Abstract
The Covid-19 pandemic required rapid scale of telemedicine as well as other digital workflows to maintain access to care while reducing infection risk. Both patients and clinicians who hadn’t used telemedicine before were suddenly faced with a multi-step setup process to log into a virtual meeting. Unlike in-person examination rooms, locking a virtual meeting room was more error-prone and posed a risk of multiple patients joining the same online session. There was administrative burden on the practice staff who were generating and manually sending links to patients, and educating patients on device set up was time-consuming and unsustainable. A solution had to be deployed rapidly system-wide, without the usual roll out across months. Our answer was to design and implement a novel EHR-integrated web application called the Switchboard, in just two weeks. The Switchboard leverages a commercial, cloud-based video meeting platform and facilitates an end-to-end virtual care encounter workflow, from pre-visit reminders to post-visit SMS text message-based measurement of patient experience, with tools to extend contact-less workflows to in-person appointments. Over the first 11 months of the pandemic, the in-house platform has been adopted across 6 hospitals and >200 practices, scaled to 8,800 clinicians who at their peak conducted an average of 30,000 telemedicine appointments/week, and enabled over 10,000–20,000 text messages/day to be exchanged through the platform. Furthermore, it enabled our organization to convert from an average of 75% of telehealth visits being conducted via telephone to 75% conducted via video within weeks.
Keywords: Innovation, Telemedicine, Connected health, Digital transformation, Health IT, Informatics
Penn Medicine needed to facilitate telemedicine encounters for patients and clinicians at the start of the Covid-19 pandemic. The dramatically increased demand for virtual visits overwhelmed the legacy video platform, requiring a replacement but also a way to meet new needs arising from a health system-wide operation. In two weeks, an internal team of clinicians and software developers engaged with frontline providers to create the Switchboard, a web platform with a suite of contextually-designed, workflow-tested, high yield tools to support digital workflows necessary for telemedical and in-person encounters. This platform has helped the organization effectively deliver >1 M telemedicine appointments in 11 months and is now used by >8,800 Penn Medicine employees/day.
1. Key takeaways
-
●
Design end-to-end experiences, not just features. Successful implementation of novel care delivery methods requires removing friction and frustration at every point along the clinician, staff, and patient journeys, not just fulfilling a checklist of features.
-
●
Embrace text messaging. Although the functionality of EHR-based patient portals may be comprehensive, simple SMS-based messaging is a more equitable primary channel for engaging patients due to its reliability, wider access, and ease of use.
-
●
Expect and enable constant evolution. To rapidly design technology that works, embed a development team in front line care—where patients meet clinicians—who can drive daily change cycles. Early deployment of changes and response to feedback is an accelerated way to get features right and inspire further innovations.
-
●
Empower decision-making on a small team. Rapid decision-making depends on ongoing collaborative group chats, ad-hoc meetings when decisions require more consensus, the use of objective data when available, and reliance on intuition and contextual insights. Design, technical, and clinical perspectives make a strong cross-functional sprint team.
2. Organizational context and problem
When the Covid-19 pandemic began and shelter-in-place orders were instituted, the need to deliver care via virtual modalities at health system scale, particularly video, arose nearly overnight. Although many video-conferencing platforms were available, including HIPAA-compliant (compliant with laws governing privacy and use of protected health information) ones already in use in our organization, none were integrated into workflow and paired with clinical encounters in the electronic health record. All required downloading an application, and none addressed language barriers contributing to disparities and inefficient care.
Penn Medicine is a Philadelphia-based academic health care system serving 6.7 million patients in six hospitals and 200 clinics primarily across two states. At the onset of the Covid-19 pandemic, we aimed to support virtual care across both the ambulatory and inpatient settings using a single platform. In the ambulatory setting, virtual video visits were primarily required for individual and group visits with clinicians. In the inpatient setting, clinicians needed to engage with patients virtually for safe and efficient consults or family meetings. We recognized the value of a single interface for all these activities.
A small core team of five clinical operations and software development roles contributed to the design, development, implementation, and wide-scale user support of the solution platform, with additional programmatic operational support supplemented by allocating and educating existing health system teams and staff. The CMIO of Penn Medicine served as the team’s executive advisor, and partners from the health system’s IS application development and electronic health record teams supported the necessary infrastructure to enable real-time APIs (application programming interfaces) with data from the EHR.
3. Solution
3.1. Launch of early operational program, and birth of a virtual care platform
Over March 14 and 15, 2020, the first weekend of the shelter-in-place order in Philadelphia, we adopted a new cloud-based video platform to support patient contact on Monday, March 16. The video conferencing software vendor was strategically selected for its low cost, high video resolution and performance, privacy compliance, and robust API and integration capabilities. Few if any vendors at that time intrinsically had all the features necessary to support virtual care workflows in practice. Over the weekend, mass licensing and sign on activations were coordinated. A telemedicine patient and clinician support center was created, and staffed internally from teams who traditionally led EHR education and optimization efforts across the health system and medical student volunteers. Two weekly enterprise-wide town halls were scheduled and broadcast live to source and distribute information.
Despite these critical early steps, the feedback from those who attempted conducting virtual clinics revealed foundational barriers: the burden of signing into a new application, manually sending patients links to custom virtual meeting rooms, and the near-impossible timing and coordination of clinicians and patients joining/leaving meetings on time. With no virtual equivalent of a waiting room, the greatest worry was that multiple patients would join the same virtual exam room at the same time. We confirmed these challenges by experiencing them ourselves--conducting our own telemedicine visits as clinicians, or as patients, and shadowing practice staff virtually.
Rather than relying on pre-covid build cycles of weeks to months, our small core team of clinicians and developers decided to take a more rapid, agile approach. We embarked on a one-week design sprint to resolve the biggest gaps by seeing first-hand the patient and clinician digital experience and testing changes to the application in real-time with our end-users. We tackled the must-haves like private, patient-specific meeting links, and single sign-on in our first iteration, but further uncovered other pain-points by monitoring patient text replies to their appointment reminders or attending our own virtual appointments. Our experience-generated insights, along with intuition and educated guesswork, guided our subsequent technical build changes, often launched to production overnight. We soft-launched a minimum viable product with a single practice and three early-adopter clinicians ready to provide feedback after every session. Their in-depth input refined the working prototype for the next 30 users, and we emerged with a minimum viable product to facilitate a schedule of unique, video visits to mirror a clinical day schedule. We called it the Switchboard to reflect our view of the need to facilitate one on one connections securely (See Fig. 1 , Table 1 ). The rapid, iterative process of development created a virtuous cycle for engaging our clinicians, who saw the impact of their input. Unprompted, they praised the process as much as the product: “Brilliant idea. It only gets better each week!”
Fig. 1.
Step-by-step workflow of a telemedicine visit.
Table 1.
Switchboard current feature set designed around user workflow and high level goals.
| Goal | Workflow needs | Supporting platform features |
|---|---|---|
| Enabling secure, private virtual connections between clinicians and patients | Automating the meeting creation process with adequate passcode lengths to meet security standards, reducing administrative burden and errors | Unique, passcode-enabled meeting links per appointment generated automatically at the time of scheduling, and expiring 24h after appointment |
| Ensuring successful patient technical setup and readiness for virtual visit | Providing staff visibility into patient setup progress Creating an escalation model of patient setup, to let practice staff time efficiently close the gaps for those most in need of hands-on support |
Reminder sent history, highlighting when delivery failed Translated versions of setup instructions with pictures and video Text bot, embedded into appointment reminder text messages, to walk patients through step by step download and setup process Visible “successfully setup“ status for patients who completed self-setup using the text bot process, AND all patients who were detected to have joined any historical meetings (prior appointments, or testing the room). Appointment notes from EHR for staff to document any manual setup outreach calls and outcome. |
| Enabling flexible troubleshooting | Ability to send meeting link directly to any phone number or email on-demand, or send to others, along with real-time two way messaging capabilities. | |
| Eliminating barriers related to app download requirement | Ability to launch web-based, app-less meetings from a link, built by video vendor | |
| Crafting a rich digital messaging experience for timely patient communication | Enabling staff to find the best, reliable channel for reaching patients – across phone, email, text | Real time, two-way text messaging feature including full patient-centric text thread, embedded language text translation, outbound and inbound popup notifications and audio chimes for staff/clinicians. Validation of mobile numbers vs landlines (not SMS-capable) Visible status when automated reminder messages failed delivery – due to landline numbers or patients who opted out of texting |
| Providing message shortcuts for frequent scenarios for improved patient clinic experience and transparency | Shortcut templated messages for use when clinician is running late Virtual waiting room message to reassure patients they are in the right place and clinician will be with them shortly Pre-visit reminders about labs or medications, option to include clinician photo |
|
| Messaging for in-person visits: Avoiding congestion and controlling patient entry from car to waiting room, reinforcing safety measures to ensure social distancing | Messaging options specific to in-person visits – shortcut to “wait in car” or “enter the building” Personalized companion passes for approved patients to be optionally attached and sent via text message for proof-of-entry. |
|
| Ensuring successful clinician navigation through clinic day | Creating an integrated platform with contextual information re: patient and day schedule that was browser-based and device agnostic | Mobile and desktop-friendly web application Single sign on to eliminate login to external vendor app Relevant contextual patient information from EHR such as medical record numbers, patient phone numbers, appointment notes, other appointments or procedures occurring the same day Verification of mobile numbers and direct link to integrating applications for anonymized calling (i.e. Doximity Dialer) QR code for easy pairing of a secondary device to conduct video visits Live participant statuses, auto-calculated meeting duration Integrated translation vendor services, two-clicks to ‘invite a translator to join meeting’, with preferred language |
| Enabling tailored workflows for unique, team-based models of care | Facilitating attending/trainee precepting workflows, group patient visits that send identical meeting link to multiple patients, multidisciplinary visits that only send reminders to the first in a series of appointments | Live meeting statuses List of other appointments for the patient that day Free text comments tagged by date and author |
Contrary to a more traditional enterprise development approach, our rapid changes unexpectedly increased trust in the platform because each change was in response to a valid user need. A higher level of design and functionality risk was tolerable at this smaller scale, knowing feedback could be depended on to course correct. And as the platform grew, necessary downtime procedures, a closely monitored support email, error banners, and offline reports of static meeting links assured users of operational reliability and helped mitigate the interruptions caused by unforeseen break-fix events – which were addressed within minutes. Ultimately, these early sprint-like development cycles accelerated our ability to discover the right design and functionality to serve both user needs and wants, for both the clinician and the patient, and gathered the momentum required for organic enterprise scale adoption.
3.2. Patient experience
When an appointment is scheduled, Switchboard (in conjunction with another Penn Medicine app, the Visit Guide, and our video vendor’s API), generates a unique meeting link for that patient’s encounter with the clinician. The patient automatically receives an SMS or email notification including appointment details and instructions on how to join, along with practice-specific customizations to remind patients to prepare medications or blood sugar readings prior to the visit, for example. The visit reminder contains a link that begins the visit—functionality designed for individual or group visits, and for inviting caregivers and guests to the visit.
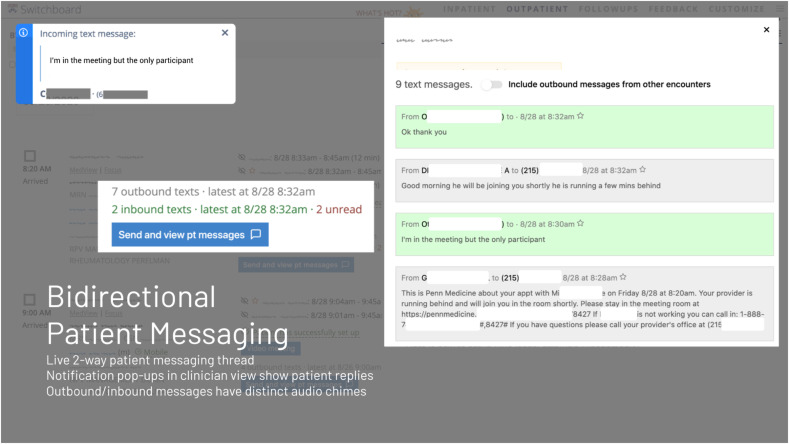
In our first weeks, we monitored all incoming patient replies to their appointment reminders, and saw patients facing technical setup barriers, anxiously waiting for their providers, or caregivers sharing the best way to reach their family members. Some simply vented: “App not working. Totally frustrated. Please call my cell.” In response, we built two-way SMS texting into the platform so physicians and patients could pivot how they contacted each other in real-time. Patients could also receive pre-visit texts when clinicians were running late, or instructions to “please wait in the parking lot and let us know when you arrive” to control in-person flow. Responses from the patient are seen by the care team in real time on the Switchboard as an audible and visible notification (Fig. 2 ). Leveraging built-in audio notifications and additional timed messages have enabled more efficient alternatives to phone outreach for coordinating follow-up scheduling and testing for patients post-encounter as well.
Fig. 2.
Bidirectional patient messaging functionality.
To further enhance the ability to respond to patient needs, at the end of encounters, Switchboard engages patients about their experience via short text message or phone call (interactive voice response) surveys. These surveys can be delivered at key times in relation to encounters (such as checkout or discharge from the hospital) to capture salient, precise snapshots of experience at points along the patient journey. Results are displayed in a summary view enabling aggregated analysis by sentiment and content, and service recovery using replies within Switchboard.
3.3. Clinician experience
The heart of the clinician experience is the ability to launch a video meeting via a vendor platform directly from Switchboard, while maintaining situational awareness of clinic flow, having flexible device options, and seamlessly accessing interpreter services.
The core foundational features include the ability to launch Switchboard from any type of device via browser for mobile and desktop, secured by single sign-on, protected by VPN. The Switchboard clinician view is generated from the daily clinic schedule, replacing static, manually organized lists of meeting links clinicians and staff fumbled through to orchestrate a clinic day. Both telemedicine and in-person encounters are included, to help conduct mixed sessions or days leveraging both to retain clinic volumes.
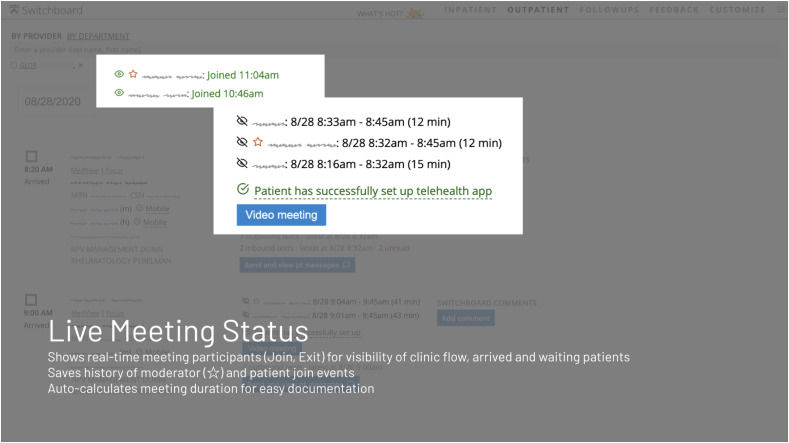
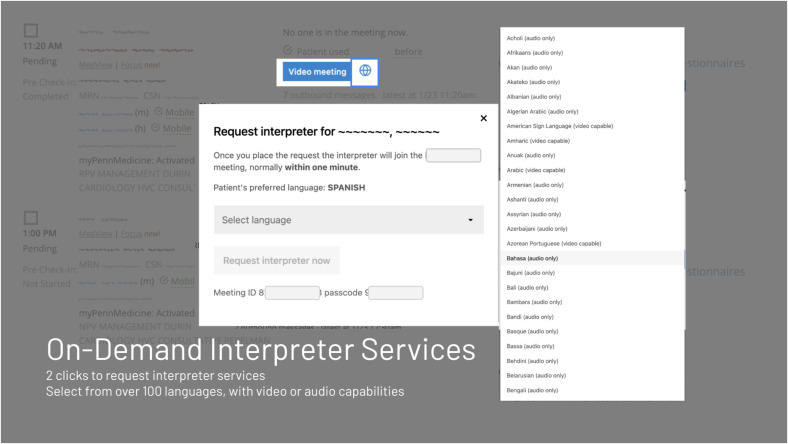
Additionally, we wanted to support workflows surrounding the video visit itself. Without physical touchdown spaces and hallways, teams had difficulty coordinating complex workflows when remote, such as preceptors leapfrogging between trainees or practice staff tag-teaming on intake and pre-visit payment processes. That led us to enable multiple people to view and join any set of scheduled appointments. Switchboard also displays real-time meeting participants (both patients and clinicians) as well as the length of time each participant spends in the room, allowing clinicians to enter the room once a patient is present, or to join after their colleague has left. (Fig. 3 ). Working from home, clinicians often relied on their own personal devices to launch meetings and needed the flexibility to mix and match devices. A meeting can be joined via link through the Switchboard directly or via a QR code scanned by another handheld device (Fig. 4 ). They also can add a medical interpreter to a video visit with two clicks, much quicker than alternative workflows (Fig. 5 ).
Fig. 3.
Example of live meeting status indicator.
Fig. 4.
Provider workflow of launching a video visit.
Fig. 5.
Example of integration of interpreter services into telemedicine workflow.
To streamline clinic flow, many logistical hurdles were removed by leveraging just-in-time text and email messaging. Clinicians and staff can alert patients instantly if the clinician is running late. Message pre-built templates further facilitate rule-based messages sent to populations of patients at once, triggered by available elements and events within the EHR. For example, dermatology patients are prompted to reply with a photo of their lesion 15 minutes after their appointment is scheduled and a week prior to their visit, and rheumatology patients to complete the RAPID3 patient questionnaire two days before their visit. And at the end of the visit, a ‘virtual checkout desk’ model is possible, where practice staff directly join the patients at the end of the appointment to coordinate next steps, facilitated by an audio chime indicating when a clinician has left a room.
4. Results
Since the start of the pandemic, the Switchboard has helped Penn Medicine deliver > 1 M virtual care encounters, for 8,800 unique users with an average of 2,000–3,000 appointments/week (Fig. 6 ). 75% of these encounters have occurred via video, compared to 75% occurring via phone prior to Switchboard. We eliminated incidences of multiple patients inadvertently joining the same session. Switchboard received a Net Promoter Score +38 (n = 206) from physician users in the first month of adoption.
Fig. 6.
Graph of adoption of telemedicine solution.
4.1. Lessons for the field
Equity revealed itself as the primary patient hurdle in the implementation of Switchboard-based virtual care.1, 2, 3 The use of simple SMS messaging about appointment reminders – rather than depending exclusively on an app-based patient portal -- was a key equalizer in reaching patients, especially those without smartphones, with limited internet or email access, or with less technical literacy. Furthermore, older, Black and Latinx, and lower-income patients, among other demographics, were less likely to use video for their virtual care visits, despite pre-visit instructions and a textbot we implemented to walk patients through the steps to download our video vendor application, even with a version translated into Spanish. The multi-step process itself was burdensome. In response, we worked with our video vendor to help them deploy a web-based, rather than app-based, video client for mobile iOS and Android devices – eliminating the requirement to download an app prior to a telemedicine encounter. These vendor partnerships were critical to shaping the end-to-end experience - and by advocating for needs felt on the ground, we were able to inform priorities and collaborate on adapting core features to the benefit of all.
A second equity hurdle is the lack of easy language (including sign language) interpreter services. It took a manual process to coordinate the request and invitation process in a timely fashion for a live clinical interpreter to successfully join a virtual patient encounter, and much of those logistics fell on the physician. To resolve this, we partnered with our existing interpretation vendor to implement an API-based two-click method of requesting and admitting the appropriate interpreter into a virtual exam room. Then to reduce language barriers in communicating visit logistics, we utilized cloud interpretation services for bidirectional text interpretation of messages between English and >100 other languages, achieved with one click. These direct integrations into our internally developed platform were far simpler and quicker to implement than alternative routes requiring integration through a vendor or our enterprise EHR.
The largest clinician hurdle in implementing a new platform has been addressing the needs for education, troubleshooting support, and process changes across our large organization. In order to do that, we have created several standing meetings which include a large sampling of clinical and administrative leaders across the organization, and with designated operational leads at each entity who serve as local experts and first responders to questions or issue escalation. During the initial part of the pandemic, weekly town halls spread the word about important legal, workflow, and billing updates and recommendations to ensure the wide-scale practice of reimbursable, compliant virtual care. These also became forums for highlighting new technical features as new tools were rolled out on a weekly basis. Smaller forums with open-ended agendas provide localized education to operational champions to troubleshoot and fill gaps in knowledge or functionality. Finally, entity champions and leaders across the organization receive a slide deck of the latest telemedicine developments on a weekly basis via email, along with a self-service support website that hosts resources and educational materials updated with the latest developments. For any questions not answered through these channels, we have also created an email inbox monitored by our team and used by individuals throughout our organization to ensure questions ranging from technical to legal to privacy are answered.
Going forward, we will continue to build and iterate on our platform to support the use of virtual care in new settings and care team models. We plan to integrate and embed the platform into our EHR environment (rather than as a separate application) and leverage the platform for conducting and facilitating inpatient telemedicine consults, integrating multiple video vendor platforms and hardware device workflows into a single user experience.
By insourcing a virtual care solution, we were able to develop a feature-rich, user-friendly, sustainable – and most importantly, an adaptable – platform that has met all the challenges and changing demands faced by our front-line clinicians. The rapid deployment and success at scale depended on tight feedback loops, user-informed design, and an embedded development team collaborating with front-line clinicians and staff. Virtual care is here to stay, and our unique implementation illustrates how existing internal capacity and technology investments accelerated our ability to incorporate innovations quickly and seamlessly into daily practice during a crisis.4 We hope this experience encourages learning health systems to build the infrastructure for digital transformation today to make tomorrow’s technology-enabled models of care possible.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Special thanks to: Glenn Fala, Richard Urbani, Gregory Fil, Catherine Shi, Mohan Balachandran, Debra Laumer, Ann Marie Huffenberger, Gregory Kruse, Dave Masi, Christine Vanzandbergen, Michael Restuccia, Philynn Hepschmidt
References
- 1.Eberly Lauren A., Khatana Sameed Ahmed M., Nathan Ashwin S., et al. Telemedicine outpatient cardiovascular care during the COVID-19 pandemic. Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Julien Howard M., Eberly Lauren A., Srinath Adusumalli. Telemedicine and the forgotten America. Circulation. 2020;142(4):312–314. doi: 10.1161/CIRCULATIONAHA.120.048535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eberly L.A., Kallan M.J., Julien H.M., et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi K., Adusumalli S., Lee K., Rosin R., Asch D.A. 5 lessons from Penn medicine’s crisis response. Harv Bus Rev. 2020 https://hbr.org/2020/06/5-lessons-from-penn-medicines-crisis-response [Google Scholar]