Abstract
The impact of intraoperative esophageal device insertion (EDI) on endotracheal tube (ET) cuff inflation pressure remains unclear. Electronic databases including Medline, Embase, Google scholar, Web of Science™ and Cochrane Central Register of Controlled Trials were searched for studies involving EDI after placement of ETs from inception to July 7, 2022. The primary outcome was risk of high cuff pressure, while the secondary outcomes were increases in cuff pressure following EDI. Difference between adults and children was investigated with subgroup analysis. There were ten eligible studies (observation study, n = 9, randomized controlled study, n = 1) involving a total of 468 participants. EDI notably increased the risk of high cuff pressure (n = 7, risk ratio: 12.82, 95% confidence interval: 4.9 to 33.52, subgroup analysis: p = 0.008). There were significant elevations in cuff pressure in adults and children both during (13.42 and 7.88 cmH2O, respectively, subgroup analysis: p = 0.15) and after (10.09 and 3.99 cmH2O, respectively, subgroup analysis: p = 0.0003) EDI. Our results revealed an over 12-fold increase in the risk of high endotracheal tube cuff pressure in patients, especially adults, receiving EDI under endotracheal anesthesia. There were significant increases in both adults and children despite a higher increase in the former after device insertion.
Subject terms: Medical research, Risk factors
Introduction
Maintaining the cuff pressure of endotracheal tube (ETT) within a suitable range is of paramount importance as under- or over-inflation could be associated with clinically significant complications1; while under-inflation may result in ineffective sealing of the tracheal opening and an elevated risk of pulmonary aspiration, over-inflation may compromise tracheal mucosal circulation and result in tracheal injury2–5. Over-inflation of an ETT cuff is defined as the injection of a volume of air more than that needed to create an adequate seal between the cuff and the tracheal wall6. It is well known that tracheal injury is correlated with cuff pressure as compromise of tracheal mucosal blood flow is an important contributor to intubation-related tracheal morbidity2.
Previous studies have shown that a cuff pressure of > 30 cmH2O may impede local tissue blood flow and cause damage to the tracheal mucosal wall as well as the surrounding anatomical structures6,7, resulting in complications ranging from sore throat8,9, hoarseness, recurrent laryngeal nerve injuries10, tracheal ulceration, necrosis, stenosis11, the formation of tracheal diverticulum12 and tracheo-esophageal fistula13–18 to the life-threatening condition of tracheal rupture during cardiac resuscitation19. Besides, evidence from animal experiments demonstrated consistent tracheal mucosal damage even only after a brief exposure to an over-inflated tracheal cuff20. Physiologically, blood flow to the antero-lateral part of the trachea has been reported to be compromised at pressures exceeding 30 cmH2O and become obstructed at pressures exceeding 50 cmH2O21. Previous studies have also shown that hyperinflation of ETT cuff could result in the herniation of the cuff balloon in front of the tube’s end22 or upwards through the glottis23, thereby jeopardizing gas exchange. Hence, general practice guidelines recommended a cuff inflation pressure below 30 cmH2O (22 mmHg)7.
Despite careful monitoring of cuff pressure after tracheal intubation for anesthesia, intra-operative insertion of esophageal devices may alter the cuff pressure24. Indeed, previous studies have revealed that insertion of a medical device into the esophagus, which is situated between the rigid cervical spine and the trachea, in a patient under endotracheal anesthesia may increase ETT cuff pressure24–31. In addition, the use of a bougie in patients undergoing bariatric surgery may be related to an increased risk of esophageal complications32,33, while the insertion of a transesophageal echocardiography (TEE) probe during cardiac surgery may be associated with additional risks of airway complications (e.g., ETT obstruction)34,35. However, the clinical significance of such impacts in adults and children has not been systematically reviewed based on pooled evidence.
Therefore, the present meta-analysis aimed at elucidating the risk of high cuff pressure in patients undergoing endotracheal general anesthesia for procedures involving the insertion of esophageal devices. We also investigated the increases in cuff pressure during and after their insertion and compared the differences between adults and children in an attempt to provide evidence-based guidance for clinical practice.
Materials and methods
Guidelines and registration
This meta-analysis was conducted based on the recommendation of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and was registered with PROSPERO (CRD42021232644).
Search strategy
The databases of Medline, Embase, Google scholar, Web of Science™ and the Cochrane Central Register of Controlled Trials (CENTRAL) were searched for reports using the keywords: ("Tracheal intubation" or "Endotracheal intubation" or "general anesthesia") AND ("Nasogastric tube*" or "NG tube*" or "Bougie*" or "Transesophageal echocardiography probe*" or "Orogastric tube*" or "Probe*" or "Transesophageal probe*" or "esophagogastroduodenoscopy probe*" or "Esophageal Stethoscope*" or "Gastrointestinal Intubation" or "Nasogastric Intubations") AND ("Cuff pressure*" or "Intracuff pressure*" or "intracuff measurement") from inception to April 11, 2021 (Updated on July 7, 2022). Subject headings (e.g., MeSH terms in Cochrane Library) were also used to assist in searching. We manually searched the Google scholar and references included in all the retrieved articles to identify potentially eligible studies not identified during our electronic screening. No restriction on publication date was applied, but only studies published in English were reviewed.
Inclusion and exclusion criteria
The abstracts and titles of the retrieved studies were independently screened by two investigators who also read the full text of the potentially eligible articles and discussed the contents. Conflicts were resolved by a third investigator. Another investigator screened additional references from the included articles. The criteria for eligibility of studies included: (1) patients receiving tracheal intubation with cuffed ETTs, (2) studies involving esophageal insertion of medical devices after the ETT placement, (3) available data regarding change in cuff pressure. The exclusion criteria were (1) studies with unavailable information about changes in cuff pressure, (2) the use of nitrous oxide for maintenance of general anesthesia as nitrous oxide is associated with an increase in endotracheal cuff pressure2, and (3) articles not formally published (e.g., those in Research Square). Two authors independently investigated the eligibility of the selected trials for final analysis, while two other reviewers independently extracted necessary data. On encountering disagreements, a third author was consulted to reach a consensus. We contacted the corresponding authors of trials that did not provide data on primary or secondary outcomes to retrieve the missing information.
Primary outcome and secondary outcomes
The primary outcome was the risk of high cuff pressure, the definition of which was according to that of each study. The secondary outcomes were the increases in cuff pressure during and after EDI. Subgroup analyses were also performed to investigate the difference between adults and children as well as that between cardiac and non-cardiac surgery in adult patients.
Risk of bias assessment
Studies deemed eligible were assessed for methodological quality and risk of bias by two independent reviewers using the Cochrane Collaboration risk of bias tool36, and the Newcastle–Ottawa Scale (NOS)37 for randomized controlled trials and comparative studies (cohorts and case–control studies), respectively. The NOS for observational studies was based on three domains, namely, study group selection, group comparability, and outcome of interest ascertainment. For the Selection, Comparability, and Outcome domains, a maximum of four, two, and three stars could be assigned, respectively. A higher number of stars denotes a better quality of the study with nine stars indicating the highest quality37. A study with a low risk of bias was defined as one having seven stars or more. Disagreements were resolved through discussion.
Statistical analysis
Based on the random effects model, the risk ratios (RRs) with 95% confidence intervals (CIs) were computed for dichotomous outcomes which were pooled with the Mantel–Haenszel (MH) method38,39. On the other hand, the mean difference (MD) represented the effect size for continuous outcomes. The I2 statistic was used to assess the degree of variability in effect estimates attributable to heterogeneity rather than error in sampling. We also conducted sensitivity analyses to test the robustness of our findings by omitting one trial at a time from the meta-analysis to evaluate the potential influence of a particular study on the overall outcomes. A funnel plot was examined for symmetry to assess the probabilities of publication and reporting bias on encountering 10 or more studies reporting on a specific outcome. To assess the impact of demographic characteristics on changes in cuff pressure in adult patients, univariate analysis with a meta-regression approach was performed through including one covariate at a time [i.e., age, prevalence of male gender, body mass index (BMI)]. For all analyses, we set the significance level at 0.05 and used the Cochrane Review Manager (RevMan 5.4; Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014) for data synthesis. Meta-regression was conducted using the Open Meta-Analyst software (Brown University, Providence, RI; http://www.cebm.brown.edu/openmeta/).
Results
Study selection
A flow chart summarizing the process of study selection and exclusion is shown in Fig. 1. Of the 136 articles initially retrieved from the electronic databases, 112 were excluded due to duplicates (n = 28) or irrelevance (n = 84). Of the remaining 24 records assessed with a full-text review, 14 were excluded because of the informal nature of publication (i.e., Research Square) (n = 3), conference abstract (n = 4), and irrelevance (n = 7). Finally, a total of ten studies were included in the present meta-analysis24–31,40,41.
Figure 1.
Summary of the process of study selection for the current meta-analysis.
Characteristics of included studies and risk of bias assessment
Ten studies involving 468 participants published between 2011 and 2022 were analyzed24–31,40,41. Characteristics of the studies including patient demographics, surgical setting, type of esophageal devices, and size of ETTs are described in Table 1. The number of patients in the included studies ranged from 13 to 80. Of the ten studies, seven reported on adult patients24,26,27,30,40–42, two focused on the pediatric population25,28, and one included both adult and pediatric patients31. The median or mean age of patients was between 0.5 and 66.8 years with a male prevalence of 28.3%-86.4%. One study did not offer detail regarding gender distribution28. Nine studies provided the BMI of the participants that ranged from 15.3 to 44.5 kg/m2, while this information was unavailable in the other study25. Seven studies involved cardiac surgery24,26,28,31,40–42, two investigated bariatric surgery27,30, and the other was on esophagogastroduodenoscopy25. One study, which examined the change in cuff pressure among patients undergoing endotracheal intubation with single and double lumen ETTs29, was split into two (i.e., Kim 2015a, Kim 2015b) to differentiate the study outcomes between the two devices. Focusing on the impact of age on cuff pressure, we divided the results of another report on changes in cuff pressure based on the age of the participants31 into five studies (i.e., Pan 2020a; Pan 2020b; Pan 2020c; Pan 2020d; Pan 2020e). Of the ten studies, nine observational studies compared the changes in cuff pressure before and after EDI24–29,31,40,41 and one was a randomized controlled trial30.
Table 1.
Characteristics of included studies (n = 10).
| Study (year) | Age (years) | Male (%) | BMI (kg/m2) | Procedure | ED | n | Airway device size |
Definition of HCP (cmH2O) | Incidence of HCP | Mean CP change (cmH2O) | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tan 201124 | 60.3 | 79 | 25.1 | CS | TEE probe | 38 | 7–7.5 mm¶ | > 35 | 45% | 8.5 | 8 |
| Hung 201427 | 34 | 28.3 | 37.7 | BS | OG tube | 60 | 7–8 mm¶ | > 30 | 50% | 8.3 | 8 |
| Kim 201529 | 66.8¶; 61.8‡ |
86.4¶ 59.1‡ |
23.4¶ 23.7‡ |
CS | TEE probe | 44 | 7–7.5 mm¶, 32-39Fr‡ | > 40 |
18.2%¶, 40.9%‡ |
6.9 12 |
8 |
| Ozayar 201630 | 38 | 35 | 44.5 | BS | OG tube | 40 | 7.5–8 mm¶ | NA | NA | 5.6 | NA§ |
| Balaban 201725 | 11.3 | 50 | NA | EGD | EGD probe | 13 | NA¶ | NA | NA | 5 | 8 |
| Kamata 201728 | 0.5–14 | NA | 15.3–20.3 | CS | TEE probe | 80 | 3–7 mm¶ | > 30 | 22.50% | 3.6 | 8 |
| Borde 202026 | 55 | 69.3 | 23.3 | CS | TEE probe | 65 | 7–8.5 mm¶ | > 30 | 40% | 8 | 8 |
| Pan 202031 | 2.9–24.6 | 60.3 | 22.2 | CS | TEE probe | 58 | 3–7.5 mm¶ | > 30 | 23–77.5% | 3–12.3 | 8 |
| Maddali 202240 | 55.7 | 73.5 | 28.7 | CS | TEE probe | 34 | 7.5–9 mm¶ | NA | NA | 20.3 | 8 |
| Parajuli 202141 | 40.5 | 61.1 | 23.6 | CS | TEE probe | 36 | 7–7.5 mm¶ | > 30 | 50% | 7.64 | 8 |
BMI body mass index; EGD esophagogastroduodenoscopy; OG orogastric tube; TEE transesophageal echocardiography; HCP high cuff pressure; CP cuff pressure; BS Bariatric surgery; CS Cardiac surgery; NA not available; ED Esophageal device; ¶single tracheal tube; ‡DLT double lumen tube; NOS Newcastle − Ottawa scale; §risk of bias assessed using the Cochrane Collaboration risk of bias tool.
Regarding the association of EDI with adverse effects, only airway complications were mentioned in the included studies. Eight studies reported no EDI-related complications (e.g., air leak or changes in ventilator parameters) after EDI24–28,31,40,41, while one study did not provide relevant information29. The other study reported an increased severity of sore throat in patients with EDI compared to those without at postoperative 30 min, 2 h, and 24 h30. No other ETT-associated respiratory complication or adverse events (e.g., esophageal injury) was reported in all studies.
The risks of bias of the nine observational studies are shown in Table 1. While the nine observational articles all showed a low risk of bias (i.e., total NOS score of 8 for each study), the risk of random sequence generation for the randomized controlled trial30 was deemed unclear because of a lack of specific information. In addition, the risk of bias for blinding of participants and personnel was high in this study30 as blinding of participants was impossible in this clinical setting.
Study outcomes
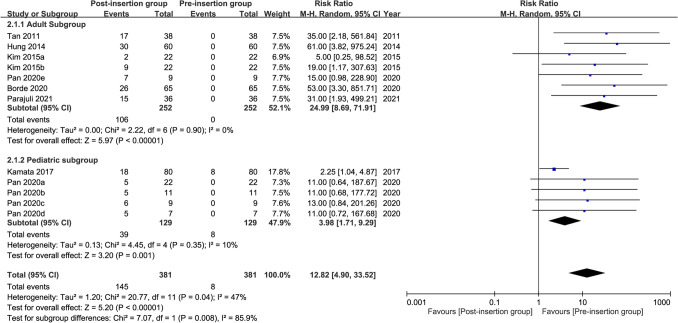
Risk of high cuff pressure
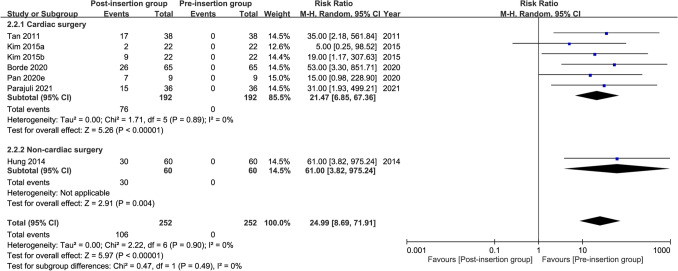
Seven studies were available for the analysis24,26–28,31,41,42. A forest plot revealed a high risk of high cuff pressure following EDI (RR = 12.82, 95% CI 4.9 to 33.52, p < 0.00001; I2 = 47%) (Fig. 2). Subgroup analysis demonstrated a significant difference between adults and children (RR: 24.99 and 3.98 for adults and children, respectively, p = 0.008), implying a positive association between age and the risk of high cuff pressure. The heterogeneity within each subgroup among the included studies was low (i.e., I2 = 0% and 10% for adults and children, respectively). Sensitivity analysis showed no significant impact on outcome by omitting certain studies. For adult patients, meta-regression showed that age, prevalence of male gender, and BMI were not associated with the risk of high cuff pressure (Fig. 3). Similarly, the type of surgery (i.e., cardiac vs. non-cardiac) had no impact on the risk of high cuff pressure in adult patients (subgroup difference: p = 0.49)(Fig. 4).
Figure 2.
Forest plot comparing the risk of high cuff pressure after esophageal medical device insertion. CI confidence interval; M–H Mantel–Haenszel.
Figure 3.
Meta-regression plot showing the association of patient characteristics (i.e., age, prevalence of male gender, and body mass index) with the risk of high cuff pressure.
Figure 4.
Forest plot comparing the risk of high cuff pressure after esophageal medical device insertion in adults undergoing cardiac and non-cardiac surgery. CI confidence interval; M–H Mantel–Haenszel.
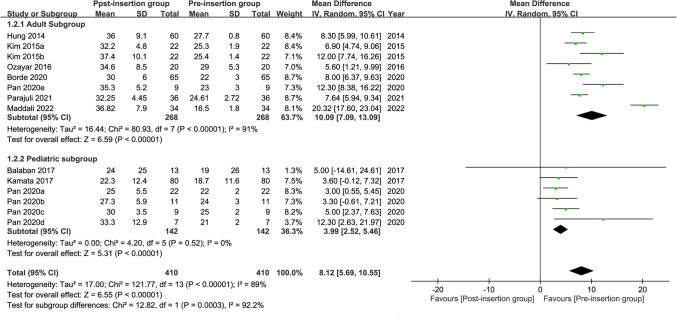
Change in cuff pressure during esophageal device insertion
Merged results from eight studies24–26,28,30,40–42 showed a significant rise in cuff pressure during EDI with increases in pressure being 13.42 and 7.88 cmH2O for adults and children, respectively (mean difference = 12.35 cmH2O, 95% CI: 6.72 to 17.97, p < 0.0001; I2 = 97%) (Fig. 5). Subgroup analysis found no significant difference between adults and children in this outcome (p = 0.15), suggesting that age was not significantly related to the change in cuff pressure during EDI. However, there was a high heterogeneity among the results from the adult subgroup across the included studies (I2 = 98%). Sensitivity analysis showed no significant impact on outcome by omitting certain studies.
Figure 5.
Forest plot for the comparison of changes in cuff pressure during esophageal medical device insertion. CI confidence interval; IV inverse variance.
Change in cuff pressure after esophageal device insertion
The forest plot on the nine available studies25–28,30,31,40–42 demonstrated a significant elevation in tracheal cuff pressure following EDI in both adults and children (10.09 and 3.99 cmH2O, respectively) (pooled mean difference = 8.12 cmH2O, 95% CI: 5.69 to 10.55, p < 0.00001; I2 = 89%) (Fig. 6). Subgroup analysis revealed a significant difference between adults and children (p = 0.0003), indicating that age was a significant factor affecting the change in cuff pressure after EDI with an elevation in adults higher than that in children. The heterogeneity in the adult subgroup across the included studies was high (i.e., I2 = 91%). Sensitivity analysis showed no significant impact on outcome by omitting certain trials.
Figure 6.
Forest plot for the comparison of changes in cuff pressure after esophageal medical device insertion. CI confidence interval; IV inverse variance.
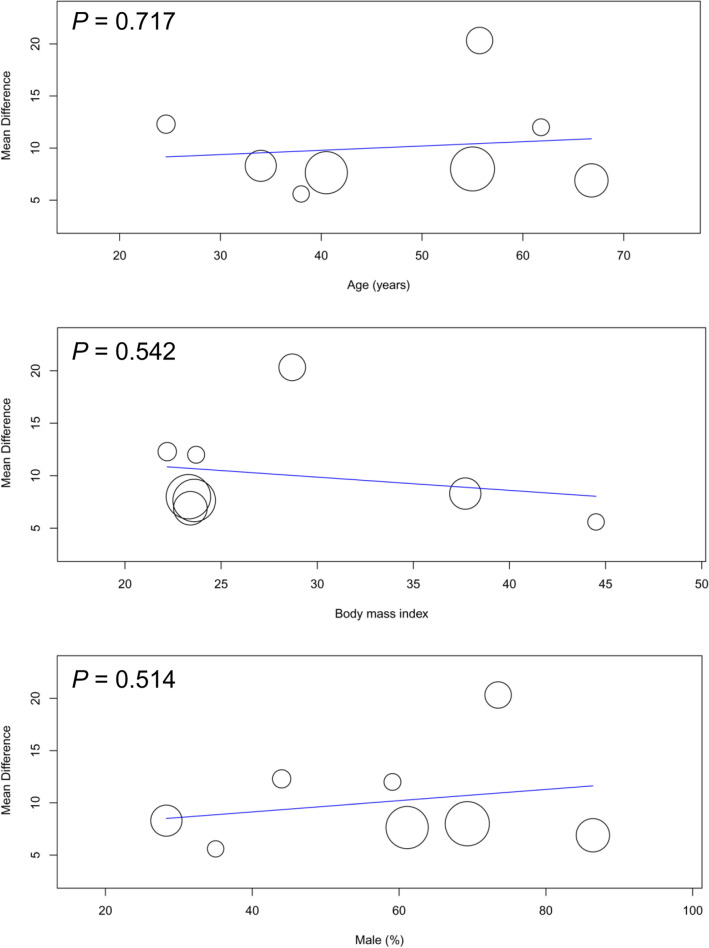
Meta-regression showed that the age, prevalence of male gender, and BMI were not correlated with changes in cuff pressure in adult patients (Fig. 7). Subgroup analysis in adult patients demonstrated that the type of surgery (i.e., cardiac vs. non-cardiac) had no impact on the changes in cuff pressure (subgroup difference: p = 0.13) (Fig. 8).
Figure 7.
Meta-regression plot showing the association of patient characteristics (i.e., age, prevalence of male gender, and body mass index) with the mean difference in cuff pressure.
Figure 8.
Forest plot for the comparison of changes in cuff pressure after esophageal medical device insertion in adults undergoing cardiac and non-cardiac surgery. CI confidence interval; M–H Mantel–Haenszel.
Discussion
Despite the importance of maintaining the ETT cuff inflation pressure within an appropriate range2–5, the issue of changes in cuff pressure in procedures involving EDI was not systematically reviewed. To our best knowledge, the current meta-analysis is the first to address the impact of EDI on ETT cuff pressure based on available clinical evidence. Our results demonstrated an over 12-fold increase in risk of high cuff pressure (i.e., RR: 12.82) associated with the insertion of esophageal devices during endotracheal anesthesia. In addition, there were significant increases in cuff pressure both during and after device insertion in adults and children, highlighting the need for clinical concern regarding the impact of using esophageal devices on ETT cuff inflation pressure.
Previous studies have shown a prevalence of high cuff pressure in different clinical settings, including the operating theater in which the cuffs tend to be overinflated43, intensive care unit in which the cuff pressure may not be closely monitored44, and the emergency department in which physicians focus on life-threatening conditions45. The pressure inside the ETT cuff is also known to be affected by several factors, including lateral wall pressure, pneumoperitoneum46, duration of ETT placement6, patient position47, head position48, cuff position49, cuff volume, temperature50, use of nitrous oxide51, design of cuff52 and other less commonly reported factors.
Effort has also been made to modify the design of the cuff of ETT to minimize injury to the tracheal mucosa. To minimize the risk of overinflation associated with the conventional high-pressure low-volume cuff, the high-volume low-pressure ETT cuff has been introduced to avoid pressure-induced compromise of tracheal blood flow. However, previous studies showed that low-pressure cuffs may easily be overinflated to yield pressures that exceed capillary perfusion pressure7 for which cuff pressure monitoring is still vital.
On the other hand, the lack of accuracy of the two common methods of cuff pressure assessment, namely the fixed volume and pilot balloon palpation approaches53,54, may contribute to the high incidence of unnoticed cuff pressure elevation. A previous investigation has shown that actual measurement of the cuff pressure estimated by palpation with personal experience is often much higher than the optimal value when measured with manometry52. Although the minimal leak test has been introduced to evaluate cuff pressure, the accuracy of measurement is also questionable55. Another reason that may discourage the measurement of cuff pressure is the possible associated risk; it may lead to a drop in cuff pressure, which may cause leakage of secretions on the cuffs56.
The problem of cuff overinflation is further aggravated by the insertion of esophageal devices during endotracheal anesthesia when the cuff pressure is not usually monitored. Since the esophagus is in contact with the posterior membranous tracheal wall, introduction of an esophageal device (e.g., TEE probe) may directly compress the trachea and increase ETT cuff pressure, thereby compromising the microcirculation of trachea and its surrounding structures24. Indeed, a previous experimental investigation has demonstrated a notable negative impact of an increased cuff pressure on tracheal blood flow regardless of the duration20, underscoring the risk of adverse consequences from high cuff pressure triggered by esophageal device insertion for even a brief procedure. Therefore, manometry-guided control of cuff pressure has been proposed to reduce ETT-associated respiratory complications such as sore throat, hoarseness, cough, and blood-tinged expectoration even for procedures of short durations (i.e., 1–3 h)52. Nevertheless, although previous investigations have shown an increase in ETT cuff pressure induced by insertion of esophageal devices24–31, there was no pooled evidence identifying the risk of high cuff pressure and the net increases in pressure during and after device insertion as well as addressing the issue of difference between adults and children.
The choice of esophageal device may have a direct influence on cuff pressure. In the current study, there were three devices being introduced into the esophagus in the adult study population, namely the TEE probe, orogastric tube (i.e., bougie) for bariatric surgery, and the insertion tube of an endoscope. On the other hand, there was only one device used in children (i.e., TEE probe). Despite the relative noninvasiveness57 and usefulness of TEE probe as an intraoperative monitoring device for providing valuable information about the patient’s cardiac pathophysiological status58, it may be associated with the risks of pneumonia59 and other respiratory complications including airway compression and ETT malpositioning57,60. Moreover, cuff overinflation is another concern because monitoring of cuff pressure is not a routine practice among anesthetists during cardiac surgeries61. Consistently, an increase in cuff pressure may increase the risk of post-intubation tracheal stenosis in patients undergoing cardiac procedures11. Since TEE examination is usually performed in patients with hemodynamic instability, the hypotension–related reduction in tracheal mucosal perfusion pressure may further predispose patients to the risk of tracheal mucosal injury from tracheal cuff overinflation29. The use of orogastric tubes, which serve as both calibration tool and a volume reference device in bariatric surgery (e.g., laparoscopic sleeve gastrectomy), has also been implicated in respiratory tract complications such as arytenoid dislocation62 and hypopharyngeal perforation63. In addition to the reported elevation in the incidence of post-intubation sore throat in patients undergoing bariatric surgeries64 due to the likeliness of their need for difficult airway management65, the results of the current study suggest a possible further increase in the incidence of sore throat attributable to cuff overinflation if cuff pressure monitoring is unavailable.
In the current meta-analysis, we found a significantly higher risk of high cuff pressure in the adults (RR = 24.99) compared to the pediatric population (RR = 3.98). Nevertheless, a previous case report on a 12-year-old girl has demonstrated an association of EDI with airway obstruction34, highlighting the need for careful monitoring of cuff pressure as well as airway-related complications in the pediatric population. For adult patients, we recommended routine monitoring of cuff pressure because of our finding of an elevated risk of high cuff pressure after EDI.
A previous study that investigated the associations of the type of tracheal tube (i.e., single vs. double lumen), age, body height and weight as well as tracheal diameter with change in cuff pressure after EDI in adults using univariate analysis identified the type of tracheal tube as the only predictor29. In the current study, to assess the impact of demographic factors on change in cuff pressure in adult patients, univariate analysis with a meta-regression approach was conducted through including one covariate at a time (i.e., age, prevalence of male gender, BMI). The results showed that age, prevalence of the male gender, and BMI did not correlate with the risk of high cuff pressure and change in cuff pressure after EDI in adult patients. Therefore, our findings were consistent with those of that study29. In addition, our subgroup analysis on adults further demonstrated no significant impact of the type of surgery (i.e., cardiac vs. non-cardiac) on change in cuff pressure. These findings underscored the importance of routine monitoring of cuff pressure in adult patients regardless of their age, gender, BMI, and the type of surgery that they receive.
Limitations
There were several limitations in the current study. First, the definitions of high cuff pressure varied among the included studies (e.g., > 3026–28,31,41, > 3524, or 40 cmH2O42. Therefore, the actual risk of high cuff pressure was underestimated in the present study when using > 30 cmH2O as a cut-off point for defining a high cuff pressure. Second, there was a high overall heterogeneity regarding the change in cuff pressure during EDI among the included studies probably attributable to the differences in patient population (i.e., adults vs. children) and the medical device chosen for each study. Previous studies have reported variations in cuff pressure with a number of factors including the size of ETT66, the design (e.g., shape) of the cuff42,67, and intubation time68 which, however, were not described in details in the included studies. Nevertheless, despite the possible variation in the size of ETT in children, the heterogeneity was acceptably low among the included studies. Finally, our results on children were only from three studies that used the same device (i.e., TEE probe) that may account for a relatively minor elevation in cuff pressure compared with that in adults so that the result could not be extrapolated to other devices in the pediatric population.
Conclusions
The results of the current meta-analysis demonstrated an over 12-fold elevation in the risk of high endotracheal tube cuff inflation pressure especially in adult patients receiving esophageal device insertion under endotracheal anesthesia. There were significant increases in cuff pressure associated with the use of esophageal devices in both adults and children despite a higher increase in the former. The high heterogeneity across the included studies in the present investigation warrants further clinical trials to support its findings.
Acknowledgements
Professional assistance offered by the head librarian of E-Da Hospital medical library, Miss Su-Ying Chiu, with literature search for the current meta-analysis is sincerely acknowledged.
Author contributions
K.-C.H. and Y.-J.C.: Conceptualization, methodology, software; Y.-P.C.: Data Curation; K.-C.H. and P.-W.H.: writing—original draft preparation; C.-N.H. and K.-M.L.: visualization, investigation; C.-K.S.: supervision; J.-Y.C. and L.-K.W.: software, validation; K.-C.H. and C.-K.S.: writing—reviewing and editing. P.-W.H. and C.-K.S. contributed equally as corresponding authors to this work.
Funding
None declared.
Data availability
The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Ping-Wen Huang and Cheuk-Kwan Sun.
References
- 1.Kumar CM, Seet E, Van Zundert T. Measuring endotracheal tube intracuff pressure: no room for complacency. J. Clin. Monit. Comput. 2021;35:3–10. doi: 10.1007/s10877-020-00501-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tu HN, Saidi N, Leiutaud T, Bensaid S, Menival V, Duvaldestin P. Nitrous oxide increases endotracheal cuff pressure and the incidence of tracheal lesions in anesthetized patients. Anesth. Analg. 1999;89:187–190. doi: 10.1097/00000539-199907000-00033. [DOI] [PubMed] [Google Scholar]
- 3.Metheny NA, Schallom L, Oliver DA, Clouse RE. Gastric residual volume and aspiration in critically ill patients receiving gastric feedings. Am. J. Crit. Care. 2008;17:512–519. [PMC free article] [PubMed] [Google Scholar]
- 4.Poetker DM, Ettema SL, Blumin JH, Toohill RJ, Merati AL. Association of airway abnormalities and risk factors in 37 subglottic stenosis patients. Otolaryngol. Head Neck Surg. 2006;135:434–437. doi: 10.1016/j.otohns.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Sengupta P, Sessler DI, Maglinger P, Wells S, Vogt A, Durrani J, et al. Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol. 2004;4:8. doi: 10.1186/1471-2253-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sultan P, Carvalho B, Rose BO, Cregg R. Endotracheal tube cuff pressure monitoring: A review of the evidence. J. Perioper. Pract. 2011;21:379–386. doi: 10.1177/175045891102101103. [DOI] [PubMed] [Google Scholar]
- 7.Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. BMJ. 1984;288:965–968. doi: 10.1136/bmj.288.6422.965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puthenveettil N, Kishore K, Paul J, Kumar L. Effect of cuff pressures on postoperative sore throat in gynecologic laparoscopic surgery: An observational study. Anesth. Essays Res. 2018;12:484–488. doi: 10.4103/aer.AER_72_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: A systematic review. Anaesthesia. 2016;71:706–717. doi: 10.1111/anae.13438. [DOI] [PubMed] [Google Scholar]
- 10.Taylor JW, Soeyland K, Ball C, Lee JC, Serpell J. Changes in tracheal tube cuff pressure and recurrent laryngeal nerve conductivity during thyroid surgery. World J. Surg. 2020;44:328–333. doi: 10.1007/s00268-019-05185-7. [DOI] [PubMed] [Google Scholar]
- 11.Liu J, Zhang CP, Li Y, Dong S. Post-intubation tracheal stenosis after management of complicated aortic dissection: A case series. J. Cardiothorac. Surg. 2015;10:148. doi: 10.1186/s13019-015-0357-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma M, Bulathsinghala CP, Khan A, Surani SR. An unusual case of iatrogenic tracheal diverticulum found in a mechanically ventilated patient: To treat or not to treat. Cureus. 2019;11:e5911. doi: 10.7759/cureus.5911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoffman RJ, Kato Y, Rivera LC, Sheth S, Prokofieva A, Parwani V. ETT cuff inflation and assessment. The experience and practice of Fire Department of New York paramedics. EMS Mag. 2009;38:64–66. [PubMed] [Google Scholar]
- 14.Knowlson GT, Bassett HF. The pressures exerted on the trachea by endotracheal inflatable cuffs. Br. J. Anaesth. 1970;42:834–837. doi: 10.1093/bja/42.10.834. [DOI] [PubMed] [Google Scholar]
- 15.Delgado Moya FP, Valiente Fernandez M, Gonzalez L, de Aledo A. Post-intubation tracheal laceration. Over-insufflation of the cuff as risk factor. Med Intensiva. 2020;44:394–395. doi: 10.1016/j.medin.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Nobre de Jesus G, Freitas F, Fernandes SM, Alvarez A. Post-intubation tracheal laceration. Intens. Care Med. 2019;45:521–522. doi: 10.1007/s00134-018-5450-z. [DOI] [PubMed] [Google Scholar]
- 17.Fan CM, Ko PC, Tsai KC, Chiang WC, Chang YC, Chen WJ, et al. Tracheal rupture complicating emergent endotracheal intubation. Am. J. Emerg. Med. 2004;22:289–293. doi: 10.1016/j.ajem.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 18.Guyton DC, Barlow MR, Besselievre TR. Influence of airway pressure on minimum occlusive endotracheal tube cuff pressure. Crit. Care Med. 1997;25:91–94. doi: 10.1097/00003246-199701000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Jung HM, Durey A, Han SB, Kim JH. Tracheal rupture related to endotracheal intubation during cardiopulmonary resuscitation. J. Emerg. Trauma Shock. 2019;12:58–60. doi: 10.4103/JETS.JETS_34_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sinha R, Correia R, Gardner D, Grau-Roma L, de Brot S, Hardman J, et al. Mucosal injury following short-term tracheal intubation: A novel animal model and composite tracheal injury score. Laryngosc. Investig. Otolaryngol. 2018;3:257–262. doi: 10.1002/lio2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seegobin RD, van Hasselt GL. Aspiration beyond endotracheal cuffs. Can. Anaesth. Soc. J. 1986;33:273–279. doi: 10.1007/BF03010737. [DOI] [PubMed] [Google Scholar]
- 22.Kao MC, Yu YS, Liu HT, Tsai SK, Lin SM, Huang YC. Airway obstruction caused by endotracheal tube cuff herniation during creation of tracheal stoma. Acta Anaesthesiol. Taiwan. 2005;43:59–62. [PubMed] [Google Scholar]
- 23.Wright D, Baruch M. Herniation of tracheal tube cuffs: A simple teaching model. Anaesthesia. 2001;56:277. doi: 10.1046/j.1365-2044.2001.01918-9.x. [DOI] [PubMed] [Google Scholar]
- 24.Tan PH, Lin VC, Chen HS, Hung KC. The effect of transoesophageal echocardiography probe insertion on tracheal cuff pressure. Anaesthesia. 2011;66:791–795. doi: 10.1111/j.1365-2044.2011.06789.x. [DOI] [PubMed] [Google Scholar]
- 25.Balaban O, Kamata M, Hakim M, Tumin D, Tobias JD. The effect of esophagogastroduodenoscopy probe insertion on the intracuff pressure of airway devices in children during general anesthesia. J. Anesth. 2017;31:278–281. doi: 10.1007/s00540-016-2297-8. [DOI] [PubMed] [Google Scholar]
- 26.Borde DP, Pande S, Asegaonkar B, Khade S, George A, Joshi S. Does the endotracheal tube cuff pressure increases with transesophageal probe insertion? Ann. Card. Anaesth. 2020;23:460. doi: 10.4103/aca.ACA_52_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hung K-C. To assess the changes of tracheal cuff pressure after a calibrating orogastric tube insertion. J. Anesth. 2014;28:128–131. doi: 10.1007/s00540-013-1673-x. [DOI] [PubMed] [Google Scholar]
- 28.Kamata M, Hakim M, Tumin D, Krishna SG, Naguib A, Tobias JD. The effect of transesophageal echocardiography probe placement on intracuff pressure of an endotracheal tube in infants and children. J. Cardiothorac. Vasc. Anesth. 2017;31:543–548. doi: 10.1053/j.jvca.2016.09.032. [DOI] [PubMed] [Google Scholar]
- 29.Kim TK, Min JJ, Seo J-H, Lee Y-H, Ju J-W, Bahk J-H, et al. Increased tracheal cuff pressure during insertion of a transoesophageal echocardiography probe: A prospective, observational study. Eur. J. Anaesthesiol. 2015;32:549–554. doi: 10.1097/EJA.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 30.Ozayar E, Kurtay A, Gulec H, Sahap M, Bulus H, Horasanli E. Bougie effects on endotracheal cuff pressure and sore throat in bariatric surgery. Bariatr. Surg. Pract. Patient Care. 2016;11:11–14. [Google Scholar]
- 31.Pan SJ, Frabitore SZ, Ingram AR, Nguyen KN, Adams PS. Transesophageal probe placement increases endotracheal tube cuff pressure but is not associated with postoperative extubation failure after congenital cardiac surgery. Ann. Card. Anaesth. 2020;23:447. doi: 10.4103/aca.ACA_143_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tadayon SMK, Moeinvaziri N, Amini M, Setoodeh M, Haghighat N. Esophageal perforation during laparoscopic sleeve gastrectomy: Complication of bougie insertion. Int. J. Surg. Case Rep. 2021;81:105793. doi: 10.1016/j.ijscr.2021.105793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel A, Hsin MC, Huang CK. Bougie-induced esophageal perforation during laparoscopic Roux-en-Y gastric bypass surgery with hiatus hernia repair. Obes. Surg. 2020;30:3249–3250. doi: 10.1007/s11695-020-04546-9. [DOI] [PubMed] [Google Scholar]
- 34.Singh A, Tewari P. Right main bronchus obstruction caused by transesophageal echocardiography probe in a pediatric patient during complete repair of tetralogy of fallot. Ann. Card. Anaesth. 2021;24:402–404. doi: 10.4103/aca.ACA_87_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davies EA, Templeton R. Tracheal tube obstruction as a complication of transoesophageal echocardiography. Anaesth. Rep. 2021;9:110–113. doi: 10.1002/anr3.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford; 2000.
- 38.Hung KC, Wang LK, Lin YT, Yu CH, Chang CY, Sun CK, et al. Association of preoperative vitamin D deficiency with the risk of postoperative delirium and cognitive dysfunction: A meta-analysis. J. Clin. Anesth. 2022;79:110681. doi: 10.1016/j.jclinane.2022.110681. [DOI] [PubMed] [Google Scholar]
- 39.Hung KC, Yew M, Lin YT, Chen JY, Wang LK, Chang YJ, et al. Impact of intravenous and topical lidocaine on clinical outcomes in patients receiving propofol for gastrointestinal endoscopic procedures: A meta-analysis of randomised controlled trials. Br. J. Anaesth. 2022;128:644–654. doi: 10.1016/j.bja.2021.08.036. [DOI] [PubMed] [Google Scholar]
- 40.Maddali MM, Al Hadifi TSM, Sathiya PM, Jose S. The effect of intraoperative transesophageal echocardiography probe placement on the endotracheal tube cuff pressure in adult patients undergoing on-pump cardiac surgery. J. Cardiothorac. Vasc. Anesth. 2022;36(8):3084–9. doi: 10.1053/j.jvca.2022.02.037. [DOI] [PubMed] [Google Scholar]
- 41.Parajuli SS, Gyawali PK, Suraj KC. The effect of transesophageal echocardiography probe insertion in endotracheal tube cuff pressure in adult cardiac surgical patients. Nepal. Heart J. 2021;18:49–51. [Google Scholar]
- 42.Kim HC, Lee YH, Kim E, Oh EA, Jeon YT, Park HP. Comparison of the endotracheal tube cuff pressure between a tapered- versus a cylindrical-shaped cuff after changing from the supine to the lateral flank position. Can. J. Anaesth. 2015;62:1063–1070. doi: 10.1007/s12630-015-0394-z. [DOI] [PubMed] [Google Scholar]
- 43.Stevens GJ, Warfel JW, Aden JK, Blackwell SD. Intraoperative endotracheal cuff pressure study: How education and availability of manometers help guide safer pressures. Mil. Med. 2018;183:e416–e419. doi: 10.1093/milmed/usx127. [DOI] [PubMed] [Google Scholar]
- 44.Vyas D, Inweregbu K, Pittard A. Measurement of tracheal tube cuff pressure in critical care. Anaesthesia. 2002;57:275–277. doi: 10.1046/j.1365-2044.2002.2404_3.x. [DOI] [PubMed] [Google Scholar]
- 45.Chopra M, Jones L, Boulanger C, Benger J, Higginson I, Williamson D, et al. Prospective observational measurement of tracheal tube cuff pressures in the emergency department. Emerg. Med. J. 2010;27:270–271. doi: 10.1136/emj.2009.075200. [DOI] [PubMed] [Google Scholar]
- 46.Yildirim ZB, Uzunkoy A, Cigdem A, Ganidagli S, Ozgonul A. Changes in cuff pressure of endotracheal tube during laparoscopic and open abdominal surgery. Surg. Endosc. 2012;26:398–401. doi: 10.1007/s00464-011-1886-8. [DOI] [PubMed] [Google Scholar]
- 47.Lizy C, Swinnen W, Labeau S, Poelaert J, Vogelaers D, Vandewoude K, et al. Cuff pressure of endotracheal tubes after changes in body position in critically ill patients treated with mechanical ventilation. Am. J. Crit. Care. 2014;23:e1–8. doi: 10.4037/ajcc2014489. [DOI] [PubMed] [Google Scholar]
- 48.Brimacombe J, Keller C, Giampalmo M, Sparr HJ, Berry A. Direct measurement of mucosal pressures exerted by cuff and non-cuff portions of tracheal tubes with different cuff volumes and head and neck positions. Br. J. Anaesth. 1999;82:708–711. doi: 10.1093/bja/82.5.708. [DOI] [PubMed] [Google Scholar]
- 49.Bernhard WN, Yost L, Joynes D, Cothalis S, Turndorf H. Intracuff pressures in endotracheal and tracheostomy tubes. Related cuff physical characteristics. Chest. 1985;87:720–725. doi: 10.1378/chest.87.6.720. [DOI] [PubMed] [Google Scholar]
- 50.Rubes D, Klein AA, Lips M, Rulisek J, Kopecky P, Blaha J, et al. The effect of adjusting tracheal tube cuff pressure during deep hypothermic circulatory arrest: A randomised trial. Eur. J. Anaesthesiol. 2014;31:452–456. doi: 10.1097/EJA.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 51.Patel RI, Oh TH, Chandra R, Epstein BS. Tracheal tube cuff pressure. Changes during nitrous oxide anaesthesia following inflation of cuffs with air and saline. Anaesthesia. 1984;39:862–864. doi: 10.1111/j.1365-2044.1984.tb06570.x. [DOI] [PubMed] [Google Scholar]
- 52.Kumar P, Abhilasha SJ, Kaur K, Bharadwaj M, Singh A. Evaluation of audible leak versus pressure volume loop closure for polyvinyl chloride cuff and polyurethane microcuff in endotracheal tube inflated with air: a prospective randomized study. Med. Gas Res. 2021;11:6–11. doi: 10.4103/2045-9912.310053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rahmani F, Soleimanpour H, Zeynali A, Mahmoodpoor A, Shahsavari Nia K, Rahimi Panahi J, et al. Comparison of tracheal tube cuff pressure with two techniques: Fixed volume versus pilot balloon palpation. J. Cardiovasc. Thorac. Res. 2017;9:196–199. doi: 10.15171/jcvtr.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hockey CA, van Zundert AA, Paratz JD. Does objective measurement of tracheal tube cuff pressures minimise adverse effects and maintain accurate cuff pressures? A systematic review and meta-analysis. Anaesth. Intensive Care. 2016;44:560–570. doi: 10.1177/0310057X1604400503. [DOI] [PubMed] [Google Scholar]
- 55.Harvie DA, Darvall JN, Dodd M, De La Cruz A, Tacey M, D'Costa RL, et al. The minimal leak test technique for endotracheal cuff maintenance. Anaesth. Intensive Care. 2016;44:599–604. doi: 10.1177/0310057X1604400512. [DOI] [PubMed] [Google Scholar]
- 56.Xiang L, Cao M, Song X, Tan M, Deng T, Wang Y, et al. The effect of different inflating volume on the measurement accuracy of the modified cuff pressure measurement method. J. Clin. Monit. Comput. 2021;36:521–528. doi: 10.1007/s10877-021-00681-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arima H, Sobue K, Tanaka S, Morishima T, Ando H, Katsuya H. Airway obstruction associated with transesophageal echocardiography in a patient with a giant aortic pseudoaneurysm. Anesth. Analg. 2002;95:558–560. doi: 10.1097/00000539-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 58.Couture P, Denault AY, McKenty S, Boudreault D, Plante F, Perron R, et al. Impact of routine use of intraoperative transesophageal echocardiography during cardiac surgery. Can. J. Anaesth. 2000;47:20–26. doi: 10.1007/BF03020726. [DOI] [PubMed] [Google Scholar]
- 59.Bagate F, Rouzé A, Zerimech F, Boissier F, Labbe V, Razazi K, et al. Transesophageal echocardiography-associated tracheal microaspiration and ventilator-associated pneumonia in intubated critically ill patients: A multicenter prospective observational study. Crit. Care. 2020;24:679. doi: 10.1186/s13054-020-03380-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kallmeyer IJ, Collard CD, Fox JA, Body SC, Shernan SK. The safety of intraoperative transesophageal echocardiography: A case series of 7200 cardiac surgical patients. Anesth. Analg. 2001;92:1126–1130. doi: 10.1097/00000539-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 61.Da Costa LLM, Da Silva GM, Araújo Neto JA, Pinto LMM, Guimarães ARF, Lisboa Cordeiro AL. Effects of anesthesiologists awareness on the control of cuff pressure in patients submitted to cardiac surgery. J. Card. Surg. 2020;35:1243–1246. doi: 10.1111/jocs.14568. [DOI] [PubMed] [Google Scholar]
- 62.Hung KC, Chen YT, Chen JY, Kuo CY, Wu SC, Chiang MH, et al. Clinical characteristics of arytenoid dislocation in patients undergoing bariatric/metabolic surgery: A STROBE-complaint retrospective study. Medicine. 2019;98:e15318. doi: 10.1097/MD.0000000000015318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang MY, Huang CK, Chang PC. Hypopharyngeal perforation with mediastinal dissection during orogastric tube placement: A rare complication of bariatric surgery. Surg. Obes. Relat. Dis. 2016;12:e17–e19. doi: 10.1016/j.soard.2015.08.522. [DOI] [PubMed] [Google Scholar]
- 64.Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: a prospective evaluation. Eur. J. Anaesthesiol. 2005;22:307–311. doi: 10.1017/s0265021505000529. [DOI] [PubMed] [Google Scholar]
- 65.Juvin P, Lavaut E, Dupont H, Lefevre P, Demetriou M, Dumoulin JL, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesth. Analg. 2003;97:595–600. doi: 10.1213/01.ANE.0000072547.75928.B0. [DOI] [PubMed] [Google Scholar]
- 66.Krishna SG, Hakim M, Sebastian R, Dellinger HL, Tumin D, Tobias JD. Cuffed endotracheal tubes in children: the effect of the size of the cuffed endotracheal tube on intracuff pressure. Paediatr. Anaesth. 2017;27:494–500. doi: 10.1111/pan.13099. [DOI] [PubMed] [Google Scholar]
- 67.Seo H, Bang JY, Oh J, Choi WJ, Song JG, Hwang GS. Effect of tracheal cuff shape on intracuff pressure change during robot-assisted laparoscopic surgery: The tapered-shaped cuff tube versus the cylindrical-shaped cuff tube. J. Laparoendosc. Adv. Surg. Tech. A. 2015;25:724–729. doi: 10.1089/lap.2015.0152. [DOI] [PubMed] [Google Scholar]
- 68.Kako H, Goykhman A, Ramesh AS, Krishna SG, Tobias JD. Changes in intracuff pressure of a cuffed endotracheal tube during prolonged surgical procedures. Int. J. Pediatr. Otorhinolaryngol. 2015;79:76–79. doi: 10.1016/j.ijporl.2014.11.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.