Abstract
Background:
People experiencing homelessness have diverse patterns of healthcare use. This study examined the distribution and determinants of healthcare encounters among adults with a history of homelessness.
Methods:
Administrative healthcare records were linked with survey data for a general cohort of adults with a history of homelessness and a cohort of homeless adults with mental illness. Binary and count models were used to identify factors associated with hospital admissions, emergency department visits and physician visits for comparison across the 2 cohorts.
Results:
During the 1-year follow-up period, a higher proportion of people in the cohort with a mental illness used any inpatient (27% vs 14%), emergency (63% vs 53%), or physician services (90% vs 76%) compared to the general homeless cohort. People from racialized groups were less likely use nearly all health services, most notably physician services. Other factors, such as reporting of a regular source of care, poor perceived general health, and diagnosed chronic conditions were associated with higher use of all health services except psychiatric inpatient care
Conclusion:
When implementing interventions for patients with the greatest health needs, we must consider the unique factors that contribute to higher healthcare use, as well as the barriers to healthcare access.
Keywords: Homeless persons, emergency department, physician services, hospital, healthcare utilization
Background
People experiencing homelessness are often exposed to harsh living conditions that increase their risk of poor health outcomes and premature mortality.1 The ability to manage chronic conditions may be further complicated by experiences of mental illness, physical comorbidities, and substance-related disorders.2 The stressful experiences of homelessness, coupled with chronic conditions and poor access to disease management, can contribute to an elevated need for health services. Notably, people experiencing homelessness are more likely to be hospitalized, visit the emergency department (ED), and visit a primary care provider compared to low-income controls.3 Homeless patients are also more likely to return to the ED or be readmitted to a psychiatric unit, and less likely to see a psychiatrist within 30 days of discharge, when compared with non-homeless patients.4 These findings may be a consequence of poor healthcare coordination at hospital discharge or may indicate a greater need for acute health services due to the complex health challenges experienced by people who are homeless.
While the average person experiencing homelessness is more likely to use health services than non-homeless controls, it is important to remember that healthcare use is not uniform. Instead, it is a relatively small group of people who use the most services.3,5 In a cohort of homeless adults in Toronto, Ontario, the top 10% of healthcare users accounted for over 60% of ED encounters and over 80% of hospitalizations over a 5-year observation period. Meanwhile, 5% of the sample did not use any healthcare services.3 For the group of the people experiencing homelessness who repeatedly use services, the healthcare system can be a useful place to intervene with tailored housing and support services that meet the needs of the individual. Provision of adequate supports could further reduce use of resource intensive services downstream. However, it is important to understand factors that are associated with frequent use of primary and acute health services among these individuals to ensure resources are adequately allocated and services are personalized to serve the patients with the greatest need.
People living with mental illness are an important subgroup to consider. Psychiatric illness is prevalent within the homeless population (30%-35%) and can worsen because of homelessness.2,6,7 People with a mental illness experiencing homelessness encounter barriers to adequate treatment which can further impede their ability to cope with their disorder and living circumstances. Reasons for unmet treatment needs include competing priorities, experiences of stigma and discrimination in healthcare settings, and limited access to health services.8 It is therefore important to recognize that people living with mental illness may have different risk factors that contribute to healthcare use compared to people without mental illness.
The literature on factors associated with health care use among people experiencing homelessness can be grouped into 3 study types based on the data available: surveys with self-report healthcare data, administrative records with limited data on individual-level characteristics, or data linkage of surveys with health records. In 2001, a cross-sectional study of people experiencing homelessness in the United States was conducted to identify factors associated with higher odds of a self-report hospitalization.9 Although many confidence intervals crossed the null value (n = 2974), a number of factors were associated with higher odds of past year hospitalization, including female sex, veteran status, presence of insurance, a higher number of chronic conditions, mental health conditions, alcohol abuse, and drug abuse.9 In later years, the use of administrative health records led to greater focus on diagnosed conditions, with one study finding that mental illness, physical conditions, and health insurance were associated with higher rates of hospital admissions.10 Many studies focus on a single type of healthcare utilization and apply seemingly arbitrary definitions to identify “frequent users” (eg, emergency department classifications ranged from ⩾3 to ⩾12 visits in a year) .9,11,12 Fewer studies examin factors associated with physician visits, and most existing work is limited to self-report data.9,11,13
It can be challenging to draw meaningful comparisons across studies due to differences in study inclusion criteria, use of survey data versus administrative records, operationalization of healthcare utilization (eg, any vs none, frequent use categories, number of visits), choice of statistical analysis technique, and access to health insurance. For instance, studies that are restricted to patients with mental illness may not be applicable to a more general population of people with experiences of homelessness.
This study aimed to expand our understanding of important factors that are associated with healthcare use, such as psychiatric and non-psychiatric hospitalizations, ED visits, and physician visits among people experiencing homelessness. Survey data from 2 cohort studies were linked with administrative health records to examine the determinants of healthcare encounters among adults with a history of homelessness. We examined data from a representative cohort of the general adult homeless population and a cohort of individuals with a diagnosed mental illness.
Methods
Survey data from the At Home/Chez Soi study and the Health and Housing in Transition study were linked with administrative health records in Ontario, Canada. Research ethics approval was obtained from the St. Michael’s Hospital Research Ethics Board (REB) for the Toronto study sites and the University of Ottawa REB for the Ottawa site. Additional approval was obtained from St. Michael’s Hospital REB to combine these study samples and use their linked data for this analysis.
Survey Data
At Home/Chez Soi Study
The At Home/Chez Soi study was a randomized controlled trial of Housing First, a supportive housing intervention for people experiencing homelessness with a mental illness.14 The trial was conducted from 2009 to 2013 in Toronto, Vancouver, Winnipeg, Montreal, and Moncton. The eligibility criteria have previously been described.15 Briefly, participants were at least 18 years old, living with a diagnosed mental illness, and experiencing homelessness. Following enrollment (2009-2011), participants were stratified by their level of mental health needs prior to being randomized to receive either Housing First or treatment as usual.14-16
The Housing First intervention was a modified version of the Pathways to Housing model from New York City.14 Rent supplements were provided to offset the cost of living so no more than 30% of each participant’s income went toward housing. The high needs participants received support services from an Assertive Community Treatment team, with a ratio of 10 participants to 1 staff who offered services 24 hours a day for 7 days a week. The moderate needs participants were given a less expensive Intensive Case Management approach, with a ratio of 20 participants to 1 staff who offered services 12 hours a day for 7 days a week.
In comparison, the treatment as usual condition approximated real world circumstances where the Housing First intervention did not exist. Participants could access existing resources in their community, which may include housing and support services, but availability was not guaranteed.14 For the remainder of this article, participants from the At Home/Chez Soi study will be referred to as “the cohort with a mental illness.”
Health and Housing in Transition study
The Health and Housing in Transition study was a longitudinal study of single adults with a history of homelessness. This prospective cohort study was conducted between 2009 and 2014 in Toronto, Ottawa, and Vancouver. To be eligible for inclusion, participants were either homeless, defined as living in a shelter, public place, vehicle, abandoned building, or someone else’s place, or vulnerably housed, defined as living in their own room, apartment, or place, having experienced homelessness in the past year.17,18 For the remainder of this paper, participants from the Health and Housing in Transition study will be referred to as the “general homeless cohort.”
Administrative healthcare data
Ontario residents are eligible for health insurance under a universal single payer program called the Ontario Health Insurance Plan (OHIP). Services covered by OHIP include primary care and hospital services for all residents, and prescription drug costs for residents on social assistance or disability pension. Provincial data on these health services are collected and stored at ICES (formerly the Institute for Clinical Evaluative Sciences), a not-for-profit research institute that is authorized to securely collect Ontario’s health-related data for the purpose of health system evaluation, analysis, and decision support. All residents are assigned a unique ICES key number based on their health card number, name, and date of birth. This unique identifier is stored in the Registered Persons Database and enables linkage across internal and external datasets at ICES.
Participants
Participants from the Ontario sites of the At Home/Chez Soi study (Toronto) and the Health and Housing in Transition study (Toronto and Ottawa) were eligible for inclusion if they provided informed consent to link their survey data with administrative health records. Deterministic linkage was used to match the participant’s health card number with an associated ICES key number in the Registered Persons Database. This linkage connected the survey data with a set of healthcare databases including the Canadian Institute for Health Information Discharge Abstract Database (CIHI-DAD), the Ontario Mental Health Reporting System (OMHRS), the National Ambulatory Care Reporting System (NACRS), and the Ontario Health Insurance Plan (OHIP). All datasets were linked using unique encoded identifiers and analyzed at ICES.
Independent variables: Predisposing, enabling, and need factors
The Behavioral Model for Vulnerable Populations was used to identify variables of interest for this study, as described previously.19,20 This framework describes factors related to health status and health-related behaviors of vulnerable populations.21 Predisposing factors include sociodemographic information (age, gender, marital status, racial identity, education, employment), housing history, mental illness, substance use, criminal behavior, and victimization. Housing history comprised homeless status at enrollment (homeless versus precariously or vulnerably housed, based on inclusion criteria) and duration of homelessness prior to enrollment. Mental illness was classified as psychotic disorders, other mental disorders, or no mental disorder based on diagnostic codes from administrative health records. For the At Home/Chez Soi participants, the Mini International Neuropsychiatric Interview supplemented the administrative data. Substance use in the past 12 months was defined using the MINI and Alcohol Use Disorders Identification Test (AUDIT) for problematic alcohol use and the MINI and Drug Abuse Screening Test (DAST-10) for problematic drug use. Criminal behavior was defined by experiences of incarceration or arrests in the past 6 to 12 months. Victimization included reports of physical or sexual victimization experienced in the past 6 to 12 months.
Enabling or impeding factors comprise personal and community resources, such as region of residence, regular source of care, perceived barriers to care, and competing needs (eg, an indicator of food insecurity). Need factors include perceived health and self-reported or observed health conditions. The list of predisposing, enabling, and need factors are described in Supplemental Table S1.20 Data on these factors were either collected from baseline surveys or administrative healthcare records during the 1-year period prior to enrollment.
Dependent variables: Hospitalizations, ED visits, and physician visits
Healthcare encounter data was ascertained from administrative healthcare records during the 1-year period after enrollment. Psychiatric hospitalizations to a designated mental health bed were ascertained from OMHRS, while the remaining psychiatric and non-psychiatric hospitalizations were identified from the CIHI-DAD database. ED visits were reported in the NACRS database. Physician visits including primary, medical specialist, or mental health specialist visits were reported in OHIP. The OHIP database also captures shadow billings for physician services provided under the capitation model or at shelters. Shadow billing enables service delivery to be tracked when physicians provide services that are renumerated outside the fee-for-service system However, physicians at community health centers are not required to submit shadow billing. Data on physician encounters may be incomplete for people who access services at these centers.
Cohort description
The cohort characteristics were compared across the 2 studies using Analysis of Variance (mean) and Kruskal-Wallis tests (median) for continuous variables and chi-squared tests for binary variables (α = .05). We present the proportion of each type of encounter that was attributed to psychiatric and non-psychiatric medical conditions.
Analysis strategy
Most individuals were not admitted to an inpatient hospital unit even once during the follow-up period (73% for the cohort with a mental illness and 86% for the general homeless cohort). Therefore, the outcomes of psychiatric and non-psychiatric hospital admissions were modeled as binary variables to estimate risk ratios using a modified Poisson regression model with a robust error estimator.22 ED and physician visits are more common and were modeled as count variables using generalized linear models with a negative binomial distribution to estimate rate ratios that account for overdispersion in the data.
As the objectives of this work were not causal, the main reported models were unadjusted to describe real world situations where individual characteristics are interconnected, rather than adjusting away important effects.23,24 Since future research may assess a causal relationship between these exposures and healthcare utilization outcomes, age adjusted and fully adjusted models were reported as part of the supplementary documentation.
An additional consideration was the possible impact of the Housing First intervention on these findings within the cohort with a mental illness. A sensitivity analysis was conducted for participants of the At Home/Chez Soi study to examine whether the findings changed following adjustment for the intervention. An indicator variable for the intervention was included in each model. Finally, approximately half of the general cohort with a history of homelessness had a mental illness. A sensitivity analysis was restricted to patients without a mental illness to ensure the experience of having a mental illness was not driving the other observed associations.
Missing data was handled with a 2-step process. First, administrative healthcare records were used to fill in missing survey data where applicable (eg, past year service use for alcohol abuse or dependence was used as a proxy for problematic alcohol use). For the unadjusted analyses, missing data were reported as a characteristic and modeled as a predictor. For the secondary, fully adjusted models, multiple imputation methods were applied with bootstrapped modeling techniques to ensure accurate estimation of the confidence intervals.25 Multiple imputation was conducted using the mi, fcs command in SAS version 9.4, with 100 imputed datasets combined using the mianalyze command.26 All analyses were completed using SAS software version 9.4.27
Results
Cohort characteristics
Participant inclusion is described in Supplemental Figure S1. For the cohort with a mental illness, 575 participants were enrolled in the Toronto site of the At Home/Chez Soi study. Of these, 8 people did not consent to data linkage and 42 could not be linked due to insufficient identifiers. The final cohort included 525 participants (91% linkage). For the general homeless cohort, there were 796 participants enrolled in the Toronto and Ottawa sites of the Health and Housing in Transition study. Of these, 11 people did not consent to data linkage and 108 could not be linked. Therefore, 677 participants were successfully linked to administrative records (85% linkage). The final cohort was reduced to 655 after removing the 22 duplicate records for participants who were also in the cohort with a mental illness.
Table 1 describes the cohort characteristics. On average, the cohort with a mental illness was younger (40 vs 43 years old), and more likely to report a regular source of care (67% vs 59%), perceive a barrier to care (40% vs 35%), and report not enough food to eat (52% vs 32%). They were also more likely to access non-mental health acute care in the past year (62% vs 47%), and report poor or fair health (51% vs 42%) compared to the general homeless cohort. Due to enrollment criteria, the participants from the cohort with a mental illness were also more likely to reside in Toronto (100% vs 51%), identify as Black or another racialized group (63% vs 35%), have a psychotic disorder (43% vs 13%), be absolutely homeless at enrollment (93% vs 50%), and access acute mental health care in the past year (53% vs 20%). Missing data was more common in the cohort with a mental illness than the general homeless cohort (15% vs 8%). For both studies, lifetime duration of homelessness had the most missing data (4-5%) and administrative data variables had the least missing data (0%).
Table 1.
Sample characteristics for the cohort with a mental illness and the general homeless cohort.
| Characteristics | Cohort with a mental illness (n = 525) | General homeless cohort (n = 655) | χ2 testa
P-value |
Missing data |
|---|---|---|---|---|
| Predisposing factors | ||||
| Age | - | |||
| Mean ± SE | 39.9 ± 11.8 | 42.9 ± 10.5 | <.001 | |
| Median (IQR) | 41 (30-48) | 44 (36-50) | <.001 | |
| Age group | <.001 | - | ||
| 18-34 | 34.9% | 21.8% | ||
| 35-49 | 44.4% | 51.3% | ||
| 50+ | 20.8% | 26.9% | ||
| Genderb | .826 | - | ||
| Female | 30.1% | 30.7% | ||
| Male | 69.9% | 69.3% | ||
| Marital status | <.001 | 2-3% | ||
| Single, never married | 69.5% | 60.6% | ||
| Widow, separated, divorced | 27.5% | 28.0% | ||
| Partnered, married | 3.0% | 11.3% | ||
| Race | <.001 | 1-2% | ||
| Black | 32.4% | 12.0% | ||
| Other racialized groups | 30.9% | 23.2% | ||
| White | 36.8% | 64.8% | ||
| Place of birth | <.001 | 1-2% | ||
| Canada | 55.0% | 81.8% | ||
| Education | .058 | 2-3% | ||
| Graduated high school | 51.3% | 56.9% | ||
| Employment status | <.001 | 2-3% | ||
| Currently employed | 4.2% | 10.4% | ||
| Housing statusc | <.001 | - | ||
| Precariously or vulnerably housed | 7.4% | 50.1% | ||
| Homeless | 92.6% | 49.9% | ||
| Years spent homeless | 4-5% | |||
| Mean ± SE | 5.21 ± 6.10 | 5.32 ± 6.22 | .760 | |
| Median (IQR) | 3 (1-7) | 3 (1-7) | .954 | |
| ⩾2 years spent homeless | 61.7% | 58.6% | .282 | |
| Criminal behavior | .455 | 1-2% | ||
| (Past 6-12 months) | 39.2% | 37.1% | ||
| Victimization | .451 | 2-3% | ||
| (Past 6-12 months) | 35.1% | 37.2% | ||
| Diagnosed mental illnessd | <.001 | - | ||
| Psychotic disorder | 43.0% | 13.3% | ||
| Other disorder | 57.0% | 25.6% | ||
| No disorder | - | 61.1% | ||
| Problematic alcohol used | <.001 | - | ||
| (Past 12 months) | 45.1% | 20.2% | ||
| Problematic drug used | <.001 | - | ||
| (Past 12 months) | 50.7% | 35.9% | ||
| Smoking status | ||||
| Current, daily smoker | 65.1% | 75.5% | <.001 | 2-3% |
| Enabling factors | ||||
| Region | <.001 | - | ||
| Toronto | 100.0% | 50.8% | ||
| Ottawa | - | 49.2% | ||
| Regular source of care | 66.7% | 59.2% | .009 | 1-2% |
| Perceived barrier to care | .08 | 2-3% | ||
| (Past 6-12 months) | 40.2% | 35.2% | ||
| Food insecurity | <.001 | 1-2% | ||
| (Not enough food to eat) | 51.8% | 32.2% | ||
| Acute mental healthcaree
(Past 12-months) |
<.001 | - | ||
| Yes | 52.8% | 20.2% | ||
| No | 47.2% | 79.8% | ||
| Acute non-mental healthcaree
(Past 12-months) |
<.001 | - | ||
| Yes | 62.1% | 47.0% | ||
| No | 37.9% | 53.0% | ||
| Need factors | ||||
| Perceived general health | .003 | 1-2% | ||
| Poor | 19.2% | 13.1% | ||
| Fair | 31.7% | 28.9% | ||
| Good, very good, excellent | 49.1% | 58.0% | ||
| Diagnosed chronic conditions (administrative data) | - | |||
| Mean ± SE | 0.59 ± 0.84 | 0.57 ± 0.85 | .672 | |
| Median (IQR) | 0 (0-1) | 0 (0-1) | .489 | |
| Self-report chronic conditionsf
(Survey data) |
1-2% | |||
| Mean ± SE | 1.01 ± 1.28 | 1.06 ± 1.25 | .511 | |
| Median (IQR) | 1 (0-1) | 1 (0-2) | .298 | |
| Any missing datag | 15.4% | 7.9% | <.001 | - |
P-values were calculated using Analysis of Variance (mean) and Kruskal-Wallis tests (median) for continuous variables, and chi-squared tests for binary variables. The significance level for all tests was α= .05.
Twelve participants identified as transgender. Due to small numbers, they were classified according to sex.
Vulnerable housing was defined as current residence in one’s own room, apartment, or place with an experience of homelessness or 2 or more moves in the past 12 months. Precarious housing was defined as a primary residence in a single room occupancy, rooming house, hotel, or motel, with 2 or more episodes of absolute homelessness in the past year.
Mental illness was classified based on administrative diagnostic codes in the 1-year prior to index date. The Mini International Neuropsychiatric Interview supplemented the administrative data for the cohort with a mental illness, as mental illness was a requirement of study enrollment.
Acute healthcare includes emergency department visits or inpatient hospital admissions.
Self-reported chronic conditions were restricted to the conditions captured in administrative databases. These include asthma, hypertension, myocardial infarction or heart disease, chronic obstructive pulmonary disorder, bowel disorders, HIV, diabetes, and cancer.
Missing data does not include self-reported chronic conditions as administrative data
Distribution of healthcare encounters
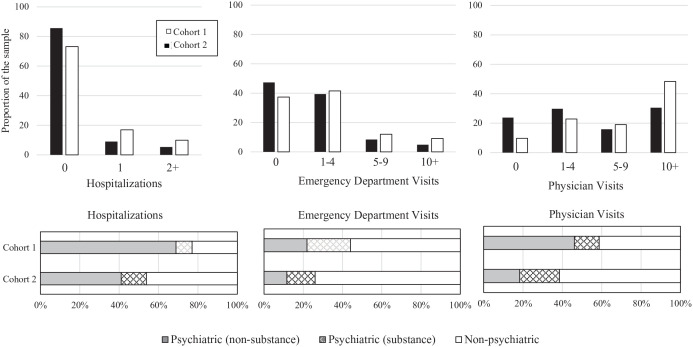
The cohort with a mental illness used services more often than the general homeless cohort (Figure 1). For instance, a higher proportion of the cohort with mental illness had 2 or more hospitalizations (10% vs 5%), 5 or more emergency department visits (21% vs 13%) and 5 or more physician visits (67% vs 46%). In comparison, more people in the general homeless cohort had no hospitalizations (86% vs 73%), emergency department visits (47% vs 37%) or physician visits (24% vs 10%) during the 1-year follow-up period.
Figure 1.
The distribution of healthcare encounters for the cohort with a mental illness and the general homeless cohort during a 1-year period.
Cohort 1 = Cohort with a mental illness (At Home/Chez Soi study).
Cohort 2 = General homeless cohort (Health and Housing in Transition study.
Determinants of healthcare utilization
Associations are reported in Table 2 (risk of hospitalizations) and Table 3 (rates of ED visits and physician visits). Certain predisposing, enabling, and need factors were associated with multiple types of health services. Race is a predisposing factor that has service use implications for people experiencing homelessness. In both cohorts, Black participants were approximately 40% less likely to be admitted to a non-psychiatric hospital unit, and they had lower rates of emergency department visits (25%-34% lower rate) and physician visits (32%-50% lower rate) than white participants. People from other racialized groups had nearly 20% lower risk of psychiatric hospitalization and 25% lower rate of physician visits. Participants born outside Canada had lower risk of nearly all healthcare encounters compared to Canadian-born participants, with the strongest associations reported for emergency department visits (27%-53% lower rate).
Table 2.
Unadjusted risk ratios for the predisposing, enabling, and need factors associated with hospitalizations among the cohort with a mental illness and the general homeless cohort.
| Study |
Cohort with a mental illness (n = 525) |
General homeless cohort (n = 655) |
||
|---|---|---|---|---|
| Health service | Psychiatric hospitalizations | Non-psychiatric hospitalizations | Psychiatric hospitalizations | Non-psychiatric hospitalizations |
| Predisposing factors | ||||
| Age | ||||
| Per 1-year increase | 0.98 (0.97, 1.00) | 1.04 (1.01, 1.06) | 1.00 (0.97, 1.02) | 1.03 (1.00, 1.05) |
| Age group | ||||
| 18-34 | ||||
| 35-49 | 0.82 (0.56, 1.19) | 1.01 (0.47, 2.18) | 1.42 (0.66, 3.04) | 2.02 (0.79, 5.17) |
| 50+ | 0.69 (0.42, 1.14) | 2.01 (0.95, 4.26) | 0.84 (0.33, 2.13) | 3.00 (1.16, 7.79) |
| Gender | ||||
| Female | 1.44 (1.02, 2.03) | 1.12 (0.61, 2.06) | 1.48 (0.85, 2.58) | 1.87 (1.12, 3.13) |
| Marital status | ||||
| Single, never married | 1.35 (0.89, 2.06) | 0.46 (0.26, 0.82) | 0.77 (0.44, 1.32) | 0.85 (0.50, 1.42) |
| Race | ||||
| Black | 0.95 (0.64, 1.41) | 0.57 (0.26, 1.23) | 0.48 (0.15, 1.51) | 0.60 (0.22, 1.64) |
| Other racialized groups | 0.78 (0.51, 1.19) | 1.06 (0.56, 2.01) | 0.82 (0.42, 1.62) | 0.93 (0.50, 1.74) |
| Place of birth | ||||
| Not Canada | 0.96 (0.68, 1.37) | 0.87 (0.48, 1.57) | 0.77 (0.35, 1.67) | 0.47 (0.19, 1.15) |
| Education | ||||
| Graduated high school | 1.11 (0.78, 1.59) | 1.21 (0.67, 2.19) | 0.70 (0.40, 1.20) | 0.79 (0.47, 1.32) |
| Employment | ||||
| Currently employed | 0.47 (0.13, 1.79) | 1.18 (0.31, 4.56) | 0.57 (0.18, 1.80) | 0.52 (0.17, 1.61) |
| Homeless status | ||||
| Homeless | 2.07 (0.80, 5.31) | 1.65 (0.41, 6.55) | 1.00 (0.58, 1.73) | 0.83 (0.49, 1.39) |
| Years spent homeless | ||||
| Per 1-year increase | 0.97 (0.94, 1.01) | 1.00 (0.96, 1.05) | 1.02 (0.98, 1.06) | 1.01 (0.97-1.04) |
| ⩾2 years spent homeless | 0.89 (0.63, 1.25) | 1.16 (0.63, 2.11) | 1.08 (0.62, 1.88) | 1.26 (0.74, 2.17) |
| Diagnosed mental illness | ||||
| Psychotic disorder | 1.25 (0.89, 1.75) | 1.15 (0.65, 2.04) | 3.69 (1.86, 7.29) | 0.68 (0.30, 1.54) |
| Other disorder (reference) | - | - | - | - |
| No disorder | - | - | 0.61 (0.29, 1.29) | 0.55 (0.31, 0.95) |
| Substance use | ||||
| Problematic alcohol use | 0.88 (0.63, 1.24) | 0.96 (0.54, 1.71) | 1.32 (0.71, 2.47) | 2.21 (1.31, 3.75) |
| Problematic drug use | 0.76 (0.54, 1.07) | 0.77 (0.43, 1.37) | 1.39 (0.80, 2.40) | 1.08 (0.64, 1.84) |
| Current daily smoker | 0.76 (0.53, 1.08) | 0.93 (0.51, 1.71) | 0.98 (0.52, 1.83) | 1.37 (0.70, 2.66) |
| Criminal behavior | ||||
| (Past 6-12 month) | 1.12 (0.79, 1.60) | 0.72 (0.38, 1.36) | 0.70 (0.38, 1.28) | 1.64 (0.98, 2.74) |
| Victimization | ||||
| (Past 6-12 month) | 1.11 (0.77, 1.59) | 1.94 (1.08, 3.49) | 1.11 (0.63, 1.93) | 1.29 (0.77, 2.17) |
| Enabling factors | ||||
| Regular source of care | ||||
| 0.81 (0.57, 1.16) | 1.36 (0.70, 2.64) | 0.88 (0.51, 1.53) | 2.96 (1.51, 5.78) | |
| Perceived barrier to care | ||||
| (Past 6-12 month) | 0.77 (0.53, 1.11) | 0.77 (0.41, 1.43) | 1.30 (0.74, 2.28) | 1.01 (0.58, 1.74) |
| Food insecurity | ||||
| (Not enough food to eat) | 0.81 (0.57, 1.15) | 1.31 (0.72, 2.39) | 0.87 (0.47, 1.62) | 1.08 (0.63, 1.87) |
| Acute mental health care | ||||
| (Past 12 month) | 5.49 (3.27, 9.22) | 1.24 (0.70, 2.22) | 4.68 (2.74, 7.99) | 2.81 (1.69, 4.69) |
| Acute non-mental health care | ||||
| (Past 12 month) | 2.11 (1.39, 3.21) | 2.67 (1.26, 5.64) | 1.58 (0.91, 2.74) | 1.86 (1.09, 3.17) |
| Need factors | ||||
| Perceived general health | ||||
| Fair | 0.61 (0.40, 0.95) | 1.91 (0.94, 3.86) | 1.19 (0.66, 2.16) | 1.82 (1.00, 3.30) |
| Poor | 0.84 (0.53, 1.33) | 2.36 (1.12, 4.99) | 0.82 (0.32, 2.06) | 2.74 (1.43, 5.24) |
| Diagnosed conditions | ||||
| 1 | 0.89 (0.60, 1.32) | 1.62 (0.81, 3.20) | 0.70 (0.32, 1.50) | 1.22 (0.64, 2.31) |
| 2 | 0.72 (0.38, 1.36) | 2.73 (1.29, 5.77) | 1.88 (0.90, 3.94) | 2.28 (1.12, 4.63) |
| 3+ | 0.76 (0.27, 2.19) | 2.88 (0.93, 8.88) | 2.13 (0.80, 5.62) | 2.86 (1.19, 6.86) |
| Self-reported conditions | ||||
| 1 | 0.81 (0.54, 1.22) | 1.80 (0.85, 3.78) | 1.08 (0.56, 2.11) | 0.82 (0.39, 1.73) |
| 2 | 0.79 (0.43, 1.46) | 1.40 (0.47, 4.18) | 1.30 (0.59, 2.87) | 1.37 (0.62, 3.05) |
| 3+ | 0.57 (0.30, 1.09) | 3.07 (1.42, 6.65) | 1.14 (0.49, 2.62) | 2.92 (1.57, 5.42) |
| Missing data | 1.92 (1.24, 3.00) | 0.58 (0.14, 2.30) | 0.76 (0.24, 2.35) | 1.18 (0.49, 2.84) |
Table 3.
Unadjusted rate ratio estimates for the predisposing, enabling, and need factors associated with emergency department visits or physician visits among the cohort with a mental illness and the general homeless cohort.
| Study |
Cohort with a mental illness (n = 525) |
General homeless cohort (n = 655) |
||
|---|---|---|---|---|
| Health service | Emergency department visits | Physician visits | Emergency department visits | Physician visits |
| Predisposing factors | ||||
| Age | ||||
| Per 1-year increase | 0.98 (0.97, 1.00) | 1.01 (1.00, 1.02) | 1.00 (0.98, 1.01) | 0.99 (0.98, 1.00) |
| Age group | ||||
| 18-34 | - | - | - | - |
| 35-49 | 0.76 (0.51, 1.12) | 1.07 (0.86, 1.35) | 1.03 (0.69, 1.54) | 1.13 (0.81, 1.59) |
| 50+ | 0.64 (0.41, 1.00) | 1.19 (0.89, 1.60) | 0.94 (0.59, 1.51) | 0.81 (0.58, 1.15) |
| Gender | ||||
| Female | 0.76 (0.49, 1.18) | 1.33 (1.08, 1.64) | 1.55 (1.11, 2.16) | 1.14 (0.88, 1.47) |
| Marital status | ||||
| Single, never married | 1.38 (0.93, 2.04) | 0.78 (0.63, 0.97) | 1.08 (0.80, 1.45) | 1.12 (0.86, 1.46) |
| Race | ||||
| Black | 0.66 (0.44, 0.98) | 0.68 (0.54, 0.85) | 0.75 (0.44, 1.28) | 0.50 (0.37, 0.68) |
| Other racialized groups | 1.09 (0.57, 2.09) | 0.77 (0.61, 0.97) | 1.00 (0.70, 1.43) | 0.75 (0.55, 1.03) |
| Place of birth | ||||
| Outside Canada | 0.47 (0.31, 0.73) | 0.84 (0.70, 1.02) | 0.73 (0.48, 1.11) | 0.90 (0.67, 1.22) |
| Education | ||||
| Graduated high school | 0.61 (0.38, 0.97) | 1.15 (0.95, 1.40) | 0.72 (0.52, 0.98) | 0.96 (0.74, 1.24) |
| Employment | ||||
| Currently employed | 0.45 (0.23, 0.89) | 0.94 (0.36, 2.43) | 1.01 (0.63, 1.61) | 0.57 (0.35, 0.93) |
| Housing status | ||||
| Homeless | 1.56 (0.91, 2.60) | 0.89 (0.63, 1.25) | 1.21 (0.88, 1.64) | 0.74 (0.57, 0.95) |
| Years spent homeless | ||||
| Per 1-year increase | 1.04 (0.99, 1.10) | 0.98 (0.97, 1.00) | 1.01 (0.99, 1.03) | 0.99 (0.97, 1.00) |
| ⩾2 year spent homeless | 1.50 (0.97, 2.29) | 0.80 (0.66, 0.98) | 1.20 (0.86, 1.66) | 1.10 (0.85, 1.43) |
| Criminal behavior (Past 6-12 month) |
1.54 (0.91, 2.60) | 1.01 (0.83, 1.22) | 1.43 (1.04, 1.98) | 1.25 (0.96, 1.63) |
| Victimization (Past 6-12 month) |
1.29 (0.92, 1.82) | 1.08 (0.88, 1.31) | 1.43 (1.04, 1.97) | 1.14 (0.87, 1.48) |
| Diagnosed of mental illness | ||||
| Psychotic disorder | 1.28 (0.78, 2.11) | 0.91 (0.75, 1.10) | 1.28 (0.81, 2,04) | 0.99 (0.72, 1.35) |
| Other disorder (reference) | - | - | - | - |
| No disorder | - | - | 0.46 (0.33, 0.64) | 0.41 (0.31, 0.55) |
| Substance use | ||||
| Problematic alcohol use | 2.22 (1.45, 3.42) | 1.00 (0.82, 1.21) | 2.41 (1.69, 3.44) | 0.94 (0.70, 1.27) |
| Problematic drug use | 1.63 (1.03, 2.57) | 1.18 (0.97, 1.43) | 1.53 (1.12, 2.10) | 3.45 (2.78, 4.28) |
| Current daily smoker | 0.74 (0.41, 1.34) | 0.86 (0.70, 1.05) | 0.59 (0.40, 0.87) | 1.26 (0.97, 1.65) |
| Enabling factors | ||||
| Regular source of care | 1.25 (0.79, 1.98) | 1.55 (1.25, 1.93) | 1.30 (0.92, 1.85) | 1.71 (1.28, 2.28) |
| Perceived barrier to care (Past 6-12 month) |
0.79 (0.50, 1.23) | 1.13 (0.92, 1.38) | 1.17 (0.81, 1.69) | 1.42 (1.09, 1.84) |
| Food insecurity (Not enough food) |
1.37 (0.85, 2.21) | 0.87 (0.72, 1.06) | 0.90 (0.65, 1.23) | 1.40 (1.08, 1.83) |
| Acute mental healthcare (Past 12 month) |
4.55 (3.18, 6.50) | 1.45 (1.20, 1.76) | 3.17 (2.32, 4.32) | 1.71 (1.32, 2.21) |
| Acute non-mental health care (Past 12 month) |
4.68 (3.26, 6.72) | 1.47 (1.20, 1.80) | 4.18 (3.14, 5.57) | 1.96 (1.52, 2.54) |
| Need factors | ||||
| Perceived general health | ||||
| Fair | 0.79 (0.53, 1.20) | 1.13 (0.90, 1.42) | 1.17 (0.81, 1.69) | 1.35 (1.02, 1.80) |
| Poor | 1.66 (0.77, 3.59) | 1.23 (0.96, 1.57) | 1.43 (0.98, 2.09) | 1.95 (1.36, 2.78) |
| Diagnosed conditions (Administrative records) |
||||
| 1 | 1.58 (0.81, 3.09) | 1.41 (1.14, 1.73) | 1.41 (0.99, 2.01) | 1.53 (1.13, 2.06) |
| 2 | 1.52 (0.91, 2.54) | 1.91 (1.40, 2.62) | 1.75 (1.19, 2.55) | 1.38 (0.90, 2.11) |
| 3+ | 1.46 (0.82, 2.62) | 1.33 (0.95, 1.87) | 2.36 (0.98, 5.69) | 2.29 (1.58, 3.30) |
| Self-reported conditions (Survey data) |
||||
| 1 | 0.87 (0.58, 1.31) | 1.06 (0.85, 1.33) | 1.65 (1.11, 2.44) | 1.43 (1.03, 1.99) |
| 2 | 1.10 (0.60, 2.00) | 1.31 (0.88, 1.97) | 1.21 (0.79, 1.85) | 2.12 (1.48, 3.03) |
| 3+ | 1.80 (0.68, 4.77) | 1.49 (1.16, 1.92) | 2.06 (1.31, 3.23) | 1.87 (1.30, 2.68) |
| Missing data | 2.67 (0.88, 8.11) | 0.78 (0.54, 1.12) | 0.95 (0.56, 1.61) | 0.84 (0.53, 1.33) |
Enabling factors, such as regular source of care and past year acute service use, were associated with multiple forms of healthcare utilization as well. Participants in the general homeless cohort who reported having a regular source of care were nearly 3 times more likely to have a non-psychiatric hospitalization. In both cohorts, they also had higher rates of emergency department (25%-30% higher) and physician visits (55%-71% higher) compared to people who did not report a regular source of care. Use of acute services in the past year were also important predictors of future healthcare use. The strongest associations were a nearly 5 times higher risk of psychiatric hospitalization following use of mental health acute services and a nearly 4 times higher rate of emergency department visits following use of non-mental health acute services.
Finally, the need factors that were associated with many types of health services utilization were poor perceived health and number of chronic conditions. People with 3 or more chronic conditions or poor perceived health had nearly 3 times higher risk of non-psychiatric hospitalization, and up to 2 times higher rate of emergency department and physician visits than people with no chronic conditions or good/very good/excellent perceived health.
Sensitivity analyses
Supplemental Table S2 reports the risk ratio and rate ratio estimates for the cohort with a mental illness following adjustment for the Housing First intervention. There were no notable changes in the findings after adjusting for the intervention. In the fully adjusted models, some of the findings were attenuated (Supplemental Tables S3- S6). For instance, the associations for past year acute mental healthcare were attenuated toward the null but remained strongly associated with risk of psychiatric hospitalization and rate of ED visits.
Supplemental Table S7 reports the sensitivity analysis restricted to participants with no mental illness in the general homeless cohort. Hospitalizations were grouped into one category since few participants in this subgroup were admitted to hospital during the follow-up period. Many factors remained associated with healthcare utilization when restricted to participants with no mental illness, but there were a few noted differences as well. Older age was strongly associated with hospitalizations, reaching 3 times higher risk of any hospitalization among participants 35 to 49 or 50+ years old compared to 18- to 34-year old. Females had higher risk of hospitalizations and higher rates of ED or physician visits compared to male participants, but the relative rate of ED visits was attenuated in this analysis. In all analyses, Black participants were less likely to be admitted to hospital, visit the ED, or visit a physician. For participants from other racialized groups, the rates of ED visits were even higher than white participants among those without mental illness. Problematic alcohol and drug use were associated with risk of hospitalization and rate of ED visits, with problematic drug use remaining strongly associated with the rate of physician visits. Criminal behavior was not associated with hospitalization among participants without mental illness; however, it remained associated with ED visits and physician visits. The association for victimization and ED visits was stronger for participants without a mental illness, but the association for physician visits was closer to the null value. Participants who reported a regular source of care or a perceived barrier to care had higher rate of ED visits and physician visits, as did participants with acute mental or non-mental healthcare in the past year. Acute healthcare was also strongly associated with higher risk of hospitalization. Finally, poor perceived general health and number of chronic conditions remained strongly associated with high use of services.
Discussion
Summary of main findings
As homelessness persists in Canada and globally, it is necessary to implement tailored solutions to address individual needs. The healthcare system is an important point of intervention for many people experiencing homelessness, especially those with complex mental and physical conditions. This study highlights the distribution of healthcare encounters and factors associated with increased use to support development of tailored housing and support services.
To start, there were some factors associated with lower use of health services. Black participants were less likely to use physician services than white participants. For instance, the rate of physician visits was 50% lower for Black participants in the general homeless cohort and 32% lower in the cohort with a mental illness. They were also less likely to use ED services or be admitted to a non-psychiatric inpatient unit. The impact of discrimination toward racialized groups in healthcare can contribute to limited access to adequate healthcare and poor health outcomes.28 Specifically, it has been noted that implicit bias by healthcare providers and societal resistance to race-focused health policies contribute to these evident disparities in healthcare use.29,30 Structural racism in other societal systems and institutions have also been implicated as key contributors to homelessness within Black communities.31 While working to dismantle the systems of racism that perpetuate homelessness and discrimination in healthcare settings, it is also important to recognize that people from racialized groups may not benefit from strategies that use the healthcare system to intervene against homelessness.
Other predisposing factors, such as mental illness (psychotic disorder), problematic alcohol and drug use, criminal behavior, and victimization are associated with higher rate of emergency department visits. Notably, these associations were strong in both the cohort with a mental illness and the general homeless cohort. Interventions that leverage the emergency department as a point of contact should incorporate a trauma-informed, multi-disciplinary approach to housing and support services. Not only do people experiencing homelessness experience physical trauma due to violence related injury,32 but they also report adverse childhood experiences and ongoing trauma from housing instability and mistreatment.33 Trauma-informed care recognizes that the past traumatic experiences of people who present to the emergency department can impact how they receive care.34 This approach is based on a set of guiding principles for healthcare organizations and providers to improve their understanding of trauma and ability to recognize and respond to signs of trauma while mitigating risk of re-traumatization.35
For people with psychotic illnesses, support services should consider access to psychiatric treatment and other services such as intensive case management or assertive community treatment, as described in the At Home/Chez Soi protocol.14 Similarly, people with substance use disorders could benefit from tailored community-led programs that focus on harm reduction over abstinence. Harm reduction strategies aim to minimize substance-related harm by providing safe and low-barrier access to services.36,37 Providers of Housing First models of care also integrate a harm reduction lens when working with people who use substances. Client-provider relationships and building trust are integral to provision of effective care and housing supports.38 Finally, some people who have experiences with the criminal justice system may require legal or employment services, depending on the nature of their police contact, arrest, or incarceration. People experiencing homelessness may also require legal representation for other unmet needs related to housing (evictions, foreclosures) or parental rights (child support).39 It is important for all services to ensure patient-centered care is rooted in informed choice.
The Housing First intervention has been shown to reduce the number of days spent in hospital and associated costs within the first 24 months; however, the evidence for reductions in emergency department visits is conflicting.40 Over the long term, it has been suggested that Housing First plus assertive community treatment may reduce emergency department visits and length of hospital stay for participants with high mental health needs; however, similar findings were not observed for participants with moderate mental health needs who received Housing First plus intensive case management supports.41 Despite limited and conflicting evidence for reductions in emergency department use following these interventions, Housing First is a promising intervention that has demonstrated benefit to the health and well-being of people experiencing homelessness.42,43
Enabling factors such as regular source of care and past year acute mental and non-mental health care were associated with elevated use of acute services. It is important to note that the use of acute services is not an inherently negative outcome. Hospital services are a necessary part of the health system; however, the goal should be to minimize the need for acute services by promoting adequate treatment and management of chronic health conditions and providing adequate housing and support services. Research suggests that multidisciplinary, tailored approaches to primary care can improve health outcomes.44 Past year acute mental and non-mental health care were also strong determinants of acute service use. Inadequate discharge planning contributes to hospital re-admissions for both homeless and housed patients; yet, the risk of re-admission is higher for patients experiencing homelessness4 and even more for those with mental illness.45
Finally, need factors such as poor perceived general health and chronic comorbidities were also associated with use of acute services, which suggests that interventions could incorporate tailored approaches to improve treatment and self-management of chronic diseases for people with complex healthcare needs. Given the extensive barriers that are documented for long-term management of chronic conditions,46 such strategies may include provision of healthier food options, storage facilities for medications, and access to primary care services.
There were a few differences in associations observed across the cohorts that warrant mention, specifically for psychotic disorders and problematic alcohol use. Psychotic disorders were associated with nearly 4 times higher risk of psychiatric hospitalization in the general homeless cohort and only 25% higher risk within the cohort with a mental illness (compared to non-psychotic disorders). Further, problematic alcohol use was associated with higher risk of psychiatric and non-psychiatric hospitalizations within the general homeless cohort only. These differences in strength of association may result from study eligibility criteria, such as the requirement for At Home/Chez Soi participants to have a mental illness with moderate or high need for mental health services. It is expected that the reference group (other mental illness) in this cohort still experienced more severe mental illness than most participants of the general homeless cohort due to the high prevalence of bipolar disorder (10.6%), mood disorders with psychotic features (eg, bipolar disorder, depression), and alcohol (28.9%) or substance dependence (37.9%) in the At Home/Chez Soi cohort.15 This likely contributed to a higher rate of psychiatric hospitalizations in the reference group (and a lower relative rate of hospitalizaitons) for the cohort with a mental illness than the general homeless cohort.
Strengths
The strength of this work centers on the ability to leverage survey data from 2 large cohorts of homeless adults linked with administrative health records. The simultaneous assessment of a cohort of homeless adults with mental illness and a general homeless cohort highlights some of the heterogeneity that exists among people with experiences of homelessness. Further, data linkage with administrative health records was able to overcome common limitations of reliance on self-report healthcare data or the limited individual characteristics captured in health administrative databases. While most studies focus on ED visits, this study also examined factors associated with the risk of hospitalization (psychiatric and non-psychiatric) and rate of physician visits, which provides a more comprehensive depiction of healthcare utilization patterns.
Limitations
There are also limitations that should be considered. First, participants were primarily recruited from shelters, hospitals, and meal programs. It is possible that the individuals enrolled in the studies were more connected to services than other individuals who were not enrolled in these studies. Further, the included sample were required to consent to participate in the initial study and to have their data linked with administrative records. They also needed to present a valid Ontario health card number to be included in this analysis. Therefore, these findings may not be representative of people who avoid participating in research studies or who are not eligible for provincial health coverage.
Second, to enable comparison across studies, mental illness was identified using administrative health records, which likely misclassified some individuals as not having any mental illness due to lack of healthcare encounters. For instance, it is notable that 20% of the cohort with a mental illness were inaccurately classified as not having a mental illness in administrative databases. In this cohort specifically, the Mini-International Neuropsychiatric Interview was used to as an alternative method to identify mental illness among the cohort with a mental illness based on DSM-IV criteria.47 This interview was not asked of the general homeless cohort, and it is likely that some participants were misclassified as not having mental illness.
Third, the use of administrative health records captures all health records attached to an individual’s health card. Approximately 1% to 2% of hospitalizations and ED visits recorded at ICES are not connected to a health card number.48-50 Therefore, the number of encounters may be underestimated. The physician services that were not covered by fee-for-service billings or did not require shadow billings (eg, community health centers) were not captured in these data. Further, many non-physician services are not captured with ICES data, including those delivered by social workers, psychologists, and other programs offered through community health centers.
Fourth, while the cohorts were relatively large, estimates for rare characteristics were imprecise. For instance, within the cohort with a mental illness, few participants were married or partnered (3%); therefore, this category was combined with widowed, separated, or divorced. In addition, few participants were currently employed (4%) which resulted in wide confidence intervals.
Finally, this study was conducted before the COVID-19 pandemic. People living in congregated living settings, such as homeless shelters, with limited access to hygiene supplies or ability to physically distance or self-isolate, experienced high transmissibility and prevalence of SARS-CoV-2 infection.51 High prevalence of chronic comorbidities, mental disorders and substance use was further expected to contribute to a disproportionate impact of COVID-19 on the health of people experiencing homelessness.52,53 Given the scope of our data, we are not able to comment directly on the impact of COVID-19 on healthcare utilization within our cohorts. However, the rapid shift from in-person to virtual primary care during the pandemic may have exacerbated existing disparities in access to care for people experiencing homelessness.
Conclusions
The development of effective healthcare-driven strategies to address homelessness should consider the distribution of healthcare utilization and the individual-level characteristics, behaviors, and health outcomes that contribute to elevated use of health services. There are different factors associated with use of health services within subgroups of people experiencing homelessness, such as people with a mental illness. Given the high prevalence of mental illness among people who are homeless, it is necessary to consider their unique needs when designing studies and interventions to provide support during health crises and reduce preventable healthcare utilization.
The importance of tailored and flexible strategies is supported by a clinical review and guidelines with recommendations for health providers who deliver medical care to people experiencing homelessness.54,55 These documents re-iterate the need for interdisciplinary approaches to housing and support services that are patient-centered and trauma-informed to meet individual needs. Other research has focused on how hospital practices can be improved to ensure safe transfers of care that minimize discharge into homelessness. Early coordination across multidisciplinary teams and use of intermediate step-down residential facilities were effective strategies; however, funding and access to supportive housing options may limit ability to implement these discharge schemes.56 Further, while the health system represents one area for intervention, people who do not access services will not benefit from tailored healthcare-driven strategies to support people who are homeless in these settings. Improving access to housing and increasing investment in support services for all people experiencing homelessness should remain the immediate priority.
Supplemental Material
Supplemental material, sj-docx-1-his-10.1177_11786329221127150 for Determinants of Hospital Use and Physician Services Among Adults With a History of Homelessness by Kathryn Wiens, Laura C Rosella, Paul Kurdyak, Simon Chen, Tim Aubry, Vicky Stergiopoulos and Stephen W Hwang in Health Services Insights
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). The At Home/Chez Study was supported by the Mental Health Commission of Canada, the MOH/MLTC (HSRF-259), and the Canadian Institute of Health Research (CIHR, MOP-130405 and FDN-167263). The Health and Housing in Transition study was supported by CIHR (MOP-86765 and HOA-80066). Parts of this material are based on information compiled and provided by the MOH/MLTC and the Canadian Institute for Health Information. The analyses, conclusions, opinions and statements expressed are solely those of the authors and do not reflect those of the funding or data sources.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: KW and SWH conceptualized the study. KW designed the study, analyzed the data, and wrote the manuscript with guidance from SWH, LCR, and PK. SC provided administrative data expertise. SWH, TA, VS were principal investigators of the Health and Housing in Transition (SWH, TA) and At Home Chez Soi studies (SWH, VS) and provided additional content expertise to this work. All authors have reviewed the final manuscript.
Research Ethics Approval: Ethics approval was obtained from the St. Michael’s Hospital Research Ethics Board (REB) for the Toronto study sites and the University of Ottawa REB for the Ottawa site of the Health and Housing in Transition Study. Ethics approval for this administrative data analysis was obtained from Unity Health (REB #18-186), formerly the St. Michael’s Hospital REB.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Aldridge RW, Story A, Hwang SW, et al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391:241-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5:e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hwang SW, Chambers C, Chiu S, et al. A comprehensive assessment of health care utilization among homeless adults under a system of universal health insurance. Am J Public Health. 2013;103:S294-S301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Laliberté V, Stergiopoulos V, Jacob B, Kurdyak P. Homelessness at discharge and its impact on psychiatric readmission and physician follow-up: a population-based cohort study. Epidemiol Psychiatr Sci. 2019;29:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wodchis WP, Austin PC, Henry DA. A 3-year study of high-cost users of health care. CMAJ. 2016;188:182-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Frankish CJ, Hwang SW, Quantz D. Homelessness and health in Canada: research lessons and priorities. Can J Public Health. 2005;96:S23-S29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hossain MM, Sultana A, Tasnim S, et al. Prevalence of mental disorders among people who are homeless: an umbrella review. Int J Soc Psychiatr. 2020;66:528-541. [DOI] [PubMed] [Google Scholar]
- 8. Omerov P, Craftman ÅG, Mattsson E, Klarare A. Homeless persons’ experiences of health- and social care: a systematic integrative review. Health Soc Care Community. 2020;28:1-11. [DOI] [PubMed] [Google Scholar]
- 9. Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001;285:200-206. [DOI] [PubMed] [Google Scholar]
- 10. Lin W-C, Bharel M, Zhang J, O’Connell E, Clark RE. Frequent emergency department visits and hospitalizations among homeless people with Medicaid: Implications for Medicaid expansion. Am J Public Health. 2015;105:S716-S722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002;92:778-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Loubière S, Tinland A, Taylor O, et al. Determinants of healthcare use by homeless people with schizophrenia or bipolar disorder: results from the French Housing First Study. Public Health. 2020;185:224-231. [DOI] [PubMed] [Google Scholar]
- 13. Zhang L, Norena M, Gadermann A, et al. Concurrent Disorders and health care utilization among homeless and vulnerably housed persons in Canada. J Dual Diagn. 2018;14:21-31. [DOI] [PubMed] [Google Scholar]
- 14. Goering PN, Streiner DL, Adair C, et al. The at home/Chez Soi trial protocol: a pragmatic, multi-site, randomised controlled trial of a housing first intervention for homeless individuals with mental illness in five Canadian cities. BMJ Open. 2011;1:e000323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hwang SW, Stergiopoulos V, O’Campo P, Gozdzik A. Ending homelessness among people with mental illness: the at home/Chez Soi randomized trial of a Housing First intervention in Toronto. BMC Public Health. 2012;12:787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Goering P, Veldhuizen S, Watson A, et al. National at Home/ Chez Soi Final Report. Mental Health Commission of Canada; 2014. [Google Scholar]
- 17. Hwang SW, Aubry T, Palepu A, et al. The health and housing in transition study: a longitudinal study of the health of homeless and vulnerably housed adults in three Canadian cities. Int J Public Health. 2011;56:609-623. [DOI] [PubMed] [Google Scholar]
- 18. To MJ, Palepu A, Aubry T, et al. Predictors of homelessness among vulnerably housed adults in 3 Canadian cities: a prospective cohort study. BMC Public Health. 2016;16:1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wiens K, Rosella LC, Kurdyak P, et al. Factors associated with higher healthcare costs in a cohort of homeless adults with a mental illness and a general cohort of adults with a history of homelessness. BMC Health Serv Res. 2021;21:555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wiens K, Rosella LC, Kurdyak P, Hwang SW. Patterns and predictors of high-cost users of the health system: a data linkage protocol to combine a cohort study and randomised controlled trial of adults with a history of homelessness. BMJ Open. 2020;10:e039966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273-1302. [PMC free article] [PubMed] [Google Scholar]
- 22. Zou G. A modified Poisson regression approach to prospective studies with binary Data. Am J Epidemiol. 2004;159:702-706. [DOI] [PubMed] [Google Scholar]
- 23. Kaufman JS. Statistics, adjusted statistics, and maladjusted statistics. Am J Law Med. 2017;43:193-208. [DOI] [PubMed] [Google Scholar]
- 24. Conroy S, Murray EJ. Let the question determine the methods: descriptive epidemiology done right. Br J Cancer. 2020;123:1351-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harrell FE. Regression Modeling Strategies [Electronic Resource] : With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. 2nd ed. Springer International Publishing; 2015. [Google Scholar]
- 26. SAS Institute Inc. SAS/STAT 14.1 User’s Guide. SAS Institute Inc; 2015. [Google Scholar]
- 27. SAS Institute Inc. SAS Software Version 9.4 [Computer Program]. SAS Institute Inc; 2013. [Google Scholar]
- 28. Lee C, Ayers SL, Kronenfeld JJ. The association between perceived provider discrimination, healthcare utilization and health status in racial and ethnic minorities. Ethn Dis. 2009;19:330-337. [PMC free article] [PubMed] [Google Scholar]
- 29. Shavers VL, Klein WM, Fagan P. Research on race/ethnicity and health care discrimination: where we are and where we need to go. Am J Public Health. 2012;102:930-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financ Rev. 2000;21:75-90. [PMC free article] [PubMed] [Google Scholar]
- 31. Paul DW, Knight KR, Olsen P, Weeks J, Yen IH, Kushel MB. Racial discrimination in the life course of older adults experiencing homelessness: results from the HOPE HOME Study. J Soc Distress Homeless. 2020;29:184-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Topolovec-Vranic J, Schuler A, Gozdzik A, et al. The high burden of traumatic brain injury and comorbidities amongst homeless adults with mental illness. J Psychiatr Res. 2017;87:53-60. [DOI] [PubMed] [Google Scholar]
- 33. Pope ND, Buchino S, Ascienzo S. “Just like Jail”: trauma experiences of older homeless men. J Gerontol Soc Work. 2020;63:143-161. [DOI] [PubMed] [Google Scholar]
- 34. Fischer KR, Bakes KM, Corbin TJ, et al. Trauma-informed care for violently injured patients in the emergency department. Ann Emerg Med. 2019;73:193-202. [DOI] [PubMed] [Google Scholar]
- 35. Substance Abuse and Mental Health Services Administration. SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- 36. Collins SE, Clifasefi SL, Nelson LA, et al. Randomized controlled trial of harm reduction treatment for alcohol (HaRT-A) for people experiencing homelessness and alcohol use disorder. Int J Drug Policy. 2019;67:24-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Parkes T, Matheson C, Carver H, et al. A peer-delivered intervention to reduce harm and improve the well-being of homeless people with problem substance use: the SHARPS feasibility mixed-methods study. Health Technol Assess. 2022;26:1-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kerman N, Polillo A, Bardwell G, et al. Harm reduction outcomes and practices in housing first: a mixed-methods systematic review. Drug Alcohol Depend. 2021;228:109052. [DOI] [PubMed] [Google Scholar]
- 39. Tsai J, Jenkins D, Lawton E. Civil Legal Services and medical-legal partnerships needed by the homeless population: a national survey. Am J Public Health. 2017;107:398-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tinland A, Loubière S, Boucekine M, et al. Effectiveness of a housing support team intervention with a recovery-oriented approach on hospital and emergency department use by homeless people with severe mental illness: a randomised controlled trial. Epidemiol Psychiatr Sci. 2020;29:e169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lachaud J, Mejia-Lancheros C, Durbin A, et al. The effect of a housing first intervention on acute health care utilization among homeless adults with mental illness: long-term outcomes of the at Home/Chez-Soi randomized pragmatic trial. J Urban Health. 2021;98:505-515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. O’Campo P, Stergiopoulos V, Nir P, et al. How did a Housing First intervention improve health and social outcomes among homeless adults with mental illness in Toronto? Two-year outcomes from a randomised trial. BMJ Open. 2016;6:e010581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Stergiopoulos V, Gozdzik A, Misir V, et al. Effectiveness of Housing First with intensive case management in an ethnically diverse sample of homeless adults with mental illness: a randomized controlled trial. PLoS One. 2015;10:e0130281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jego M, Abcaya J, Ștefan D-E, Calvet-Montredon C, Gentile S. Improving health care management in primary care for homeless people: a literature review. Int J Environ Res Public Health. 2018;15:309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lam CN, Arora S, Menchine M. Increased 30-Day emergency department revisits among homeless patients with mental health conditions. West J Emerg Med. 2016;17:607-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Merdsoy L, Lambert S, Sherman J. Perceptions, needs and preferences of chronic disease self-management support among men experiencing homelessness in Montreal. Health Expect. 2020;23:1420-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22-33, quiz 34-57. [PubMed] [Google Scholar]
- 48. Canadian Institute for Health Information. Data quality documentation ontario mental health reporting system. Published 2018-2019. Accessed August 3, 2020. https://secure.cihi.ca/free_products/omhrs-data-quality-2018-2019-report-en.pdf
- 49. Canadian Institute for Health Information. Data quality documentation discharge abstract database. Published 2018-2019. Accessed August 3, 2020. https://www.cihi.ca/sites/default/files/document/current-year-information-dad-2018-2019-en-web.pdf
- 50. Canadian Institute for Health Information. Data quality documentation national ambulatory care reporting system. Published 2018-2019. Accessed August 3, 2020. https://www.cihi.ca/sites/default/files/document/current-year-information-nacrs-2018-2019-en-web.pdf
- 51. Mohsenpour A, Bozorgmehr K, Rohleder S, Stratil J, Costa D. SARS-Cov-2 prevalence, transmission, health-related outcomes and control strategies in homeless shelters: systematic review and meta-analysis. EClinicalMedicine. 2021;38:101032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Health. 2020;5:e186-e187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Perri M, Dosani N, Hwang SW. COVID-19 and people experiencing homelessness: challenges and mitigation strategies. Can Med Assoc J. 2020;192:E716-E719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pottie K, Kendall CE, Aubry T, et al. Clinical guideline for homeless and vulnerably housed people, and people with lived homelessness experience. Can Med Assoc J. 2020;192:E240-E254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Andermann A, Bloch G, Goel R, et al. Caring for patients with lived experience of homelessness. Can Fam Physician. 2020;66:563-570. [PMC free article] [PubMed] [Google Scholar]
- 56. Cornes M, Aldridge RW, Biswell E, et al. Health Services and delivery research. Improving Care Transfers for Homeless Patients After Hospital Discharge: A Realist Evaluation. Southampton (UK): NIHR Journals Library; 2021. 10.3310/hsdr09170 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-his-10.1177_11786329221127150 for Determinants of Hospital Use and Physician Services Among Adults With a History of Homelessness by Kathryn Wiens, Laura C Rosella, Paul Kurdyak, Simon Chen, Tim Aubry, Vicky Stergiopoulos and Stephen W Hwang in Health Services Insights