This systematic review and meta-analysis evaluates whether the COVID-19 pandemic is associated with changes in neurodevelopmental outcomes during infancy.
Key Points
Question
Are neurodevelopmental outcomes during infancy changed by the COVID-19 pandemic?
Findings
This meta-analysis of 8 studies including 21 419 infants found that 7% of infants who had neurodevelopmental screening during the COVID-19 pandemic were at risk of neurodevelopmental impairment, and 12% of those with gestational exposure to SARS-CoV-2 were at risk for neurodevelopmental impairment. Communication impairment was the sole neurodevelopmental domain of significantly increased risk of occurrence during the COVID-19 pandemic.
Meaning
These findings suggest that overall neurodevelopment was not changed by the COVID-19 pandemic, but birth or being raised during the SARS-CoV-2 pandemic, regardless of gestational exposure, was associated with a significant risk of communication impairment among the infants.
Abstract
Importance
Primary studies proposed that aberrant maternal antiviral immunity and/or giving birth in quarantine, such as during the ongoing COVID-19 pandemic, may be associated with the risk of neurodevelopmental impairment (NDI) in offspring.
Objectives
To evaluate the associations of birth and being raised during the COVID-19 pandemic with risk of NDI among infants and to assess the association of gestational exposure to SARS-CoV-2 with risk of NDI.
Data Sources
PubMed, Web of Science, Scopus, Embase, and preprint servers were systematically searched from inception to March 25, 2022.
Study Selection
Studies evaluating the neurodevelopment of infants born during the SARS-CoV-2 pandemic were included in this systematic review and meta-analysis. Studies using Ages and Stages Questionnaires, Third Edition (ASQ-3), were used for quantitative meta-analysis.
Data Extraction and Synthesis
Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses, a random-effects model meta-analysis was used to pool the proportion and odds ratios (ORs) of overall NDI, as well as each developmental domain on ASQ-3 with the corresponding 95% CI.
Main Outcomes and Measures
The primary outcome was the risk of overall NDI among infants screened during the pandemic vs prepandemic. The secondary outcome was the comparison of NDI by ASQ-3 domain among infants born to women with known gestational exposure to SARS-CoV-2 vs no exposure.
Results
A total of 8 studies were included, including 21 419 infants (11 438 screened in pandemic and 9981 in prepandemic period). NDI was present in 330 of 8992 infants (7%; 95% CI, 4%-10%) screened during the COVID-19 pandemic from January 2020 to January 2021. Among the pandemic cohort, the prevalence of NDI among infants with gestational exposure to SARS-CoV-2 was 77 of 691 (12%; 95% CI, 6%-18%). Compared with the prepandemic cohort (2015-2019), the pandemic cohort was more likely to have communication impairment (OR, 1.70; 95% CI, 1.37-2.11; P < .001), without significant differences in other ASQ-3 domains (eg, gross motor, fine motor, personal-social, and problem-solving). In contrast, maternal SARS-CoV-2 infection was not associated with significant differences in any neurodevelopment domain in offspring, except for increasing the odds of fine motor impairment (OR, 3.46; 95% CI, 1.43-8.38; P < .001).
Conclusions and Relevance
In this systematic review and meta-analysis examining the association between COVID-19 pandemic and the risk of NDI, findings suggest that overall neurodevelopment in the first year of life was not changed by either being born or raised during the SARS-CoV-2 pandemic or by gestational exposure to SARS-CoV-2. Interestingly, the first year of life during the COVID-19 pandemic, regardless of maternal infection, was significantly associated with the risk of communication delay among the offspring.
Introduction
COVID-19, caused by SARS-CoV-2, persists as a global health emergency.1 Preliminary reports showed that pregnant individuals are at a higher risk of mortality and severe morbidity due to COVID-19, and consensus from the US Centers for Disease Control and Prevention supports the disproportionate risk that pregnancy imparts.2,3,4 According to the results of a living systematic review and meta-analysis,5 10% of pregnant women attending or admitted to hospitals for any reason, not only obstetrics-related issues, were suspected of having or had a diagnosis of COVID-19. At present, our understanding of the effects of maternal COVID-19 infection on short-term and long-term aspects of maternal-fetal health, including neurodevelopmental outcomes during infancy, remains limited.2
Neurodevelopmental disorders, such as autism spectrum disorder, intellectual disability, and attention-deficit/hyperactivity disorder, have heterogeneous causes associated with impaired cognition, communication, adaptive behavior, and psychomotor skills.6 The neurodevelopment of a fetus can be affected by different endogenous (direct fetal infection, maternal infection with vertical transmission, and neurologic abnormalities) or exogenous (maternal immune activation in the absence of vertical transmission, maternal environmental chemical or dietary factors, or marked and persistent maternal stress) factors.7,8,9,10,11 Maternal immune activation hypothesis proposes that inflammatory perturbations in utero can affect fetal neurodevelopment, and evidence from human epidemiological studies8,9 supports an association between maternal inflammation during pregnancy and offspring neurodevelopmental disorders.
Fortunately, maternal-fetal vertical transmission of SARS-CoV-2 is rare, although the impact of maternal infection on fetal and postnatal neurodevelopment is still poorly understood.12 Recently, a few cohort studies13,14,15,16 on this clinically important issue have been published with controversial results. Shuffrey et al,15 as one of the largest cohorts, assessed 255 infants born during the pandemic, and exposure to maternal SARS-CoV-2 infection was not associated with differences in neurodevelopmental screening scores at age 6 months, regardless of infection timing or severity. However, both infants with and without SARS-CoV-2 exposure born during that period had significantly lower scores on gross motor, fine motor, and personal-social subdomains compared with the prepandemic cohort.15
The net impact of the COVID-19 pandemic on potential risk of neurodevelopmental impairment (NDI) is of extreme importance. The current study aimed to determine whether (1) being born or raised during the COVID-19 pandemic and (2) gestational exposure to SARS-CoV-2 are associated with an increased risk of NDI during the first year of life using the Ages and Stages Questionnaires, Third Edition (ASQ-3), neurodevelopmental screening tool.
Methods
This systematic review and meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline. The study protocol for this systematic review was registered in the PROSPERO international prospective register of systematic reviews (Registration number: CRD42022315849).
Search Strategy
A literature search was performed by 2 independent authors (K.H. and N.Z.) using PubMed, Web of Science, and Embase from inception to March 25, 2022. The search was conducted from March 19 to March 25, 2022, with no language restriction using the following keywords: (COVID-19 OR Coronavirus OR Severe Acute Respiratory Syndrome OR Corona-virus OR 2019nCoV OR Corona Virus OR COVID OR COVID19 OR SARS CoV 2 OR SARS-CoV OR SARS-CoV-2) AND (neurodevelopment OR neurodevelopmental OR development disorder* OR developmental disorder* OR intellectual disability OR intellectual developmental disorder* OR mental retardation OR global developmental delay OR communication disorders OR gross motor OR fine motor OR personal social OR problem solving). The detailed search strategy is shown in eTable 1 in the Supplement. References of relevant articles were manually reviewed, and eligible studies were added to the results from the electronic literature search. Literature search and study selection were performed by 2 independent authors (N.Z. and A.N.), and discrepancies were resolved by consulting the third investigator (A.A.S.).
Eligibility Criteria
This review included only observational studies evaluating the risk of NDI among infants who had their neurodevelopmental screening during the COVID-19 pandemic. Only studies presenting data on infants undergoing neurodevelopmental screening up to 12 months corrected age follow-up were deemed eligible for inclusion. To be eligible for quantitative synthesis, studies were included if they defined “being at risk of NDI” as a composite or domain score at least 2 SDs below the established mean of the normal population reported by the standardized neurodevelopmental assessment tool of ASQ-3. Articles designed as case reports, narrative reviews, case series, dissertations, and letters or editorials were excluded. In terms of defining comparison groups, the risk of NDI was assessed among those who had screening during the pandemic vs those who had screening before the pandemic. As a secondary analysis, the risk of NDI was also assessed among those who were born during the pandemic with documented maternal SARS-CoV-2 infection vs those born during the pandemic with no maternal SARS-CoV-2 infection.
Study Selection
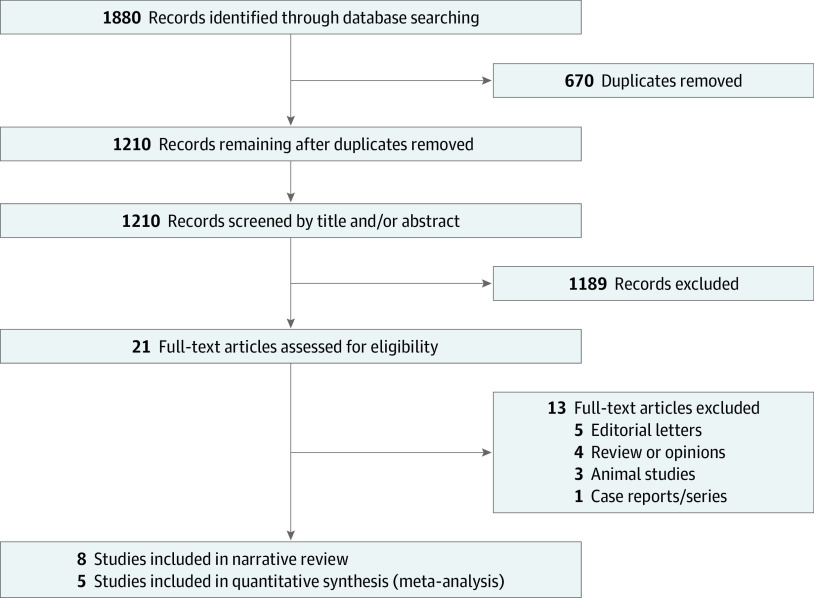
A total of 1880 articles were retrieved. Of these, 670 articles were excluded as duplicates, and the remaining 1210 studies were screened for eligibility. Screening of the title and abstract resulted in 21 potentially eligible studies. Following full-text assessment, 8 studies met the inclusion criteria defined earlier (Figure 1).
Figure 1. Study Flowchart.
Ages and Stages Questionnaires, Third Edition
The ASQ-3 is a parent-completed comprehensive neurodevelopmental screener with 30 items in 5 developmental domains: communication, gross motor, fine motor, problem-solving, and personal-social. Each of the 30 items describes a skill, ability, or behavior to which the parent responds yes (10 points), sometimes (5 points), or not yet (0 points).17 For the quantitative meta-analysis, the score calculated for each domain was categorized as normal development (above cutoff) or at risk of NDI, if the score was 2 SDs below the mean, which indicates a possible delay that requires further follow-up or referral.
Primary and Secondary Outcomes
The primary outcome measure was the prevalence of infants (up to 12 months after birth) at risk of NDI who had their neurodevelopmental screening during the COVID-19 pandemic compared with the prevalence of infants at high risk of NDI who had their screening before the pandemic. The secondary outcome measure was to compare the risk of NDI among pandemic-born infants who had in utero exposure to SARS-CoV-2 vs those who were born during the same time frame but with no in utero exposure to SARS-CoV-2.
Data Extraction
Data abstraction of included articles was performed by 2 independent authors (K.H. and N.Z.) using a standardized sheet. The following data were abstracted: author’s name, publication year, study design, the sample size of pandemic and prepandemic cohorts, maternal SARS-CoV-2 status during pregnancy, patients’ perinatal data, the definition of NDI, and age at neurodevelopmental screening. The corresponding author was contacted in case of missing data in an included study.
Quality Assessment
Newcastle-Ottawa Scale (NOS) was used to evaluate the quality of included studies and the risk of bias. NOS comprises participant selection, comparability of study groups, and assessment of outcome or exposure. A score of 7 or above was considered to be of high quality.18 Quality assessment selection was performed by 2 independent authors (K.H. and N.Z.), and discrepancies were resolved by the third investigator (A.A.S.).
Statistical Analysis
Statistical analysis was performed using Stata statistical software version 17 (StataCorp). Pooled effect sizes were presented as odds ratio (OR) with a 95% CI for categorical variables using DerSimonian and Laird method. Subgroup analysis was conducted to assess the risk of NDI according to the infantile age in which screening was performed (6 vs 12 months after birth). A 2-sided I2 test was used to examine heterogeneity across the included studies; I2 ≥ 50% and P < .05 indicate heterogeneity. A random-effects model was used due to the anticipated heterogeneity of included studies. Furthermore, publication bias was assessed using Egger and Begg tests.
Results
Demographic Characteristics
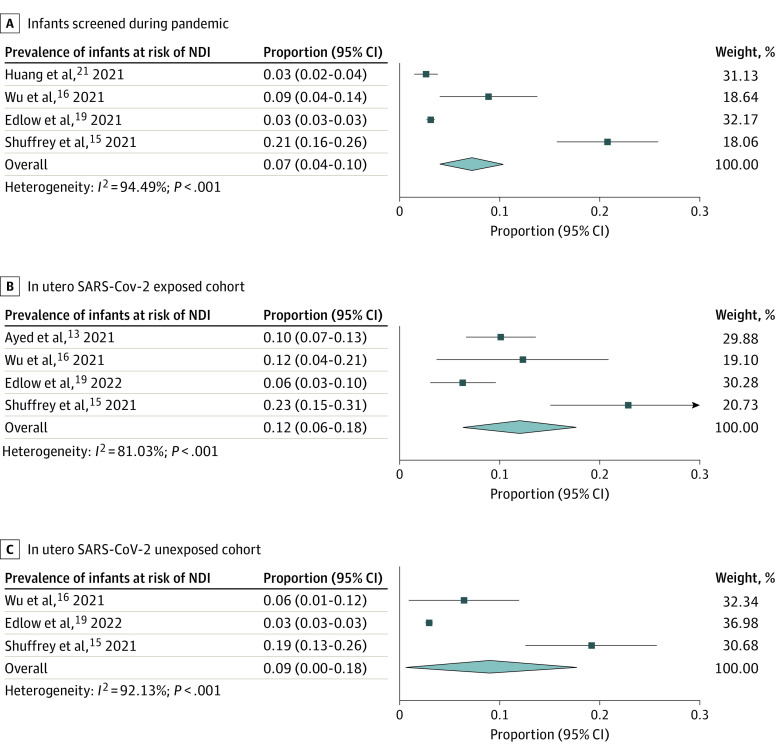
The Table presents characteristics of the included studies, drawn from an initial search strategy inclusive of 1210 titles for screening. All included studies were published between 2021 and 2022. Three studies were conducted in the US,15,19,20 3 in China,16,21,22 1 in Kuwait,13 and 1 in Canada.23 Five studies were designed as prospective,13,15,16,21,23 1 study as retrospective,19 and designs were not reported for 2 studies.20,22 A total of 21 419 infants who underwent neurodevelopmental screening were included in this systematic review, of whom 11 438 and 9981 were screened during the pandemic and prepandemic periods, respectively. Among those infants screened during the pandemic, 700 had documented confirmed maternal infection with SARS-CoV-2 during pregnancy, 7778 had no documented maternal infection, and the status of maternal SARS-CoV-2 exposure or infection was not known for the remainder (2960). As shown in Figure 2A, 7% (330 of 8992 infants; 95% CI, 4%-10%) of infants who had their neurodevelopmental screening during the pandemic were found to be at risk of NDI. Among the pandemic-born cohort, the prevalence of NDI among infants with confirmed maternal COVID-19 during pregnancy was 12% (77 of 691 infants; 95% CI, 6%-18%) (Figure 2B). For those who were born during the pandemic but had no maternal COVID-19 infection, the risk of NDI was 9% (330 of 8992 patients; 95% CI, 0%-18%) (Figure 2C).
Table. Characteristics of Studies Included in Both Quantitative and Qualitative Systematic Review and Meta-analyses.
| Source (Location) | Study design | Pandemic cohort, No. (No. COVID-19 positive/ No. COVID-19 negative) | Trimester of pregnancy at the time of COVID-19 infection | Prepandemic cohort, No. | Study period | Age at follow-up, mo | Infants, No./total No. (%) | NDI assessment tool | NOS score | |
|---|---|---|---|---|---|---|---|---|---|---|
| Incidence of NDI during pandemic | Incidence of NDI among COVID-19–positive population | |||||||||
| Studies included in systematic review and meta-analysis (quantitative analysis) | ||||||||||
| Shuffrey et al,15 2021, (US) | Prospective | 255 (114/141) | 30.7% in the third, 47.4% in the second, 21.9% in the first trimester | 62 | Oct 7, 2020, to Jun 17, 2021 | 6 | 53/255 (20.8) | 26/114 (22.8) | ASQ-3 | 8 |
| Wu et al,16 2021, (China) | Prospective | 135 (57/78) | 93% in the third and 7% in the second trimester | NR | May 1 to Oct 31, 2020 | 3 | 12/135 (8.9) | 7/57 (13.5) | ASQ-3 | 7 |
| Imboden et al,20 2021 (US) | NR | 506 (NR) | NR | 518 | Oct 2020 to Jan 2021 | 6 and 12 | NR | NR | ASQ-3 | 6 |
| Huang et al,21 2021 (China) | Prospective | 831 (NR) | NR | 5223 | March 1 to May 15, 2020 | 6 and 12 | 24/830 (2.9) | NR | ASQ-3 | 7 |
| Giesbrecht et al,23 2022 (Canada) | Prospective | 1623 (NR) | NR | 4178 | Started from Apr 2020 | 12 | NR | NR | ASQ-3 | 6 |
| Studies included in systematic review only (qualitative analysis) | ||||||||||
| Cheng et al,22 2021 (China) | NR | 18 (9/9) | 100% in the third trimester | NA | NR | 3 | NR | NR | ASQ-3 | 6 |
| Ayed et al,13 2021 (Kuwait) | Prospective | 298 (298/0) | 91.6% in the third, 6.7% in the second, and 1.7% in the first trimester | NA | Apr 1 to Dec 30, 2020 | 10-12 | NR | 30/298 (10.1) | ASQ-3 | 8 |
| Edlow et al,19 2021 (US) | Retrospective | 7772 (222/7550) | 72% in the third, 27% in the second, and 0.5% in the first trimester | NA | Between Mar and Sep 2020 | 12 | 241/7772 (3.1) | 14/222 (6.3) | ICD-10 | 7 |
Abbreviations: ASQ-3, Age and Stage Questionnaire, Third Edition; ICD-10, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; NA, not applicable; NDI, neurodevelopmental impairment; NOS, Newcastle Ottawa Scale; NR, not reported.
Figure 2. Prevalence of Risk for Neurodevelopmental Impairment (NDI) Among Infants Screened During the Pandemic, In Utero SARS-CoV-2–Exposed Cohort, and In Utero SARS-CoV-2–Unexposed Cohort.
Analyses used a random-effects DerSimonian Laird model.
Neurodevelopment Screening During the COVID-19 Pandemic vs Before Pandemic
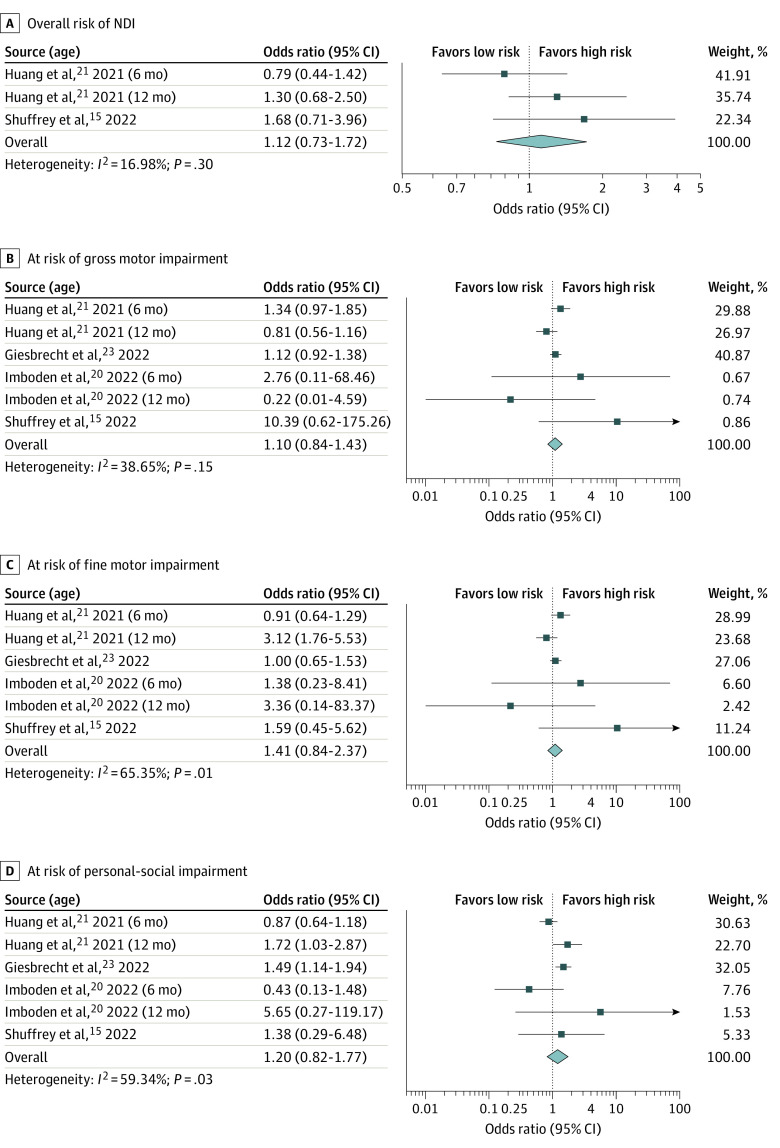
Overall, there was no significant difference regarding the overall risk of NDI, adjusted for prematurity, among infants screened during the pandemic compared with those screened before the pandemic (OR, 1.12; 95% CI, 0.73-1.72; P = .61; I2 = 17%). Additionally, there was no significant difference in terms of ASQ-3 domains, including gross motor (OR, 1.10; 95% CI, 0.84-1.43; P = .49; I2 = 39%), fine motor (OR, 1.41; 95% CI, 0.84-2.37; P = .20; I2 = 65%), personal-social (OR, 1.20; 95% CI, 0.82-1.77; P = .34; I2 = 59%), and problem-solving (OR, 0.97; 95% CI, 0.79-1.19; P = .75; I2 = 0.0%), except for an increased risk of communication impairment (OR, 1.70; 95% CI, 1.37-2.11; P < .001; I2 = 0.0%) among infants who were born during the pandemic (Figure 3 and eFigure 1 in the Supplement).
Figure 3. Meta-analysis of Overall Risk of Neurodevelopmental Impairment and Gross Motor, Fine Motor, and Personal-Social Domains Among Infants Screened During Pandemic vs Before Pandemic.
Analyses used a random-effects DerSimonian Laird model.
Subgroup analysis was performed according to the infantile age in which neurodevelopmental screening was performed. At age 6 months, the risk of NDI was comparable between pandemic and prepandemic screening groups. However, infants screened during the pandemic were more likely to have higher risk of communication (OR, 1.86; 95% CI, 1.15-3.00; P = .01; I2 = 70%) and personal-social (OR, 1.55; 95% CI, 1.22-1.96; P < .001; I2 = 0.0%) impairment at age 12 months (eTable 2 in the Supplement).
Risk of NDI According to the Status of In Utero Exposure to SARS-CoV-2
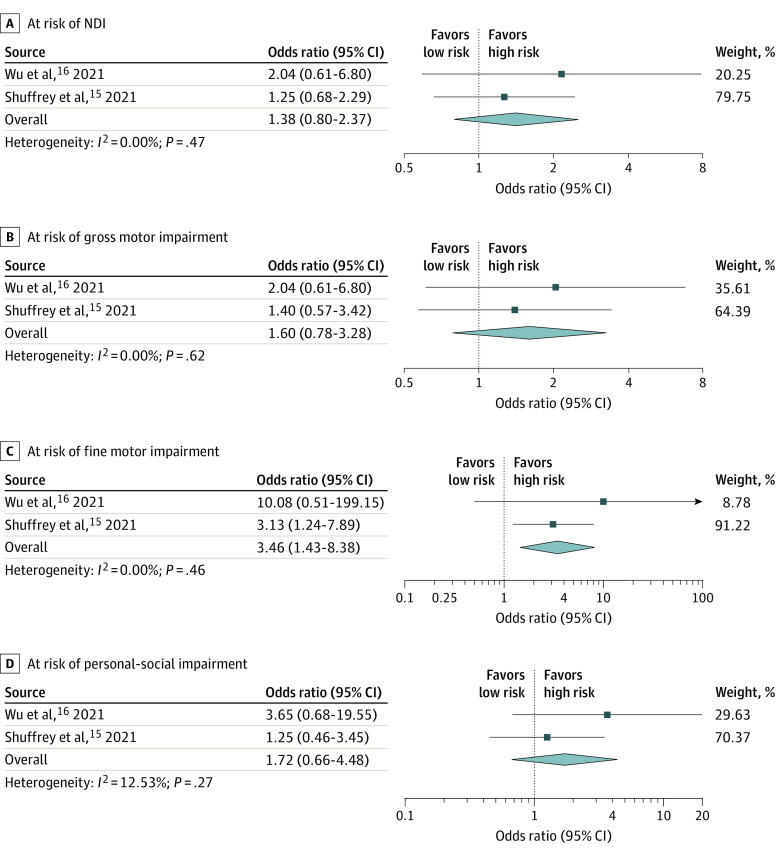
There was no significant difference regarding the overall NDI risk among infants born after gestational exposure to SARS-CoV-2 compared with those who had no exposure (OR, 1.38; 95% CI, 0.80-2.37; P = .24; I2 = 0.0%). Additionally, there was no significant difference in terms of ASQ-3 domains, including gross motor (OR, 1.60; 95% CI, 0.78-3.28; P = .46; I2 = 0.0%), communication (OR, 0.53; 95% CI, 0.15-1.89; P = .33; I2 = 0.0%), personal-social (OR, 1.72; 95% CI, 0.66-4.49; P = .27; I2 = 13%), and problem-solving (OR, 1.20; 95% CI, 0.57-2.51; P = .63; I2 = 0.0%), except for an increased risk of fine motor impairment (OR, 3.46; 95% CI, 1.43-8.38; P = .006; I2 = 0.0%) among infants who were exposed to SARS-CoV-2 in utero (Figure 4 and eFigure 2 in the Supplement).
Figure 4. Meta-analysis of Overall Risk of Neurodevelopmental Impairment (NDI) and Gross Motor, Fine Motor, and Personal-Social Domains Among In Utero Exposed vs Unexposed Pandemic-Born Cohorts.
Analyses used a random-effects DerSimonian Laird model.
Quality Assessment
The overall score for the studies was between 6 and 8 out of a possible score of 9 (Table). Three studies20,22,23 had score of 6, 3 studies16,19,21 had score of 7, and 2 studies13,15 had score of 8. There was no publication bias for risk of overall NDI according to either the Egger test or the Begg test.
Discussion
This systematic review and meta-analysis reports the potential association of the COVID-19 pandemic during pregnancy with neurodevelopmental outcomes during infancy. For infants screened before and during the pandemic, we found no significant differences in the overall risk of NDI. However, analyses of individual domains of development revealed infants screened during the pandemic were more likely to be at risk of communication impairment compared with their prepandemic counterparts. Our findings suggest that known maternal SARS-CoV-2 infection was associated with a significantly greater risk of fine motor impairment but no increased risk of impairment in any other domain of neurodevelopment.
Neurodevelopmental impairments presenting during infancy can be secondary to genetic susceptibility,6 preterm birth,24 perinatal inflammation, infection,7 diet,25 socioeconomic factors, maternal and placental health, and congenital anomalies. Maternal infection with SARS-CoV-2 during pregnancy is associated with preterm birth5 and inflammation26 and can lead to mental health problems including anxiety and depression.27 Unlike Zika virus, which has a fairly high maternal-fetal vertical transmission rate associated with a well-described spectrum of congenital manifestations, including microcephaly, cerebral palsy, and developmental delays,11,28 SARS-CoV-2 rarely crosses the placenta and is not associated with overt placental pathology.14,29,30 During the COVID-19 pandemic, financial strain, social isolation, and decreased family support have been associated with increased maternal depressive and anxiety symptoms in the perinatal period,31 which are known to be associated with neurodevelopmental and behavioral disorders. Higher levels of COVID-19–related stress were reported for both mothers and fathers of infants aged 0 to 6 months and were associated with insensitive parenting practices, including decreased emotional responsiveness in only mothers, which could lessen the reciprocal exchanges that support language development in early childhood.32,33 Additionally, opportunities to promote language and social development through new experiences outside the home, including visits with extended family and friends or attendance at a child care center, were lessened for many during the pandemic.
Strengths and Limitations
Among the most important strengths of this study included not limiting our included studies to only English publications, incorporating a highly sensitive search strategy inclusive of 1210 titles for screening, and a novel question with unanticipated findings. Our study is also prone to limitations in the heterogeneity of outcome measures, including limitations of quantitative analyses in 5 studies. An inherent limitation of the ASQ-3 questionnaire is its use as a screening instrument based on parent reports rather than objective assessment. Additionally, the sensitivity in detecting subtle but significant impairments in infancy is challenging compared with severe impairments or at later developmental stages. Given the novel finding of communication impairment as a result of being born during the COVID-19 pandemic, we were limited by a lack of data regarding the prevalence of social distancing among affected vs unaffected participants. Additionally, to better understand the subtle association of maternal SARS-CoV-2 infection during pregnancy with NDI warrants further investigation, with granular data on maternal-fetal COVID-19 illness and rigorous assessments of the potential for fetal SARS-CoV-2 exposures, which is beyond the scope of this review.
The ASQ-3 was administered by trained psychological evaluators in the Huang et al21 study, whereas in other included studies, the ASQ-3 is completed by caregivers or mothers. This might introduce variability in the results which should be interpreted with caution.
Clearly, although our observations raise potential concerns regarding the early developmental trajectory of children born during the COVID-19 pandemic, long-term follow-up behavioral assessments would be necessary to see whether this is borne out during early childhood or indeed whether catch-up occurring after the follow-up period is limited to the first year of life, and to extrapolate further into early childhood. As such, we consider the principal value of our current meta-analysis lies in its importance in generating novel hypotheses warranting further study.
Conclusions
This systematic review and meta-analysis reveals a novel set of observations showing that being born and raised during the COVID-19 pandemic is associated with the risk of communication impairment among infants, with no evident association with other measures of neurodevelopment. More extensive studies with extended follow-up periods would provide more concrete insights into the long-term neurodevelopmental outcomes for infants and young children born during the pandemic and are, thus, warranted.
eTable 1. Search Strategy
eTable 2. Subgroup Analysis of Neurodevelopmental Impairment According to the Age at Which Screening Has Been Performed
eFigure 1. Meta-analysis Results on Risk of (a) Problem-solving and (b) Communication Among Infants Screened During Pandemic vs Before Pandemic
eFigure 2. Meta-analysis Results on Risk of (a) Problem-solving and (b) Communication Among In Utero Exposed vs Unexposed Pandemic-Born Cohorts
References
- 1.The Lancet . COVID-19: learning as an interdependent world. Lancet. 2021;398(10306):1105. doi: 10.1016/S0140-6736(21)02125-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Centers for Disease Control and Prevention . COVID-19 during pregnancy. 2022. Accessed April 1, 2022. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19/what-cdc-is-doing.html
- 3.Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, et al. Maternal death due to COVID-19. Am J Obstet Gynecol. 2020;223(1):109.e1-109.e16. doi: 10.1016/j.ajog.2020.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hessami K, Homayoon N, Hashemi A, Vafaei H, Kasraeian M, Asadi N. COVID-19 and maternal, fetal and neonatal mortality: a systematic review. J Matern Fetal Neonatal Med. 2022;35(15):2936-2641. doi: 10.1080/14767058.2020.1806817 [DOI] [PubMed] [Google Scholar]
- 5.Allotey J, Stallings E, Bonet M, et al. ; for PregCOV-19 Living Systematic Review Consortium . Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320. doi: 10.1136/bmj.m3320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parenti I, Rabaneda LG, Schoen H, Novarino G. Neurodevelopmental disorders: from genetics to functional pathways. Trends Neurosci. 2020;43(8):608-621. doi: 10.1016/j.tins.2020.05.004 [DOI] [PubMed] [Google Scholar]
- 7.Al-Haddad BJS, Oler E, Armistead B, et al. The fetal origins of mental illness. Am J Obstet Gynecol. 2019;221(6):549-562. doi: 10.1016/j.ajog.2019.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jash S, Sharma S. Pathogenic infections during pregnancy and the consequences for fetal brain development. Pathogens. 2022;11(2):193. doi: 10.3390/pathogens11020193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernandes DJ, Spring S, Roy AR, et al. Exposure to maternal high-fat diet induces extensive changes in the brain of adult offspring. Transl Psychiatry. 2021;11(1):149. doi: 10.1038/s41398-021-01274-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lautarescu A, Craig MC, Glover V. Prenatal stress: effects on fetal and child brain development. Int Rev Neurobiol. 2020;150:17-40. doi: 10.1016/bs.irn.2019.11.002 [DOI] [PubMed] [Google Scholar]
- 11.Ades AE, Soriano-Arandes A, Alarcon A, et al. Vertical transmission of Zika virus and its outcomes: a bayesian synthesis of prospective studies. Lancet Infect Dis. 2021;21(4):537-545. doi: 10.1016/S1473-3099(20)30432-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kotlyar AM, Grechukhina O, Chen A, et al. Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224(1):35-53.e3. doi: 10.1016/j.ajog.2020.07.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ayed M, Embaireeg A, Kartam M, et al. Neurodevelopmental outcomes of infants secondary to in utero exposure to maternal SARS-CoV-2 infection: a national prospective study in Kuwait. medRxiv. Preprint posted online November 14, 2021. doi: 10.1101/2021.11.12.21266291 [DOI]
- 14.Edlow AG, Li JZ, Collier AY, et al. Assessment of maternal and neonatal SARS-CoV-2 viral load, transplacental antibody transfer, and placental pathology in pregnancies during the COVID-19 pandemic. JAMA Netw Open. 2020;3(12):e2030455. doi: 10.1001/jamanetworkopen.2020.30455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shuffrey LC, Firestein MR, Kyle MH, et al. Association of birth during the COVID-19 pandemic with neurodevelopmental status at 6 months in infants with and without in utero exposure to maternal SARS-CoV-2 infection. JAMA Pediatr. 2021;176(6):e215563.doi: 10.1186/1471-2288-14-4510.1001/jamapediatrics.2021.5563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu T, Chen L, Wang Y, et al. Effects of SARS-CoV-2 infection during late pregnancy on early childhood development: a prospective cohort study. Front Pediatr. 2021;9:750012. doi: 10.3389/fped.2021.750012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Squires J, Bricker DD. Ages & Stages Questionnaires. Paul H Brookes; 2009. [Google Scholar]
- 18.Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45. doi: 10.1186/1471-2288-14-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edlow AG, Castro VM, Shook LL, Kaimal AJ, Perlis RH. Neurodevelopmental outcomes at one year in offspring of mothers who test positive for SARS-CoV-2 during pregnancy. medRxiv. Preprint posted online December 16, 2021. doi: 10.1101/2021.12.15.21267849 [DOI]
- 20.Imboden A, Sobczak BK, Griffin V. The impact of the COVID-19 pandemic on infant and toddler development. J Am Assoc Nurse Pract. 2022;34(3):509-519. doi: 10.1097/JXX.0000000000000653 [DOI] [PubMed] [Google Scholar]
- 21.Huang P, Zhou F, Guo Y, et al. Association between the COVID-19 pandemic and infant neurodevelopment: a comparison before and during COVID-19. Front Pediatr. 2021;9:662165. doi: 10.3389/fped.2021.662165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng Y, Teng H, Xiao Y, Yao M, Yin J, Sun G.. Impact of SARS-CoV-2 infection during pregnancy on infant neurobehavioral development: a case-control study. Front Pediatr. 2021;9:762684. doi: 10.3389/fped.2021.762684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giesbrecht G, Lebel C, Dennis C-L, Tough S, McDonald S, Tomfohr-Madsen L. Increased risk for developmental delay among babies born during the pandemic. PsyArXiv. Preprint posted online February 3, 2022. doi: 10.31234/osf.io/j7kcn [DOI]
- 24.Hee Chung E, Chou J, Brown KA. Neurodevelopmental outcomes of preterm infants: a recent literature review. Transl Pediatr. 2020;9(suppl 1):S3-S8. doi: 10.21037/tp.2019.09.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bragg M, Chavarro JE, Hamra GB, et al. Prenatal diet as a modifier of environmental risk factors for autism and related neurodevelopmental outcomes. Curr Environ Health Rep. 2022;9(2):324-338. doi: 10.1007/s40572-022-00347-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ragab D, Salah Eldin H, Taeimah M, Khattab R, Salem R. The COVID-19 cytokine storm: what we know so far. Front Immunol. 2020;11:1446. doi: 10.3389/fimmu.2020.01446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loades ME, Chatburn E, Higson-Sweeney N, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59(11):1218-1239.e3. doi: 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carvalho A, Sales HF, Ventura P, Gnoatto-Medeiros M, Brites C, Lucena R. The neurodevelopmental spectrum of congenital Zika infection: a scoping review. Dev Med Child Neurol. 2020;62(12):1356-1362. doi: 10.1111/dmcn.14675 [DOI] [PubMed] [Google Scholar]
- 29.Huynh A, Sehn JK, Goldfarb IT, et al. SARS-CoV-2 placentitis and intraparenchymal thrombohematomas among COVID-19 infections in pregnancy. JAMA Netw Open. 2022;5(3):e225345. doi: 10.1001/jamanetworkopen.2022.5345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hessami K, Aagaard KM, Castro EC, et al. Placental vascular and inflammatory findings from pregnancies diagnosed with coronavirus disease 2019: a systematic review and meta-analysis. Am J Perinatol. May 31, 2022. doi: 10.1055/a-1787-7933 [DOI] [PubMed] [Google Scholar]
- 31.Chatterjee P, Nirgude A, Chatterjee PK. Healthy eating—a modifiable contributor to optimize healthy living in the COVID-19 pandemic: a review. J Sci Food Agric. 2022;102(5):1751-1758. doi: 10.1002/jsfa.11650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buechel C, Nehring I, Seifert C, et al. A cross-sectional investigation of psychosocial stress factors in German families with children aged 0-3 years during the COVID-19 pandemic: initial results of the CoronabaBY study. Child Adolesc Psychiatry Ment Health. 2022;16(1):37. doi: 10.1186/s13034-022-00464-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hessami K, Romanelli C, Chiurazzi M, Cozzolino M. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2020;35(20):4014-4021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Search Strategy
eTable 2. Subgroup Analysis of Neurodevelopmental Impairment According to the Age at Which Screening Has Been Performed
eFigure 1. Meta-analysis Results on Risk of (a) Problem-solving and (b) Communication Among Infants Screened During Pandemic vs Before Pandemic
eFigure 2. Meta-analysis Results on Risk of (a) Problem-solving and (b) Communication Among In Utero Exposed vs Unexposed Pandemic-Born Cohorts