Abstract
Background/Purpose:
Surgical indications and techniques have changed over the last fifteen years. The number of Pediatric Surgery training programs has also increased. We sought to examine the effect of these changes on resident education by examining case log data.
Methods:
Accreditation Council for Graduate Medical Education (ACGME) case logs for graduating Pediatric Surgery residents were examined from 2004-2018. Using the summary statistics provided, linear regression analysis was conducted on each case log code and category.
Results:
In 2004, there were 24 Pediatric Surgery training programs and 24 Pediatric Surgery residents graduating with an average of 979.8 total cases logged. In 2018, there were 36 programs with 38 residents graduating with an average of 1260.2 total cases logged. Total case volume of graduating residents significantly increased over the last 15 years (p<0.001). Significant increases were demonstrated in skin/soft tissue/musculoskeletal (p<0.01), abdominal (p<0.001), hernia repair (p<0.001), genitourinary (p<0.01), and endoscopy (p<0.001). No significant changes were seen in the head and neck, thoracic, cardiovascular, liver/biliary, and non-operative trauma categories. No categories significantly decreased over the time period. No significant changes were seen in the number of multiple index congenital cases, including tracheoesophageal fistula/esophageal atresia repair, omphalocele, gastroschisis, choledochal cyst excision, perineal procedure for imperforate anus, and major hepatic resections for tumors. Pertinent increases in specific procedures include diaphragmatic hernia repair (p<0.01), ECMO cannulation/decannulation(p<0.05), thyroidectomy (p<0.001), parathyroidectomy (p<0.001), biliary atresia (p<0.001), and circumcision (p<0.001) as well as most laparoscopic abdominal procedures. Specific procedure codes with significant decreases include tracheostomy (p<0.05), minimally invasive decortication/pleurectomy/blebectomy (p<0.001), laparoscopic splenectomy (p<0.001), as well as most open abdominal procedures.
Conclusion:
Despite increasing numbers of Pediatric Surgery residents and training programs, the number of cases performed by each graduating resident has increased. This increase is primarily fueled by increase in abdominal, skin/soft tissue/musculoskeletal, hernia repair, genitourinary, and endoscopic cases.
Keywords: Surgical Education, Pediatric Surgery Residency, Accreditation Council for Graduate Medical Education
Introduction
Surgical education and training have undergone notable changes in the last 15-20 years. Surgical education has long followed the Halstedian model of experiential training. However, there has been a recent shift towards milestone and competency-based learning.1 For surgical trainees, case logs have been used as a surrogate for operative skill, a key component of resident training.2,3 Work hour restrictions, changes in surgical techniques and indications, and an increase in both the number of Pediatric Surgery training programs and Pediatric Surgery residents have driven these changes. Previous studies have demonstrated a decline in the operative experience of General Surgery residents in Pediatric Surgery cases, as well as a general narrowing of the experience of many General Surgery residents.4-6 However, the only changes reported for Pediatric Surgery residents has been a general stabilization of case volume.7
In this study, we sought to use operative case logs to examine the effects of increasing number of the trainees as well as changing surgical indications and techniques on Pediatric Surgery resident education over the last 15 years.
Methods
Study Design and Data Source
This was a retrospective cross-sectional study of publicly available, aggregated case log summary reports from the Accreditation Council for Graduate Medical Education (ACGME). Each resident’s case log represents the entire sum total of all cases performed during their Pediatric Surgery residency. At time of analysis, case logs were available from academic year 2003-4 until academic year 2017-8, representing fifteen years of data collection. For simplicity throughout the manuscript, we will refer to the year of graduation as the year of each case log. We used all available case logs from 2004-2018. The total number of cases logged as surgeon were used in analysis. We eliminated any cases logged as teaching assistant or logs that aggregated teaching assistant and surgeon data. Very few teaching assistant cases were logged over the study period and their inclusion would increase the number of confounders without substantive benefit to the analysis.
In 2009, significant changes were made to the case log. A large proportion of case log codes were split into open and laparoscopic procedures. For these cases, we utilized the more recent definition and only analyzed cases logged from 2009-2018.
Statistical Analysis
Using the mean and standard deviation (SD) summary statistics provided by the ACGME case logs, linear regression analysis was utilized. The average number of cases per resident per year was graphed, and average operative volume was assessed using simple linear regression. This allowed us to discern whether there was a significant trend, and the direction of this trend. All statistical analyses were performed using GraphPad Prism 7.0 (La Jolla, CA).
Results
Total Cohort Characteristics
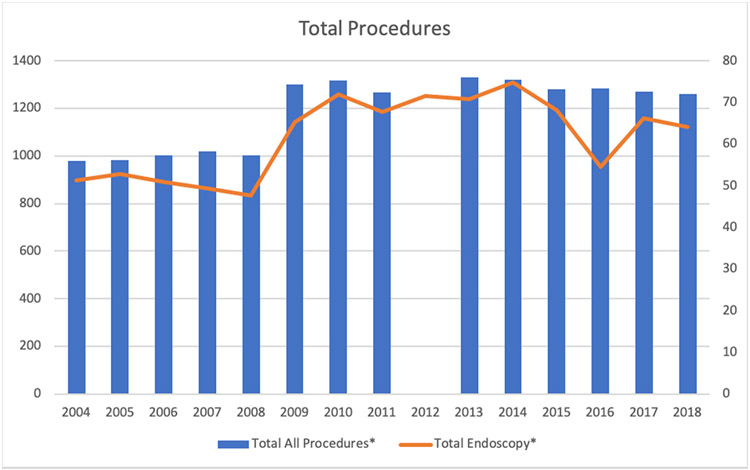
The number of Pediatric Surgery residents increased from 24 in 2004 to 38 in 2018. In 2017 at 45 residents graduated from Pediatric Surgery residency, the highest number in the study period. The number of Pediatric Surgery training programs increased from 24 in 2004 to 36 in 2018. The total number of procedures performed by graduating Pediatric Surgery residents significantly increased over the study period from 979.8 ± 208 in 2004 to 1260.2 ± 261 in 2018 (p<0.001, Figure 1). Total endoscopic cases also significantly increased over the study period from 51.2 ± 25 in 2004 to 64.0 ± 30 in 2018 (p<0.001, Figure 1). A summary of yearly means and SD for all graphically represented results is included in Appendix A.
Figure 1:
Summary Statistics. Total surgical and endoscopic cases for all graduating Pediatric Surgery residents from 2004-2018. Surgical cases are plotted along the left axis and endoscopic cases are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
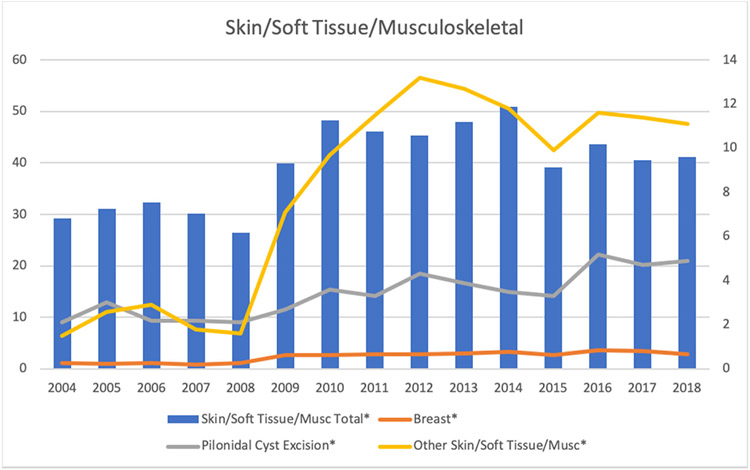
Skin/Soft Tissue/Musculoskeletal
The number of skin/soft tissue/musculoskeletal procedures significantly increased over the study period from 29.2 ± 30 in 2004 to 41.1 ± 30 in 2018 (p<0.01, Figure 2). Significant increases were seen in breast (1.2 ± 1 vs. 2.9 ± 3, p<0.001, Figure 2), pilonidal cyst excision (2.1 ± 2 vs. 4.9 ± 5, p<0.001, Figure 2), and other (1.5 ± 5 vs. 11.1 ± 8, p<0.001, Figure 2) procedures.
Figure 2:
Select Skin/Soft Tissue/Musculoskeletal Procedures. Total skin/soft tissue/musculoskeletal, breast, pilonidal cyst excision, and other skin/soft tissue musculoskeletal cases for all graduating Pediatric Surgery residents from 2004-2018. Total category skin/soft tissue/musculoskeletal is plotted along the left axis and the procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
No significant decreases were seen in any procedure over the study period. No significant changes were seen in burn debridement (6.7 ± 19 vs. 7.7 ± 16, p>0.05), complex wound closure (3.3 ± 4 vs. 5.8 ± 14, p>0.05), major soft tissue repair for trauma (4.1 ± 4 vs. 4.1 ± 5, p>0.05) or major excision soft tissue tumor (8.2 ± 5 vs. 6.8 ± 6, p>0.05).
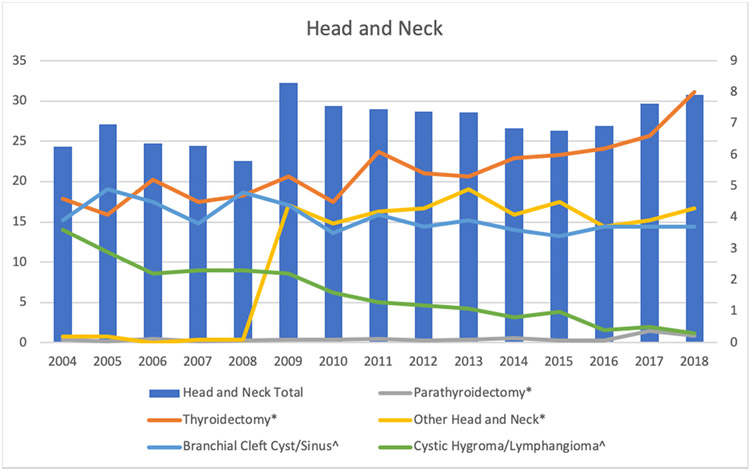
Head and Neck
The number of head and neck procedures did not significantly change over the study period from 24.3 ± 11 in 2004 to 30.8 ± 12 in 2018 (p>0.05, Figure 3). Significant increases were seen in thyroidectomy (4.3 ± 3 vs. 8.0 ± 8, p<0.001, Figure 3), parathyroidectomy (0.4 ± 1 vs. 0.9 ± 1, p<0.001, Figure 3), and other head and neck (0.2 ± 0 vs. 4.3 ± 4, p<0.001, Figure 3) procedures.
Figure 3.
Select Head and Neck Procedures. Total head and neck, thyroidectomy, parathyroidectomy, other head and neck, branchial cleft cyst/sinus, and cystic hygroma/lymphangioma cases for all graduating Pediatric Surgery residents from 2004-2018. Total category head and neck is plotted along the left axis and the procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
Significant decreases were seen in branchial cleft cyst/sinus (3.9 ± 2 vs. 3.7 ± 3, p<0.05, Figure 3) and cystic hygroma/lymphangioma (3.6 ± 2 vs. 0.3 ± 1, p<0.001, Figure 3) procedures. No significant changes were seen in thyroglossal duct cyst/sinus (3.2 ± 2 vs. 3.3 ± 3, p>0.05), dermoid/other cyst (6.2 ± 8 vs. 7.8 ± 8, p>0.05), or major tumor head and neck procedures (2.3 ± 2 vs. 2.5 ± 3, p>0.05).
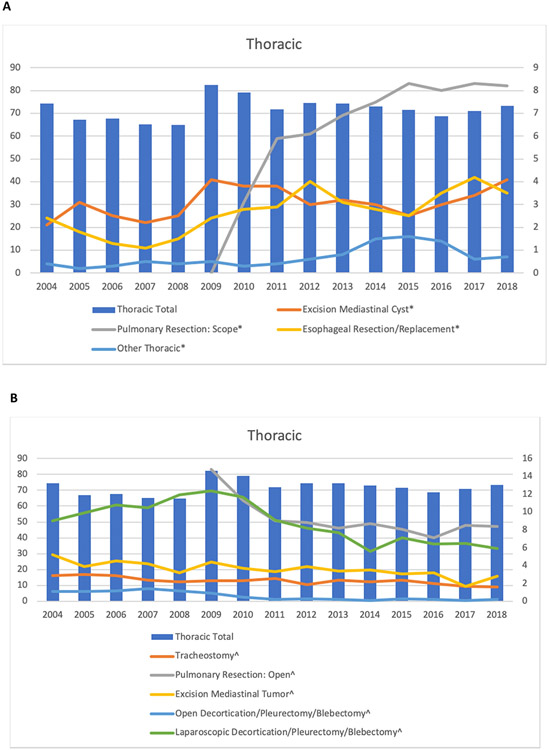
Thoracic
The number of thoracic procedures did not significantly change over the study period from 74.4 ± 27 in 2004 to 73.4 ± 26 in 2018 (p>0.05, Figures 4A and 4B). Significant increases were seen in excision mediastinal cyst (2.1 ± 2 vs. 4.1 ± 3, p<0.001, Figure 4A), pulmonary resection: scope (0 ± 0 vs. 8.2 ± 5 p<0.001, Figure 4A), esophageal resection/replacement (2.4 ± 2 vs. 3.5 ± 5, p<0.001, Figure 4A), and other thoracic (0.4 ± 1 vs. 0.7 ± 1, p<0.001, Figure 4A) procedures.
Figure 4:
Select Thoracic Procedures. (A) Total thoracic, excision mediastinal cyst, pulmonary resection: scope, esophageal resection/replacement, other thoracic and (B) Total thoracic, tracheostomy, pulmonary resection: open, excision mediastinal tumor, open decortication/pleurectomy/blebectomy, laparoscopic decortication/pleurectomy/blebectomy cases for all graduating Pediatric Surgery residents from 2004-2018. Total category thoracic is plotted along the left axis and the procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
Significant decreases were seen in tracheostomy (2.9 ± 3 vs. 1.6 ± 3, p<0.05, Figure 4B), pulmonary resection: open (14.8 ± 7 vs. 8.4 ± 7, p<0.001, Figure 4B), excision mediastinal tumor (5.2 ± 3 vs. 2.8 ±2, p<0.001, Figure 4B), and both open (1.1 ± 1 vs. 0.2 ± 0, p<0.001, Figure 4B) and scope (9 ± 7 vs. 5.9 ± 4, p<0.001, Figure 4B) decortication/pleurectomy/blebectomy procedures.
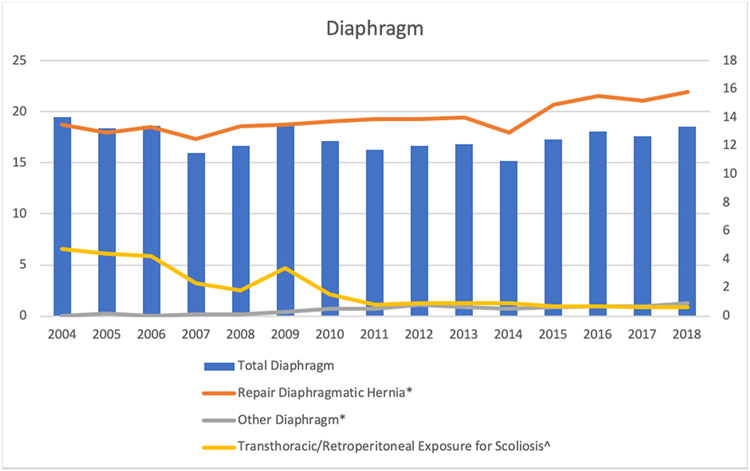
Diaphragm
The number of diaphragm procedures did not significantly change over the study period from 19.5 ± 8 in 2004 to 18.5 ± 9 in 2018 (p>0.05, Figure 5). Significant increases were seen in repair of congenital diaphragmatic hernia (CDH) (13.5 ± 6 vs. 15.8 ± 9, p<0.01, Figure 5) and other diaphragm procedures (0 ± 0 vs. 0.9 ± 1, p<0.001, Figure 5).
Figure 5:
Select Diaphragm Procedures. Total diaphragm, repair diaphragmatic hernia, other diaphragm, transthoracic/retroperitoneal exposure for scoliosis cases for all graduating Pediatric Surgery residents from 2004-2018. Total category diaphragm is plotted along the left axis and the procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
Significant decreases were seen in transthoracic/retroperitoneal exposure for scoliosis (4.7 ± 6 vs. 0.6 ± 1, p<0.001, Figure 5) procedures. No significant changes were seen in plication of the diaphragm (1.3 ± 1 vs. 1.2 ± 1, p>0.05) procedures.
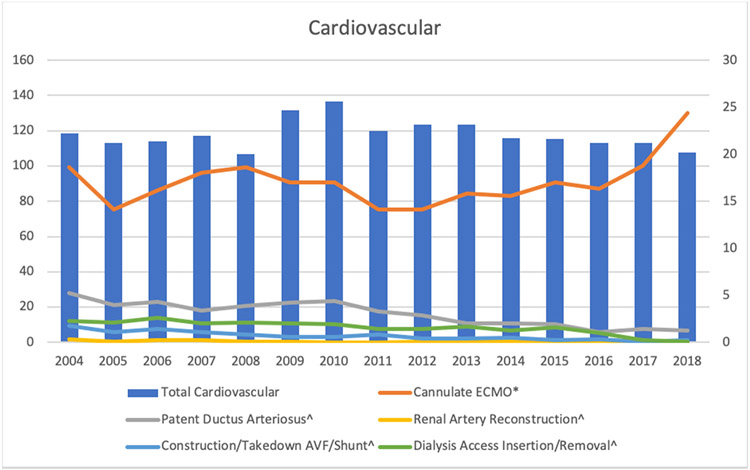
Cardiovascular
The number of cardiovascular procedures did not significantly change over the study period from 118.5 ± 54 in 2004 to 107.7 ± 58 in 2018 (p>0.05, Figure 6). The only significant increase was seen in extracorporeal membrane oxygenation (ECMO) cannulation (18.6 ± 10 vs. 24.4 ± 10, p<0.05, Figure 6).
Figure 6:
Select Cardiovascular Procedures. Total cardiovascular, cannulate ECMO, patent ductus arteriosus, renal artery reconstruction, construction or take down AVF/shunt, and dialysis access insertion/removal cases for all graduating Pediatric Surgery residents from 2004-2018. Total category cardiovascular is plotted along the left axis and the procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
Significant decreases were seen in patent ductus arteriosus (5.2 ± 9 vs. 1.3 ± 4, p<0.01, Figure 6), renal artery reconstruction (0.3 ± 1 vs. 0.1 ± 0, p<0.01, Figure 6), construction or take down of AV fistula/shunt (1.8 ± 3 vs. 0.2 ± 1, p<0.001, Figure 6) and dialysis access insertion/removal (2.3 ± 3 vs. 0.1 ± 0, p<0.001, Figure 6) procedures. No significant changes were seen in coarctation (0 ± 0 vs. 0 ± 0, p>0.05), vascular ring (0.3 ± 0 vs. 0.3 ± 1, p>0.05), any open heart (0 ± 0 vs. 0 ± 0, p>0.05), any closed heart (0 ± 0 vs. 0.1 ± 0, p.0.05), aortopexy (0.6 ± 1 vs. 0.8 ± 2, p>0.05), peripheral artery reconstruction (0.2 ± 1 vs. 0.2 ± 1, p>0.05), major vessel reconstruction (1.9 ± 3 vs. 1.5 ± 2, p<0.05), or surgical placement/removal of central access line (87.3 ± 52 vs. 78.2 ± 53, p.0.05) procedures.
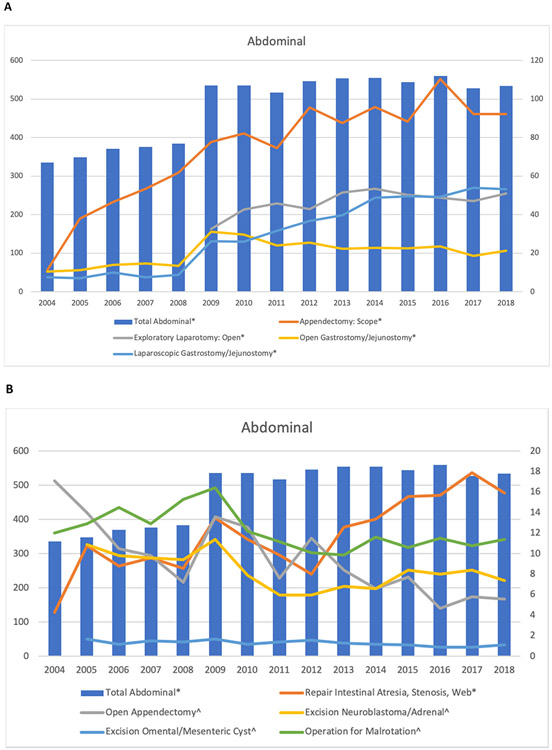
Abdominal
The number of abdominal cases significantly increased over the study period from 335.8 ± 101 in 2004 to 534.3 ± 149 in 2018 (p<0.001, Figures 7A and 7B). Significant increases included laparoscopic appendectomy (11.3 ± 8 vs. 92.3 ± 69, p<0.001, Figure 7A), exploratory laparotomy (32.5 ± 23 vs. 50.9 ± 31, p<0.001, Figure 7A), repair intestinal atresia, stenosis or web (4.3 ± 4 vs. 15.9 ± 7, p<0.001, Figure 7B), and open (10.5 ± 7 vs, 21.3 ± 14, p<0.001, Figure 7A) and laparoscopic (7.6 ± 12 vs. 53.3 ± 29, p<0.001, Figure 7A) gastrostomy/jejunostomy procedures. Other significant increases included laparoscopic pyloromyotomy(1.3 ± 8 vs. 25.1 ±10, p<0.001), laparoscopic intestinal resection (0.1 ± 0 vs. 2.9 ± 2, p<0.001), laparoscopic ostomy creation for anorectal malformation (0 ± 0 vs. 1.5 ± 2, p<0.001), laparoscopic ostomy creation for Hirschsprung’s (0 ± 0 vs. 1.7 ± 2, p<0.001), urachal remnant resection (2.5 ± 2 vs. 3.2 ± 3, p<0.05), excision sacrococcygeal teratoma (1.8 ± 1 vs. 2.7 ± 2, p<0.05), and diagnostic laparoscopy (2.1 ± 1 vs. 28.6 ± 29, p<0.001) procedures.
Figure 7:
Select Abdominal Procedures. (A) Total abdominal, appendectomy: scope, exploratory laparotomy: open, open gastrostomy/jejunostomy, laparoscopic gastrostomy/jejunostomy and (B) Total abdominal, repair intestinal atresia, stenosis, web, open appendectomy, excision neuroblastoma/adrenal, excision of omenal/mesenteric cyst, and operation for malrotation cases for all graduating Pediatric Surgery residents from 2004-2018. Total category abdominal is plotted along the left axis and the procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
Significant decreases were seen in open appendectomies (17.1 ± 8 vs. 5.6 ± 6, p<0.001, Figure 7B), excision of neuroblastoma/adrenal (10.9 ± 6 vs. 7.4 ± 4, p<0.001, Figure 7B), excision of omental/mesenteric cyst (1.7 ± 2 vs. 1.1 ± 1, p<0.01, Figure 7B), and operation for malrotation (12 ± 7 vs. 11.4 ± 5, p<0.001, Figure 7B) procedures. Other significant decreases included open antireflux procedures (25.4 ± 23 vs. 4.8 ± 5, p<0.001), open pyloromyotomy (35.2 ± 19 vs. 4.6 ± 6, p<0.001), open intestinal resection (39.8 ± 15 vs. 29.3 ± 10, p<0.01), open ostomy for anorectal malformation (6.2 ± 4 vs. 3.8 ± 3, p<0.001), open ostomy for Hirschsprung’s (6.9 ± 5 vs. 1.4 ± 1, p<0.001), open pullthrough for Hirschsprung’s (7.3 ± 4 vs. 5.3 ± 4, p<0.05), laparoscopic pullthrough for inflammatory bowel disease or polyposis (0.9 ± 1 vs. 0.8 ± 1, p<0.001), and open pullthrough for inflammatory bowel disease or polyposis (2.3 ± 2 vs. 0.7 ± 1, p<0.001) procedures.
No significant changes were seen in laparoscopic antireflux procedures (23.5 ± 20 vs. 23.3 ± 16, p>0.05), laparoscopic pyloroplasty/gastric resection (1.1 ± 6 vs. 1 ± 2, p>0.05), duodenal atresia (4.1 ± 3 vs. 5.5 ± 4, p>0.05), perineal procedure for imperforate anus (13.4 ± 8 vs. 14.6 ± 7, p>0.05), laparoscopic pullthrough for Hirschsprung’s (2.8 ± 2 vs. 3.8 ± 3, p>0.05), exploratory laparoscopy (3 ± 7 vs. 4.3 ± 5 , p>0.05), omphalocele (5 ± 3 vs. 5 ± 2, p>0.05), and gastroschisis procedures (14.2 ± 12 vs. 11.3 ± 8, p>0.05) procedures.
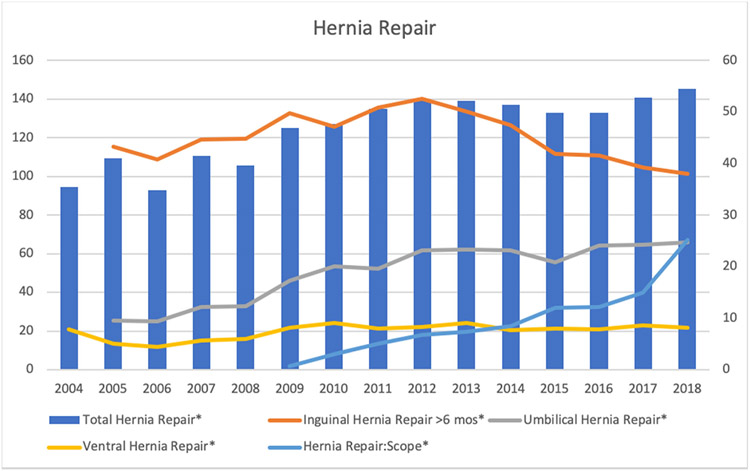
Hernia Repair
The number of hernia repair cases significantly increased over the study period from 94.7 ± 39 in 2004 to 145.1 ± 55 in 2018 (Figure 8). Significant increases were seen in pediatric repair of inguinal hernia at greater than 6 months of age (43.2 ± 27 vs. 38.0 ± 18, p<0.001, Figure 8), repair of umbilical hernias (9.6 ± 8 vs. 24.7 ± 18, p<0.001, Figure 8), ventral hernia repair (5.1 ± 4 vs. 8.1 ± 6, p<0.001, Figure 8), and laparoscopic hernia repair (0.7 ± 3 vs. 25.2 ± 28, p<0.001, Figure 8) procedures.
Figure 8:
Select Hernia Repair Procedures. Total hernia repair, inguinal hernia repair greater than 6 months of age, umbilical hernia repair, ventral hernia repair, and hernia repair: scope cases for all graduating Pediatric Surgery residents from 2004-2018. Total category hernia repair is plotted along the left axis and procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
No significant decreases were seen in any hernia repair procedure over the study period. No significant changes were seen in infant repair of inguinal hernias at younger than 6 months of age (51 ± 26 vs. 46.2 ± 17, p>0.05), repair of femoral hernia (0.1 ± 0 vs. 0.2 ± 0, p>0.05), and other hernia repair (3.6 ± 3 vs. 2.8 ± 3, p>0.05) procedures.
Liver Biliary
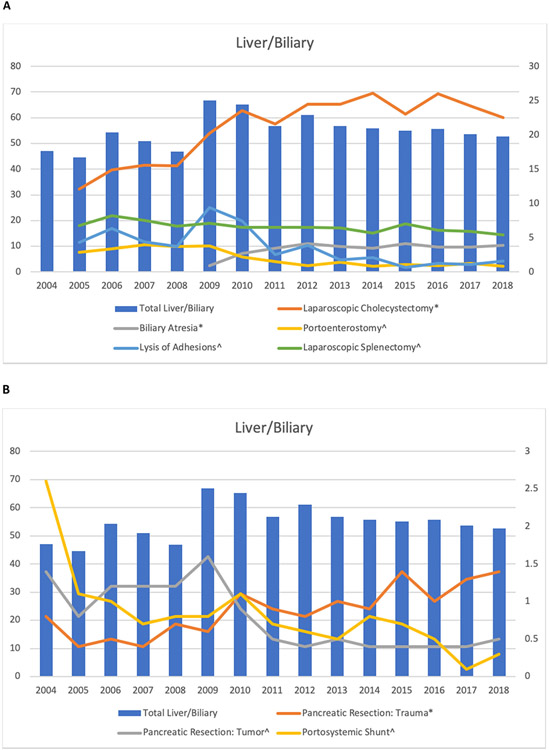
The number of liver biliary procedures did not significantly change from 47.1 ± 21 in 2004 to 52.6 ± 17 in 2018 (Figures 9A and 9B). Significant increases were seen in laparoscopic cholecystectomy (12.7 ± 7 vs. 22.5 ± 13, p<0.001, Figure 9A), exploration for biliary atresia (0.9 ± 2 vs. 3.9 ± 2, p<0.001, Figure 9A) and pancreatic resection for trauma (0.8 ± 3 vs. 1.4 ± 1, p<0.001, Figure 9B) procedures.
Figure 9:
Select Liver/Biliary Procedures. (A) Total liver/biliary, laparoscopic cholecystectomy, biliary atresia, portoenterostomy, laparoscopic splenectomy and (B) Total liver/biliary, pancreatic resection for trauma, pancreatic resection for tumor, lysis of adhesions, and portosystemic shunt cases for all graduating Pediatric Surgery residents from 2004-2018. Total category liver/biliary is plotted along the left axis and procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
Significant decreases were seen in portoenterostomy (2.9 ± 2 vs. 0.8 ± 1, p,0.001, Figure 9A), pancreatic resection for tumor (1.4 ± 5 vs. 0.5 ± 1, p<0.001, Figure 9B), lysis of adhesions (4.3 ± 4 vs. 1.6 ± 2, p<0.001, Figure 9A), portosystemic shunts (2.6 ± 3 vs. 0.3 ± 1, p<0.01, Figure 9B), and laparoscopic splenectomy (6.8 ± 4 vs. 5.4 ± 3, p<0.001, Figure 9A) procedures. No significant changes were noted in major hepatic resections for tumor (2.5 ± 2 vs. 3.1 ± 3, p>0.05) and trauma (0.6 ± 1 vs. 0.7 ± 1, p>0.05), liver transplantation (1.1 ± 3 vs. 0.7 ± 2, p>0.05), open cholecystectomy (1.4 ± 2 vs. 1.8 ± 2, p>0.05), choledochal cyst excision (3.7 ± 3 vs. 3.6 ± 3, p>0.05), and open splenectomy (2 ± 2 vs. 1.7 ± 2, p>0.05) procedures.
Genitourinary
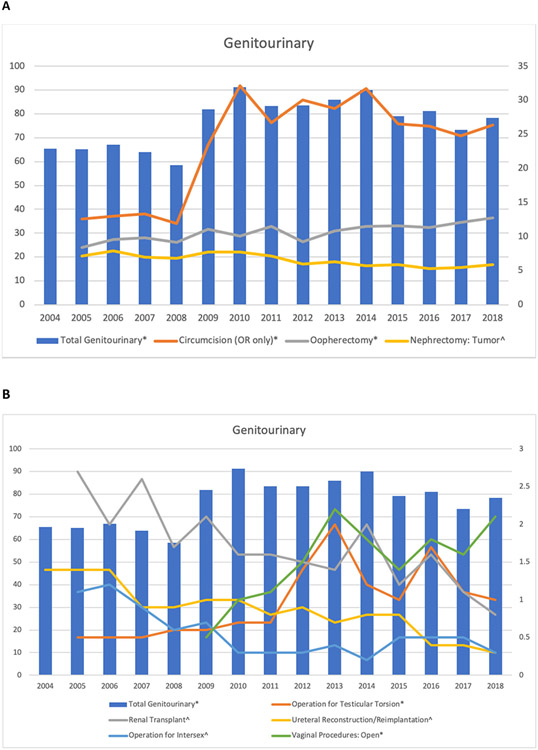
The number of genitourinary procedures significantly increased from 65.5 ± 32 in 2004 to 78.3 ± 32 in 2018 (Figures 10A and 10B). Significant increases were seen in circumcisions (12.6 ± 13 vs. 26.4 ± 18, p<0.001, Figure 10A), open vaginal procedures (0.5 ± 1 vs. 2.1 ± 2, p<0.001, Figure 10B), oophorectomy (8.4 ± 4 vs. 12.7 ± 7, p<0.001, Figure 10A), and operation for testicular torsion (0.5 ± 1 vs. 1 ± 2, p<0.05, Figure 10B) procedures.
Figure 10:
Select Genitourinary Procedures. (A) Total genitourinary, circumcision (operating room only), oophorectomy, nephrectomy: tumor and (B) Total genitourinary, operation for testicular torsion, renal transplant, ureteral reconstruction/reimplantation, open vaginal procedures, and operation for intersex cases for all graduating Pediatric Surgery residents from 2004-2018. Total category genitourinary is plotted along the left axis and procedures are plotted along the right axis. Significance denoted as follows: *: significantly increased; ^: significantly decreased.
Significant decreases included renal transplantation (2.7 ± 5 vs. 0.8 ± 2, p<0.001, Figure 10B), nephrectomy for tumor (7.1 ± 4 vs. 5.9 ± 4, p<0.001, Figure 10A), ureteral reconstruction/reimplantation (1.4 ± 2 vs. 0.3 ± 1, p<0.001, Figure 10B), and operation for intersex (1 ± 1 vs. 0.3 ± 1, p<0.001, Figure 10B) procedures. No significant changes were seen in nephrectomy for trauma (0.1 ± 0 vs. 0.1 ± 0, p>0.05), cystectomy (0.2 ± 1 vs. 0.2 ± 0, p>0.05), enteric conduit (0.3 ± 1 vs. 0.3 ± 1, p.0.05), bladder augmentation (0.5 ± 1 vs. 0.1 ± 0, p>0.05), orchidopexy (16.4 ± 8 vs. 14.5 ± 9, p>0.05), orchiectomy (1.1 ± 2 vs. 1.2 ± 1, p>0.05), laparoscopic variococele (0.5 ± 1 vs. 0.1 ± 0, p>0.05), and hysterectomy/salpingectomy (0.7 ± 1 vs. 0.6 ± 1, p>0.05) procedures.
Discussion
Our results demonstrated that the overall case volume of graduating Pediatric Surgery residents significantly increased over the last 15 years. Significant increases were seen in the skin/soft tissue/musculoskeletal, abdominal, hernia repair, genitourinary, and endoscopy categories. No significant changes were seen in the head and neck, thoracic, cardiovascular and liver biliary categories. No categories significantly decreased over the study period. In addition, several procedure-level trends were noted including an increase in laparoscopic cases with a corresponding decrease in open cases as well as no significant change in the number of multiple congenital index cases, such as tracheoesophageal fistula/esophageal atresia, omphalocele, gastroschisis, choledochal cyst excision, perineal procedure for imperforate anus, and major hepatic resections for tumor.
Changing surgical indications and techniques have significantly impacted Pediatric Surgery resident education. For example, the number of cystic hygroma/lymphangioma cases has significantly decreased over the study period. While the preferred modality for treating cystic hygroma remains complete surgical excision, an increasing number of remarkable results have been achieved with sclerosing agents.8 Intralesional bleomycin has shown to be remarkably effective 9-12, and the development of OK-432 has also shown to be helpful in the management of these lesions.13-15 Similarly, we demonstrated significant decreases in both open and minimally invasive decortication/pleurectomy/blebectomy procedures which represents changing practices in managing those disease processes.
We also demonstrated an increase in ECMO cannulation as well as CDH repair procedures, which is also likely secondary to a change in surgical indications. The current trend is towards early initiation of ECMO with early repair of CDH.16 Retrospective analysis in some centers have demonstrated an increase in survival rates in CDH with ECMO utilization17 and improvement in ECMO technology have lead to lower complication rates.18 While the traditional approach advocates for surgical repair of CDH after successful weaning from ECMO, careful anticoagulation techniques have reduced complications from bleeding for surgical repair while on ECMO.19 Additionally, there is a theoretical benefit to surgical repair on ECMO support via restoration of the normal anatomy.20,21
Advanced laparoscopic surgery has become the mainstay of modern surgical practices, and this change is reflected in Pediatric Surgery resident education. We demonstrated a significant increase in most laparoscopic abdominal procedures including laparoscopic appendectomy and laparoscopic cholecystectomy as well as increases in thoracoscopic pulmonary resections and laparoscopic hernia repair. Laparoscopic surgery in adults has been increasing since 1994,22 and by 2000, 82% of United States Pediatric Surgeons were performing laparoscopic surgery.23 However, there are concerns that despite the advantages of current technology, there will always be a role for open surgical intervention.24 As surgical techniques continue to evolve, attention may need to be paid towards the number of open surgical cases that trainees need in order to maintain competence in open surgical techniques. However, trainee’s education should accurately reflect the current practice guidelines that they will be employing in practice. Training programs must strike a careful balance between ensuring a well-rounded, but also representative education.
Pediatric Surgery resident education has been impacted by changes in surgical education structuring as well. Our results demonstrated a significant decrease in most cardiovascular cases, including patent ductus arteriosus repair, over the study period. In 2007, congenital cardiac surgery became a recognized fellowship by the ACGME with board certification provided through the American Board of Thoracic Surgery. The number of trainees since that time has exponentially increased from 2 in 2008 to 44 in 2014.25 As this field and other surgical subspecialties continue to grow, it is expected that the scope of training for most Pediatric Surgery trainees will continue to be narrowed. Similar changes have already been observed in General Surgery training.5 To ensure broad-based training, additional resources may be necessary including off-service rotations and experiences like those employed in General Surgery training programs.
As the number of pediatric cases performed by General Surgery residents continues to decline,4 there has been less integration of adult surgeons into pediatric surgical care models. The distribution of pediatric surgeons tends towards more populous states and major urban centers.26 Multiple studies have linked superior patient outcomes to procedural volume in acute care surgeries, not specialty.27-29 Despite this evidence, there has been an increase in centralization of medical services driven by concerns for the adequate care of children both surgically and in the perioperative setting.29 Our data demonstrated a significant increase in several acute care procedures over the past 15 years, particularly laparoscopic appendectomies and cholecystectomies. As we move towards competency-based education practices, the utility of performing additional non-index cases will have to be carefully weight against the benefits of other educational opportunities.
Our study has several limitations. Case log data has not been shown to be completely accurate. An audit of general surgery program case logs reveals that there is up to a 25% discordance between cases audited and cases logged, particularly by lower-level residents.30 Of particular concern is dual logging of procedures by several residents, which may inflate both their role in the case and the number of these cases truly being performed at individual institutions. Studies have also demonstrated that increased case volume does not correlate with overall competence in practice.31-33 Additionally, some cases may not be captured accurately by examining the case logs. The increase in skin/soft tissue/musculoskeletal cases was primarily driven by procedures being logged as other. Similarly, a significant increase was seen in other head and neck cases. It is unclear whether there is the same educational value in cases logged as other as there is in other procedures in the category. A new code, biliary atresia, first appeared in the case logs in 2009 in order to provide a way to log exploration for biliary atresia. At the same time, we saw a decrease in the number of portoenterostomies being logged. This highlights another uncertainty in case log data. While these data may be accurate, it is also possible that prior to 2009, residents were logging exploration for biliary atresia as portoenterostomy cases, inflating the numbers.
Conclusion
Despite increasing numbers of Pediatric Surgery residents and training programs, the number of cases performed by each resident has increased. This is fueled by an increase in abdominal, skin/soft tissue/musculoskeletal, hernia repair, genitourinary, and endoscopic cases. These case log data indicates that training volume is adequate to support the current number of Pediatric Surgery residents with no evidence of underexposure to index cases. However, Pediatric Surgery resident education has been significantly impacted by both changes in surgical indications and techniques as well as the changing educational landscape for other surgical specialties.
Funding
CBC is supported by a grand from the National Institute of General Medical Sciences of the National Institutes of Health under Award Number T32GM008256. KBJ is supported by a research career development award (K12HD052023: Building Interdisciplinary Research Careers in Women’s Health Program – BIRCWH; Berenson, PI) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) at the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations
- ACGME
Accreditation Council for Graduate Medical Education
- CDH
Congenital Diaphragmatic Hernia
- ECMO
Extracorporeal Membrane Oxygenation
- SD
Standard Deviation
APPENDIX A
| Procedure | Case Volume by Graduating Year (Mean ± SD) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
| Total All Cases* | 979.8 ± 208 | 983 ± 255 | 1003 ± 256 | 1020.7 ± 231 | 1002.3 ± 189 | 1299.8 ± 205 | 1316.9 ± 295 | 1266.1 ± 254 | N/A | 1329.3 ± 279 | 1320.6 ± 239 | 1281 ± 252 | 1282.4 ± 376 | 1269 ± 278 | 1260.2 ± 261 |
| Total All Endoscopy* | 51.2 ± 25 | 52.9 ± 28 | 50.8 ± 26 | 49.3 ± 24 | 47.6 ± 22 | 65.2 ± 35 | 71.9 ± 30 | 67.7 ± 32 | 71.6 ± 43 | 70.7 ± 34 | 74.7 ± 39 | 68.1 ± 27 | 54.5 ± 26 | 66.2 ± 28 | 64 ± 30 |
| Total Skin/Soft Tissue/Musc* | 29.2 ± 30 | 31.1 ± 22 | 32.4 ± 31 | 30.2 ± 28 | 26.4 ± 19 | 39.9 ± 27 | 48.3 ± 35 | 46.1 ± 28 | 45.3 ± 23 | 48 ± 23 | 50.9 ± 49 | 39.2 ± 26 | 43.6 ± 34 | 40.6 ± 29 | 41.1 ± 30 |
| Breast* | 1.2 ± 1 | 1 ± 1 | 1.1 ± 2 | 0.8 ± 1 | 1.1 ± 2 | 2.7 ± 3 | 2.7 ± 2 | 2.9 ± 2 | 2.9 ± 2 | 3 ± 2 | 3.4 ± 3 | 2.7 ± 3 | 3.7 ± 6 | 3.5 ± 4 | 2.9 ± 3 |
| Pilonidal Cyst Excision* | 2.1 ± 2 | 3 ± 3 | 2.2 ± 3 | 2.2 ± 3 | 2.1 ± 2 | 2.7 ± 3 | 3.6 ± 4 | 3.3 ± 3 | 4.3 ± 3 | 3.9 ± 4 | 3.5 ± 4 | 3.3 ± 3 | 5.2 ± 7 | 4.7 ± 5 | 4.9 ± 5 |
| Other Skin/Soft Tissue/Musc* | 1.5 ± 5 | 2.6 ± 4 | 2.9 ± 4 | 1.8 ± 4 | 1.6 ± 3 | 7.1 ± 5 | 9.7 ± 7 | 11.5 ± 7 | 13.2 ± 9 | 12.7 ± 7 | 11.8 ± 8 | 9.9 ± 7 | 11.6 ± 7 | 11.4 ± 8 | 11.1 ± 8 |
| Total Head and Neck | 24.3 ± 11 | 27.1 ± 13 | 24.7 ± 11 | 24.4 ± 12 | 22.6 ± 9 | 32.3 ± 13 | 29.4 ± 12 | 29 ± 14 | 28.7 ± 14 | 28.6 ± 12 | 26.6 ± 11 | 26.3 ± 11 | 26.9 ± 11 | 29.7 ± 14 | 30.8 ± 12 |
| Thyroidectomy* | 4.6 ± 3 | 4.1 ± 3 | 5.2 ± 4 | 4.5 ± 4 | 4.7 ± 5 | 5.3 ± 4 | 4.5 ± 4 | 6.1 ± 5 | 5.4 ± 5 | 5.3 ± 6 | 5.9 ± 7 | 6 ± 6 | 6.2 ± 6 | 6.6 ± 7 | 8 ± 8 |
| Parathyroidectomy* | 0.4 ± 1 | 0.2 ± 1 | 0.5 ± 1 | 0.2 ± 0 | 0.3 ± 1 | 0.4 ± 1 | 0.4 ± 1 | 0.5 ± 1 | 0.3 ± 1 | 0.4 ± 1 | 0.6 ± 1 | 0.3 ± 1 | 0.3 ± 1 | 1.5 ± 1 | 0.9 ± 1 |
| Other Head and Neck | 0.2 ± 0 | 0.2 ± 1 | 0 ± 0 | 0.1 ± 1 | 0.1 ± 0 | 4.4 ± 4 | 3.8 ± 3 | 4.2 ± 3 | 4.3 ± 4 | 4.9 ± 3 | 4.1 ± 3 | 4.5 ± 4 | 3.7 ± 3 | 3.9 ± 3 | 4.3 ± 4 |
| Branchial Cleft Cyst/Sinus^ | 3.9 ± 2 | 4.9 ± 4 | 4.5 ± 3 | 3.8 ± 3 | 4.8 ± 2 | 4.4 ± 2 | 3.5 ± 2 | 4.1 ± 3 | 3.7 ± 2 | 3.9 ± 2 | 3.6 ± 2 | 3.4 ± 3 | 3.7 ± 3 | 3.7 ± 2 | 3.7 ± 3 |
| Cystic Hygroma/Lymphangioma^ | 3.6 ± 2 | 2.9 ± 2 | 2.2 ± 2 | 2.3 ± 2 | 2.3 ± 3 | 2.2 ± 2 | 1.6 ± 2 | 1.3 ± 1 | 1.2 ± 2 | 1.1 ± 1 | 0.8 ± 1 | 1 ± 1 | 0.4 ± 1 | 0.5 ± 1 | 0.3 ± 1 |
| Total Thoracic | 74.4 ± 27 | 67.1 ± 24 | 67.7 ± 22 | 65.2 ± 19 | 64.8 ± 17 | 82.3 ± 24 | 79.2 ± 26 | 71.8 ± 21 | 74.5 ± 31 | 74.4 ± 24 | 73.1 ± 24 | 71.6 ± 24 | 68.8 ± 26 | 70.9 ± 26 | 73.4 ± 26 |
| Excision Mediastinal Cyst* | 2.1 ± 2 | 3.1 ± 2 | 2.5 ± 2 | 2.2 ± 2 | 2.5 ± 2 | 4.1 ± 3 | 3.8 ± 3 | 3.8 ± 3 | 3 ± 3 | 3.2 ± 3 | 3 ± 2 | 2.5 ± 2 | 3 ± 2 | 3.4 ± 3 | 4.1 ± 3 |
| Pulmonary Resection: Scope* | N/A | N/A | N/A | N/A | N/A | 0 ± 0 | 3.1 ± 2 | 5.9 ± 6 | 6.1 ± 4 | 6.9 ± 5 | 7.5 ± 4 | 8.3 ± 5 | 8 ± 7 | 8.3 ± 6 | 8.2 ± 5 |
| Esophageal Resection/Replacement* | 2.4 ± 2 | 1.8 ± 1 | 1.3 ± 1 | 1.1 ± 1 | 1.5 ± 2 | 2.4 ± 2 | 2.8 ± 2 | 2.9 ± 2 | 4 ± 8 | 3.1 ± 6 | 2.8 ± 2 | 2.5 ± 2 | 3.5 ± 4 | 4.2 ± 4 | 3.5 ± 5 |
| Other Thoracic* | 0.4 ± 1 | 0.2 ± 1 | 0.3 ± 1 | 0.5 ± 1 | 0.4 ± 1 | 0.5 ± 1 | 0.3 ± 1 | 0.4 ± 1 | 0.6 ± 1 | 0.8 ± 1 | 1.5 ± 3 | 1.6 ± 3 | 1.4 ± 2 | 0.6 ± 1 | 0.7 ± 1 |
| Tracheostomy^ | 2.9 ± 3 | 3 ± 4 | 2.9 ± 4 | 2.4 ± 3 | 2.2 ± 3 | 2.3 ± 4 | 2.3 ± 4 | 2.6 ± 4 | 1.9 ± 3 | 2.4 ± 3 | 2.2 ± 3 | 2.4 ± 4 | 2 ± 3 | 1.7 ± 3 | 1.6 ± 3 |
| Pulmonary Resection: Open^ | N/A | N/A | N/A | N/A | N/A | 14.8 ± 7 | 11.3 ± 8 | 9 ± 7 | 8.8 ± 8 | 8.2 ± 8 | 8.7 ± 7 | 8.1 ± 9 | 7.1 ± 6 | 8.5 ± 8 | 8.4 ± 7 |
| Excision Mediastinal Tumor^ | 5.2 ± 3 | 3.9 ± 3 | 4.5 ± 4 | 4.2 ± 3 | 3.2 ± 2 | 4.4 ± 3 | 3.7 ± 3 | 3.3 ± 3 | 3.9 ± 3 | 3.4 ± 3 | 3.5 ± 3 | 3.1 ± 3 | 3.2 ± 4 | 1.7 ± 2 | 2.8 ± 2 |
| Open Decortication/Pleurectomy/Blebectomy^ | 1.1 ± 1 | 1.1 ± 1 | 1.2 ± 2 | 1.4 ± 2 | 1.2 ± 2 | 0.9 ± 1 | 0.5 ± 1 | 0.2 ± 1 | 0.3 ± 1 | 0.2 ± 1 | 0.1 ± 0 | 0.3 ± 1 | 0.2 ± 0 | 0.1 ± 0 | 0.2 ± 0 |
| Laparoscopic Decortication/Pleurectomy/Blebectomy^ | 9 ± 7 | 9.9 ± 7 | 10.8 ± 6 | 10.5 ± 6 | 11.9 ± 6 | 12.4 ± 7 | 11,7 ± 8 | 9.1 ± 5 | 8.2 ± 5 | 7.7 ± 4 | 5.6 ± 4 | 7.1 ± 1 | 6.4 ± 4 | 6.5 ± 4 | 5.9 ± 4 |
| Total Diaphragm | 19.5 ± 8 | 18.4 ± 8 | 18.6 ± 7 | 16 ± 6 | 16.7 ± 7 | 18.6 ± 9 | 17.1 ± 7 | 16.3 ± 6 | 16.7 ± 7 | 16.8 ± 8 | 15.2 ± 7 | 17.3 ± 8 | 18.1 ± 9 | 17.6 ± 8 | 18.5 ± 9 |
| Repair Diaphragmatic Hernia* | 13.5 ± 6 | 12.9 ± 4 | 13.3 ± 5 | 12.5 ± 5 | 13.4 ± 6 | 13.5 ± 6 | 13.7 ± 5 | 13.9 ± 5 | 13.9 ± 6 | 14 ± 7 | 12.9 ± 6 | 14.9 ± 7 | 15.5 ± 8 | 15.2 ± 8 | 15.8 ± 9 |
| Other Diaphragm* | 0 ± 0 | 0.2 ± 0 | 0 ± 0 | 0.1 ± 0 | 0.1 ± 0 | 0.3 ± 1 | 0.3 ± 1 | 0.5 ± 1 | 0.8 ± 1 | 0.6 ± 1 | 0.5 ± 1 | 0.6 ± 1 | 0.7 ± 1 | 0.7 ± 1 | 0.9 ± 1 |
| Transthoracic/Retroperitoneal Exposure for Scoliosis^ | 4.7 ± 6 | 4.4 ± 5 | 4.2 ± 5 | 2.3 ± 3 | 1.8 ± 3 | 3.4 ± 5 | 1.5 ± 2 | 0.8 ± 1 | 0.9 ± 2 | 0.9 ± 2 | 0.9 ± 2 | 0.7 ± 1 | 0.7 ± 2 | 0.6 ± 1 | 0.6 ± 1118 |
| Total Cardiovascular | 118.5 ± 54 | 113.2 ± 57 | 114.2 ± 58 | 117 ± 52 | 106.7 ± 53 | 131.7 ± 54 | 136.6 ± 64 | 120 ± 60 | 123.3 ± 57 | 123.4 ± 49 | 115.8 ± 47 | 115.5 ± 52 | 113.1 ± 54 | 113.2 ± 60 | 107.7 ± 58 |
| Cannulate ECMO* | 18.6 ± 10 | 14.1 ± 8 | 16.2 ± 9 | 18 ± 11 | 18.6 ± 9 | 17 ± 10 | 17 ± 9 | 14.1 ± 7 | 14.1 ± 8 | 15.8 ± 7 | 15.6 ± 8 | 17 ± 8 | 16.3 ± 9 | 18.8 ± 10 | 24.4 ± 10 |
| Patent Ductus Arteriosus^ | 5.2 ± 9 | 4 ± 7 | 4.3 ± 8 | 3.4 ± 7 | 3.9 ± 9 | 4.2 ± 7 | 4.4 ± 9 | 3.3 ± 7 | 2.9 ± 6 | 2 ± 5 | 2 ± 5 | 1.9 ± 5 | 1.1 ± 4 | 1.4 ± 4 | 1.3 ± 45 |
| Renal Artery Reconstruction^ | 0.3 ± 1 | 0.1 ± 0 | 0.2 ± 1 | 0.2 ± 0 | 0.1 ± 0 | 0.1 ± 0 | 0 ± 0 | 0 ± 0 | 0.1 ± 0 | 0.1 ± 0 | 0.1 ± 0 | 0.1 ± 0 | 0.1 ± 0 | 0 ± 0 | 0.1 ± 0 |
| Construction or Takedown AVF/Shunt^ | 1.8 ± 3 | 1.1 ± 2 | 1.4 ± 2 | 1.1 ± 2 | 0.8 ± 1 | 0.6 ± 1 | 0.6 ± 2 | 0.8 ± 2 | 0.4 ± 1 | 0.4 ± 1 | 0.5 ± 1 | 0.2 ± 1 | 0.3 ± 1 | 0.1 ± 0 | 0.2 ± 1 |
| Dialysis Access Insertion/Removal^ | 2.3 ± 3 | 2.1 ± 3 | 2.6 ± 3 | 2 ± 2 | 2.1 ± 3 | 2 ± 3 | 1.9 ± 3 | 1.4 ± 3 | 1.4 ± 4 | 1.7 ± 3 | 1.3 ± 2 | 1.6 ± 2 | 1 ± 2 | 0.2 ± 0 | 0.1 ± 0 |
| Total Abdominal* | 335.8 ± 101 | 348.5 ± 122 | 370.5 ± 131 | 376.3 ± 91 | 383.8 ± 79 | 535.3 ± 121 | 535.3 ± 158 | 516.6 ± 131 | 546.6 ± 148 | 553.9 ± 159 | 554.3 ± 114 | 544.2 ± 138 | 559.6 ± 224 | 527.3 ± 149 | 534.3 ± 149 |
| Appendectomy: Scope* | 11.3 ± 8 | 38.1 ± 25 | 46.6 ± 40 | 53.4 ± 34 | 61.9 ± 40 | 77.8 ± 41 | 82.2 ± 57 | 74.6 ± 47 | 95.6 ± 55 | 87.6 ± 46 | 95.8 ± 60 | 88.3 ± 47 | 110.4 ± 98 | 92.2 ± 56 | 92.3 ± 69 |
| Exploratory Laparotomy: Open* | N/A | N/A | N/A | N/A | N/A | 32.5 ± 23 | 42.7 ± 35 | 45.8 ± 30 | 42.9 ± 30 | 51.4 ± 41 | 53.5 ± 27 | 50.2 ± 24 | 48.7 ± 35 | 47.1 ± 22 | 50.9 ± 31 |
| Repair Intestinal Atresia, Stenosis, Web* | 4.3 ± 4 | 10.8 ± 6 | 8.8 ± 6 | 9.6 ± 6 | 8.6 ± 5 | 13.5 ± 7 | 11.4 ± 7 | 9.9 ± 5 | 8 ± 5 | 12.6 ± 8 | 13.4 ± 8 | 15.6 ± 10 | 15.7 ± 8 | 17.9 ± 11 | 15.9 ± 7 |
| Open Gastrostomy/Jejunostomy* | 10.5 ± 7 | 11.2 ± 12 | 14 ± 11 | 14.7 ± 10 | 13.4 ± 10 | 31.1 ± 15 | 29.6 ± 20 | 24.1 ± 18 | 25.4 ± 17 | 22.3 ± 17 | 22.9 ± 15 | 22.5 ± 15 | 23.4 ± 17 | 18.6 ± 12 | 21.3 ± 14 |
| Laparoscopic Gastrostomy/Jejunostomy* | 7.6 ± 12 | 7 ± 9 | 9.9 ± 19 | 7.6 ± 9 | 8.7 ± 9 | 26.2 ± 27 | 26 ± 21 | 31.5 ± 22 | 36.7 ± 25 | 39.6 ± 24 | 48.9 ± 30 | 49.4 ± 28 | 49.2 ± 28 | 54 ± 32 | 53.5 ± 29 |
| Open Appendectomy^ | 17.1 ± 8 | 14 ± 16 | 10.5 ± 9 | 9.8 ± 13 | 7.2 ± 7 | 13.6 ± 13 | 12.6 ± 13 | 7.6 ± 9 | 11.5 ± 12 | 8.4 ± 10 | 6.6 ± 8 | 7.7 ± 8 | 4.7 ± 5 | 5.8 ± 7 | 5.6 ± 6 |
| Excision Neuroblastoma/Adrenal^ | N/A | 10.9 ± 6 | 9.8 ± 5 | 9.6 ± 5 | 9.4 ± 4 | 11.4 ± 5 | 7.9 ± 5 | 6 ± 5 | 6 ± 4 | 6.8 ± 5 | 6.6 ± 3 | 8.4 ± 5 | 8 ± 4 | 8.4 ± 5 | 7.4 ± 4 |
| Excision of Omental/Mesenteric Cyst^ | N/A | 1.7 ± 2 | 1.2 ± 1 | 1.5 ± 2 | 1.4 ± 1 | 1.7 ± 2 | 1.2 ± 2 | 1.4 ± 1 | 1.6 ± 2 | 1.3 ± 2 | 1.2 ± 1 | 1.1 ± 1 | 0.9 ± 2 | 0.9 ± 1 | 1.1 ± 1 |
| Operation for Malrotation^ | 12 ± 7 | 12.9 ± 6 | 14.5 ± 6 | 12.9 ± 4 | 15.3 ± 7 | 16.4 ± 6 | 12.2 ± 6 | 11.2 ± 7 | 10.1 ± 6 | 9.9 ± 5 | 11.6 ± 5 | 10.6 ± 6 | 11.5 ± 8 | 10.8 ± 6 | 11.4 ± 5 |
| Total Hernia Repair* | 94.7 ± 39 | 109.2 ± 50 | 92.9 ± 43 | 110.4 ± 51 | 105.7 ± 46 | 125 ± 42 | 127.1 ± 50 | 134.8 ± 52 | 139.1 ± 60 | 139.1 ± 47 | 136.9 ± 43 | 132.7 ± 54 | 133 ± 60 | 140.5 ± 57 | 145.1 ± 55 |
| Inguinal Hernia Repair > 6 mo.* | N/A | 43.2 ± 27 | 40.7 ± 25 | 44.6 ± 26 | 44.8 ± 26 | 49.8 ± 24 | 47.1 ± 25 | 50.9 ± 25 | 52.6 ± 26 | 50.1 ± 23 | 47.4 ± 19 | 41.9 ± 19 | 41.5 ± 26 | 39.2 ± 21 | 38 ± 18 |
| Umbilical Hernia Repair* | N/A | 9.6 ± 8 | 9.4 ± 10 | 12.2 ± 10 | 12.3 ± 10 | 17.2 ± 11 | 20 ± 15 | 19.6 ± 15 | 23.2 ± 17 | 23.3 ± 13 | 23.1 ± 14 | 20.8 ± 16 | 24 ± 22 | 24.2 ± 20 | 24.7 ± 18 |
| Ventral Hernia Repair* | 7.9 ± 9 | 5.1 ± 4 | 4.5 ± 3 | 5.6 ± 5 | 5.9 ± 5 | 8.1 ± 6 | 9.1 ± 6 | 8 ± 6 | 8.3 ± 5 | 9 ± 6 | 7.7 ± 5 | 8 ± 5 | 7.9 ± 7 | 8.6 ± 6 | 8.1 ± 6 |
| Hernia Repair: Scope* | N/A | N/A | N/A | N/A | N/A | 0.7 ± 3 | 3.1 ± 6 | 5.1 ± 10 | 6.8 ± 13 | 7.4 ± 11 | 8.4 ± 15 | 12 ± 19 | 12.2 ± 19 | 15 ± 20 | 25.2 ± 28 |
| Total Liver/Biliary | 47.1 ± 21 | 44.6 ± 16 | 54.3 ± 19 | 50.9 ± 19 | 46.9 ± 13 | 66.8 ± 23 | 65.1 ± 28 | 56.7 ± 18 | 61 ± 17 | 56.7 ± 19 | 55.8 ± 16 | 55 ± 18 | 55.7 ± 18 | 53.6 ± 18 | 52.6 ± 17 |
| Laparoscopic Cholecystectomy* | N/A | 12.1 ± 7 | 14.9 ± 8 | 15.6 ± 8 | 15.5 ± 7 | 20.2 ± 9 | 23.5 ± 11 | 21.6 ± 9 | 24.5 ± 12 | 24.5 ± 11 | 26.1 ± 12 | 23 ± 10 | 26 ± 13 | 24.2 ± 11 | 22.5 ± 13 |
| Biliary Atresia* | N/A | N/A | N/A | N/A | N/A | 0.9 ± 2 | 2.7 ± 2 | 3.5 ± 3 | 4.1 ± 3 | 3.7 ± 3 | 3.5 ± 3 | 4.1 ± 3 | 3.6 ± 3 | 3.6 ± 3 | 3.9 ± 2 |
| Portoenterostomy^ | N/A | 2.9 ± 2 | 3.4 ± 2 | 4 ± 3 | 3.7 ± 2 | 3.8 ± 3 | 2.2 ± 2 | 1.5 ± 2 | 0.9 ± 1 | 1.4 ± 2 | 0.8 ± 1 | 1.1 ± 1 | 0.9 ± 2 | 1.3 ± 2 | 0.8 ± 1 |
| Pancreatic Resection: Trauma* | 0.8 ± 3 | 0.4 ± 1 | 0.5 ± 1 | 0.4 ± 1 | 0.7 ± 1 | 0.6 ± 1 | 1.1 ± 2 | 0.9 ± 1 | 0.8 ± 1 | 1 ± 1 | 0.9 ± 1 | 1.4 ± 1 | 1 ± 1 | 1.3 ± 2 | 1.4 ± 1 |
| Pancreatic Resection: Tumor^ | 1.4 ± 5 | 0.8 ± 1 | 1.2 ± 2 | 1.2 ± 1 | 1.2 ± 2 | 1.6 ± 1 | 0.9 ± 1 | 0.5 ± 1 | 0.4 ± 1 | 0.5 ± 1 | 0.4 ± 1 | 0.4 ± 1 | 0.4 ± 1 | 0.4 ± 1 | 0.5 ± 1 |
| Lysis of Adhesions^ | N/A | 4.3 ± 4 | 6.3 ± 7 | 4.4 ± 4 | 3.7 ± 4 | 9.4 ± 11 | 7.4 ± 12 | 2.5 ± 4 | 3.9 ± 6 | 1.8 ± 5 | 2.1 ± 4 | 0.7 ± 1 | 1.3 ± 3 | 1.1 ± 2 | 1.6 ± 2 |
| Portosystemic Shunt^ | 2.6 ± 3 | 1.1 ± 4 | 1 ± 3 | 0.7 ± 2 | 0.8 ± 2 | 0.8 ± 2 | 1.1 ± 4 | 0.7 ± 3 | 0.6 ± 2 | 0.5 ± 3 | 0.8 ± 4 | 0.7 ± 2 | 0.5 ± 1 | 0.1 ± 1 | 0.3 ± 1 |
| Laparoscopic Splenectomy^ | N/A | 6.8 ± 4 | 8.2 ± 5 | 7.5 ± 3 | 6.7 ± 3 | 7.1 ± 4 | 6.5 ± 4 | 6.5 ± 4 | 6.5 ± 3 | 6.4 ± 2 | 5.7 ± 3 | 7 ± 4 | 6.1 ± 3 | 5.9 ± 3 | 5.4 ± 3 |
| Total Genitourinary* | 65.5 ± 32 | 65.1 ± 30 | 67 ± 39 | 63.9 ± 30 | 58.6 ± 31 | 81.9 ± 31 | 91.2 ± 42 | 83.4 ± 37 | 83.5 ± 39 | 85.9 ± 36 | 90.1 ± 36 | 79.1 ± 36 | 81.1 ± 39 | 73.4 ± 29 | 78.3 ± 32 |
| Circumcision (OR only)* | N/A | 12.6 ± 13 | 13 ± 13 | 13.3 ± 13 | 11.9 ± 10 | 23.4 ± 13 | 32.1 ± 30 | 26.7 ± 26 | 30 ± 29 | 28.8 ± 23 | 31.7 ± 20 | 26.5 ± 22 | 26.2 ± 21 | 24.8 ± 19 | 26.4 ± 18 |
| Vaginal Procedures: Open* | N/A | N/A | N/A | N/A | N/A | 0.5 ± 1 | 1 ± 1 | 1.1 ± 1 | 1.5 ± 1 | 2.2 ± 3 | 1.8 ± 2 | 1.4 ± 2 | 1.8 ± 2 | 1.6 ± 2 | 2.1 ± 2 |
| Oopherectomy* | N/A | 8.4 ± 4 | 9.6 ± 6 | 9.8 ± 7 | 9.1 ± 6 | 11.1 ± 5 | 10.1 ± 6 | 11.5 ± 7 | 9.2 ± 6 | 10.8 ± 7 | 11.5 ± 7 | 11.6 ± 7 | 11.3 ± 9 | 12.1 ± 7 | 12.7 ± 7 |
| Operation for Testicular Torsion* | N/A | 0.5 ± 1 | 0.5 ± 1 | 0.5 ± 1 | 0.6 ± 1 | 0.6 ± 1 | 0.7 ± 1 | 0.7 ± 1 | 1.4 ± 3 | 2 ± 5 | 1.2 ± 3 | 1 ± 2 | 1.4 ± 4 | 1.1 ± 3 | 1 ± 2 |
| Renal Transplant^ | N/A | 2.7 ± 5 | 2 ± 4 | 2.6 ± 5 | 1.7 ± 3 | 2.1 ± 6 | 1.6 ± 3 | 1.6 ± 4 | 1.5 ± 4 | 1.4 ± 3 | 2 ± 5 | 1.2 ± 4 | 1.6 ± 4 | 1.1 ± 4 | 0.8 ± 2 |
| Nephrectomy: Tumor^ | N/A | 7.1 ± 4 | 7.9 ± 4 | 7 ± 4 | 6.8 ± 3 | 7.7 ± 4 | 7.7 ± 4 | 7.1 ± 4 | 6 ± 3 | 6.3 ± 3 | 5.7 ± 3 | 5.9 ± 4 | 5.3 ± 3 | 5.5 ± 4 | 5.9 ± 4 |
| Ureteral Reconstruction/Reimplantation^ | 1.4 ± 2 | 1.4 ± 2 | 1.4 ± 2 | 0.9 ± 2 | 0.9 ± 2 | 1 ± 2 | 1 ± 2 | 0.8 ± 1 | 0.9 ± 2 | 0.7 ± 2 | 0.8 ± 1 | 0.8 ± 1 | 0.4 ± 1 | 0.4 ± 1 | 0.3 ± 1 |
| Operation for Intersex^ | N/A | 1 ± 1 | 1.2 ± 2 | 0.9 ± 1 | 0.6 ± 1 | 0.7 ± 1 | 0.3 ± 1 | 0.3 ± 1 | 0.3 ± 1 | 0.4 ± 1 | 0.2 ± 0 | 0.5 ± 1 | 0.5 ± 1 | 0.5 ± 1 | 0.3 ± 1 |
Denotes procedures or categories with a statistically significant increase over the study period
Denotes procedures or categories with a statistically significant decrease over the study period
N/A: Represents unavailable data
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Level of Evidence: Level II Abbreviations
Conflict of Interest
The authors do not have any conflicts of interest to declare
References
- 1.Sachdeva AK. The changing paradigm of residency education in surgery: a perspective from the American College of Surgeons. Am Surg. 2007;73(2):120–129. [PubMed] [Google Scholar]
- 2.Shin S, Britt R, Britt LD. Effect of the 80-hour work week on resident case coverage: corrected article. J Am Coll Surg. 2008;207(1):148–150. [DOI] [PubMed] [Google Scholar]
- 3.Shin S, Britt R, Doviak M, Britt LD. The impact of the 80-hour work week on appropriate resident case coverage. J Surg Res. 2010;162(1):33–36. [DOI] [PubMed] [Google Scholar]
- 4.Gow KW, Drake FT, Aarabi S, Waldhausen JH. The ACGME case log: general surgery resident experience in pediatric surgery. J Pedlatr Surg. 2013;48(8):1643–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fairfax LM, Christmas AB, Green JM, Miles WS, Sing RF. Operative experience in the era of duty hour restrictions: is broad-based general surgery training coming to an end? Am Surg. 2010;76(6):578–582. [PubMed] [Google Scholar]
- 6.Raines A, Garwe T, Adeseye A, et al. The effects of the addition of a pediatric surgery fellow on the operative experience of the general surgery resident. Am Surg. 2015;81(6):610–613. [PubMed] [Google Scholar]
- 7.Fingeret AL, Stolar CJ, Cowles RA. Trends in operative experience of pediatric surgical residents in the United States and Canada. J Pedlatr Surg. 2013;48(1):88–94. [DOI] [PubMed] [Google Scholar]
- 8.Mirza B, Ijaz L, Saleem M, Sharif M, Sheikh A. Cystic hygroma: an overview. J Cutan Aesthet Surg. 2010;3(3):139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Niramis R, Watanatittan S, Rattanasuwan T. Treatment of cystic hygroma by intralesional bleomycin injection: experience in 70 patients. Eur J Pediatr Surg. 2010;20(3):178–182. [DOI] [PubMed] [Google Scholar]
- 10.Orford J, Barker A, Thonell S, King P, Murphy J. Bleomycin therapy for cystic hygroma. J Pediatr Surg. 1995;30(9):1282–1287. [DOI] [PubMed] [Google Scholar]
- 11.Tanigawa N, Shimomatsuya T, Takahashi K, et al. Treatment of cystic hygroma and lymphangioma with the use of bleomycin fat emulsion. Cancer. 1987;60(4):741–749. [DOI] [PubMed] [Google Scholar]
- 12.Sounding the alarm. AIDS update no. 403 Asiaweek. 1994:13. [PubMed] [Google Scholar]
- 13.Ogita S, Tsuto T, Nakamura K, Deguchi E, Iwai N. OK-432 therapy in 64 patients with lymphangioma. J Pediatr Surg. 1994;29(6):784–785. [DOI] [PubMed] [Google Scholar]
- 14.Ogita S, Tsuto T, Nakamura K, Deguchi E, Tokiwa K, Iwai N. OK-432 therapy for lymphangioma in children: why and how does it work? J Pediatr Surg. 1996;31(4):477–480. [DOI] [PubMed] [Google Scholar]
- 15.Hall N, Ade-Ajayi N, Brewis C, et al. Is intralesional injection of OK-432 effective in the treatment of lymphangioma in children? Surgery. 2003;133(3):238–242. [DOI] [PubMed] [Google Scholar]
- 16.Rafat N, Schaible T. Extracorporeal Membrane Oxygenation in Congenital Diaphragmatic Hernia. Front Pediatr. 2019;7:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schaible T, Hermle D, Loersch F, Demirakca S, Reinshagen K, Varnholt V. A 20-year experience on neonatal extracorporeal membrane oxygenation in a referral center. Intensive Care Med. 2010;36(7):1229–1234. [DOI] [PubMed] [Google Scholar]
- 18.Turek JW, Nellis JR, Sherwood BG, et al. Shifting Risks and Conflicting Outcomes-ECMO for Neonates with Congenital Diaphragmatic Hernia in the Modern Era. J Pediatr. 2017;190:163–168 e164. [DOI] [PubMed] [Google Scholar]
- 19.Kays DW, Islam S, Larson SD, Perkins J, Talbert JL. Long-term maturation of congenital diaphragmatic hernia treatment results: toward development of a severity-specific treatment algorithm. Ann Surg. 2013;258(4):638–644; discussion 644–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yoder BA, Lally PA, Lally KP, Congenital Diaphragmatic Hernia Study G. Does a highest pre-ductal O(2) saturation <85% predict non-survival for congenital diaphragmatic hernia? J Perinatol. 2012;32(12):947–952. [DOI] [PubMed] [Google Scholar]
- 21.Prabhu S, Mattke AC, Anderson B, et al. Repair of congenital diaphragmatic hernia during extracorporeal life support: experience with six neonates. ANZ J Surg. 2016;86(9):711–716. [DOI] [PubMed] [Google Scholar]
- 22.Soper NJ, Brunt LM, Kerbl K. Laparoscopic general surgery. N Engl J Med. 1994;330(6):409–419. [DOI] [PubMed] [Google Scholar]
- 23.Tam PK. Laparoscopic surgery in children. Arch Dis Child. 2000;82(3):240–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCoy AC, Gasevic E, Szlabick RE, Sahmoun AE, Sticca RP. Are open abdominal procedures a thing of the past? An analysis of graduating general surgery residents' case logs from 2000 to 2011. J Surg Educ. 2013;70(6):683–689. [DOI] [PubMed] [Google Scholar]
- 25.Kogon B, Karamlou T, Baumgartner W, Merrill W, Backer C. Congenital cardiac surgery fellowship training: A status update. J Thorac Cardiovasc Surg. 2016;151(6):1488–1495. [DOI] [PubMed] [Google Scholar]
- 26.Snyder CL. Temporal geomapping of pediatric surgeons in the United States. J Pediatr Surg. 2008;43(3):424–429. [DOI] [PubMed] [Google Scholar]
- 27.Emil SG, Taylor MB. Appendicitis in children treated by pediatric versus general surgeons. J Am Coll Surg. 2007;204(1):34–39. [DOI] [PubMed] [Google Scholar]
- 28.Chen K, Cheung K, Sosa JA. Surgeon volume trumps specialty: outcomes from 3596 pediatric cholecystectomies. J Pediatr Surg. 2012;47(4):673–680. [DOI] [PubMed] [Google Scholar]
- 29.Evans C, van Woerden HC. The effect of surgical training and hospital characteristics on patient outcomes after pediatric surgery: a systematic review. J Pediatr Surg. 2011;46(11):2119–2127. [DOI] [PubMed] [Google Scholar]
- 30.Nygaard RM, Daly SR, Van Camp JM. General Surgery Resident Case Logs: Do They Accurately Reflect Resident Experience? J Surg Educ. 2015;72(6):e178–183. [DOI] [PubMed] [Google Scholar]
- 31.Fronza JS, Prystowsky JP, DaRosa D, Fryer JP. Surgical residents' perception of competence and relevance of the clinical curriculum to future practice. J Surg Educ. 2012;69(6):792–797. [DOI] [PubMed] [Google Scholar]
- 32.Bell RH Jr., Biester TW, Tabuenca A, et al. Operative experience of residents in US general surgery programs: a gap between expectation and experience. Ann Surg. 2009;249(5):719–724. [DOI] [PubMed] [Google Scholar]
- 33.Safavi A, Lai S, Butterworth S, Hameed M, Schiller D, Skarsgard E. Does operative experience during residency correlate with reported competency of recent general surgery graduates? Can J Surg. 2012;55(4):S171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]