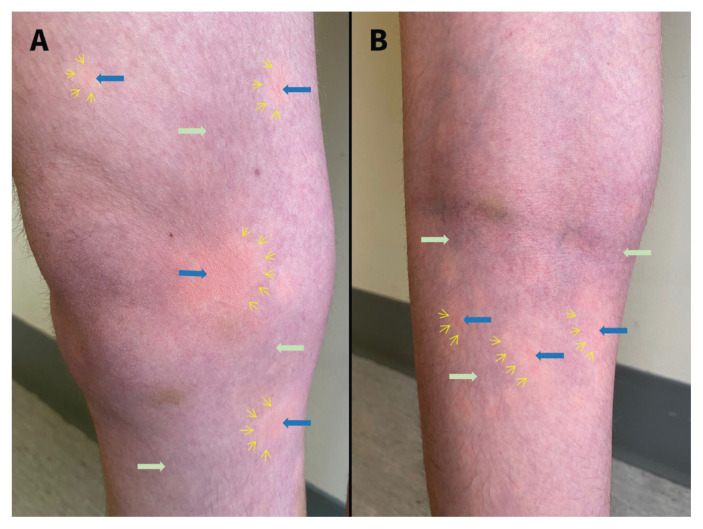
A 19-year-old woman with idiopathic gastroparesis and a jejunostomy tube presented to hospital with a recurrent pruritic eruption over the legs (Figure 1), which appeared several minutes after standing, with associated lightheadedness and weakness. The skin lesions disappeared minutes after lying down. Fourteen months previously, she had received a diagnosis of postural orthostatic tachycardia syndrome (POTS) confirmed by tilt table testing; her electrocardiogram was normal. Her symptoms were partially controlled with ivabradine and fludrocortisone. Based on the triad of morphologic features triggered by standing (Figure 1), we made a diagnosis of BASCULE (Bier anemic spots, cyanosis, and urticaria-like eruption) syndrome. We prescribed 20 mg of loratadine once daily and she reported an improvement in pruritis.
Figure 1:
Photographs of the (A) anterior and (B) posterior leg of a 19-year-old woman with the clinical triad of BASCULE (Bier anemic spots, cyanosis and urticaria-like eruption) syndrome, showing anemic white papules (yellow arrows); a cyanotic background (green arrows); and multiple red-to-orange, urticaria-like patches and thin plaques that look like oil stains with an irregular border (blue arrow).
First reported in 2016, BASCULE syndrome is an uncommon vasomotor dermatosis that occurs most frequently in females aged 12–15 years.1 It can be mistaken for urticaria, but the triad of clinical signs are differentiating and diagnostic. Bier anemic spots result from a poor venoarteriolar reflex in the dermal ascending arterioles, and the central urticaria-like lesions are secondary to mast cell degranulation induced by hypoxia.2 Cyanosis is attributed to arterial hypoxia secondary to accumulation of venous blood from standing.2 The eruption is triggered by standing but resolves with lying down or walking.1 Pruritus, pain and edema may be present and may warrant treatment.1
The importance of diagnosing BASCULE syndrome lies in its association with a spectrum of orthostatic intolerance conditions, including syncope, orthostatic hypotension and POTS (a condition associated with mast cell activation and hypermobility spectrum disorders).2,3 Less commonly, it is associated with changes detected by electrocardiography, including prolonged QT interval and first-degree atrioventricular block.1 A diagnosis of BASCULE syndrome should prompt assessment for orthostatic intolerance and electrocardiogram abnormalities. Involvement of a cardiologist and an allergist or immunologist may be considered. Limited evidence is available to guide the treatment of BASCULE syndrome. A single case report showed improvement of cutaneous symptoms with bilastine (40 mg, twice daily).2
Footnotes
Competing interests: None declared.
This article has been peer reviewed.
The authors have obtained patient consent.
References
- 1.Guillen-Climent S, Porcar Saura S, Pons Benavent M, et al. BASCULE syndrome associated with presyncopal episodes and first-degree atrioventricular block. Int J Dermatol 2021;60:e400–2. [DOI] [PubMed] [Google Scholar]
- 2.Cunningham L, Dvorakova V, Browne F, et al. High-dose bilastine for the treatment of BASCULE syndrome. Clin Exp Dermatol 2021;46:357–8. [DOI] [PubMed] [Google Scholar]
- 3.Raj SR, Fedorowski A, Sheldon RS. Diagnosis and management of postural orthostatic tachycardia syndrome. CMAJ 2022;194:E378–85. [DOI] [PMC free article] [PubMed] [Google Scholar]