Abstract
Background
Severally ill COVID-19 patients may require urgent transport to a specialized facility for advanced care. Prehospital transport is inherently risky; the patient’s health may deteriorate, and potentially fatal situations may arise. Hence, early detection of clinically worsening patients in a prehospital setting may enable selecting the best receiving facility, arranging for swift transportation, and providing the most accurate and timely therapies. The incidence and predictors of abrupt prehospital clinical deterioration among critically ill patients in Ethiopia are relatively limited.
Study objectives
This study was conducted to determine the incidence of sudden clinical deterioration during prehospital transportation and its predictors.
Methods
A prospective cohort study of 591 COVID-19 patients transported by a public EMS in Addis Ababa. For data entry, Epi data V4.2 and SPSS V 25 were used for analysis. To control the effect of confounders, the candidate variables for multivariable analysis were chosen using a p 0.25 inclusion threshold from the bivariate analysis. A statistically significant association was declared at adjusted relative risk (ARR) ≠ 1 with a 95 % confidence interval (CI) and a p value < 0.05 after adjusting for potential confounders.
Results
The incidence of prehospital sudden clinical deterioration in this study was 10.8%. The independent predictors of prehospital sudden clinical deterioration were total prehospital time [ARR 1.03 (95%; CI 1.00–1.06)], queuing delays [ARR 1.03 (95%; CI 1.00–1.06)], initial prehospital respiratory rate [ARR 1.07 (95% CI 1.01–1.13)], and diabetic mellitus [ARR 1.06 (95%; CI 1.01–1.11)].
Conclusion
In the current study, one in every ten COVID-19 patients experienced a clinical deterioration while an EMS provider was present. The factors that determined rapid deterioration were total prehospital time, queueing delays, the initial respiratory rate, and diabetes mellitus. Queueing delays should be managed in order to find a way to decrease overall prehospital time. According to this finding, more research on prehospital intervention and indicators of prehospital clinical deterioration in Ethiopia is warranted.
Keywords: Prehospital, Sudden clinical deterioration, COVID-19, Addis Ababa, Ethiopia
Background
Prehospital care address a diverse set of diseases or conditions including infectious diseases, noncommunicable conditions, obstetrics, and injuries [1–3]. It comprises basic strategies with proven effectiveness, such as accessible and rapid transportation, and the deployment of personnel with at least basic life-support skills [1].
Nowadays, there is an increasing need for prehospital care both in high- and low-income countries as a consequence of the global increase in the emerging and evolving burden of diseases that need emergence medical services (EMS) [1, 3, 4]. In severe cases, COVID-19 may get worse and the illness may deteriorate to acute respiratory distress syndrome (ARDS) or multiple organ failure [5–8]. So, critically ill COVID-19 patients may require emergent transport to get advanced treatment such as non-invasive ventilatory support, invasive respiratory support, or admission to an intensive care unit [9–11]. However, the transportation of critically ill patients is not risk-free, and in some cases, the shortest transport could even be led to life-threatening conditions [12–15].
Several factors can contribute to sudden clinical deterioration in the prehospital setting and adverse events during transportation are one of the leading factors [16]. An increase in total prehospital time, unstable vital signs, neurological conditions, the profession of transferring personnel, and omission of necessary interventions were among the factors contributing to prehospital clinical deterioration [1, 17, 18]. Failure to detect and provide intervention for clinically deteriorating patients during emergency care also increases the risk of adverse events during the continuum of emergency care and may lead to devastating results [18–20]. Therefore, early identification of deteriorating patients is important in preventing or reducing the risk of sudden prehospital deterioration [11].
Early identification of clinically deteriorating patients in a prehospital setting may help to choose the appropriate receiving facility, rapid transportation, and provision of the most accurate and prompt interventions [21–23]. It could also help to anticipate the involvement of the senior staff such as the emergency department or critical-care professionals in the receiving facility [23]. Moreover, it has a proven impact on improving outcomes and management of critically ill patients [24].
Although early identifications of clinically deteriorating patients in prehospital settings have the aforementioned benefits, the available study in Ethiopia only focused on the clinical deterioration of hospitalized COVID-19 patients [25]. In addition, the available studies in Ethiopia that have assessed prehospital care independent of COVID-19 were mainly focused on the prevalence of prehospital care rather than addressing the incidence of prehospital clinical deterioration, types of prehospital care provided to the patients, and predictors of sudden deterioration [26–30]. Thus, there is a dearth of literature on the incidence of sudden clinical deterioration and its predictors in the prehospital setting in Ethiopia. So, this study aimed to examine the characteristics, incidence, and predictors of sudden prehospital deterioration among COVID-19 patients transported by EMS in Addis Ababa, Ethiopia.
Methods
Study design and setting
A prospective cohort study was implemented to assess the incidence of prehospital sudden deterioration among COVID-19 patients transported by public ambulances in Addis Ababa, Ethiopia. Addis Ababa is the capital city of Ethiopia and the seat of the African Union headquarter. In response to the COVID-19 outbreak in Ethiopia, the Addis Ababa city health bureau in collaboration with the Federal Ministry of Health established emergency operating centers (EOC) to provide prehospital care services to COVID-19 patients. The city has 10 dispatch centers and one central dispatch center dedicated to providing emergency medical services to COVID-19 patients. The centers have basic and advanced ambulances equipped with essential drugs and equipment. The ambulances were also staffed with different health care professionals including general practitioners and nurses. When an emergency call is received, the closest available ambulance is sent to the place to transport the COVID-19 patient to the nearest COVID-19 centers.
Eligibility criteria
The study included all successful ambulance dispatches that transported COVID-19 patients aged 12 and up between May and August 2021. Failure to dispatch and insufficient information to determine sudden clinical deterioration during transportation to the receiving facility were exclusion criteria.
Sample size and sampling procedure
The sample size for the study was calculated using single population proportion formula with the following consideration. The level of confidence (α) was set at 0.05 (Z (1-α) = 1.96), and the margin of error was considered at 0.05. It was reported that adverse events in the prehospital setting are one of the leading factors that cause sudden clinical deterioration in the prehospital setting [16]. Thus, the proportion of adverse events in the prehospital setting among COVID-19 patients in Addis Ababa was taken as 44.2% [31]. Considering 10% for contingency and a design effect of 1.5, the calculated sample size was 625. A cohort of COVID-19 patients who met eligibility criteria and were consecutively transported between May to August 2021 by Addis Ababa’s EOC was purposively recruited to the study.
Data collection technique
The data collection tool was prepared by the investigators following reviews of previous works of literature [20, 32–34]. The data were collected by general practitioners and nurses working on the ambulance at each dispatch center in Addis Ababa. The tool consisted of information such as prehospital response time, source of EMS call, educational background of EMS providers, patients’ demographic data, clinical characteristics of the patients, and prehospital care provided to the patients.
Outcome measures
The outcome of interest was sudden clinical deterioration during the prehospital transportation. The event must have occurred between the time of departure from the referring facility or home and the time of arrival at the receiving facility. Prehospital sudden clinical deterioration was measured by evaluating a change in any of the following physiological status components from the last recorded observations to the most recent [33]. These physiological changes include (A) change in pulse rate: either a sudden increase in pulse rate of 20 beats per minute above the previous reading, or the recently recorded pulse rate of greater than 110 beats per minute, or less than 50 beats per minute [33]; (B) change in blood pressure: either a sudden drop of blood pressure of 20 mmHg or more since the last reading or a fall below 90 mmHg systolic in the recent reading [33]; (C) change in respiratory rate: either a sudden increase in respiratory rate of 10 breaths per minute above previous reading or greater than 29 breaths per minute or less than 10 per breaths minute [33]; (D) change in the conscious state: either a sudden decrease in a conscious state of 2 points in either component (eye-opening, best verbal response, best motor response) of the Glasgow Coma Scale (GCS) or a newly recorded GCS score of <13 [33, 35]; and (E) cardio-pulmonary arrest [33].
Data analysis
Epi data version 4.2 was used for data entry and SPSS version 25 was used for the analysis. Descriptive statistics such as frequency, percentage, mean, and standard deviation were used to summarize the findings, and tables and figures were used to present the information. A modified (Robust) Poisson regression was used to determine the relative risk summary metric and predictors of prehospital sudden clinical deterioration. We selected all candidate variables for multivariable analysis using a threshold for inclusion of p < 0.25 from bivariate analysis to control the effect of confounders. After adjusting for potential confounders, a statistically significant association was declared at adjusted relative risk (ARR) ≠ 1 with a 95% confidence interval (CI) and a p value less than 0.05.
Operational definitions and definitions of terms
Sudden prehospital deterioration: the patient was categorized as suddenly deteriorated if there was any change in the components of physiological parameters mentioned under the measurement section from the last recorded observations to the most recent.
Response time: the time from the emergency call until arrival at the scene [36].
On-scene time: the time from arrival at the scene until departure from the scene [36].
Total prehospital time: the time from the emergency call until hospital arrival [36].
Transport time: the time from scene departure until hospital arrival [36].
Queueing delays: refers to delays when no ambulance is available to dispatch [37].
Results
Baseline characteristics
A total of 591 patients that met eligibility criteria were included in the analyses. The mean age of the study participants was 52.4 years with a standard deviation (SD) of 17.6 years. The majority of the COVID-19 patients included in this study were within the age group of ≥65 years followed by the age group of 45–54 years, which accounts for 173 (29.3%) and 111 (18.8%), respectively. Nearly two thirds of 388 (65.7%) study participants were male. Two out of three 394 (66.7%) COVID-19 patients included in this study were transported to the treatment center by ambulances staffed by general practitioners. The majority 404 (68.4%) of the COVID-19 patients were transported from the community to COVID-19 treatment centers (Table 1).
Table 1.
Baseline characteristics of the COVID-19 patients transported by Addis Ababa’s emergency medical system, May to August 2021, Ethiopia
| Variables | Frequency | Percentage |
|---|---|---|
| Age in years | (Mean=52.4; SD=17.6) | |
| <25 | 50 | 8.5 |
| 25–34 | 53 | 9.0 |
| 35–44 | 97 | 16.4 |
| 45–54 | 111 | 18.8 |
| 55–64 | 107 | 18.1 |
| ≥65 | 173 | 29.3 |
| Sex | ||
| Male | 388 | 65.7 |
| Female | 203 | 34.3 |
| Educational status of the patients | ||
| Cannot read and write | 45 | 7.6 |
| Primary school | 160 | 27.1 |
| Secondary school | 142 | 24.0 |
| Diploma or vocational school | 127 | 21.5 |
| Bachelor degree and above | 117 | 19.8 |
| The profession of EMS provider | ||
| Nurses | 197 | 33.3 |
| General practitioner | 394 | 66.7 |
| Source of the patient | ||
| Community | 404 | 68.4 |
| Health care facility | 187 | 31.6 |
Clinical characteristics of the study participants
Of the total study participants, about 40% had a history of at least one chronic medical illness. Hypertension was the commonest 156 (26.4%) identified chronic illness among the study participants followed by diabetic mellitus 140 (23.7%). Among all patients transported by EMS provider, 121 (20.5%) had an initial prehospital systolic blood pressure of >130 mm Hg, 154 (26.1%) had an initial pulse rate of >100 beats per minute, the majority 356 (60.2%) had an initial prehospital respiratory rate of 21 to 30 per minute, nearly half 287 (47.7%) of the transported COVID-19 patients had an initial prehospital oxygen saturation of <90 percentage, while 26 (4.4%) of the patients had initial prehospital Glasgow coma scale (GCS) score of <13. Of the total transported patients, 64 (10.8%) of them experienced sudden prehospital clinical deterioration in the presence of an EMS provider. The incidence of sudden prehospital clinical deterioration identified in this study was 64 (10.8%) (Table 2).
Table 2.
Clinical profiles of the COVID-19 patients transported by Addis Ababa’s emergency medical system, May to August 2021, Ethiopia
| Variables | Frequency (n=591) | Percentage |
|---|---|---|
| Having at least one comorbid chronic illness | ||
| Yes | 234 | 39.6 |
| No | 357 | 60.4 |
| Known diabetic mellitus | ||
| Yes | 140 | 23.7 |
| No | 451 | 76.3 |
| Known hypertensive | ||
| Yes | 156 | 26.4 |
| No | 435 | 73.6 |
| History of chronic heart disease | ||
| Yes | 35 | 5.9 |
| No | 556 | 94.1 |
| Asthma or COPD | ||
| Yes | 50 | 8.5 |
| No | 541 | 91.5 |
| Living with HIV/AIDS | ||
| Yes | 18 | 3.0 |
| No | 573 | 97.0 |
| Initial prehospital systolic blood pressure in mmHg | ||
| <90 | 8 | 1.4 |
| 90–130 | 462 | 78.2 |
| >130 | 121 | 20.5 |
| Initial prehospital pulse rate in beats per minute | ||
| <60 | 6 | 1.0 |
| 60–100 | 431 | 72.9 |
| >100 | 154 | 26.1 |
| Initial prehospital respiratory rate, breaths per minute | ||
| 12–20 | 179 | 30.3 |
| 21–30 | 356 | 60.2 |
| >30 | 55 | 9.3 |
| Initial prehospital oxygen saturation in percentage | ||
| <90 | 282 | 47.7 |
| 90–94 | 180 | 30.5 |
| ≥95 | 129 | 21.8 |
| GCS | ||
| <13 | 26 | 4.4 |
| 13–15 | 565 | 95.6 |
| Prehospital sudden deterioration | ||
| Yes | 64 | 10.8 |
| No | 527 | 89.2 |
Prehospital contextual characteristics
EMS performance times are shown in Table 3. The average response time in the present study was 46.2 min with an SD of 19.6 min. For about 30.1% of the COVID-19 patients, the response time was 31 to 45 min while for approximately one in five patients, 111 (18.8%), the EMS response time took over 60 min. The mean observed on-scene time in this study was 7.5 min. In the majority of 323 (54.7%) of the transported patients, the observed on-scene time was less than 5 min. The average total prehospital time spent transporting COVID-19 patients in this study was 81.4 min with an SD of 26.4 min. Prehospital queuing delays were observed in 82 (13.9%) COVID-19 patients transported by EMS. Delays in locating the patient address were experienced in 48 (8.1%) of the study participants (Table 3).
Table 3.
Prehospital contextual characteristics of COVID-19 19 patients transported by Addis Ababa’s emergency medical system, May to August 2021, Ethiopia
| Variables | Frequency | Percentage |
|---|---|---|
| Response time in minutes | Mean=46.2; SD=19.6 | |
| ≤15 | 19 | 3.2 |
| 16–30 | 136 | 23.0 |
| 31–45 | 178 | 30.1 |
| 46–60 | 147 | 24.9 |
| >60 | 111 | 18.8 |
| On-scene time in minutes | Mean=7.5; SD=4.7 | |
| <5 | 323 | 54.7 |
| 6–10 | 179 | 30.3 |
| 11–15 | 61 | 10.3 |
| >15 | 28 | 4.7 |
| Total prehospital time in minutes | Mean=81.4; SD=26.4 | |
| ≤45 | 42 (7.1) | 7.1 |
| 46–60 | 108 | 18.3 |
| 61–75 | 122 | 20.6 |
| 76–90 | 140 | 23.7 |
| ≥90 | 179 | 30.3 |
| Queuing delays | ||
| Yes | 82 | 13.9 |
| No | 509 | 86.1 |
| Delays in locating the patient address | ||
| Yes | 48 | 8.1 |
| No | 543 | 91.9 |
| Omission of care due to lack of equipment | ||
| Yes | 152 | 25.7 |
| No | 439 | 74.3 |
| Omission of care due to lack of medication | ||
| Yes | 80 | 13.5 |
| No | 511 | 86.5 |
The prehospital interventions provided to the patients
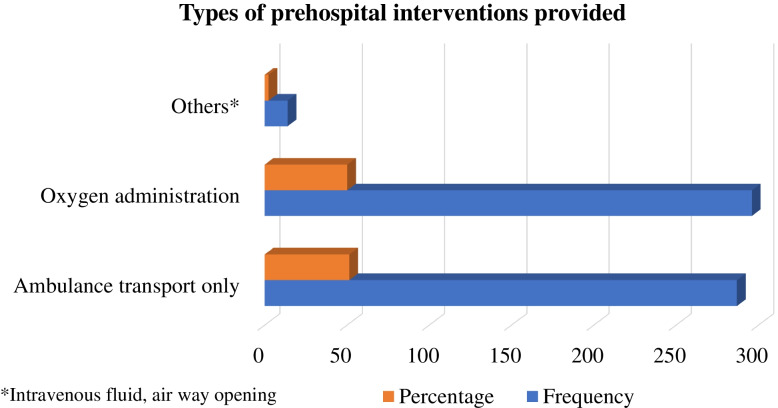
The majority of 296 (50.1%) of the patients received oxygen administration in prehospital. Meanwhile, slightly less than half of 287 (48.6%) of the patients received transportation by ambulance alone from an EMS provider (Fig. 1).
Fig. 1.
Types of prehospital intervention provided to COVID-19 patients
Determinant of prehospital sudden deterioration
We have examined the influence of possible predictive factors on prehospital sudden clinical deterioration among COVID-19 patients. Total prehospital time independently determines prehospital sudden deterioration in this study [ARR 1.03 (95%; CI 1.00–1.06)]. Implying that the risk of prehospital sudden clinical deterioration was 1.03 times greater for those COVID-19 patients who had a total prehospital time of more than 60 min compared to those transported within 1 h. Similarly, queuing delays were associated with prehospital clinical deterioration in this study after controlling for the potential confounders [ARR 1.03 (95%; CI 1.00–1.06)]. COVID-19 patients who encountered queuing delays due to shortages of an ambulance to dispatch by dispatch centers were at about a 3% increase in the risk of sudden prehospital deterioration compared to those without queuing delays (Table 4).
Table 4.
A modified Poisson regression analysis showing determinants of prehospital sudden clinical deterioration among the cohort of COVID-19 patients trasnsported by EMS, May to August 2021, Addis Ababa, Ethiopia
| Variables | Prehospital sudden deterioration | CRR (95%) CI | ARR (95%) CI | |
|---|---|---|---|---|
| Yes | No | |||
| The profession of EMS provider | ||||
| Nurses | 33 | 164 | 1 | |
| General practitioner | 31 | 363 | 0.95 (0.92–0.98) | 0.98 (0.96–1.01) |
| Response time in minutes | ||||
| ≤30 | 9 | 146 | 1 | |
| >30 | 55 | 381 | 1.04 (1.01–1.06) | 1.02 (0.99–1.04) |
| Total prehospital time in minutes | ||||
| <60 | 10 | 139 | 1 | 1 |
| ≥60 | 54 | 338 | 1.03 (1.00–1.06) | 1.03 (1.00–1.06)* |
| Queuing delays | ||||
| Yes | 24 | 58 | 1.13 (1.06–1.19) | 1.20 (1.04–1.16)** |
| No | 40 | 469 | 1 | 1 |
| Delays in locating the patient address | ||||
| Yes | 11 | 37 | 1.07 (1.00–1.15) | 1.01 (0.95–1.07) |
| No | 53 | 490 | 1 | 1 |
| The initial prehospital RR | ||||
| ≤30 breath/minutes | 52 | 483 | 1 | 1 |
| >30 breath/minutes | 12 | 43 | 1.07 (1.00–1.14) | 1.07 (1.01–1.13)* |
| Having ≥1 comorbid chronic illness | ||||
| Yes | 43 | 191 | 1.07 (1.04–1.10) | 1.01 (0.96–1.04) |
| No | 21 | 336 | 1 | 1 |
| Known diabetic | ||||
| Yes | 32 | 108 | 1.09 (1.05–1.13) | 1.06 (1.01–1.11)* |
| No | 32 | 419 | 1 | 1 |
| Known hypertensive | ||||
| Yes | 30 | 126 | 1.06 (1.03–1.10) | 1.02 (0.98–1.07) |
| No | 34 | 401 | 1 | 1 |
| Chronic heart disease | ||||
| Yes | 10 | 25 | 1.11 (1.02–1.21) | 1.03 (0.95–1.12) |
| No | 54 | 502 | 1 | 1 |
| Asthmatic or COPD | ||||
| Yes | 16 | 34 | 1.14 (1.05–1.23) | 1.07 (0.98–1.15) |
| No | 48 | 493 | 1 | 1 |
| Omission of care due to lack of medication | ||||
| Yes | 16 | 64 | 1.06 (1.01–1.11) | 1.04 (0.99–1.09) |
| No | 48 | 483 | 1 | 1 |
| Omission of care due to lack of equipment | ||||
| Yes | 27 | 125 | 1.05 (1.01–1.09) | 1.01 (0.98–1.05) |
| No | 37 | 402 | 1 | 1 |
*P < 0.05, **P <0.01, 1 reference, CRR crude relative risk, ARR adjusted relative risk, CI confidence interval
The initial prehospital respiratory rate was also independently determined prehospital clinical deterioration [ARR 1.07 (95%; CI 1.01–1.13)]. Implying that a COVID-19 patient with an initial respiratory rate of greater than 30 breaths per minute was about 7% times at increased risk of prehospital sudden clinical deterioration compared to their counterparts (Table 4). The study also found that COVID-19 patients with a history of diabetic mellitus were about 6% at higher risk of prehospital sudden clinical deterioration compared to those without a history of diabetic mellitus [ARR 1.06 (95%; CI 1.01–1.11)] (Table 4).
Although statistically significant associations were not observed on multivariate analysis, unadjusted analysis showed a significant association for the following variables: profession of EMS providers [CRR 0.95 (95%; CI 0.92–0.98)], EMS response time [CRR 1.04(95%;CI: 1.01-1.06)], delays in locating the patient address [CRR 1.07(95%; CI: 1.00-1.15)], having at least one comorbid illness [CRR 1.07(95%;CI:1.04-1.10)], hypertension [CRR 1.06 (95%; CI 1.03–1.10)], chronic heart disease [CRR 1.11 (95%; CI 1.02–1.21)], being asthmatic or COPD [CRR 1.14 (95%; CI 1.05–1.23)], omission of care due to lack of medication [CRR 1.06 (95%; CI 1.01–1.11)], and omission of care due to lack of equipment [CRR 1.05 (95%; CI 1.01–1.09)] (Table 4).
Discussion
The present study showed that more than two thirds of the patients were transported from the community to receiving facility. Contrary to this finding, a previous study conducted in the same city reported that ambulance was mainly used for inter-facility transportation of critically ill patients. According to the study, 87.6% of ambulance-utilized patients were transported between health care facilities [38]. The disparities in the finding could be attributable to the fact that the present study was conducted among COVID-19 patients, and in response to the COVID-19 outbreak in Ethiopia, there were EMS services with organized dispatch centers, manpower, and ambulances that were dedicated to transporting COVID-19 patients from the community and between facilities as opposed to the previous study.
In severe cases, COVID-19 may lead to hypoxemic respiratory failure that may meet the criteria for acute ARDS [5–7]. Independent of COVID-19, ARDS has commonly been encountered in the prehospital setting and its management involves oxygen delivery and treatments of the underlying cause [39, 40]. In this study, oxygen administration was the commonest prehospital intervention provided to COVID-19 patients in addition to ambulance transportation. Oxygen administration using a facial mask and procedures such as intravenous line and fluid administration was rare. Advanced procedures such as non-invasive airway management and prehospital intubation were not considered although there was a need for such procedures. This could be due to the fact that the scope of prehospital practice in Ethiopia is not well established and there is also a lack of resources to provide advanced intervention in the prehospital setting. This finding suggests that there is a need to consider a two-tiered ambulance system for effective prehospital care with trained manpower on basic and advanced life support. However, the use of such a system should be done with caution as such systems need accurate classification of patient severity to avoid complications and under or over triage during ambulance dispatch [41].
Ambulance response time is a basic indicator of emergency medical services across the globe [42]. In the present study, the mean emergency response time was 46.2 min. Our findings were in line with the reported perceived ambulance waiting time by the residents of Addis Ababa city in the previous study, which reported an ambulance waiting time of 40 min [30]. However, the present findings were higher than the average response times reported from Brazil and Ghana, which reported 27 and 17 min, respectively [42, 43]. A possible explanation could be that the present study focused on the transportation of critically ill COVID-19 patients and ambulance that transport COVID-19 patients may need more extra time in preparation before the ambulance gets back into the service because of additional disinfectant protocols as compared to the ambulance that transport non-COVID-19 patients. The availability of ambulances to respond to emergency calls could be another reason for the discrepancy as nearly 14% of the patients in the present study experienced queuing delays due to a shortage of ambulances to dispatch. In addition, difficulty in locating the patient’s address and a notorious delay due to road traffic are of much concern in Addis Ababa. On the other hand, the mean prehospital time in this study was 81.4 min. The present findings were in line with the findings from Accra, Ghana, which reported an average prehospital transportation time of 82 min [43]. The present findings suggest that there is a need to reduce ambulance response time and total prehospital time to nationally and internationally accepted standards.
The incidence of prehospital sudden clinical deterioration in this study was 10.8%. Our figure is higher than some findings from Australia, which used similar predefined criteria to address the sudden prehospital clinical deterioration in trauma patients [32, 33]. The difference in the advancement of the EMS system between Australia and Ethiopia could be the reason for the disparity in the findings, as the EMS system in Ethiopia is a recent phenomenon [30, 44]. In addition, treatment-seeking delay by the patients or delayed inter-hospital transfer could be another factor as a significant proportion of the patients included in this study were critically ill and had unstable vital signs before transportations.
Our findings indicate that COVID-19 patients are at higher risk of sudden clinical deterioration in prehospital settings with increasing total prehospital time. A previous study conducted among trauma patients supported our findings [34]. We also identified that an increase in EMS response time was associated with an increased risk of sudden clinical deterioration in the prehospital setting without adjusting for potential confounders. Although we could not find literature on critically ill COVID-19 patients, it was reported that longer EMS response time was associated with prehospital adverse outcomes in trauma patients [43]. Moreover, queuing delays were another factor that independently determined prehospital sudden clinical deterioration in the present study. Further studies are needed to confirm the association between EMS response time, queuing delays, and prehospital sudden clinical deterioration in critically ill patients.
Respiratory distress in COVID-19 patients was reported as a considerable challenge for the prehospital EMS [45]. In the present study, we found an independent association between an increased initial respiratory rate and prehospital sudden clinical deterioration. In agreement with our findings, increased respiratory rate was independently associated with clinical deterioration among hospitalized COVID-19 patients [46, 47]. Previous findings also reported that COVID-19 patients may even rapidly deteriorate without showing any sign of respiratory distress or with little distress, which is called silent hypoxia [48, 49]. Therefore, identification of the initial respiratory rate could help in the early detection and prevention of prehospital sudden clinical deterioration in COVID-19 patients.
Limitations
Despite the fact that this study used a prospective cohort design, the findings should be interpreted with vigilance. Variables such as transport distance, ambulance type, and COVID-19 severity level were excluded from the analysis because the majority of the data for these variables was missing. Future research incorporating the aforementioned variables may reveal a variety of findings. Besides that, this study only looked at prehospital outcomes. As a result, the current study did not investigate the relationship between prehospital characteristics and subsequent in-hospital outcomes. Further to that, the current study was conducted on COVID-19 patients and had geographical limitations because it only included public EMS in Addis Ababa. As a result, the study’s findings may be limited in their applicability to non-COVID-19 patients and other settings.
Conclusion
Prehospital clinical sudden deterioration is relatively common among COVID-19 patients in Addis Ababa, with approximately one in ten patients experiencing sudden clinical deterioration in the presence of an EMS provider. Determinants of a sudden deterioration in the prehospital setting were total prehospital time, queuing delays, the initial respiratory rate, and diabetic mellitus. Most of the predictors of sudden prehospital clinical deterioration identified in this study are modifiable and could be averted. Implementing an action to reduce total prehospital time and queuing delays should be a management objective. In addition, early identification and management of COVID-19 patients with an increased initial respiratory rate could help in reducing the risk of sudden prehospital clinical deterioration. Moreover, this finding highlights the need for further research on prehospital care and predictors of prehospital clinical deterioration in Ethiopia.
Authors’ contributions
Conceptualization: Ararso Baru Olani, Menbeu Sultan, Lemlem Beza Demisse, Micheal Alemayehu. Data curation: Ararso Baru Olani and Lemlem Beza Demisse. Formal analysis: Ararso Baru Olani and Lemlem Beza Demisse. Funding acquisition: Ararso Baru Olani, Menbeu Sultan, Lemlem Beza Demisse, Micheal Alemayehu. Investigation: Ararso Baru Olani, Menbeu Sultan, Lemlem Beza Demisse. Methodology: Ararso Baru Olani, Menbeu Sultan, Lemlem Beza Demisse. Project administration: Ararso Baru Olani. Resources: Ararso Baru Olani, Menbeu Sultan, Lemlem Beza Demisse, and Micheal Alemayehu. Software: Ararso Baru Olani and Lemlem Beza Demisse. The authors read, endorsed and approved the final manuscript.
Funding
The Ethiopian Ministry of Health funded the data collection for this research project.
Availability of data and materials
The datasets produced and/or analyzed during the current study are not publicly available even though public data sharing was not approved by the IRB, but they are available from the corresponding author (PI) upon reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval was obtained from the institutional review board (IRB) of St. Paul Hospital Millennium Medical College. Permission from the Federal Ministry of Health and respective dispatch centers was also obtained before conducting the study. Prior to data collection, the purpose, general content, and nature of the study were explained in the language preferred by the study participants, and informed consent was obtained from all participants. All procedures involved in this study have adhered to the principles of the Helsinki declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kobusingye OC, Hyder AA, Bishai D, Hicks ER, Mock C. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83(8):626–631. [PMC free article] [PubMed] [Google Scholar]
- 2.Srivastava R, Canto JG. Use of emergency medical services in acute myocardial infarction and subsequent quality of care. Cardiovasc Rev Reports. 2003;24(10):527–531. [Google Scholar]
- 3.Mehmood A, Rowther AA, Kobusingye O, Hyder AA. Assessment of pre-hospital emergency medical services in low-income settings using a health systems approach. International journal of emergency medicine. 2018;11(1):1-0. [DOI] [PMC free article] [PubMed]
- 4.Burkholder TW, Hill K, Hynes EJC. Developing emergency care systems: a human rights-based approach. Bull World Health Organ. 2019;97(9):612–619. doi: 10.2471/BLT.18.226605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan E, Beitler JR, Brochard L, Calfee CS, Ferguson ND, Slutsky AS, et al. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted? Lancet Respir Med. 2020;8(8):816–821. doi: 10.1016/S2213-2600(20)30304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020:1–10. [DOI] [PMC free article] [PubMed]
- 8.Rubin SJS, Falkson SR, Degner NR, Blish C. Clinical characteristics associated with COVID-19 severity in California. J Clin Transl Sci. 2020;(Table 2):1–4. [DOI] [PMC free article] [PubMed]
- 9.Fernandez AR, Crowe RP, Bourn S, Matt SE, Brown AL, Hawthorn AB, et al. COVID-19 preliminary case series: characteristics of EMS encounters with linked hospital diagnoses. Prehospital Emerg Care. 2020;0(0):000. doi: 10.1080/10903127.2020.1792016. [DOI] [PubMed] [Google Scholar]
- 10.Torjesen I. COVID-19: patients to use pulse oximetry at home to spot deterioration. BMJ. 2020;(October):m4151.
- 11.Docherty AB, Harrison EM, Green CA, Hardwick HE, Pius R, Norman L, et al. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: Prospective observational cohort study. BMJ. 2020;369. [DOI] [PMC free article] [PubMed]
- 12.Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020:E933–43. [DOI] [PMC free article] [PubMed]
- 13.Allen R, Wanersdorfer K, Zebley J, Shapiro G, Coullahan T, Sarani B. Interhospital transfer of critically ill patients because of coronavirus disease 19–related respiratory failure. Air Med J. 2020;000:4–7. doi: 10.1016/j.amj.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bergman LM, Pettersson ME, Chaboyer WP, Carlström ED, Ringdal ML. Safety hazards during intrahospital transport: a prospective observational study. Crit Care Med. 2017;45(10):e1043–e1049. doi: 10.1097/CCM.0000000000002653. [DOI] [PubMed] [Google Scholar]
- 15.Papson JPN, Russell KL, Taylor DMD. Unexpected events during the intrahospital transport of critically ill patients. Acad Emerg Med. 2007;14(6):574–577. doi: 10.1197/j.aem.2007.02.034. [DOI] [PubMed] [Google Scholar]
- 16.Gauss T, Ageron FX, Devaud ML, Debaty G, Travers S, Garrigue D, et al. Association of prehospital time to in-hospital trauma mortality in a physician-staffed emergency medicine system. JAMA Surg. 2019;154(12):1117–1124. doi: 10.1001/jamasurg.2019.3475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Srithong K, Sindhu S, Wanitkun N, Viwatwongkasem C. Incidence and risk factors of clinical deterioration during inter-facility transfer of critically ill patients; a cohort study. Arch Acad Emerg Med. 2020;8(1):1–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Hayward RA, Asch SM, Hogan MM, Hofer TP, Kerr EA. Sins of omission: getting too little medical care may be the greatest threat to patient safety. J Gen Intern Med. 2005;20(8):686–691. doi: 10.1111/j.1525-1497.2005.0152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stang AS, Wingert AS, Hartling L, Plint AC. Adverse events related to emergency department care: a systematic review. PLoS One. 2013;8(9). [DOI] [PMC free article] [PubMed]
- 20.Hagiwara MA, Magnusson C, Herlitz J, Seffel E, Axelsson C, Munters M, et al. Adverse events in prehospital emergency care: a trigger tool study. BMC Emerg Med. 2019;19(1):1–10. doi: 10.1186/s12873-019-0228-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kitahara O, Nishiyama K, Yamamoto B, Inoue S, Inokuchi S. The prehospital quick SOFA score is associated with in-hospital mortality in noninfected patients: a retrospective, cross-sectional study. PLoS One. 2018;13(8). [DOI] [PMC free article] [PubMed]
- 22.Maciver M. Pre-hospital use of early warning scores to improve detection and outcomes of sepsis. Br J Community Nurs. 2021;26(3):122–129. doi: 10.12968/bjcn.2021.26.3.122. [DOI] [PubMed] [Google Scholar]
- 23.Semeraro F, Corona G, Scquizzato T, Gamberini L, Valentini A, Tartaglione M, et al. New early warning score: EMS off-label use in out-of-hospital patients. J Clin Med. 2021;10(12):2617. doi: 10.3390/jcm10122617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smith GB, Prytherch DR, Schmidt PE, Featherstone PI. Review and performance evaluation of aggregate weighted “track and trigger” systems. Resuscitation. 2008;77(2):170–179. doi: 10.1016/j.resuscitation.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 25.Baker KF, Hanrath AT, van der Loeff IS, Kay LJ, Back J, Duncan CJA. National Early Warning Score 2 (NEWS2) to identify inpatient COVID-19 deterioration: a retrospective analysis. Clin Med J R Coll Physicians London. 2021;21(2):84–89. doi: 10.7861/clinmed.2020-0688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seid M, Azazh A, Enquselassie F, Yisma E. Injury characteristics and outcome of road traffic accident among victims at Adult Emergency Department of Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia: a prospective hospital based study. BMC Emerg Med. 2015;15(1):1–9. doi: 10.1186/s12873-015-0035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baru A, Azazh A, Beza L. Injury severity levels and associated factors among road traffic collision victims referred to emergency departments of selected public hospitals in Addis Ababa, Ethiopia: the study based on the Haddon matrix. BMC Emerg Med. 2019;19(1):1–10. doi: 10.1186/s12873-018-0206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gebresenbet RF, Aliyu AD. Injury severity level and associated factors among road traffic accident victims attending emergency department of Tirunesh Beijing Hospital, Addis Ababa, Ethiopia: a cross sectional hospital-based study. PLoS One. 2019;14(9):1–16. doi: 10.1371/journal.pone.0222793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Debebe F, Woldetsadik A, Laytin AD, Azazh A, Maskalyk J. The clinical profile and acute care of patients with traumatic spinal cord injury at a tertiary care emergency centre in Addis Ababa, Ethiopia. African J Emerg Med. 2016;6(4):180–184. doi: 10.1016/j.afjem.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sultan M, Abebe Y, Tsadik AW, Ababa A, Yesus AG, Mould-Millman NK. Trends and barriers of emergency medical service use in Addis Ababa, Ethiopia. BMC Emerg Med. 2019;19(1):1–8. doi: 10.1186/s12873-019-0242-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ararso Baru, Menbeu Sultan and Lemlem Beza. The status of prehospital care delivery for COVID-19 patients in Addis Ababa, Ethiopia: the study emphasizing adverse events occurring in prehospital transport and associated factors. Unpubl Rep; 2021. [DOI] [PMC free article] [PubMed]
- 32.Boyle M. Trauma patients who suddenly deteriorate in the care of paramedics: an Australian case. J Paramed Pract. 2011;3(11):638–646. [Google Scholar]
- 33.Boyle MJ, Smith EC, Archer F. A review of patients who suddenly deteriorate in the presence of paramedics. BMC Emerg Med. 2008;8:1–11. doi: 10.1186/1471-227X-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kai TR, Broady MJ, Davenport DL, Bernard AC. The effect of emergency medical system transport time on in route clinical decline in a rural system. J Trauma Acute Care Surg. 2020;88(6):734–741. doi: 10.1097/TA.0000000000002675. [DOI] [PubMed] [Google Scholar]
- 35.Majidi S, Siddiq F, Qureshi AI. Prehospital neurologic deterioration is independent predictor of outcome in traumatic brain injury: analysis from National Trauma Data Bank. Am J Emerg Med. 2013;31(8):1215–1219. doi: 10.1016/j.ajem.2013.05.026. [DOI] [PubMed] [Google Scholar]
- 36.Ageta K, Naito H, Yorifuji T, Obara T, Nojima T, Yamada T, et al. Delay in emergency medical service transportation responsiveness during the COVID-19 pandemic in a minimally affected region. Acta Med Okayama. 2020;74(6):513–520. doi: 10.18926/AMO/61210. [DOI] [PubMed] [Google Scholar]
- 37.Ingolfsson A, Budge S, Erkut E. Optimal ambulance location with random delays and travel times. Health Care Manag Sci. 2008;11(3):262–274. doi: 10.1007/s10729-007-9048-1. [DOI] [PubMed] [Google Scholar]
- 38.Sultan M, Abebe Y, Tsadik AW, Jennings CA, Mould-Millman NK. Epidemiology of ambulance utilized patients in Addis Ababa, Ethiopia. BMC Health Serv Res. 2018;18(1):1–7. doi: 10.1186/s12913-018-3820-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pandor A, Thokala P, Goodacre S, Poku E, Stevens JW, Ren S, et al. Pre-hospital non-invasive ventilation for acute respiratory failure: a systematic review and cost-effectiveness evaluation. Health Technol Assess (Rockv). 2015;19(42):1–8. doi: 10.3310/hta19420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Goodacre S, Stevens JW, Pandor A, Poku E, Ren S, Cantrell A, et al. Prehospital noninvasive ventilation for acute respiratory failure: systematic review, network meta-analysis, and individual patient data meta-analysis. Acad Emerg Med. 2014;21(9):960–970. doi: 10.1111/acem.12466. [DOI] [PubMed] [Google Scholar]
- 41.Dami F, Golay C, Pasquier M, Fuchs V, Carron PN, Hugli O. Prehospital triage accuracy in a criteria based dispatch centre. BMC Emerg Med. 2015;15(1). [DOI] [PMC free article] [PubMed]
- 42.Cabral ELDS, Castro WRS, de Medeiros Florentino DR, de Araújo Viana D, da Costa Junior JF, de Souza RP, et al. Response time in the emergency services. Acta Cir Bras. 2018;33(12):1110–1121. doi: 10.1590/s0102-865020180120000009. [DOI] [PubMed] [Google Scholar]
- 43.Mahama MN, Kenu E, Bandoh DA, Zakariah AN. Emergency response time and pre-hospital trauma survival rate of the national ambulance service, Greater Accra (January - December 2014). BMC Emerg Med. 2018;18(1). [DOI] [PMC free article] [PubMed]
- 44.Mosadeghrad AM, Gebru AA, Sari AA, Getu MA. Emergency medical services in Ethiopia: drivers, challenges and opportunities. Hum Antibodies. 2019;27(S1):S33–S41. doi: 10.3233/HAB-190368. [DOI] [PubMed] [Google Scholar]
- 45.Mæhlen JO, Mikalsen R, Heimdal HJ, Rehn M, Hagemo JS, Ottestad W. Pre-hospital critical care management of severe hypoxemia in victims of Covid-19: a case series. Scand J Trauma Resusc. Emerg Med. 2021;29(1). [DOI] [PMC free article] [PubMed]
- 46.Cecconi M, Piovani D, Brunetta E, Aghemo A, Greco M, Ciccarelli M, et al. Early predictors of clinical deterioration in a cohort of 239 patients hospitalized for COVID-19 infection in Lombardy, Italy. J Clin Med. 2020;9(5):1548. doi: 10.3390/jcm9051548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ottestad W, Seim M, Mæhlen JO. COVID-19 med stille hypoksemi. Tidsskr den Nor Laegeforening. 2020;140(7). [DOI] [PubMed]
- 49.Sheikh S, Baig MA. Silent hypoxia in COVID-19: what is old is new again! J Coll Physicians Surg Pakistan. 2020;30(1):S70–S71. doi: 10.29271/jcpsp.2020.Supp1.S70. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets produced and/or analyzed during the current study are not publicly available even though public data sharing was not approved by the IRB, but they are available from the corresponding author (PI) upon reasonable request.