Abstract
Background
Pediatric tuberculous meningitis (TBM) commonly causes death or disability. In adults, high-dose rifampicin may reduce mortality. The role of fluoroquinolones remains unclear. There have been no antimicrobial treatment trials for pediatric TBM.
Methods
TBM-KIDS was a phase 2 open-label randomized trial among children with TBM in India and Malawi. Participants received isoniazid and pyrazinamide plus: (i) high-dose rifampicin (30 mg/kg) and ethambutol (R30HZE, arm 1); (ii) high-dose rifampicin and levofloxacin (R30HZL, arm 2); or (iii) standard-dose rifampicin and ethambutol (R15HZE, arm 3) for 8 weeks, followed by 10 months of standard treatment. Functional and neurocognitive outcomes were measured longitudinally using Modified Rankin Scale (MRS) and Mullen Scales of Early Learning (MSEL).
Results
Of 2487 children prescreened, 79 were screened and 37 enrolled. Median age was 72 months; 49%, 43%, and 8% had stage I, II, and III disease, respectively. Grade 3 or higher adverse events occurred in 58%, 55%, and 36% of children in arms 1, 2, and 3, with 1 death (arm 1) and 6 early treatment discontinuations (4 in arm 1, 1 each in arms 2 and 3). By week 8, all children recovered to MRS score of 0 or 1. Average MSEL scores were significantly better in arm 1 than arm 3 in fine motor, receptive language, and expressive language domains (P < .01).
Conclusions
In a pediatric TBM trial, functional outcomes were excellent overall. The trend toward higher frequency of adverse events but better neurocognitive outcomes in children receiving high-dose rifampicin requires confirmation in a larger trial.
Clinical Trials Registration
Keywords: pediatric tuberculous meningitis, neuropsychological, clinical trial, levofloxacin, high-dose rifampicin
In this first-ever antibiotic treatment trial for pediatric tuberculous meningitis, children receiving high-dose rifampicin (with or without levofloxacin) had similar functional outcomes and a trend toward better neurocognitive outcomes than those receiving a standard-dose rifampicin-containing regimen.
Tuberculous meningitis (TBM) is a devastating illness, with high risk of mortality or neurologic sequelae [1]. Young children are at high risk for disseminated tuberculosis (TB) [2], including TBM [3]. While neurologic injury may occur in patients of all ages—via direct bacterial effects, vasculitis from host response, or blockage of cerebrospinal circulation [4]—risk of developmental sequelae is unique to children, as the disease and its treatment occur during critical periods of neurocognitive development [5–8].
The current standard of care (SOC) for treatment of TBM according to the World Health Organization (WHO) is the same as for pulmonary TB: an intensive phase of 2 months of isoniazid, rifampicin, pyrazinamide, and ethambutol, followed by a continuation phase of isoniazid and rifampicin, with doses the same as for pulmonary TB [9, 10]. The only difference is that treatment for TBM is prolonged to 12 months, and in adults, the WHO suggests that streptomycin replace ethambutol. Recommendations do not account for differences in central nervous system (CNS) penetration. While isoniazid and pyrazinamide easily access the blood and cerebrospinal fluid (CSF) [11], rifampicin, ethambutol, and streptomycin do not [12, 13]. Recent trials in adults with TBM suggest that increasing the dose of rifampicin may reduce mortality [14]. Fluoroquinolones have excellent CNS penetration. Whether or not fluoroquinolones provide benefit in TBM remains unclear [15].
Based on emerging evidence from adult TBM trials suggesting that higher-dose rifampicin provided benefit and fluoroquinolones could potentially improve outcomes, we developed pharmacokinetic/pharmacodynamic (PK/PD) models to select doses of rifampicin and levofloxacin for children [16]. We designed the TuBerculous Meningitis in Kids (TBM-KIDS) trial to test regimens employing those doses. Additionally, since children have different outcomes than adults, they require different tools to measure them. We used the Modified Rankin Scale (MRS) to measure functional status. We adapted the Mullen Scales of Early Learning (MSEL) tool to assess neurocognitive status longitudinally [17–19]. Here we report results from TBM-KIDS, the first randomized clinical trial (RCT) of antimicrobials for children with TBM.
METHODS
Study Design and Participants
TBM-KIDS (NCT02958709) is a phase 2, open-label RCT among children with TBM. The trial was approved by local ethics committees at each site, the Johns Hopkins University institutional review board, and national regulatory bodies in each country. The trial was monitored by an independent data and safety monitoring committee. Participants’ parent(s) provided written informed consent, and children >7 years of age provided assent, when their neurologic status permitted.
Three sites participated in the study: BJ Government Medical College and Sassoon Hospital, Pune, India; Indian Council of Medical Research–National Institute for Research in Tuberculosis and Institute of Child Health and Hospital for Children (Chennai, India); and University of North Carolina Project Malawi and Kamuzu Central Hospital (Lilongwe, Malawi). Sites were selected based on affiliations with hospitals that could care for critically ill children and had demonstrated experience with pediatric TB trials. Inclusion criteria were age 6 months to 12 years; weight >6 kg; and probable or definite TBM by consensus research case definition (children with possible TBM committed to TBM treatment by their treating clinicians could also participate) [20]. Children were excluded for >10 days of TB treatment prior to enrollment; exposure to or personal history of rifampicin-resistant TB; death expected within 24 hours; grade >2 creatinine, alanine aminotransferase, or direct bilirubin; and human immunodeficiency virus with planned use of protease inhibitors or nevirapine.
Randomization
Trial randomization was computer-generated centrally, with 1:1:1 allocation. Randomization was stratified by study site and age group (<2 years, 2 to <5 years, 5–12 years).
Study Treatment and Procedures
Families of hospitalized children with symptoms of meningoencephalitis (eg, fever, confusion, neurologic abnormality) and/or plans to undergo lumbar puncture (LP) were approached. Clinical data were collected via medical record review and parental interview. At screening, head computed tomography or magnetic resonance imaging, CSF laboratory tests (cell count, glucose, protein; Gene Xpert; mycobacterial culture), and safety laboratory tests (complete blood count, comprehensive metabolic panel) were performed. Possible, probable, definite, or no TBM status was assigned based on Consensus Research Definition (Supplementary Table 1) [20]. Children underwent staging of disease severity by Medical Research Council scale [21], assessment of neurologic function by MRS [22], and neurocognitive assessment by MSEL at entry [17, 23].
Participants were randomized to treatment arm and received study treatment for 8 weeks via directly observed therapy. All patients received isoniazid (H) and pyrazinamide (Z) at standard doses. In arm 1, participants additionally received high-dose rifampicin and ethambutol (HR30ZE); in arm 2, participants received high-dose rifampicin and levofloxacin (HR30ZL); in arm 3, participants received SOC per WHO guidelines (HR15ZE) (Supplementary Table 2). Children were then transitioned to study-provided isoniazid and rifampicin at standard doses to complete 12 months of therapy.
Children underwent regular clinical assessments and safety evaluations (Supplementary Table 3). MRS was repeated at weeks 8, 24, and 52. MSEL was done at weeks 8 and study completion (week 52 or 72). On-treatment LPs were performed at weeks 1 and 6 (±2), to coincide with intensive plasma PK sampling. Protocol-defined criteria for early treatment discontinuation included treatment with disallowed medications, drug toxicity that met permanent drug discontinuation criteria, sustained nonadherence, or diagnosis of drug-resistant TB. Early in the study, participants were followed for 72 weeks; later, follow-up ended at 52 weeks in the context of study completion timelines.
Outcomes
The primary clinical outcome measure was MRS (scale of 0 [no symptoms] to 6 [death], (Supplementary Table 4) [22]. We employed the Gross Motor Function Classification System—Expanded and Revised to more objectively assign an MRS value [24]. The primary safety outcome was grade 3 or higher adverse events (Division of AIDS Grading Table, version 2.1, March 2017). MSEL score, a secondary endpoint, was adapted for local use, as previously described [17], and available in Hindi, Marathi, Tamil, or Chichewa. Overall score and subscale scores were recorded. TB treatment outcome was recorded.
Statistical Considerations
Statistical analyses were performed using Stata version 17.0 (StataCorp, College Station, Texas). For safety, adverse events were summarized using frequencies and percentages and compared using a Fisher exact test at 5% level of significance. For MRS, using study site and children as random effects, change in MRS over time across treatment arms was estimated using a multilevel ordered logistic regression model adjusted for age, sex, and baseline MRS. For MSEL, T-scores were calculated for each domain and summarized using median and interquartile range (IQR). Adjusted differences in T-scores by treatment arm were estimated using a multilevel mixed-effects model with random effects for study site and baseline MRS score. The sample size target was 100 children to achieve >80% power to detect a 30% difference in treatment efficacy using a longitudinally measured graded outcome of functional status, measured by MRS. Based on previous studies in pediatric TBM, we posited a distribution of outcomes in the SOC arm of 35% death or severe impairment, 30% moderate disability, 15% mild disability, and 20% full recovery.
RESULTS
Demographics
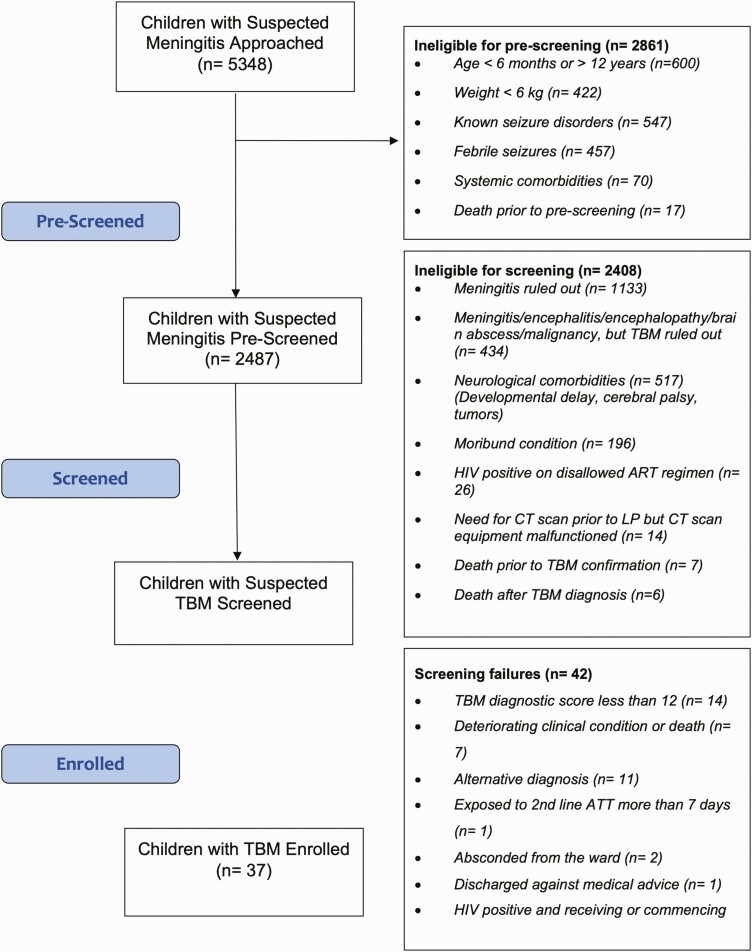
Between March 2017 and November 2019, 2487 children were prescreened, 79 were screened, and 37 were enrolled. The target sample size could not be reached owing to slower-than-expected enrollment. Reasons for low enrollment have been described in detail previously [25] (Figure 1). Children presenting with neurologic complaints, fever, or other indication for LP were numerous, with a broad range of diagnoses and reasons for prescreening failure (Figure 1) [26]. The most common cause for screening failure was TBM diagnostic score <12. Median age was 72 (IQR, 22–98) months, and 49%, 43%, and 8% had stage I, II, and III disease, respectively (Table 1). The majority (57%) had definite TBM. Common symptoms included reduced playfulness (84%), lethargy (68%), fever (57%), irritability (49%), neck stiffness (46%), and altered consciousness (38%) (Supplementary Table 6).
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) diagram. Abbreviations: ART, antiretroviral therapy; ATT, antitubercular treatment; CT, computed tomography; HIV, human immunodeficiency virus; LP, lumbar puncture; TB, tuberculosis.
Table 1.
Demographic and Clinical Information About Enrolled Participants, by Arm
| Baseline Characteristic | Overall (N = 37) |
Arm 1: R30HZE (n = 12 |
Arm 2: R30HZL (n = 11 |
Arm 3: R15HZE (n = 14) |
|---|---|---|---|---|
| Age, y, median (IQR) | 72 (22–98) | 56 (16–100) | 57 (29–125) | 72 (22–91) |
| Female sex | 14 (38) | 4 (33) | 5 (45) | 5 (36) |
| Weight, kg, median (IQR) | 11 (6.9–21.0) | 18.1 (10.4–22.0) | 11.0 (1.0–21.0) | 8.7 (6.9–20.0) |
| Head CT | ||||
| Normal | 7 (19) | 3 (25) | 1 (9) | 3 (21) |
| Abnormal | 26 (70) | 7 (58) | 10 (91) | 9 (64) |
| Not done | 4 (11) | 2 (17) | 0 | 2 (14) |
| CSF laboratory tests, median (IQR) | ||||
| WBC count, cells/µL | 59 (7–140) | 99 (6–360) | 35 (0–68) | 70 (20–140) |
| Lymphocytes, % | 85 (25–98) | 90 (65–97) | 57 (40–90) | 75 (25–98) |
| Glucose, mg/dL | 45 (25–68) | 45 (19–68) | 38 (25–70) | 49 (25–68) |
| Total protein, g/dL | 109 (48–211) | 131 (62–311) | 90 (50–152) | 105 (38–141) |
| TBM classificationa | ||||
| Definite | 21 (57) | 9 (75) | 5 (46) | 7 (50) |
| Probable | 10 (27) | 3 (25) | 3 (27) | 4 (29) |
| Possible | 6 (16) | 0 | 3 (27) | 3 (21) |
| Baseline Modified Rankin Scale score, median (range) | 3 (1–4) | 4 (1–5) | 1 (1–4) | 2 (1–5) |
| Stage | ||||
| I | 18 (49) | 3 (25) | 8 (73) | 7 (50) |
| IIA | 10 (27) | 5 (42) | 2 (18) | 3 (21) |
| IIB | 6 (16) | 2 (17) | 1 (9) | 3 (21) |
| III | 3 (8) | 2 (17) | 0 | 1 (7) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: CSF, cerebrospinal fluid; IQR, interquartile range; R15HZE, standard-dose rifampicin (15 mg/kg/day), isoniazid, pyrazinamide, ethambutol; ; R30HZE, high-dose rifampicin (30 mg/kg/day), isoniazid, pyrazinamide, ethambutol; R30HZL, high-dose rifampicin (30 mg/kg/day), isoniazid, pyrazinamide, levofloxacin; TBM, tuberculous meningitis; WBC, white blood count.
As per the consensus TBM research definitions by Marais et al [20].
Efficacy Outcomes
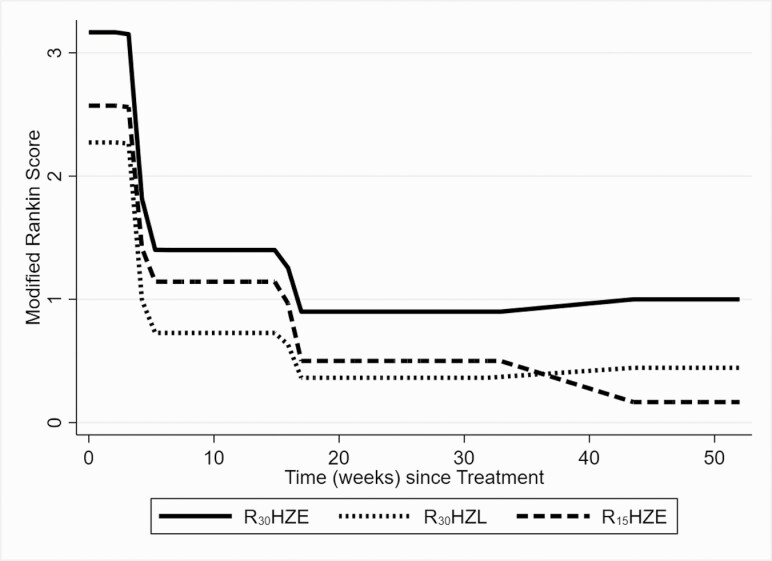
At entry, median (range) MRS scores were 4 (1–5), 1 (1–4), and 2 (1–5) in arms 1–3, respectively. Rapid improvement was seen by week 8 in all arms with almost all children recovering to a score of 0 or 1 (little to no disability) by week 24 (Figure 2). Compared to SOC, after adjusting for age, sex, and baseline MRS, the adjusted ratio of the odds of having a higher rather than lower MRS over the study period was 3.31 (95% confidence interval [CI], .17–63.8; P = .43, arm 1 vs arm 3) and 1.52 (95% CI, .06–36.9; P = .80, arm 2 vs arm 3). Because functional outcomes were excellent across the board, planned primary PK/PD analyses linking PK to MRS could not be performed. In neurocognitive assessments, compared to SOC, children receiving high-dose rifampicin (arm 1) had statistically significantly better longitudinal fine motor, receptive language, and expressive language scores, after adjusting for age and baseline MRS (Table 2). There was a trend toward better neurocognitive outcomes in arm 2 compared to arm 3, but these were modest and only statistically significant for gross motor function. One child with probable TBM (CSF Gene Xpert and culture negative; grandfather with drug-sensitive TB) in arm 1 who initially responded well to treatment developed a spinal abscess at month 8 with Mycobacterium tuberculosis discovered to be resistant to rifampicin and isoniazid [27]. There were no other treatment failures or relapses.
Figure 2.
Modified Rankin Score, over time, with treatment, by arm. Abbreviations: R15HZE, standard-dose rifampicin (15 mg/kg/day), isoniazid, pyrazinamide, ethambutol; R30HZE, high-dose rifampicin (30 mg/kg/day), isoniazid, pyrazinamide, ethambutol; R30HZL, high-dose rifampicin (30 mg/kg/day), isoniazid, pyrazinamide, levofloxacin.
Table 2.
Neurocognitive Outcomes, Comparing the 3 Arms, Assessed Longitudinally Over the Course of Study Participation
| Outcome Variable | Study Arm | Univariable Analysis | Multivariable Analysisa | ||
|---|---|---|---|---|---|
| Estimated Difference (95% CI) | P Value | Estimated Difference (95% CI) | P-Value | ||
| Visual reception | R15HZE | Ref | Ref | ||
| R30HZE | 1.96 (–5.65 to 9.57) | .61 | 3.56 (–2.72 to 9.83) | .27 | |
| R30HZL | 0.45 (–7.13 to 8.03) | .91 | –2.83 (–9.77 to 4.10) | .42 | |
| Fine motor | R15HZE | Ref | Ref | ||
| R30HZE | 10.7 (3.19–18.28) | .005 | 12.0 (5.46–18.5) | <.01 | |
| R30HZL | 5.20 (–2.39 to 12.8) | .18 | 2.40 (–4.82 to 9.62) | .52 | |
| Receptive language | R15HZE | Ref | Ref | ||
| R30HZE | 11.78 (3.61–20.0) | .005 | 12.2 (5.87–18.5) | <.01 | |
| R30HZL | 4.80 (–3.36 to 13.0) | .25 | 1.30 (–5.68 to 8.28) | .72 | |
| Expressive language | R15HZE | Ref | .03 | Ref | |
| R30HZE | 13.2 (1.4–24.9) | .22 | 14.9 (4.45–25.28) | .01 | |
| R30HZL | 7.2 (–4.4 to 18.8) | 2.64 (–8.45 to 13.7) | .64 | ||
| Gross motor | R15HZE | Ref | .24 | Ref | |
| R30HZE | 5.02 (–3.37 to 13.41) | 4.15 (–1.20 to 9.50) | .13 | ||
| R30HZL | 16.02 (7.37–25.54) | <.001 | 7.20 (–.31 to 14.71) | .06 | |
Abbreviations: CI, confidence interval; R15HZE, standard-dose rifampicin (15 mg/kg/day), isoniazid, pyrazinamide, ethambutol; R30HZE, high-dose rifampicin (30 mg/kg/day), isoniazid, pyrazinamide, ethambutol; R30HZL, high-dose rifampicin (30 mg/kg/day), isoniazid, pyrazinamide, levofloxacin.
Adjusted for age, sex, and baseline Modified Rankin Scale.
Safety and Tolerability Results
Grade 3 or higher adverse events were common, occurring in 49% of participants: 7 of 12 (58%) in arm 1, 6 of 11 (55%) in arm 2, and 5 of 14 (36%) in arm 3 (P = .50) (Supplementary Table 7). There were 6 early treatment discontinuations, 4 in arm 1 (3 for toxicity), 1 in arm 2 (for toxicity), and 1 in arm 3 (disallowed medicine). Of the 4 early treatment discontinuations for toxicity, only 2 occurred during experimental therapy, while the other 2 occurred during standard continuation phase treatment. There was 1 death, in arm 1, in the setting of critical illness characterized by worsening mental status, end organ damage (including liver injury), and worsening CSF parameters. All other children completed the study.
DISCUSSION
We report here outcomes from the first RCT of antimicrobials for the treatment of pediatric TBM. Unexpectedly, almost all children who participated in the trial did well from a functional standpoint, with most children having no detectable physical disabilities by the end of 8 weeks of study treatment or upon longer-term follow-up, many having started their treatment with earlier-stage disease. Given the excellent functional outcomes across study arms and limited sample size, we were unable to detect differences in functional outcome by treatment assignment, perhaps in part because the MRS scale is unlikely to detect more subtle effects on functional status. While adverse events were common, as would be expected in a cohort of ill, hospitalized children receiving multidrug therapy for TBM, most did not result in early treatment discontinuation, and those that did were equally likely to occur during the intensive phase of TBM (when experimental treatment was offered) as during the continuation phase (when SOC was provided to all children). Importantly, children receiving higher-dose rifampicin had statistically better neurocognitive outcomes in fine motor, receptive language, and expressive language domains than children receiving SOC dosing, a finding that requires confirmation in a larger trial. These data are consistent with cohort studies reporting favorable outcomes among children given regimens that are high-dose rifampicin based.
Despite having better functional outcomes than expected in TBM-KIDS and not meeting the target sample size, we were able to detect a treatment effect on neurocognitive outcomes. Given the small sample size, this finding will need to be replicated in larger trials to ensure it is a true finding. In addition to neurologic sequelae, children with brain injury due to TBM or other causes often suffer “invisible disabilities” related to effects of the disease or its treatment on the developing brain. In the case of CNS TB, there is an additional feature—M. tuberculosis replicates in microglia, cells that both participate in the immune response to the pathogen and also play a critical role in neurodevelopment [5]. Higher-dose rifampicin, delivered early in treatment, appeared to improve the neurocognitive outcomes in children with TBM, in fine motor, receptive language, and expressive language domains. Our study highlights the importance of studying treatments in special populations rather than extrapolating from adult trials when outcomes are expected to be different. Our trial and observational studies point to the need for neurocognitive testing among children with TBM and provision of comprehensive rehabilitation focused not just on physical therapy but also on speech and language therapy plus other tailored services [8, 28]. Testers described children as being inattentive and behaviorally dysregulated. Parents may benefit from training in management of challenging behaviors, and educational supports may be needed.
It is common for outcomes in TB treatment trials to be better than in general practice, including in SOC control arms [29–31]. This is related, in part, to trial conditions—patients in trials are monitored closely via frequent visits and provided enhanced adherence support. Equally importantly, but less frequently chronicled, individuals who are qualified for and choose to enroll in a trial are often different from those who do not or cannot. The same appears to be true for pediatric TBM. Meta-analyses and scoping reviews conclude that among children with TBM, about 20% die, while more than half who survive have significant disabilities [32, 33]. In TBM-KIDS, outcomes were excellent, with rates of mortality and functional disability very low, across treatment arms. To participate in a TBM trial, a child must survive long enough to undergo diagnostic testing and treatment initiation, have parents who live in the trial site catchment area and agree for their critically ill child to participate, speak a language provided on a consent form, and meet laboratory inclusion criteria [26]. Children cannot have been on treatment for more than a few days before joining a therapeutic trial, so children doing poorly on treatment initiated at outside centers cannot join. Additionally, children may be identified to have TBM earlier at a trial site and therefore treated earlier. Thus, even in areas where TB rates are high, enrollment into a pediatric TBM trial is challenging, and participants do not mirror the general population of children with TBM.
In adults with TBM, high-dose rifampicin appears to reduce mortality [14], though this finding is not universal [34], and benefit is likely to be dose-dependent. There are several phase 3 trials of 35 mg/kg underway in adults, which will provide a definitive answer to this question [35]. From a clinical pharmacology standpoint, it is logical to choose drugs and doses that achieve therapeutic concentrations at the site of disease, and rifampicin displays poor penetration into the brain and CSF [12, 36, 37]. A cohort study in Vietnam that recruited children with later-stage disease demonstrated that rifampicin concentrations were higher in those children who recovered well than in those with neurologic sequelae [36]. Together, these results, those from cohort studies in South Africa in which high-dose rifampicin is used routinely, and results from our trial suggest that children with TBM should receive higher doses of rifampicin. We were unable to detect a benefit of using a fluoroquinolone rather than ethambutol, perhaps because of small sample size, but this lack of benefit is consistent with adult trials [34, 38]. It is unclear whether or not use of fluoroquinolones negated, in part, the benefit from high-dose rifampicin [39], as the high-dose rifampicin treatment effect was reduced and not statistically significant in the arm that included a fluoroquinolone. Whether or not higher doses of isoniazid or use of drugs with better CNS penetration like ethionamide, linezolid, or delamanid will improve outcomes in adults or children with TBM remains to be proven. WHO guidelines were recently updated to include a 6-month regimen of higher-dose rifampicin (22–30 mg/kg) and isoniazid plus pyrazinamide and ethionamide, otherwise known as the “Cape Town regimen,” as an alternative for children with TBM [40].
Our trial has several limitations. First, we did not achieve the target sample size [26, 41]. With coronavirus disease 2019 and given the slow enrollment pace, enrollment was closed in March of 2020 at the request of the funder so children could complete study visits prior to the funding end date of 2021. Prior to our trial, only about 500 children had ever been enrolled in RCTs for pediatric TBM, including assessments of anti-inflammatory medications and surgical interventions. To evaluate regimens for TBM more fully and efficiently, informative translational work plus a large network of sites will be needed, given that TBM in children is rare and there is significant variability in disease presentation and response to therapy. Second, we could not compare safety across arms conclusively given the small sample size. The safety profile of high-dose rifampicin in adults and children with pulmonary TB and TBM in other studies appears to be generally favorable [42, 43]. Fluoroquinolones may be less safe in TBM, with 1 meta-analysis suggesting higher risk of vision loss or seizures [15]. More data in children with TBM are needed. Third, the dose of rifampicin that we tested may have been too low. While it was based on pre-trial modeling work [16], even higher doses may be more efficacious [14]. Fourth, assessing neurocognitive outcomes across a broad range of ages (0–12 years) and different culture settings using a single, consistently applied tool is challenging [8, 17, 26, 41]. While MSEL was culturally adapted to trial settings, with systematic and longitudinal training of all testers in TBM-KIDS, other tools are needed to facilitate studies such as ours. Last, this study was open-label, which may have introduced bias. However, a placebo-controlled blinded trial was not feasible, as pill burdens were high and there were a large number of weight bands, to allow precision dosing across children of all different ages. Neurocognitive testers were masked to treatment arm.
CONCLUSIONS
In this first-ever trial of antimicrobials specifically for pediatric TBM, functional outcomes were favorable, across arms. Neurocognitive outcomes were statistically better in children who received high-dose rifampicin compared to those who did not, but this finding requires replication in larger trials. There was no discernable benefit of levofloxacin, though small sample size precluded a thorough assessment of the potential risks and benefits of levofloxacin substitution for ethambutol.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Financial support. This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) at the National Institutes of Health (NIH) (award number R01HD074944). Additional support was provided by the National Institute of Allergy and Infectious Diseases (NIAID) at the NIH (award number K24AI150349 to K. E. D.). ColorDx color vision testing kits were donated by Konan Medical.
Acknowledgments. The authors acknowledge the following study team members for their contributions (in alphabetical order): BJ Government Medical College (BJGMC)–Johns Hopkins University Clinical Research Site, Pune: Shivali Agiwal, Rupali Ahire, Usha Balasubramanian, Manjushree Bendre, Jyoti Chandane, Kavita Chopade, Shamala Dalimbkar, Prasad Deshpande, Rajendra Dhage, Mahesh Ithape, Varsha Jadhav, Sonali Kante, Pallavi Kapre, Nawshaba Khan, Vandana Kulkarni, Renu Madewar, Shashibhushan Meshram, Kunal Muttha, Vaishali Nadgeri, Arti Nagargoje, Amita Nagraj, Aparna Nijampurkar, Prerana Onawale, Namrata Pawar, Prashant Pawar, Neeta Pradhan, Varsha Shaikh, Zaheda Shaikh, Dhananjay Shere, Gouri Wani. BJGMC and Sassoon General Hospital: Rajesh Kulkarni, Uday Rajput. Indian Council of Medical Research–National Institute for Research in Tuberculosis, Chennai (ICMR-NIRT): Mangalambal Ganesan, Gunasundari Arasan, Shakila Shankar, S. Stella Mary, Sureshwari Karuppaiah, Leema Pauline, Arunagiri, Snegha Karunakaran Pramila, Priyadharshini Arul, Prabhavathy, Sankar Ganesh, Luke Elizabeth Hanna, K. Ramesh, M. Kannan, Ruthra Vijayakumar, Surekha, S. Sivakumar, K. Devika, Sathya, A. Radhakrishnan, A. R. Preethi, S. Rajkumar, Kwasakar, N. Saravanan, Geetha Ramachandran, A. K. Hemanth Kumar, Jayakumar, M. Dharman, V. Sudha, Syed Hissar, Valarmathi Nagarajan, Linda Jennifer, R. Supriya, R. Manimegalai, Santhanam Kandan, Archana Maniselvi, Oli Puspha, S. Vaishnavi, R. Selvi, Logeswari Neelakandan. University of North Carolina Project Malawi, Lilongwe: Mary Chiunda, Moreen Chunga, Madalo Kamanga, Portia Kamthunzi, Elizabeth Kanthiti, Abineli Mbewe, Emmie Msiska, Noel Mumba, Ian Zifa Phiri, Victor Palichina, Dorothy Sichali. Johns Hopkins University: Vivian Rexroad. Additionally, we are thankful for the guidance of our data and safety monitoring board, comprised of Drs Anneke Hesseling, Y. K. Gupta, and Patrick Phillips.
Contributor Information
Mandar S Paradkar, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Johns Hopkins India, Pune, India.
Bella Devaleenal D, Department of Clinical Research, Indian Council of Medical Research–National Institute for Research in Tuberculosis, Chennai, India.
Tisungane Mvalo, UNC Project Malawi, Lilongwe, Malawi; Department of Pediatrics, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, USA.
Ana Arenivas, Section of Neuropsychology, Neurological Institute, Cleveland Clinic Foundation, Cleveland, Ohio, USA.
Kiran T Thakur, Department of Neurology, Columbia University Irving Medical Center/New York Presbyterian Hospital, New York, New York, USA.
Lisa Wolf, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA.
Smita Nimkar, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Johns Hopkins India, Pune, India.
Sadaf Inamdar, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Johns Hopkins India, Pune, India.
Prathiksha Giridharan, Department of Clinical Research, Indian Council of Medical Research–National Institute for Research in Tuberculosis, Chennai, India.
Elilarasi Selladurai, Institute of Child Health and Hospital for Children, Chennai, India.
Aarti Kinikar, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Department of Pediatrics, BJ Government Medical College, Pune, India.
Chhaya Valvi, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Department of Pediatrics, BJ Government Medical College, Pune, India.
Saltanat Khwaja, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Johns Hopkins India, Pune, India.
Daphne Gadama, UNC Project Malawi, Lilongwe, Malawi.
Sarath Balaji, Department of Clinical Research, Indian Council of Medical Research–National Institute for Research in Tuberculosis, Chennai, India.
Krishna Yadav Kattagoni, Department of Clinical Research, Indian Council of Medical Research–National Institute for Research in Tuberculosis, Chennai, India.
Mythily Venkatesan, Department of Clinical Research, Indian Council of Medical Research–National Institute for Research in Tuberculosis, Chennai, India.
Radojka Savic, Department of Bioengineering and Therapeutic Sciences, University of California, San Francisco, San Francisco, California, USA.
Soumya Swaminathan, World Health Organization, Geneva, Switzerland.
Amita Gupta, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA.
Nikhil Gupte, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Johns Hopkins India, Pune, India; Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA.
Vidya Mave, BJ Government Medical College–Johns Hopkins Clinical Research Site, Pune, India; Johns Hopkins India, Pune, India; Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA.
Kelly E Dooley, Department of Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA.
TuBerculous Meningitis in Kids (TBM-KIDS) Study Team:
Shivali Agiwal, Rupali Ahire, Usha Balasubramanian, Manjushree Bendre, Jyoti Chandane, Kavita Chopade, Shamala Dalimbkar, Prasad Deshpande, Rajendra Dhage, Mahesh Ithape, Varsha Jadhav, Sonali Kante, Pallavi Kapre, Nawshaba Khan, Vandana Kulkarni, Renu Madewar, Shashibhushan Meshram, Kunal Muttha, Vaishali Nadgeri, Arti Nagargoje, Amita Nagraj, Aparna Nijampurkar, Prerana Onawale, Namrata Pawar, Prashant Pawar, Neeta Pradhan, Varsha Shaikh, Zaheda Shaikh, Dhananjay Shere, Gouri Wani, Rajesh Kulkarni, Uday Rajput, Mangalambal Ganesan, Gunasundari Arasan, Shakila Shankar, S Stella Mary, Sureshwari Karuppaiah, Leema Pauline, Snegha Karunakaran Pramila, Priyadharshini Arul, Sankar Ganesh, Luke Elizabeth Hanna, K Ramesh, M Kannan, Ruthra Vijayakumar, Surekha S Sivakumar, K Devika, A Radhakrishnan, A R Preethi, S Rajkumar, N Saravanan, Geetha Ramachandran, A K Hemanth Kumar, M Dharman, V Sudha, Syed Hissar, Valarmathi Nagarajan, Linda Jennifer, R Supriya, R Manimegalai, Santhanam Kandan, Archana Maniselvi, Oli Puspha, S Vaishnavi, R Selvi, Logeswari Neelakandan, Mary Chiunda, Moreen Chunga, Madalo Kamanga, Portia Kamthunzi, Elizabeth Kanthiti, Abineli Mbewe, Emmie Msiska, Noel Mumba, Ian Zifa Phiri, Victor Palichina, Dorothy Sichali, Vivian Rexroad, Anneke Hesseling, Y K Gupta, and Patrick Phillips
References
- 1. Wilkinson RJ, Rohlwink U, Misra UK, et al. . Tuberculous meningitis. Nat Rev Neurol 2017; 13:581–98. [DOI] [PubMed] [Google Scholar]
- 2. Marais BJ, Schaaf HS.. Tuberculosis in children. Cold Spring Harb Perspect Med 2014; 4:a017855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wolzak NK, Cooke ML, Orth H, van Toorn R.. The changing profile of pediatric meningitis at a referral centre in Cape Town, South Africa. J Trop Pediatr 2012; 58:491–5. [DOI] [PubMed] [Google Scholar]
- 4. Rock RB, Olin M, Baker CA, et al. . Central nervous system tuberculosis: pathogenesis and clinical aspects. Clin Microbiol Rev 2008; 21:243–61, table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tucker EW, Pokkali S, Zhang Z, et al. . Microglia activation in a pediatric rabbit model of tuberculous meningitis. Dis Models Mech 2016; 9:1497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rohlwink UK, Donald K, Gavine B, et al. . Clinical characteristics and neurodevelopmental outcomes of children with tuberculous meningitis and hydrocephalus. Dev Med Child Neurol 2016; 58:461–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schoeman J, Wait J, Burger M, et al. . Long-term follow up of childhood tuberculous meningitis. Dev Med Child Neurol 2002; 44:522–6. [DOI] [PubMed] [Google Scholar]
- 8. Davis AG, Nightingale S, Springer PE, et al. . Neurocognitive and functional impairment in adult and paediatric tuberculous meningitis. Wellcome Open Res 2019; 4:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. Treatment of tuberculosis guidelines. 4th ed. WHO/HTM/TB/2009.420. Geneva, Switzerland: WHO, 2010. [PubMed] [Google Scholar]
- 10. World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. 2nd ed. WHO/HTM/TB/2014.03. Geneva, Switzerland: WHO, 2014. [PubMed] [Google Scholar]
- 11. Donald PR. The chemotherapy of tuberculous meningitis in children and adults. Tuberculosis 2010; 90:375–92. [DOI] [PubMed] [Google Scholar]
- 12. Tucker EW, Guglieri-Lopez B, Ordonez AA, et al. . Noninvasive (11)C-rifampin positron emission tomography reveals drug biodistribution in tuberculous meningitis. Sci Transl Med 2018; 10:eaau0965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ellard GA, Humphries MJ, Allen BW.. Cerebrospinal fluid drug concentrations and the treatment of tuberculous meningitis. Am Rev Respir Dis 1993; 148:650–5. [DOI] [PubMed] [Google Scholar]
- 14. Svensson EM, Dian S, Te Brake L, et al. . Model-based meta-analysis of rifampicin exposure and mortality in Indonesian tuberculosis meningitis trials. Clin Infect Dis 2020; 71:1817–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rizvi I, Malhotra HS, Garg RK, Kumar N, Uniyal R, Pandey S.. Fluoroquinolones in the management of tuberculous meningitis: systematic review and meta-analysis. J Infect 2018; 77:261–75. [DOI] [PubMed] [Google Scholar]
- 16. Savic RM, Ruslami R, Hibma JE, et al. . Pediatric tuberculous meningitis: Model-based approach to determining optimal doses of the anti-tuberculosis drugs rifampin and levofloxacin for children. Clin Pharmacol Ther 2015; 98:622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nimkar S, Joshi S, Kinikar A, et al. . Mullen scales of early learning adaptation for assessment of Indian children and application to tuberculous meningitis. J Trop Pediatr 2021; 67:fmaa034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mailankody S, Dangeti GV, Soundravally R, et al. . Cerebrospinal fluid matrix metalloproteinase 9 levels, blood-brain barrier permeability, and treatment outcome in tuberculous meningitis. PLoS One 2017; 12:e0181262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J.. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988; 19:604–7. [DOI] [PubMed] [Google Scholar]
- 20. Marais S, Thwaites G, Schoeman JF, et al. . Tuberculous meningitis: a uniform case definition for use in clinical research. Lancet Infect Dis 2010; 10:803–12. [DOI] [PubMed] [Google Scholar]
- 21. van Toorn R, Springer P, Laubscher JA, Schoeman JF.. Value of different staging systems for predicting neurological outcome in childhood tuberculous meningitis. Int J Tuberc Lung Dis 2012; 16:628–32. [DOI] [PubMed] [Google Scholar]
- 22. Banks JL, Marotta CA.. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke 2007; 38:1091–6. [DOI] [PubMed] [Google Scholar]
- 23. Mullen EM. Mullen Scales of Early Learning. AGS ed. Circle Pines, MN: American Guidance Service, 1995. [Google Scholar]
- 24. Palisano RRP, Bartlett D, Livingston M.. Gross Motor Function Classification System—Expanded and Revised. 2007. Available at: https://www.canchild.ca/system/tenon/assets/attachments/000/000/058/original/GMFCS-ER_English.pdf. Accessed 20 December 2021.
- 25. Paradkar M, Devaleenal DB, Valvi C, ed. High-dose rifampicin with or without levofloxacin for the treatment of pediatric TBM: results from the TBM-KIDS Trial. In: International Union Against Tuberculosis and Lung Disease World Conference, 2021.
- 26. Paradkar M, Devaleenal DB, Mvalo T, et al. . Challenges in conducting trials for pediatric tuberculous meningitis: lessons from the field. Int J Tuberc Lung Dis 2019; 23:1082–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Giridharan P, Selladurai E, Balaji S, et al. . Drug resistant TB spine in a two year old child: a case report. Indian J Tuberc 2020; 67:374–7. [DOI] [PubMed] [Google Scholar]
- 28. Schoeman CJ, Herbst I, Nienkemper DC.. The effect of tuberculous meningitis on the cognitive and motor development of children. S Afr Med J 1997; 87:70–2. [PubMed] [Google Scholar]
- 29. Nunn AJ, Phillips PPJ, Meredith SK, et al. . A trial of a shorter regimen for rifampin-resistant tuberculosis. N Engl J Med 2019; 380:1201–13. [DOI] [PubMed] [Google Scholar]
- 30. Conradie F, Diacon AH, Ngubane N, et al. . Treatment of highly drug-resistant pulmonary tuberculosis. N Engl J Med 2020; 382:893–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nunn AJ, Phillips PP, Gillespie SH.. Design issues in pivotal drug trials for drug sensitive tuberculosis (TB). Tuberculosis 2008; 88:S85–92. [DOI] [PubMed] [Google Scholar]
- 32. Chiang SS, Khan FA, Milstein MB, et al. . Treatment outcomes of childhood tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect Dis 2014; 14:947–57. [DOI] [PubMed] [Google Scholar]
- 33. Daniel BD, Grace GA, Natrajan M.. Tuberculous meningitis in children: clinical management and outcome. Indian J Med Res 2019; 150:117–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Heemskerk AD, Bang ND, Mai NT, et al. . Intensified antituberculosis therapy in adults with tuberculous meningitis. N Engl J Med 2016; 374:124–34. [DOI] [PubMed] [Google Scholar]
- 35. Marais S, Cresswell FV, Hamers RL, et al. . High dose oral rifampicin to improve survival from adult tuberculous meningitis: a randomised placebo-controlled double-blinded phase III trial (the HARVEST study). Wellcome Open Res 2019; 4:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Panjasawatwong N, Wattanakul T, Hoglund RM, et al. . Population pharmacokinetic properties of antituberculosis drugs in Vietnamese children with tuberculous meningitis. Antimicrob Agents Chemother 2020; 65:e00487-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cresswell FV, Meya DB, Kagimu E, et al. . High-dose oral and intravenous rifampicin for the treatment of tuberculous meningitis in predominantly HIV-positive Ugandan adults: a phase II open-label randomised controlled trial. Clin Infect Dis 2021; 73:876–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kalita J, Bhoi SK, Betai S, Misra UK.. Safety and efficacy of additional levofloxacin in tuberculous meningitis: a randomized controlled pilot study. Tuberculosis 2016; 98:1–6. [DOI] [PubMed] [Google Scholar]
- 39. van der Laan LE, Schaaf HS, Solomons R, et al. . Probable levofloxacin-associated secondary intracranial hypertension in a child with multidrug-resistant tuberculosis. Pediatr Infect Dis J 2016; 35:706–8. [DOI] [PubMed] [Google Scholar]
- 40. van Toorn R, Schaaf HS, Laubscher JA, van Elsland SL, Donald PR, Schoeman JF.. Short intensified treatment in children with drug-susceptible tuberculous meningitis. Pediatr Infect Dis J 2014; 33:248–52. [DOI] [PubMed] [Google Scholar]
- 41. Paradkar M, Devaleenal DB, Mvalo T, Arenivas A, Thakur KT, Afrin S, et al. . Challenges in conducting trials for pediatric tuberculous meningitis: lessons from the field. Int J Tuberc Lung Dis 2019; 23:1082–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cresswell FV, Meya DB, Kagimu E, et al. . High-dose oral and intravenous rifampicin for the treatment of tuberculous meningitis in predominantly human immunodeficiency virus (HIV)-positive Ugandan adults: a phase II open-label randomized controlled trial. Clin Infect Dis 2021; 73:876–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Garcia-Prats AJ, Svensson EM, Winckler J, et al. . Pharmacokinetics and safety of high-dose rifampicin in children with TB: the Opti-Rif trial. J Antimicrob Chemother 2021; 76:3237–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.