Abstract
The COVID-19 pandemic has heightened interest in how physician mental health can be protected and optimised, but uncertainty and misinformation remain about some key issues. In this Review, we discuss the current literature, which shows that despite what might be inferred during training, physicians are not immune to mental illness, with between a quarter and a third reporting increased symptoms of mental ill health. Physicians, particularly female physicians, are at an increased risk of suicide. An emerging consensus exists that some aspects of physician training, working conditions, and organisational support are unacceptable. Changes in medical training and health systems, and the additional strain of working through a pandemic, might have amplified these problems. A new evidence-informed framework for how individual and organisational interventions can be used in an integrated manner in medical schools, in health-care settings, and by professional colleagues is proposed. New initiatives are required at each of these levels, with an urgent need for organisational-level interventions, to better protect the mental health and wellbeing of physicians.
Introduction
Being a physician has long been considered one of the most rewarding and sought-after occupations. However, this work also comes with stressors, some unique to the medical profession, others typical of high-pressure, highly skilled occupations. International attention on mental ill health and suicide among physicians has increased.1 Similar discussions have occurred within other professions, including lawyers, first responders, construction workers, and teachers, with each profession concerned that there might be something inherently psychologically toxic about their work that contributes to the high rates of mental ill health that are reported in these industries.2, 3 In the medical community, this concern has escalated after a number of high-profile suicide clusters among physicians and, over time, by an increasing amount of data highlighting high rates of mental health symptoms,4, 5 suicidal ideation,6 and completed suicide.7, 8, 9 These reports have forced the medical profession to reconsider its own vulnerability. In this context, key professional bodies in different countries have issued calls to action, demanding a greater focus on physician mental health within training programmes, workplaces, and the health service more broadly.10, 11, 12 The importance of this issue goes beyond the desire of the medical professional to look after their peers. Having a healthy, functional workforce of physicians is one of the most important parts of any country's health system,13 with prospective studies showing, for example, that depressed physicians make six times more medication errors than healthy staff,14 with mental ill health or substance misuse a common cause for impairment inquiries by medical regulators.
Despite the rapid increase in the prominence of physician mental health as a topic of interest, uncertainty and misinformation remain about some of the most basic facts surrounding physician wellbeing, and which individual, organisational, and systemic interventions should be prioritised, if any. In this Review, we summarise the available international evidence, to clarify some of the main facts surrounding physician mental health. We also consider a range of potential solutions, including the evidence base for each, and offer recommendations for health services and those in charge of medical training worldwide.
Definitions
The term physician can have different meanings in different countries. Although many of the following issues apply to an array of health-care occupations, we focus specifically on physicians who are medical doctors. We also take a broad view of mental health, to include both the absence of mental disorder as well as a positive state of mental wellbeing.
How common are mental health problems among physicians?
Physicians can be affected by the full spectrum of mental disorders, as well as a range of issues that affect their wellbeing, such as burnout. Like in the general population, the most common mental disorders reported among physicians are depression and anxiety. Given that depression is most likely to emerge before 30 years of age and anxiety disorders tend to have an even earlier age of onset,15 it is unsurprising that most of the studies examining mental health disorders among physicians tend to focus on those in training, or resident physicians. In 2015, a landmark systematic review and meta-analysis collated the results from 54 separate cross-sectional and longitudinal studies involving over 17 500 resident physicians from 18 countries.4 Similar numbers of physicians with depression symptoms were reported regardless of the country and specialty being examined, with a pooled estimate of depression caseness (the number of physicians scoring highly enough on a measure of depression to be considered as having clinically significant depressive symptoms) of 28·8% (95% CI 25·3–32·5).4 Fewer studies have examined anxiety disorders among physicians, with the small number of cross-sectional studies suggesting rates of generalised anxiety disorder as high as 24%,16 and rates of post-traumatic stress disorder ranging between 4% and 16%.17, 18
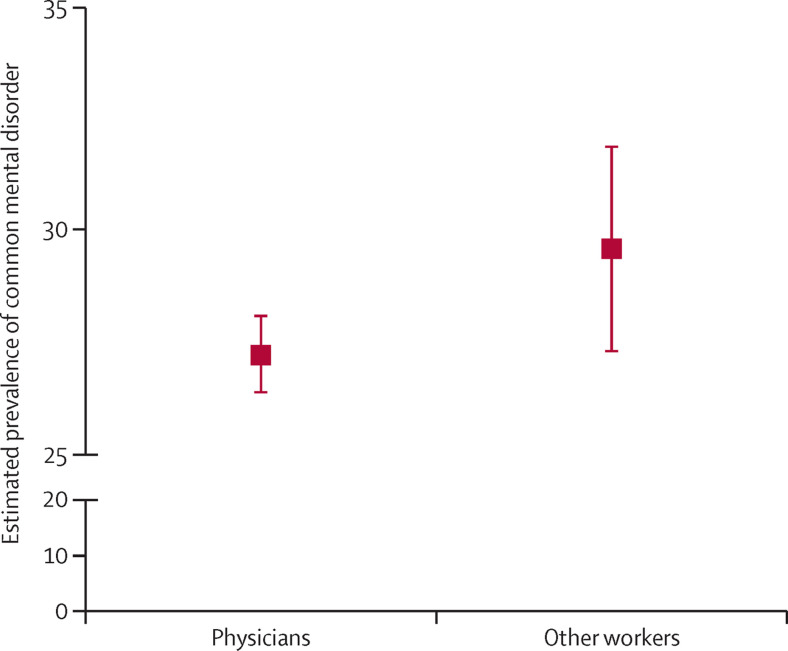
The results of these cross-sectional surveys often lead to statements that the rates of mental disorder in physicians are substantially higher than those in general population surveys. However, further consideration should be given into whether general population surveys are the most appropriate comparison group. A meta-analysis done by Goodwin and colleagues19 reported strong evidence that occupational studies tend to produce higher estimates of depression and anxiety symptoms than general population surveys, regardless of which occupational group is considered. The authors suggest that symptoms might be over-reported when participants know that they have been recruited to a study on the basis that they belong to a specific occupational group, particularly when these same surveys focus on reports of workplace stress. In this case, over-reporting of symptoms might reflect job dissatisfaction rather than mental ill health more generally. Given that occupation studies might report inflated estimates of mental health symptoms, a more appropriate comparison for surveys of physicians might be pooled estimates from similar surveys of other occupational groups. A survey of over 12 000 Australian physicians showed that 27·2% (95% CI 26·4–28·1) reported symptoms of depression and anxiety above a predefined cutoff score that indicated a high likelihood of a minor psychiatric disorder, using the General Health Questionnaire 28 (GHQ-28).20 Goodwin and colleagues’ meta-analysis reported a pooled prevalence estimate for caseness using a shortened, equivalent measure (GHQ-12) across all occupational surveys at 29·6% (95% CI 27·3–31·9).19 This finding implies that the results of this Australian survey, and most other international surveys of physicians, might be better described as showing that physicians are not immune to the types of mental health problems seen in other occupations (figure 1 ).
Figure 1.
Estimated prevalence of common mental disorders in physicians compared with other occupational groups
Comparison between rates of common mental disorder (as measured by self-reported symptoms using the General Health Questionnaire) among physicians and other occupational groups (including teachers, academics, manual workers, military personnel, social workers, and white-collar workers).19, 20
Burnout among physicians
Burnout is a concept that was first described by Freudenberger,21 although its measurement and consequences have been made more widely known by Maslach.22 Described as primarily a social or organisational problem, not an individual one,23, 24 burnout is characterised by emotional exhaustion, cynicism, and feelings of being ineffective.22 In 2019, WHO further described burnout in the 11th Revision of the International Classification of Diseases as a syndrome (not an illness or health condition) resulting from “workplace stress that has not been successfully managed”.25 Even before this recognition by WHO, a range of research reports had suggested that a large, and increasing, number of physicians might be experiencing burnout.26, 27, 28, 29, 30
Symptoms subsumed within the construct of burnout are common among physicians and are associated with substantial suffering, physicians leaving the profession or reducing their hours, and moral distress. In terms of individual health, burnout symptoms are associated with a higher risk of road traffic collisions,31 sickness absence for both mental and cardiovascular disorders,32 and all-cause mortality.33 At an organisational level, burnout is associated with higher sickness absence rates, reduced productivity, and early retirement.32, 33, 34, 35, 36 Several studies have also linked physician burnout with adverse clinical events, unprofessional behaviour, and lower quality of patient care.37, 38, 39, 40
However, the construct of burnout also presents some difficulties. As a relatively newly defined phenomenon, definitions, measures, and thresholds are in evolution, and such imprecision has made rigorously investigating burnout among physicians challenging. A 2018 systematic review of 182 studies of burnout in physicians done across 45 countries reported that studies used different definitions of burnout, although studies using the more common measures (such as the 22-item Maslach Burnout Inventory–Human Services Survey criteria) reported a prevalence of 25% to 50%.41 Although the effects of relatively mild or infrequent symptoms on the individual might be debatable,42, 43 taken collectively, any changes in burnout throughout an organisation might be an important indicator of organisational culture and wellbeing.
Furthermore, debate continues regarding the association between burnout and depression.44 Although there is symptomatic and epidemiological overlap, burnout is defined as arising predominantly from workplace problems, whereas depression is agnostic to the cause; it is possible to be burned out and not depressed, and vice versa, or both. Burnout and depression are related but have distinct symptoms and, as a result, require different prevention and management approaches; for example, antidepressant medications are a proven treatment for depression, but these medications might not be an appropriate intervention for burnout. Care must be taken to ascertain whether physicians reporting burnout might have an underlying depressive disorder amenable to evidence-based treatment if appropriately identified, and whether physicians’ reports of depression suggest occupational factors that contribute to distress. Also, overlap might exist between a diagnosis of post-traumatic stress disorder and anxiety disorders with health professionals’ experiences of vicarious trauma, moral distress, and workplace abuse, but these associations have been better described in nurses than in physicians.45
Physician suicide
General and most cause-specific mortality rates are low in physicians compared with the general population,46 presumably due to an enhanced version of the healthy worker effect, which occurs when observational studies underestimate mortality rates in employed populations compared with the general population because employed populations exclude individuals who are ill or disabled and therefore unable to work.47 Education and high incomes might also drive lower mortality rates. However, suicide rates appear to be a notable exception,48 with a 2019 systematic review and meta-analysis calculating an overall standardised mortality rate of 1·44 for suicides among physicians.49 Female physicians appear to be at particular risk, with a 2020 meta-analysis reporting female physicians had a suicide rate that was significantly higher than women in the general population.50 Estimates suggest that, in the USA, one doctor dies by suicide per day.10 Although physicians have similar prevalence rates of depression and anxiety to those reported by other occupations, they are at disparate risk of suicide. This risk contrasts with the general trend for greater risk of suicide in lower skilled occupational groups.51 In a Danish national register-based study, physicians had a higher risk of suicide than any of the 55 other occupations considered, and risk estimates further increased after sociodemographic factors were taken into account.52
Access to lethal means, and the knowledge to effectively use such means, is one of the most important reasons for the increased risk of suicide in physicians.53 This hypothesis is supported by the observation of a similarly high suicide rate in other health professionals with such access, including nurses, dentists, and pharmacists.9 A further factor in explaining suicide rates among physicians might be specific barriers that prevent timely access to treatment and support. The small number of published studies have estimated rates of help-seeking among physicians with mental disorders to be between 13% and 36%.54, 55, 56, 57 Physicians with mental health problems might be more reluctant than non-physicians to seek help for a variety of reasons,58 with major barriers including fears regarding confidentiality, the potential consequences for their career, medical registration, and licensure, as well as insufficient time and a belief that they can manage any symptoms by themselves.20, 59 Qualitative studies of physicians who have had mental health problems have shown a high prevalence of self-stigma, often driven by views that doctors should be invincible, as well as a fear of discrimination.60 These factors act as major barriers to seeking help and recovery, alongside considerable cultural stigma among the medical profession.60
Notably, there is emerging evidence of a link between area of specialty and risk of suicide, with a 2019 review suggesting that anaesthetists, psychiatrists, general practitioners, and general surgeons might have higher rates of suicide than other specialists.61 If confirmed, it is unclear if this finding is due to these specialists having higher rates of mental ill health, greater access to high lethality means, more barriers to seeking help, or a combination of these and other factors. For example, the apparent increased risk of suicide among anaesthetists appears to be related to a combination of higher rates of psychological distress in addition to access to lethal means.20
Substance misuse among physicians
Most research investigating alcohol and substance misuse among physicians has been done through large-scale self-report surveys. Research suggests that between 5% and 20% of doctors across a range of high-income countries consume alcohol problematically (usually determined by the Alcohol Use Disorders Identification Test scores or related instruments). In a sample of 7209 American physicians, 1100 (15·3%) reported scores indicative of alcohol abuse or alcohol dependence,62 with a similar prevalence reported in American surgeons.63 In a national sample of Danish doctors (comprising specialists, trainees, and general practitioners), the prevalence of hazardous alcohol use was identified in 18·9% of respondents.64 This study also reported that of the 383 physicians who reported risky substance misuse (alcohol or other drugs, or both), 76·9% felt their substance misuse was unproblematic. A smaller UK-based study reported that 22 (20%) of 109 doctors drank alcohol nearly exceeding, or exceeding, recommended levels,65 although only 5% of doctors from another study met the criteria for alcohol dependence.66 These results suggest that, compared with the general population, physicians might consume alcohol at a similar rate, or perhaps at a higher rate.62, 67 This trend appears to have been maintained over the past 30 years.68
Self-report data suggest that a substantial proportion of physicians have experimented with illicit substances at some point in their lifetime.68 However, use in the 12-month period before the study was lower than for the general population. An exception to this finding is the use of prescription drugs (eg, benzodiazepines and minor opiates), which was higher than general population estimates and often self-prescribed.68, 69, 70 This trend appears to remain consistent over time and across different countries, with 2012 data from Australian doctors finding 5% reported using illicit substances at some point, and 6% reported using self-prescribed drugs for the treatment of symptoms of depression or anxiety daily.20
Whether an association exists between certain medical subspecialties and the use of different substances is often debated, with much anecdotal evidence and some older studies focusing on anaesthesiology as a specialty perceived as being at high risk.71, 72, 73 In the past 10 years, studies have reported a different pattern, with the highest prevalence of hazardous alcohol consumption among dermatologists and orthopaedic surgeons,62 or internal and emergency medicine specialities.64 Contrary to this finding, data from Australia suggested little difference between doctors working in different specialty areas in terms of alcohol use.20
Unfortunately, it is difficult for physicians to seek help for alcohol or substance misuse problems. The lack of early help-seeking among physicians is concerning, given the potential effect of substance misuse on a physician's work performance. A survey of American surgeons and a similar study of physicians found that in the 3 months before the study, most physicians who reported a medical error also reported alcohol abuse or dependence.62, 63 Estimates suggest that the effects of alcohol could account for up to 5% of instances of suboptimal patient care.74
Risk factors for mental ill health and suicide among physicians
Although mental ill health appears no more prevalent in physicians than in other occupational groups, the fact that it is not lower should be concerning. Many of the risk factors for poor mental health reflect psychosocial disadvantage,75 which is relatively uncommon among physicians. One factor often cited when physician mental health is discussed is their exposure to human suffering and death. Physicians working in conflict zones or in low-income and middle-income countries (LMICs) face unique challenges, including threats to their own or their family's safety,76 and that physicians and other health-care workers are often at the frontline of public health responses to major critical incidents and emergencies, such as natural disasters,77 terrorism, or as recently evidenced, infectious disease outbreaks such as COVID-19.78 Although major events can cause increases in mental ill health among physicians, routine exposure to human ill health and suffering is not always the precipitant of mental ill health among physicians.79 Instead, more typical psychosocial workplace risk factors,80 such as excessive or conflicting job demands, an imbalance of work and family life, long working hours, and interpersonal conflict, are often more important in explaining much of the variation in mental ill health among physicians.81, 82 Additional risk factors appear relevant for junior physicians during training, including excessive working hours, study, and examinations.83, 84
Although the role of work-based risk factors can be important, it is essential that the role of protective factors in the workplace also be considered. Decades of research has shown that the mental health impact of demanding jobs can be buffered, to some degree, by high levels of control at work, peer-based social support,85, 86 and a belief that one's efforts are adequately rewarded through pay and intangibles.87 For many years, most physicians have enjoyed high levels of autonomy, control over their working lives, social support from their peer networks, as well as public esteem, renumeration, and social status.88 All of these factors probably have provided some protection against the negative effects of the stressful aspects of a medical career. However, in many countries physicians face increasing bureaucratic and administrative burden and an erosion of many of these protective factors.
In addition to risk factors common to all physicians, there might be additional risk factors that operate at certain stages of a physician's career. A review of prospective studies identified particularly high rates of depression and suicidal ideation among physicians during their first postgraduate internship year.89 These findings are consistent with a later prospective cohort study of 740 interns from multiple specialties across 13 institutions in the USA, finding an increase in depression symptoms across the intern year of six times that of physicians further along in their career.90 Other international studies have reported that rates of depressive symptoms and suicidal ideation appear to be consistently higher during training and residency, before reducing among consultants and more experienced physicians.20 Although to some extent these differences probably mirror the different prevalence rates observed in the general population among different age groups, the differences might also reflect the effects of unique stressors operating during physician training, such as examination stress, financial pressures, and job insecurity.
Are things getting worse for physicians?
Recent trends in the mental health of physicians
There is some evidence that rates of mental ill health symptoms might have gradually increased among physicians in the past three decades, with one meta-analysis suggesting that the prevalence of depression has increased an average of 0·5% per year.4 Some of this apparent trend might reflect an underlying cohort effect present in the observed rise of mental ill health in young people (<25 years) in the general population. Additionally, medical courses have changed radically in many countries, with a widespread move to more graduate medical education.91 Although this shift does not appear to have brought about the hoped for improvements in medical school completion rates or intern year performance,92 more years as a student has resulted in junior doctors qualifying with more debt and a higher likelihood of having competing family responsibilities during early training, both of which are risk factors for poor mental health.
At the same time that some risk factors appear to have increased, a number of protective factors previously present for physicians have been on the decline.93 Physicians’ sense of control and autonomy have been undermined by increased administrative burden, external roster scheduling, electronic records, and health system constraints that have tended to increase year on year.94 Furthermore, there has been a shift in physicians’ expectations of their career, with medical schools producing graduates who tend to be much more focused on achieving an acceptable work–life balance, not just because of a more balanced gender mix, but because society and successive generations have placed a higher value on work–life balance.95
The ongoing COVID-19 pandemic has raised further concerns about physician mental health. Across the world, physicians have been on the front line while caring for patients infected with SARS-CoV-2. Health systems in many countries have been overwhelmed with unprecedented pressure on critical care facilities, forcing physicians to make decisions about the allocation of scant resources.96 Early in the pandemic, there were shortages of personnel protective equipment, with as many as 20% of the workforce caring for those with COVID-19 becoming infected themselves, meaning many physicians witnessed their colleagues becoming seriously unwell or dying due to their work.97 Over the past 12 months, there has been a surge of studies examining the mental health impact of COVID-19 on the health-care workforce. These studies tend to show an increase in acute self-reported symptoms of depression and anxiety, as well as high rates of insomnia and distress.98 For example, a study surveying health-care workers (including 493 physicians) from areas most affected by the COVID-19 pandemic, such as China, showed that 225 (46%) reported mild-to-severe depression symptoms, 200 (41%) reported mild-to-severe anxiety symptoms, and 330 (67%) reported mild-to-severe post-traumatic stress symptoms.99 Long-term follow-up studies of health workers who have worked in previous pandemics, such as the 2003 outbreak of severe acute respiratory syndrome, suggest that for some individuals (potentially as many as one in ten) these early distress symptoms will progress to longer lasting mental health conditions, such as post traumatic stress disorder.100
The mental health of physicians in LMICs
Most evidence available on physician mental health comes from high-income countries.4 Physicians working in LMICs face a range of specific challenges. The health systems and health policies in LMICs are often less well developed and have fewer resources than high-income countries. Physicians comprise a smaller proportion of the health-care workforce in LMICs, with a greater reliance on non-specialist, lower-skilled health-care providers. The global shortage of physicians in LMICs, estimated to be a deficit of 2·8 million physicians by 2030,101 means that those physicians remaining in these systems often face highly stressful working conditions, major resource and infrastructure constraints, poor career and development opportunities, and income disparities, all of which can negatively affect mental health. If physicians in LMICs develop mental health symptoms, they might be less able to access evidence-based psychological treatments than physicians in higher-income countries.102, 103
Single studies of small samples have shown substantial rates of depression, stress, and anxiety symptoms among physicians from a specific LMIC, such as Vietnam,104 North India,105 China,106 Bangladesh,107 Turkey,108 Pakistan,109 and occupied Palestinian territory.110 A smaller number of studies of medical residents have also shown that burnout can also be an important issue among physicians in LMICs.111, 112 However, to our knowledge, there has been no comprehensive analysis published concerning the overall burden of common mental disorders among physicians across LMICs. Almost all of the studies examining suicide among medical professionals have also been done primarily in high-income countries, meaning the scale of this issue among LMICs is largely unknown.
Potential solutions
Interventions to improve physician mental health
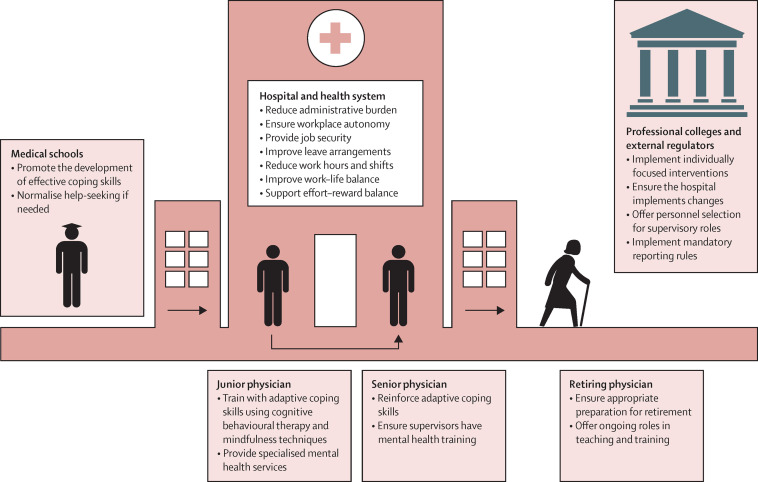
Multiple medical professional bodies have called for a greater focus on physician mental health.10, 11, 12 Although arguing that action is needed is relatively straight forward, defining what actions the medical profession, education, and health-care systems should take is more difficult. The best evidence for how to create more mentally healthy workplaces suggests that a coordinated range of different initiatives are needed, extending from prevention through to recovery and return-to-work, and implemented at both the individual and organisational level.3, 113, 114 Although this type of framework has been used effectively in other industries, such as first responders, the unique characteristics of the health-care system and medical training mean that such frameworks will need to be modified for physicians.115, 116 Most obviously, many physicians do not have a single line manager to whom they report; they might be employed by a health service, but report to a professional college for their training or accreditation, while having a separate agency as their regulator. Trainee physicians also change colleagues, seniors, and work settings frequently, and undertake rural or regional placements, challenging their engagement with uncoordinated initiatives. Given this complexity, any systematic attempt to improve the mental health of physicians will need to consider how this mobile group can be provided with a coherent suite of interventions and policies that follow physicians from the start of their medical career through to retirement, across different training and employing institutions. A model for how this approach might operate is shown in figure 2 , which highlights the three key levels at which interventions focused on physicians’ mental health need to operate: the individual physician, the health system and the professional colleges, and the external regulators. Although interventions aimed at individual physicians are discussed in this Review, this approach should not be considered the most important. Quite the contrary is true; there is clear evidence that physicians as a group do not have a deficit in resilience,117 and that a greater focus on organisational measures is urgently needed.118
Figure 2.
A model for how individual and organisational measures could operate to improve physician mental health throughout a physician's career
The individual physician
The foundation for developing physicians who are able to develop healthy habits and self-awareness, can ask for help when needed, and use effective coping mechanisms at times of stress needs to be established in medical schools. Simply inserting mental health awareness lectures into an already crowded medical student curriculum is unlikely to be effective and might even have adverse consequences, such as creating unnecessary anxiety and fostering a sense of vulnerability. What is more likely to be effective, but is still untested, is the evolution of a medical student curriculum that allows for progressive development of self-awareness and effective coping skills and that encourages peer support, resilience, and optimism, while normalising appropriate help-seeking when needed.119, 120
There is often a marked increase in mental health symptoms in the first few years of a junior doctor's working life. This transition period probably represents a further opportunity for reinforcing adaptive coping skills. A 2019 systematic review reported that individually-focused interventions for physicians, including teaching cognitive behavioural therapy or mindfulness-based techniques to deal with stressful situations or early symptoms, resulted in a moderate reduction in symptoms of depression and anxiety as well as reduced symptoms of suicidal ideation.121 Similar results have also been noted for individual-level interventions aimed at reducing physician burnout.30, 122, 123 One of the key challenges for these interventions is how they can be taken to scale. One potential solution is the use of eHealth and mobile phone apps, which have been shown to be an effective and more feasible way (than face-to-face) to deliver these types of interventions in other occupational groups.124 To our knowledge, there is only one published randomised controlled trial of this type of eHealth intervention among physicians, which was able to halve the rates of suicidal ideation among interns,125 with a trial of a mental health app for trainee physicians underway in Australia.
Although encouraging help-seeking among physicians is important, it is vital to ensure that good quality services and appropriate treatment is available when physicians seek additional support. In some countries, specialist mental health services have been created for physicians. The potential advantage of such services is that additional steps can be taken to ensure confidentiality and physicians can be reassured that they are working with specialists in managing other medical practitioners.126 The outcome data from a specialist service set up for physicians in the UK suggest that such services are well liked and used and are able to promote successful return to functioning for many individuals who use them.127
The health system
Modifications within the health system should aim to minimise work-based risk factors and promote protective factors. Although conceptually compelling, organisational interventions have been under-researched among physicians. Systematic reviews have supported the idea that there have been no published randomised controlled trials of organisational interventions that consider mental disorder as an outcome, and that there have been only three trials focused on organisational interventions for burnout.30, 121 Although very limited in number, these studies have showed that interventions such as modifications to work processes and shortening of shifts can lead to an improvement in some mental health outcomes.30 In fact, the result of one meta-analysis suggests that the positive effects of such organisational interventions on burnout symptoms are significantly greater than a range of individually-focused interventions.128 Given that burnout is conceptualised as an organisational problem, such findings are not surprising. Team training, reducing cognitive load resulting from meaningless administrative tasks and poorly-designed electronic health records, and flexible scheduling also might help to reduce burnout.30, 129 Using clinician wellbeing and the financial costs associated with burnout as quality metrics for health-care organisations might draw attention to the problem and promote change in the organisation of health-care delivery, to promote greater clinician wellbeing.130, 131, 132 A consensus study report by the US National Academy of Medicine has provided guidelines aimed at redesigning clinical systems to allow physicians to focus on the human aspects of care and to promote physician wellbeing. The organisation recommend a multifaceted system-based approach, including initiatives to reduce administrative burden, to optimise use of health-care technologies, and to foster a more positive working environment.133
Given what is known about the role of risk and protective factors, it is probable that there are other (currently untested) organisational interventions that could also be effective in improving physician mental health. These interventions include strategies to improve physician autonomy and control in the workplace, job security, leave, and other policies that reduce work–family conflicts, as well as a range of other initiatives to support an appropriate effort–reward balance.80
Professional colleges and external regulators
In many countries, the professional medical colleges have near absolute control of specialty training programmes and the requirements of both the individual physicians and the health-care systems that train them. Therefore, these agencies are in a powerful position to influence the job design and working conditions of junior physicians as well as to promote, or even mandate, some of the individual-focused and organisational-focused interventions. Additionally, training colleges can also ensure that the individuals who they place in charge of mentoring and training junior physicians are equipped to be able to better support and manage the next generation of physicians. In other industry groups, training leaders to recognise and respond to junior staff in need of assistance has been shown to result in sustained improvements in their own behaviour, with some measurable benefits reported among those individuals who they manage.134, 135 Although similar trials are yet to occur among medical leaders, a number are in process (eg, ACTRN12619001496101) and it is hoped that similar positive results will be observed.
In addition to this role of controlling specialty training programmes, external regulators set the environment in which physicians need to operate when considering seeking help for a mental health condition. Rules regarding the mandatory reporting of mental ill health can affect physicians’ willingness to seek help. In one US study, physicians working in a state where medical licence applications and renewal forms asked specifically about mental illness were 20% less likely to ask for help if needed.59 Early intervention for psychiatric symptoms, as well as ensuring that decisions about registration and ability to work are focused on functional impacts of symptoms (not specific diagnoses or treatments), is essential in preventing attrition from medical training and premature retirement.
Conclusions and future directions
The mental health and wellbeing of physicians has been neglected for too long. There is overwhelming evidence that, despite what might be inferred during traditional undergraduate and postgraduate education, physicians are not immune to mental illness and are, in fact, at greater risk of suicide than most other professional groups. The strain placed on physicians across the world during the COVID-19 pandemic has probably worsened this situation. Action is needed to better protect the mental health and wellbeing of physicians, particularly those early in their career.
There is an emerging consensus that some aspects of physician training, working conditions, and support are unacceptable. Importantly, there is also a recognition that many of the changes that have occurred in medical training and health systems over the past three decades have amplified these problems and eroded the protective factors that previously offset the risks inherent in physician work. Common issues, such as administrative and bureaucratic burden, job insecurity, reduced job control, and a shift in the age and priorities of medical graduates, appear across the international medical community and probably help to explain some of the growing mental health concerns among physicians. There remains a striking absence of information about the mental health of physicians working in LMICs, although there are sound reasons to suggest these physicians might be under great strain.
Urgent action from a range of stakeholders is needed to radically rethink the training and employment conditions of physicians. In this Review, we have outlined how a range of integrated initiatives can be implemented at the level of the individual physician, health system, and professional colleges and external regulators. New initiatives are required at each of these levels, but there is a particularly urgent need for organisational-level interventions. Although evidence shows that individual-level interventions are important, there is a risk that interventions solely focused on the individual physician might lead to the perception that lower levels of individual resilience is the key problem.117 This is not the case. The role of training programmes, leadership, and the broader health-care system must be given prominence, and evidence-based interventions focused on these areas must be given the greatest priority.
Search strategy and selection criteria
We identified references for this Review through searches of MEDLINE, Embase, PsycINFO, and Google Scholar. These searches were done in 2019, with focused updated searches done in 2020. We searched for studies published from databases’ inception to Nov 3, 2020. Publications in English were identified with various search terms for “mental disorder”, “burnout”, “substance misuse”, or “suicide” combined with “physicians” or “doctors”.
Declaration of interests
Contributors
MH and SBH developed the concept for this Review. SBH, RME, NG, KP, JS, AG, KD, and MH wrote sections of the original draft of the Review. KP led project administration, and JS, SBH, and KP created the figures. All authors reviewed and edited the Review and had responsibility for the decision to submit this Review.
SBH and KP reports grant income from iCare Foundation and NSW Health. MH was a consultant psychiatrist at the Practitioner Health Programme between 2010 and 2015. All other authors declare no competing interests.
References
- 1.Gerada C. Doctors and mental health. Occup Med (Lond) 2017;67:660–661. doi: 10.1093/occmed/kqx090. [DOI] [PubMed] [Google Scholar]
- 2.Harvey SB, Henderson M. Occupational Psychiatry. Psychiatry. 2009;8:174–178. [Google Scholar]
- 3.Henderson M, Harvey SB, Overland S, Mykletun A, Hotopf M. Work and common psychiatric disorders. J R Soc Med. 2011;104:198–207. doi: 10.1258/jrsm.2011.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mata DA, Ramos MA, Bansal N, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314:2373–2383. doi: 10.1001/jama.2015.15845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Firth-Cozens J. In: Understanding doctors' performance. Cox JK, Hutchinson A, McAvoy P, editors. Radcliffe Publishing; Oxford: 2006. Chapter 2: a perspective on stress and depression; pp. 22–25. [Google Scholar]
- 6.Tyssen R, Vaglum P, Grønvold NT, Ekeberg O. Suicidal ideation among medical students and young physicians: a nationwide and prospective study of prevalence and predictors. J Affect Disord. 2001;64:69–79. doi: 10.1016/s0165-0327(00)00205-6. [DOI] [PubMed] [Google Scholar]
- 7.Agerbo E, Gunnell D, Bonde JP, Mortensen PB, Nordentoft M. Suicide and occupation: the impact of socio-economic, demographic and psychiatric differences. Psychol Med. 2007;37:1131–1140. doi: 10.1017/S0033291707000487. [DOI] [PubMed] [Google Scholar]
- 8.Hem E, Haldorsen T, Aasland OG, Tyssen R, Vaglum P, Ekeberg O. Suicide rates according to education with a particular focus on physicians in Norway 1960–2000. Psychol Med. 2005;35:873–880. doi: 10.1017/s0033291704003344. [DOI] [PubMed] [Google Scholar]
- 9.Hawton K, Agerbo E, Simkin S, Platt B, Mellanby RJ. Risk of suicide in medical and related occupational groups: a national study based on Danish case population-based registers. J Affect Disord. 2011;134:320–326. doi: 10.1016/j.jad.2011.05.044. [DOI] [PubMed] [Google Scholar]
- 10.Center C, Davis M, Detre T, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289:3161–3166. doi: 10.1001/jama.289.23.3161. [DOI] [PubMed] [Google Scholar]
- 11.Thomas LR, Ripp JA, West CP. Charter on physician well-being. JAMA. 2018;319:1541–1542. doi: 10.1001/jama.2018.1331. [DOI] [PubMed] [Google Scholar]
- 12.Smith R. Why are doctors so unhappy? There are probably many causes, some of them deep. BMJ. 2001;322:1073–1074. doi: 10.1136/bmj.322.7294.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 14.Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488–491. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 16.Ruitenburg MM, Frings-Dresen MH, Sluiter JK. The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: a cross-sectional study. BMC Health Serv Res. 2012;12:292–298. doi: 10.1186/1472-6963-12-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weiniger CF, Shalev AY, Ofek H, Freedman S, Weissman C, Einav S. Posttraumatic stress disorder among hospital surgical physicians exposed to victims of terror: a prospective, controlled questionnaire survey. J Clin Psychiatry. 2006;67:890–896. doi: 10.4088/jcp.v67n0605. [DOI] [PubMed] [Google Scholar]
- 18.Wilberforce N, Wilberforce K, Aubrey-Bassler FK. Post-traumatic stress disorder in physicians from an underserviced area. Fam Pract. 2010;27:339–343. doi: 10.1093/fampra/cmq002. [DOI] [PubMed] [Google Scholar]
- 19.Goodwin L, Ben-Zion I, Fear NT, Hotopf M, Stansfeld SA, Wessely S. Are reports of psychological stress higher in occupational studies? A systematic review across occupational and population based studies. PLoS One. 2013;8 doi: 10.1371/journal.pone.0078693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.BeyondBlue . BeyondBlue; Melbourne: 2013. National Mental Health Survey of Doctors and Medical Students. [Google Scholar]
- 21.Freudenberger HJ. The staff burn-out syndrome in alternative institutions. Psychotherapy (Chic) 1975;12:73–82. [Google Scholar]
- 22.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 23.Maslach C. Finding solutions to the problem of burnout. Consult Psychol J. 2017;69:143–152. [Google Scholar]
- 24.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15:103–111. doi: 10.1002/wps.20311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Lancet ICD-11. Lancet. 2019;393 doi: 10.1016/S0140-6736(19)31205-X. [DOI] [PubMed] [Google Scholar]
- 26.Curtis JR, Puntillo K. Is there an epidemic of burnout and post-traumatic stress in critical care clinicians? Am J Respir Crit Care Med. 2007;175:634–636. doi: 10.1164/rccm.200702-194ED. [DOI] [PubMed] [Google Scholar]
- 27.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 28.Shanafelt TD, Sinsky C, Dyrbye LN, Trockel M, West CP. Burnout among physicians compared with individuals with a professional or doctoral degree in a field outside of medicine. Mayo Clin Proc. 2019;94:549–551. doi: 10.1016/j.mayocp.2018.11.035. [DOI] [PubMed] [Google Scholar]
- 29.Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019;94:1681–1694. doi: 10.1016/j.mayocp.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 30.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 31.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 32.Toppinen-Tanner S, Ojajärvi A, Väänänen A, Kalimo R, Jäppinen P. Burnout as a predictor of medically certified sick-leave absences and their diagnosed causes. Behav Med. 2005;31:18–27. doi: 10.3200/BMED.31.1.18-32. [DOI] [PubMed] [Google Scholar]
- 33.Ahola K, Väänänen A, Koskinen A, Kouvonen A, Shirom A. Burnout as a predictor of all-cause mortality among industrial employees: a 10-year prospective register-linkage study. J Psychosom Res. 2010;69:51–57. doi: 10.1016/j.jpsychores.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 34.Tawfik DS, Scheid A, Profit J, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171:555–567. doi: 10.7326/M19-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dewa CS, Jacobs P, Thanh NX, Loong D. An estimate of the cost of burnout on early retirement and reduction in clinical hours of practicing physicians in Canada. BMC Health Serv Res. 2014;14:254. doi: 10.1186/1472-6963-14-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Linzer M. Clinician burnout and the quality of care. JAMA Intern Med. 2018;178:1331–1332. doi: 10.1001/jamainternmed.2018.3708. [DOI] [PubMed] [Google Scholar]
- 38.Salyers MP, Bonfils KA, Luther L, et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. 2017;32:475–482. doi: 10.1007/s11606-016-3886-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dewa CS, Loong D, Bonato S, Trojanowski L. The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-015141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dyrbye LN, Massie FS, Jr, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173–1180. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 41.Rotenstein LS, Torre M, Ramos MA, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320:1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwenk TL, Gold KJ. Physician burnout—a serious symptom, but of what? JAMA. 2018;320:1109–1110. doi: 10.1001/jama.2018.11703. [DOI] [PubMed] [Google Scholar]
- 43.Bianchi R. A reflection on the measurement of the burnout syndrome. Acad Emerg Med. 2015;22:378. doi: 10.1111/acem.12611. 378. [DOI] [PubMed] [Google Scholar]
- 44.Privitera MR. Is burnout a form of depression? 2018. https://www.medscape.com/viewarticle/896537
- 45.Rushton C. Oxford University Press; New York, NY: 2018. Moral resilience: transforming moral suffering in healthcare. [Google Scholar]
- 46.Torre DM, Wang N-Y, Meoni LA, Young JH, Klag MJ, Ford DE. Suicide compared to other causes of mortality in physicians. Suicide Life Threat Behav. 2005;35:146–153. doi: 10.1521/suli.35.2.146.62878. [DOI] [PubMed] [Google Scholar]
- 47.Chowdhury R, Shah D, Payal AR. Healthy worker effect phenomenon: revisited with emphasis on statistical methods—a review. Indian J Occup Environ Med. 2017;21:2–8. doi: 10.4103/ijoem.IJOEM_53_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schernhammer ES, Colditz GA. Suicide rates among physicians: a quantitative and gender assessment (meta-analysis) Am J Psychiatry. 2004;161:2295–2302. doi: 10.1176/appi.ajp.161.12.2295. [DOI] [PubMed] [Google Scholar]
- 49.Dutheil F, Aubert C, Pereira B, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One. 2019;14 doi: 10.1371/journal.pone.0226361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Duarte D, El-Hagrassy MM, Couto TCE, Gurgel W, Fregni F, Correa H. Male and female physician suicidality: a systematic review and meta-analysis. JAMA Psychiatry. 2020;77:587–597. doi: 10.1001/jamapsychiatry.2020.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Milner A, Spittal MJ, Pirkis J, LaMontagne AD. Suicide by occupation: systematic review and meta-analysis. Br J Psychiatry. 2013;203:409–416. doi: 10.1192/bjp.bp.113.128405. [DOI] [PubMed] [Google Scholar]
- 52.Agerbo E, Gunnell D, Bonde JP, Mortensen PB, Nordentoft M. Suicide and occupation: the impact of socio-economic, demographic and psychiatric differences. Psychol Med. 2007;37:1131–1140. doi: 10.1017/S0033291707000487. [DOI] [PubMed] [Google Scholar]
- 53.Hawton K, Clements A, Simkin S, Malmberg A. Doctors who kill themselves: a study of the methods used for suicide. QJM. 2000;93:351–357. doi: 10.1093/qjmed/93.6.351. [DOI] [PubMed] [Google Scholar]
- 54.Fridner A, Belkić K, Marini M, Gustafsson Sendén M, Schenck-Gustafsson K. Why don't academic physicians seek needed professional help for psychological distress? Swiss Med Wkly. 2012;142 doi: 10.4414/smw.2012.13626. [DOI] [PubMed] [Google Scholar]
- 55.Holmes EG, Connolly A, Putnam KT, et al. Taking care of our own: a multispecialty study of resident and program director perspectives on contributors to burnout and potential interventions. Acad Psychiatry. 2017;41:159–166. doi: 10.1007/s40596-016-0590-3. [DOI] [PubMed] [Google Scholar]
- 56.Jones N, Nguyen J, Strand NK, Reeves K. What should be the scope of physicians' roles in responding to gun violence? AMA J Ethics. 2018;20:84–90. doi: 10.1001/journalofethics.2018.20.1.pfor2-1801. [DOI] [PubMed] [Google Scholar]
- 57.Grover S, Dua D, Shouan A, Nehra R, Avasthi A. Perceived stress and barriers to seeking help from mental health professionals among trainee doctors at a tertiary care centre in North India. Asian J Psychiatr. 2019;39:143–149. doi: 10.1016/j.ajp.2018.12.020. [DOI] [PubMed] [Google Scholar]
- 58.Hawton K, Malmberg A, Simkin S. Suicide in doctors. A psychological autopsy study. J Psychosom Res. 2004;57:1–4. doi: 10.1016/S0022-3999(03)00372-6. [DOI] [PubMed] [Google Scholar]
- 59.Dyrbye LN, West CP, Sinsky CA, Goeders LE, Satele DV, Shanafelt TD. Medical licensure questions and physician reluctance to seek care for mental health conditions. Mayo Clin Proc. 2017;92:1486–1493. doi: 10.1016/j.mayocp.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 60.Henderson M, Brooks SK, Del Busso L, et al. Shame! Self-stigmatisation as an obstacle to sick doctors returning to work: a qualitative study. BMJ Open. 2012;2 doi: 10.1136/bmjopen-2012-001776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dutheil F, Aubert C, Pereira B, et al. Suicide among physicians and health-care workers: a systematic review and meta-analysis. PLoS One. 2019;14 doi: 10.1371/journal.pone.0226361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Oreskovich MR, Shanafelt T, Dyrbye LN, et al. The prevalence of substance use disorders in American physicians. Am J Addict. 2015;24:30–38. doi: 10.1111/ajad.12173. [DOI] [PubMed] [Google Scholar]
- 63.Oreskovich MR, Kaups KL, Balch CM, et al. Prevalence of alcohol use disorders among American surgeons. Arch Surg. 2012;147:168–174. doi: 10.1001/archsurg.2011.1481. [DOI] [PubMed] [Google Scholar]
- 64.Sørensen JK, Pedersen AF, Bruun NH, Christensen B, Vedsted P. Alcohol and drug use among Danish physicians. A nationwide cross-sectional study in 2014. Dan Med J. 2015;62:62. [PubMed] [Google Scholar]
- 65.Savage E, Sowole L, Shah S, Mirza Z, Cotzias C. Self-reported alcohol consumption in doctors. Occup Med (Lond) 2020;70:439–441. doi: 10.1093/occmed/kqaa111. [DOI] [PubMed] [Google Scholar]
- 66.Medisauskaite A, Kamau C. Does occupational distress raise the risk of alcohol use, binge-eating, ill health and sleep problems among medical doctors? A UK cross-sectional study. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-027362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ohida N, Otsuka Y, Kaneita Y, et al. factors related to alcohol consumption among Japanese physicians. Asia Pac J Public Health. 2018;30:296–306. doi: 10.1177/1010539518754539. [DOI] [PubMed] [Google Scholar]
- 68.Hughes PH, Brandenburg N, Baldwin DC, Jr, et al. Prevalence of substance use among US physicians. JAMA. 1992;267:2333–2339. [PubMed] [Google Scholar]
- 69.Marshall EJ. Doctors' health and fitness to practise: treating addicted doctors. Occup Med (Lond) 2008;58:334–340. doi: 10.1093/occmed/kqn081. [DOI] [PubMed] [Google Scholar]
- 70.Merlo LJ, Gold MS. Prescription opioid abuse and dependence among physicians: hypotheses and treatment. Harv Rev Psychiatry. 2008;16:181–194. doi: 10.1080/10673220802160316. [DOI] [PubMed] [Google Scholar]
- 71.Lutsky I, Hopwood M, Abram SE, Jacobson GR, Haddox JD, Kampine JP. Psychoactive substance use among American anesthesiologists: a 30-year retrospective study. Can J Anaesth. 1993;40:915–921. doi: 10.1007/BF03010092. [DOI] [PubMed] [Google Scholar]
- 72.Beaujouan L, Czernichow S, Pourriat JL, Bonnet F. Prévalence et facteurs de risque de l'addiction aux substances psychoactives en milieu anesthésique: résultats de l'enquête nationale. Ann Fr Anesth Reanim. 2005;24:471–479. doi: 10.1016/j.annfar.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 73.Berry CB, Crome IB, Plant M, Plant M. Substance misuse amongst anaesthetists in the United Kingdom and Ireland. The results of a study commissioned by the Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2000;55:946–952. doi: 10.1046/j.1365-2044.2000.01758.x. [DOI] [PubMed] [Google Scholar]
- 74.Firth-Cozens J, Greenhalgh J. Doctors' perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–1022. doi: 10.1016/s0277-9536(96)00227-4. [DOI] [PubMed] [Google Scholar]
- 75.Compton MT, Shim RS. The social determinants of mental health. Focus Am Psychiatr Publ. 2015;13:419–425. doi: 10.1176/appi.focus.18104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fouad FM, Sparrow A, Tarakji A, et al. Health workers and the weaponisation of health care in Syria: a preliminary inquiry for The Lancet–American University of Beirut Commission on Syria. Lancet. 2017;390:2516–2526. doi: 10.1016/S0140-6736(17)30741-9. [DOI] [PubMed] [Google Scholar]
- 77.Hansoti B, Kellogg DS, Aberle SJ, et al. Preparing emergency physicians for acute disaster response: a review of current training opportunities in the US. Prehosp Disaster Med. 2016;31:643–647. doi: 10.1017/S1049023X16000820. [DOI] [PubMed] [Google Scholar]
- 78.Hick JL, Biddinger PD. Novel coronavirus and old lessons—preparing the health system for the pandemic. N Engl J Med. 2020;382:e55. doi: 10.1056/NEJMp2005118. [DOI] [PubMed] [Google Scholar]
- 79.Harvey SB, Laird B, Henderson M, et al. National Clinical Assessment Service; London: 2009. The mental health of health care professionals: a review for the Department of Health.https://webarchive.nationalarchives.gov.uk/20130123201334/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_113540 [Google Scholar]
- 80.Harvey SB, Modini M, Joyce S, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med. 2017;74:301–310. doi: 10.1136/oemed-2016-104015. [DOI] [PubMed] [Google Scholar]
- 81.Lee RT, Lovell BL, Brotheridge CM. Tenderness and steadiness: relating job and interpersonal demands and resources with burnout and physical symptoms of stress in Canadian physicians. J Appl Soc Psychol. 2010;40:2319–2342. [Google Scholar]
- 82.Firth-Cozens J. Interventions to improve physicians' well-being and patient care. Soc Sci Med. 2001;52:215–222. doi: 10.1016/s0277-9536(00)00221-5. [DOI] [PubMed] [Google Scholar]
- 83.Petrie K, Crawford J, Shand F, Harvey SB. Workplace stress, common mental disorder and suicidal ideation in junior doctors. Intern Med J. 2020 doi: 10.1111/imj.15124. published online Nov 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tyssen R, Vaglum P. Mental health problems among young doctors: an updated review of prospective studies. Harv Rev Psychiatry. 2002;10:154–165. doi: 10.1080/10673220216218. [DOI] [PubMed] [Google Scholar]
- 85.Stansfeld SA, Fuhrer R, Shipley MJ, Marmot MG. Work characteristics predict psychiatric disorder: prospective results from the Whitehall II Study. Occup Environ Med. 1999;56:302–307. doi: 10.1136/oem.56.5.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Harvey SB, Sellahewa DA, Wang MJ, et al. The role of job strain in understanding midlife common mental disorder: a national birth cohort study. Lancet Psychiatry. 2018;5:498–506. doi: 10.1016/S2215-0366(18)30137-8. [DOI] [PubMed] [Google Scholar]
- 87.Siegrist J. In: The handbook of stress and health. Cooper CL, Quick JC, editors. John Wiley & Sons; Hoboken, NJ: 2017. The effort–reward imbalance model; pp. 24–35. [Google Scholar]
- 88.Milner A, Witt K, Spittal MJ, et al. The relationship between working conditions and self-rated health among medical doctors: evidence from seven waves of the Medicine In Australia Balancing Employment and Life (Mabel) survey. BMC Health Serv Res. 2017;17:609. doi: 10.1186/s12913-017-2554-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Tyssen R, Vaglum P. Mental health problems among young doctors: an updated review of prospective studies. Harv Rev Psychiatry. 2002;10:154–165. doi: 10.1080/10673220216218. [DOI] [PubMed] [Google Scholar]
- 90.Sen S, Kranzler HR, Krystal JH, et al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry. 2010;67:557–565. doi: 10.1001/archgenpsychiatry.2010.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Horton R. Why graduate medical schools make sense. Lancet. 1998;351:826–828. doi: 10.1016/S0140-6736(98)02290-9. [DOI] [PubMed] [Google Scholar]
- 92.Garrud P, McManus IC. Impact of accelerated, graduate-entry medicine courses: a comparison of profile, success, and specialty destination between graduate entrants to accelerated or standard medicine courses in UK. BMC Med Educ. 2018;18:250. doi: 10.1186/s12909-018-1355-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Arnetz BB. Psychosocial challenges facing physicians of today. Soc Sci Med. 2001;52:203–213. doi: 10.1016/s0277-9536(00)00220-3. [DOI] [PubMed] [Google Scholar]
- 94.Edwards N, Kornacki MJ, Silversin J. Unhappy doctors: what are the causes and what can be done? BMJ. 2002;324:835–838. doi: 10.1136/bmj.324.7341.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. The new generation of family physicians--career motivation, life goals and work-life balance. Swiss Med Wkly. 2008;138:305–312. doi: 10.4414/smw.2008.12473. [DOI] [PubMed] [Google Scholar]
- 96.Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368 doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 97.The Lancet COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107 doi: 10.1016/j.pnpbp.2021.110247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.WHO . World Health Organization; Geneva: 2016. Global strategy on human resources for health: workforce 2030. [Google Scholar]
- 102.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 103.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 104.Pham T, Bui L, Nguyen A, et al. The prevalence of depression and associated risk factors among medical students: an untold story in Vietnam. PLoS One. 2019;14 doi: 10.1371/journal.pone.0221432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grover S, Sahoo S, Bhalla A, Avasthi A. Psychological problems and burnout among medical professionals of a tertiary care hospital of North India: a cross-sectional study. Indian J Psychiatry. 2018;60:175–188. doi: 10.4103/psychiatry.IndianJPsychiatry_254_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gong Y, Han T, Chen W, et al. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: a cross-sectional study. PLoS One. 2014;9 doi: 10.1371/journal.pone.0103242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sadiq MS, Morshed NM, Rahman W, Chowdhury NF, Arafat S, Mullick MSI. Depression, anxiety, stress among postgraduate medical residents: a cross sectional observation in Bangladesh. Iran J Psychiatry. 2019;14:192–197. [PMC free article] [PubMed] [Google Scholar]
- 108.Erdur B, Ergin A, Turkcuer I, Parlak I, Ergin N, Boz B. A study of depression and anxiety among doctors working in emergency units in Denizli, Turkey. Emerg Med J. 2006;23:759–763. doi: 10.1136/emj.2006.035071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Atif K, Khan HU, Ullah MZ, Shah FS, Latif A. Prevalence of anxiety and depression among doctors; the unscreened and undiagnosed clientele in Lahore, Pakistan. Pak J Med Sci. 2016;32:294–298. doi: 10.12669/pjms.322.8731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Shawahna R, Hattab S, Al-Shafei R, Tab'ouni M. Prevalence and factors associated with depressive and anxiety symptoms among Palestinian medical students. BMC Psychiatry. 2020;20:244. doi: 10.1186/s12888-020-02658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ashkar K, Romani M, Musharrafieh U, Chaaya M. Prevalence of burnout syndrome among medical residents: experience of a developing country. Postgrad Med J. 2010;86:266–271. doi: 10.1136/pgmj.2009.092106. [DOI] [PubMed] [Google Scholar]
- 112.Malik AA, Bhatti S, Shafiq A, et al. Burnout among surgical residents in a lower-middle income country—are we any different? Ann Med Surg (Lond) 2016;9:28–32. doi: 10.1016/j.amsu.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Joyce S, Modini M, Christensen H, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med. 2016;46:683–697. doi: 10.1017/S0033291715002408. [DOI] [PubMed] [Google Scholar]
- 114.Petrie K, Joyce S, Tan L, et al. A framework to create more mentally healthy workplaces: a viewpoint. Aust N Z J Psychiatry. 2018;52:15–23. doi: 10.1177/0004867417726174. [DOI] [PubMed] [Google Scholar]
- 115.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92:129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 116.National Academies of Sciences, Engineering, and Medicine. National Academy of Medicine. Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being . The National Academies Press; Washington, DC: 2019. Taking action against clinician burnout: a systems approach to professional well-being; p. 332. [PubMed] [Google Scholar]
- 117.West CP, Dyrbye LN, Sinsky C, et al. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.9385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Goroll AH. Addressing burnout-focus on systems, not resilience. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.9514. [DOI] [PubMed] [Google Scholar]
- 119.Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-017858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Martin A, Chilton J, Gothelf D, Amsalem D. Physician self-disclosure of lived experience improves mental health attitudes among medical students: a randomized study. J Med Educ Curric Dev. 2020;7 doi: 10.1177/2382120519889352. 2382120519889352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Petrie K, Crawford J, Baker STE, et al. Interventions to reduce symptoms of common mental disorders and suicidal ideation in physicians: a systematic review and meta-analysis. Lancet Psychiatry. 2019;6:225–234. doi: 10.1016/S2215-0366(18)30509-1. [DOI] [PubMed] [Google Scholar]
- 122.Ruotsalainen J, Serra C, Marine A, Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health. 2008;34:169–178. doi: 10.5271/sjweh.1240. [DOI] [PubMed] [Google Scholar]
- 123.Scheepers RA, Emke H, Epstein RM, Lombarts KMJMH. The impact of mindfulness-based interventions on doctors' well-being and performance: a systematic review. Med Educ. 2020;54:138–149. doi: 10.1111/medu.14020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Tratton E, Lampit A, Choi I, Calvo RA, Harvey SB, Glozier N. Effectiveness of eHealth interventions for reducing mental health conditions in employees: a systematic review and meta-analysis. PLoS One. 2017;12 doi: 10.1371/journal.pone.0189904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Guille C, Zhao Z, Krystal J, Nichols B, Brady K, Sen S. Web-based cognitive behavioral therapy intervention for the prevention of suicidal ideation in medical interns: a randomized clinical trial. JAMA Psychiatry. 2015;72:1192–1198. doi: 10.1001/jamapsychiatry.2015.1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Brooks SK, Gerada C, Chalder T. The specific needs of doctors with mental health problems: qualitative analysis of doctor-patients' experiences with the Practitioner Health Programme. J Ment Health. 2017;26:161–166. doi: 10.1080/09638237.2016.1244712. [DOI] [PubMed] [Google Scholar]
- 127.Brooks SK, Gerada C, Chalder T. Doctors and dentists with mental ill health and addictions: outcomes of treatment from the Practitioner Health Programme. J Ment Health. 2013;22:237–245. doi: 10.3109/09638237.2012.734647. [DOI] [PubMed] [Google Scholar]
- 128.Panagioti M, Panagopoulou E, Bower P, et al. Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med. 2017;177:195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
- 129.Sinsky CA. Designing and regulating wisely: removing barriers to joy in practice. Ann Intern Med. 2017;166:677–678. doi: 10.7326/M17-0524. [DOI] [PubMed] [Google Scholar]
- 130.Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714–1721. doi: 10.1016/S0140-6736(09)61424-0. [DOI] [PubMed] [Google Scholar]
- 131.Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170:784. doi: 10.7326/M18-1422. [DOI] [PubMed] [Google Scholar]
- 132.Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med. 2017;177:1826–1832. doi: 10.1001/jamainternmed.2017.4340. [DOI] [PubMed] [Google Scholar]
- 133.National Academies of Sciences, Engineering, and Medicine. National Academy of Medicine. Committee on Systems Approaches to Improve Patient Care by Supporting Clinician Well-Being . The National Academies Press; Washington, DC: 2019. Taking action against clinician burnout: a systems approach to professional well-being; p. 332. [PubMed] [Google Scholar]
- 134.Gayed A, Milligan-Saville JS, Nicholas J, et al. Effectiveness of training workplace managers to understand and support the mental health needs of employees: a systematic review and meta-analysis. Occup Environ Med. 2018;75:462–470. doi: 10.1136/oemed-2017-104789. [DOI] [PubMed] [Google Scholar]
- 135.Milligan-Saville JS, Tan L, Gayed A, et al. Workplace mental health training for managers and its effect on sick leave in employees: a cluster randomised controlled trial. Lancet Psychiatry. 2017;4:850–858. doi: 10.1016/S2215-0366(17)30372-3. [DOI] [PubMed] [Google Scholar]