Depend. 193, 69–74. 10.1016/j.drugalcdep.2018.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazhnaya A, O’Rourke A, White RH, Park JN, Kilkenny ME, Sherman SG, Allen ST, 2020. Fentanyl preference among people who inject drugs in West Virginia. Subst. Use Misuse 55 (11), 1774–1780. 10.1080/10826084.2020.1762653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales KB, Park JN, Glick JL, Rouhani S, Green TC, Sherman SG, 2019. Preference for drugs containing fentanyl from a cross-sectional survey of people who use illicit opioids in three United States cities. Drug Alcohol Depend. 204, 107547 10.1016/j.drugalcdep.2019.107547. [DOI] [PubMed] [Google Scholar]
- Novak SP, Bluthenthal R, Wenger L, Chu D, Kral AH, 2016. Initiation of heroin and prescription opioid pain relievers by birth cohort. Am. J. Public Health 106 (2), 298–300. 10.2105/AJPH.2015.302972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Salomone A, Bigiarini R, Vincenti M, Acosta P, Tofighi B, 2019. Testing hair for fentanyl exposure: a method to inform harm reduction behavior among individuals who use heroin. Am. J. Drug Alcohol Abus 45 (1), 90–96. 10.1080/00952990.2018.1550652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiper NC, Clarke SD, Vincent LB, Ciccarone D, Kral AH, Zibbell JE, 2019. Fentanyl test strips as an opioid overdose prevention strategy: Findings from a syringe services program in the Southeastern United States. Int. J. Drug Policy 63, 122–128. 10.1016/j.drugpo.2018.08.007. [DOI] [PubMed] [Google Scholar]
- Rao SR, Broome KM, Simpson DD, 2004. Depression and hostility as predictors of long-term outcomes among opiate users. Addiction 99 (5), 579–589. 10.1111/j.1360-0443.2004.00686.x. [DOI] [PubMed] [Google Scholar]
- Ray LA, Bujarski S, Yardley MM, Roche DJO, Hartwell EE, 2017. Differences between treatment-seeking and non treatment-seeking participants in medication studies for alcoholism: do they matter? Am. J. Drug Alcohol Abus 43 (6), 703–710. 10.1080/00952990.2017.1312423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothberg RL, Stith K, 2018. Fentanyl: a whole new world? J. Law, Med. Ethics 46 (2), 314–324. 10.1177/1073110518782937. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Kelly SM, O’Grady KE, Peterson JA, Reisinger HS, Mitchell SG, Wilson ME, Agar MH, Brown BS, 2008. In-treatment vs. out-of-treatment opioid dependent adults: drug use and criminal history. Am. J. Drug Alcohol Abus 34 (1), 17–28. 10.1080/00952990701653826. [DOI] [PubMed] [Google Scholar]
- Shearer D, Young S, Fairbairn N, Brar R, 2022. Challenges with buprenorphine inductions in the context of the fentanyl overdose crisis: a case series. Drug Alcohol Rev. 41 (2), 444–448. 10.1111/dar.13394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein SM, Daniulaityte R, Martins SS, Miller SC, Carlson RG, 2019. “Everything is not right anymore”: buprenorphine experiences in an era of illicit fentanyl. Int. J. Drug Policy 74, 76–83. 10.1016/j.drugpo.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spadaro A, Sarker A, Hogg-Bremer W, Love JS, O’Donnell N, Nelson LS, Perrone J, 2022. Reddit discussions about buprenorphine associated precipitated withdrawal in the era of fentanyl. Clin. Toxicol 1–8. 10.1080/15563650.2022.2032730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, Patton JH, 2009. Fifty years of the barratt impulsiveness scale: an update and review. Personal. Individ. Differ 47 (5), 385–395. 10.1016/j.paid.2009.04.008. [DOI] [Google Scholar]
- Varshneya NB, Thakrar AP, Hobelmann JG, Dunn KE, Huhn AS, 2022. Evidence of buprenorphine-precipitated withdrawal in persons who use fentanyl. J. Addict. Med 10.1097/ADM.0000000000000922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Peiper NC, Duhart Clarke SE, Salazar ZR, Vincent LB, Kral AH, Feinberg J, 2021. Consumer discernment of fentanyl in illicit opioids confirmed by fentanyl test strips: lessons from a syringe services program in North Carolina. Int. J. Drug Policy 93, 103128. 10.1016/j.dmgpo.2021.103128. [DOI] [PubMed] [Google Scholar]