Abstract
Introduction
Hypertension is an important cause of morbidity and mortality worldwide. Undiagnosed hypertension is a serious issue that leads to increased morbidity and mortality. In this study, we aim to identify the prevalence of undiagnosed hypertension in the healthy Jordanian population, as well as identify predictors of high blood pressure readings in presumably healthy Jordanians.
Materials and Methods
We recruited healthy visitors accompanying patients at our Jordan University Hospital Clinics ranging from 18 to 80 years of age. We measured each participant’s systolic and diastolic blood pressure at our outpatient clinics on two different days, one week apart. We also obtained demographic data, weight, height, smoking status, and family history of hypertension and cardiovascular diseases.
Results
A total of 896 participants were included in this study with a mean age of 48 years. The median of systolic blood pressure readings was 125 mmHg, and the median of diastolic blood pressure readings was 83 mmHg. 38.5% had undiagnosed stage 1 hypertension and 30.5% had undiagnosed stage 2 hypertension according to the American College of Cardiology/American Heart Association guidelines. On the other hand, 25.4% had undiagnosed grade 1 hypertension and 5.1% had undiagnosed grade 2 hypertension according to the European Society of Hypertension guidelines.
Conclusion
According to the ACC/AHA guidelines, 68.5% of previously healthy Jordanians met the criteria to be diagnosed with hypertension. Predictors of high systolic blood pressure were age, BMI and family history of CAD, while female gender is associated with a lower systolic blood pressure. For diastolic blood pressure, only BMI and family history of CAD were associated with significantly higher diastolic blood pressure, while female gender and exercise were significantly associated with lower diastolic blood pressure.
Keywords: blood pressure, hypertension, systolic, diastolic
Introduction
Hypertension is an important cause of morbidity and mortality worldwide, directly causing around 7.5 million deaths worldwide yearly, accounting for 12.8% of all deaths and 3.7% of disability adjusted life years (DALYs).1 Hypertension is one of the leading risk factors for cardiovascular diseases (CVD), the most common cause of death worldwide.2 In the Eastern Mediterranean Region (EMR), one-third of all deaths are related to CVDs, with one-half of them being due to high systolic blood pressure3 Furthermore, the age-standardized DALY rate for CVDs was found to be considerably higher in the EMR than the global average.3 The risk factors and predictors of hypertension in the general population are well established, with increasing age, male gender, and higher weight being important predictors.4 The prevalence of hypertension in the Arab world is reported to be 29.5%, higher than the USA and Sub-Saharan Africa.5
Prevalence of hypertension in the general Jordanian population is comparable to the average in the Arab world, with almost one in every three Jordanian adults having elevated blood pressure.6 Of those with hypertension, almost 60% were aware of their diagnosis, a significant increase from 2009 when awareness was reported to be 40% in males and 52% in females.6
The prevalence rate of hypertension in Jordan is high and rising.7 At the same time, the level of awareness is low along with suboptimal treatment and control among Jordanian hypertensive patients.7
Undiagnosed hypertension is a serious issue that leads to increased morbidity and mortality due to the delay of starting treatment. In the USA, the predicted prevalence of undiagnosed hypertension is 3.3–8.3%.8 In the Arab world, the awareness towards a diagnosis of hypertension ranged between 14% and 82%, indicating the presence of barriers to optimal healthcare systems and appropriate diagnosis of hypertension.9
There are two main guidelines to diagnose hypertension; the American College of Cardiology (ACC)/American Heart Association (AHA) guidelines published in 2017 and the European Society of Cardiology (ESC)/European Society of Hypertension (ESH) guidelines in published in 2018.10 Table 1 shows the comparison between the ACC/AHA and ESC/ESH guidelines to diagnose hypertension.
Table 1.
Comparison Between the ACC/AHA and ESC/ESH Guidelines to Diagnose Hypertension
| ACC/AHA (2017) | ESC/ESH (2018) | |
|---|---|---|
| Definition of Hypertension (mm Hg) | ≥130/80 | ≥140/90 |
| Normal Blood Pressure ranges (mm Hg) | Normal: <120/80 Elevated: 120–129/<80 |
Optimal: <120/80 Normal: 120–129/80–84 High normal: 130–139/85–89 |
| Hypertension Stages (mm Hg) | Stage 1: 130–139/80–89 Stage 2: ≥140/90 |
Grade 1: 140–159/90–99 Grade 2: 160–179/100–109 Grade 3: ≥180/110 |
Abbreviations: ACC, American College of Cardiology; AHA, American Heart Association; ESC, European Society of Cardiology; ESH, European Society of Hypertension.
In this study, we aim to identify the prevalence of undiagnosed hypertension in the healthy Jordanian population, as well as identify predictors of high blood pressure readings in healthy Jordanians.
Methods
Study Design
This was a cross-sectional study conducted in a tertiary referral hospital in Jordan. This study was approved by the University of Jordan Institutional Review Board committee and was conducted in concordance with the Declaration of Helsinki’s latest report. Each included participant signed an informed consent after detailing the nature and the purpose of the study. This study was conducted from June 2021 through June 2022 at Jordan University Hospital (JUH), a tertiary medical center in Jordan.
Participants
We recruited healthy visitors accompanying patients at our Jordan University Hospital Clinics ranging from 18 to 80 years of age. Jordan University Hospital is one of the main tertiary centers in Jordan that provide services to people from all over Jordan and we had chosen participants in our study in a way to cover most of the geographical areas in the country of Jordan. We only included healthy subjects who were not previously diagnosed with hypertension, diabetes or cardiac diseases based on a detailed history and reviewing their medical records. We recruited participants via an announcement published at different locations at our healthcare facilities.
Assessment
Each eligible participant was instructed not to drink coffee, tea or other caffeinated drinks for at least one hour prior to BP measurement. Proper steps for blood pressure measurement were taken such as having the participant sit and relax for at least 5 minutes prior to taking blood pressure readings, removing all clothing over the participant’s arm, placing the BP cuff at the level of the heart, and supporting the arm and back during measurement. We checked the BP on two different days one week apart. We measured each participant’s blood pressure in the left arm two times on each day two minutes apart. We used the average of the averaged two readings to estimate the participant’s level of BP. We also measured each participant’s height and weight. We also recorded each participant’s exercise activity, in which participants performing at least 150 minutes per week of moderate-intensity aerobic activity or 75 minutes per week of vigorous aerobic activity, or a combination of both, were considered participants doing adequate routine exercise.
For blood pressure measurement, we used an upper arm automated blood pressure device (an Omron 705IT (HEM-759-E)) for blood pressure measurement, a validated blood pressure device.11 We also obtained personal history of smoking, family history of hypertension and cardiovascular diseases. The prevalence of undiagnosed hypertension was calculated among our sample according to the American College of Cardiology/American Heart Association and the European Society of Hypertension guidelines.12,13
Statistical Analysis
All data were collected in a computerized database and analyzed by Statistical Package for the Social Science software version 26 (SPSS Inc., Chicago, IL, USA). A minimum sample size of 320 to 323 study participants was determined by single population proportion sample size calculation formula taking prevalence of hypertension among Arab and Jordanian adults as 29.5% and 30% respectively,5,6 CI of 95%, and absolute precision or tolerable margin of error of 5%. The sample distributions of demographic and clinical characteristics were examined using standard descriptive statistics with continuous variables being summarized using medians and interquartile-ranges, and categorical variables being described using frequencies and percentages. Normal distribution of the quantitative variables was assessed by Shapiro–Wilk test. Chi-square test was used to explore qualitative factors associated with undiagnosed hypertension.
To identify independent determinants of systolic and diastolic blood pressure levels, we performed a bivariate and multivariate linear regression analysis for each of them separately. Bivariate analysis through linear regression was used to calculate the unadjusted relationships between demographic, clinical and anthropometric indices as predictors and systolic or diastolic blood pressure readings as outcome variables. Predictor variables that were found to have P-values <0.20 on bivariate analyses were included in the multivariate regression model. A multiple linear regression analysis with backward-selection was conducted to develop a parsimonious predictive model for the each of the dependent variables (ie, systolic and diastolic blood pressure readings). The criterion for the removal of the candidate predictor variables from the multivariate model was set at P<0.10. The assumption of residual variance homogeneity and residual independency was also assessed and confirmed by scatter plot of residuals versus predicted values and Durbin–Watson statistics, respectively. There was no collinearity among independent variables which were assessed by variance inflation factor (values <10). Further data screening was conducted to ensure no violations of the assumptions of normality, linearity, homoscedasticity, and no additivity. The level of statistical significance was set at 0.05.
Results
A total of 896 participants were included in this study with a median age was 48 (27) years, they were 429 (47.9%) men and 467 (52.1%) women. Table 2 presents the characteristics of the whole sample, which included 896 participants, not previously diagnosed with hypertension, diabetes, or coronary artery disease (CAD). Categorical variables are expressed as percentages and continuous variables are expressed as median (IQR). The median BMI was 26.7 (6.2) kg/m2 corresponding to being overweight. The percentage of current smokers was 28.7%. The median of systolic blood pressure readings was 125 (22) mmHg, while the median of diastolic blood pressure readings was 83 (13) mmHg.
Table 2.
Sociodemographic Data and Characteristics of Study Sample (N = 896)
| Demographics and Characteristics | |
|---|---|
| Age | 48 (27) Years |
| % Males | 429/896 (47.9%) |
| BMI | 26.7 (6.2) kg/m2 |
| % Smokers | 257/896 (28.7%) |
| Systolic Blood Pressure | 125 (22) mmHg |
| Diastolic Blood Pressure | 83 (13) mmHg |
| American College of Cardiology/American Heart Association (ACC/AHA) | |
| Stage 1 (130–139 or 80–89) | 345/896 (38.5%) |
| Stage 2 (≥ 140/90) | 274/896 (30.5%) |
| Stage 1(among males) | 161/429 (37.5%) |
| Stage 2 (among males) | 159/429 (37.0%) |
| Stage 1 (among females) | 184/467 (39.4%) |
| Stage 2 (among females) | 115/467 (24.6%) |
| European Society of Hypertension | |
| Grade 1 (140–159/90–99) | 228/896 (25.4%) |
| Grade 2/3 (≥160/100) | 46/896 (5.1%) |
| Grade 1 (among males) | 133/429 (31.0%) |
| Grade 2 (among males) | 26/429 (6.1%) |
| Grade 1 (among females) | 95/467 (20.0%) |
| Grade 2 (among females) | 20/467 (4.3%) |
Among the included sample, 38.5% had undiagnosed stage 1 hypertension and 30.5% had undiagnosed stage 2 hypertension according to the American College of Cardiology/American Heart Association guidelines. Among males, 37.5% had undiagnosed stage 1 hypertension and 37.0% had undiagnosed stage 2 hypertension, as compared to 39.4% with undiagnosed stage 1 hypertension and 24.6% with undiagnosed stage 2 hypertension among females according to the American College of Cardiology/American Heart Association guidelines.
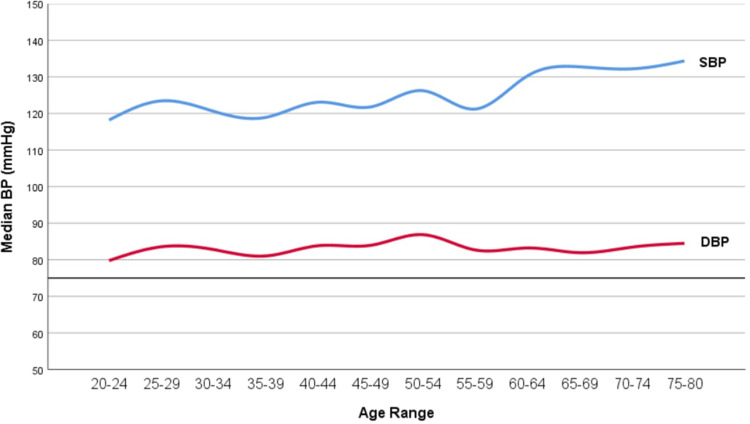
On the other hand, 25.4% had undiagnosed grade 1 hypertension and 5.1% had undiagnosed grade 2 hypertension according to the European Society of Hypertension guidelines. Among males, 31.0% had undiagnosed grade 1 hypertension and 6.1% had undiagnosed grade 2 hypertension, as compared to 20.0% with undiagnosed grade 1 hypertension and 4.3% with undiagnosed grade 2 hypertension among females according to the European Society of Hypertension guidelines. Table 3 presents the median of systolic and diastolic blood pressure readings among each age group, along with the prevalence of undiagnosed hypertension. Factors significantly associated with having undiagnosed hypertension according to the American College of Cardiology/American Heart Association guidelines were higher age (p < 0.001), female gender (p = 0.001), obesity (p = 0.002), and family history of CAD (p = 0.002). Factors significantly associated with having undiagnosed hypertension according to the European Society of Hypertension guidelines were similar to the American guidelines, but additionally family history of HTN was a significant factor associated with undiagnosed hypertension (p = 0.002) (Tables 3 and 4). Figure 1 illustrates the trends of systolic and diastolic blood pressure among different age groups.
Table 3.
Mean Systolic and Diastolic Blood Pressure Readings and the Prevalence of Undiagnosed Hypertension Among Study Sample Stratified by Age Groups
| Age Group (Years) | American College of Cardiology/American Heart Association | European Society of Hypertension | Systolic BP (mmHg) | Diastolic BP (mmHg) | ||
|---|---|---|---|---|---|---|
| Stage 1 | Stage 2 | Grade 1 | Grade 2/3 | |||
| 20–29 | 72/165 (43.6%) | 29/165 (17.6%) | 24 /165 (14.5%) | 5 /165 (3.0%) | 118 (20.0) | 81 (12.0) |
| 30–39 | 44/123 (35.8%) | 31/123 (25.2%) | 27/123 (22.0%) | 4 /123 (3.2%) | 117 (23.0) | 81 (13.0) |
| 40–49 | 64/164 (39.0%) | 46/164 (28.0%) | 35/164 (21.3%) | 11/164 (6.7%) | 122 (21.0) | 84 (15.0) |
| 50–59 | 46/130 (35.4%) | 47/130 (36.1%) | 35/130 (26.9%) | 12/130 (9.2%) | 125 (22.0) | 85 (15.0) |
| 60–69 | 83/205 (40.5%) | 71/205 (34.6%) | 62/205 (30.2%) | 9/205 (4.4%) | 131 (14.6) | 84 (15.0) |
| 70–80 | 35/106 (33.0%) | 50/106 (47.2%) | 45/106 (42.4%) | 5/106 (4.7%) | 135 (19.0) | 86 (11.0) |
Note: Prevalence of undiagnosed hypertension was significantly different among the age groups (P value <0.001 using Chi square test).
Table 4.
Association Between Several Factors of Interest and Undiagnosed Hypertension
| Factor | American College of Cardiology/American Heart Association | P value | European Society of Hypertension | P value | ||
|---|---|---|---|---|---|---|
| Hypertensive | Non-hypertensive | Hypertensive | Non-hypertensive | |||
| Gender (% of Males) | 320/619 (51.7%) | 109/277 (39.6%) | 0.001 | 159/274 (58.0%) | 270/622 (43.4%) | 0.000 |
| Obesity (% of BMI ≥ 30 kg/m2) | 149/619 (24.1%) | 41/277 (14.8%) | 0.002 | 80/274 (30.0%) | 110/622 (17.7%) | 0.000 |
| % Of Smokers | 181/619 (29.2%) | 76/277 (27.4%) | 0.581 | 86/274 (31.4%) | 171/622 (27.5%) | 0.235 |
| %Family History of CAD | 183/619 (29.6%) | 54/277 (19.5%) | 0.002 | 103/274 (37.6%) | 134/622 (21.5%) | 0.000 |
| %Family History of HTN | 365/619 (59.0%) | 153/277 (55.2%) | 0.323 | 180/274 (65.7%) | 338/622 (54.3%) | 0.002 |
Note: P value determined by Chi-squared test.
Figure 1.
Graph illustrating the trends of blood pressure readings among different age groups. X-axis represents the different age ranges among our study sample, while the Y-axis represents the median BP reading in each age range. Upper line (Blue) represents the systolic BP trend while the lower line (Red) represents the diastolic BP trend.
Upon analyzing predictors of systolic blood pressure, bivariate analyses identified age, gender, BMI, smoking status, and family history of CAD as being associated with systolic blood pressure at P < 0.2 and as candidate predictors for multivariate regression analysis. Table 5 depicts results from the multiple linear regression that was performed to predict systolic BP from the candidate predictors identified in the bivariate analyses. The total variance in systolic BP explained by the final parsimonious model, with all variables controlling for each other, was 19.7% (p < 0.001). Three predictor variables were identified that were independently significantly associated with higher systolic blood pressure readings: (1) older age (Beta = 0.20, P < 0.001), (2) higher BMI (Beta = 0.18, P < 0.001), (3) family history of CAD (Beta = 0.15, P < 0.001). On the other hand, female gender was identified to be independently significantly associated with lower systolic blood pressure readings (Beta = −0.25, P < 0.001).
Table 5.
Multiple Linear Regression Analysis to Predict Systolic Blood Pressure Readings Among Participants from the General Population, Not Previously Diagnosed to Have Hypertension, Diabetes, or Coronary Artery Disease
| Final Model* | b (Unstandardized Coefficients) | SE(b) | Beta (Standardized Coefficients) | P-value |
|---|---|---|---|---|
| Age | 0.19 | 0.03 | 0.20 | <0.001 |
| Female Gender (Compared to reference Male gender) | −8.06 | 0.97 | −0.25 | <0.001 |
| BMI | 0.55 | 0.09 | 0.18 | <0.001 |
| Family History of CAD | 5.587 | 1.143 | 0.15 | <0.001 |
Notes: Dependent variable was systolic blood pressure readings, age, continuous variable, Gender, dichotomous variable with male gender as the reference, BMI, continuous variable, Family history of CAD, dichotomous variable with no family history of CAD as the reference. *Backward-selection method was used; variables with P >0.10 removed from models. Model one (-) smoking status. Final Model includes age, gender, BMI, and Family history of CAD with an overall R Square of 0.197.
Upon analyzing predictors of diastolic blood pressure, bivariate analyses identified age, gender, BMI, smoking status, routine exercise, and family history of CAD as being associated with diastolic blood pressure levels at P < 0.2 and as candidate predictors for multivariate regression analysis. Table 6 depicts results from the multiple linear regression that was performed to predict diastolic BP from the candidate predictors identified in the bivariate analyses. The total variance in diastolic BP explained by the final parsimonious model, with all variables controlling for each other, was 7.8% (p < 0.001). Two predictor variables were independently significantly associated with higher diastolic blood pressure readings: (1) higher BMI (Beta = 0.19, P < 0.001), (2) family history of CAD (Beta = 0.09, P = 0.019). On the other hand, two other predictor variables were identified to be independently significantly associated with lower diastolic blood pressure readings: (1) female gender (Beta = −0.17, P < 0.001), (2) routine exercise (Beta = −0.08, P = 0.043).
Table 6.
Multiple Linear Regression Analysis to Predict Diastolic Blood Pressure Readings Among Participants from the General Population, Not Previously Diagnosed to Have Hypertension, Diabetes, or Coronary Artery Disease
| Final Model* | b (Unstandardized Coefficients) | SE(b) | Beta (Standardized Coefficients) | P-value |
|---|---|---|---|---|
| Female Gender (Compared to reference Male gender) | −3.25 | 0.76 | −0.17 | <0.001 |
| BMI | 0.30 | 0.06 | 0.19 | <0.001 |
| Exercise | −1.63 | 0.80 | −0.08 | 0.043 |
| Family History of CAD | 1.86 | 0.79 | 0.09 | 0.019 |
Notes: Dependent variable was diastolic blood pressure readings, Gender, dichotomous variable with male gender as the reference, BMI, continuous variable, Exercise, dichotomous variable with “no routine exercise activity“ as the reference, Family history of CAD, dichotomous variable with ”no family history of CAD” as the reference. *Backward-selection method was used; variables with P >0.10 removed from models. Model one (-) age. Model 2 (-) smoking status. Final Model includes gender, BMI, Exercise, and Family history of CAD with an overall R Square of 0.78.
Discussion
This study examined the prevalence of undiagnosed hypertension in the healthy Jordanian population and the factors associated with high systolic and diastolic blood pressure. According to the ACC/AHA guidelines, 68.5% of previously healthy Jordanians met the criteria to be diagnosed with hypertension. About systolic blood pressure, age, BMI, and family history of CAD were significant predictors of higher blood pressure, and female gender is associated with a significantly lower systolic blood pressure. For diastolic blood pressure, BMI and family history of CAD were associated with significantly higher DBP, and female gender and exercise were significantly associated with lower DBP. We also found that the median of systolic blood pressure readings was found to follow an increasing trend as age increases. Additionally, the prevalence of undiagnosed hypertension was the greatest among the oldest age group (70–80 years) corresponding to 80.2% with undiagnosed stage 1 or stage 2 hypertension according to the American College of Cardiology/American Heart Association guidelines, and 47.2% with undiagnosed grade 1 or grade 2 hypertension according to the European Society of Hypertension guidelines.
One of the more important findings in our study is the high prevalence of undiagnosed hypertension. Due to the recent, yet albeit controversial, changes in the guidelines for hypertension classification according to the ACC/AHA; slightly over two thirds of our population had either stage 1 or stage 2 hypertension. Khader et al reported that the prevalence of hypertension in the Jordanian population is 34% in adult males and 29% in adult females, with approximately 40% of them unaware of their hypertensive status.6 However, Khader et al used the British guidelines for diagnosing hypertension, taking hypertension as BP readings >140/90, equal to stage two hypertension in our study.13 When considering this definition, we report similar, yet slightly lower, unawareness of hypertension, with 30.5% of the healthy population falling under stage 2. This difference may be due to the characteristics of our study, since all patients in our sample were considered healthy volunteers without a prior diagnosis of hypertension, DM, or CAD. In their sample, all Jordanian adults, regardless of previous health status, were included, with slightly above 40% of their population having DM. The prevalence of hypertension in DM patients is 1.5–2 times greater than the healthy population,14 and patients who are diagnosed with DM, or have yet to be diagnosed with DM but met the criteria according to Khader et al, may have undiagnosed hypertension. It is well worth noting that awareness towards hypertensive status has greatly increased in the last ten years, largely due to the improved access of Jordanians to healthcare services.6
In the Arab world, awareness towards hypertensive status ranges between 14% and 82%, with some of the lowest rates of awareness found in Oman, Morocco, and a highly disadvantaged community in Jordan.9 While some have reported that the likelihood of having undiagnosed hypertension is higher in lower socioeconomic classes,15,16 it is interesting to note that even in high-income countries such as KSA and Oman, who have numerous health campaigns, had low rates of hypertension awareness.9 In Akl et al’s cascade of care review, their findings show that there is a loss of large proportions of hypertensive in each stage of the cascade of care (awareness of disease, treatment, and control), and that more missed opportunities result from unawareness of hypertension, indicating the presence of barriers to proper diagnosis of hypertension that need to be addressed.9
In our study, age, male gender, family history of CAD and obesity were significantly associated with higher prevalence of undiagnosed hypertension. In contrast to our study, Khader et al, reported that those older than 50 and those with family history of hypertension were more likely to be aware of their hypertension.6 About gender, we found that there is a significant association between male gender and unawareness of hypertension, which agrees with most studies in the Arab world.9 On the other hand, only two Arab studies, in Egypt17 and KSA,18 reported that males had significantly higher awareness of their hypertension status. Increasing BMI is a well-established risk factor for hypertension, and obesity in specific is thought to cause hypertension via the effect of leptin, which is found in higher concentrations in more obese individuals, on the sympathetic nervous system.19
A previous study revealed that the prevalence of hypertension among healthy university students of our institution (The University of Jordan) was surprisingly high at 35.2% for stage 1 and 13.5% for stage 2 according to the European Society of Hypertension guidelines but that study was based on a one time screening blood pressure measurement.20 In our study, factors significantly associated with increased SBP include age, BMI, and family history of CAD. This association with age is expected, as systolic blood pressure is reported to increase with age due to the increased stiffening of large arteries.21 In our study, an increase in age by one year predicts an independent average increase of 0.19 mmHg in systolic BP. Furthermore, in our study, every increase in BMI by 1 kg/m2 predicts an average independent increase of 0.55 mmHg in SBP. It has been previously reported that increased BMI leads to significantly higher SBP, and that this is a causal association.22 Khader et al also previously reported that increased waist circumference is a significant risk factor for hypertension in the Jordanian population.6
Having a routine exercise program predicts a lower average diastolic BP of −1.63 mmHg when compared to those without routine exercise programs after controlling other variables in our population. Decreasing resting blood pressure in hypertensive and normotensive patients is found to have profound effects on morbidity and mortality, with a decrease in five mmHg DBP being associated with a 34% reduction in stroke and a 21% reduction in coronary heart disease.23
In our study, gender was associated with both changes in SBP and DBP. For SBP, the female gender predicts an independently lower SBP of an average of 8.06 mmHg when compared to males after controlling other variables. In DBP, female gender predicts an independently lower diastolic BP of an average of −3.25 mmHg when compared to males after controlling other variables. The difference in blood pressure readings between males and females is likely due to the effect of sex hormones on renal sodium handling and vascular resistance.24
The status of hypertension in Jordan is a serious concern that must be addressed. While the rate of hypertension awareness and hypertensive control is increasing in Jordan,6 more work needs to be done to control modifiable risk factors in Jordan. One important modifiable risk factor is tobacco use, and more than 40% of Jordanians above the age of 15 smoke tobacco.25 This starts at a young age, with some Jordanians starting smoking cigarettes or water pipe as early as 11 or 12 years.26 Young adults that actively smoke cigarettes or water pipe, as well as those that drink alcohol, were significantly associated with higher BP readings than those who did not share the same lifestyle.27 These findings are alarming, and it is already being reported that there is a high prevalence of ischemic heart disease (IHD) in young Jordanian adults, and two significantly associated factors with IHD are smoking and hypertension.28
Participants who were found to have high blood pressure readings during any of the visits were advised to start lifestyle modifications and to follow with the primary care clinics.
The findings of this study are subject to some limitations. The cross-sectional design in which no follow up data of the subjects was obtained. Another limitation was the lack of out-of-office blood pressure measurements, which were not feasible among the majority of our sample due to issues of cost and inconvenience, in which we took the mean of two office readings one week apart. This may have led to include patients with white coat hypertension among our sample. We also recruited healthy visitors accompanying patients at our hospital, they can be related, and so participants could have a higher chance of having hypertension as a familial factor if patients were to have hypertension.
Conclusion
According to the ACC/AHA guidelines, 68.5% of previously healthy Jordanians met the criteria to be diagnosed with hypertension. Predictors of high systolic blood pressure were age, BMI and family history of CAD, while female gender is associated with a lower systolic blood pressure. For diastolic blood pressure, only BMI and family history of CAD were associated with significantly higher diastolic blood pressure, while female gender and exercise were significantly associated with lower diastolic blood pressure.
Funding Statement
The authors received no financial support for this study.
Data Sharing Statement
Data are available upon request.
Disclosure
All authors declare no conflict of interest.
References
- 1.Who.int. Indicator metadata registry details; 2022. Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3155. Accessed October 20, 2022.
- 2.Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020;75(2):285–292. doi: 10.1161/HYPERTENSIONAHA.119.14240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2015 Eastern Mediterranean Region Cardiovascular Disease Collaborators. Burden of cardiovascular diseases in the Eastern Mediterranean Region, 1990–2015: findings from the Global Burden of Disease 2015 study. Int J Public Health. 2018;63(S1):137–149. doi: 10.1007/s00038-017-1012-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Horan MJ, Lenfant C. Epidemiology of blood pressure and predictors of hypertension. Hypertension. 1990;15(2_supplement):I20. doi: 10.1161/01.HYP.15.2_Suppl.I20 [DOI] [PubMed] [Google Scholar]
- 5.Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: a systematic review: hypertension in Arab countries. Nurs Health Sci. 2014;16(1):126–130. doi: 10.1111/nhs.12060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khader Y, Batieha A, Jaddou H, et al. Hypertension in Jordan: prevalence, awareness, control, and its associated factors. Int J Hypertens. 2019;2019:1–8. doi: 10.1155/2019/3210617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jaddou HY, Batieha AM, Khader YS, Kanaan AH, El-Khateeb MS, Ajlouni KM. Hypertension prevalence, awareness, treatment and control, and associated factors: results from a national survey, Jordan. Int J Hypertens. 2011;2011:1–8. doi: 10.4061/2011/828797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park S, Gillespie C, Baumgardner J, et al. Modeled state-level estimates of hypertension prevalence and undiagnosed hypertension among US adults during 2013–2015. J Clin Hypertens. 2018;20(10):1395–1410. doi: 10.1111/jch.13388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akl C, Akik C, Ghattas H, Obermeyer CM. The cascade of care in managing hypertension in the Arab world: a systematic assessment of the evidence on awareness, treatment and control. BMC Public Health. 2020;20(1):835. doi: 10.1186/s12889-020-08678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang MD. Comparison of the ACC/AHA and ESC/ESH hypertension guidelines. Available from: https://www.acc.org/latest-in-cardiology/articles/2019/11/25/08/57/comparison-of-The-acc-aha-and-esc-esh-hypertension-guidelines. Accessed October 20, 2022.
- 11.Omboni S, Riva I, Giglio A, Caldara G, Groppelli A, Parati G. Validation of the Omron M5-I, R5-I and HEM-907 automated blood pressure monitors in elderly individuals according to the International Protocol of the European Society of Hypertension. Blood Press Monit. 2007;12:233–242. doi: 10.1097/MBP.0b013e32813fa386 [DOI] [PubMed] [Google Scholar]
- 12.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;71(19):e127–248. doi: 10.1016/j.jacc.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 13.Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ. 2004;328(7440):634–640. doi: 10.1136/bmj.328.7440.634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simonson DC. Etiology and prevalence of hypertension in diabetic patients. Diabetes Care. 1988;11(10):821–827. doi: 10.2337/diacare.11.10.821 [DOI] [PubMed] [Google Scholar]
- 15.Hasan MD, Tasnim F, Tariqujjaman M, Ahmed S, Cleary A, Mamun A. Examining the prevalence, correlates and inequalities of undiagnosed hypertension in Nepal: a population-based cross-sectional study. BMJ Open. 2020;10(10):e037592. doi: 10.1136/bmjopen-2020-037592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Banigbe BF, Itanyi IU, Ofili EO, Ogidi AG, Patel D, Ezeanolue EE. High prevalence of undiagnosed hypertension among men in North Central Nigeria: results from the healthy beginning initiative. PLoS One. 2020;15(11):e0242870. doi: 10.1371/journal.pone.0242870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohamed M, Shafek M, El Damaty S, Seoudi S. Hypertension control indicators among rural population in Egypt. J Egypt Public Health Assoc. 2000;75(5–6):391–401. [PubMed] [Google Scholar]
- 18.Kalantan K, Mohamed A, Al-Taweel A, Abdul Ghani H. Hypertension among attendants of primary health care centers in Al-Qassim region, Saudi Arabia. Saudi Med J. 2001;22(11):960–963. [PubMed] [Google Scholar]
- 19.Rahmouni K, Correia ML, Haynes WG, Mark AL. Obesity-associated hypertension: new insights into mechanisms. Hypertension. 2005;45(1):9–14. doi: 10.1161/01.HYP.0000151325.83008.b4 [DOI] [PubMed] [Google Scholar]
- 20.Alhawari HH, Al-Shelleh S, Alhawari HH, et al. Blood pressure and its association with gender, body mass index, smoking, and family history among university students. Int J Hypertens. 2018;2018:1–5. doi: 10.1155/2018/4186496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Izzo JL, Levy D, Black HR. Importance of systolic blood pressure in older Americans. Hypertension. 2000;35(5):1021–1024. doi: 10.1161/01.HYP.35.5.1021 [DOI] [PubMed] [Google Scholar]
- 22.Drøyvold WB, Midthjell K, Nilsen TIL, Holmen J. Change in body mass index and its impact on blood pressure: a prospective population study. Int J Obes. 2005;29(6):650–655. doi: 10.1038/sj.ijo.0802944 [DOI] [PubMed] [Google Scholar]
- 23.Kelley GA, Kelley KA, Vu Tran Z. Aerobic exercise and resting blood pressure: a meta-analytic review of randomized, controlled trials. Prev Cardiol. 2001;4(2):73–80. doi: 10.1111/j.1520-037X.2001.00529.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oparil S, Miller AP. Gender and blood pressure. J Clin Hypertens. 2005;7(5):300–309. doi: 10.1111/j.1524-6175.2005.04087.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Bank Group. Jordan: overview of tobacco use, tobacco control legislation, and taxation. WBG global tobacco control program; 2019. Washington, DC: World Bank. © World Bank. License: CC BY 3.0 IGO. Available from: https://openknowledge.worldbank.org/handle/10986/31954. Accessed October 20, 2022. [Google Scholar]
- 26.Al-Sheyab N, Alomari M, Shah S, Gallagher P, Gallagher R. Prevalence, patterns and correlates of cigarette smoking in male adolescents in Northern Jordan, and the influence of waterpipe use and asthma diagnosis: a descriptive cross-sectional study. IJERPH. 2014;11(9):9008–9023. doi: 10.3390/ijerph110909008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Safi SA, Aboul-Enein FH, Aboul-Enein BH, Manuel B. Influence of family history and lifestyle on blood pressure and heart rate in young adults in Jordan. Public Health. 2006;120(11):1027–1032. doi: 10.1016/j.puhe.2006.06.009 [DOI] [PubMed] [Google Scholar]
- 28.Raffee L, Alawneh K, Ibdah R. Prevalence, clinical characteristics, and risk among patients with ischemic heart disease in the young Jordanian population. OAEM. 2020;12:389–397. doi: 10.2147/OAEM.S272961 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request.