Abstract
We sought to assess COVID-19 vaccination rates, as well as attitudes and beliefs towards the vaccine, of patients in a Spanish-speaking student-run free clinic in Columbus, Ohio. A cross-sectional study was performed. Surveys were distributed to all individuals over 18 years who presented to La Clínica Latina between July, 2022 and September, 2022. A convenience sample was used: patients in the waiting room and their accompanying family members or friends were invited to participate. Subjects were excluded if under the age of 18 or over the age of 75, or if non-Spanish speaking. Of the 158 individuals who agreed to participate in our study, 146 responded to the question regarding vaccination status, revealing 90.4% of respondents had received a COVID-19 vaccination. Most respondents learned about the vaccine from social media (26.4%) or television (22.7%). The majority of participants sought answers to questions surrounding the vaccine by asking their doctor (49.1%). The most common reason among unvaccinated participants for not undergoing vaccination was fear of an adverse reaction to the vaccine (n = 11). We found that a large proportion (90.4%) of individuals seeking care at a Spanish-speaking free clinic were vaccinated against COVID-19. Our study also provides perspective on the means of health knowledge acquisition and behaviors in this predominantly Latinx patient population in central Ohio. We can utilize our results to optimize and tailor clinic services and initiatives for COVID-19 boosters to meet the needs of this community.
Keywords: COVID-19, Free clinic, Spanish-speaking, Latinx, Hispanic
Introduction
Numerous studies have demonstrated the presence of vaccine hesitancy in the Latinx or Hispanic (hereafter: Latinx) population in the United States [1–5]. These trends have persisted throughout the introduction and administration of a COVID-19 vaccine: Latinx individuals are less willing than White individuals to receive a COVID-19 vaccine and are more likely to delay receiving the vaccine. [6–9] General mistrust of vaccines and fear of infection accounted for the most prominent association with vaccine hesitancy [10]. One study found that age was the salient factor associated with discrepancies in vaccine hesitation: more younger adults (age 18–49) preferred to “wait and see” if they would receive vaccination compared to older Latinx adults over the age of 50 who intended to get vaccinated “as soon as they can.” [11]
SARS-CoV-2 has disproportionately impacted the Latinx population in the United States with infection rates, hospitalization rates, and COVID-19-related mortality rates significantly higher among Latinx populations when compared with non-Latinx White people (with similar rates of case fatality) [12–14]. Specifically in Ohio, individuals identifying as Latinx had a COVID-19 case rate twice that of White, Non-Hispanic individuals. [15]
A myriad of reasons explains why the Latinx population in the United States was (and is still currently) at a particularly increased risk of acquiring SARS-CoV-2. Latinx individuals are more likely to hold jobs deemed “essential,” increasing the risk and probability of COVID-19 exposure, particularly when industries did not provide employees with proper personal protective equipment [16, 17]. As Macias Gil et al. point out, the Latinx population is overrepresented in critical industries, “with a quarter of [Latinx individuals] working in key service occupations (eg., ensuring food supply for the general population).” [18] This distribution of employment contributes to an existing disparity in the ability to telecommute: only 16.2% of this population held jobs that allowed them to work from home, compared to 31.4% of their non-Latinx counterparts [18]. Latinx individuals in the United States also endure a higher health burden due to comorbid conditions, such as obesity, diabetes, and renal disease, which puts them at higher risk for severe outcomes if infected with COVID-19 [19]. In addition, Latinx individuals may live in multigenerational homes, making social distancing practices more difficult [18]. Other factors documented throughout the pandemic contributing to the higher disease burden of COVID-19 in Latinx patients than non-Hispanic Whites include higher rates of being uninsured, concerns related to immigration status, language and cultural barriers, and an established mistrust in the healthcare system. [14, 18, 20]
La Clínica Latina is a student-run free clinic in Columbus, Ohio, entirely operated by a multidisciplinary, interprofessional team of volunteers, which includes licensed medical providers, medical students, other healthcare professional students, and undergraduate students. Our patient population predominantly consists of Spanish-speaking patients who frequently encounter barriers to the established healthcare system, such as lack of insurance, fear of documentation status and subsequent discrimination, low-socioeconomic status and subsequent lack of financial resources, or language barriers and an associated shortage of interpreters. These obstacles, and more, cause difficulties for these vulnerable patients in navigating the medical system, and they are more likely to experience adverse health outcomes due to low health literacy [21, 22]. Therefore, in addition to providing acute and chronic care, La Clínica Latina strives to implement sustainable preventative healthcare programs and is continually re-assessing and engaging with our patient population to align initiatives with current needs and unmet gaps.
As the COVID-19 pandemic continues and new variants of the SARS-CoV-2 virus emerge, additional boosters of a COVID-19 vaccine are recommended [23–25]. Consequently, there is an ongoing and critical necessity to identify vaccination rates and understand the rationales behind potential vaccine hesitancy in the Latinx population to effectively and directly tailor public health efforts to address them. Our study aimed to assess COVID-19 vaccination rates, as well as attitudes and beliefs towards the vaccine, among a Latinx population utilizing our student-run free clinic.
Materials and Methods
Our study was deemed exempt by The Ohio State University Institutional Review Board. We conducted a cross-sectional study between July 2022 and September 2022. All individuals over 18 years old receiving medical care at La Clínica Latina were invited to complete the survey. Family members and friends accompanying patients were also invited to participate. Subjects were excluded if under 18 years old, over 75 years old, or non-Spanish speaking.
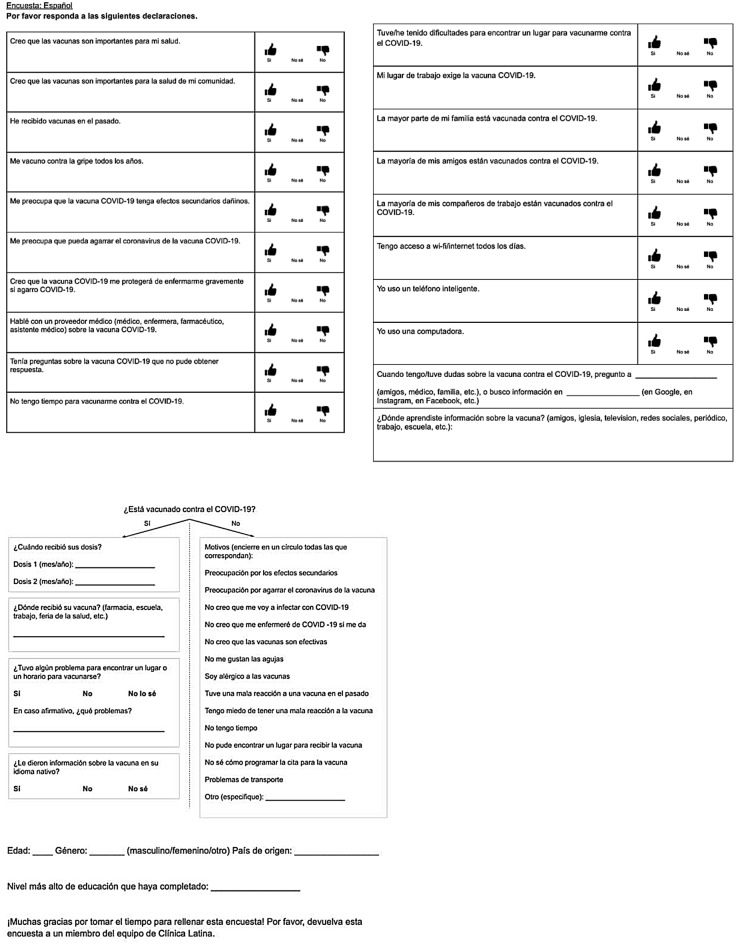
The survey was adapted from the CDC’s Vaccine Confidence Survey Question Bank [26]. It included questions regarding knowledge, beliefs, and access to the COVID-19 vaccine, potential barriers to receiving a COVID-19 vaccine, or reasons for not receiving a vaccine, if applicable (Fig. 1). The first part of the survey consisted of a list of statements to which the participant was asked to indicate “yes,” “no,” or “I don’t know” based on their level of agreement with each statement. Additionally, there were some questions with free text answers. The survey then proceeded with a yes/no question regarding the participant’s COVID-19 vaccination status. Patients self-defined vaccination status by selecting “yes” or “no” in response to “Are you vaccinated against COVID-19?” The survey also requested data regarding the patient’s age, gender, and country of origin. Survey data were kept confidential and no personally identifiable information was collected. Participation in the survey was voluntary. Participants were made aware that the decision of whether or not to complete the survey, as well as the answers provided on the survey, would remain confidential and would have no impact whatsoever on the patient’s clinical care received at La Clínica Latina.
Fig. 1.
Survey that was administered to participants
Completed printed forms were collected after survey administration by study personnel and were stored safely in a locked cabinet only accessible to study personnel. Data were entered into a password-protected Excel document and descriptive data analysis was conducted. We performed subgroup analyses by separating patients by vaccination status to better understand this population’s attitudes and beliefs towards the COVID-19 vaccine and by age group, gender, and country of origin. We used Excel to analyze data and calculate descriptive statistics.
Results
Between July 2022 and September 2022, 158 individuals agreed to participate in our study. Of the 158 participants, 146 completed the question regarding vaccination status. There were 132 participants (90.4%) who received a COVID-19 vaccine and 14 (9.6%) who had not received a COVID-19 vaccine. Of the patients who were vaccinated, 55 (43.0%) were male and 74 (57.8%) were female; of the patients who were not vaccinated, 5 (35.7%) were male and 9 were female (64.3%). The median age of patients vaccinated was 45.1 years; the median age of patients who were not vaccinated was 40.3 years. A breakdown of the distribution of the respondents’ ages is presented in Table 1.
Table 1.
Baseline characteristics of participants by vaccination status
| Baseline characteristics | Vaccinated against COVID-19 | |
|---|---|---|
| Yes (n = 132) n (%) |
No (n = 14) n (%) |
|
| Age group (years) | ||
| 18–29 | 15 (11.7) | 3 (21.4) |
| 30–44 | 47 (36.72) | 4 (28.6) |
| 45–59 | 49 (38.3) | 5 (35.7) |
| 60–69 | 17 (13.3) | 2 (14.3) |
| 70–75 | 2 (1.6) | 0 (0) |
| Total # responses | 130 | 14 |
| Median age (years) | 45.1 [18, 73] | 40.3 [21, 62] |
| Gender | ||
| Male | 55 (43.0) | 5 (35.7) |
| Female | 74 (57.8) | 9 (64.3) |
| Total # responses | 129 | 14 |
| Country of origin | ||
| Mexico | 39 (31.0) | 9 (64.3) |
| Venezuela | 34 (27.0) | 0 (0) |
| El Salvador | 16 (12.7) | 4 (28.6) |
| Colombia | 9 (7.1) | 0 (0) |
| Dominican Republic | 5 (4.0) | 0 (0) |
| Guatemala | 4 (3.2) | 1 (7.1) |
| Honduras | 4 (3.2) | 0 (0) |
| Brazil | 3 (2.4) | 0 (0) |
| Ecuador | 3 (2.4) | 0 (0) |
| Puerto Rico | 3 (2.4) | 0 (0) |
| Spain | 2 (1.6) | 0 (0) |
| Argentina | 1 (0.8) | 0 (0) |
| Costa Rica | 1 (0.8) | 0 (0) |
| Cuba | 1 (0.8) | 0 (0) |
| Nicaragua | 1 (0.8) | 0 (0) |
| USA | 1 (0.8) | 0 (0) |
| Total # responses | 127 | 14 |
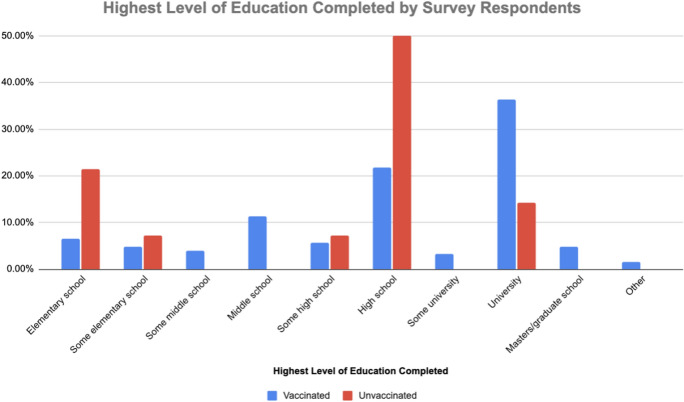
Respondents who participated in our study were from a total of 16 countries. Those vaccinated against COVID-19 indicated they originated from 16 countries; those not vaccinated against COVID-19 originated from 3 countries. The distribution of respondents’ countries of origin is presented in Table 1. The median highest level of schooling for vaccinated patients was university (n = 45, 36.3%). For unvaccinated respondents, the median highest level of education attained was high school (n = 7, 50.0%) (Fig. 2).
Fig. 2.
Highest level of education completed by survey respondents
The most common location where patients received their COVID-19 vaccine was a pharmacy (58.5%, n = 65), followed by a health fair (20.0%), La Clínica Latina (9.2%), doctor’s office other than La Clínica Latina (9.2%), health department (1.5%), and shelter (1.5%).
When asked where patients gathered information about the COVID-19 vaccine, 26.4% of respondents indicated they used social media, 22.7% from TV, and 13.0% from friends. The remaining methods respondents used to acquire information regarding the COVID-19 vaccine and the respective distribution is presented in Fig. 3. When asked whom patients seek if they have/had questions regarding the COVID-19 vaccine, respondents most commonly ask their doctor (49.1%), followed by utilizing the internet/google (21.8%), asking their friends (14.5%), asking their family members (10.9%), and asking their questions to other sources (3.6%) (Fig. 4).
Fig. 3.
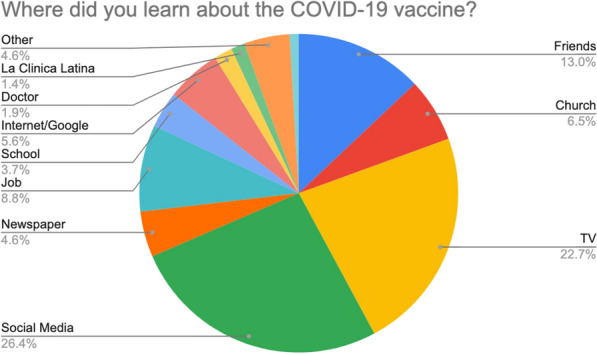
Sources of information from which respondents learned about a COVID-19 vaccine
Fig. 4.
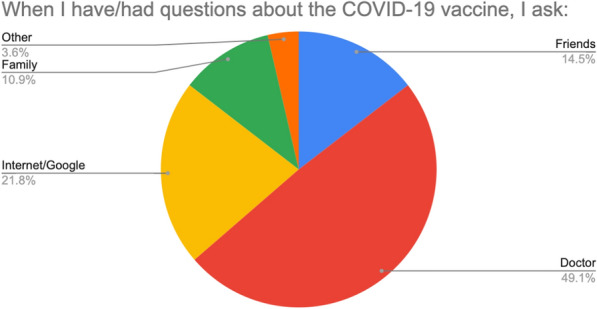
Sources utilized by patients to answer their questions about the COVID-19 vaccine
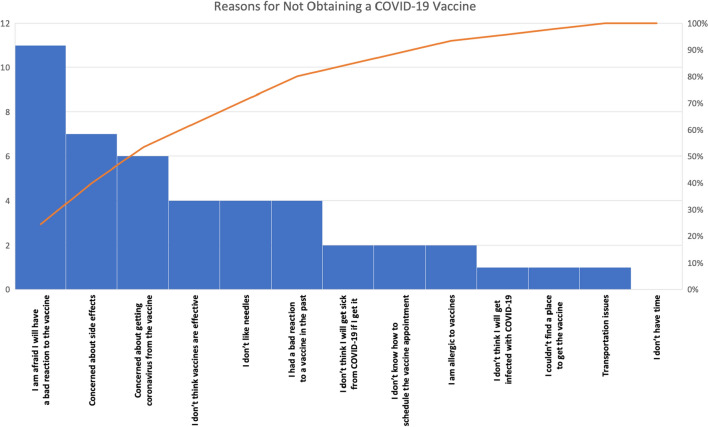
Among patients who have not received a COVID-19 vaccine, the most commonly indicated reason for not being vaccinated was: “I am afraid I will have a bad reaction to the vaccine” (n = 11), followed by “Concerned about side effects” (n = 7) (Fig. 5).
Fig. 5.
Reasons for not obtaining a COVID-19 vaccine
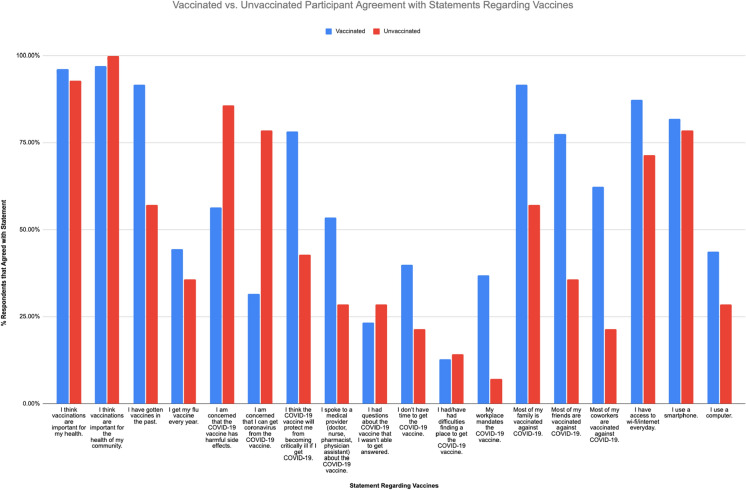
Results from the 18-item survey on vaccine beliefs and hesitancy are illustrated in Fig. 6. Of note, vaccinated participants reported a higher vaccination rate among their family members, friends, and coworkers compared to unvaccinated respondents. Among vaccinated participants, 91.7% reported most of their family members are vaccinated against COVID-19, 77.4% reported most of their friends are vaccinated, and 62.4% reported most of their coworkers are vaccinated. Whereas, among unvaccinated participants, 57.1% reported most of their family members are vaccinated against COVID-19, 35.7% reported most of their friends are vaccinated, and 21.4% reported most of their coworkers are vaccinated.
Fig. 6.
Results from the 18-item survey about vaccine beliefs and attitudes
Discussion
Our study assessed the COVID-19 vaccination rates of Latinx individuals receiving healthcare at a free clinic. Our results showed that the overwhelming majority (90.4%) reported receiving a COVID-19 vaccine at the time of our study. These results surpass the current COVID-19 vaccination rates of Latinx patients in Franklin County and Ohio, which are 63.81 and 64.14%, respectively. [27] Furthermore, our results contradict previous studies that demonstrated hesitancy and unwillingness to receive the COVID-19 vaccine within the Latinx population. [28, 29]
Consistent with previous studies, the participants in our study who were not vaccinated against COVID-19 (9.8%) cited reasons primarily centered around fears of side effects and reactions to the vaccine or becoming sick with COVID-19 due to the vaccine [30, 31]. Only one respondent indicated not knowing where to obtain the vaccine and transportation, which has been cited as a barrier to vaccination for Latinx individuals [32, 33]. Although not explicitly examined in our study, it is essential to recognize that Latinx patients’ hesitancy toward the COVID-19 vaccine may stem from and be perpetuated by structural racism and systemic disparities in the United States, as well as patients’ previous experiences with healthcare system abuse in their country of origin. [20, 29, 32]
In our study, more participants vaccinated against COVID-19 indicated most of their family, friends, and co-workers had also received a COVID-19 vaccine than participants who had not received a COVID-19 vaccine (Fig. 6). Latinx patients with a positive vaccine experience are likely to share information with those around them and even actively reach out and recommend the COVID-19 vaccine to their family and friends, which may contribute to the high proportion of vaccinated patients in our study [34–36]. This highlights the influence of family and friends on health behaviors and the potential to employ social networks as public health strategies. [37]
When asked about sources of information regarding the COVID-19 vaccine, social media platforms were indicated as the most common (26.4%), followed by TV (22.7%), similar to the results of El-Mohandes, et al. [38] Social media is commonly used worldwide for a plethora of reasons, and seeking healthcare information is one of many reasons [39–41]. Previous studies have raised concerns regarding the accuracy of COVID-19 and other healthcare information that is disseminated on social media and the lack of verification by healthcare professionals [42–44]. In addition, some studies indicate that relying on social media and other forms of media for information is negatively associated with willingness to receive the COVID-19 vaccine, and these individuals are more likely to demonstrate vaccine-hesitancy [43, 45]. Considering this, we should encourage providers to regularly engage patients to ask questions about healthcare information acquired from social media. This strategy may effectively address misinformation and vaccine hesitancy since almost half (49.1%) of our participants indicated they sought answers from a doctor/healthcare provider for questions regarding the COVID-19 vaccine (Fig. 4).
Since a large proportion of the patient population served at La Clínica Latina is vaccinated against COVID-19, clinic initiatives can focus on CDC-recommended boosters, as well as other clinically-appropriate vaccines. Most participants received their COVID-19 vaccine from a pharmacy or health fair, and only 9.5% at La Clínica Latina; therefore, we can direct our efforts towards facilitating vaccinations for patients who prefer to utilize pharmacies and health fairs while continuing the current scale of La Clínica Latina vaccination services. This could be accomplished by providing patients with locations, times, and necessary steps to receive a COVID-19 booster, as well as assessing for potential barriers and working with patients to overcome them.
As previously discussed, social media is a primary source many of our patients use for information on the COVID-19 vaccine. Therefore, we can utilize La Clínica Latina’s social media platforms (Facebook, Instagram, etc.) to disseminate evidence-based, culturally-relevant information about COVID-19 boosters. Efforts to increase patients’ social media involvement and interactions with La Clínica Latina could involve the following: including social media handles on after-visit summaries given to patients, increasing the frequency of posting validated health information, partnering with other organizations and community pages to share medically sound information on their social media platforms (such as Columbus Latinx Facebook groups), and optimizing the clinic’s website for patients to access social media pages easily.
Limitations
As with any convenience sample, there is a risk of bias in our participant population. We attempted to mitigate this bias by opening the survey to individuals accompanying patients rather than patients alone. The cultural phenomenon of “respeto” and the possibility that participants felt inclined to participate out of respect for the clinic and its providers may also introduce bias [46]. Additionally, our survey relied on participant recall, posing the possibility of recall bias. Given the voluntary nature of the study, there is the possibility that self-selection bias influenced the decision whether to participate: patients who had not been vaccinated may have been less willing to engage in a survey related to vaccination status, while patients who were vaccinated may have been more likely to participate. Additionally, our survey intentionally did not collect protected health information to emphasize that participation is unrelated to clinical care and to preserve patients’ privacy. Therefore, we did not pursue efforts to verify positive self-reporting of a participant’s vaccination status, date(s), or location of vaccination, as this would identify the respondents. It is possible that patients self-reported “yes” in response to the question about vaccination status without having received the vaccine, or without having completed the vaccination series in full. In the future, it would be of interest to have study personnel verify positive self-reporters by requesting proof of vaccination in the form of CDC vaccination cards; however, this would compromise the anonymity of the survey.
By conducting this study at a single site, the population from which we selected participants is limited and may share similar viewpoints. Future directions include expanding this study to additional medical practices with Spanish-speaking populations, including clinics and hospitals alike.
A proportion of patients did not complete the survey in its entirety. Future directions for a survey-based project would include converting the paper survey to an online format such that participants are alerted of blank sections and have the opportunity to revisit and complete any missed questions.
Conclusion
Most of our survey respondents (90.4%) were vaccinated against COVID-19 at the time of data collection. It is reassuring that this vulnerable population is seeking and obtaining this important preventative healthcare measure, despite the significant barriers imposed upon them. Our study provides perspective on the means of health knowledge acquisition and behaviors regarding important and current health topics, such as vaccination, as well as barriers and concerns that our patients face when approaching these topics. The goal of La Clínica Latina is to reduce barriers for these patients and to provide the Latinx patient population of Central Ohio with optimal care. From this study, we can now optimize and tailor our preventative healthcare services and initiatives, such as COVID-19 vaccination boosters or other recommended vaccinations, to meet the needs of and fill gaps within this patient population.
Author Contributions
All authors contributed to the study conception and design. Material preparation was performed by TP, AS, SS, and KW. Data collection was performed by TP and AS. Data input was performed by HS and TW. Data analysis was performed by TP and AS. The first draft of the manuscript was written by TP and AS, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
No external funding was required for this study.
Data Availability
The data that support the findings of this study are available from the corresponding author upon request.
Code Availability
All statistical analyses for this study were performed using Microsoft Excel.
Declarations
Conflict of interest
The authors have no disclosures or conflicts of interest to report.
Ethical Approval
This study was deemed exempt by the Ohio State University Institutional Review Board (IRB) per institutional policy as STUDY2022E0517.
Consent to Participate
The following consent statements were read and provided to eligible participants prior to survey administration: English: We are inviting you to participate in a survey for research to better understand your views and perceptions about the COVID-19 vaccine. We want to better understand how our patients feel about the COVID-19 vaccine, and how many of our patients are vaccinated or unvaccinated, as well as reasons leading to each decision. This survey is completely voluntary. There are no negative consequences if you choose not to take it. Neither your decision to participate nor your answers to the questions on the survey will affect your clinical care or treatment at La Clínica Latina. If you decide to start the survey and change your mind, you may stop at any time. Spanish: Lo invitamos a participar en una encuesta de investigación para comprender mejor su punto de vista y percepciones sobre la vacuna COVID-19. Queremos comprender mejor cómo se sienten nuestros pacientes acerca de la vacuna contra el COVID-19 y cuántos de nuestros pacientes están vacunados o no, así como las razones que llevan a cada decisión. Esta encuesta es completamente voluntaria. No hay consecuencias negativas si elige no tomarlo. Ni su decisión de participar ni sus respuestas a las preguntas de la encuesta afectarán su atención clínica o tratamiento en La Clínica Latina. Si decide comenzar la encuesta y cambia de opinión, puede detenerla en cualquier momento.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alexandra Scheiber and Teresa B. Prinster shared first-authorship.
References
- 1.Boakye EA, Betelihem TB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: Racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Human Vaccines & Immunotherapeutics. 2017;11:2713–2722. doi: 10.1080/21645515.2017.1363133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindsay AC, Pineda JA, Valdez MJ, Torres MI, Granberry PJ. Central American immigrant parents’ awareness, acceptability, and willingness to vaccinate their adolescent children against human papillomavirus: A pilot cross-sectional study. International Journal of Environmental Research and Public Health. 2020;17(8):2869. doi: 10.3390/ijerph17082869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wooten KG, Wortley PM, Singleton JA, Euler GL. Perceptions matter: Beliefs about influenza vaccine and vaccination behavior among elderly white, black and Hispanic Americans. Vaccine. 2012;30(48):6927–6934. doi: 10.1016/j.vaccine.2012.08.036. [DOI] [PubMed] [Google Scholar]
- 4.Khodadadi AB, Redden DT, Scarinci IC. HPV vaccination hesitancy among Latina immigrant mothers despite physician recommendation. Ethnicity & Disease. 2020;30(4):661–670. doi: 10.18865/ed.30.4.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moran MB, Chatterjee JS, Frank LB, et al. Individual, cultural and structural predictors of vaccine safety confidence and influenza vaccination among Hispanic female subgroups. Journal of Immigrant and Minority Health. 2017;19(4):790–800. doi: 10.1007/s10903-016-0428-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. Journal of Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kricorian K, Turner K. COVID-19 vaccine acceptance and beliefs among black and Hispanic Americans. PLoS ONE. 2021;8:e0256122. doi: 10.1371/journal.pone.0256122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson HS, Manning M, Mitchell J, et al. Factors associated with racial/ethnic group-based medical mistrust and perspectives on COVID-19 vaccine trial participation and vaccine uptake in the US. JAMA Network Open. 2021;4(5):e2111629. doi: 10.1001/jamanetworkopen.2021.11629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Momplaisir FM, Kuter BJ, Ghadimi F, et al. Racial/ethnic differences in COVID-19 vaccine hesitancy among health care workers in 2 large academic hospitals. JAMA Network Open. 2021;4(8):e2121931. doi: 10.1001/jamanetworkopen.2021.21931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Willis DE, Andersen JA, Bryant-Moore K, et al. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clinical and Translational Science. 2021;14(6):2200–2207. doi: 10.1111/cts.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kearney, A., Lopes, L., & Brodie, M. (2021, January 14). Vaccine Hesitancy Among Hispanic Adults. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/vaccine-hesitancy-among-hispanic-adults/
- 12.De Ramos IP, Lazo M, Schnake-Mahl A, et al. COVID-19 outcomes among the Hispanic population of 27 large US cities, 2020–2021. American Journal of Public Health. 2022;112(7):1034–1044. doi: 10.2105/AJPH.2022.306809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review. Annals of Internal Medicine. 2021;174(3):362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baquero B, Gonzalez C, Ramirez M, Santos EC, Orneas IJ. Understanding and addressing latinx COVID-19 disparities in Washington State. Health Education & Behavior. 2020;47(6):845–849. doi: 10.1177/1090198120963099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohio Latino Affairs Commission. (2022, April 3). The Impact of COVID-19 on Ohio’s Hispanic/Latinx Communities. The State of Ohio. https://ochla.ohio.gov/wps/portal/gov/ochla/home
- 16.Zamarripa, R. & Roque, L. (2021, March 3). Latinos Face Disproportionate Health and Economic Impacts From COVID-19. Center for American Progress. https://www.americanprogress.org/article/latinos-face-disproportionate-health-economic-impacts-covid-19/
- 17.Axon, R., Bagenstose, K., & Chadde, S. (2020, June 6). Coronavirus outbreaks climb at U.S. meatpacking plants despite protections, Trump order. USA Today. https://www.usatoday.com/story/news/investigations/2020/06/06/meatpacking-plants-cant-shake-covid-19-cases-despite-trump-order/3137400001/
- 18.Macias Gil R, Marcelin JR, Zuniga-Blanco B, Marquez C, Mathew T, Piggott DA. COVID-19 pandemic: Disparate health impact on the Hispanic/Latinx population in the United States. Journal of Infectious Diseases. 2020;222(10):1592–1595. doi: 10.1093/infdis/jiaa474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Velasco-Mondragon E, Jimenez A, Palladino-Davis AG, et al. Hispanic health in the USA: A scoping review of the literature. Public Health Reviews. 2016;37:31. doi: 10.1186/s40985-016-0043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Page KR, Flores-Miller A. Lessons we’ve learned—Covid-19 and the undocumented latinx community. New England Journal of Medicine. 2021;384(1):5–7. doi: 10.1056/NEJMp2024897. [DOI] [PubMed] [Google Scholar]
- 21.Mas FS, Jacobson HE. Advancing health literacy among Hispanic immigrants: The intersection between education and health. Health Promotion Practice. 2019;20(2):251–257. doi: 10.1177/1524839918761865. [DOI] [PubMed] [Google Scholar]
- 22.Jacquez F, Vaughn L, Zhen-Duan J, Graham C. Health care use and barriers to care among Latino immigrants in a new migration area. Journal of Health Care for the Poor and Underserved. 2016;27(4):1761–1778. doi: 10.1353/hpu.2016.0161. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. (2022, September 1). CDC Recommends the First Updated COVID-19 Booster. U.S. Department of Health and Human Services. https://www.cdc.gov/media/releases/2022/s0901-covid-19-booster.html
- 24.Straten, K.V.D., Guerra, D., Gils, M.J.V., et al. (2022). Mapping the antigenic diversification of SARS-CoV-2. Doi:10.1101/2022.01.03.21268582
- 25.Burki TK. Omicron variant and booster COVID-19 vaccines. The Lancet Respiratory Medicine. 2022;10(2):e17. doi: 10.1016/S2213-2600(21)00559-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. (2021). Vaccine Confidence Survey Question Bank. U.S. Department of Health and Human Services. https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence/rca-guide/downloads/CDC_RCA_Guide_2021_Tools_AppendixD_Surveys-508.pdf
- 27.Ohio Department of Health. (2022). COVID-19 Vaccination Dashboard. The State of Ohio. https://coronavirus.ohio.gov/dashboards/covid-19-vaccine/covid-19-vaccination-dashboard
- 28.Dhanani LY, Franz B. A meta-analysis of COVID-19 vaccine attitudes and demographic characteristics in the United States. Public Health. 2022;207:31–38. doi: 10.1016/j.puhe.2022.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Siegel M, Critchfield-Jain I, Boykin M, et al. Racial/ethnic disparities in state-level COVID-19 vaccination rates and their association with structural racism. Journal Racial Ethnicity Health Disparities. 2021 doi: 10.1007/s40615-021-01173-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McFadden SA, Demeke J, Dada D, et al. Confidence and hesitancy during the early roll-out of COVID-19 vaccines among black, Hispanic, and undocumented immigrant communities: A review. Journal of Urban Health. 2022;99(1):3–14. doi: 10.1007/s11524-021-00588-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen KH, Srivastav A, Razzaghi H, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, September and December 2020. American Journal of Transplantation. 2021;21(4):1650–1656. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Migrant Clinicians Network. (2021, March 4). COVID-19 Vaccine for Refugees, Immigrants, and Migrants: Building Trust on the Fontilines. https://www.migrantclinician.org/blog/2021/mar/covid-19-vaccine-refugees-immigrants-and-migrants-building-trust-frontlines.html
- 33.Hamel, L., Lopes, L., Kirzinger, A., Sparks, G., Stokes, M., & Bodie, M. (2021, November 8). KFF COVID-19 Vaccine Monitor: Media and Misinformation. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-media-and-misinformation/
- 34.Wojcicki JM, Escobar M, Mendez AD, Martinez SM. Household and social characteristics associated with COVID-19 vaccine intent among Latino families in the San Francisco Bay Area. BMC Infectious Diseases. 2022;22(1):527. doi: 10.1186/s12879-022-07467-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kirzinger, A., Sparks, G., & Brodie, M. (2021, July 2013). KFF COVID-19 Vaccine Monitor: In Their Own Words, Six Months Later. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-in-their-own-words-six-months-later/
- 36.Marquez C, Kerkhoff AD, Naso J, et al. A multi-component, community-based strategy to facilitate COVID-19 vaccine uptake among Latinx populations: From theory to practice. PLoS ONE. 2021;16(9):e0257111. doi: 10.1371/journal.pone.0257111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hunter RF, de la Hayle K, Murray JM, et al. Social network interventions for health behaviours and outcomes: A systematic review and meta-analysis. PLoS Medicine. 2019;16(9):e1002890. doi: 10.1371/journal.pmed.1002890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.El-Mohandes A, White MT, Wyka K, et al. COVID-19 vaccine acceptance among adults in four major US metropolitan areas and nationwide. Science and Reports. 2021;11:21844. doi: 10.1038/s41598-021-00794-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen J, Wang Y. Social media use for health purposes: Systematic review. Journal of Medical Internet Research. 2021;23(5):e17917. doi: 10.2196/17917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Galvin AM, Garg A, Moore JD, Litt DM, Thompson EL. Quality over quantity: Human papillomavirus vaccine information on social media and associations with adult and child vaccination. Human Vaccines & Immunotherapeutics. 2021;17(10):3587–3594. doi: 10.1080/21645515.2021.1932219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smailhodzic E, Hooijsma W, Boonstra A, Langley DJ. Social media use in healthcare: A systematic review of effects on patients and on their relationship with healthcare professionals. BMC Health Services Research. 2016;16(1):442. doi: 10.1186/s12913-016-1691-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Human Vaccines & Immunotherapeutics. 2020;16(11):2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Al-Hasan A, Khuntia J, Yim D. Does seeing what others do through social media influence vaccine uptake and help in the herd immunity through vaccination? A cross-sectional analysis. Front Public Health. 2021;9:715931. doi: 10.3389/fpubh.2021.715931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crilly P, Jair S, Mahmood Z, et al. Public views of different sources of health advice: Pharmacists, social media and mobile health applications. The International Journal of Pharmacy Practice. 2018;27(1):88–95. doi: 10.1111/ijpp.12448. [DOI] [PubMed] [Google Scholar]
- 45.Piltch-Loeb R, Harriman NW, Healey J, et al. COVID-19 vaccine concerns about safety, effectiveness, and policies in the United States, Canada, Sweden, and Italy among unvaccinated individuals. Vaccines. 2021;9(10):1138. doi: 10.3390/vaccines9101138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Flores G. Culture and the patient-physician relationship: Achieving cultural competency in health care. Journal of Pediatrics. 2000;136(1):14–23. doi: 10.1016/s0022-3476(00)90043-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.
All statistical analyses for this study were performed using Microsoft Excel.