Achievements and challenges
Before the advent of modern medicine, childbirth carried extremely high risk of mortality, both maternal and perinatal (the period beginning at the 20–28th week of gestation and ending at 1–4 weeks after delivery). Fortunately, with advances in prenatal healthcare, the prevalence of maternal and perinatal mortalities has significantly reduced. A press conference held on May 30, 2022, by the National Health Commission of the People’s Republic of China, reviewed the major progress and achievements in Chinese maternal and child health over the past decade. It highlighted that the maternal mortality rate dropped to 161 per million in 2021, the lowest level in recorded history. However, gestational hypertension, postpartum hemorrhage, maternal infection, and other complications related to pregnancy continue to endanger pregnant women. Hence, there is a need to implement pragmatic measures to ensure the prolonged health of women during and after pregnancy.
Faced with the challenge of an aging population in China, the central government has advocated the “three-child policy” since 2021 to optimize the population structure. This policy also stressed the importance of maintaining optimal maternal health. The probability of birth defects, such as Down syndrome, neural tube malformation, and congenital heart disease, has been effectively controlled by popularizing the new-generation high-sensitivity prenatal screening tools. These include the “double-index method” to investigate cardiac murmurs and transcutaneous oxygen saturation for timely detection of congenital heart disease. However, the high occurrence of preterm births (e.g., ∼7.8% in China,1 ∼5.9% in Zhejiang2) is still a concern. Preterm birth can increase the risks of multiple birth defects, including extremely low birth weight, immature organ development, cerebral palsy, and mental retardation due to secondary infections.
Continued efforts
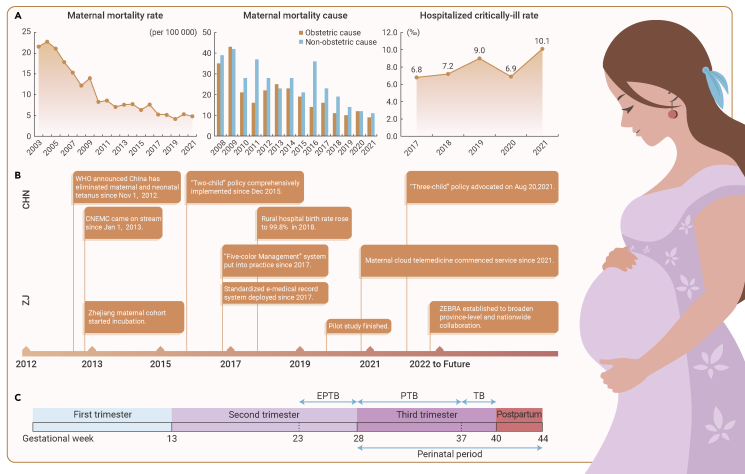
With its high economic and technological development, Zhejiang is a model province for maternal and child health security. Maternal mortality in Zhejiang (4.8/100,000 in 2021, Figure 1) is almost a quarter of the national average level (17.8/100,000 in 2019),1 partly due to the strict implementation of a hierarchical maternal healthcare system. To explore the intergenerational associations of congenital and developmental diseases by artificial intelligence-based multi-omics methodologies, the Children’s Hospital, School of Medicine, Zhejiang University launched the Zhejiang University Birth Cohort in early 2021, focusing on newborn prospective follow-up. Additionally, Zhejiang has taken multiple follow-up measures for high-risk pregnant women to ensure maternal and child health through all stages, from pregnancy and delivery to the postpartum period. However, efforts in protecting public health are never finished. The elimination of maternal risk is always the ultimate goal. Recent literature points out the impact of environmental exposures on maternal health, including but not limited to air pollutants, green spaces, and extreme temperatures.3, 4, 5 These hazards led to the 2022 establishment of the Zhejiang Environmental and Birth health Research Alliance (ZEBRA), under leadership from the Health Commission of Zhejiang Province, which aims to explore the associations between endogenous physiological factors, exogenous environmental factors, and maternal health.
Figure 1.
Chronicle of maternal health career in China and Zhejiang Province
(A) Recent progress on maternal health in Zhejiang Province.
(B) Milestones of the past decade. CNEMC, China National Environmental Monitoring Center; CHN, China; ZJ, Zhejiang Province.
(C) Division of maternal trimesters and definition of preterm birth. TB, term birth; PTB, preterm birth; EPTB, extreme preterm birth.
Standardized electronic medical records have been archived since 2017 in the Women’s Hospital, School of Medicine, Zhejiang University. Using these records, ZEBRA retrospectively traced pregnancy admission during 2017–2021 (∼0.1 million entries) and continues to register through the upcoming 5 years (>0.1 million) for prospective follow-up, to ultimately establish an ambidirectional cohort of at least 0.2 million pregnant women. The hospital administers the hierarchical maternal healthcare system at the province level, enabling the ZEBRA maternity cohort to represent pregnancy cases across two sub-provincial cities and nine prefecture-level cities.
Missions and commitments
At the cohort participant level, ZEBRA collects basic physical information (age, height, weight, etc.), sociodemographic information (occupation, education attainment, etc.), pregnancy and childbirth history (gravidity, parity, starting date of current pregnancy inferred by ultrasound, etc.), disease, surgery, and allergy history, as well as the results of the routine blood test, urinalysis, and oral glucose tolerance test. From the environmental exposure aspect, historical exposure levels to ambient air pollutants (particulate matters, nitrogen dioxide, ozone, etc.), organic pollutants (pesticides, phthalates, endocrine-disrupting chemicals, etc.), ambient air temperature (extreme high and low temperatures and the temperature range), and greenness can be assigned according to the address of the participant. A pilot study randomly sampled ∼6,000 patients during 2013–2017 and reported a positive association between preterm birth risks and ambient air pollution exposure.2 However, there is an adequate space for methodological correction and inference optimization, which will all be revised in new studies designed by ZEBRA.
Before being handed over to ZEBRA Data Mining Group for analysis, the cohort information will be anonymized by replacing the name, resident identification number, hospital medical record number, and other personal information of the patient, with a unique serial index only used among data analysts. Two PIs (i.e., H.Z.S. and X.B.) guarantee data transmission security and scientific research integrity. Studies on the ZEBRA cohort are approved by the ethics committee of Women’s Hospital, School of Medicine, Zhejiang University (IRB-20220189-R).
Target research questions
ZEBRA plans to answer the following major scientific questions. First, are the endogenous physiological features and exogenous maternal environmental exposures associated with complications of pregnancy, such as preterm birth? Second, do the endogenous and exogenous risk factors modify the effect of each other on the risk of developing pregnancy-related complications? Third, can the alterations in physiological and biochemical markers of pregnant mothers indicate any potential complication? Fourth, is it possible to predict the risks of pregnancy-related complications during the middle or early stages of pregnancy using routine clinical tests to ensure perinatal and newborn health? In the process of epidemiological analysis, ZEBRA promises to share periodic findings with China Cohort Consortium, as well as cohort study improving strategies suitable for Chinese economic development and folk customs.
There are still some limitations at this stage. First, the personal medical records of the participants lack the residence period of the current address, which compromises the feasibility of tracking longer-term (e.g., >10 years) environmental exposure. Second, a large proportion of records of mid-term pregnancy examination is seriously missing due to the low coverage of mid-term examination, and different hospital choices with delivery. The cross-hospital medical records for the same patients are expected to be matched in the following years. Third, individual lifestyle features are not available, including but not limited to dietary habits, sleeping patterns, intake of nutrients, supplements, and medicine, exercise frequency, etc. ZEBRA expects to collect these pieces of non-sensitive personal information with a mobile questionnaire for further risk factor screening.
Looking to the future
ZEBRA has resolved to provide evidence-based research conclusions on maternal health for the Chinese population, given that most of the high-quality cohort studies are established in the Western world. ZEBRA aspires to demonstrate a paradigm in the standardized management of electronic medical records for mother-child pairs, from provincial to national scale. Models optimized by data mining for screening risk prediction and risk factors can be instantly applied to newly admitted pregnant women, which will enhance maternal health risk assessment and update interactively with the inclusion of cohort participants. ZEBRA will also assume responsibility for the dissemination of maternal health research to the general public, with the hope that risks can be reduced as early as possible.
Perinatal health protection requires joint efforts, both familial and societal, which is a critical step for upholding gender justice. The health of women and children is the epitome of population health and reflects a country’s development. At present, multiple factors are suppressing birth rates among young people. However, gynecologists, physicians, nurses, and medical students still aim to provide the most professional and comprehensive life and healthcare services for women who wish to give birth. The medical and research community will ensure no one is left behind. Through the establishment of ZEBRA, Zhejiang is determined to contribute to realizing the "Healthy China 2030" vision as well as the United Nations’ Sustainable Development Goals (e.g., SDG3 in maternal and child health), and provide epidemiological evidence for global maternal and child healthcare by publishing high-quality research reports.
Acknowledgments
Special appreciations to Professor Weiguo Lu, director of the Key Laboratory of Women’s Reproductive Health (Hangzhou, Zhejiang Province); Dr. Yuanying Ma, deputy director of the Department of Maternal Healthcare, Women’s Hospital, School of Medicine, Zhejiang University; and Dr. Wei Xu, deputy director of the Maternal and Child Health Division, Health Commission of Zhejiang Province, for their comprehensive supports in the establishment of ZEBRA. Research receives funding from Zhejiang Province Health Innovative Talent Project (A0466) and International Cooperation Seed Program of Women's Hospital, Zhejiang University (GH2022B008-01).
Declaration of interests
The authors declare no competing interests.
Published Online: October 11, 2022
Contributor Information
Haitong Zhe Sun, Email: zs347@cam.ac.uk.
Xiaoxia Bai, Email: baixiaoxia@zju.edu.cn.
References
- 1.Qiao J., Wang Y., Li X., et al. A Lancet Commission on 70 years of women's reproductive, maternal, newborn, child, and adolescent health in China. Lancet. 2021;397:2497–2536. doi: 10.1016/S0140-6736(20)32708-2. [DOI] [PubMed] [Google Scholar]
- 2.Sun Z., Yang L., Bai X., et al. Maternal ambient air pollution exposure with spatial-temporal variations and preterm birth risk assessment during 2013-2017 in Zhejiang Province, China. Environ. Int. 2019;133:105242. doi: 10.1016/j.envint.2019.105242. [DOI] [PubMed] [Google Scholar]
- 3.Bekkar B., Pacheco S., Basu R., DeNicola N. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw. Open. 2020;3:e208243. doi: 10.1001/jamanetworkopen.2020.8243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang L., Shi S., Wu S., et al. Effects of greenness on preterm birth: a national longitudinal study of 3.7 million singleton births. Innovation. 2022;3:100241. doi: 10.1016/j.xinn.2022.100241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Y.Y., Li Q., Guo Y., et al. Ambient temperature and the risk of preterm birth: a national birth cohort study in the mainland China. Environ. Int. 2020;142:105851. doi: 10.1016/j.envint.2020.105851. [DOI] [PubMed] [Google Scholar]