Abstract
Telemedicine has been an essential form of care since the onset of the COVID-19 pandemic. However, telemedicine may exacerbate disparities for populations with limited digital literacy or access, such as older adults, racial minorities, patients of low income, rural residences, or limited English proficiency. From March 2020 to March 2022, this retrospective cohort study analyzed the use of in-person, phone/message, and telemedical care at a single tertiary care center in an oncology department. We investigated the association between economic, racial, ethnic, socioeconomic factors and forms of care, including in-person visits, telemedicine-based visits, and telephone/messages. The study results show that telemedicine utilization is lower among patients 65 and older, female patients, American Indian or Alaska Native patients, uninsured patients, and patients who require interpreters during clinical visits. As a result, it is unlikely that telemedicine will provide equal access to clinical care for all populations. On the other hand, in-person care utilization remains low in low-income and rural-living patients compared to the general population, while telephone and message use remains high in low-income and rural-living patients. We conclude that telemedicine is currently unable to close the utilization gap for populations of low socioeconomic status. Patients with low socioeconomic status use in-person care less frequently. For the disadvantaged, unusually high telephone or message utilization is unlikely to provide the same quality as in-person or telemedical care. Understanding the causes of disparity and promoting a solution to improve equal access to care for all patients is critical.
Keywords: Telemedicine, Oncology, Remote Care, Health Disparity
Introduction
The COVID-19 pandemic affected healthcare delivery, with ambulatory outpatient visits declining by up to 70% in 2020 [1]. The reduction was partially complemented by telemedical care. A major part of telemedical care, such as virtual visits, decreases the risk of viral transmission and reduces the transportation costs [2]. Regulatory changes, such as support of payment equivalency between telemedicine and in-person visits [3], also encourage the shift to virtual care in the United States. As a result, the adoption of telemedicine surged at the onset of the pandemic [4]. Medical providers and payers quickly shift to a new normal of virtual care for efficient healthcare delivery and management [5].
However, we observe that the rise of telemedicine adoption did not reach all patients equally [6]. Our previous study [7] found that socioeconomic determinants are associated with telemedicine adoption. The inequality of socioeconomic status may exacerbate health care disparities. The disparities also exist in many clinical fields [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], departments, and countries, but no evidence shows the disparity in the oncology department currently. In this study, we demonstrated patients' forms of care adoption are associated with socioeconomic characteristics during the transition. We propose that technological transitions, such as telemedical care, should not exacerbate health disparities. Our findings are key to promoting equal access to telemedical care and establishing practices to mitigate inequalities.
Methods
Data source
This retrospective cohort study adopted Electronic Health Records from the Clinical Research Data Warehouse, a component of the Clinical and Translational Science Institute of Southeast Wisconsin. The Clinical Research Data Warehouse maintains a database of the Froedtert and Medical College Electronic Health Records. The database currently contains 2.3 million individual patient records. Clinical data is available upon registration for institutional members at Clinical and Translational Science Institute. Non-institutional researchers may register as community members for data access. The Froedtert Health Center and its IRB board approved the use of data for this study. Some data fields (zip code, address, and income) were redacted to maintain the anonymity of the individuals concerned.
Data collection
All patients signed up and visited the facility in the Department of Oncology at least once between March 2020 and March 2022. Each visit took the form of either in-person, telemedicine, or telephone/message. For each patient, we acquired the following variables: sub-department visited, age, sex, race, ethnicity, insurance status, employment status, interpreter required, Area Deprivation Index, and Rural-Urban Continuum Codes. Age was calculated at the date of visit minus the date of birth for each patient. Sex, race, ethnicity, employment status, and requirements of an interpreter during a clinical visit were acquired from electronic health records. Insurance status was classified into public, private, other, and uninsured based on the payer's information from the database. The Area Deprivation Index and Rural-Urban Continuum Codes are alternative variables of income and address to comply with the privacy regulations in this study.
The Area Deprivation Index (ADI) is based on a measure created by the Health Resources & Services Administration. It allows for rankings of neighborhoods by socioeconomic disadvantage in a region of interest. ADI ranges on a scale from 0 (least disadvantaged) to 100 (most disadvantaged) according to mixed factors, including income, education, employment, and housing quality. ADI can be used to inform socioeconomic status, health delivery, and policy conditions, especially for the most disadvantaged neighborhood groups.
The Rural-Urban Continuum Codes (RUCC) is a classification scheme that distinguishes metropolitan counties by the population size of their metropolitan areas, and nonmetropolitan counties by the degree of urbanization and adjacency to a metropolitan area. We split RUCC into two categories of metropolitan counties and non-metropolitan counties. Metropolitan counties refer to counties in all metropolitan areas defined by the Office of Management and Budget as of February 2013; non-metropolitan counties include all non-metro counties, as well as completely unlisted rural areas. RUCC can be used to assess a patient's living area and inform rural and urban differences with other social and economic variables.
Outcomes and results
The primary results were as follows: (1) patient demographics, departmental counts, and count of patients in telemedicine, in-person, and phone/message since the onset of the pandemic; (2) the association of socioeconomic characteristics and three forms of healthcare adoption. Socioeconomic characteristics include Age, Sex, Race, Ethnicity, Insurance Status, Employment Status, Interpreter needed, Area Deprivation index, Rural-urban continuum codes; (3) The results of the statistical models showing the association between forms of care and patient demographics.
Three forms of healthcare include in-person care, telemedical care, and patient phone or message. Patients receiving both telemedicine and in-person care were categorized as telemedicine visits for the purposes of this analysis, regardless of the order of visits. Patients with both telemedicine and phone/message visits are counted as telemedicine visits; similarly, patients with in-person and phone/message visits are counted as in-person visits.
Statistical analysis
A power analysis was undertaken beforehand to ensure that the sample size was large enough to support the analysis and yield significant results (see Appendix). All statistical analyses are performed in R programming language. Statistical tests were 2-sided, and alpha was set at 0.05. We calculated P-values using chi-square tests for categorical variables. In Table 2, we compare the difference in patient characteristics between the prior-pandemic group and the during-pandemic group. A 95% confidence interval was calculated based on a normal distribution of two populations. In Table 3, we use the odds ratio (OR) to measure the association between the telemedicine group and the in-person group for patient characteristics. Odds ratios are calculated through a two-by-two table. The table compares the effect size between the telemedicine group and the in-person group. For each patient characteristic, an odds ratio larger than 1 indicates patients with corresponding characteristics are more likely to visit telemedicine; an odds ratio smaller than 1 indicates patients with corresponding characteristics are less likely to adopt telemedicine. The 95% confidence interval shows the 95% likelihood range of the odds ratio based on a normal distribution. A P-value of less than 0.05 indicates the difference in patient characteristics between the two groups is significant.
Table 2.
Number of patients, March 2020 – March 2022, Froedtert Health Center Department of Oncology.
| Department |
In-person |
% | Telemedicine | % | Telephone or Message | % | Total number of patients |
|---|---|---|---|---|---|---|---|
| Hematology/Oncology | 23235 | 60.8% | 10251 | 26.8% | 28808 | 75.4% | 38210 |
| Medical Oncology | 7982 | 64.6% | 2614 | 21.2% | 8757 | 70.9% | 12354 |
| Neurologic Oncology | 434 | 49.2% | 185 | 21.0% | 558 | 63.2% | 883 |
| Gynecology/Oncology | 2326 | 67.2% | 427 | 12.3% | 2943 | 85.1% | 3460 |
| Radiation Oncology | 7854 | 78.7% | 1113 | 11.2% | 5527 | 55.4% | 9979 |
| Surgical Oncology | 7081 | 69.9% | 987 | 9.7% | 8465 | 83.5% | 10132 |
Table 3.
Characteristics of patients who participated in telemedicine, in-person care, and/or who made contact via telephone or text (SMS) message (March 2020 - March 2022).
| Patient Characteristics | In-person vs Telemedicine | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Telemedicine | In-person | Telephone or Message | Odds ratio | 95% CI | P-value | ||||
| Number of patients | 14152 | 32314 | 37990 | ||||||
| Age | 1 | ||||||||
| Median, (± SD) | 63.1 (46.6, 79.6) | 64.5 (48.8, 80.2) | 63.4 (47.2, 79.6) | <0.001 | |||||
| 0 - 17 years old | 0.2% | 24 | 0.3% | 113 | 0.2% | 80 | 0.48 | (0.31,0.75) | <0.001 |
| 18 - 44 years old | 19.4% | 2746 | 15.2% | 4920 | 17.9% | 6817 | 1.34 | (1.27,1.41) | <0.001 |
| 45 - 64 years old | 35.1% | 4961 | 35.8% | 11575 | 36.1% | 13701 | 0.97 | (0.93,1.01) | 0.113 |
| >65 years old | 45.4% | 6421 | 48.6% | 15705 | 45.8% | 17390 | 0.88 | (0.84,0.91) | <0.001 |
| Sex | 1 | ||||||||
| Female | 56.4% | 7984 | 57.1% | 18442 | 56.4% | 21428 | 0.97 | (0.94,1.01) | 0.189 |
| Male | 43.6% | 6168 | 42.9% | 13872 | 43.6% | 16557 | 1.03 | (0.99,1.07) | 0.189 |
| Race | 1 | ||||||||
| White | 81.4% | 11513 | 83.4% | 26937 | 82.1% | 31184 | 0.87 | (0.83,0.92) | <0.001 |
| Black | 14.0% | 1982 | 11.8% | 3798 | 11.8% | 4500 | 1.22 | (1.15,1.3) | <0.001 |
| Asian | 1.3% | 188 | 1.4% | 458 | 1.4% | 537 | 0.94 | (0.79,1.11) | 0.451 |
| Other | 2.9% | 409 | 3.1% | 987 | 3.3% | 1238 | 0.94 | (0.84,1.06) | 0.34 |
| Ethnicity | 1 | ||||||||
| Hispanic | 96.9% | 13711 | 96.6% | 31207 | 95.1% | 36139 | 1.1 | (0.99,1.23) | 0.087 |
| Non-Hispanic | 2.8% | 396 | 3.1% | 991 | 3.2% | 1229 | 0.91 | (0.81,1.02) | 0.117 |
| Type of Insurance | 1 | ||||||||
| Private | 46.5% | 6581 | 52.7% | 17018 | 45.3% | 17222 | 0.78 | (0.75,0.81) | <0.001 |
| Public | 52.9% | 7488 | 46.2% | 14923 | 50.7% | 19258 | 1.31 | (1.26,1.36) | <0.001 |
| Other | 0.4% | 60 | 1.0% | 322 | 0.9% | 331 | 0.42 | (0.32,0.56) | <0.001 |
| Uninsured | 0.2% | 22 | 0.2% | 49 | 0.1% | 52 | 1.03 | (0.62,1.70) | 0.923 |
| Employment Status | 1 | ||||||||
| Retired | 44.2% | 6261 | 46.7% | 15088 | 43.1% | 16382 | 0.91 | (0.87,0.94) | <0.001 |
| Full Time | 26.7% | 3785 | 27.1% | 8770 | 27.7% | 10513 | 0.98 | (0.94,1.02) | 0.378 |
| Not Employed | 10.2% | 1446 | 8.8% | 2859 | 9.5% | 3613 | 1.17 | (1.1,1.25) | <0.001 |
| Disabled | 8.2% | 1165 | 6.6% | 2118 | 7.1% | 2713 | 1.28 | (1.19,1.38) | <0.001 |
| Part Time | 5.0% | 702 | 4.9% | 1580 | 4.8% | 1834 | 1.02 | (0.93,1.11) | 0.745 |
| Self Employed | 3.7% | 521 | 3.8% | 1224 | 3.8% | 1462 | 0.97 | (0.87,1.08) | 0.579 |
| Student - Full Time | 1.1% | 159 | 1.0% | 330 | 1.1% | 426 | 1.1 | (0.91,1.33) | 0.32 |
| Student - Part Time | 0.0% | 7 | 0.1% | 22 | 0.1% | 24 | 0.73 | (0.31,1.7) | 0.46 |
| On Active Military Duty | 0.0% | 6 | 0.0% | 10 | 0.0% | 13 | 1.37 | (0.5,3.77) | 0.54 |
| Interpreter Needed | 1 | ||||||||
| Y | 0.7% | 104 | 1.5% | 483 | 1.4% | 543 | 0.49 | (0.39,0.6) | <0.001 |
| N | 99.3% | 14046 | 98.5% | 31819 | 98.6% | 37063 | 2.05 | (1.66,2.54) | <0.001 |
| Area Deprivation Index | 1 | ||||||||
| (Higher SE status) 0 - 25 | 11.1% | 1104 | 11.6% | 2532 | 11.2% | 2850 | 0.96 | (0.89,1.03) | 0.254 |
| 25 - 50 | 38.5% | 3815 | 39.2% | 8579 | 38.3% | 9760 | 0.97 | (0.92,1.02) | 0.211 |
| 50 - 75 | 30.7% | 3041 | 30.7% | 6714 | 31.1% | 7946 | 1 | (0.95,1.05) | 0.971 |
| (Lower SE status) 75 -100 | 19.7% | 1949 | 18.5% | 4038 | 19.4% | 4958 | 1.08 | (0.98,1.15) | 0.111 |
| Rural-Urban Continuum Codes | |||||||||
| Metropolitan Counties | 91.2% | 9406 | 91.3% | 20875 | 90.5% | 24123 | 0.99 | (0.91,1.07) | 0.721 |
| Non-Metropolitan Counties | 8.8% | 907 | 8.7% | 1983 | 9.5% | 2531 | 1.02 | (0.93,1.1) | 0.721 |
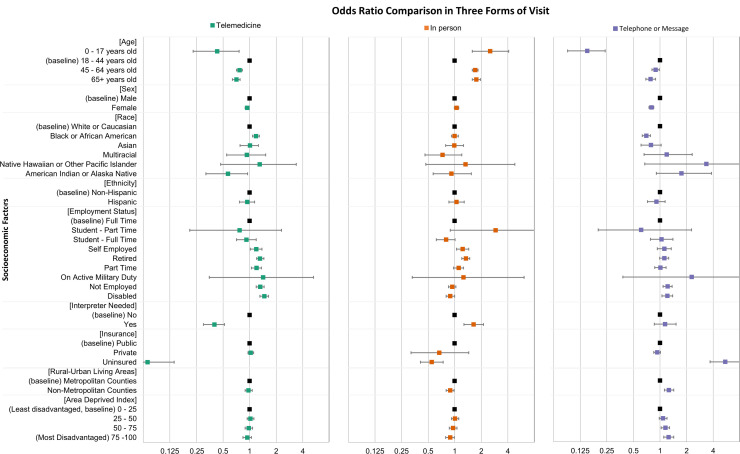
Table 4 recorded three additional multivariate logistic regression analyses to associate demographic factors with telemedicine vs in-person vs phone/message visits. The use of telemedicine, in-person care, and phone/message care were measured for each patient group separately. For each analysis, we build predictor variables including age, sex, race, ethnicity, employment status, insurance status, interpreter needed, Area deprivation index split into four quartiles, and rural-urban continuum codes. The dependent variables are in-person, telemedicine, and phone/message utilization. Finally, we integrated the three multivariate logistic regression models and compiled a forest plot (Fig. 3) in which the odds ratios and confidence intervals may be compared for each form of visit.
Table 4.
Association between patient characteristics and forms of care.
| OR,, Telemedicine | 95% CI | P-value | OR, In person | 95% CI | P-value | OR,Phone / Message |
95% CI | P-value | |
|---|---|---|---|---|---|---|---|---|---|
| Sex | |||||||||
| Male | 1 | 1 | 1 | ||||||
| Female | 0.94 | (0.89, 0.99) | 0.024 | 1.05 | (0.99, 1.11) | 0.100 | 0.8 | (0.75, 0.85) | <0.001 |
| Race | |||||||||
| White or Caucasian | 1 | 1 | 1 | ||||||
| Black or African American | 1.18 | (1.08, 1.29) | <0.001 | 1.0 | (0.92, 1.1) | 0.963 | 0.7 | (0.63, 0.78) | <0.001 |
| Asian | 0.99 | (0.78, 1.26) | 0.961 | 0.99 | (0.79, 1.26) | 0.956 | 0.79 | (0.61, 1.03) | 0.080 |
| American Indian or Alaska Native | 0.57 | (0.32, 0.95) | 0.040 | 0.92 | (0.57, 1.54) | 0.753 | 1.75 | (0.91, 3.82) | 0.120 |
| Multiracial | 0.93 | (0.55, 1.52) | 0.774 | 0.73 | (0.46, 1.2) | 0.210 | 1.19 | (0.66, 2.31) | 0.577 |
| Native Hawaiian or Other Pacific Islander | 1.3 | (0.47, 3.37) | 0.589 | 1.33 | (0.47, 4.79) | 0.622 | 3.34 | (0.67, 60.7) | 0.245 |
| Ethnicity | |||||||||
| Non-Hispanic | 1 | 1 | 1 | ||||||
| Hispanic | 0.94 | (0.77, 1.14) | 0.520 | 1.05 | (0.86, 1.28) | 0.628 | 0.91 | (0.72, 1.14) | 0.399 |
| Employment Status | |||||||||
| Full Time | 1 | 1 | 1 | ||||||
| Part Time | 1.2 | (1.05, 1.36) | 0.005 | 1.11 | (0.97, 1.26) | 0.124 | 1.01 | (0.87, 1.17) | 0.944 |
| Self Employed | 1.19 | (1.02, 1.38) | 0.024 | 1.23 | (1.05, 1.44) | 0.010 | 1.12 | (0.93, 1.34) | 0.227 |
| Student - Full Time | 0.92 | (0.71, 1.19) | 0.526 | 0.8 | (0.62, 1.01) | 0.063 | 1.04 | (0.78, 1.4) | 0.794 |
| Student - Part Time | 0.77 | (0.21, 2.3) | 0.659 | 2.91 | (0.89, 13.2) | 0.108 | 0.61 | (0.2, 2.27) | 0.408 |
| On Active Military Duty | 1.42 | (0.35, 5.28) | 0.604 | 1.26 | (0.33, 6.11) | 0.748 | 2.28 | (0.38, 43.9) | 0.451 |
| Retired | 1.32 | (1.2, 1.45) | <0.001 | 1.33 | (1.2, 1.48) | <0.001 | 1.12 | (0.99, 1.25) | 0.062 |
| Not Employed | 1.32 | (1.19, 1.46) | <0.001 | 0.94 | (0.85, 1.03) | 0.195 | 1.22 | (1.08, 1.37) | 0.001 |
| Disabled | 1.47 | (1.31, 1.64) | <0.001 | 0.89 | (0.8, 1) | 0.058 | 1.21 | (1.05, 1.39) | 0.010 |
| Insurance | |||||||||
| Public | 1 | 1 | 1 | ||||||
| Private | 1.03 | (0.96, 1.11) | 0.417 | 0.67 | (0.32, 1.44) | 0.286 | 0.93 | (0.85, 1.01) | 0.086 |
| Uninsured | 0.07 | (0.04, 0.14) | <0.001 | 0.55 | (0.41, 0.74) | <0.001 | 5.46 | (3.69, 8.39) | <0.001 |
| Interpreter Needed? | |||||||||
| No | 1 | 1.000 | 1 | 1 | |||||
| Yes | 0.4 | (0.30, 0.52) | <0.001 | 1.64 | (1.27, 2.12) | <0.001 | 1.14 | (0.86, 1.52) | 0.365 |
| Age | |||||||||
| 0 - 17 years old | 0.43 | (0.23, 0.76) | 0.009 | 2.52 | (1.58, 4.09) | <0.001 | 0.15 | (0.09, 0.24) | <0.001 |
| 18 - 44 years old | 1 | 1 | 1 | ||||||
| 45 - 64 years old | 0.77 | (0.71, 0.83) | <0.001 | 1.71 | (1.58, 1.84) | <0.001 | 0.89 | (0.81, 0.98) | 0.014 |
| 65+ years old | 0.71 | (0.64, 0.78) | <0.001 | 1.76 | (1.58, 1.96) | <0.001 | 0.78 | (0.69, 0.89) | 0.0001 |
| Area Deprived Index | |||||||||
| (Least disadvantaged) 0 - 25 | 1 | 1 | 1 | ||||||
| 25 - 50 | 1.02 | (0.94, 1.12) | 0.634 | 1.01 | (0.92, 1.11) | 0.798 | 1.08 | (0.98, 1.2) | 0.132 |
| 50 - 75 | 0.98 | (0.89, 1.08) | 0.690 | 0.96 | (0.87, 1.06) | 0.413 | 1.15 | (1.03, 1.28) | 0.012 |
| (Most Disadvantaged) 75 -100 | 0.94 | (0.84, 1.05) | 0.282 | 0.89 | (0.79, 0.99) | 0.039 | 1.25 | (1.10, 1.43) | <0.001 |
| Rural-Urban Living Areas | |||||||||
| Metropolitan Counties | 1 | 1 | 1 | ||||||
| Non-Metropolitan Counties | 0.97 | (0.89, 1.07) | 0.594 | 0.89 | (0.80, 0.98) | 0.014 | 1.26 | (1.12, 1.43) | <0.001 |
Fig. 3.
Comparison of odds ratio for each type of visit.
Results
Comparison of patient characteristics in pre-pandemic and during-pandemic years
Table 1 shows changes in patient characteristics since COVID-19 in oncology. During January 2019–February 2020, a total of 33,184 individual patients visited the oncology department. During the pandemic, a total of 46,943 individual patients visited the department.
Table 1.
Patient characteristics before pandemic and during pandemic.
| Before pandemic(a) Jan 2019 – Feb 2020 |
During pandemic Mar 2020 – Mar 2022 |
Diff, % | 95% CI, %(b) | P-value(c) | |||
|---|---|---|---|---|---|---|---|
| Number of patients | 33184 | 46943 | NA | NA | NA | ||
| Age | |||||||
| Median, (± SD) | 63.3 (47.3 - 79.4) | 63.2 (46.9 - 79.3) | NA | NA | 0.003(d) | ||
| 0 - 17 years old | 0.4% | 126 | 0.4% | 183 | 0.01 | (-0.08, 0.1) | 0.82 |
| 18 - 44 years old | 16.9% | 5592 | 18.1% | 8479 | 1.21 | (0.68, 1.74) | <0.001 |
| 45 - 64 years old | 37.5% | 12437 | 35.9% | 16848 | -1.59 | (-2.27, -0.91) | <0.001 |
| >65 years old | 45.3% | 15029 | 45.7% | 21430 | 0.36 | (-0.34, 1.06) | 0.312 |
| Sex | |||||||
| Female | 56.9% | 18897 | 57.4% | 26968 | 0.50 | (-0.18, 1.21) | 0.147 |
| Male | 43.1% | 14286 | 42.5% | 19968 | -0.50 | (-1.21, 0.18) | 0.147 |
| Race | |||||||
| White | 82.1% | 27232 | 81.5% | 38272 | -0.54 | (-1.08, 0.01) | 0.053 |
| Black | 12.4% | 4103 | 12.3% | 5788 | -0.04 | (-0.5, 0.43) | 0.884 |
| Asian | 1.3% | 446 | 1.5% | 694 | 0.13 | (-0.03, 0.3) | 0.114 |
| Other(e) | 3.0% | 988 | 3.2% | 1498 | 0.21 | (-0.03, 0.46) | 0.086 |
| Unknown | 1.3% | 415 | 1.5% | 691 | 0.22 | (0.06, 0.38) | 0.008 |
| Ethnicity | |||||||
| Hispanic | 3.1% | 1001 | 3.3% | 1506 | 0.21 | (-0.03, 0.46) | 0.096 |
| Non-Hispanic | 96.9% | 31796 | 96.7% | 44653 | -0.21 | (-0.46, 0.03) | 0.096 |
| Type of Insurance | |||||||
| Private | 43.6% | 14475 | 45.6% | 21401 | 1.97 | (1.27, 2.67) | <0.001 |
| Public | 53.3% | 17702 | 50.4% | 23645 | -2.98 | (-3.68, -2.27) | <0.001 |
| Other | 0.8% | 272 | 0.8% | 381 | -0.01 | (-0.13, 0.12) | 0.901 |
| Uninsured | 2.0% | 677 | 3.1% | 1443 | 1.03 | (0.82, 1.25) | <0.001 |
| Employment Status | |||||||
| Retired | 46.5% | 15019 | 43.9% | 19996 | -2.55 | (-3.25, -1.84) | <0.001 |
| Full Time | 26.1% | 8443 | 28.8% | 13121 | 2.70 | (2.07, 3.34) | <0.001 |
| Part Time | 4.9% | 1583 | 5.0% | 2286 | 0.12 | (-0.19, 0.43) | 0.434 |
| Self Employed | 3.9% | 1252 | 3.9% | 1761 | -0.01 | (-0.28, 0.27) | 0.97 |
| Not Employed | 9.3% | 2997 | 9.8% | 4450 | 0.50 | (0.09, 0.92) | 0.019 |
| Disabled | 8.2% | 2635 | 7.1% | 3251 | -1.01 | (-1.39, -0.63) | <0.001 |
| Student - Full Time | 1.1% | 347 | 1.3% | 598 | 0.24 | (0.09, 0.39) | 0.003 |
| Student - Part Time | 0.1% | 22 | 0.1% | 30 | 0.00 | (-0.04, 0.03) | 0.908 |
| On Active Military Duty | 0.0% | 13 | 0.0% | 17 | 0.00 | (-0.03, 0.03) | 0.84 |
| Interpreter needed? | |||||||
| N | 98.6% | 32369 | 98.6% | 45805 | -0.02 | (-0.18, 0.15) | 0.849 |
| Y | 1.4% | 461 | 1.4% | 660 | 0.02 | (-0.15, 0.18) | 0.849 |
| Area Deprivation Index | |||||||
| (Higher SE status) 0 - 25 | 10.9% | 2575 | 11.4% | 3592 | 0.41 | (-0.12, 0.94) | 0.129 |
| 25 - 50 | 38.8% | 9144 | 38.2% | 12089 | -0.65 | (-1.47, 0.18) | 0.123 |
| 50 - 75 | 31.1% | 7317 | 30.9% | 9772 | -0.21 | (-0.99, 0.57) | 0.605 |
| (Lower SE status) 75 -100 | 19.1% | 4502 | 19.6% | 6192 | 0.44 | (-0.22, 1.11) | 0.195 |
| Rural-Urban Continuum Codes | |||||||
| Metropolitan Counties | 90.5% | 22244 | 90.9% | 30053 | 0.42 | (-0.06, 0.89) | 0.089 |
| Non-Metropolitan Counties | 9.5% | 2329 | 9.1% | 2995 | -0.42 | (-0.89, 0.06) | 0.089 |
Data is expressed as the percentage and number of patients. Numbers may not sum to the total number of patients due to missing data. Percentages have been rounded and may not sum to an accurate total of 100%.
Calculated based on a percentage difference and a 95% confidence interval.
Unless otherwise indicated, values are calculated using a chi-square test.
Calculated using the Kruskal-Wallis test.
Includes American Indian or Alaska Native, Native Hawaiian or Pacific Islander, Mixed Race, and Other
(f)Acronyms and Abbreviations: CI: Confidence Interval; SD: Standard Deviation; NA: Not applicable; SE: Socioeconomic.
Age and Sex: The median age of patients who visited the department during the pandemic was slightly but significantly younger than pre-pandemic years (Median [± 1 Standard Deviation]: 63.3 [47.3 – 79.4] vs 63.2 [46.9 - 79.3], P=0.003). Patients between 18 and 44 years old had a larger proportion during the pandemic years compared with pre-pandemic years (16.9% [5,592] vs 18.1% [8,479]; difference: +1.21% [95% CI: 0.68%, 1.74%]; P<0.001). Patients between 45 and 64 years old consisted of a smaller proportion since the onset of pandemic (37.5% [12,437] vs 35.9% [16,848]; difference: -1.59% [95% CI: -2.27%, -0.91%], P<0.001). This result showed a larger group of young adults who visited the hospital during the pandemic compared with pre-pandemic years. Also, there was a small increase in the proportion of female patients (difference: +0.50%), but the increase is not statistically significant (P=0.147).
Race and ethnicity: There was no significant difference in proportion changes. The differences in proportion were -0.54%, -0.04%, 0.13%, 0.21% for White, Black, Asian, and other races. The proportion of patients with a Hispanic ethnicity increased by 0.2% (difference: 0.21, 95% CI: [-0.03%, 0.46%], P=0.096). All racial and ethnic changes were not significant.
Insurance: During the pandemic, there was an increase in the proportion of patients with private insurance (43.6% [14,475] vs 45.6% [21,401], difference: 1.97%, 95% CI: [1.27%, 2.67%], P<0.001). Less proportion of patients use public insurance of Medicare and Medicaid (53.3% [17,702] vs 50.4% [23,645]; difference: -2.98%; 95% CI: -3.68%, -2.27%; P < 0.001). We also see a higher proportion of uninsured patients (2.0% [677] vs 3.1% [1,443], difference: +1.03%, 95% CI: [0.82%, 1.25%], P<0.001).
Employment status: There was an increase in the proportion of full-time employed patients (26.1% [8,443] vs 28.8% [13,121], difference: +2.70%, 95% CI: [2.07%, 3.34%], P<0.001). At the same time, we see a comparable decrease in the proportion of retired patients (46.5% [15,019] vs 43.9% [19,996], difference: -2.55%, 95% CI [-3.25%, -1.84%], P<0.001). The proportion of patients with disability also decreased (8.2% [2,635] vs 7.1% [3,251], difference: -1.01%, 95% CI: [-1.39%, -0.63%], P<0.001). A slight increase is shown in the proportion of unemployed patients (9.3% [2,997] vs 9.8% [4,450], difference: +0.50%, 95% CI: [0.09%, 0.92%], P=0.019) and full-time students (1.1% [347] vs 1.3% [598], difference: +0.24%, 95% CI: [0.24%, 0.39%]). Patients of other employment status, including part-time employees and students, self-employed patients, and patients on active military duty have no significant changes in proportions.
Language, Socioeconomic statusand rural-urban factors: The proportion of patients needing an interpreter showed an insignificant increase (+0.02%, 95% CI: -0.15%, +0.18%, P=0.849). During the pandemic, there was a relative decrease in the proportion of patients from non-metropolitan counties (9.5% [2,329] vs 9.1% [2,995], difference: -0.42%, 95% CI: [-0.89%, 0.06%], P=0.089). For the Area Deprivation Index factors, we observed no considerable changes. However, a larger proportion of patients who come from the highest quartile of ADI shows a slight increase (10.9% [2,575] vs 11.4% [3,592], difference: +0.41%, P = 0.129)
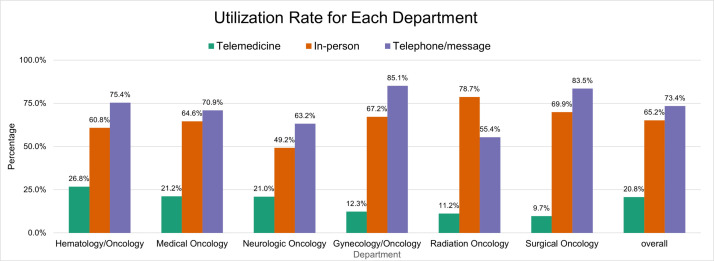
Patient count during the pandemic by sub-department
During the pandemic between March 2020 and March 2022, a total of 46,943 patients visited the oncology department. 57.4% were female. The overall utilization rate of telephone or messages is 73.4% among all patients, which means 73.4% of all patients had phone calls or sent messages to providers. The overall utilization of in-person care is 65.2%, and the utilization of telemedical care is 20.8%. Fig. 1 shows the utilization rate for each sub-department. The Hematology/Oncology service had the highest proportion of telemedical care utilization (26.8%). The Gynecology/Oncology service had the highest telephone/message utilization (85.1%) compared to other departments and specialties. Radiation Oncology had the highest in-person utilization rate (78.7%). Table 2 shows the number of patients and percentage of patients who chose different forms of care. While the overall utilization of in-person care and telephone/message remains high, the telemedicine adoption rate is considerably lower than the other two forms of care.
Fig. 1.
Utilization rate for each department.
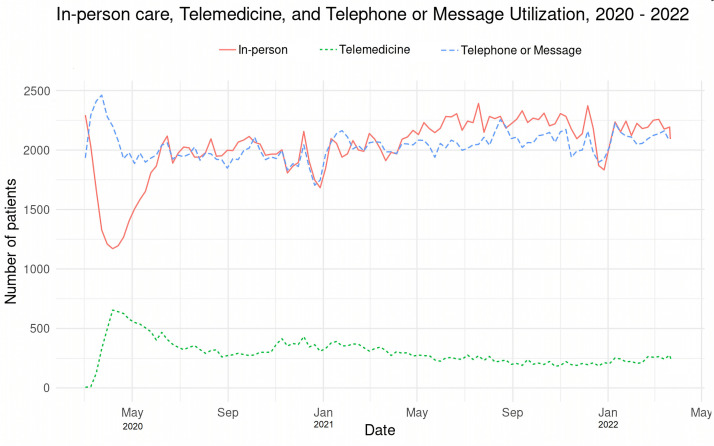
Change in number of patients during pandemic
Fig. 1 shows the weekly changes of new patients who utilized each form of care. Before the onset of the COVID-19 Pandemic, almost all patients adopted either in-person or telephone/message, with close-to-zero patients who exclusively used telemedical care. Beginning in March 2020, the count of in-person patients declined from 2268 to as low as 1197 in mid-March. The reduction was accompanied by a simultaneous rise in the number of weekly visits, peaking from zero to 704 in late March. After April, there was a subsequent rise in the in-person patient count. The rising trends last from late March to mid-June and remain at the same level as before the pandemic. The adoption of telemedicine experienced a slight but steady decline until the end of 2020. Since 2021, the count of telemedicine patients ranged from 200 to 300. The second wave of pandemics from August 2020 to February 2021 does not cause a significant change in forms of care, except for a slight increase in telemedicine at the end of 2020. The number of patients who use telephone/message peaked at 2488 in mid-March of 2020. The telemedicine and message counts return to the same level, roughly equal to the in-person patient counts. (Fig. 2 ).
Fig. 2.
Weekly numbers of patients according to form of treatment: in-person care, telemedical care, and telephone or message service.
Relationship between forms of care and patient characteristics
Table 3 shows three groups of patients who used telemedicine, in person, by phone, or by message, as well as their racial, social, and economic characteristics. During the pandemic, 14,152, 32,314 and 37,990 patients received telemedical care, in-person care, and telephone/message care, respectively. The median age of telemedicine patients was 63.1 ([median ± standard deviation]: [46.6, 79.6]), and 64.5 ([median ± standard deviation] (48.8, 80.2) for in-person patients. The difference in median age is significant (P<0.001). Patients over the age of 65 are 0.88 times more likely to visit telemedicine than patients under the age of 65 (OR: 0.88, 95% CI: [0.84,0.91], P<0.001). Patients aged 0 to 17 are less likely to use telemedicine (OR: 0.48, 95% CI: [0.31, 0.75], P<0.001) than patients aged 18 and up. In comparison to a total of two populations of telemedicine and in-person patients as a baseline, we discovered that patients aged 18 to 44 are 1.34 (95% CI: [1.27, 1.41], P<0.001) times more likely to use telemedicine than other patients not in this age range. There is no correlation between sex and telemedicine or in-person care. Furthermore, when compared to other racial factors, the black race is associated with a higher receipt of telemedical care (OR = 1.22, 95% CI: [1.15, 1.30], P<0.001). There is no correlation between the type of care and Hispanic patient characteristics. In terms of insurance, privately insured patients are less likely to use telemedicine and more likely to use in-person care (OR: 0.78, 95% CI: [0.75, 0.81], P<0.001). Publicly insured patients are more likely to receive telemedical care (OR: 1.31, 95% CI: [1.26, 1.36], P<0.001). Retired patients are less likely to use telemedical care than other employment status patients (OR: 0.91, 95% CI: [0.87, 0.94], P<0.001). Patients with disabilities, on the other hand, are more likely to prefer telemedical care over in-person care (OR: 1.28, 95% CI: [1.19, 1.38], P<0.001). The increased use of telemedical care is also seen in unemployed patients, with an odds ratio of 1.17 (95% CI: [1.10, 1.25], P<0.001). Patients who require an interpreter during visits have a significantly lower utilization of telemedicine (OR =0.49, 95% CI [0.39, 0.6]). P<0.001). There are no significant differences in telemedical care for patients with varying levels of area deprivation. Furthermore, we find no correlations between rural/urban factors and changes in telemedical care utilization.
Table 4 shows the characteristics of patients who participated in telemedicine, in-person, and phone/message utilization. A comparison of three forms of care shows the odds of utilization for patients of various demographical and socioeconomical characteristics. Fig. 3 is a visualization of Table 4. It shows odds ratios from three different logistic regression models. We showed the patient demographic and socioeconomic factors associated with changes in three forms of care.
Age: When compared to patients aged 18 to 44 years old, patients aged from 0 to17 years old have lower telemedicine utilization, higher in-person care utilization, and lower telemedicine/message use. Patients between the ages from 45 to 64 are less likely to use telemedicine and more likely to visit in person. Patients aged from 18 too44 are also less likely to use the phone or send a text message. This trend is slightly stronger among patients over 65, who are 0.71 (95% CI: [0.64, 0.78], P<0.001) times more likely to use telemedicine than patients aged from 18 to44. The odds ratio for a face-to-face visit is 1.76 (95% CI: [1.58, 1.96], P<0.001), and the odds ratio for phone or message use is 0.78 (95% CI: [0.69, 0.89], P<0.001).Sex: Female patients are 0.94 (95% CI: [0.89, 0.99], P=0.024) times more likely than male patients to use telemedical care. Female patients are more likely than males to visit in person (OR: 1.05, 95% CI: [0.99, 1.11]), but the odds ratio is not significant. Males are significantly less likely to use the phone/message (OR: 0.80, 95% CI: [0.75, 0.85], P<0.001).
Race and ethnicity: When compared to white patients, black patients had a higher likelihood of using telemedicine (OR: 1.18, 95% CI: [1.08, 1.29], P=0.0002). There are no significant differences in the likelihood of receiving in-person care (OR = 1.0, 95 CI: [0.92, 1.1]) among black patients. Patients of the black race were significantly less likely than white patients to use the phone/message (OR = 0.70, 95% CI: [0.63, 0.78]). The odds of using telemedicine and in-person care are the same for Asian patients as for white patients, but the odds of using phone/message are lower (OR = 0.79, 95% CI: [0.61, 1.03], P=0.08). Patients who were American Indian or Alaska Native had a significantly lower chance of receiving telemedical care (OR: 0.57, 95% CI: [0.32, 0.95], P=0.04). The associations between other races and types of care were not significant. Similarly, Hispanic factors are not linked to any type of care.
Employment Status: Compared with full-time-employed patients, full-time students had lower odds of using in-person care (OR = 0.8, 95% CI: [0.62, 1.01], P=0.063). There are no significant associations between full-time student status and the changes in telemedicine or telephone/message utilization. Self-employed patients had higher odds of using telemedicine (OR: 1.19, 95% CI: [1.02, 1.38], P=0.024) and in-person care (OR: 1.23, 95% CI: [1.05, 1.44], P=0.01). Retired patients are at a significantly higher odds of utilization in Telemedicine (OR: 1.32, 95% CI: [1.2, 1.45], P<0.001), in-person visits (OR: 1.33, 95% CI: [1.2, 1.48], P<0.001) and Phone or Messages (OR = 1.12, 95% CI: [0.99, 1.25], P=0.062). For unemployed patients, the odds of using telemedicine (OR: 1.32, 95% CI: [1.19, 1.46], P<0.001) and phone/message (OR =1.22, 95% CI: [1.08, 1.37], P=0.001) are higher than full-time employed patients. For patients with disability, it shows higher odds of telemedicine (1.47, 95% CI: [1.31, 1.64], P<0.001) and Phone/Message (OR=1.21, 95% CI: [1.05, 1.39]). The chances of in-person visits for patients with disability are significantly lower than full-time employed patients, with an odd ratio of 0.89 (95% CI: [0.80, 1.00], P=0.058).
Insurance status: Compared with public-insured patients, there is no significant odds difference between private insured patients. However, we observed uninsured patients had a particularly low chance of telemedicine utilization (OR: 0.07, 95% CI: [0.04, 0.14], P<0.001). The in-person visit odds for uninsured patients are also low (OR: 0.55, 95% CI: [0.41. 0.74], P<0.001). Meanwhile, the odds of utilization on phone/message are more than five times (OR: 5.46, 95% CI: [3.69, 8.39], P<0.001), which shows that most uninsured patients rely considerably more on telephone/message for healthcare needs.
Language, socioeconomic status, and rural-urban factors: Patients who require an interpreter during a visit are less likely to use telemedicine (OR: 0.40, 95% CI: [0.30, 0.52], P<0.001) and more likely to visit in person (OR:1.64, 95% CI: [1.27, 2.12], P<0.001). In terms of socioeconomic status, there is no significant difference between the four levels of categorization and the odds of telemedicine utilization. The plot demonstrates a trend in which patients in more disadvantaged areas have a lower utilization of telemedical care and in-person care. Patients who live in more disadvantaged areas are also more likely to use the phone or send text messages. Rural and urban factors are also linked to different types of care utilization. Patients living in non-metropolitan counties had a lower likelihood of in-person visits (OR: 0.89, 95% CI: [0.8, 0.98], P=0.014) and a higher likelihood of phone/message use (OR: 1.26, 95% CI: [1.12, 1.43], P<0.001). The likelihood of using telemedicine did not change significantly.
Discussion
While the COVID-19 pandemic necessitated the use of telemedicine, its use may exacerbate disparities in populations with limited digital literacy or access, such as older adults, racial minorities, patients of low income, rural residences, or limited English proficiency. In this study, we found disparities in demographics of patients who used telemedicine, in person and phone/message for oncology care during the pandemic in a single tertiary care center. Although telemedicine is increasingly considered an approach to decreasing health care disparities, we found that telemedicine adoption rates are low in certain populations, especially for socioeconomically disadvantaged groups. Instead, the particularly high utilization of telephone/message may not be able to bridge the gap in quality of care.
Telemedicine adoption in oncology department
Because of the COVID-19 pandemic, telemedicine has expanded for diagnosis, treatment, monitoring, and follow-up. Telemedicine adoption rates vary by specialty, but it is still underutilized in the oncology department. In comparison to the high utilization rates for telephone/message (73.4%) and in-person care (65.2%), telemedicine utilization is significantly lower (20.8%). The adoption following a stay-at-home order in March 2020 declined to a low level (200-300 weekly patients) after May 2020. This could be due to the nature of cancer and its treatments. In-person visits are required for physical, surgical, radiological, or pharmaceutical interventions. The lack of treatment options in telemedicine may be the primary reason for the low adoption rate of telemedical care.
Compared with other care delivery centers, the utilization rate at Froedtert Health was significantly lower. As of August 2020, UT San Antonio Mays Cancer Center reported about 40% of cancer patient visits occurred by telehealth [18]. At the University of New Mexico Comprehensive Cancer Center (Albuquerque, NM), approximately 35% of patients choose to visit virtually [19]. The low adoption rate in the oncology department could be attributed to limited programs of remote treatment plans, such as home-based immunotherapy or chemotherapy infusions. Most patients on regimens of intravenous therapy must physically come to the cancer center for administration.
Specialist online oncology consultancy services may be a viable alternative for quickly integrating telemedicine into support services such as remote home monitoring, knowledge learning, and remote consulting [20]. As oncology involves physical and new targets and treatments, a sub-specialist expert can provide a critical supplement for general oncologists managing patients with ten or more different types of cancer. Telemedicine makes it possible to provide direct insights from oncology specialists. [6] These services may also include genetic counselors, pathologists, palliative care specialists, nutritionists, and social workers, who are not always available in cancer centers.
Inequality of telemedicine access and in-person access
Successful implementation of telemedical practices has been demonstrated in psychology [21], otolaryngology [13], endocrinology [22], surgery [23], pediatrics [24], and ophthalmology [12]. However, data shows patients with lower socioeconomic status often fail to enjoy the convenience of telemedical care. This inequality exacerbated the disparity between patients adopting telemedical care and those adopting in-person care. We demonstrated that this situation also exists in the oncology department.
Our study found that patients aged 65 years and older, female patients, American Indian or Alaska Native patients, uninsured patients, and patients requiring interpreters during clinical visits had a lower utilization of telemedicine than the overall population. Other studies have reported similar disparities [9,[25], [26], [27]]. Some reasons may explain the decreased use of telemedicine in socioeconomically disadvantaged populations, such as the unavailability of digital devices among socioeconomically disadvantaged groups, lower technological literacy, and higher transportation costs for patients living in rural areas. As COVID-19 disproportionally impacted low-income families and low-socioeconomic-status populations [28], it is essential to implement innovative care delivery solutions to avoid further exacerbation of disparities. Further investigation of the causes of demographic disparities for each economic, racial, and social variable is needed to bridge the utilization gap for patients in need of telemedical care.
The utilization of in-person care also differs from patient characteristics. Patients who are older and require an interpreter's assistance are more likely to visit in person and less likely to visit in telemedicine. Patients with disabilities, or uninsured, or living in a socioeconomically disadvantaged area, or in rural areas are less likely to visit in person. This indicates the utilization of in-person care also varies in populations.
Our study suggests a lack of quality care
It is important to understand the reasons behind the changes in telemedicine and in-person utilization rates. The rate change can be one of three reasons: (1) Lower telemedical care utilization and higher in-person care utilization may indicate that a certain population did not transition to telemedicine; (2) Lower in-person care utilization and higher telemedical care utilization may indicate a successful transition from in-person care to telemedicine. (3) A group experiencing a lack of quality care may have a lower utilization of both telemedical care and in-person care.
In this study, we found that three situations co-exist simultaneously. Firstly, female patients, those aged from 45 to 64, those aged 65 and up, and those who require an interpreter have lower telemedicine adoption and higher in-person care adoption. We believe patients with these characteristics continue to receive traditional in-person care and have not switched to telemedicine. Second, patients with disabilities or those with private insurance use telemedicine more frequently but receive less in-person care. These characteristics may make a successful transition to telemedicine more likely. Finally, patients who are uninsured, live in a socioeconomically disadvantaged area, or live in a rural area use telemedicine and in-person care less frequently. This could be a sign of inequality. Furthermore, we found that uninsured patients (OR=5.46), patients living in non-metropolitan counties (OR=1.26), and patients living in the most socially disadvantaged areas (OR=1.25) used the phone and messages the most (OR=1.25). The population's high use of telephone/message care and low use of in-person and telemedicine care clearly demonstrates unmet medical care needs. As a result, statistical analyses show that patients who are uninsured, live in rural areas, or are socioeconomically disadvantaged do not receive the same level of care.
Socioeconomic status is associated with telemedicine adoption
Successful adoption of telemedicine requires broadband internet and digital devices, which creates two barriers compared with in-person visits: First, a patient must have access to the internet to accommodate audio and visual data, which can be sometimes unpractical for low-income families. Also, the quality of the digital devices in households, including the camera and microphone, has a significant impact on communication quality and visual diagnostic accuracy. Increasing the quality of the Internet in low-income populations could encourage telemedical care. We believe that healthcare systems, local governments, and private Internet companies should create partnerships to benefit a wider range of households.
Limited English proficiency is another barrier that complicates telemedical care. Although only 1.5% of in-person visits require interpreters, only half the number of patients (0.7%) are not able to communicate in English for telemedicine visits (Table 3). This may indicate the half number of patients did not choose telemedicine service because they were afraid to use interpreters on a telemedical system. The need for trained medical interpreters complicated the delivery of telemedical care to non-English-speaking patients. Although the telemedical system applications integrate the functionality of interpreters, the additional resources and effort is required to use the function. Patients are concerned about a user interface that is difficult to use. The fear may deter patients from using telemedicine. The intensive use of staff resources, combined with a limited number of non-English-speaking patients, results in lower adoption among non-English-speaking patients. This problem can be solved by staff training. Patients may also be encouraged to use online interpreting services. Appropriate training can reduce patients’ concerns about uncertainty. Staff can work with third-party interpreters seamlessly, causing as less barrier as possible.
Telephone/message should not replace telemedicine
We found that the telephone/message is a common choice of care. The utilization of telephone/message is also associated with patient characteristics. Patients who are more than 65 years old, or female, or black race have lower utilization of telephone/message. This reveals patients’ preferences in choosing different forms of telemedical care. Compared with telephone visits, video-based telemedical visits allow parts of physical and clinical examination, especially for skin diseases. Telemedical visits also construct more personal connections between clinicians and patients. However, the telemedicine visit is not likely to be accessible for patients without technical literacy and broadband internet connection [29]. For example, The Federal Communications Commission reported that at least 21 million people lack broadband internet access in the United States [30]. Thus, many of them are not ready to adopt the new forms of visits.
In addition, technical difficulties are another barrier for patients and clinicians getting involved in telemedicine-visiting workflows. The factors of technical difficulty and unavailability may be the reason for lower video-based telemedical care adoption for specific patient groups. This difficulty reveals the trade-off between choosing video-based telemedicine and the telephone. Video provides higher quality care, but it has higher technical barriers. Although the telephone is more accessible, it is not appropriate for clinical needs. We think health systems are supposed to support patients for the maximum sake of patients’ health. When investing in video-visit infrastructure can promote care for patients, it is necessary to adopt technologically difficult solutions. In the meantime, keep everything simple when the telephone is sufficient. Therefore, we suggest future work should establish a clinical decision process to determine in which cases the telephone is the most appropriate. The same standard should also apply to video visits to ensure the most efficient communication. The lack of clinical decision quality on video or telephone is not a reason to promote telephone visits but an incentive to expedite a clear solution to bridge the disparity and achieve health equality in the future.
Limitations
We accept that this study has some limitations. First, retrospective data may introduce potential bias because the electronic health records may contain errors or inconsistencies. The missing information on race, ethnicity, type of insurance, employment status, rural/urban categorization, and Area Deprived Index may lead to inaccurate results in statistical analysis. Second, patients with systemic comorbidities may have opted for telemedicine over in-person care because of the coronavirus infection risk; conversely, patients who received in-person care for other conditions may have felt more comfortable attending in-person visits. This may introduce bias to the result. Lastly, the target is a single practice at Froedtert Health in Milwaukee, United States, which may not be generalizable to other clinical facilities. Our future studies will investigate how clinical outcomes are associated with changes in forms of clinical care. Some common diseases are more prevalent in historically marginalized populations. For example, diabetes is more prevalent among populations with lower incomes and a high body mass index. Addressing the inequality related to clinical outcomes will be valuable in clinical practice.
Conclusion
Telemedical care adoption is associated with disparities between patients of different demographics and socioeconomic status during the COVID-19 pandemic. Patients cannot access remote care equally for social and economic reasons. The uptake of telemedicine was lower for those patients who were older, female, or American Indian or Alaska Native, or who needed an interpreter during a visit, or who lived in the most disadvantaged area indicated by the last quartile of the Area Deprived Index. The lower utilization of telemedicine was complemented by a higher utilization of in-person visits than the overall average for certain patients, such as those between 45 and 64 years old, those over 65 years old, those retired, and those who need interpreters during visits. However, we observed no increase in either in-person or telemedical care for patients living in areas with a high Area Deprivation Index, the uninsured, or those living in non-metropolitan areas. Data of phone or message utilization shows the marginalized populations are not receiving equal access to in-person or telemedical care. The potential exacerbation of health inequalities in oncology telemedicine necessitates the importance of focusing on equitable health care delivery through telemedicine in the future. Future investigation is needed to discover other reasons for disparities. We believe preventive strategies require concentrated action between medical facilities, governments, and internet service providers to achieve equitable access to telemedical care.
Research ethics and IRB approval
No human or animal subjects were involved in this project. The Froedtert Health Center and IRB board approved the use of Electronic Health Records for this study. Some data fields (zip code, address, and income) have been removed to maintain the anonymity of the individuals concerned.
Declaration of Competing Interest
All authors declare no conflict of interest.
Acknowledgements
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, Award Number UL1TR001436. The content is solely the responsibility of the author(s) and does not necessarily represent the official views of the NIH.
This project is also funded by the Research and Education Program Fund, a component of the Advancing a Healthier Wisconsin Endowment at the Medical College of Wisconsin.
Appendix: Power analysis on Telemedicine vs In-person age groups
Executive summary
With a sample of 2,319 subjects per group, the study will have a power of 80%. This means that there is an 80% likelihood that the study will yield a statistically significant effect and allows us to conclude that the percentage of subjects in '0 - 17 years old' differs for telemedicine versus in person.
Details
The study will compare two groups (telemedicine versus in-person) on a collection of categories called Visit Type. The collection is composed of the following 4 categories: '0 - 17 years old', '18 - 44 years old', '45 - 64 years old', and '65 + years old'.
Our focus is on the category called '0 - 17 years old'. The null hypothesis is that the proportion of subjects in this category is identical in telemedicine and in-person. Our intent is to disprove the null, and conclude that this proportion is different in the two groups.
The computation of sample size is based on the following assumptions and decisions.
Telemedicine group
The expected pattern of responses for Telemedicine is as follows (see plot). '0 - 17 years old' (0.2%), '18 - 44 years old' (19%), '45 - 64 years old' (34%), '65 + years old' (45%). In particular, the percentage in '0 - 17 years old' is 0.2%.
In-person group
The expected pattern of responses for in-person is as follows (see plot). 0 - 17 years old (0.3%), 18 - 44 years old (19%), 45 - 64 years old (35%), 65 + years old (45%). In particular, the percentage in 0 - 17 years old is 0.3%.
Missing
In computing the sample size, we assume that there will be no missing data.
Sample size
The study will need to enroll 2,319 people per group, for a total of 4,638 people. With this sample size, there is an 80% likelihood that the study will yield a statistically significant result, and allow us to conclude that the percentage of subjects in '0 - 17 years old' is different for telemedicine than for in-person.
Understanding the assumptions
The decision to use a sample size of 2,319 per group is based on the assumptions outlined above. If these assumptions are correct, then this sample size will result in power of 80%. However, if these assumptions are incorrect, then the sample size needed to yield power of 80% will be higher or lower than 2,319 per group. Therefore, it is instructive to consider what sample size would be required if we adopted a different set of assumptions.
The computation of the required sample size is based on five factors, as follows.
Difference between groups
One factor that determines the required sample size is the mean difference between groups. A small difference is relatively hard to detect, and therefore requires a larger sample size. Conversely, a large difference is relatively easy to detect, and therefore requires a smaller sample size.
The sample size of 2319 assumes that groups differ by one percentage point.
Absolute value of the proportions
Another factor that determines the required sample size is the absolute value of the proportions. The sample size required to detect a one percentage point difference will be larger if the proportions fall near 50%, and will be smaller if the proportions fall near 0% or near 100%.
Missing data
Another factor that determines the required sample size is the percent of missing data. We compute the number of subjects actually needed for the analysis, and then adjust that number to ensure that we will have that number of responses after the missing subjects are excluded.
In computing the sample size to be 2,319, we assume that there will be no missing data. If the actual rate of missing data is 2%, we would need a sample size of 2,366 per group.
Note that the adjustment for missing data assumes that the data is missing completely at random. No attempt is made to adjust for the possibility that people who fail to respond differ in some ways from people who do provide a response.
Alpha
Another factor that has an impact on the required sample size is alpha, the criterion used for statistical significance. We used an alpha of 0.05, which is often the default value, in computing the required sample size of 2,319 per group.
It is sometimes appropriate to select a more conservative criterion. For example, with alpha set at 0.01 the required sample size would be 3,450 per group. Conversely, it is sometimes appropriate to select a less conservative criterion. For example, with alpha set at 0.10 the required sample size would be 1,826 per group.
Tails
The final factor we need to consider is whether the significance test is one-tailed or two-tailed. We assumed that the study would use a two-tailed test, which is usually appropriate, and computed the required sample size as 2,319 per group.
If it were appropriate to use a one-tailed test (with alpha at 0.05) the required sample size would be 1,826 per group.
Concluding remarks
This discussion is intended to highlight the importance of the assumptions in computing sample size. Where possible, it may be a good idea to take account of alternate assumptions to ensure that the sample size is adequate even if (for example) the mean difference is smaller than expected.
References
- 1.Chatterji P, Li Y. Effects of the COVID-19 pandemic on outpatient providers in the United States. Med. Care. 2021;59(1):58–61. doi: 10.1097/MLR.0000000000001448. [DOI] [PubMed] [Google Scholar]
- 2.Bokolo Anthony Jnr. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J. Med. Syst. 2020;44(7):1–9. doi: 10.1007/S10916-020-01596-5/FIGURES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency | HHS.gov. Accessed December 20, 2021. https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html.
- 4.Zanaboni P, Wootton R. Adoption of telemedicine: from pilot stage to routine delivery. BMC Med. Inf. Decis. Making. 2012;12(1):1–9. doi: 10.1186/1472-6947-12-1/FIGURES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bashshur RL, Shannon GW, Krupinski EA, et al. National telemedicine initiatives: essential to healthcare reform. https://home.liebertpub.com/tmj. 2009;15(6):600-610. doi: 10.1089/TMJ.2009.9960. [DOI] [PubMed]
- 6.Thomas-Jacques T, Jamieson T, Shaw J. Telephone, video, equity and access in virtual care. npj Digit. Med. 2021;4(1):1–3. doi: 10.1038/s41746-021-00528-y. 2021 4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo J, Tong L, Crotty BH, et al. Telemedicine adoption during the COVID-19 pandemic: gaps and inequalities. Appl. Clin. Inform. 2021;12(4):836–844. doi: 10.1055/S-0041-1733848/ID/JR210042RA-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lam K, Lu AD, Shi Y, Covinsky KE. Assessing telemedicine unreadiness among older adults in the United States During the COVID-19 pandemic. JAMA Intern. Med. 2020;180(10):1389–1391. doi: 10.1001/JAMAINTERNMED.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. J. Am. Med. Inform. Assoc. 2021;28(1):33–41. doi: 10.1093/JAMIA/OCAA217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miyawaki A, Tabuchi T, Ong MK, Tsugawa Y. Age and social disparities in the use of telemedicine during the COVID-19 pandemic in japan: cross-sectional study. J. Med. Internet Res. 2021;23(7):e27982. doi: 10.2196/27982. https://www.jmir.org/2021/7/e27982 2021;23(7):e27982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang X, Hidrue MK, del Carmen MG, Weiner RB, Wasfy JH. Sociodemographic disparities in outpatient cardiology telemedicine during the COVID-19 pandemic. Circulation: Cardiovasc. Qual. Outcomes. 2021 doi: 10.1161/CIRCOUTCOMES.121.007813. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen EM, Andoh JE, Nwanyanwu K. Socioeconomic and demographic disparities in the use of telemedicine for ophthalmic care during the COVID-19 pandemic. Ophthalmology. 2022;129(1):15–25. doi: 10.1016/J.OPHTHA.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tam S, Wu VF, Williams AM, et al. Disparities in the uptake of telemedicine during the COVID-19 surge in a multidisciplinary head and neck cancer population by patient demographic characteristics and socioeconomic status. JAMA Otolaryngol.–Head Neck Surg. 2021;147(2):209–211. doi: 10.1001/JAMAOTO.2020.3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roghani A, Panahi S. Does telemedicine Reduce health disparities? Longitudinal evidence during the COVID-19 pandemic in the US. medRxiv. Published online March 2, 2021:2021.03.01.21252330. doi: 10.1101/2021.03.01.21252330. [DOI]
- 15.Bakhtiar M, Elbuluk N, Lipoff JB. The digital divide: how COVID-19’s telemedicine expansion could exacerbate disparities. J. Am. Acad. Dermatol. 2020;83(5):e345–e346. doi: 10.1016/J.JAAD.2020.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thomas A, Flanary V, Friedland DR, et al. The impact of social determinants of health and clinical comorbidities on post-tympanotomy tube otorrhea. Int. J. Pediatr. Otorhinolaryngol. 2021 doi: 10.1016/J.IJPORL.2021.110986. Published online November 20, [DOI] [PubMed] [Google Scholar]
- 17.Poetker DM, Friedland DR, Adams JA, Tong L, Osinski K, Luo J. Socioeconomic determinants of tertiary rhinology care utilization: OTO open. 2021;5(2). doi: 10.1177/2473974X211009830. [DOI] [PMC free article] [PubMed]
- 18.Mesa R. Telemedicine and cancer care: lessons from the COVID-19 pandemic commentary overview. Published online 2020.
- 19.Knudsen KE, Willman C, Winn R. Optimizing the use of telemedicine in oncology care: postpandemic opportunities. Clin. Cancer Res. 2021;27(4):933–936. doi: 10.1158/1078-0432.CCR-20-3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boehm K, Ziewers S, Brandt MP, et al. Telemedicine online visits in urology during the COVID-19 pandemic—potential, risk factors, and patients’ perspective. Eur. Urol. 2020;78(1):16–20. doi: 10.1016/j.eururo.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Valenzuela J, Crosby LE, Harrison RR. Commentary: reflections on the COVID-19 pandemic and health disparities in pediatric psychology. J. Pediatr. Psychol. 2020;45(8):839–841. doi: 10.1093/JPEPSY/JSAA063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myers A, Presswala L, Bissoonauth A, et al. Telemedicine for disparity patients with diabetes: the feasibility of utilizing telehealth in the management of uncontrolled type 2 diabetes in black and hispanic disparity patients; a pilot study. J. Diabet. Sci. Technol. 2020;15(5):1034–1041. doi: 10.1177/1932296820951784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lattimore CM, Kane WJ, Fleming MA, et al. Disparities in telemedicine utilization among surgical patients during COVID-19. PLoS One. 2021;16(10) doi: 10.1371/JOURNAL.PONE.0258452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Katzow MW, Steinway C, Jan S. Telemedicine and health disparities during COVID-19. Pediatrics. 2020;146(2) doi: 10.1542/PEDS.2020-1586/36919. [DOI] [PubMed] [Google Scholar]
- 25.Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J. Telemed. Telecare. 2020 doi: 10.1177/1357633X20963893. Published online October 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wegermann K, Wilder JM, Parish A, et al. Racial and socioeconomic disparities in utilization of telehealth in patients with liver disease during COVID-19. Dig. Dis. Sci. 2021;1:1–7. doi: 10.1007/S10620-021-06842-5/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aziz K, Moon JY, Parikh R, et al. Association of patient characteristics with delivery of ophthalmic telemedicine during the COVID-19 pandemic. JAMA Ophthalmol. 2021;139(11):1174–1182. doi: 10.1001/JAMAOPHTHALMOL.2021.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Dorn A, RE Cooney, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet North Am. Ed. 2020;395(10232):1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am. J. Manag. Care. 2021;27(1):21–26. doi: 10.37765/AJMC.2021.88573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.2019 Broadband deployment report | federal communications commission. Accessed December 20, 2021. https://www.fcc.gov/reports-research/reports/broadband-progress-reports/2019-broadband-deployment-report.