Abstract
Background
Medical tourism has grown increasingly popular in the past few decades. Cosmetic surgery centers have developed in vacation locales, offering procedures at lower prices. However, surgeons and patients alike are often unprepared for management of complications after patients return to the USA. The aim of this study is to provide an overview of US cosmetic surgery tourism patients and the complications faced by US healthcare providers.
Methods
A systematic review was performed using the Web of Science, Cochrane, Embase, Scopus, and PubMed databases up to February 2022; included articles were full-text, English language, and reported complications of patients receiving postoperative care in the USA after cosmetic surgery abroad. Two independent reviewers performed screening for article eligibility with a 3rd for conflict resolution. Patient demographics, procedure characteristics, and outcomes were extracted and aggregated.
Results
Twenty studies were included, describing 214 patients. Most patients were female (98.1%, n = 210), middle-aged, and Hispanic. The most common destination country was the Dominican Republic (82.7%, n = 177) and the most common surgical procedure was abdominoplasty (35.7%, n = 114). Complications were mainly infectious (50.9%, n = 112) and required prolonged treatment periods often greater than two months, with high rates of hospitalization (36.8%) and surgical management (51.8%).
Conclusions
Cosmetic surgery tourism is a growing industry with adverse implications for the US healthcare system and patients themselves. This review aims to serve as a reference to prepare plastic surgeons for the scope of complications associated with cosmetic tourism and improve counseling to better prepare patients for the financial and health risks.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Keywords: Cosmetic surgery, Medical tourism, Plastic surgery, Surgery abroad, Complication, Body contouring
Introduction
The number of patients seeking medical care abroad, a practice called “medical tourism,” has grown dramatically in recent decades, to an over $100 billion market-value annually [1–3]. Historically, the direction of travel for medical care was from less-developed to wealthier nations, but that trend has reversed: patients from wealthy nations with high healthcare costs, including the USA, are now seeking discounted health services in lower-income countries, [4] and facilities in these destinations have expanded to meet the demand [2]. As elective procedures with often out-of-pocket costs, aesthetic surgeries are particularly disposed to medical tourism, and an entire subset of the industry has developed specifically to support cosmetic surgery tourism, affecting not only patients but also US physicians. Over 80% of American plastic surgeons report experience with patients who traveled abroad for cosmetic procedures, [5] and this number is expected to grow.Please check the edit made in the article title.This edit is appropriate
Patients are motivated to consider surgery abroad by perceived affordability [6, 7], shorter wait times, and familiarity with the host country [8]. Medical treatments can be a part of “packages,” in which the destination surgical center manages and arranges flights and hotel accommodations [9]. Aesthetic surgery centers are often built in desirable tourism destinations, offering elective procedures in vacation locales at discounted costs [10, 11]. But the vacation-like experience can be followed by costly complications when patients return home, with limited support from the original surgeon. While risk is inherent to all surgery, those risks may be amplified in countries with lenient regulations, limited preoperative counseling, and truncated postoperative care. Studies show that when patients seek care abroad, short stays and lack of follow-up lead them to seek treatment for complications back in their home country [12].
As aesthetic surgery tourism rapidly grows in popularity, more patients, physicians, and hospitals in the USA contend with these complications. But it is unclear just how many cosmetic tourism patients are treated in the USA for complications of surgery performed abroad, as well as the scope of complications or their treatment courses and costs. Incomplete medical records, uncommon bacterial infections [13], and unfamiliar surgical practices pose significant challenges for US physicians managing these complications while high costs pose an issue for the healthcare system as a whole [14].
In this study, we present a review of the literature on aesthetic surgery tourism complications treated by US physicians. Understanding the current landscape of cosmetic surgery tourism in the USA and pertinence to plastic surgery can help prepare American surgeons in the face of this growing trend, and help them prepare patients. In this review, we aim to characterize the patient population seeking cosmetic surgery abroad, as well as the scope of complications treated back home in the USA. We also evaluate the treatment course and outcomes of these patients.
Methods
Literature Search
A systematic review was performed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analyses statement (PRISMA) [15]. A comprehensive literature search of Web of Science, Cochrane, Embase, Scopus, and PubMed databases was conducted in February 2022. Keywords and Medical Subject Headings (MeSH) were used in a search strategy designed to capture the concepts of “cosmetic surgery” and “medical tourism.” For primary screening, two independent reviewers conducted title, abstract screening according to inclusion and exclusion criteria (see below). Relevant articles underwent full-text review. An independent third reviewer resolved conflicts at each stage of screening.
Only primary literature was reviewed. Articles were included if they were written in the English language, full-text, and reported complications of patients receiving postoperative care in the United States after undergoing aesthetic surgical procedures abroad. Articles reporting complications of domestic or non-cosmetic medical tourism procedures, as well as reviews and commentaries were excluded.
Outcomes and Analysis
The primary outcome of this study was type of complication reported. Secondary outcomes included patient demographics, location of surgery, type of procedures performed, and management of complications. Data extraction also included study characteristics. Complication and surgery categories are not mutually exclusive. The patients included in one study [6] were captured by another, larger study [16] and only counted once to avoid double-counting patients.
Results
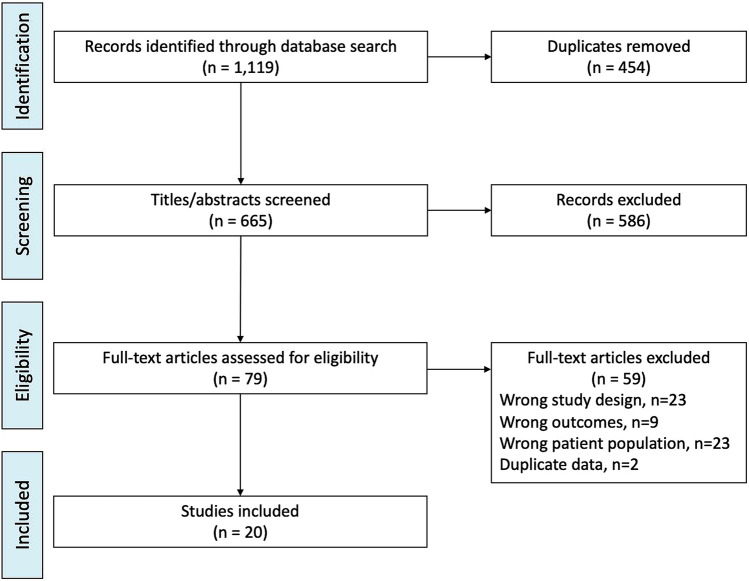
Literature search yielded 1,119 records (Fig. 1). After 454 duplicates were removed, a total of 665 articles were screened for inclusion/exclusion criteria. Ultimately 20 articles published from 2008 to 2021 were included, reporting complications of 214 unique patients.
Fig. 1.
Flowchart of search strategy and screening
An average of 12.55 patients were included in each article, and nine articles were single-patient case reports (Table 1). Of the patients with reported demographics, 97.1% were female, 1% were male and 1.5% were transgender females, with an age range of 19–64. BMI was infrequently reported; reported averages were 30.77kg/m2, [14] 29kg/m2, [6] 28.3kg/m2, [17] and 24.1 kg/m2[18]. Race and ethnicity were also infrequently reported. Patients reported Hispanic race, and Dominican, Colombian, Laotian, Puerto Rican, and Mexican ethnicities.
Table 1.
Demographics and study characteristics
| First Author, Year (refs) | Study type | No. of patients | No. of Female (%) | Age range, years | Age, years (SD) | BMI, kg/m2 (SD) | Race/Ethnicity |
|---|---|---|---|---|---|---|---|
| Adabi, 2020 [16] | Retrospective Review | 53 | 52 (98) | – | – | – | 100% Hispanic |
| Adabi 2017 [5]* | Retrospective Review | 42 | 41 (98) | 20–60 | Average 35 (11) | 29 (4.4) | – |
| Cai 2016 [20] | Retrospective Review | 2 | 2 (100) | 43, 46 | – | – | |
| Cusumano 2017 [27] | Retrospective Review | 4 | 4 (100) | 31–50 | Average 45.3 | – | – |
| Furuya 2008 [23] | Retrospective Review | 19 | 19 (100) | 19–57 | Median 33 | – | 100% Hispanic |
| Green 2017 [22] | Case Report | 1 | 1 (100) | 55 | – | – | |
| Guhan 2021 [35] | Retrospective Review | 2 | 2 (100) | 25, 36 | – | – | |
| Jhaveri 2020 [36] | Case Report | 1 | 1 (100) | 36 | – | – | |
| Kantak 2014 [18] | Case Report | 1 | 1 (100) | 64 | – | – | |
| Lee 2018 [17] | Retrospective Review | 10 | 10 (100) | 23–59 | Average 40 | – | – |
| Lee 2019 [26] | Case Report | 1 | 1 (100) | 49 | – | – | |
| Leto Barone 2020 [21] | Case Report | 1 | 1 (100) | 46 | – | – | |
| Ross 2018 [20] | Retrospective Review | 78 | 76 (97) | – | Average 43 | 28.3 | 63% Dominican 22% declined to respond 3% Colombian 9% Puerto Rican, 2% Laotian, 2% Mexican |
| Schnabel 2014 [25] | Retrospective Review | 19 | 19 (100) | 18–59 | – | – | 72% Dominican |
| Sharma 2016 [24] | Case Report | 1 | 1 (100) | 34 | – | – | |
| Singh 2016 [8] | Retrospective Review | 3 | 3 (100) | 29, 36, 44 | – | – | |
| Tran 2014 [11] | Case Report | 1 | 1 (100) | – | – | – | – |
| Venditto 2021 [14]** | Retrospective Review | 6 | 6 (100) | 19–47 | 32.7 | 30.77 | – |
| Zheng 2019 [31] | Retrospective Review | 10 | 8 (80) | 28–69 | – | – | 100% Hispanic |
| Zhitny 2020 [28] | Case Report | 1 | 1 (100) | 47 | 24.1 | – |
*All patients captured in reference 16, therefore excluded from analysis
**Demographics include domestic patients
Surgeries were performed in thirteen different countries (Table 2): 82.7% of the surgeries took place in the Dominican Republic, 4.2% in Mexico, and 3.7% in Colombia.
Table 2.
Countries where procedures were performed
| Country | Patients, n (%) |
|---|---|
| Dominican Republic | 177 (82.7) |
| Mexico | 9 (4.2) |
| Colombia | 8 (3.7) |
| Multiple/Unknown | 5 (2.3) |
| Brazil | 4 (1.9) |
| Venezuela | 3 (1.4) |
| Guatemala | 1 (0.5) |
| Puerto Rico | 1 (0.5) |
| Argentina | 1 (0.5) |
| China | 1 (0.5) |
| El Salvador | 1 (0.5) |
| Turkey | 1 (0.5) |
| Syria | 1 (0.5) |
| Panama | 1 (0.5) |
| Total | 214 (100.0) |
The most common surgical procedure was abdominoplasty (35.7%, n = 114), followed by liposuction (17.8%, n = 57), breast augmentation (16.3%, n = 52) and foreign body (free silicone or unknown substance) injection of any region (6.2%, n = 20) (Table 3). Surgical procedures were not mutually exclusive (Table 4).
Table 3.
Surgical procedures
| Procedure | No. Performed, n (%) |
|---|---|
| Abdominoplasty | 114 (35.7) |
| Liposuction | 57 (17.8) |
| Breast augmentation | 52 (16.3) |
| FOREIGN BODY INJECTIONS (ANY AREA) | 20 (6.2) |
| Breast reduction/Mastopexy | 18 (5.6) |
| Buttock augmentation/Brazilian Butt Lift (BBL) | 15 (4.7) |
| Fat grafting (Any Area) | 2 (0.6) |
| Face lift/Blepharoplasty | 2 (0.6) |
| Facial implants | 2 (0.6) |
| Breast implant exchange | 1 (0.3) |
| Rhinoplasty | 1 (0.3) |
| Unspecified procedures | 34 (10.6) |
| Total | 319 (100.0) |
BBL = Brazilian Butt Lift
Table 4.
Complication frequency
| Complication | Patients, n (%) |
|---|---|
| Infection* | 112 (50.9) |
| Pain | 17 (7.8) |
| Wound dehiscence/healing issues | 16 (7.3) |
| Granuloma | 14 (6.4) |
| Cosmetic Complaint | 12 (5.5) |
| Seroma | 10 (4.6) |
| Emboli (PE/DVT/Fat) | 7 (3.2) |
| Abscess | 6 (2.8) |
| Fat Necrosis | 6 (2.8) |
| Capsular contracture | 5 (2.3) |
| Unwanted implant | 4 (1.8) |
| Hernia | 3 (1.4) |
| Ruptured implant | 3 (1.4) |
| Drain issue | 1 (0.5) |
| Perforated bowel | 1 (0.5) |
| Pyelonephritis | 1 (0.5) |
| Total | 218 (100.0) |
*Defined as superficial surgical site infection and/or cellulitis
Complications
Overall reported complications included 112 cases of infection, 16 cases of wound dehiscence, 14 granulomatous complications, 12 cosmetic complaints, 10 seromas, and 7 thromboembolic events. Two patients had retained foreign objects, one gossypiboma [19] and one unspecified [17]. Thirteen papers reported exclusively infectious complications, including surgical site infection and abscess. Eleven studies reported non-tuberculous mycobacterial (NTM) infections [8, 16, 20–28], with treatments including extensive operative debridement and long-term antibiotics.
Treatments
The time from destination surgery to home clinical presentation varied across studies (Table 5). Notably, studies reporting mycobacterial infections [8, 16, 20–28] reported delays in diagnosis from initial presentation. Delays in diagnosis were also reported due to patients presenting to multiple emergency departments. One study [18] reported a patient had been refused evaluation by multiple plastic surgeons before undergoing surgical treatment.
Table 5.
Treatment courses
| Time from surgery to clinical presentation (weeks) | Duration of therapy (weeks) | Proportion Requiring Hospitalization | Proportion surgically treated | Average Cost | Insurance (n) | |
|---|---|---|---|---|---|---|
| Adabi 2020 [16] | – | – | – | 13/37 | $25,979 in conservative group, $15,083 in surgical | – |
| Adabi 2017 [5]* | Mean 7.2 +– 9.5 | – | 20/42 | 13/42 | $18,211 | 6 Medicaid |
| 3 Private | ||||||
| 1 Medicare | ||||||
| 1 Uninsured | ||||||
| Cai 2016 [20] | 3, 4 | 12, 24 | 2/2 | 2/2 | – | – |
| Cusumano 2017 [27] | 6, 8, 11, 12 | 38, 38, 28, 52 | – | 4/4 | – | – |
| Furuya 2008 [23] | Median 7 weeks to symptoms, 3 more weeks to presentation | Mean 24 | 5/8 | 15/19 | – | – |
| Green 2017 [22] | 12 | 44 | – | 1/1 | – | – |
| Guhan 2021 [35] | – | Mean 10 | – | 0/2 | – | – |
| Jhaveri 2020 [36] | 4 | 18 | 1/1 | 1/1 | – | – |
| Kantak 2014 [18] | 28 | – | – | 1/1 | – | – |
| Lee 2018 [17] | – | – | 4/9 | 8/9 | $98,835 | – |
| Lee 2019 [26] | 12 | 40 | – | 1/1 | – | – |
| Leto Barone 2020 [21] | 6 | 34 | 1/1 | 1/1 | – | – |
| Ross 2018 [20] | – | – | 12/78 | – | – | 48 Medicaid |
| 15 Private | ||||||
| 8 Medicare and MassHealth | ||||||
| 4 Massachusetts | ||||||
| Health Safety Net | ||||||
| 3 Uninsured | ||||||
| Schnabel 2014 [25] | – | – | 14/19 | – | – | – |
| Sharma 2016 [24] | 3 | 28 | 1/1 | 1/1 | – | – |
| Singh 2016 [8] | 3, 3, 4 | Mean 12 | – | 3/3 | – | – |
| Tran 2014 [11] | 1 | – | – | 1/1 | $77,693.50 | – |
| Venditto 2021 [14]** | – | – | 1/1 | 1/1 | $154,700.79 | 6 Private |
| 6 Medicaid | ||||||
| 4 Uninsured | ||||||
| Zheng 2019 [31] | 1–25 years | – | 1/1 | 8/10 | – | 9 Medicaid or dual Medicaid/Medicare |
| 1 Medicare | ||||||
| 1 Private | ||||||
| 1 Uninsured | ||||||
| Zhitny 2020 [28] | 2 | 8 | – | 1/1 | – | – |
*Two domestic patients included in insurance breakdown
**Details only reported on one international patient
36.8% of patients required hospital admission for treatment. One study examined average length of stay in conservatively managed infections versus surgically managed infections, and found the length was lower in the surgical group although statistical significance was not assessed (8.8 vs 13.4 days) [29].
Overall, 51.8% of patients with reported treatment courses required operative management, including debridement, implant removal, foreign body removal, breast reconstruction, and ventral hernia repair. Undesired cosmetic outcomes included deformity [30], dissatisfaction with cosmesis [31], and significant scarring [32, 33].
The average duration of therapy across the studies was consistently longer than 2 months, with some patients requiring ongoing treatments for up to a year [34]. Many of the long treatment courses were due to repeated operative debridement or long-term antibiotic therapy. Adverse antibiotic reactions were reported in six studies [20, 21, 23, 28, 35, 36] and included ototoxicity, peripheral neuropathy, severe leukopenia, hyperpigmentation, and nephrotoxicity. Complications of these antibiotic treatments included severe GI distress and hearing impairment, as well as indirect costs of long-term intravenous infusions.
Costs of Treatment and Insurance Coverage
When reported, costs of complication management ranged from $15,083 (average) to $154,700 (single patient) (Table 5). Insurance information was available for 117 patients: 59% had Medicaid, 21% had commercial, 9% had Medicare and 11% were uninsured. One patient reported loss of home due to financial strain [37].
Discussion
Medical tourism, the practice of patients seeking medical services abroad, is rapidly becoming more popular [2], with increasing impact on US patients and physicians. The internet has facilitated this practice by enabling patients to access information about foreign hospitals, and delivering advertisements for discounted aesthetic surgical procedures [4]. It is yet to be seen how the COVID-19 pandemic and widespread shutdown of elective procedures in the USA may have influenced interest in cosmetic tourism in the USA, but early analysis from Ireland found increased interest in elective surgery abroad during these shutdowns [1]. As the number of patients seeking care abroad grows, so does the number of returning patients presenting to US providers with complications. Aesthetic surgery abroad renders the purported benefits of confidentiality and decreased costs [4] at the expense of unavailable records, less stringent health standards, and non-optimal care. For US physicians, the impact of management and costs of complications after the patient is home remains an open question. There is limited understanding regarding the range of complications treated by US physicians and the impact on patients. In our survey of the literature, we found most domestic patients seeking cosmetic surgery abroad are middle-aged, Hispanic females, traveling to the Dominican Republic. The most commonly performed procedures are abdominoplasty, liposuction, and breast augmentation, and the most common complications are by far infectious. The treatment course for most of these patients is prolonged, often requiring hospitalization and surgical management.
Many complications reviewed in this work were infectious (50.9%, n=112). Infection after surgery abroad is a well-known phenomenon [8]. Mycobacterial infections in particular are a notable complication [38], as they are rarely seen in the United States but have become more common with medical tourism. Insufficient sterilization of surgical instruments [39] and contaminated tap water [22] have been suggested as causes in the destination countries. Appropriate diagnosis can be challenging for US physicians to make due to lack of familiarity with the signs and symptoms and poor growth on routine cultures, which can delay care [40]. Mycobacterial infections are particularly challenging to treat in immunodeficient patients, who can have disseminated disease, and pregnant women who cannot take certain antibiotics [41]. The treatment itself can involve prolonged, high-intensity antibiotic regimens with adverse effects, as seen in the range of antibiotic side effects reported above. The authors of this review see this as a concerning issue, as results suggest this population is of child-bearing age. Besides the infectious, many morbid complications were reported in this review including fat emboli, thromboembolic events, and surreptitiously placed implants. 6.4% of the patients captured in our review presented with silicone granulomas, likely from free silicone injections, known to be dangerous and illegal in the USA [42]. Seven embolic complications were also reported. Notably in this population, patients often board a flight just days after a surgical procedure, a known hypercoagulable state.
The patients captured in this review most commonly traveled to the Dominican Republic for surgery. While other recent review studies have similarly found many patients underwent cosmetic surgery in the Dominican Republic [8, 13, 43], this country is not always identified as a popular destination for cosmetic tourism [2, 44]. The top identified countries for global cosmetic procedures identified in a 2008 Deloitte study were Brazil, Medico, India, and Thailand. Mexico and Brazil represented 4.2% and 1.9% of our captured countries, respectively. And more recently, the annual 2020 International Society for Aesthetic Plastic Surgery (ISAPS) Global Survey found Americans were the most frequent foreign cosmetic surgery patients in Brazil, Colombia, Mexico, and Russia [44]—the Dominican Republic was not mentioned. While the absolute volume of surgery performed in this country may be small as compared to much larger nations, 80% of plastic surgery patients in the Dominican Republic were medical tourists as of 2005 [45]. The Joint Commission International is an independent organization that accredits international institutions meeting qualifications with the goal of healthcare quality and patient safety. There are no such accredited institutions in the Dominican Republic.
The population in our review included only American departure patients and mostly captured patients who traveled to Central and South America. Other studies examining residents of Europe and Australia have found reports of procedures performed in Asian countries [46–48]. An analysis of NHS medical tourism patients found that while distance, cost, expertise, and treatment availability were important factors in deciding where to go, the biggest influence was personal networks including the internet and personal recommendations [49]. A study in this review found that patients often return to their country of ethnicity [17] and another found that patients in their study knew an average of five family members or friends that had gone abroad for a procedure [6]. While race and ethnicity were rarely reported for patients in this review, most were of Hispanic ethnicity.
The majority of patients in this review required surgical management of their complications, and the average duration of treatment was over two months in all studies. An overall theme of the papers in this review is that patients who underwent early, more radical treatments did better in the long term, with lower readmission rates and hospital length of stay [16, 20, 28]. This may have been due to the nature of the reviews: many were series of patients with mycobacterial infections which required extensive operative debridement. The prolonged treatment courses and surgical management required may have driven the high treatment costs reported: five studies reported costs, all in the tens of thousands of dollars. Most patients captured in this study were insured by Medicaid or uninsured, which has implications for the US healthcare system. One study reporting mean costs of domestic and international medical tourism complications reported a mean cost per patient of $26,657, with physicians retaining only 9% of billed charges [14]. Cost analyses of medical tourism complications among UK patients found an average cost in the €5000–7000 range per patient, significantly lower [48, 50].
Patients interest in cosmetic surgery abroad is reported to be high, [7] motivated by lower cost, reduced wait time, and availability of any procedure regardless of FDA approval. But the downsides are apparent in our results, which demonstrate how medical tourism complications can cause severe complications, extended treatment periods, disfigurement, and financial ruin. A patient captured in this review called her surgery and complication the “worst experience of [her] life,” and a patient survey in the same study found most patients would not go abroad for surgery again. However, we acknowledge that the patients captured in our review are a small subset of all cosmetic tourism patients, capturing only those patients who experienced complications. This leaves an open question around patient satisfaction of the overall population. A series of 460 international patients receiving cosmetic surgery at a private practice in Cartagena, Colombia were asked about their satisfaction, and results showed that 98.2% responded that they would refer the surgery center to friends and family [51]. Studies like this one may encourage patients to feel safer when considering surgery abroad. But while some facilities may have safer practices, others can be the source of many complications [23], and no resources exist to help patients differentiate higher quality offshore destinations from unsafe facilities. Also, the surveys in this single-institution study were administered after the “final postoperative appointment,” which limits generalizability as many patients who travel for cosmetic medical tourism receive no postoperative care whatsoever from the operating surgeon [52].
There are several limitations of this study. First, the aggregated results could only be reported with granularity allowed by the primary literature. Additionally, many of the studies captured are individual case reports, which may not be generalizable. Additionally, the patients captured by this review may not be representative of cosmetic tourism patients overall, as we only included patients who experienced complications. This review also did not address domestic medical tourism, or medical tourism involving patients traveling from non-US countries. Both of these practices are an important part of this global phenomenon, but outside the scope of this review.
We hope this review sheds light on the landscape of medical tourism complications in the USA, and some of the key points of concern: high morbidity for patients, high costs for the US healthcare system, and challenging management for treating physicians. Patients return to the USA with complications and may be unprepared for the limited postoperative care, risks of complications, financial burden of postoperative management back in the USA, and lack of legal recourse [53]. An abdominoplasty may be less than half the cost abroad as compared to the USA [4], but the risks are unknown to patients. Patients even sometimes return with drains in [17], presumably to be managed by an unaware US physician. In a survey of patients by Ross et al., despite experiencing complications, some patients returned to their original surgeon and suffered from additional complications due to a second procedure [17]. This indicates that while patient awareness and appropriate counseling are important, introduction of guidelines may be a necessary course of action. It is the authors’ opinion that the prevalence of this phenomenon is likely underestimated by the literature. And the complications of the current boom of medical tourists, such as silicone emboli, may not be apparent for many years. There may be clinics that routinely have complications or perform dangerous procedures such as silicone injection, but lack of a feedback system prevents this from being known. Therefore we propose a national or international reporting system could be the next step, to understand the true scope of the issue, as well as inform patients. But until that happens, further publishing of medical experiences, as well as legal and ethical perspectives is invaluable.
Conclusions
US plastic surgeons treat a range of complications from cosmetic surgical procedures performed abroad, with potentially devastating outcomes. Life-threatening infections, thromboembolic events, significant scarring, antibiotic reactions, and financial devastation are all possible consequences of these procedures. We hope that by characterizing the scope and impact of these complications this review can help prepare surgeons and patients for the issues associated with cosmetic tourism.
Funding
The authors declare that they have no funding.
Declarations
Conflict of interest
JPF is a consultant for BD, Gore, AbbVie, Integra, and Baxter. JPF has received grant funding from the National Institutes of Health (NIH), Plastic Surgery Foundation (PSF), and the Institution for Translational Medicine and Therapeutics at the University of Pennsylvania.
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murphy D, Lane O’Neill B, Dempsey MP. COVID-19 and cosmetic tourism: a google trends analysis of public interests and the experience from a tertiary plastic surgery centre. J Plast Reconstr Aesthetic Surg. 2022;25:1. doi: 10.1016/j.bjps.2022.01.040. [DOI] [PubMed] [Google Scholar]
- 2.Kreckley P, Underwood H. Medical tourism. Consumers in search of Value. Published online 2008. doi:10.1580/1080-6032(2001)012[0066:MT]2.0.CO;2
- 3.Smith RD, Chanda R, Tangcharoensathien V. Trade in health-related services. Lancet. 2009;373:593–601. doi: 10.1016/S0140. [DOI] [PubMed] [Google Scholar]
- 4.Lunt N, Smith R, Exworthy M, Stephen T, Horsfall D, Mannion R. Medical Tourism: Treatments , Markets and Health System Implications: scoping review. Dir Employment, Labour Soc Aff. Published online 2011:1-55. http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Medical+Tourism+:+Treatments+,+Markets+and+Health+System+Implications+:+scoping+review#0
- 5.Melendez MM, Alizadeh K. Complications from international surgery tourism. Aesthetic Surg J. 2011;31(6):694–697. doi: 10.1177/1090820X11415977. [DOI] [PubMed] [Google Scholar]
- 6.Adabi K, Stern CS, Weichman KE, et al. Population health implications of medical tourism. Plast Reconstr Surg. 2017;140(1):66–74. doi: 10.1097/PRS.0000000000003459. [DOI] [PubMed] [Google Scholar]
- 7.Nassab R, Hamnett N, Nelson K, et al. Cosmetic tourism: Public opinion and analysis of information and content available on the internet. Aesthetic Surg J. 2010;30(3):465–469. doi: 10.1177/1090820X10374104. [DOI] [PubMed] [Google Scholar]
- 8.Singh M, Dugdale CM, Solomon IH, et al. Rapid-growing mycobacteria infections in medical tourists: Our experience and literature review. Aesthetic Surg J. 2016;36(8):246–253. doi: 10.1093/asj/sjw047. [DOI] [PubMed] [Google Scholar]
- 9.Turner L. “Medical tourism” and the global marketplace in health services: US patients, international hospitals, and the search for affordable health care. Int J Heal Serv. 2010;40(3):443–467. doi: 10.2190/HS.40.3.d. [DOI] [PubMed] [Google Scholar]
- 10.Connell J. Medical tourism: sea, sun, sand and surgery. Tour Manag. 2006;27(6):1093–1100. doi: 10.1016/j.tourman.2005.11.005. [DOI] [Google Scholar]
- 11.Tran BAP, Kludt N, Wong MS. The cost of medical tourism: Penny-wise and pound-foolish. Plast Reconstr Surg. 2014;133(6):908–909. doi: 10.1097/PRS.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 12.Pereira RT, Malone CM, Flaherty GT. Aesthetic journeys: a review of cosmetic surgery tourism. J Travel Med. 2018;25(1):1–8. doi: 10.1093/jtm/tay042. [DOI] [PubMed] [Google Scholar]
- 13.Padilla P, Ly P, Dillard R, Boukovalas S, Zapata-Sirvent R, Phillips LG. Medical tourism and postoperative infections: a systematic literature review of causative organisms and empiric treatment. Plast Reconstr Surg. 2018;142(6):1644–1651. doi: 10.1097/PRS.0000000000005014. [DOI] [PubMed] [Google Scholar]
- 14.Venditto C, Gallagher M, Hettinger P, et al. Complications of cosmetic surgery tourism: case series and cost analysis. Aesthetic Surg J. 2021;41(5):627–634. doi: 10.1093/asj/sjaa092. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Adabi K, Stern CS, Kinkhabwala CM, et al. Early Surgical management of medical tourism complications improves patient outcomes. Plast Reconstr Surg. 2020;145(5):1147–1154. doi: 10.1097/PRS.0000000000006728. [DOI] [PubMed] [Google Scholar]
- 17.Ross KM, Moscoso AV, Bayer LR, Rosselli-Risal L, Orgill DP. Plastic surgery complications from medical tourism treated in a US academic medical center. Plast Reconstr Surg. 2018;141(4):517–523. doi: 10.1097/PRS.0000000000004214. [DOI] [PubMed] [Google Scholar]
- 18.Zhitny VP, Iftekhar N, Caravella P, Young JP, Zide B, Stile F. Abdominal flap necrosis and wound dehiscence following a medical tourist tummy tuck. Case Rep Surg. 2020;2020:1–4. doi: 10.1155/2020/8819102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kantak N, Reish R, Salvin S, Lin S. Gossypiboma: an approach to diagnosis in the era of medical tourism. Plast Reconstr Surg. 2014;133:443e–444e. doi: 10.1097/01.prs.0000438499.85598.53. [DOI] [PubMed] [Google Scholar]
- 20.Cai SS, Chopra K, Lifchez SD. Management of mycobacterium abscessus infection after medical tourism in cosmetic surgery and a review of literature. Ann Plast Surg. 2016;77(6):678–682. doi: 10.1097/SAP.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 21.Leto Barone AA, Grzelak MJ, Frost C, et al. Atypical mycobacterial infections after plastic surgery procedures abroad: a multidisciplinary algorithm for diagnosis and treatment. Ann Plast Surg. 2020;84(3):257–262. doi: 10.1097/SAP.0000000000002061. [DOI] [PubMed] [Google Scholar]
- 22.Green DA, Whittier S, Greendyke W, Win C, Chen X, Hamele-Bena D. Outbreak of rapidly growing nontuberculous mycobacteria among patients undergoing cosmetic surgery in the Dominican republic. Ann Plast Surg. 2017;78(1):17–21. doi: 10.1097/SAP.0000000000000746. [DOI] [PubMed] [Google Scholar]
- 23.Furuya EY, Paez A, Srinivasan A, et al. Outbreak of Mycobacterium abscessus wound infections among “lipotourists” from the United States who underwent abdominoplasty in the Dominican Republic. Clin Infect Dis. 2008;46(8):1181–1188. doi: 10.1086/529191. [DOI] [PubMed] [Google Scholar]
- 24.Sharma P, Guillamet LJ V, Miljkovic G. Atypical Mycobacterial Infection after Abdominoplasty Overseas: A Case Report and Literature Review. Case Rep Infect Dis. Published online 2016. doi:10.1155/2016/3642567 [DOI] [PMC free article] [PubMed]
- 25.Schnabel D, Gaines J, Nguyen DB, et al. Notes from the field: rapidly growing nontuberculous Mycobacterium wound infections among medical tourists undergoing cosmetic surgeries in the Dominican Republic--multiple states, March 2013-February 2014. MMWR Morb Mortal Wkly Rep. 2014;63(9):201-202. http://www.pubmedcentral.nih.gov/articlerender.fcgi? [PMC free article] [PubMed]
- 26.Lee JC, Morrison KA, Maeng MM, Ascherman JA, Rohde CH. Financial implications of atypical mycobacterial infections after cosmetic tourism: is it worth the risk? Ann Plast Surg. 2018;81(3):269–273. doi: 10.1097/SAP.0000000000001563. [DOI] [PubMed] [Google Scholar]
- 27.Lee RA, Wigmore R. A case of lipotourism-associated multidrug-resistant Mycobacterium abscessus infection. J Glob Infect Dis. 2019;11(2):83–85. doi: 10.4103/jgid.jgid. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cusumano LR, Tran V, Tlamsa A, et al. Rapidly growing Mycobacterium infections after cosmetic surgery in medical tourists: the Bronx experience and a review of the literature. Int J Infect Dis. 2017;2017(63):1–6. doi: 10.1016/j.ijid.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 29.Adabi K, CS S, CM K,, et al. Early surgical management of medical tourism complications improves patient outcomes. Plast Reconstr Surg. 2020;145:1147–1154. doi: 10.1097/PRS.0000000000006728. [DOI] [PubMed] [Google Scholar]
- 30.Bap T, Kludt N. The cost of medical tourism: penny-wise and pound-foolish? Plast Reconstr Surg. 2014;133:908. doi: 10.1097/PRS.0000000000000195. [DOI] [PubMed] [Google Scholar]
- 31.Zheng C, Quentzel J, Brust JCM. Complications of silicone cosmetic procedures among medical tourists from the Bronx, New York: A retrospective analysis. J Clin Aesthet Dermatol. 2019;12(10 PG-24-28):24-28. https://www.embase.com/search/results?subaction=viewrecord&id=L2004831900&from=export NS - [PMC free article] [PubMed]
- 32.Ss C, Chopra K. Management of mycobacterium abscessus infection after medical tourism in cosmetic surgery and a review of literature. Ann Plast Surg. 2016;77:678–682. doi: 10.1097/SAP.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 33.Frost C, et al. Atypical mycobacterial infections after plastic surgery procedures abroad: a multidisciplinary algorithm for diagnosis and treatment. Ann Plast Surg. 2020;84:257–262. doi: 10.1097/SAP.0000000000002061. [DOI] [PubMed] [Google Scholar]
- 34.Lr C, Tran V, Tlamsa A, et al. Rapidly growing Mycobacterium infections after cosmetic surgery in medical tourists: the Bronx experience and a review of the literature. Int J Infect Dis. 2017;63:1–6. doi: 10.1016/j.ijid.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 35.Guhan SM, O’Connor DM, Gunasekera NS, Avram AS, Hoang MP, LaChance AH. Granuloma formation secondary to surreptitiously placed silicone. Dermatol Surg. 2021;47(6):849–851. doi: 10.1097/DSS.0000000000002630. [DOI] [PubMed] [Google Scholar]
- 36.Jhaveri VV, Singhal D, Riedel S, Rowley CF, Nathavitharana RR. Surgical cure of clarithromycin resistant Mycobacterium chelonae breast implant infection: a case report and review of the literature. J Clin Tuberc Other Mycobact Dis. 2020;21:100183. doi: 10.1016/j.jctube.2020.100183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.JC L, KA M, MM M, JA A, CH R. Financial Implications of Atypical Mycobacterial Infections After Cosmetic Tourism: Is It Worth the Risk? Ann Plast Surg. 2018;81: 269-273. doi:10.1097/SAP.0000000000001563 [DOI] [PubMed]
- 38.Centers for Disease Control and Prevention (CDC). Nontuberculous mycobacterial infections after cosmetic surgery--Santo Domingo, Dominican Republic, 2003-2004. MMWR Morb Mortal Wkly Rep. 2004;53(23):509. Accessed May 5, 2022. https://pubmed.ncbi.nlm.nih.gov/15201844/ [PubMed]
- 39.Rapidly growing mycobacterial infection following liposuction and liposculpture--Caracas, Venezuela, 1996-1998. MMWR Morb Mortal Wkly Rep. 1998;47(49):1065-1067. Accessed May 5, 2022. https://pubmed.ncbi.nlm.nih.gov/9879630/ [PubMed]
- 40.Paez A, Srinivasan A, et al. Outbreak of Mycobacterium abscessus wound infections among “lipotourists” from the United States who underwent abdominoplasty in the Dominican Republic. Clin Infect Dis. 2008;46:1181–1188. doi: 10.1086/529191. [DOI] [PubMed] [Google Scholar]
- 41.Singhal D, Riedel S. Surgical cure of clarithromycin resistant Mycobacterium chelonae breast implant infection: A case report and review of the literature. J Clin Tuberc Other Mycobact Dis. 2020;21:100183. doi: 10.1016/j.jctube.2020.100183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leonardi NR, Compoginis JM, Luce EA. Illicit cosmetic silicone injection: a recent reiteration of history. Ann Plast Surg. 2016;77(4):485–490. doi: 10.1097/SAP.0000000000000756. [DOI] [PubMed] [Google Scholar]
- 43.Raggio BS, Brody-Camp SA, Jawad BA, Winters RD, Aslam R. Complications associated with medical tourism for facial rejuvenation: a systematic review. Aesthetic Plast Surg. 2020;44(3):1058–1065. doi: 10.1007/s00266-020-01638-w. [DOI] [PubMed] [Google Scholar]
- 44.Hackworth S. ISAPS International Survey on Aesthetic/Cosmetic Procedures Performed in 2011. Published online 2011:1-11
- 45.Corderi V. Plastic surgery tourism? Dateline NBC. https://www.nbcnews.com/id/wbna7222253. Published March 18, 2005.
- 46.Schlarb D, Idelevich EA, Krause-Bergmann A, Stollwerck P. Successful interdisciplinary radical treatment of Mycobacterium fortuitum infection in a lipotourist from Germany after abdominoplasty in Turkey. New Microbes New Infect. 2015;8:21–23. doi: 10.1016/J.NMNI.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yau B, Lang C, Plas F, Sawhney R. Mycobacterium Abscessus Abscess Post-thread Facial Rejuvenation Procedure. Eplasty. 2015;15:ic19. Accessed May 5, 2022. /pmc/articles/PMC4392889/ [PMC free article] [PubMed]
- 48.Miyagi K, Auberson D, Patel AJ, Malata CM. The unwritten price of cosmetic tourism: an observational study and cost analysis. J Plast Reconstr Aesthetic Surg. 2012;65(1):22–28. doi: 10.1016/j.bjps.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 49.Hanefeld J, Lunt N, Smith R, Horsfall D. Why do medical tourists travel to where they do? the role of networks in determining medical travel. Soc Sci Med. 2015;124:356–363. doi: 10.1016/J.SOCSCIMED.2014.05.016. [DOI] [PubMed] [Google Scholar]
- 50.Henry N, Abed H, Warner R. The ever-present costs of cosmetic surgery tourism: a 5-year observational study. Aesthetic Plast Surg. 2021;45(4):1912–1919. doi: 10.1007/S00266-021-02183-W/TABLES/2. [DOI] [PubMed] [Google Scholar]
- 51.Campbell A, Restrepo C, Navas G. Patient Satisfaction with Medical Tourism: A Review of 460 International Plastic Surgery Patients in Colombia. Plast Reconstr Surg - Glob Open. Published online 2021:1-5. doi:10.1097/GOX.0000000000003230 [DOI] [PMC free article] [PubMed]
- 52.Birch J, Caulfield R, Ramakrishnan V. The complications of ‘cosmetic tourism’ – an avoidable burden on the NHS. J Plast Reconstr Aesthetic Surg. 2007;60(9):1075–1077. doi: 10.1016/J.BJPS.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 53.Franzblau LE, Chung KC. Impact of medical tourism on cosmetic surgery in the United States. Plast Reconstr Surg. 2013;1(7):1–7. doi: 10.1097/GOX.0000000000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]