Abstract
Background
Through Community Care Networks (CCNs) implemented with the VA MISSION Act, VA expanded provider contracting and instituted network adequacy standards for Veterans’ community care.
Objective
To determine whether early CCN implementation impacted community primary care (PC) appointment wait times overall, and by rural/urban and PC shortage area (HPSA) status.
Design
Using VA administrative data from February 2019 through February 2020 and a difference-in-differences approach, we compared wait times before and after CCN implementation for appointments scheduled by VA facilities that did (CCN appointments) and did not (comparison appointments) implement CCNs. We ran regression models with all appointments, and stratified by rural/urban and PC HPSA status. All models adjusted for Veteran characteristics and VA facility–level clustering.
Appointments
13,720 CCN and 40,638 comparison appointments.
Main Measures
Wait time, measured as number of days from authorization to use community PC to a Veteran’s first corresponding appointment.
Key Results
Overall, unadjusted wait times increased by 35.7 days ([34.4, 37.1] 95% CI) after CCN implementation. In adjusted analysis, comparison wait times increased on average 33.7 days ([26.3, 41.2] 95% CI, p < 0.001) after CCN implementation; there was no significant difference for CCN wait times (across-group mean difference: 5.4 days, [−3.8, 14.6] 95% CI, p = 0.25). In stratified analyses, comparison wait time increases ranged from 29.6 days ([20.8, 38.4] 95% CI, p < 0.001) to 42.1 days ([32.9, 51.3] 95% CI, p > 0.001) after CCN implementation, while additional differences for CCN appointments ranged from 13.4 days ([3.5, 23.4] 95% CI, p = 0.008) to −15.1 days ([−30.1, −0.1] 95% CI, p = 0.05) for urban and PC HPSA appointments, respectively.
Conclusions
After early CCN implementation, community PC wait times increased sharply at VA facilities that did and did not implement CCNs, regardless of rural/urban or PC HPSA status, suggesting community care demand likely overwhelmed VA resources such that CCNs had limited impact.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07800-1.
KEY WORDS: Veterans, primary, care, health, outcomes
INTRODUCTION
Untimely healthcare can lead patients to seek care in emergency departments or forgo care altogether.1 The Veterans Health Administration (VA)―the largest US health system, with over 9 million enrolled Veterans2―is experiencing increased demand for care, which is contributing to longer wait times.3–5 In part in response to this issue, Congress passed the Veterans Access, Choice, and Accountability Act (Choice Act; Public Law 113-146) in 2014,6 which allowed Veterans to use VA-purchased care in the community if wait time, or travel distance/burden for VA facility care was too great. Yet, use of community primary care (PC) in the Choice program was initially low, in part due to limited numbers of community PC providers,7, 8 and wait time for community PC was significantly longer than at VA facilities during this time.9
To improve upon the Choice Act, in 2018 Congress passed the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks Act (MISSION Act; Public Law 115-182),10 consolidating community care under the Veterans Community Care Program (VCCP) and broadening Veteran eligibility. Importantly, at a time when health plans are implementing narrow networks, steering patients to higher-value, lower-cost providers,11 the MISSION Act provisioned for new Community Care Networks (CCNs) comprising expanded networks of community providers, resulting in an increase of > 300,000 VA-contracted community providers (K. Mattocks, PhD, e-mail communication, November 2020). Furthermore, VA instituted new network adequacy standards—the ability to provide enrollees with timely access to an adequate number of in-network providers12—in CCNs13—the ability to provide enrollees with timely access to an adequate number of in-network providers. For PC, CCN network adequacy determinations are based on drive time of 30 to 60 min depending on level of rurality, and wait time of 30 days for routine appointments.14 Yet, like other health plans, VA has faced challenges setting and implementing these standards.14
Passage of the Choice and MISSION Acts has expanded VA’s role as purchaser of care. In 2021, VA allocated nearly one-quarter of its healthcare budget to purchasing community care and community care spending is estimated to reach $21.3 billion by 2022.15 Relatedly, research has documented increased demand for community care16 including PC17 among Veterans, portending new challenges and responsibilities for VA. For example, network adequacy determinations rely on the accuracy of provider directories, which are difficult to maintain and when inaccurate can lead to care delays and mask network deficiencies.18, 19 In addition, legislation mandates VA pay community providers Medicare rates, leaving VA with limited ability to regulate network adequacy through rate negotiations. Relatedly, VA facilities report strained relationships with community providers who refuse to accept VA patients.16 Compounding these issues, in rural areas where more Veterans live farther from VA facilities, initiatives to expand provider networks may be infeasible.20 Finally, because Veterans historically received most of their care at VA facilities, VA has had difficulty predicting demand for community care and targeting resources accordingly.21
To begin to assess the impact of the MISSION Act on Veteran care, we exploit a natural experiment of CCN contracting, studying whether wait time for community PC appointments changed after provider network expansions and new network adequacy standards. In addition, to explore the impact of CCNs in areas with more potential need for community care, we examine whether appointment wait times for Veterans residing in rural and PC health professional shortage areas changed after CCN implementation. Findings from this research will help purchasers including VA, providing evidence on whether larger provider networks coupled with network adequacy standards improves timeliness of care, or whether other strategies such as telehealth and subsidized transportation may be needed.
METHODS
Setting
VA has a unique community care appointment–making process (Appendix 1): First, a request or referral for community care is made.21 This is reviewed by VA staff and if eligible, the Veteran is authorized to use community care. Next, scheduling preferences are discussed with the Veteran, and VA or CCN staff schedule the appointment with a community provider. Authorizations for community care last from 3 to 12 months. If a Veteran has continued need for community care after an authorization ends, this process begins anew.
Prior to CCN implementation, community provider networks were administered by TriWest, a third-party administrator (TPA) who performed functions on behalf of VA such as scheduling appointments and paying community provider claims. With implementation of CCNs, VA now contracts with two TPAs, TriWest and Optum, which are tasked with developing and administering CCNs with transparency, accountability, quality, and in accordance with new network adequacy requirements. In addition, under CCNs, VA staff rather than TPAs are primarily responsible for scheduling community care appointments. Furthermore, VA modernized its information technology systems to reduce delays in community care eligibility determinations, appointments, and claims processing and payment.
The VA Office of Community Care developed a regional timeline for the transition from Choice-era to CCN contracts. VA facilities where CCNs are managed by Optum were the first to begin implementing CCN contacts (Appendix 2) between September and December 2019 in the Northeast; between November and December 2019 in the Midwest; and during November 2019 in the South. CCN regions managed by TriWest―the West and Alaska―were the last to implement CCN contracts in the latter half of 2020.
Data and Study Population
We used data from the VA Corporate Data Warehouse (CDW),22 Health Resources and Services Administration (HRSA),23 and University of Wisconsin School of Medicine and Public Health.24 The CDW houses information from the VA electronic health record on Veteran characteristics, health conditions, and healthcare utilization. We linked information on Veteran address in the CDW with the University of Wisconsin Area Deprivation Index file and HRSA PC and mental health professional shortage area (HPSA) files. These data were linked with VA facility–level PC coordination scores from the VA Survey of Healthcare Experiences of Patients (SHEP).25
Our study population included community PC appointments that were authorized and took place between February 1, 2019, and February 29, 2020. To reduce potential bias related to process and outcome variation between the TriWest and Optum TPAs, appointments that took place in the West and Alaska CCN regions—regions managed by TriWest TPA where CCNs were not implemented until mid- to late-2020―were excluded from this analysis, which represented about half of community PC appointments during the study period. With these exclusions, the final study population comprised 54,358 community PC appointments among 32,002 Veterans (Appendix 3).
Measures
Dependent Variable
Our dependent variable was wait time for first community PC appointment, measured as the number of days between a Veteran’s authorization for community PC and their first corresponding appointment (Steps 2 through 5, Appendix 1). If a Veteran had multiple authorizations during the study period, their first corresponding appointment after each authorization was included.
Following the approach outlined by Burgess et al. (2011), we identified PC appointments using procedure codes for PC and codes indicative of PC that could be accompanied by a PC visit (e.g., influenza immunizations, health screenings).26 To ensure appointments were for PC, we matched PC appointments to community PC authorization periods.
Independent Variables
Our main independent variables were a binary CCN appointment variable (CCN vs. comparison appointments [reference level]), a binary post-CCN implementation period variable (appointments that took place during vs. before CCN contracting [reference level]), and an interaction term for the CCN appointment and post-CCN period variables. A community care appointment was considered a CCN appointment if scheduled by a VA facility that implemented CCN contracting during the study period and a comparison appointment if scheduled by a VA facility that did not implement CCN contracting during the study period. For comparison appointments, the start of the post-CCN period was assigned as the median of the region-specific CCN contracting dates of sites that implemented CCN contracts.
Veteran-Level Covariates
Inclusion of Veteran-level covariates assigned to appointments was based on factors influencing Veteran healthcare use and appointment wait times.17, 27–33 Sociodemographic covariates included age group; sex; race; ethnicity; marital status; VA copay group; insurance coverage; and new VA enrollee status, where enrollees were considered new if they enrolled in VA after June 30, 2018. Regarding clinical covariates, we used the Elixhauser comorbidity method to calculate a risk-adjusted comorbidity score.34, 35 Geographic covariates included drive distance from Veteran residence to the nearest VA PC facility; rurality of residence; residence in a PC or mental health HPSA; and residence in a socioeconomically deprived area. Finally, we assigned VA facility–level PC coordination scores from the VA SHEP to Veterans’ appointments.25
Statistical Analyses
Descriptive statistics included frequencies and percentages for categorical variables and means and SDs for continuous variables. To compare characteristics of CCN and comparison appointments, we calculated absolute standardized mean differences (SMD) between appointments.36–38
We employed a difference-in-differences (DID) approach and appointment-level multivariable linear regression models with VA facility–level clustering to estimate the effect of CCN contracting on wait times. We examined wait times for CCN and comparison appointments before and after CCN contracting and adjusted for covariates described above. In addition, we stratified analyses by rurality (rural and urban appointments) and PC HPSA status (PC HPSA and non-PC HPSA appointments).
All analyses were performed using R version 4.0.2.39 Cluster-robust standard errors were calculated using the multiwayvcov package version 1.2.3.40 For SMD, effect sizes were determined at 0.2 = small effect, 0.5 = medium effect, 0.8 = large effect.41 Statistical significance of regression model coefficients was determined at p < 0.05. The Hines and Portland VA Research Committees approved this project.
Parallel Trends Analyses
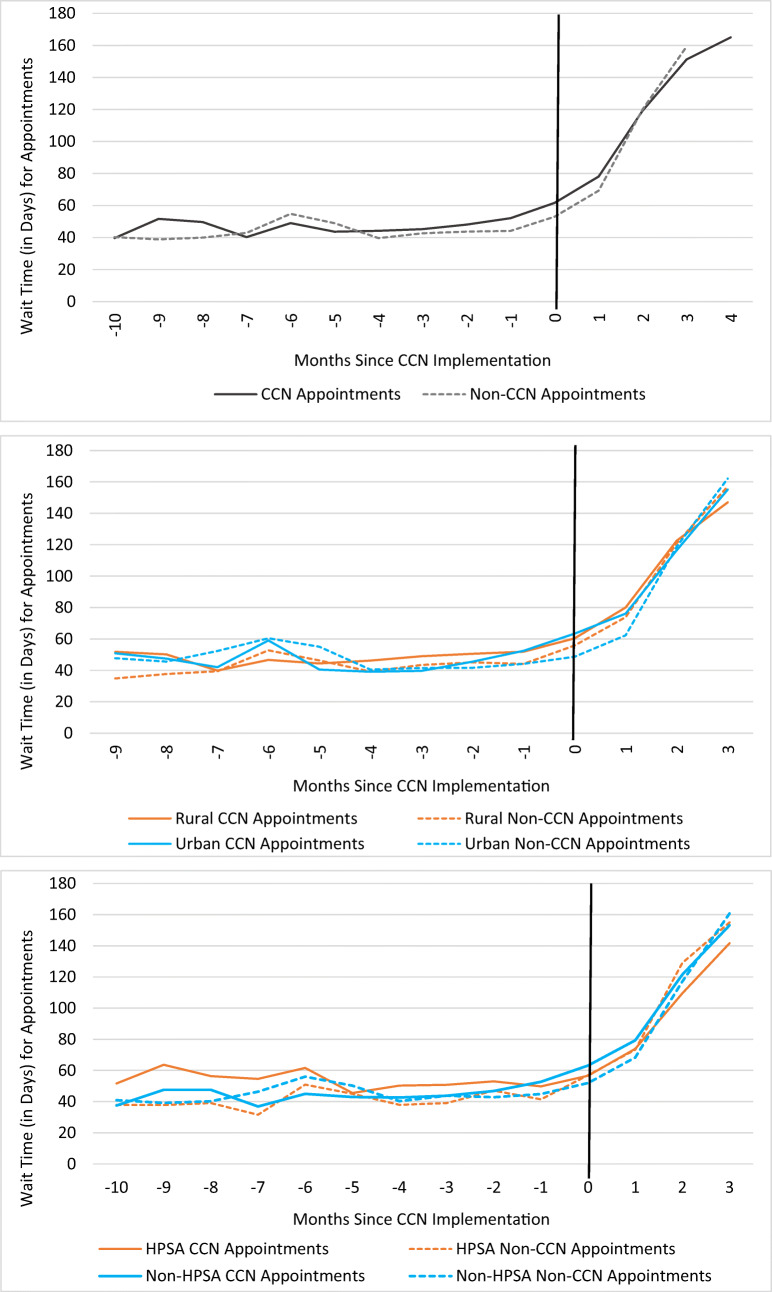
We examined the parallel trends assumption through examination of unadjusted wait times during the pre-CCN period (Fig. 1) and an appointment-level linear regression model similar to the main analysis but with a continuous month variable and an interaction term between the continuous month and CCN appointment variables. We found no evidence of differential trends in wait time between CCN and comparison appointments prior to CCN implementation (Appendix 4).
Figure 1.
Unadjusted mean wait times for community primary care appointments by CCN status and months since CCN implementation (N = 54,358 appointments), overall and by rural/urban status and primary care HPSA status. Notes: The vertical line in each plot delineates the pre- and post-CCN periods. Due to the assignment of CCN contracting dates for comparison sites, comparison sites had a maximum of 3 months of post-CCN period data, whereas CCN sites had a maximum of 5 months of post-CCN period data. Months with unstable mean wait time estimates due to small group-specific cell size (n > 20 appointments) were excluded from plots. Abbreviations: CCN, Community Care Network; HPSA, health professional shortage area.
Sensitivity Analyses
We conducted several sensitivity analyses for our overall model. First, we added Nosos score, a risk-adjustment measure that predicts healthcare costs for VA patients.42 Next, we tested the sensitivity of using the median for the assigned post-CCN period for comparison appointments, estimating models with alternative post-CCN periods. In four separate models, we assigned comparison appointments the same post period—September, October, November, or December. Finally, because some Veterans (50.2%) had multiple appointments, we tested a model that accounted for both VA facility–level and Veteran-level clustering.
RESULTS
Appointment Characteristics
During the study period, 54,358 community PC appointments took place (Table 1). Of those, about one-quarter were CCN appointments. CCN and comparison appointments were similar along most observable characteristics, and were primarily for Veterans who were older; male; white race; non-Hispanic/Latino ethnicity; married; and resided in rural areas and farther from VA PC facilities. Residence in socioeconomically deprived areas and mental health HPSAs occurred more often for comparison appointments, and VA facility–level SHEP care coordination scores were lower for comparison appointments.
Table 1.
Community Primary Care Appointment Characteristics by CCN Status (N = 54,358 appointments)
| Characteristics | All | CCN | Comparison | Test statistic |
|---|---|---|---|---|
| (N (%)) | (N (%)) | (N (%)) | (SMD) | |
| Unique appointments | 54,358 (100) | 13,720 (25.2) | 40,638 (74.8) | |
| Unique patients | 32,002 (100) | 8477 (26.5) | 23,525 (73.5) | |
| Age category | 0.04 | |||
| < 45 years | 14,030 (25.8) | 3624 (26.4) | 10,406 (25.6) | |
| 45–54 years | 8779 (16.2) | 2307 (16.8) | 6472 (15.9) | |
| 55–64 years | 12,396 (22.8) | 3152 (23.0) | 9244 (22.7) | |
| ≥ 65 years | 19,153 (35.2) | 4637 (33.8) | 14,516 (35.7) | |
| Sex: female | 6335 (11.7) | 1699 (12.4) | 4636 (11.4) | 0.03 |
| Race | 0.18 | |||
| White | 43,027 (79.2) | 10,313 (75.2) | 32,714 (80.5) | |
| Black | 8131 (15.0) | 2722 (19.8) | 5409 (13.3) | |
| Other | 3200 (5.9) | 685 (5.0) | 2515 (6.2) | |
| Ethnicity: Hispanic/Latino | 4654 (8.6) | 464 (3.4) | 4190 (10.3) | 0.28 |
| Marital status: single/unknown | 23,932 (44.0) | 6422 (46.8) | 17,510 (43.1) | 0.09 |
| VA copayment category | 0.09 | |||
| No copay | 31,750 (58.4) | 8474 (61.8) | 23,276 (57.3) | |
| Some copay | 16,458 (30.3) | 3802 (27.7) | 12,656 (31.1) | |
| Full copay | 6150 (11.3) | 1444 (10.5) | 4706 (11.6) | |
| New VA enrollee | 5125 (9.4) | 1829 (13.3) | 3296 (8.1) | 0.17 |
| Insurance status | 0.15 | |||
| VA only | 19,518 (35.9) | 5442 (39.7) | 14,076 (34.6) | |
| VA + private | 9674 (17.8) | 2161 (15.8) | 7513 (18.5) | |
| VA + Medicare/Medicaid | 16,331 (30.0) | 3637 (26.5) | 12,694 (31.2) | |
| VA + private + Medicare/Medicaid | 8835 (16.3) | 2480 (18.1) | 6355 (15.6) | |
| Elixhauser score (mean (SD)) | 6.79 (11.96) | 6.69 (12.00) | 6.83 (11.95) | 0.01 |
| Facility-level SHEP primary care coordination score | 60.19 (6.15) | 62.99 (6.67) | 59.24 (5.66) | 0.61 |
| County Average National ADI Rank (mean (SD)) | 67.89 (14.76) | 61.15 (17.96) | 70.16 (12.72) | 0.58 |
| Primary care HPSA | 12,359 (22.7) | 2930 (21.4) | 9429 (23.2) | 0.04 |
| Mental health HPSA | 32,480 (59.8) | 5359 (39.1) | 27,121 (66.7) | 0.58 |
| Rurality of residence | 0.07 | |||
| Urban | 19,464 (35.8) | 5266 (38.4) | 14,198 (34.9) | |
| Rural | 31,548 (58.0) | 7622 (55.6) | 23,926 (58.9) | |
| Highly rural | 3346 (6.2) | 832 (6.1) | 2514 (6.2) | |
| Distance to nearest VA primary care facility | 0.15 | |||
| 0–5 miles | 5692 (10.5) | 1497 (10.9) | 4195 (10.3) | |
| 6–10 miles | 6473 (11.9) | 1744 (12.7) | 4729 (11.6) | |
| 11–20 miles | 8113 (14.9) | 2313 (16.9) | 5800 (14.3) | |
| 21–40 miles | 12,044 (22.2) | 3326 (24.2) | 8718 (21.5) | |
| > 40 miles | 22,036 (40.5) | 4840 (35.3) | 17,196 (42.3) | |
Abbreviations: CCN, Community Care Network; SMD, standardized mean differences; VA, Veterans Affairs; ADI, Area Deprivation Index; HPSA, health professional shortage area; SHEP, Survey of Healthcare Experiences of Patients
Wait Times
Wait times for community PC appointments were skewed right with mean 52.2 days and median 30.0 days (data not shown), averaging 44.4 days (95% CI 43.8, 44.9) and 80.1 days (95% CI 78.9, 81.4) during the pre- and post-CCN periods, respectively (Table 2, Fig. 1). The unadjusted mean wait time for a CCN appointment was longer than for a comparison appointment in both the pre- and post-periods.
Table 2.
Wait Times for Community Primary Care Appointments, Pre- and Post-CCN Implementation
| All | CCN | Comparison | |
|---|---|---|---|
| N = 54,358 | N = 13,720 | N = 40,638 | |
| Unadjusted (mean/95% CI) | |||
| Pre-CCN | 44.4 (43.8, 44.9) | 47.4 (46.4, 48.4) | 43.4 (42.8, 44.1) |
| Post-CCN | 80.1 (78.9, 81.4) | 86.8 (84.7, 88.9) | 76.9 (75.4, 78.5) |
| Within-group difference | 35.7 (34.4, 37.1) | 39.4 (37.1, 41.8) | 33.5 (31.8, 35.1) |
| Across-group difference | 6.0 (3.3, 8.6) | ||
| Adjusted (mean/95% CI) | |||
| Pre-CCN | ― | 44.6 (36.6, 52.6) | 45.6 (36.3, 54.9) |
| Post-CCN | ― | 83.8 (75.5, 92.0) | 79.3 (68.2, 90.4) |
| Within-group difference | ― | 39.2 (33.5, 44.8) | 33.7 (26.3, 41.2) |
| Across-group difference | 5.4 (−3.8, 14.6) | ||
Notes: Adjusted means and 95% CIs are from multivariable linear regression models that adjusted for VA facility–level clustering and age category, sex, race, ethnicity, marital status, VA copayment category, new VA enrollee status, insurance status, county-level national ADI rank of Veteran residence, Veteran residence in a primary care HPSA, Veteran residence in a mental health HPSA, rurality of Veteran residence, distance to the nearest VA primary care facility from Veteran residence, VA facility–level SHEP care coordination score, and Elixhauser index
Abbreviations: CCN, Community Care Network; ADI, Area Deprivation Index; HPSA, health professional shortage area; SHEP, Survey of Healthcare Experiences of Patients
In the adjusted regression analysis, comparison appointment wait times increased on average 33.7 days ([26.3, 41.2] 95% CI, p < 0.001) after CCN implementation; there was no significant difference between CCN and comparison appointment wait times after CCN implementation (across-group mean difference: 5.4 days, [−3.82, 14.64] 95% CI, p = 0.25; Table 2; Appendix 5). In sensitivity analyses, altering our model parameters and assumptions did not materially impact these results (Appendix 6).
Wait Times by Rural/Urban Status and Primary Care HPSA Status
In the adjusted stratified analyses, rural comparison wait times increased 36.6 days ([29.6, 43.6] 95% CI, p < 0.001) after CCN implementation; there was no significant difference between rural CCN and comparison appointment wait times after CCN implementation (across-group mean difference: 0.4 days, [−10.8, 11.5] 95% CI, p = 0.95). Urban comparison wait times increased 29.6 days ([20.8, 38.4] 95% CI, p < 0.001), and urban CCN wait times an additional 13.4 days ([3.5, 23.4] 95% CI, p = 0.008; Table 3; Appendix 7) after CCN implementation.
Table 3.
Wait Time for Community Primary Care Appointments, Pre- and Post-CCN Implementation, by Rural/Urban Status
| Rural appointments | Urban appointments | |||||
|---|---|---|---|---|---|---|
| All | CCN | Comparison | All | CCN | Comparison | |
| N = 34,894 | N = 8454 | N = 26,440 | N = 19,464 | N = 5266 | N = 14,198 | |
| Unadjusted (mean/95% CI) | ||||||
| Pre-CCN | 43.7 (43.0, 44.3) | 48.1 (46.8, 49.4) | 42.3 (41.6, 43.1) | 45.7 (44.9, 46.6) | 46.0 (44.6, 47.4) | 45.6 (44.6, 46.7) |
| Post-CCN | 80.8 (79.1, 82.5) | 85.3 (82.1, 88.5) | 78.9 (76.9, 80.9) | 79.2 (77.4, 81.1) | 88.4 (85.6, 91.2) | 73.9 (71.5, 76.3) |
| Within-group difference | 37.1 (35.3, 38.9) | 37.2 (33.8, 40.7) | 36.6 (34.4, 38.7) | 33.5 (31.4, 35.5) | 42.4 (39.2, 45.5) | 28.3 (25.7, 30.9) |
| Across-group difference | 0.7 (−2.9, 4.2) | 14.1 (10.2, 18.0) | ||||
| Adjusted (mean/95% CI) | ||||||
| Pre-CCN | ― | 47.5 (39.6, 55.3) | 45.2 (37.6, 52.9) | ― | 43.3 (35.1, 51.6) | 52.4 (42.9, 61.8) |
| Post-CCN | ― | 84.5 (73.2, 95.7) | 81.8 (72.9, 90.6) | ― | 86.3 (78.4, 94.3) | 81.9 (70.3, 93.6) |
| Within-group difference | ― | 37.0 (28.3, 45.7) | 36.6 (29.6, 43.6) | ― | 43.0 (38.5, 47.5) | 29.6 (20.8, 38.4) |
| Across-group difference | 0.4 (−10.8, 11.5) | 13.4 (3.5, 23.4) | ||||
Notes: Adjusted means and 95% CIs are from multivariable linear regression models that adjusted for VA facility–level clustering and age category, sex, race, ethnicity, marital status, VA copayment category, new VA enrollee status, insurance status, county-level national ADI rank of Veteran residence, Veteran residence in a primary care HPSA, Veteran residence in a mental health HPSA, distance to the nearest VA primary care facility from Veteran residence, VA facility–level SHEP care coordination score, and Elixhauser index
Abbreviations: CCN, Community Care Network; ADI, Area Deprivation Index; HPSA, health professional shortage area; SHEP, Survey of Healthcare Experiences of Patients
PC HPSA comparison wait times increased 42.1 days ([32.9, 51.3] 95% CI, p < 0.001) after CCN implementation, and PC HPSA CCN wait times a lesser 15.1 days ([−30.1, −0.1] 95% CI, p = 0.049); non-PC HPSA comparison wait times increased 31.5 days ([23.9, 39.0] 95% CI, p < 0.001), and non-PC HPSA CCN wait times an additional 11.0 days ([2.2, 19.8] 95% CI, p = 0.014; Table 4; Appendix 8) after CCN implementation.
Table 4.
Wait Time for Community Primary Care Appointments, Pre- and Post-CCN Implementation, by Primary Care HPSA Status
| Primary care HPSA | Non-primary care HPSA | |||||
|---|---|---|---|---|---|---|
| All | CCN | Comparison | All | CCN | Comparison | |
| N = 12,359 | N = 2930 | N = 12,359 | N = 41,999 | N = 10,790 | N = 31,209 | |
| Unadjusted (mean/95% CI) | ||||||
| Pre-CCN | 43.4 (42.3, 44.5) | 52.6 (50.1, 55.1) | 40.9 (39.6, 42.2) | 44.6 (44.0, 45.2) | 46.0 (44.9, 47.0) | 44.2 (43.5, 44.9) |
| Post-CCN | 81.7 (78.9, 84.4) | 79.3 (74.7, 84.0) | 82.8 (79.4, 86.2) | 79.7 (78.3, 81.1) | 88.9 (86.5, 91.3) | 75.3 (73.6, 77.0) |
| Within-group difference | 38.3 (35.3, 41.2) | 26.8 (21.5, 32.0) | 41.9 (38.2, 45.5) | 35.0 (33.5, 36.6) | 42.9 (40.3, 45.5) | 31.1 (29.2, 32.9) |
| Across-group difference | −15.1 (−20.9, −9.3) | 11.8 (8.9, 14.8) | ||||
| Adjusted (mean/95% CI) | ||||||
| Pre-CCN | ― | 48.3 (35.8, 60.8) | 39.6 (29.2, 49.9) | ― | 43.8 (35.8, 51.8) | 47.5 (37.4, 57.6) |
| Post-CCN | ― | 75.4 (60.8, 89.9) | 81.7 (66.0, 97.4) | ― | 86.3 (78.6, 94.0) | 78.9 (67.6, 90.2) |
| Within-group difference | ― | 27.0 (15.4, 38.6) | 42.1 (32.9, 51.3) | ― | 42.5 (37.5, 47.4) | 31.5 (23.9, 39.0) |
| Across-group difference | −15.1 (−30.1, −0.1) | 11.0 (2.2, 19.8) | ||||
Notes: Adjusted means and 95% CIs are from multivariable linear regression models that adjusted for VA facility–level clustering and age category, sex, race, ethnicity, marital status, VA copayment category, new VA enrollee status, insurance status, county-level national ADI rank of Veteran residence, Veteran residence in a mental health HPSA, rurality of Veteran residence, distance to the nearest VA primary care facility from Veteran residence, VA facility–level SHEP care coordination score, and Elixhauser index
Abbreviations: CCN, Community Care Network; ADI, Area Deprivation Index; HPSA, health professional shortage area; SHEP, Survey of Healthcare Experiences of Patients
DISCUSSION
This study is among the first to examine the impact of the MISSION Act, assessing wait time for community PC appointments after early CCN implementation. We found that early CCN implementation was not associated with timelier community PC during the study period. Instead, wait times increased significantly and similarly for CCN and comparison appointments after CCN implementation. In addition, although there were some differences in the magnitude of wait time increases stratified by rural/urban and PC HPSA status, wait times increased sharply for both CCN and comparison appointments after CCN implementation, ranging from approximately 30 to 40 days, which is beyond VA’s new network adequacy wait time standard for community care.
Our results are consistent with a recent Government Accountability Office (GAO) report, which showed that in some areas VA underestimated demand for community care leading to delays.21 Initially, VA assumed a 10% growth in community care referrals with VCCP implementation. However, referral growth at some VA facilities ranged from 40 to 70% between June 2019 and February 2020. Lacking accurate estimates of demand, staffing models were impacted resulting in inadequate staffing to meet even modest referral growth projections. In addition, that wait time increases were somewhat smaller for rural versus urban CCN appointments and PC HPSA versus non-PC HPSA CCN appointments—areas where fewer providers may be available for CCN expansion, but where VA may have more experience managing greater community care referral volume—is also consistent with the GAO report and suggest VA’s in/ability to manage community care demand likely contributed to our results.
Next, it is plausible that even with expanded provider networks, the number of providers furnishing VA community care may not have increased substantially and CCN directories may include inactive providers, leading to challenges scheduling appointments. This phenomenon has been observed in Medicaid managed care (MCO) networks.43, 44 For example, 25% of PC providers in Medicaid MCOs provided 86% of enrollee care from 2015 to 2017;43 and in 2018 more than half of some Medicaid MCO PC provider networks were comprised of “phantom” providers who had not seen Medicaid enrollees.44 The extent to which VA network adequacy standards may not reflect actual access to care warrants further investigation, as well as dissemination of lessons learned that may inform other public and commercial health plans.
Finally, given specialty care historically comprised most VA community care,16 priority may have been given to increasing specialist rather than PC networks. Coupled with expanded Veteran eligibility for community care, this focus on CCN specialist care may have exacerbated supply-demand disequilibrium for community PC. Future research should explore which provider types were targeted for CCN expansion and the extent to which expansion aligned with changing demand for community care, including PC.
Given the myriad consequences of delayed access to PC, including deferred care, emergency department and hospital use, and poor health outcomes,27–31 it is critical that VA carefully consider whether and when to send Veterans out for community PC. VA leaders and policymakers recognize the importance of these decisions and are developing solutions, such as transferring referral management from individual clinicians to referral teams trained to optimize provider and setting selection.45 One pilot study testing this approach for sleep medicine found VA wait times were shorter under the referral team than status quo, although testing for PC has not yet been done.45 Alternatively, proponents have suggested strategic community provider contracting based on provider performance—a strategy akin to narrow network contracting in which provider networks are curated based on quality and costs,11 one VA is currently barred from practicing.46 Each strategy assumes a different underlying mechanism for wait times, yet, each requires accurate, real-time data on community provider availability, performance, and willingness to care for Veterans.
Limitations
This study has some limitations. First, to isolate the impact of CCNs from other VA appointment–making processes that may contribute to wait times, we explored wait time as the difference between the date an appointment was scheduled and when it took place (Steps 4 through 5, Appendix 1). However, appointment scheduled dates were missing during certain periods of our study. Therefore, our measure of wait time includes both wait time attributable to CCN and other VA appointment–making factors, and does not include cancelled appointments. Although cancellations account for a small percentage of VA appointments (2.3%),47 once data are available, future research should explore the impact of CCNs on cancelled appointments. In addition, we did not have information on appointment desired dates, and as such, were unable to determine whether wait times were planned. By employing a DID approach, however, unless CCN and comparison appointments were systematically different in their scheduled or desired dates, potential bias should be minimal. Lastly, there were 5 months of post-CCN data before the COVID-19 pandemic began disrupting care. Therefore, we were unable to assess the longer-range impact of CCNs on wait times. After the pandemic subsides, it will be important to monitor community care wait times and the impact of additional experience with CCNs and new network adequacy standards.
CONCLUSION
Contrary to what architects of the MISSION Act intended, findings from our study indicate that expanded contracting with community providers and new provider network adequacy standards implemented through CCNs did not, in early stages, improve timeliness of community PC among Veterans. To develop targeted solutions, research is needed to disentangle the potential impacts of staff and process issues from community provider network issues and adequacy standards on appointment wait times. Insights from these inquiries may inform, more broadly, approaches to better estimate and manage demand for services and wait times in health plan networks.
Supplementary Information
(DOCX 251 kb)
Acknowledgements
We appreciate policy insights and data guidance from colleagues in the VA Office of Community Care, especially Clinton L. Greenstone, MD; Craig Carter; Francine Sandrow, MD; and Matthew Labo, MPA. We would also like to acknowledge Brian Bartle, MPH, and Allison O’Neill, MS, who contributed to data management for the manuscript.
Author Contribution
Drs. Diana Govier and Denise Hynes conceptualized and designed the study and drafted the initial manuscript. Mr. Alex Hickok conducted the analyses, and Mr. Hickok and Drs. Govier, Hynes, and Meike Niederhausen interpreted the data. Drs. Samuel Edwards, Frances Weaver, and Howard Gordon contributed to conceptualization and design of the study, reviewed the analyses, and critically reviewed the manuscript.
Funding
This work was supported by funding from the US Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) Service grants SDR17-155 and 18-321 (PI Dr. Hynes). Dr. Govier was supported, in part, by a VA Postdoctoral Fellowship Program Award (TPH 98-000-02). Drs. Hynes and Weaver were each supported in part by a VA Research Career Scientist Award (RCS 98-352/21-136 and RCS 98-354, respectively). Dr. Edwards was supported by a VA Career Development Award (CDA 16-152). The authors all have employment or compensation arrangements with the US Department of Veterans Affairs.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to human subjects protection requirements. Requests for summary information may be submitted to the corresponding author for consideration.
Declarations
Disclaimer
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the US Department of Veterans Affairs or the US government.
Conflict of Interest
Drs. Govier, Hynes, Edwards, Weaver, and Gordon, and Mr. Hickok are VA employees and otherwise have no conflicts of interest to report. Dr. Niederhausen was supported, in part, by a US VA HSR&D Center of Innovation (CIN) grant (CIN 13-404) during the conduct of this study (PI Steve Dobscha).
Footnotes
Prior Presentations:
This work was presented as a brief abstract at the AcademyHealth 2021 Annual Research Meeting on June 14–17, 2021.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Doty M, Shah A, Fields K, et al. Comparing Nations on Timeliness and Coordination of Health Care. Findings from the 2021 Commonwealth Fund Health Policy Survey of Older Adults. Commonwealth Fund. Available at: https://www.commonwealthfund.org/sites/default/files/2021-10/PDF_Doty_timeliness_coordination_2021_intl_survey_older_adults_chartpack_v2.pdf. Accessed 22 June 2022.
- 2.Veterans Health Administration. About VHA. Available at: https://www.va.gov/health/aboutvha.asp. July 2019. Accessed 5 Dec 2021.
- 3.Bagalman E. The Number of Veterans That Use VA Health Care Services: A Fact Sheet. Congressional Research Service; 2014. Available at: https://fas.org/sgp/crs/misc/R43579.pdf. Accessed 7 Dec 2021.
- 4.Centers for Medicare and Medicaid Services Alliance to Modernize Healthcare. Independent Assessment of the Health Care Delivery Systems and Management Processes of the Department of Veterans Affairs, Volume I: Integrated Report. McLean, VA: MITRE Corporation; 2015:168. Available at: https://www.va.gov/opa/choiceact/documents/assessments/Integrated_Report.pdf. Accessed 7 Dec 2021.
- 5.Veterans Affairs Office of Budget. FY 2017 Budget Submission. U.S. Department of Veterans Affairs; 2017. Available at: https://www.va.gov/budget/products.asp. Accessed 7 Dec 2021.
- 6.Rogers H. Veterans Access, Choice, and Accountability Act of 2014. Vol 160.; 2014:1754-1803. Available at: https://www.congress.gov/bill/113th-congress/house-bill/3230. Accessed 3 Dec 2021.
- 7.Government Accountability Office. VA Health Care, Actions Needed to Improve Newly Enrolled Veterans’ Access to Primary Care. United States Government Accountability Office; 2016. Available at: https://www.gao.gov/assets/680/675867.pdf. Accessed 16 Dec 2021.
- 8.Mattocks K, Mengeling M, Sadler A, et al. The veterans choice act: a qualitative examination of rapid policy implementation in the department of veterans affairs. Med. Care. 2017;55:s71-S75. [DOI] [PubMed]
- 9.Penn M, Bhatnagar S, Kuy S, et al. Comparison of wait times for new patients between the private sector and United States Department of Veterans Affairs Medical Centers. JAMA Netw Open. 2019;2(1):e187096. 10.1001/jamanetworkopen.2018.7096. [DOI] [PMC free article] [PubMed]
- 10.Massarweh NN, Itani KMF, Morris MS. The VA MISSION Act and the Future of Veterans’ Access to Quality Health Care. JAMA. 2020;324(4):343. 10.1001/jama.2020.4505. [DOI] [PubMed]
- 11.Delbanco S, Murray R, Berenson R, et al. Payment Methods and Benefit Designs: How They Work and How They Work Together to Improve Health Care. Narrow Networks. Urban Institute; 2016. Available at: https://www.urban.org/sites/default/files/2016/05/03/04_narrow_networks.pdf. Accessed 22 June 2022.
- 12.McCarty S, Farris M. ACA Implications for State Network Adequacy Standards. Robert Wood Johnson Foundation; 2013. Available at: http://www.Rwjf.org/content/dam/farm/21eports/issue_brief s/2013/rwjf4 07486. Accessed 22 June 2022.
- 13.Mengeling M, Mattocks K, Hynes D, et al. Partnership forum: the role of research in the transformation of veterans affairs community care. Med. Care. 2021;59(6):S232-S241. [DOI] [PMC free article] [PubMed]
- 14.Mattocks K, Elwy A, Yano E, et al. Developing network adequacy standards for VA community care. Health Serv. Res. 2021;00:1-9. [DOI] [PMC free article] [PubMed]
- 15.Government Accountability Office. VA Health Care, Additional Steps Could Help Improve Community Care Budget Estimates. Government Accountability Office; 2020. Available at: https://www.gao.gov/assets/720/710082.pdf. Accessed 25 Jan 2022.
- 16.Mattocks KM, Kroll-Desrosiers A, Kinney R, Elwy AR, Cunningham KJ, Mengeling MA. Understanding VA’s use of and relationships with community care providers under the MISSION Act. Med Care. 2021;59:S252. Doi:10.1097/MLR.0000000000001545. [DOI] [PMC free article] [PubMed]
- 17.Hynes DM, Edwards S, Hickok A, et al. Veterans’ use of Veterans Health Administration primary care in an era of expanding choice. Med Care. 2021;59:S292. 10.1097/MLR.0000000000001554. [DOI] [PMC free article] [PubMed]
- 18.Wishner J, Marks J. Ensuring Compliance with Network Adequacy Standards: Lessons From Four States. Urban Institute. 2017. Available at: www.urban.org/sites/default/files/publication/88946/2001184-ensuring-compliance-with-network-adequacy-standards-lessons-fromfour-states_0.pdf. Accessed 22 June 2022.
- 19.Haeder SF, Weimer DL, Mukamel DB. Secret shoppers find access to providers and network accuracy lacking for those in marketplace and commercial plans. Health Aff. 2016;34(7):1160-1166. [DOI] [PubMed]
- 20.Ohl ME, Carrell M, Thurman A, et al. Availability of healthcare providers for rural veterans eligible for purchased care under the Veterans Choice Act. BMC Health Serv. Res. 2018;18:315. 10.1186/s12913-018-3108-8. [DOI] [PMC free article] [PubMed]
- 21.Government Accountability Office. Veterans Community Care Program, Improvements Needed to Help Ensure Timely Access to Care. United States Government Accountability Office; 2020. Available at: https://www.gao.gov/assets/710/709689.pdf. Accessed 15 Dec 2021.
- 22.Federal Register Document 2014–01497. January 2014. Available at: https://www.govinfo.gov/content/pkg/FR-2014-01-27/pdf/2014-01497.pdf. Accessed 3 May 2021.
- 23.Health Resources & Services Adminsitration. Data Downloads. Available at: https://data.hrsa.gov/data/download. Accessed 16 April 2021.
- 24.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible — the Neighborhood Atlas. N Engl J Med. 2018;378(26):2456-2458. Doi:10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed]
- 25.VA’s Survey of Healthcare Experience of Patients. Vantage Point. January 2021. Available at: https://blogs.va.gov/VAntage/83755/vas-survey-healthcare-experience-patients/. Accessed 3 May 2021.
- 26.Burgess JF, Maciejewski ML, Bryson CL, et al. Importance of health system context for evaluating utilization patterns across systems. Health Econ. 2011;20(2):239-251. 10.1002/hec.1588. [DOI] [PubMed]
- 27.Prentice JC, Pizer SD. Delayed access to health care and mortality. Health Serv Res. 2007;42(2):644-662. 10.1111/j.1475-6773.2006.00626.x. [DOI] [PMC free article] [PubMed]
- 28.Pizer SD, Prentice JC. What are the consequences of waiting for health care in the veteran population? J Gen Intern Med. 2011;26(S2):676-682. 10.1007/s11606-011-1819-1. [DOI] [PMC free article] [PubMed]
- 29.Prentice JC, Graeme Fincke B, Miller DR, Pizer SD. Primary care and health outcomes among older patients with diabetes. Health Serv Res. 2012;47(1pt1):46-67. 10.1111/j.1475-6773.2011.01307.x. [DOI] [PMC free article] [PubMed]
- 30.Wong ES, Liu CF, Hernandez SE, et al. Longer wait times affect future use of VHA primary care. Healthcare. 2018;6(3):180-185. 10.1016/j.hjdsi.2017.07.003. [DOI] [PubMed]
- 31.Weissman J, Stern R, Fielding S, Epistein A. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med. 1991;114(4):325-331. 10.7326/0003-4819-114-4-325. [DOI] [PubMed]
- 32.Doyle JM, Streeter RA. Veterans’ location in health professional shortage areas: implications for access to care and workforce supply. Health Serv Res. 2017;52:459-480. 10.1111/1475-6773.12633. [DOI] [PMC free article] [PubMed]
- 33.Hanchate AD, Frakt AB, Kressin NR, et al. External determinants of veterans’ utilization of VA Health Care. Health Serv Res. 2018;53(6):4224-4247. 10.1111/1475-6773.13011. [DOI] [PMC free article] [PubMed]
- 34.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. 10.1097/00005650-199801000-00004. [DOI] [PubMed]
- 35.Moore BJ, White S, Washington R, Coenen N, Elixhauser A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care. 2017;55(7):698-705. 10.1097/MLR.0000000000000735. [DOI] [PubMed]
- 36.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat – Simul Comput. 2009;38(6):1228-1234. 10.1080/03610910902859574.
- 37.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083-3107. 10.1002/sim.3697. [DOI] [PMC free article] [PubMed]
- 38.Yang D, Dalton J. A Unified Approach to Measuring the Effect Size Between Two Groups Using SAS. SAS Glob Forum 2012. 2012. Available at: https://www.semanticscholar.org/paper/A-unified-approach-to-measuring-theeffect-size-two-Yang-Dalton/6cf4bd36ca4c90006a5d6563f646a391c255581b. Accessed 16 Apr 2021.
- 39.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2017. Available at: https://www.r-project.org/. Accessed 3 May 2021.
- 40.Graham A. cluster.vcov: Multi-way standard error clustering in multiwayvcov: Multi-Way Standard Error Clustering. Available at: https://rdrr.io/cran/multiwayvcov/man/cluster.vcov.html. Accessed 12 July 2019.
- 41.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. L. Erlbaum Associates; 1988.
- 42.Wagner TH, Upadhyay A, Cowgill E, et al. Risk adjustment tools for learning health systems: a comparison of DxCG and CMS-HCC V21. Health Serv Res. 2016;51(5):2002-2019. 10.1111/1475-6773.12454. [DOI] [PMC free article] [PubMed]
- 43.Ludomirsky A, Schpero W, Wallace J, et al. In medicaid managed care networks care is highly concentrated among a small percentage of physicians. Health Aff. 2022;41(5). 10.1377/hlthaff.2021.01747. [DOI] [PubMed]
- 44.Zhu JM, Charlsworth CJ, Polsky D, McConnell KJ. Phantom networks: discrepancies between reported and realized mental health care access in Oregon Medicaid. Health Aff. 2022;41(7). 10.1377/hlthaff.2022.00052. [DOI] [PMC free article] [PubMed]
- 45.Donovan LM, Palen BN, Fernandes LA, et al. The referral coordination team: a redesign of specialty care to enhance service delivery and value in sleep medicine. NEJM Catal. 2021;2(2):CAT.20.0403. 10.1056/CAT.20.0403.
- 46.Harris AHS, Beilstein-Wedel EE, Rosen AK, et al. Comparing complication rates after elective total knee arthroplasty delivered or purchased by the VA. Health Aff Proj Hope. 2021;40(8):1312-1320. 10.1377/hlthaff.2020.01679. [DOI] [PubMed]
- 47.Feyman Y, Legler A, Griffith KN. Appointment wait time data for primary & specialty care in Veterans Health Administration Facilities vs. Community Medical Centers. Data Brief. 2021;36:107134. 10.1016/j.dib.2021.107134. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 251 kb)
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available due to human subjects protection requirements. Requests for summary information may be submitted to the corresponding author for consideration.